-
All close contacts of two confirmed patients with pneumonic plague who came to Beijing for medical treatment from Xilingol League, Inner Mongolia, had been released from isolation after medical observation according to protocol by 8:00 am on November 21, 2019. The news was posted on the Beijing municipal government website, Windows of the Capital[1]. As the first emergency department in Beijing since the founding of the People's Republic of China to be placed in such position, we have accumulated some prevention and control experience in response to this Infectious disease. Now we report the relevant situation as follows.
Case 1. Patient A was a 43-year-old herdsman from Sunit Left Banner, Xilingol League, Inner Mongolia Autonomous Region. He developed productive cough 10 days prior to admission (October 25, 2019), with occasional hemoptysis and intermittent fever, having a maximum temperature of 39.2 °C. His fever was reduced by antipyretic drugs. The patient was diagnosed as having ‘pulmonary infection’ in a local hospital and was subsequently admitted. His symptoms were progressive and dyspnea was obvious. Chest computerized tomography (CT) showed worsening pulmonary infection, so he was transported to Beijing for treatment via emergency vehicle. He was then transferred to the emergency treatment area after routine screening in the fever clinic of our hospital. Since the onset of the disease, he felt weak, had poor appetite, and slept poorly. He provided an occupational history of raising cattle and sheep before the onset of the disease, but not of deratization, and denied direct contact with live rats.
Initial physical examination revealed a temperature of 36.3 °C, a pulse rate of 74 beats per minute, a respiratory rate of 20 breaths per minute, a blood pressure of 126/85 mmHg and an oxygen saturation level (SpO2) of 90% while on oxygen storage mask inhaled oxygen at 10 liters per minute. When he was brought into the clinic on a rescue bed, he was conscious and kept in an autonomous position. He was short of breath but lacked the ‘three concave sign’. Breath sounds were low-pitched on both lungs, and moist rales were present. He had a heart rate of 74 beats per minute and a good rhythm. No pathological murmur was heard over any valve auscultation area. The rest of his physical examination was unremarkable.
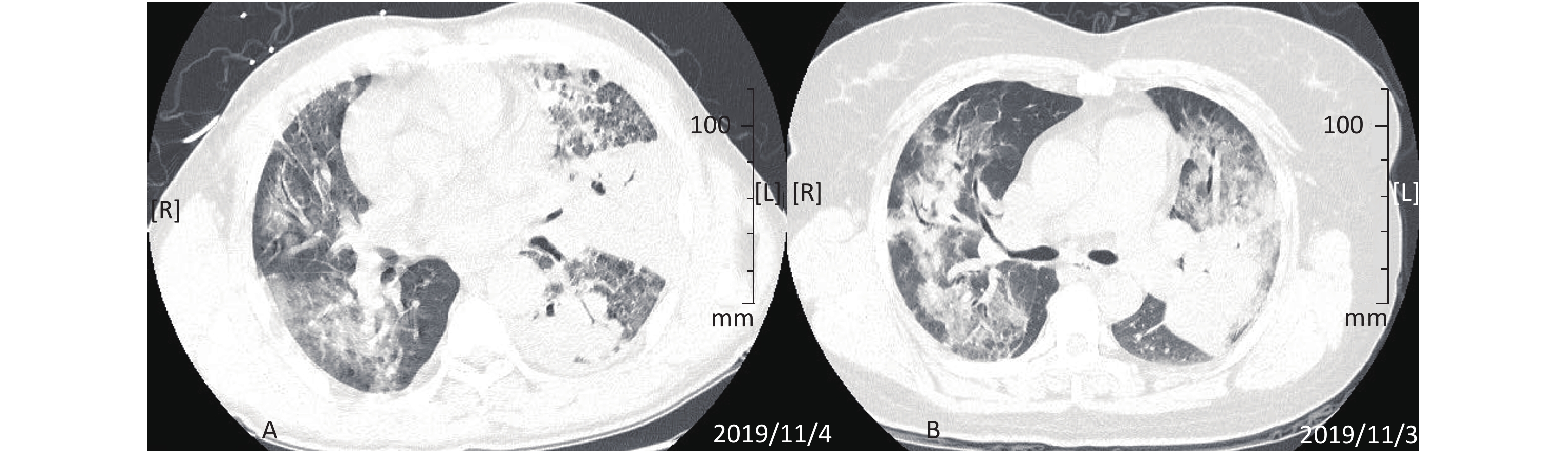
On November 4, his chest CT showed diffuse patchy and nodular changes in both lungs. Pleural effusion was noted in the left lung, as shown in Figure 1A. His electrocardiogram (EKG) was generally normal. Other tests performed on the same day included routine blood tests, blood biochemistry, coagulation tests, erythrocyte sedimentation rate, C-reactive protein (CRP), procalcitonin (PCT) and immune function tests. The results are shown in Table 1.
