-
Stroke is one of the main causes of mortality and long-term disability[1] and has become an important public health concern worldwide. Ischemic stroke accounted for nearly 87% of all strokes[2]. In recent years, obesity and C-reactive protein (CRP) levels have been investigated extensively with regard to risk of stroke and cardiovascular disease in populations[3-7]. CRP has been proven to be a sensitive systemic marker of endothelial inflammatory response; it is involved in the initiation and progression of atherosclerosis and is an important risk factor for ischemic stroke[8-11]. Assessment of CRP levels for patients with intermediate cardiovascular risk has been recommended by the American College of Cardiology Foundation[12, 13]. Obesity, defined as a body mass index (BMI) ≥ 30 kg/m2, is a modifiable risk factor for stroke[3] and has been found to be positively associated with a high CRP level[14]. Obesity, as defined by the increase in BMI, might not distinguish fat accumulation from muscle mass, although it is widely used as a measure of obesity[15]. A Body Shape Index (ABSI), a new anthropometric parameter, has been developed to evaluate obesity and can reflect more abdominal adiposity than BMI[16]. A study reported that ABSI might predict all-cause mortality independently of BMI in a large cohort of American adults[17, 18]. However, few studies have examined the combined effect between obesity defined by ABSI and CRP on the risk of ischemic stroke incidence. Hence, we investigated the cumulative effect of a combined ABSI and CRP status on the risk of ischemic stroke incidence among a Mongolian population in Inner Mongolia, China.
-
This prospective cohort study was conducted from June 2002 to July 2012 in Inner Mongolia, an autonomous region in north China. Thirty-two villages in 2 adjacent townships of Kezuohou Banner (county) and Naiman Banner were selected as study fields because they had the highest proportion of Mongolians living a traditional Mongolian lifestyle. The detailed methods for participant selection and investigation protocols have been reported previously[19]. In brief, there were a total of 3, 475 Mongolians aged 20 years and older who lived in 32 villages in 2 townships. Among them, 886 people were excluded for refusing to participate or for existing cardiovascular or endocrine diseases including hyper/hypothyroidism. A total of 2, 589 participants were included in the study. This study was approved by the Soochow University Ethics Committee. Written informed consent was obtained from all study participants.
-
Baseline data on the demographic characteristics, lifestyle risk factors, family history of cardiovascular disease (CVD), and medical histories of the participants were obtained using standard questionnaires given by trained staff. Cigarette smoking was defined as having smoked at least 1 cigarette per day for at least 1 year, and alcohol consumption was defined as consuming any type of alcoholic beverage containing at least 25 g alcohol per day on average for 1 year or more during the past few years. Three consecutive blood pressure (BP) measurements were taken for each participant in a seated position by trained staff using a mercury sphygmomanometer according to a standard protocol. The first and fifth Korotkoff sounds were recorded as systolic BP (SBP) and diastolic BP (DBP), respectively. The mean of the three BP measurements was used for data analyses. Hypertension was defined as SBP ≥ 140 mmHg, and/or DBP ≥ 90 mmHg, and/or use of antihypertensive medications in the last two weeks[20]. Body weight and height were measured by trained staff with participants wearing light clothing and no shoes. Weight in kilograms divided by the square of the height in meters was calculated as the body mass index (BMI) (kg/m2). Waist circumference (WC) was measured at the level of 1 cm above the umbilicus at the end of a normal expiration. ABSI was calculated according to the following formula: ABSI = WC/(BMI2/3 × height1/2); WC and height were expressed in meters.
Fasting blood samples were collected in the morning after all participants had been fasting for at least eight hours. Plasma and serum samples were all frozen at -80 ℃ before laboratory testing. A modified hexokinase enzymatic method was used to determine fasting plasma glucose (FPG) levels. Total cholesterol (TC), triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C) levels were measured enzymatically on a Beckman Synchrony CX5 Delta Clinical System (Beckman Coulter, Fullerton, CA, USA) using commercial reagents. Low-density lipoprotein cholesterol (LDL-C) level was calculated using the Friedewald equation for participants with TG levels less than 400 mg/dL. Serum CRP levels were assessed using an immunoturbidimetric assay on a Beckman Synchron CX5 Delta Clinical System with commercial reagents.
-
All participants were followed up from June 2002 to July 2012. The follow-up methods and outcome assessments have been previously described in detail[21]. In brief, the primary study outcome was the occurrence of ischemic stroke during the follow-up period. Participants who did not experience an ischemic stroke event, who died from other causes, or were lost to follow-up were not included in the analysis. The date of stroke incidence was defined as the endpoint date. Four county-level hospitals with modern diagnostic facilities including computed tomography (CT) and magnetic resonance imaging (MRI) provided residents in the study with medical services. After the baseline data were obtained, household surveys for all participants were conducted every two years to determine the incidence of ischemic stroke events. Trained staff interviewed either the participants or their relatives (if participants were dead or unable to communicate) and completed a questionnaire regarding their medical status. If a participant experienced a stroke event during the period since the last survey, the staff reviewed their hospital records including outpatient or admission records, the discharge summary, and especially CT or MRI scan results for confirmation. Stroke was defined as evidence of an acute disturbance in focal areas of the brain lasting for ≥ 24 h and thought to be due to intracranial hemorrhage or ischemia[22]. The participants diagnosed with ischemic stroke by head CT or MRI scans at a hospital were determined to have a positive study outcome.
