-
Obesity is a well-established independent risk factor for colorectal cancer (CRC)[1,2], accounting for an estimated 6% of CRC cases in men and 7% in women worldwide in 2012[3]. This elevated risk is further compounded by dramatic epidemiological trends: from 1975 to 2016, the global prevalence of excess body weight [body mass index (BMI) ≥ 25 kg/m2] surged from 21% to 40% in men and 24% to 40% in women[4]. In China, national estimates from 2015 to 2019 reported that 34.3% of adults were overweight and 16.4% were obese, accompanied by an increasing burden of obesity-related diseases, including metabolic abnormalities and cancers[5–7]. In response to this growing public health challenge, the Chinese government launched the “Weight Management Year” Initiative in 2024. According to a document jointly issued by 16 departments and organizations, a series of measures will be taken to form a supportive environment for weight management, significantly improve the public’s awareness and techniques in weight management, and promote the wider adoption of healthy lifestyles over the next 3 years[8]. These national efforts highlight the importance of addressing obesity not only as a metabolic disorder, but also as a key modifiable risk factor for cancer prevention. In this context, the growing burden of excess body weight and its established association with CRC call for targeted weight-adapted CRC prevention strategies.
Cumulative evidence confirms that early screening reduces CRC-specific incidence and mortality[9,10]. However, the success of screening programs depends heavily on participant adherence[11]. Although screening compliance in average-risk populations has been well studied[12,13], there remains a critical gap in understanding how excess body weight influences screening behaviors and colonoscopy findings. This knowledge gap hinders the optimization of prevention strategies tailored to this vulnerable population.
This study analyzed data from Chongqing’s Ongoing Opportunistic CRC Screening Program (2021–2022), focusing on the effects of excess body weight on colonoscopy adherence and detection outcomes. By providing BMI-specific insights into screening participation and colonoscopic CRC detection, our findings aimed to inform tailored intervention strategies to improve CRC prevention in individuals with excess body weight.
-
This cross-sectional study employed data collected between 2021 and 2022 from an ongoing opportunistic CRC screening program in Chongqing, China. Eligible participants were required to meet the following criteria: (1) registered permanent residents of Chongqing; (2) aged 35–74 years; (3) no history of malignant tumors; (4) no diagnosis of severe heart, brain, or lung diseases or renal dysfunction; (5) no prior participation in the Screening Program in Urban China (CanSPUC); and (6) provision of informed consent. The opportunistic screening program was initiated in 2021 in parallel with the CanSPUC, aiming to expand cancer screening coverage and address the substantial burden of cancers, including CRC. Opportunistic screening was integrated into routine hospital-based health checkups during which eligible individuals were invited to complete a CRC risk assessment using a standardized electronic questionnaire based on a validated risk-scoring system. Participants identified as being at high risk were recommended to undergo colonoscopy within 30 days of the initial risk evaluation. Follow-up was conducted using a combination of active (e.g., telephone calls or home visits) and passive methods (i.e., linkage to cancer registry and mortality surveillance systems) to monitor outcomes. To ensure procedural consistency and data quality, all staff involved were required to hold relevant qualifications and undergo standardized citywide and institutional-level training. Only those who passed the training assessment were permitted to participate in the program implementation. Quality control personnel were designated at both the district and institutional levels. Key quality indicators included the data entry error rate, high-risk rate, detection rate, early diagnosis rate, and follow-up rate. This study was approved by the Ethics Committee of the Chongqing University Cancer Hospital (approval no. CZLL2025-040-001) and written informed consent was obtained from all participants involved in the study.
-
Detailed descriptions of the established risk assessment system from which the CRC risk score was derived have been reported previously[14]. Risk factor data were collected through structured epidemiological questionnaires, including demographic characteristics [age, sex, education level (low: below primary school; medium: completed primary school; high: high school or above)], BMI, lifestyle factors [smoking status (nonsmoker, current smoker, former smoker), drinking status (nondrinker, regular drinker)], family history of CRC, and personal history of colonic polyps. Smokers were defined as individuals who had smoked more than one cigarette per day, either continuously or cumulatively, for at least 6 months. Regular drinkers were defined as those who consumed > 50 g of liquor per day on a persistent basis for >1 year.
-
All colonoscopies were performed in accordance with standardized clinical protocols. Abnormal lesions identified during the procedure were biopsied and subjected to pathological confirmation. Relevant clinical information, including lesion location, size, macroscopic appearance, and pathological diagnosis, was systematically recorded in the screening database.
In this study, advanced adenomas were defined as adenomas meeting any of the following criteria: size ≥10 mm, presence of villous histology, or high-grade dysplasia. The primary outcomes were adherence to colonoscopy and findings. Colonoscopy adherence was defined as the completion of a recommended colonoscopy among high-risk individuals. Colonoscopy findings were classified according to the 10th revision of the International Classification of Diseases (ICD-10), with CRC codes C18–C21.