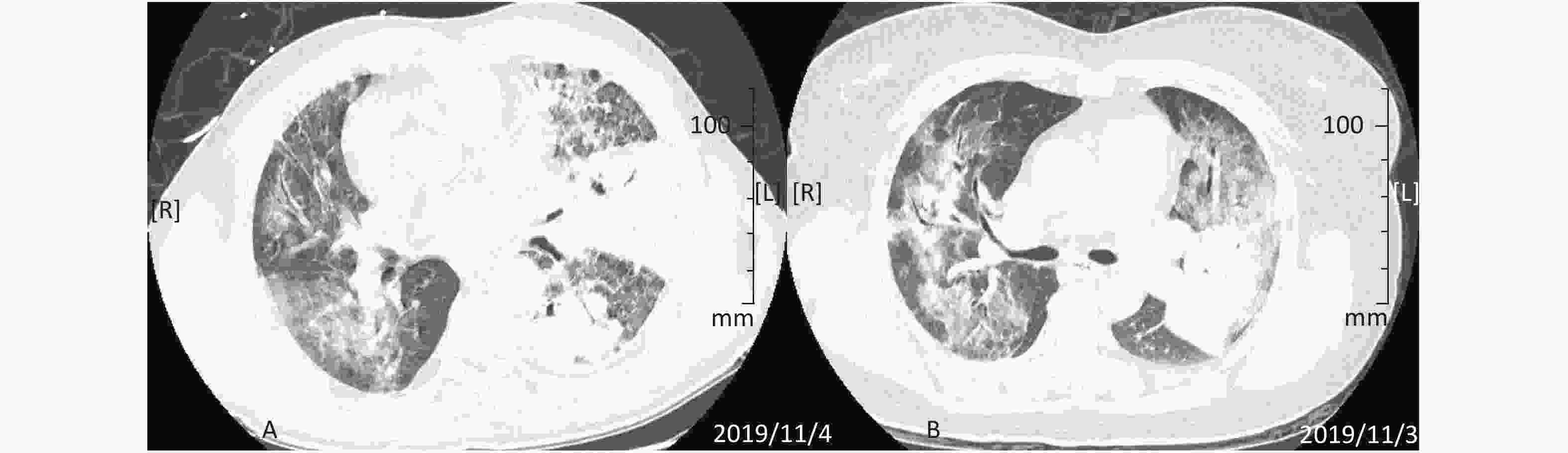
Figure 1. CT image of patient's lungs. (A) CT image of patient A's lungs (2019.11.04). Diffuse and patchy changes are seen in both lungs, with the left lung showing mild pleural effusion. (B) CT image of patient B's lungs (2019.11.03). Diffuse exudates in both lungs and a dense mass-like opacity are seen, with the left lung as the focus.