-
In our study, the participants were categorized into 2 groups according to their ABSI levels: a low ABSI level [ABSI < 0.0837 (the bottom 3 quartiles)] and a high ABSI level [ABSI ≥ 0.0837 (the upper quartile)]. The participants were also categorized into 2 groups according to their CRP levels: a low CRP level [log CRP < 1.06 mg/L (the bottom 3 quartiles)] and a high CRP level [log CRP ≥ 1.06 mg/L (the upper quartile)]. Furthermore, all participants were divided into 4 groups: low ABSI/low CRP level, low ABSI/high CRP level, high ABSI/low CRP level, and high ABSI/high CRP level. Baseline characteristics were compared across all four groups. Continuous variables were expressed as mean ± standard deviation (SD) for normal distribution and as median (interquartile ranges) for skewed distribution; categorical variables were described as frequency (percent). The distributions of conventional risk factors were compared using analysis of variance for continuous variables with normal distribution, Kruskal-Wallis H tests for continuous variables with skewed distribution, and chi-squared tests for categorical variables. By adjusting for age, gender, cigarette smoking, alcohol drinking, FPG, hypertension status, family history of cardiovascular disease, TG, HDL-C, CRP (only adjusted in models for ABSI), and BMI (only adjusted in models for CRP), multivariable Cox proportional hazard models were used to determine the hazard ratios (HRs) for ischemic stroke associated with a high ABSI and a high CRP level. Then, the cumulative risk of ischemic stroke among the 4 groups was estimated using Kaplan-Meier curves and compared with a log-rank test. We used Cox proportional hazards models to compute the HRs for ischemic stroke across the 4 groups by adjusting for important confounding factors including age, gender, cigarette smoking, alcohol drinking, FPG, hypertension, family history of cardiovascular disease, TG, and HDL-C. In addition, we tested the discriminatory ability of ABSI, BMI, WC, and CRP to predict ischemic stroke using receiver operating characteristic curves (ROCs). The DeLong non-parametric test was used to compare the different area under the curves (AUCs)[23]. A two-tailed P-value < 0.05 was considered statistically significant. All statistical analyses were conducted using SAS statistical software (version 9.4, Cary, NC, USA).
-
Until July 31, 2012, we followed 2, 589 participants for an average of 9.2 years. Six participants were lost to follow-up. Thirty-four participants were excluded for missing ABSI or CRP data, and a total of 2, 549 people were ultimately included in the analysis. Among the 2, 549 participants, 76 ischemic stroke events were recorded during the follow-up period. The cumulative incidence rates of ischemic stroke were 2.98% and the incidence density was 323 per 100, 000 person-years.
-
Our study included 1, 045 males and 1, 504 females. The mean age of the participants was 46.50 ± 12.38 years at baseline. Table 1 presents the baseline characteristics among the 4 groups. Conventional stroke risk factors, such as age, gender, cigarette smoking, alcohol drinking, family history of CVD, hypertension status, BMI, FPG, TG, TC, LDL-C, and HDL-C were significantly different among the 4 groups. Participants with the a high level of ABSI in either the low CRP level or the high CRP level group tended to be older, smokers, drinkers, hypertensive, and have higher TC levels; those with high CRP levels in either the low ABSI or the high ABSI level groups were prone to be male, have higher levels of BMI, TG, LDL-C, FPG, a family history of CVD, and lower levels of HDL-C.