-
Following the Guidelines for the Diagnosis and Treatment of Obesity (2024 edition) issued by the National Health Commission of China, in this study, participants were classified into two groups based on BMI: normal body weight (18.5 ≤ BMI < 24.0 kg/m2) and excess body weight (BMI ≥ 24.0 kg/m2)[15]. This classification differs from the World Health Organization standard, which defines excess body weight as BMI ≥ 25.0 kg/m2[16]. Baseline characteristics were summarized as frequencies and proportions for categorical variables and as means with standard deviations (SD) for continuous variables. Comparisons between the normal and excess weight groups were performed using standardized differences, calculated as the difference in means or proportions divided by the pooled SD. A standardized difference > 0.1 was considered indicative of a meaningful imbalance. Between-group differences in colonoscopy adherence and lesion detection rates were assessed using Chi-squared or Fisher’s exact tests. Two separate multivariable logistic regression models were constructed to evaluate the factors associated with (1) colonoscopy participation among high-risk individuals and (2) detection of colonic lesions among those who underwent colonoscopy. Analyses were stratified by BMI, with participants categorized into normal and excess body weight groups. Within each BMI stratum, associations between demographic characteristics (age, sex, and education level), lifestyle factors (smoking and drinking status), family history of CRC, history of colonic polyps, and the outcomes of interest were examined. All models were adjusted for ethnic group, occupation, and years of participation. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. All analyses were performed using R (v.4.4.3), with a two-sided P value < 0.05 considered statistically significant.
-
A total of 43,797 eligible residents were enrolled in this study. Due to the limited sample size of underweight participants (n = 1,518), they were excluded from analyses. Ultimately, 42,279 participants were included in the study, of whom 19,462 (46.0%) had excess body weight. During the risk assessment, 7,002 (16.6%) participants were identified as at high risk for CRC, including 3,808 (54.4%) with excess body weight.
The baseline characteristics of all participants and the high-risk subgroup are presented in Supplementary Table S1. Compared with individuals with normal body weight, those with excess body weight were more likely to be male, current or former smokers, and regular alcohol drinkers. In the high-risk subgroup, individuals in the excess body weight group were more likely to be male, older, have lower educational attainment, and less likely to have a history of colonic polyps. The standardized differences for these variables exceeded 0.1, indicating meaningful imbalances between the BMI groups.