Test Items Detection Result Normal range Patient A Patient B Routine Blood Tests WBC (x109/L) 28.6 9.76 3.5–9.5 N (%) 92.8 89.2 40–75 Hgb (g/L) 132 117 130–175 PLT (x109/L) 267 134 125–350 Blood Gas Analysis oxygen storage
mask inhaled oxygen at 10 liters per minutePH 7.49 7.44 7.35–7.45 PO2 (mmHg) 69.1 59.5 83–108 PCO2 (mmHg) 27.2 26.0 35–45 SO2 (%) 96.4 91.5 95–98 Lactic acid (mmol/L) 1.10 0.80 0.7–2.5 Biochemical Tests Total Protein (g/L) 53.1 64.4 65.0–85.0 Albumin (g/L) 29.1 36.6 40.0–55.0 Globulin (g/L) 24.0 27.8 25.0–45.0 ALT (U/L) 80 22 9–50 CK (U/L) 74 23 50–310 LDH (U/L) 285 211 120–250 HBDH (U/L) 229 169 72–182 GGT (U/L) 185 53 10–60 TBIL (μmol/L) 22.6 12.1 5.0–21.0 DBIL (μmol/L) 11.0 4.5 0–6.8 CREA (μmol/L) 44.5 50.6 57.0–97.0 CTNI (ng/mL) 0.01 0.00 0–0.04 CKMB (ng/mL) 0.7 0.2 ≤ 5.0 BNP (pg/mL) 165 76 0–100 Coagulation Studies Fbg (ng/dL) 464.5 738.0 170–400 D-dimer (mg/L FEU) 4.98 3.12 < 0.55 Erythrocyte Sedimentation Rate (ESR) (mm/h) 17 74 0–15 C-reactive protein (CRP) (ng/dL) 15.40 11.30 0–0.8 Procalcitonin (PCT) (ng/mL) 0.18 2.67 < 0.05 Immune Function Tests CD4+ T (A/μL) 487 34.9 410–112 CD8+ T (A/μL) 288 80 240–880 CD19 (A/μL) 149 113 180–324 CD19 (%) 14.4 17.6 8.5–14.0 IgG (ng/dL) 780 743 751–1,560 Table 1. Results of routine blood tests, biochemistry tests, coagulation tests, ESR, CRP, PCT, and immune function tests
At 10:45 pm on November 3, after emergency department registration, the patient was sent to the emergency rescue room. Cefoperazone/sulbactam combined with moxifloxacin was used for antibiotic treatment. In addition, an oxygen storage mask was placed for continuous oxygen supplementation (oxygen flow rate of 10 liters per minute), and other comprehensive examinations were conducted and treatments provided. He was admitted to the respiratory and critical care unit (RICU) at 3:09 pm on November 4, and stayed in the emergency department for 16 h and 24 min.
Case 2. Patient B was patient A’s wife, a 46-year-old local herdsman like her husband. She had been accompanying and caring for patient A since the onset of his symptoms. Five days prior to admission (October 30), she started to have intermittent fever, dyspnea, and cough with occasionally productive sputum. In addition, she experienced sporadic chest pain, but no hemoptysis. Her maximum recorded body temperature was 38.5 °C, with the fever being reduced by physical cooling. She was also diagnosed with a ‘lung infection’ and was treated at a local hospital, but her symptoms did not improve. Therefore, she and patient A were transferred to Beijing together, and were transferred to the emergency department after routine screening in the fever clinic. Since symptom onset, she had felt ill and listless, and had poor appetite and sleep. Like patient A, she did not provide emergency doctors with information about performing deratization and denied direct contact with live rats.
On physical examination, her temperature was 38.0 °C, pulse was 101 beats per minute, respiratory rate was 20 breaths per minute, blood pressure was 108/69 mmHg, and SpO2 was 84% without oxygen supplementation. When she was wheeled into the clinic, she had a clear sensorium but appeared despondent. Her face looked tired and she sat down repeatedly. Her breathing was rapid but there was no ‘three concave sign’ noted. Her lungs had decreased breath sounds and moist rales were detected. Her heart rate was 101 beats per minute and rhythm was regular. No pathological murmur was heard over each valve auscultation area. The rest of her physical examination was normal.
On November 3, CT images of her chest showed diffuse exudative shadows of both lungs with some mass-like, solid, high-density shadows. The lesions were mainly in the left lung, as shown in Figure 1B. Her routine blood tests, biochemical tests, coagulation studies, ESR, CRP, PCT and immune function results on November 4 are shown in Table 1. Her EKG was normal. We took her sputum for etiological examination, and the results were all negative (including tests for enterovirus 71, metapneumovirus, influenza A virus, influenza B virus, adenovirus, EB virus, new H1N1 influenza virus, respiratory syncytial virus, rhinovirus, cytomegalovirus, Coxsackie virus a16, Legionella pneumophila, Chlamydia pneumoniae, acid-fast organisms, human sporidium, and fungi). Her sputum culture was not abnormal and blood culture was also negative. Her G/GM test results were normal.