Table 1. Baseline Characteristics of 4 Subgroups According to ABSI and CRP Levels among 2, 549 Participants
Items Low ABSI/ Low CRP High ABSI/ Low CRP Low ABSI/ High CRP High ABSI/ High CRP PValue* Number of participants 1, 495 418 424 212 Age (years) 42.92 ± 10.78 55.47 ± 2.32 45.66 ± 11.23 55.70 ± 11.74 < 0.0001 Male (%) 590 (39.41) 155 (36.73) 209 (49.64) 91 (43.54) 0.0004 Cigarette smoking (%) 604 (40.35) 214 (50.71) 201 (47.74) 112 (53.59) < 0.0001 Alcohol drinking (%) 437 (29.19) 160 (37.91) 160 (38.00) 94 (44.98) < 0.0001 Family history of CVD (%) 144 (9.62) 49 (11.61) 87 (20.67) 50 (23.92) < 0.0001 Hypertension (%) 440 (29.39) 190 (45.02) 202 (47.98) 121 (57.89) < 0.0001 BMI (kg/m2) 22.05 ± 3.21 21.56 ± 3.56 23.40 ± 3.71 22.91 ± 4.01 < 0.0001 ABSI (m11/6/kg2/3) 0.0781 ± 0.0036 0.0875 ± 0.0040 0.0790 ± 0.0031 0.0878 ± 0.0038 < 0.0001 TG (mmol/L) 0.81 (0.58-1.14) 0.96 (0.70-1.35) 1.38 (0.96-2.01) 1.55 (1.08-2.46) < 0.0001 TC (mmol/L) 3.45 (2.83-4.07) 3.85 (3.23-4.60) 3.74 (3.13-4.78) 4.22 (3.38-5.04) < 0.0001 LDL-C (mmol/L) 2.04 (1.51-2.63) 2.36 (1.78-3.11) 2.36 (1.73-3.21) 2.61 (1.90-3.37) < 0.0001 HDL-C (mmol/L) 1.17 (0.98-1.38) 1.19 (1.01-1.43) 1.03 (0.86-1.27) 1.09 (0.92-1.30) < 0.0001 FPG (mmol/L) 4.7 (4.2-5.2) 4.6 (4.2-5.2) 5.3 (4.9-5.8) 5.6 (4.9-6.3) < 0.0001 logCRP (mg/L) 0.66 ± 0.24 0.70 ± 0.21 1.28 ± 0.17 1.33 ± 0.19 < 0.0001 Note.*CVD, cardiovascular disease; BMI, body mass index; ABSI, a body shape index; TG, triglyceride; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; FPG, fasting plasma glucose; CRP, C-reactive protein. -
Table 2 shows the multivariable adjusted HR for the association of ABSI and CRP levels with the risk of incident ischemic stroke. In crude models, high ABSI and high CRP levels were significantly associated with the risk of ischemic stroke with HRs (95% CI) of 3.67 (2.34-5.75) and 1.94 (1.22-3.08), respectively. After multivariate adjustments, HRs (95% CI) for ischemic stroke among the participants with high ABSI and high CRP levels were 1.46 (0.89-2.39) and 1.63 (0.95-2.79), respectively, compared to those with low ABSI or low CRP levels. Moreover, 1-SD increment of ABSI and logarithm CRP were 1.18 (0.94-1.47) and 1.18 (0.90-1.55), respectively.
Table 2. Hazard Ratios and 95% Confidence Intervals of Ischemic Stroke with ABSI and CRP
Items Unadjusted Age and Gender Adjusted Multivariable Adjusted* HR 95% CI HR 95% CI HR 95% CI Low ABSI 1.00 reference 1.00 reference 1.00 Reference High ABSI 3.67 (2.34-5.75) 1.34 (0.82-2.19) 1.46 (0.89-2.39) ABSI (per 1 SD) 1.61 (1.41-1.83) 1.13 (0.90-1.42) 1.18 (0.94-1.47) Low CRP 1.00 reference 1.00 Reference 1.00 reference High CRP 1.94 (1.22-3.08) 1.61 (1.01-2.56) 1.63 (0.95-2.79) logCRP (per 1 SD) 1.30 (1.05-1.62) 1.17 (0.93-1.46) 1.18 (0.90-1.55) Note.*Adjusted for age, gender, alcohol drinking, cigarette smoking, hypertension, FPG, TG, HDL cholesterol, family history of CVD, CRP (only adjusted in models for ABSI) and BMI (only adjusted in models for CRP). -
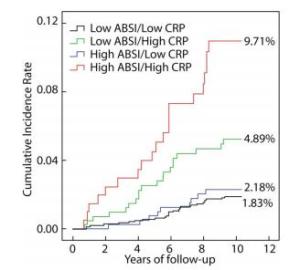
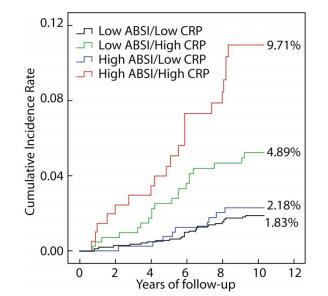
Figure 1 presents the Kaplan-Meier curves for cumulative incidence rates of ischemic stroke among the 4 groups according to ABSI and CRP levels. During the average 9.2 years of follow-up, the cumulative incidence rates of ischemic stroke among the low ABSI/low CRP, low ABSI/high CRP, high ABSI/low CRP, and high ABSI/high CRP level groups were 1.83%, 2.18%, 4.89%, and 9.71%, respectively (P < 0.0001). The cumulative incidence of ischemic stroke was highest in the high ABSI/high CRP level group.
Table 3 presents the unadjusted and multivariate adjusted HRs (95% CI) for ischemic stroke for the different combinations of ABSI and CRP levels. Compared with the low ABSI/low CRP level group, the unadjusted HRs (95% CIs) for ischemic stroke in the low ABSI/high CRP, high ABSI/low CRP and high ABSI/high CRP level groups were 1.21 (0.57-2.58), 2.80 (1.57-4.99), and 5.82 (3.27-10.39), respectively. After adjusting for multivariate factors including age, gender, cigarette smoking, alcohol drinking, hypertension, FPG, family history of CVD, TG, and HDL-C, the HRs (95% CIs) for ischemic stroke for the low ABSI/high CRP, high ABSI/low CRP, and high ABSI/high CRP level groups were 1.04 (0.46-2.35), 1.06 (0.58-1.95), and 2.52 (1.27-5.00), respectively. The HR for the high ABSI/high CRP level group remained significant although it decreased. In addition, no significant interaction was observed between ABSI and CRP levels on ischemic stroke risk in the multivariable analysis (P = 0.110).
Table 3. Adjusted Hazard Ratios for Ischemic Stroke Incidence According to ABSI with CRP Level
Items Events Person-years Unadjusted Age and Gender Adjusted Multivariable Adjusted* HR 95% CI HR 95% CI HR 95% CI Low ABSI/Low CRP 27 13948 1.00 (reference) 1.00 (reference) 1.00 (reference) Low ABSI/High CRP 9 4005 1.21 (0.57-2.58) 0.98 (0.46-2.09) 1.04 (0.46-2.35) High ABSI/Low CRP 20 3721 2.80 (1.57-4.99) 0.93 (0.50-1.71) 1.06 (0.58-1.95) High ABSI/High CRP 20 1860 5.82 (3.27-10.39) 2.12 (1.16-3.88) 2.52 (1.27-5.00) ABSI × CRP 1.72 (0.65-4.56) 2.34 (0.88-6.21) 2.30 (0.83-6.36) Note.*Adjusted for age, gender, alcohol drinking, cigarette smoking, hypertension, FPG, TG, HDL cholesterol, family history of CVD. FPG: fasting plasma glucose, TG: triglyceride, HDL: high density lipoprotein cholesterol. ROC curves which demonstrated the predictive values of ABSI, BMI, WC, and CRP on the risk of ischemic stroke are shown in Figure 2. The AUCs (95% CIs) of ABSI, CRP, BMI, and WC were 0.706 (0.688-0.724), 0.585 (0.565-0.604), 0.537 (0.517 -0.556), and 0.572 (0.552-0.591), respectively. The AUC of ABSI was significantly higher than that of BMI (P = 0.0002), WC (P = 0.0001), and CRP (P = 0.0024).

Figure 2. Area under the curve for the prediction of ischemic stroke incidence according to the baseline ABSI, CRP, BMI, and WC levels. The AUCs of ABSI, BMI, WC, and CRP were 0.706 (0.688-0.724), 0.537 (0.517 -0.556), 0.572 (0.552-0.591), and 0.585 (0.565-0.604), respectively. The AUC of ABSI is significantly higher than that of BMI (P = 0.0002), WC (P = 0.0001) and CRP (P = 0.0024).
-
In this prospective cohort study in the Inner Mongolian population, we found that individuals with higher ABSI and higher CRP levels only show a marginally significant association with increased risk of ischemic stroke although they had higher HRs of 1.46 and 1.63, respectively, after adjustment for other important cardiovascular risk factors including age, gender, cigarette smoking, alcohol drinking, hypertension, FPG, family history of CVD, TG, HDL-C, CRP (only adjusted in models for ABSI), and BMI (only adjusted in models for CRP). However, the individuals with both high ABSI and high CRP levels had a 2.52-fold higher risk of ischemic stroke after adjusting for the important cardiovascular risk factors, than those with low ABSI and low CRP levels. These findings suggest a combined effect of high ABSI and high CRP levels on the risk of ischemic stroke. To the best of our knowledge, this is the first study conducted to assess the cumulative effect of higher ABSI and higher CRP levels on ischemic stroke incidence among Mongolians in China.
Obesity, especially abdominal visceral fat, has been reported to be strongly associated with cardiovascular risks[3, 24, 25]. ABSI, a new anthropometric measure which reflect indicates the accumulation of abdominal visceral fat[17], was associated with mortality and the incidence of CVD events[26-29] as well as atherosclerosis in patients with type 2 diabetes[30]. A meta-analysis including 24 retrospective cohort studies and 14 cross-sectional studies across 15 countries found that 1 SD increase in ABSI was associated with a 21% increase for CVD and a 55% increase for all-cause mortality risk[31]. CRP is a marker of low-grade vascular inflammation and plays a key role in the development and rupture of atheromatous plaques[32, 33]. CRP may contribute to the progression of atherothrombosis[34, 35], atherosclerosis, and endothelial cell dysfunction[36], and is independently associated with the risk of cardiovascular events, including ischemic stroke[11, 37-39]. Given that both ABSI and CRP were closely associated with atherosclerosis, our study focused on the combined effect of ABSI and CRP on ischemic stroke. Although CRP had a weak association with ischemic stroke with an HR (95% CI) of 1.63 (0.95-2.79) in our study, the participants with both high ABSI and high CRP levels had the highest cumulative incidence and highest risk of ischemic stroke indicating that co-existence of high ABSI and high CRP levels had a higher risk of ischemic stroke than each factor alone. Some studies have reported that CRP increased among obese subjects whose microvascular endothelium was impaired[40-42], and visceral obesity can significantly increase insulin resistance and the risk of hyperlipidemias[43]. In turn, hyperlipidemias could evoke inflammation and contribute to ischemic lesions[44]. Furthermore, some studies have shown that CRP, TG, and obesity are interrelated and seem to act synergistically to aggravate the progression of cardiovascular diseases[41, 42, 45]. Statin therapy was confirmed to be effective in decreasing CRP concentrations and preventing coronary events[46]. These studies supported our findings that there was a combined effect of high ABSI and high CRP levels on the incidence of ischemic stroke. Horvei et al. suggested that the combination of increased CRP levels and obesity may share the same pathway in promoting arterial and venous thromboses, which increases the risk of ischemic stroke[47]. Our findings suggested that examination of CRP and TG concentrations and an evaluation of ABSI should be performed to screen high risk populations at to predict the risk of ischemic stroke.
Several strengths in our study are worth mentioning. Firstly, the study participants were homogeneous in terms of their stable genetic background and environmental exposures. Secondly, the study data were collected with rigid quality controls. Thirdly, a relatively long observation period and a low rate of loss to follow-up assured a less biased association in the analyses. However, there are some limitations that need to be considered. First, the sample size was not very large, and sub-analyses were not performed due to the limited number of study outcomes. Additionally, measures of ABSI and CRP levels were conducted only at baseline. Weight loss or CRP variations could not be assessed during the follow-up period. Moreover, information regarding any treatments for low-level inflammation and dyslipidemia was not collected. Given the low rates of awareness and treatment for diseases in the Mongolian population, the effect of these confounding factors might be minimal.
-
We found that the participants with simultaneously high ABSI and high CRP levels had the highest risk of ischemic stroke in the Mongolian population. Our findings suggest that the combination of high ABSI and high CRP levels may increase the risk of ischemic stroke.
-
We thank the study participants, their relatives and the clinical staff at all participating hospitals for their support and contribution to this project.
-
WANG Guang Li collected and researched data, and wrote the manuscript. ZHANG Rui, ZHOU Yi Ting, and XU Tian collected and researched data. LI Hong Mei, ZHANG Ming Zhi, and WANG Ai Li researched data. ZHANG Yong Hong designed the study, collected and researched data, and revised the manuscript. ZHANG Yong Hong is the guarantor of this work and, as such, had full access to the data and takes responsibility for the accuracy of data analysis.
-
There are no conflicts of interest to declare.
doi: 10.3967/bes2019.024
Combined Effects of A Body Shape Index and Serum C-reactive Protein on Ischemic Stroke Incidence among Mongolians in China
-
Abstract:
Objective We aimed to evaluate the combined effects of a high body shape index (ABSI) and a high serum C-reactive protein (CRP) level on the incidence of ischemic stroke in a Mongolian population in China. Methods A prospective cohort study was conducted among 2, 589 participants from June 2002 to July 2012 in Inner Mongolia, China. The participants were categorized into 4 groups according to their level of ABSI and CRP. Cox proportional hazards models were used to assess the hazard ratios (HRs) and 95% confidence intervals (CIs) for ischemic stroke among all groups. Results The multivariate adjusted HRs (95% CI) of ischemic stroke for high ABSI and high CRP level were 1.46 (0.89-2.39) and 1.63 (0.95-2.79), respectively. Compared with the low ABSI/low CRP level group, the multivariate adjusted HRs (95% CI) of ischemic stroke in the low ABSI/high CRP, high ABSI/low CRP, and high ABSI/high CRP groups were 1.04 (0.46-2.35), 1.06 (0.58-1.95) and 2.52 (1.27-5.00), respectively. The HR of ischemic stroke for the high ABSI/high CRP level group was the highest and most statistically significant. Conclusion We found that participants with simultaneously high ABSI and high CRP levels had the highest risk of ischemic stroke in the Mongolian population. Our findings suggest that the combination of high ABSI and high CRP levels may increase the risk of ischemic stroke. -
Key words:
- A body shape index /
- C-reactive protein /
- Ischemic stroke
-
Figure 2. Area under the curve for the prediction of ischemic stroke incidence according to the baseline ABSI, CRP, BMI, and WC levels. The AUCs of ABSI, BMI, WC, and CRP were 0.706 (0.688-0.724), 0.537 (0.517 -0.556), 0.572 (0.552-0.591), and 0.585 (0.565-0.604), respectively. The AUC of ABSI is significantly higher than that of BMI (P = 0.0002), WC (P = 0.0001) and CRP (P = 0.0024).
Table 1. Baseline Characteristics of 4 Subgroups According to ABSI and CRP Levels among 2, 549 Participants
Items Low ABSI/ Low CRP High ABSI/ Low CRP Low ABSI/ High CRP High ABSI/ High CRP PValue* Number of participants 1, 495 418 424 212 Age (years) 42.92 ± 10.78 55.47 ± 2.32 45.66 ± 11.23 55.70 ± 11.74 < 0.0001 Male (%) 590 (39.41) 155 (36.73) 209 (49.64) 91 (43.54) 0.0004 Cigarette smoking (%) 604 (40.35) 214 (50.71) 201 (47.74) 112 (53.59) < 0.0001 Alcohol drinking (%) 437 (29.19) 160 (37.91) 160 (38.00) 94 (44.98) < 0.0001 Family history of CVD (%) 144 (9.62) 49 (11.61) 87 (20.67) 50 (23.92) < 0.0001 Hypertension (%) 440 (29.39) 190 (45.02) 202 (47.98) 121 (57.89) < 0.0001 BMI (kg/m2) 22.05 ± 3.21 21.56 ± 3.56 23.40 ± 3.71 22.91 ± 4.01 < 0.0001 ABSI (m11/6/kg2/3) 0.0781 ± 0.0036 0.0875 ± 0.0040 0.0790 ± 0.0031 0.0878 ± 0.0038 < 0.0001 TG (mmol/L) 0.81 (0.58-1.14) 0.96 (0.70-1.35) 1.38 (0.96-2.01) 1.55 (1.08-2.46) < 0.0001 TC (mmol/L) 3.45 (2.83-4.07) 3.85 (3.23-4.60) 3.74 (3.13-4.78) 4.22 (3.38-5.04) < 0.0001 LDL-C (mmol/L) 2.04 (1.51-2.63) 2.36 (1.78-3.11) 2.36 (1.73-3.21) 2.61 (1.90-3.37) < 0.0001 HDL-C (mmol/L) 1.17 (0.98-1.38) 1.19 (1.01-1.43) 1.03 (0.86-1.27) 1.09 (0.92-1.30) < 0.0001 FPG (mmol/L) 4.7 (4.2-5.2) 4.6 (4.2-5.2) 5.3 (4.9-5.8) 5.6 (4.9-6.3) < 0.0001 logCRP (mg/L) 0.66 ± 0.24 0.70 ± 0.21 1.28 ± 0.17 1.33 ± 0.19 < 0.0001 Note.*CVD, cardiovascular disease; BMI, body mass index; ABSI, a body shape index; TG, triglyceride; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; FPG, fasting plasma glucose; CRP, C-reactive protein. Table 2. Hazard Ratios and 95% Confidence Intervals of Ischemic Stroke with ABSI and CRP
Items Unadjusted Age and Gender Adjusted Multivariable Adjusted* HR 95% CI HR 95% CI HR 95% CI Low ABSI 1.00 reference 1.00 reference 1.00 Reference High ABSI 3.67 (2.34-5.75) 1.34 (0.82-2.19) 1.46 (0.89-2.39) ABSI (per 1 SD) 1.61 (1.41-1.83) 1.13 (0.90-1.42) 1.18 (0.94-1.47) Low CRP 1.00 reference 1.00 Reference 1.00 reference High CRP 1.94 (1.22-3.08) 1.61 (1.01-2.56) 1.63 (0.95-2.79) logCRP (per 1 SD) 1.30 (1.05-1.62) 1.17 (0.93-1.46) 1.18 (0.90-1.55) Note.*Adjusted for age, gender, alcohol drinking, cigarette smoking, hypertension, FPG, TG, HDL cholesterol, family history of CVD, CRP (only adjusted in models for ABSI) and BMI (only adjusted in models for CRP). Table 3. Adjusted Hazard Ratios for Ischemic Stroke Incidence According to ABSI with CRP Level
Items Events Person-years Unadjusted Age and Gender Adjusted Multivariable Adjusted* HR 95% CI HR 95% CI HR 95% CI Low ABSI/Low CRP 27 13948 1.00 (reference) 1.00 (reference) 1.00 (reference) Low ABSI/High CRP 9 4005 1.21 (0.57-2.58) 0.98 (0.46-2.09) 1.04 (0.46-2.35) High ABSI/Low CRP 20 3721 2.80 (1.57-4.99) 0.93 (0.50-1.71) 1.06 (0.58-1.95) High ABSI/High CRP 20 1860 5.82 (3.27-10.39) 2.12 (1.16-3.88) 2.52 (1.27-5.00) ABSI × CRP 1.72 (0.65-4.56) 2.34 (0.88-6.21) 2.30 (0.83-6.36) Note.*Adjusted for age, gender, alcohol drinking, cigarette smoking, hypertension, FPG, TG, HDL cholesterol, family history of CVD. FPG: fasting plasma glucose, TG: triglyceride, HDL: high density lipoprotein cholesterol. -
[1] Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol, 2007; 6, 182-7. doi: 10.1016/S1474-4422(07)70031-5 [2] Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation, 2015; 131, e29-e322. [3] Goldstein LB, Adams R, Becker K, et al. Primary prevention of ischemic stroke: A statement for healthcare professionals from the Stroke Council of the American Heart Association. Circulation, 2001; 32, 280-99. http://www.ncbi.nlm.nih.gov/pubmed/11136952 [4] Ridker P, Kastelein J, Genest J, et al. C-reactive protein and cholesterol are equally strong predictors of cardiovascular risk and both are important for quality clinical care. Eur Heart J, 2013; 34, 1258-61. doi: 10.1093/eurheartj/eht022 [5] Osawa H, DoiY, Makino H, et al. Diabetes and hypertension markedly increased the risk of ischemic stroke associated with high serum resistin concentration in a general Japanese population: the Hisayama Study. Cardiovasc Diabetol, 2009; 8, 60. doi: 10.1186/1475-2840-8-60 [6] Youn C, Choi S, Kim S, et al. Serum highly selective C-reactive protein concentration is associated with the volume of ischemic tissue in acute ischemic stroke. Am J Emerg Med, 2012; 30, 124-8. doi: 10.1016/j.ajem.2010.11.006 [7] Pierdomenico S, Pierdomenico A, Cuccurullo F. Morning blood pressure surge, dipping, and risk of ischemic stroke in elderly patients treated for hypertension. Am J Hypertens, 2014; 27, 564-70. doi: 10.1093/ajh/hpt170 [8] Ridker PM, Cushman M, Stampfer MJ, et al. Inflammation, Aspirin, and the Risk of Cardiovascular Disease in Apparently Healthy Men. N Engl J Med, 1997; 336, 973-9. doi: 10.1056/NEJM199704033361401 [9] Rost N, Wolf P, Kase C, et al. Plasma concentration of C-reactive protein and risk of ischemic stroke and transient ischemic attack: the Framingham study. Stroke, 2001; 32, 2575-9. doi: 10.1161/hs1101.098151 [10] Ridker P, Rifai N, Rose L, et al. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med, 2002; 347, 1557-65. doi: 10.1056/NEJMoa021993 [11] Ridker PM, Hennekens CH, Buring JE, et al. C-Reactive Protein and Other Markers of Inflammation in the Prediction of Cardiovascular Disease in Women. N Engl J Med, 2000; 342, 836-43. doi: 10.1056/NEJM200003233421202 [12] Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult – 2009 recommendations. Can J Cardiol, 2009; 25, 567-79. doi: 10.1016/S0828-282X(09)70715-9 [13] Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol, 2010; 56, e50-e103. doi: 10.1016/j.jacc.2010.09.001 [14] Visser M, Bouter LM, McQuillan GM, et al. Elevated c-reactive protein levels in overweight and obese adults. JAMA, 1999; 282, 2131-5. doi: 10.1001/jama.282.22.2131 [15] Nevill AM, Stewart AD, Olds T, et al. Relationship between adiposity and body size reveals limitations of BMI. Am J Phys Anthropol, 2006; 129, 151-6. doi: 10.1002/(ISSN)1096-8644 [16] Dhana K, Kavousi M, Ikram MA, et al. Body shape index in comparison with other anthropometric measures in prediction of total and cause-specific mortality. J Epidemiol Community Health, 2016; 70, 90-6. doi: 10.1136/jech-2014-205257 [17] Krakauer NY, Krakauer JC. A New Body Shape Index Predicts Mortality Hazard Independently of Body Mass Index. PLoS One, 2012; 7, e39504. doi: 10.1371/journal.pone.0039504 [18] Heymsfield SB, Scherzer R, Pietrobelli A, et al. Body Mass Index as a Phenotypic Expression of Adiposity: Quantitative Contribution of Muscularity in a Population-Based Sample. Int J Obes (Lond), 2009; 33, 1363-73. doi: 10.1038/ijo.2009.184 [19] Li H, Xu T, Tong W, et al. Comparison of Cardiovascular Risk Factors Between Prehypertension and Hypertension in a Mongolian Population, Inner Mongolia, China. Circ J, 2008; 72, 1666-73. doi: 10.1253/circj.CJ-08-0138 [20] Perloff D, Grim C, Flack J, et al. Human blood pressure determination by sphygmomanometry. Circulation, 1993; 88, 2460-70. doi: 10.1161/01.CIR.88.5.2460 [21] Xu T, Bu X, Li H, et al. Smoking, Heart Rate, and Ischemic Stroke: A Population-Based Prospective Cohort Study Among Inner Mongolians in China. Stroke, 2013; 44, 2457-61. doi: 10.1161/STROKEAHA.111.000648 [22] Stroke--1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke, 1989; 20, 1407-31. [23] DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics, 1988; 44, 837-45. doi: 10.2307/2531595 [24] The Global Burden of Metabolic Risk Factors for Chronic Diseases C. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet, 2014; 383, 970-83. doi: 10.1016/S0140-6736(13)61836-X [25] Fox CS, Massaro JM, Hoffmann U, et al. Abdominal Visceral and Subcutaneous Adipose Tissue Compartments. Circulation, 2007; 116, 39-48. doi: 10.1161/CIRCULATIONAHA.106.675355 [26] Krakauer NY, Krakauer JC. Dynamic Association of Mortality Hazard with Body Shape. PLoS One, 2014; 9, e88793. doi: 10.1371/journal.pone.0088793 [27] Grant JF, Chittleborough CR, Shi Z, et al. The association between A Body Shape Index and mortality: Results from an Australian cohort. PLoS One, 2017; 12, e0181244. doi: 10.1371/journal.pone.0181244 [28] Sato Y, Fujimoto S, Konta T, et al. Body shape index: Sex-specific differences in predictive power for all-cause mortality in the Japanese population. PLoS One, 2017; 12, e0177779. doi: 10.1371/journal.pone.0177779 [29] Thomson CA, Garcia DO, Wertheim BC, et al. Body Shape, Adiposity Index, and Mortality in Postmenopausal Women: Findings from the Women's Health Initiative. Obesity, 2016; 24, 1061-9. doi: 10.1002/oby.v24.5 [30] Bouchi R, Asakawa M, Ohara N, et al. Indirect measure of visceral adiposity 'A Body Shape Index' (ABSI) is associated with arterial stiffness in patients with type 2 diabetes. BMJ Open Diabetes Res Care, 2016; 4, e000188. doi: 10.1136/bmjdrc-2015-000188 [31] Ji M, Zhang S, An R. Effectiveness of A Body Shape Index (ABSI) in predicting chronic diseases and mortality: a systematic review and meta-analysis. Obes Rev, 2018; 19, 737-59. doi: 10.1111/obr.v19.5 [32] Zimmermann O, Li K, Zaczkiewicz M, et al. C-Reactive Protein in Human Atherogenesis: Facts and Fiction. Mediators Inflamm, 2014; 2014, 561428. http://pubmedcentralcanada.ca/pmcc/articles/PMC3995305/ [33] Pepys MB, Hirschfield GM. C-reactive protein: a critical update. [J]lin Invest, 2003; 111, 1805-12. doi: 10.1172/JCI200318921 [34] Zwaka TP, Hombach V, Torzewski J. C-Reactive Protein–Mediated Low Density Lipoprotein Uptake by Macrophages: implications for atherosclerosis. Circulation, 2001; 103, 1194-7. doi: 10.1161/01.CIR.103.9.1194 [35] Lagrand WK, Visser CA, Hermens WT, et al. C-reactive protein as a cardiovascular risk factor: more than an epiphenomenon? Circulation, 1999; 100, 96-102. doi: 10.1161/01.CIR.100.1.96 [36] Libby P, Aikawa M. Effects of statins in reducing thrombotic risk and modulating plaque vulnerability. Clin Cardiol, 2003; 26, 11-4. doi: 10.1002/clc.v26:1+ [37] Sung KC, Ryu S, Chang Y, et al. C-reactive protein and risk of cardiovascular and all-cause mortality in 268 803 East Asians. Eur Heart J, 2014; 35, 1809-16. doi: 10.1093/eurheartj/ehu059 [38] Ridker PM, Buring JE, Shih J, et al. Prospective Study of C-Reactive Protein and the Risk of Future Cardiovascular Events Among Apparently Healthy Women. Circulation, 1998; 98, 731-3. doi: 10.1161/01.CIR.98.8.731 [39] Arenillas JF, Álvarez-Sabín J, Molina CA, et al. C-Reactive Protein Predicts Further Ischemic Events in First-Ever Transient Ischemic Attack or Stroke Patients With Intracranial Large-Artery Occlusive Disease. Stroke, 2003; 34, 2463-8. doi: 10.1161/01.STR.0000089920.93927.A7 [40] Thompson AM, Zhang Y, Tong W, et al. Association of obesity and biomarkers of inflammation and endothelial dysfunction in adults in Inner Mongolia, China. Int J Cardiol, 2011; 150, 247-52. doi: 10.1016/j.ijcard.2010.04.011 [41] Yang CW, Li CI, Li TC, et al. Association of Sarcopenic Obesity with Higher Serum High-Sensitivity C-Reactive Protein Levels in Chinese Older Males - A Community-Based Study (Taichung Community Health Study-Elderly, TCHS-E). PLoS One, 2015; 10, e0132908. doi: 10.1371/journal.pone.0132908 [42] Sanip Z, Ariffin FD, Al-Tahami BAM, et al. Obesity indices and metabolic markers are related to hs-CRP and adiponectin levels in overweight and obese females. Obes Res Clin Pract, 2013; 7, e315-20. doi: 10.1016/j.orcp.2012.05.002 [43] Carmena R, Ascaso JF, Real JT. Impact of obesity in primary hyperlipidemias. Nutr Metab Cardiovasc Dis, 2001; 11, 354-9. http://www.ncbi.nlm.nih.gov/pubmed/11887432 [44] Faraj M, Messier L, Bastard JP, et al. Apolipoprotein B: a predictor of inflammatory status in postmenopausal overweight and obese women. Diabetologia, 2006; 49, 1637-46. doi: 10.1007/s00125-006-0259-7 [45] Firdous S. Correlation of CRP, fasting serum triglycerides and obesity as cardiovascular risk factors. J Coll Physicians Surg Pak, 2014; 24, 308-13. http://europepmc.org/abstract/med/24848386 [46] Ridker PM, Rifai N, Clearfield M, et al. Measurement of C-Reactive Protein for the Targeting of Statin Therapy in the Primary Prevention of Acute Coronary Events. N Engl J Med, 2001; 344, 1959-65. doi: 10.1056/NEJM200106283442601 [47] Horvei LD, Grimnes G, Hindberg K, et al. C-reactive protein, obesity, and the risk of arterial and venous thrombosis. J Thromb Haemost, 2016; 14, 1561-71. doi: 10.1111/jth.13369 -



 下载:
下载:


 Quick Links
Quick Links