Among the high-risk individuals, 595 completed colonoscopy screening, resulting in an overall adherence rate of 8.5%. As shown in Table 1, a significantly lower overall adherence rate (P < 0.001) was observed in individuals with excess body weight [253 (6.6%)] than in those with normal body weight [342 (10.7%)]. This pattern remained consistent across sex and age subgroups. Specifically, adherence rates were lower in excess body weight participants for both men (8.3% vs. 13.7%, P < 0.001) and women (4.7% vs. 8.8%, P < 0.001). Similarly, significantly lower adherence in individuals with excess body weight was observed in several age groups: 40–44 years (6.0% vs. 10.1%, P = 0.029), 50–54 years (6.7% vs. 9.8%, P = 0.036), 55–59 years (7.7% vs. 13.9%, P < 0.001), 65–69 years (5.8% vs. 16.3%, P < 0.001), and 70–74 years (4.1% vs. 13.8%, P = 0.007). The largest disparity in adherence was observed in the 65–69 age group, with a difference of -10.5 percentage points.
Table 1. Comparison of colonoscopy screening participation rate between normal body weight group and excess body weight group in a high-risk population (Overall and Stratified Analyses)
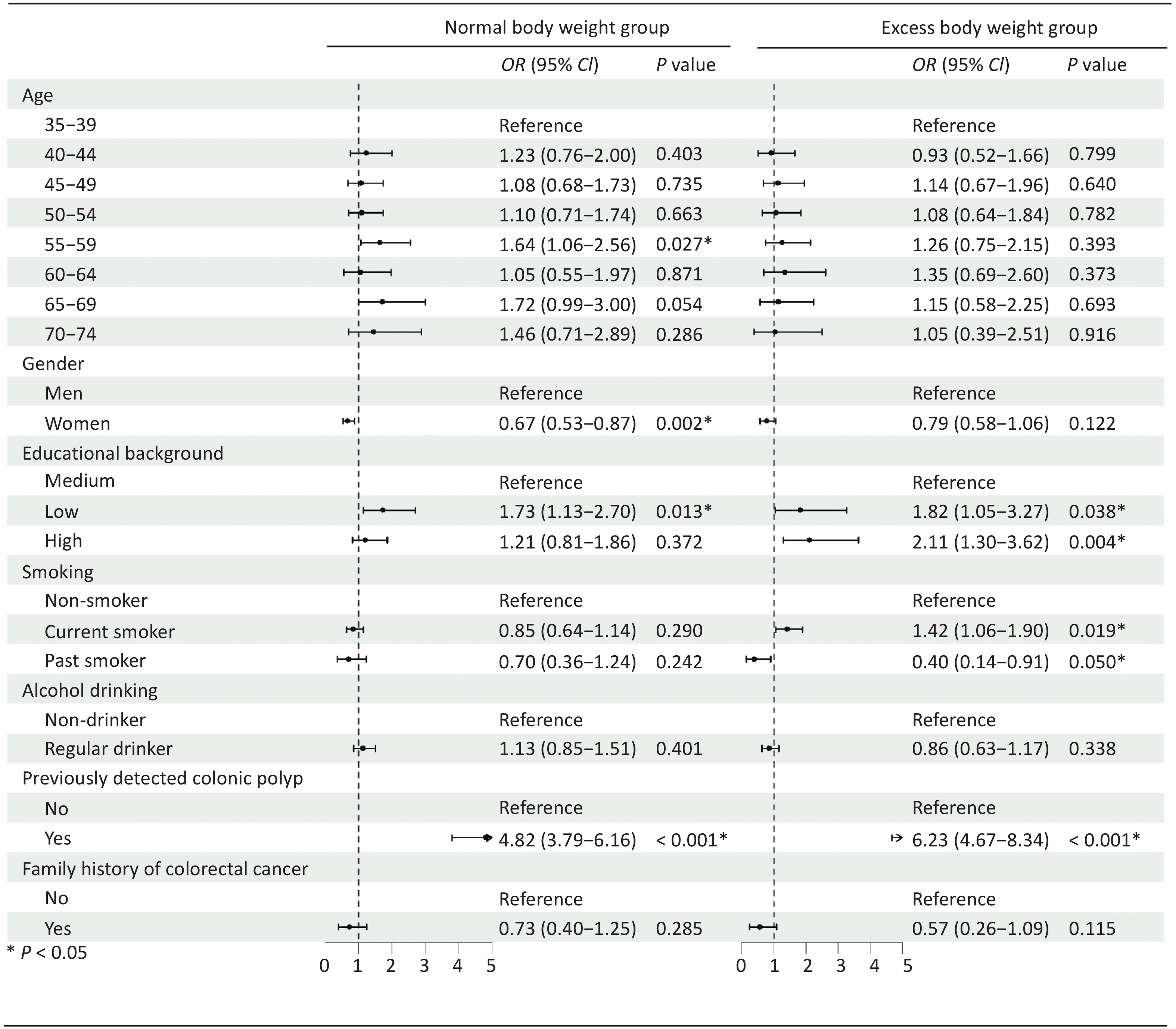
Normal body weight group (n = 3194) Excess body weight group (n = 3808) Difference in participation rate P value Overall 342 (10.7) 253 (6.6) −4.1 < 0.001 Gender stratification Men 170 (13.7) 172 (8.3) −5.4 < 0.001 Women 172 (8.8) 81 (4.7) −4.1 < 0.001 Age stratification 35–39 37 (7.6) 24 (5.8) −1.8 0.340 40–44 41 (10.1) 29 (6.0) −4.1 0.029 45–49 50 (9.0) 45 (6.9) −2.1 0.212 50–54 65 (9.8) 53 (6.7) −3.1 0.036 55–59 84 (13.9) 57 (7.7) −6.2 < 0.001 60–64 17 (9.8) 20 (8.5) −1.3 0.791 65–69 33 (16.3) 18 (5.8) −10.5 < 0.001 70–74 15 (13.8) 7 (4.1) −9.7 0.007 Note. Data were represented as n (%). Among participants with excess body weight, those with either lower [OR 1.82 (95% CI 1.05–3.27), P = 0.038] or higher [OR 2.11 (95% CI 1.30–3.62), P = 0.004] levels of education were more likely to undergo colonoscopy compared to those with medium educational background. Current smokers [OR 1.42 (95% CI 1.06–1.90), P = 0.019] and participants with a history of detected colonic polyps [OR 6.23 (95% CI 4.67–3.84), P < 0.001] were also more likely to adhere to colonoscopy screening. In contrast, past smokers were less likely to undertake colonoscopy than non-smokers [OR 0.40 (95% CI 0.14–0.91), P = 0.050]. Among the participants with normal body weight, colonoscopy screening adherence was significantly higher in individuals aged 55–59 years, males, those with lower educational attainment, and those with a history of colonic polyps (Figure 1).
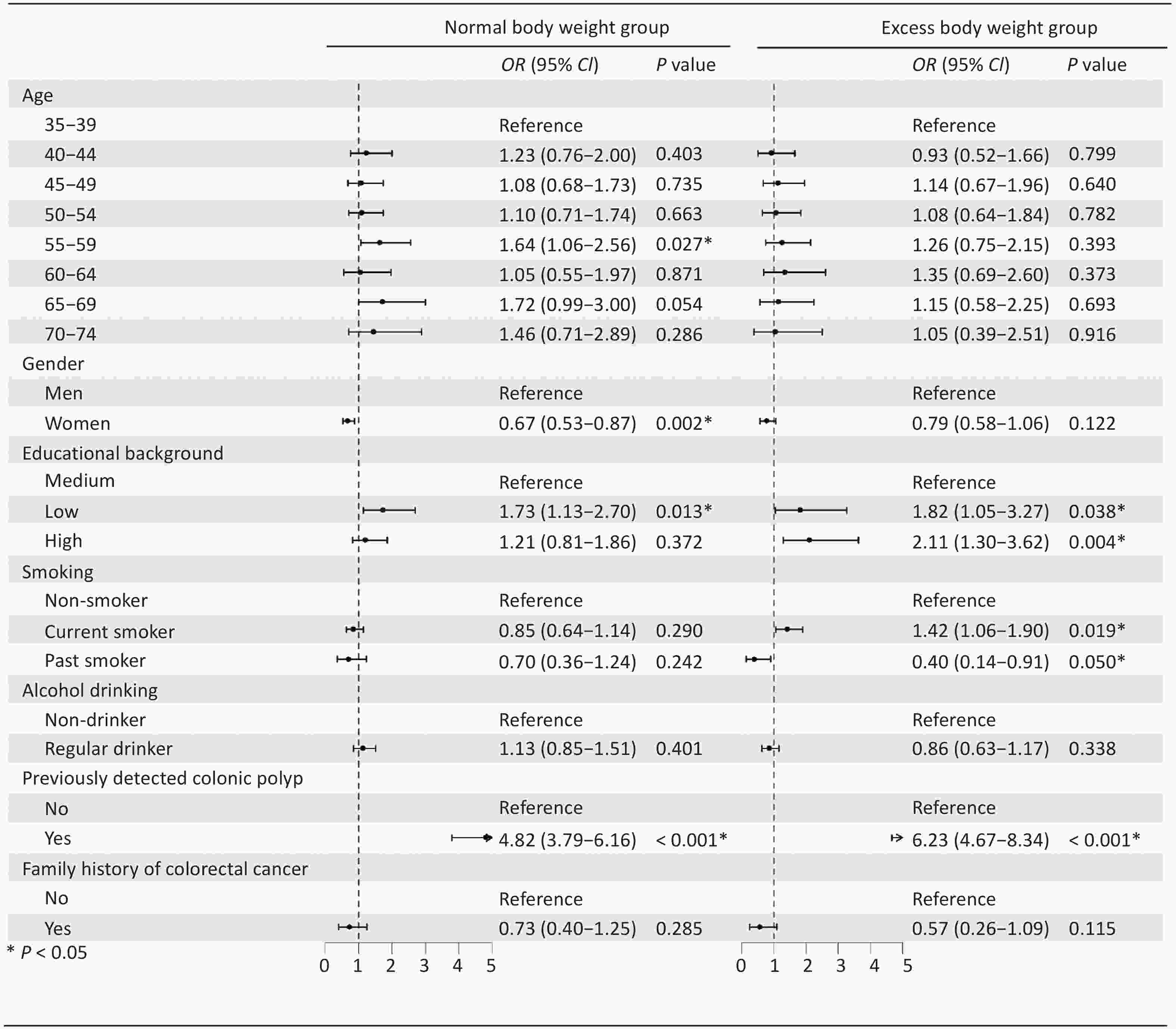
Figure 1. Odds ratios (OR) of risk factors associated with participation rate in normal body weight and excess body weight group. *P<0.05
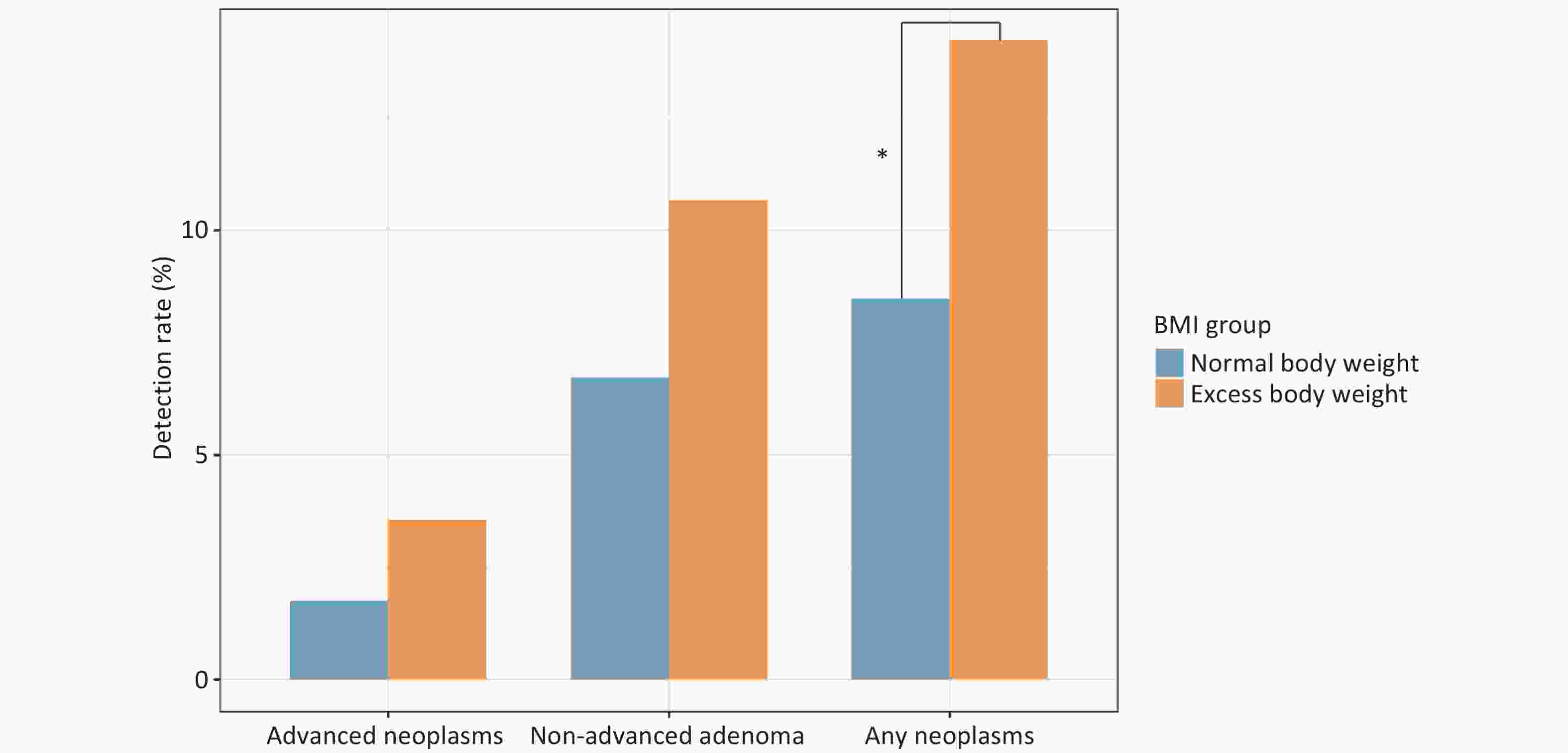
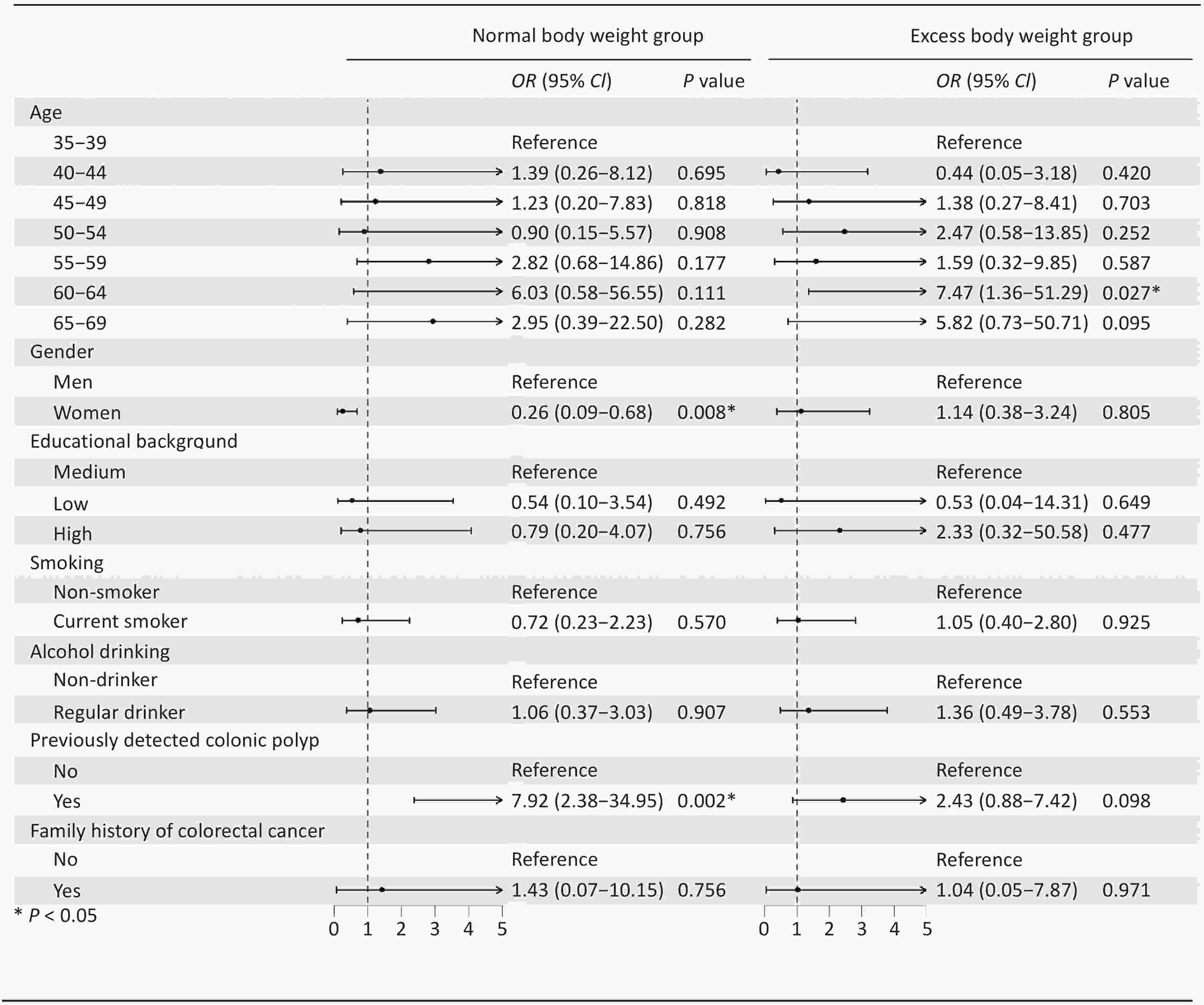
Figure 2 illustrates the colonoscopy findings in the normal and excess body weight groups during the initial screening round. The overall detection rates were 2.52% for advanced neoplasms (n = 15), 8.40% for non-advanced adenomas (n = 50), and 10.92% for any neoplasm (n = 65; the sum of advanced and non-advanced adenomas). Across all three categories, participants with excess body weight exhibited higher detection rates than those with normal body weight (advanced neoplasms, 3.56% vs. 1.75%; non-advanced adenomas, 10.67% vs. 6.73%; neoplasms, 14.23% vs. 8.48%). The difference in the detection rates for any neoplasm was statistically significant (P < 0.05). The multivariate logistic regression results for any neoplasm detection are presented in Figure 3. Distinct association patterns were observed between normal and excess body weight groups. In the normal weight group, women were less likely to have any neoplasm detected [OR 0.26 (95% CI 0.09–0.68), P = 0.008], while participants with a history of colonic polyps were more likely to have a detection [OR 7.92 (95% CI 2.38–34.95), P = 0.002]. In the excess body weight group, individuals aged 60–64 were more likely to have any neoplasm detected [OR 7.47 (95% CI 1.36–51.29), P = 0.027].
-
This study highlighted excess body weight as an important health determinant that negatively influences both participation in CRC screening and the burden of neoplastic findings. Individuals with excess body weight were significantly less likely to adhere to colonoscopy screening recommendations, yet had a markedly higher detection rate of colorectal neoplasms than those with normal body weight. This “low adherence, but high detection rate” disparity emphasizes the need to address body weight as a critical target in CRC prevention strategies.
Our study identified a significant decrease in colonoscopy screening adherence among individuals with excess body weight compared with those with normal body weight (6.6% vs. 10.7%, P < 0.001), with consistent disparities across all age and sex subgroups. This BMI-dependent disparity in adherence aligns with reports from Germany's prospective CRC screening cohort and England’s nationwide fecal occult blood test (FOBT)-based program[17,18], although some studies have reported contradictory findings, likely due to differences in the screening program design and definitions of adherence[19–21]. Health literacy has been recognized as a key factor in both the development of obesity and shaping preventive health behaviors, which may partly explain the lower adherence observed among individuals with excess body weight[22]. Moreover, because obesity is often a stigmatizing condition, individuals with obesity may experience communication barriers or discomfort in healthcare interactions, which could indirectly contribute to reduced screening adherence[23]. Physical discomfort may also act as a structural barrier to participation in screening among the obese population. These findings underscore the need to create supportive health environments for obese individuals, including targeted health education and improved provider communication. Interestingly, distinct associations between participant characteristics and colonoscopy adherence were observed among individuals with excess body weight, which differed from those in the normal weight group. These findings suggest that the behavioral drivers of screening may vary by BMI group and highlight the need for tailored strategies that account for unique motivators within different BMI groups.
Importantly, higher colonoscopic detection rates for both non-advanced and advanced colorectal neoplasms were observed in participants with excess body weight, which is consistent with the well-established association between obesity and CRC risk[1,2,24]. Although some subgroup differences did not reach statistical significance, likely due to limited power, the overall trend underscored the elevated baseline risk in this population. Moreover, distinct patterns were observed in lesion detection between BMI groups. In normal-weight individuals, sex and a history of polyps influenced detection, whereas in the excess body weight group, older age was the dominant factor. These findings highlight the significant role of excess body weight as a health determinant that may shape risk profiles and detection patterns, thus warranting BMI-specific risk stratification.
This “low adherence, high detection rate” disparity observed in our study emphasizes the need to address body weight as a critical target in CRC prevention strategies. Therefore, health education for excess weight individuals should integrate weight management with messages promoting CRC screening. National initiatives such as China’s “Weight Management Year” have already demonstrated the feasibility of population-level interventions through public education, engagement, and advocacy. Building on these experiences and acknowledging the evidence that both patient-level (e.g., knowledge and risk perception) and provider-level factors (e.g., attitudes and recommendations) influence screening behaviors, tailored strategies should be developed to enhance screening benefits among individuals with excess body weight. For instance, invitation protocols could highlight the elevated CRC risk and the potential benefits of screening when communicating with obese participants. Healthcare staff training should also address weight-related stigma, and implementing tailored navigation systems targeting this subgroup with standardized protocols may further improve adherence.
To the best of our knowledge, this is the first study to specifically examine excess body weight as a health determinant in relation to CRC screening behaviors and detection outcomes, providing evidence to support the development of tailored preventive strategies for this population. Nevertheless, this study had certain limitations. First, the use of self-reported questionnaire data may have introduced recall bias. Second, the participants were recruited from a single geographic region, which may limit the generalizability of our findings to other populations. Third, the exclusion of underweight individuals may have introduced a potential selection bias. Fourth, the relatively small number of patients with advanced neoplasia may have reduced the statistical power of the subgroup analyses. Finally, we were unable to account for certain unmeasured variables, such as prior FOBT history, which could potentially influence screening behavior.
In conclusion, excess body weight significantly affected CRC screening behavior and outcomes. Individuals with excess body weight demonstrated lower screening adherence and higher detection rates of colorectal neoplasms, highlighting the urgent need for integrated public health strategies that enhance CRC screening engagement within this high-risk population.
doi: 10.3967/bes2025.153
Excess Body Weight and Its Influence on Colonoscopy Adherence and Findings: Results from an Opportunistic Colorectal Cancer Screening Program in Chongqing
-
Abstract:
Objective To examine the effect of excess body weight on adherence and lesion detection in colorectal cancer (CRC) screening. Methods A cross-sectional analysis was conducted within an opportunistic CRC screening program in Chongqing , which enrolled 43,797 adults aged 35–74 years between 2021 and 2022. A total of 42,279 participants were included in the final analysis, of whom 19,462 (46.0%) had excess body weight (BMI > 24.0 kg/m2). Colonoscopy adherence and detection were compared between normal and excess body weight group, and associated factors were examined. Results Of the 7,002 participants recommended for colonoscopy, 3,808 (54.4%) had excess body weight. Adherence was significantly lower in the excess weight group (6.6%) than in the normal weight group (10.7%, P < 0.001), and this trend was consistent across sex and age groups. The detection rates of advanced neoplasms (3.6% vs. 1.8%) and non-advanced adenomas (10.7% vs. 6.7%) were higher in the excess weight cohort, with a significant difference for any neoplasm (14.2% vs. 8.9%, P < 0.05). Differences in adherence- and detection-related factors were also observed between the groups. Conclusion Excess body weight was associated with lower colonoscopy adherence but higher neoplasm detection. These findings support the integration of weight management with targeted screening promotion to improve CRC prevention in this high-risk population. -
Key words:
- Colorectal cancer /
- Obesity /
- Overweight /
- Opportunistic screening /
- Colonoscopy
The authors have no relevant financial or nonfinancial interests to disclose.
This study was approved by the Ethics Committee of the Chongqing University Cancer Hospital (approval no. CZLL2025-040-001) and written informed consent was obtained from all participants involved in the study.
&These authors contributed equally to this work.
注释:1) Authors’ Contributions: 2) Competing Interests: 3) Ethics: -
Table 1. Comparison of colonoscopy screening participation rate between normal body weight group and excess body weight group in a high-risk population (Overall and Stratified Analyses)
Normal body weight group (n = 3194) Excess body weight group (n = 3808) Difference in participation rate P value Overall 342 (10.7) 253 (6.6) −4.1 < 0.001 Gender stratification Men 170 (13.7) 172 (8.3) −5.4 < 0.001 Women 172 (8.8) 81 (4.7) −4.1 < 0.001 Age stratification 35–39 37 (7.6) 24 (5.8) −1.8 0.340 40–44 41 (10.1) 29 (6.0) −4.1 0.029 45–49 50 (9.0) 45 (6.9) −2.1 0.212 50–54 65 (9.8) 53 (6.7) −3.1 0.036 55–59 84 (13.9) 57 (7.7) −6.2 < 0.001 60–64 17 (9.8) 20 (8.5) −1.3 0.791 65–69 33 (16.3) 18 (5.8) −10.5 < 0.001 70–74 15 (13.8) 7 (4.1) −9.7 0.007 Note. Data were represented as n (%). -
[1] Rask-Andersen M, Ivansson E, Höglund J, et al. Adiposity and sex-specific cancer risk. Cancer Cell, 2023; 41, 1186-97. e4. [2] Lauby-Secretan B, Scoccianti C, Loomis D, et al. Body fatness and cancer—viewpoint of the IARC working group. N Engl J Med, 2016; 375, 794−8. doi: 10.1056/NEJMsr1606602 [3] Pearson-Stuttard J, Zhou B, Kontis V, et al. Worldwide burden of cancer attributable to diabetes and high body-mass index: a comparative risk assessment. Lancet Diabetes Endocrinol, 2018; 6, E6−15. [4] NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet, 2017; 390, 2627−42. doi: 10.1016/S0140-6736(17)32129-3 [5] Pan XF, Wang LM, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol, 2021; 9, 373−92. doi: 10.1016/S2213-8587(21)00045-0 [6] Liu C, Yuan YC, Guo MN, et al. Rising incidence of obesity-related cancers among younger adults in China: a population-based analysis (2007-2021). Med, 2024; 5, 1402-12. e2. [7] Xiao TL, Yuan SQ, Gao JY, et al. Predictive ability of hypertriglyceridemic waist, hypertriglyceridemic waist-to-height ratio, and waist-to-hip ratio for cardiometabolic risk factors clustering screening among Chinese children and adolescents. Biomed Environ Sci, 2024; 37, 233−41. [8] The State Council the People's Republic of China. China launches 3-year campaign on public weight management. https://english.www.gov.cn/news/202406/26/content_WS667c12e4c6d0868f4e8e8975.html. [2025-11-05] [9] Schreuders EH, Ruco A, Rabeneck L, et al. Colorectal cancer screening: a global overview of existing programmes. Gut, 2015; 64, 1637−49. doi: 10.1136/gutjnl-2014-309086 [10] Atkin W, Wooldrage K, Parkin DM, et al. Long term effects of once-only flexible sigmoidoscopy screening after 17 years of follow-up: the UK Flexible Sigmoidoscopy Screening randomised controlled trial. Lancet, 2017; 389, 1299−311. doi: 10.1016/S0140-6736(17)30396-3 [11] D’Andrea E, Ahnen DJ, Sussman DA, et al. Quantifying the impact of adherence to screening strategies on colorectal cancer incidence and mortality. Cancer Med, 2020; 9, 824−36. doi: 10.1002/cam4.2735 [12] Chen HD, Li N, Ren JS, et al. Participation and yield of a population-based colorectal cancer screening programme in China. Gut, 2019; 68, 1450−7. doi: 10.1136/gutjnl-2018-317124 [13] Senore C, Inadomi J, Segnan N, et al. Optimising colorectal cancer screening acceptance: a review. Gut, 2015; 64, 1158−77. doi: 10.1136/gutjnl-2014-308081 [14] Dong XS, Du LB, Luo ZL, et al. Combining fecal immunochemical testing and questionnaire-based risk assessment in selecting participants for colonoscopy screening in the Chinese National Colorectal Cancer Screening Programs: a population-based cohort study. PLoS Med, 2024; 21, e1004340. doi: 10.1371/journal.pmed.1004340 [15] National Clinical Practice Guideline on Obesity Management Editorial Committee. National clinical practice guideline on obesity management (2024 edition). Chin Circ J, 2025; 40, 6−30. (In Chinese) [16] World Health Organization. Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. [2025-11-05] [17] Guo F, Chen C, Schöttker B, et al. Changes in colorectal cancer screening use after introduction of alternative screening offer in Germany: prospective cohort study. Int J Cancer, 2020; 146, 2423−32. doi: 10.1002/ijc.32566 [18] Blanks RG, Benson VS, Alison R, et al. Nationwide bowel cancer screening programme in England: cohort study of lifestyle factors affecting participation and outcomes in women. Br J Cancer, 2015; 112, 1562−7. doi: 10.1038/bjc.2015.69 [19] Kendall KA, Lee E, Zuckerman IH, et al. Obesity status and colorectal cancer screening in the United States. J Obes, 2013; 2013, 920270. [20] Gangcuangco LMA, Rivas T, Basnet A, et al. Factors associated with colorectal cancer screening adherence and the impact of COVID-19 on screening patterns in Connecticut, USA. Intern Emerg Med, 2022; 17, 2229−35. doi: 10.1007/s11739-022-03053-2 [21] Li JB, Ke KJ, Zhang WL, et al. Factors associated with adherence to colonoscopy among individuals who were positive in the preliminary screening for colorectal neoplasms. Cancer Med, 2022; 11, 4321−31. doi: 10.1002/cam4.4730 [22] Upton A, Spirou D, Craig M, et al. Health literacy and obesity: a systematic scoping review. Obes Rev, 2025; 26, e13904. doi: 10.1111/obr.13904 [23] Phelan SM, Burgess DJ, Yeazel MW, et al. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev, 2015; 16, 319−26. doi: 10.1111/obr.12266 [24] Bhaskaran K, Douglas I, Forbes H, et al. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5·24 million UK adults. Lancet, 2014; 384, 755−65. doi: 10.1016/S0140-6736(14)60892-8 -




 下载:
下载:



 Quick Links
Quick Links