At 10:56 pm on November 3, after emergency department registration, the patient was transferred to the infusion area to receive cefoperazone/sulbactam combined with moxifloxacin antibiotic treatment, as well as other comprehensive examinations and treatments such as oxygen inhalation by nasal catheter (3 liters per minute). Because of the intermittent fever and the aggravation of dyspnea, the patient was transferred to the emergency room for close monitoring at 3:41 pm on November 4, and was in the RICU by 2:53 pm on November 5. Her total stay in the emergency department lasted 40 h and 18 min.
Patient A and patient B were admitted to RICU successively. The Center for Disease Prevention and Control (CDC) of Chaoyang District of Beijing examined their bronchoalveolar lavage fluid (BALF) and found them positive for the nucleic acid of Yersinia pestis (November 11), blood and sputum specimens collected from Patient A and B were tested by Beijing CDC and were found to be positive by RT-PCR and colloidal gold fluorescence immunoassay targeting the F1 antigen and by reverse-phase indirect hemagglutination assay. NGS sequencing was weakly positive for Yersinia pestis genetic material[2]. Afterwards, a diagnosis of confirmed pneumonic plague was made through expert consultation. The results are shown in Table 2.
Patient Samples Detection method Result A serum Colloidal gold fluorescence immunoassay for F1 antibody + serum and sputum Colloidal gold fluorescence immunoassay for F1 antigen + serum Reverse-phase hemagglutination assay for F1 antigen + serum and sputum RT-PCR assay + B serum Colloidal gold fluorescence immunoassay for F1 antibody + serum Reverse-phase hemagglutination assay for F1 antigen + serum RT-PCR assay + Table 2. Laboratory test results for human plague case
At 8:00 am on November 12, 2019, the Beijing CDC ordered isolation for medical observation of 37 patients in the emergency rescue room and the emergency observation room, seven of whom were identified as close contacts, and the other 30 as having close contact with the seven. The quarantine was lifted on November 21 (after 9 d). We measured and recorded the body temperature of all 37 individuals daily (every 4 h). Each new patient with fever was monitored for temperature changes and checked for lymphadenopathy. We reported the patient's temperature and other relevant information to the medical administration department at 9:00 a.m. and at 5:00 pm every day. All 37 patients were required to take prophylactic levofloxacin orally or intravenously.
Five patients died during isolation and observation. The CDC tested for Y. pestis fraction 1 (F1) antigen / antibody and nucleic acid in their blood and throat swab samples, and the results were all negative. It was concluded that all the deaths were caused by the patients’ primary diseases. After the end of the isolation and observation period, all 37 patients (including the five who died of their primary diseases) did not exhibit any symptoms and signs associated with pneumonic plague.
At the same time, 30 medical and nursing personnel were also quarantined due to contact with emergency room patients. None showed abnormalities after the disease incubation period, so they were all allowed to return to clinical work after being released from medical observation.
There were also more than 60 medical staff and auxiliary medical staff working in the isolation ward, who exhibited no abnormal findings at the end of ward isolation.
Plague is a Class A infectious disease, as stipulated in the law of the People's Republic of China on infectious diseases. It is spread by plague bacilli through flea bites, respiratory tract infection, skin wound infection and digestive tract infection. The natural foci are distributed in grassland areas of Inner Mongolia, Gansu, Ningxia, Xinjiang and other provinces in China. Both patients who were admitted to our emergency department were herdsmen in one of the plague’s natural foci. Before acquiring the disease, they had a suspicious history of contact through deratization[2]. The onset of symptoms in the two individuals was temporally related, and the results of pathogen nucleic acid testing were positive. They were diagnosed as cases of pneumonic plague through expert consultation. This was also the first confirmed incidence of pneumonic plague (two imported cases) in Beijing since the founding of the People's Republic of China[3]. It is concerning that these two patients were first diagnosed in the emergency department of a large general hospital in a densely populated city and stayed therein for nearly 60 h. We need to pay more attention towards preventing 'hidden' infectious diseases, especially those transmitted by respiratory droplets in the emergency department.
Because the early clinical manifestations of most infectious diseases are often atypical, patients tend to visit the emergency department rather than the 'fever clinic' or infectious disease hospital[4]. As a result, the medical staff in the emergency department may be exposed to the patients’ droplets, blood, body fluids, excreta, etc., underscoring the importance of compliance with standard operating procedures. The triage nurse found that the couple had a common history of fever, and gave the male patient simple airway protection in the form of a mask before sending him to the corresponding diagnosis area. Based on the medical history, particularly the presence of similar clinical symptoms of husband and wife, close attention was paid to the patients despite difficulties in making an immediate accurate diagnosis. In such cases, it is also important for patients to continue to wear masks to isolate their respiratory secretions from the environment. Concurrently, medical staff must take protective measures including the donning of masks and hats, as well as hand disinfection before and after contact with patients. It is worth mentioning that the emergency department began to implement access restrictions in the rescue area in 2017. Family members are only allowed to visit within a specified time, and they need to wear isolation clothes and masks. This measure has been proven to be effective in preventing the spread of disease between patients and their families. In fact, the implemented strategies, which included simple isolation and protection of the respiratory tract, hand disinfection, and control of facility access and visitation, played a important role in the early prevention of pneumonic plague transmission.
Under the direct guidance of CDC professionals in Beijing, the emergency department immediately started appropriate emergency procedures after receiving the epidemic notification on November 12, 2019. First, the rescue room was isolated immediately because of plague patients having been visited and seven patients who had been in close contact with the plague patients being in the hospital. Second, the emergency observation room was transformed into a medical observation ward for isolated patients with suspected disease contact. Third, other patients in the rescue room who had no direct contact with plague patients were transferred to the newly opened second isolation area for observation, and were blocked from exposure to the patients with known close contact. Fourth, the emergency department quickly set up a special rescue team to coordinate with the CDC for daily follow-up. In case of suspected fever in patients under medical observation, the rescue team was instructed to immediately contact the CDC for antigen and antibody screening. At the same time, the rescue team was responsible for the daily medical treatment of the patients in the observation area and for communication with their families, as well as for the occupational protection, disinfection and isolation of the medical staff[5]. In a relatively short period of time, the emergency department completed the set-up of the corresponding isolation area and isolation ward and formed a special rescue team, which played a positive role in the prevention and control of the epidemic. It is the implementation of all of these measures that ensured that during the incubation period of 9 days from plague infection, the 37 patients and 30 medical and nursing personnel who were isolated and under medical observation, as well as 60 medical and nursing personnel and medical assistants who worked in the isolation ward, developed no suspicious symptoms.
The emergency department attaches great importance to relevant public opinion, emphasizing that all publicly communicated information about the epidemic should be jointly approved by the CDC and the hospital in Beijing. During epidemic prevention and control, the operation of the whole department, as well as the staff's mental condition, must be stable. This not only guarantees the safety and stability of medical treatment, but also makes a good social impact, which is in turn closely related to effective public relations.
The emergency department, as the front line and main battlefield of public health event prevention, is continually presented with serious challenges from all kinds of high-risk diseases, including infectious diseases. However, it is often impossible for the emergency department to fully follow all preventive measures for infectious diseases[6]. Therefore, to become the iron gate for public health events, the emergency department needs to constantly improve its standard operating processes, including the implementation of simple and effective measures for preventing the transmission of respiratory diseases, restriction of access to critical areas, a strict visiting system, hand hygiene measures, and measures to increase sensitivity to potential hazards.
We offer special thanks to the following: The RICU medical team, two patients received standardized diagnosis and treatment in the RICU, and made great contribution to the final diagnosis.
The CDC in Beijing and the CDC in Chaoyang District for standardized prevention and control after diagnosis to ensure that no new cases appeared.
Emergency Department Experience in the Multi-dimensional Prevention and Control of Pneumonic Plague in Beijing
doi: 10.3967/bes2020.131
- Received Date: 2020-06-14
- Accepted Date: 2020-11-09
| Citation: | YANG Jun, MEI Xue, ZHAO Li Xin, LIU Ying Qing, WANG Shuo, GUO Shu Bin, HE Xin Hua. Emergency Department Experience in the Multi-dimensional Prevention and Control of Pneumonic Plague in Beijing[J]. Biomedical and Environmental Sciences, 2020, 33(12): 948-952. doi: 10.3967/bes2020.131 |






 Quick Links
Quick Links
 DownLoad:
DownLoad: