-
Life course epidemiology should practically illustrate how risk exposures and their dynamic changes influence the occurrence, development and prognosis of chronic diseases from early life to the elderly. This paper develops the lifespan risk exposure measurement instrument (LREMI) in the framework of retrospective study to collect lifestyle, diet, physical activity information across subjects' life courses from 18-years-old to current age. Through a pilot study, the result of the test-retest analysis demonstrated the reliability of LREMI. In Shandong Multicenter Cohort, the LREMI showed its feasibility, for it could measure the exposure spectrum on both individuals and population with different life experiences. Moreover, it had good differentiation ability for identifying cases versus controls in population-based case-control study. However, further studies should be conducted in an already available prospective cohort to ascertain that our results could match prospective data.
Life course epidemiology is an emerging epidemiological domain encompassing the study of chronic disease, which is the study of long-term effects on chronic disease risk of physical and social exposures during the course of one's life (gestation, childhood, adolescence, young adulthood and later adult life). This includes studies of how biological, behavioral and psychosocial pathways operate across an individual's life to influence the development of chronic diseases [1]. Theoretically, there have been proposals for both critical period models and risk accumulation conceptual models [1-4]. Critical period models identifies critical periods in which exposures have lasting or lifelong effects on the structure or function of an organism, while risk accumulation conceptual model captures patterns of exposure accumulation, raising disease risk by accumulating gradually over the life course /by combining at each life stage [1, 4]. Practically, for both models, life course epidemiology should illustrate how risk exposures and their dynamic changes influence the occurrence, development and prognosis of chronic diseases from early to later life [1-4]. However, it challenges data collection in epidemiological practice.
Ideally, for measuring the effects of lifespan exposures and their dynamic changes on the occurrence of chronic disease, a real-time longitudinal cohort must be built to collect exposures continuously. However, longitudinal cohort design could only collect the risk exposures discontinuously by restricting to limit measuring times within a specific time window [5]. In addition, it is much expensive and requires a long time to follow up. To our knowledge, there has been neither long-term longitudinal follow-up study in China, nor information on lifestyles in China before 1990. Accordingly, the only way to investigate the association of lifetime exposures with chronic disease was adopting retrospective study design for life course epidemiological study to provide an approximation of that by gathering retrospective data.
Therefore, although recall bias inevitably affects retrospective data collection, one might use it to feasibly collect exposures and their dynamic changes during a lifespan according to life course epidemiology research. For common lifestyle factors, such as smoking, drinking, diet habits, etc., usually, it is easy for participants to report their exposure experiences. This process allows us to demonstrate the dynamic changes of lifetime exposures [6], as well as explore how these time-varying exposures affect the occurrence, development and prognosis of chronic diseases. This paper develops the lifespan risk exposure measurement instrument (LREMI) in the framework of retrospective study so as to provide a simple and practical tool for life course epidemiology research. We demonstrate its reliability through a pilot study, and its feasibility and effectiveness through cohort and case-control studies. In the cohort study, we explore whether the LREMI could measure exposure spectrum on both individuals and populations with different life experiences. Moreover, in the case-control study, we will illustrate whether it had good differentiation ability to identify diseased (case) and healthy (control) status in the population.
Using a retrospective approach, we created the LREMI to collect data concerning lifestyles, diet, physical activities and other key risk factors of exposure experiences continuously over the course of subjects' lives. In design philosophy, LREMI attempts to capture the dynamic changing experiences and the turning point (cutoff) of the specific exposure factor across an individual's life course from 18-years-old to current age. In addition, we developed an app in the iOS system to help collect lifespan exposure experience and make the dynamic changing process more visual. In our LREMI app, the real-time exposure changing process could be presented dynamically with the input of exposure information; therefore, the individual's exposure spectrum in the whole life course could be presented when investigating. With the app's assistance, it was easy to check accuracy and completion during rather than after the questionnaire research, for both investigator and respondent [7].
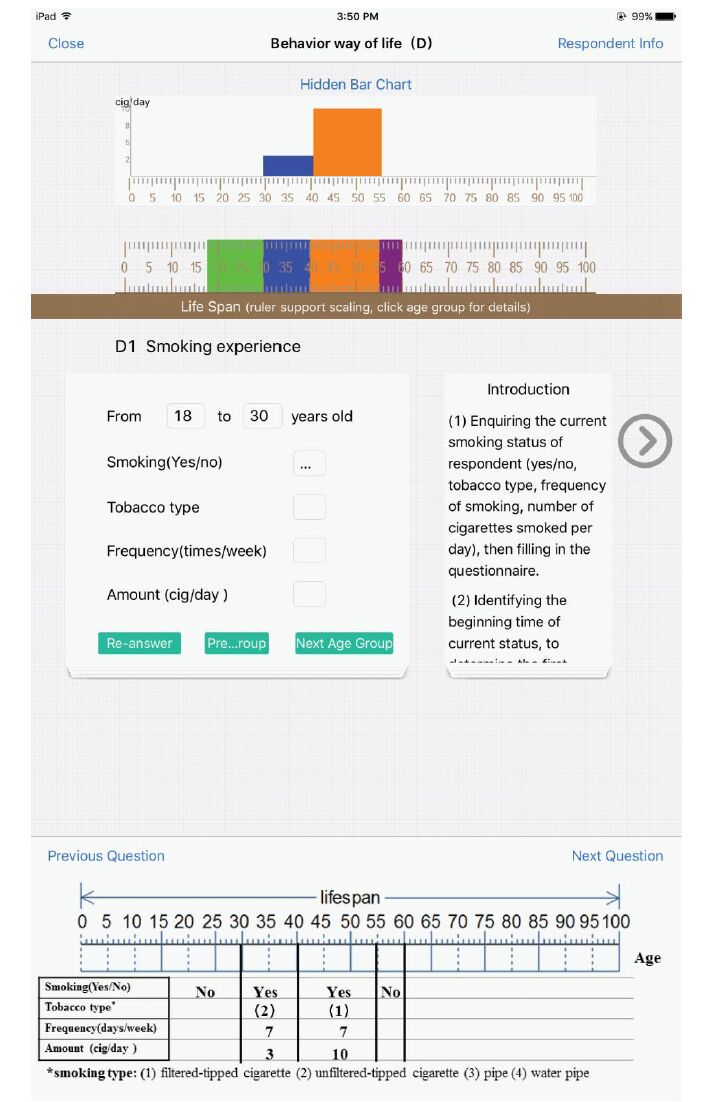
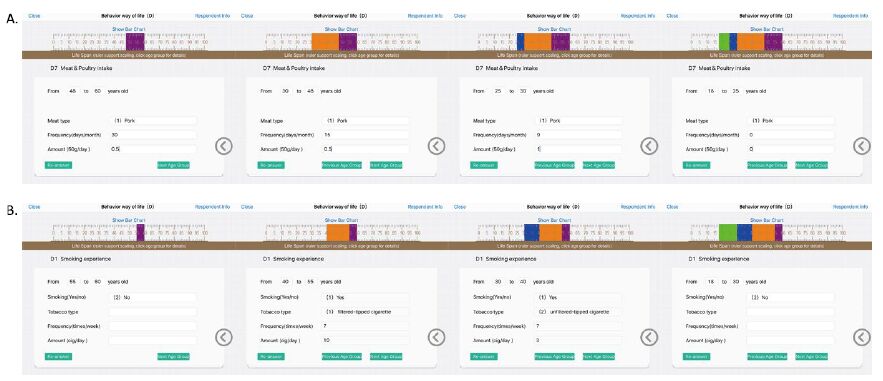
Supplement Material and Methods (Figure S1, Figure S2, see www.besjournal.com) presents the process of investigating a 60-year-old man for meat intake and smoking by using the LREMI app. The process of investagating meat intake was 1) enquiring as to the current meat intake status of the respondent (meat type, frequency of meat intake, amount), then filling in the questionnaire; 2) identifying the beginning time of current status, to determine the first turning point; 3) obtaining the meat intake status before the first turning point and the duration of it using the same routine in step 1, thereby estbalishing the second turning point; 4) repeating the whole process until getting the status of the age of 18 years.

Figure Figure S1. Introduction on how to fill in the lifespan risk exposure measurement instrument (LREMI) (A). The collecting of lifespan meat intake using Lifespan Risk Exposure Measurement Instrument (LREMI). 1) Enquiring as to the current meat intake status of the respondent (meat type, frequency of meat intake, amount), then filling in the questionnaire; 2) Identifying the beginning time of current status, to determine the first turning point; 3) Obtaining the meat intake status before the first turning point and the duration of it using the same routine in step 1, thereby establishing the second turning point; 4) Repeating the whole process until getting the status of the age of 18 years. See the bar chart below for the screenshot of LREMI app. With the input of exposure information, the average amount of smoking in the whole life-course could be presented dynamically, and it was easy for both investigator and respondent to check accuracy and completion during rather than after the questionnaire research. (B). The collecting of lifespon smoking using LRMEI. 1) Enquiring as to the current smoking status of the respondent (yes/no, tobacco type, frequency, amount), then filling in the questionnaire; 2) Identifying the beginning time of current status, to determine the first turning point; 3) Obtaining the smoking status before the first turning point and the duration of it using the same routine in step 1, thereby establishing the second turning point; 4) Repeating the whole process until getting the status of the age of 18 years.

Figure Figure S2. The lifespan smoking experience of a 60-year-old man, whose data was collected by using Lifespan Risk Exposure Measurement Instrument (LREMI).
The design of Shandong Multicenter Chronic Diseases Cohort (SD-MCS) and Yiyuan Population- based Case-Control Study was in the supplement materials. Before these two studies, we conducted a pilot study in early 2012. We conducted the test and retest survey in a random sample of 100 individuals in Yiyuan County in an interval of 20 days. The test-retest statistical method was used in the pilot study to assess the reliability of the LREMI with concern to the intra-class correlation coefficient (ICC).
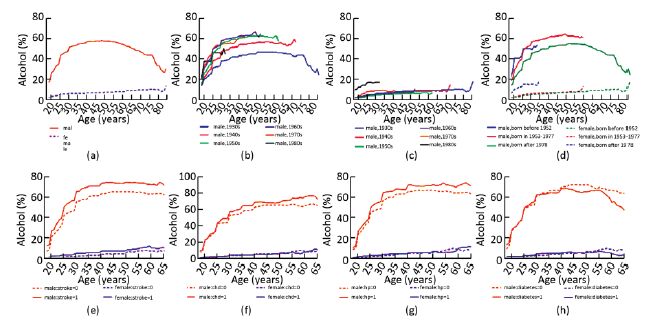
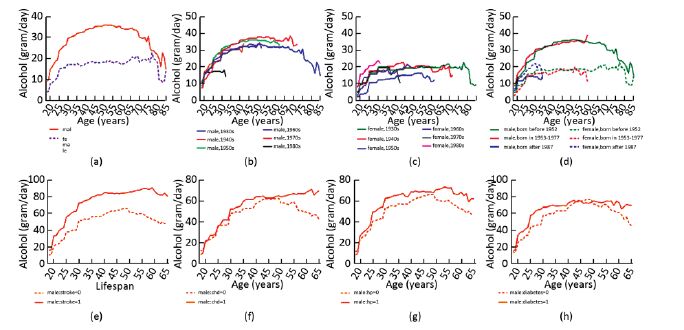
Then, we applied the calibrated LREMI in SD-MCS to assess whether it could measure and demonstrate the exposure spectrum for both individuals and population with different life experiences. To summarize and compare the distribution and dynamic pattern of each exposure factor between different compared groups (different gender and birth year), we then calculated mean and proportion with age-birth cohort curves to show the trends according to age for each sub-group.
The LREMI was further applied in a population- based case-control study to assess whether it could differentiate disease status. The exposure spectrums of each factor in different disease groups were calculate, including stroke and non-stroke, coronary heart disease (CHD) and non-CHD, hypertension and non-hypertension, as well as diabetes and non-diabetes. Line charts helped visualize their dynamic distribution, as well as demonstrate a trend of mean or percentage with the increasing of age between the case and control groups. All statistical analyses were performed using SAS statistical software V.9.2 (Cary, North Carolina, USA).
Table 1 shows the sample proportion of SD-MCS grouped by birth year in the total sample, males and females, respectively.
Item Total (%) Male (%) Female (%) Birth year 1930s 1, 266 (11.84) 628 (13.52) 638 (10.55) 1940s 2, 069 (19.34) 1, 030 (22.17) 1, 039 (17.18) 1950s 3, 049 (28.51) 1, 444 (31.08) 1, 605 (26.54) 1960s 2, 452 (22.92) 983 (21.16) 1, 469 (24.29) 1970s 1, 636 (15.30) 533 (11.47) 1, 103 (18.24) 1980s 222 (2.08) 28 (0.60) 194 (3.21) Total 10, 696 4, 648 6, 048 Table 1. Sample Size of the Shandong Multicenter Chronic Diseases Cohort (SD-MCS)
For the Yiyuan case-control study, there were 631 stroke cases, 596 CHD cases, 862 hypertension cases, 613 diabetes cases and their 1:1 age and sex matched controls (free of the above four diseases). The detailed sample characteristics are available in the supplement (Table S1, see in the website of BES, www.besjournal.com).
Age Stroke CHD Hypertension Diabetes Male Female Male Female Male Female Male Female C D C D C D C D C D C D C D C D 31- 1 1 0 0 0 0 0 0 6 6 2 2 0 0 2 2 36- 1 1 2 2 0 0 0 0 6 6 5 5 2 2 1 1 41- 9 9 4 4 2 2 7 7 17 17 36 36 9 9 22 22 46- 19 19 21 21 6 6 21 21 30 30 75 75 18 18 28 28 51- 34 34 32 32 20 20 62 62 48 48 74 74 36 36 58 58 56- 49 49 60 60 25 25 90 90 49 49 90 90 30 30 90 90 61- 65 65 55 55 36 36 74 74 65 65 74 74 35 35 74 74 66- 49 49 59 59 28 28 59 59 53 53 59 59 23 23 59 59 71- 42 42 39 39 42 42 39 39 42 42 39 39 24 24 39 39 76- 34 34 28 28 34 34 28 28 34 34 28 28 23 23 28 28 81- 18 18 10 10 13 13 10 10 20 20 10 10 2 2 10 10 Table TableS1. Sample Size of Yiyuan Population-based case-Control Study
The results of the reliability test show that the ICC ranges from 0.85 to 0.98, indicating that most variables are reliable (Table S2, see in the website of BES, www.besjournal.com).
Variable ICC Smoking 0.8806 Drinking 0.9838 Tea drinking 0.9232 Fruit intake 0.8717 Vegetable intake 0.9161 Meat intake 0.9717 Egg intake 0.9504 Fish intake 0.9393 Edible food 0.8582 Grain intake 0.9764 Oil intake 0.9968 Pickle intake 0.9823 Physical activity 0.8785 Table TableS2. Reliability Test of LREMI by the Intra-class Correlation Coefficient (ICC)
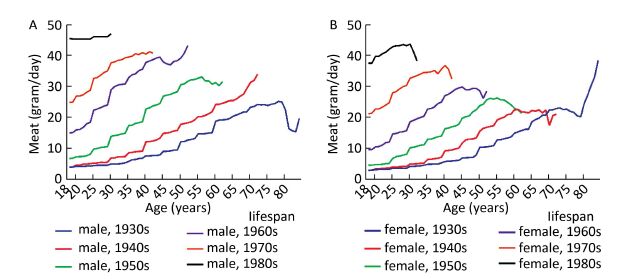
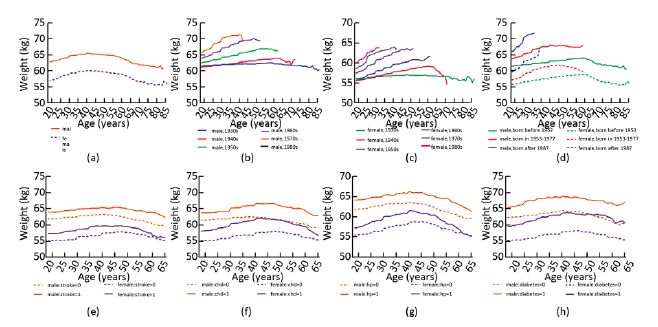
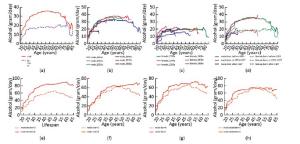
Figure 1 illustrates trends of average daily intake of meat with age for each birth cohort in males and females, respectively. Obviously, the average daily intake of meat was increasing continuously with age increment in each age-birth cohort curve. At the same age, the average daily intake of meat differed significantly in the different age-birth cohort curve; the later the birth year, the greater amount of meat intake. At 30-years-old, the average meat intake in females born in the 1980s was approximately 10 times than those born in 1930s, with a mean daily amount of 43.8 g in comparison to 4.3 g. Supplement Figure S3 a-d, S4 a-d and S5 a-d (see in the Supplement Results, www.besjournal.com) also present the age-birth cohort curves illustrating the exposure spectrum of alcohol drinking and self-reported weight in different birth cohorts.
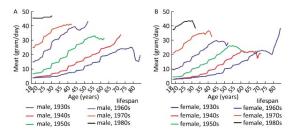
Figure 1. The average meat intake (grams/d) with age (X-axis) in Shandong Multicenter Chronic Diseases Cohort for different birth cohort in male (A) and in female (B).
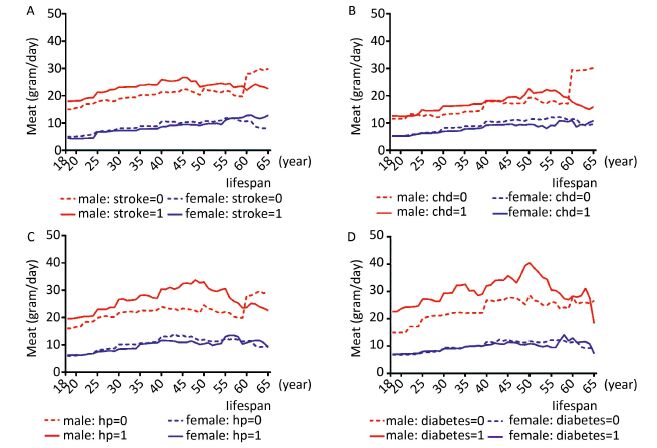
Figure 2 presents the average levels of meat intake in the disease (stroke, CHD, hypertension, and diabetes) and control groups, respectively. In general, the average amount of meat intake was higher in males than in females. As for cases and controls, in male meat consumptions in the disease groups (stroke, CHD, hypertension and diabetes) was higher than that in the controls. In the females, meat consumption in the disease groups was less than in the controls. In addition, the prevalence and amount of drinking and the changes in body weight appear in the Supplement Results (Supplement Figure S3 e-f, S4 e-f and S5 e-f, www.besjournal.com)
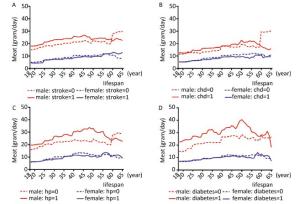
Figure 2. The average meat intake (grams/day) with age (X-axis) in Yiyuan population-based case-control study, for stroke (A), coronary heart disease (CHD, B), hypertension (HP, C) and diabetes (D) vs. controls free of the above four diseases.
This study proposes a feasible and effective tool for data collection in life course epidemiology research. To our knowledge, there has been no long-term longitudinal follow-up study in China. We designed the LREMI to collect retrospective life course exposure experience data. Through using LREMI, we collected longitudinal information on lifestyles, diet, physical activities and other key CVD-related risk factors of exposure experiences across the life course in the SD-MCS cohort and Yiyuan case-control study. These data can facilitate understanding as to how the dynamic changes of lifespan exposures affect the occurrence, development and prognosis of chronic diseases for rural populations in China, which is essential for the analysis of life course epidemiology researches. As there are no studies to consider the impact of lifetime exposure and even no records of exposures of lifestyles before 1990s in Chinese population, and prospective cohort study would be far more expensive and requires a long time, this study is valuable in supplying the impact of lifetime exposures on the risk of chronic diseases.
We demonstrated the feasibility of our LREMI tool with the SD-MCS cohort study, for it could measure the exposure spectrum in both individuals and populations with different exposure experiences. At the individual level, the LREMI could definitely show the real-time dynamic changes of exposure in the process of interviewing, with the assistance of the corresponding app. At the population level, age-birth cohort curves showed in Figure 1 demonstrated the exposure spectrum of meat intake, and illustrated obviously different trends of lifestyles changing with age in different sex and birth year groups. For example, although the means of meat intake in all groups had not reached the daily recommended nutrient requirements based on the Food Guide Pagoda 2007 [8], the average meat intake for 30-year-old females born in the 1980s was approximately 10 times higher than that of those born in the 1930s (Figure 1). This is explainable by the rapid growth of living standards in Chinese rural populations due to the latter 21st century's socio-economic development in the country [9]. Also, recent studies revealed that the average meat intake was 23.1 gram/day in 1991 and 46.6 gram/day in 2009, which was in accordance with our study [10].
We validated the effectiveness of our LREMI tool through the population-based case-control study, and the LREMI performed effectively in differentiating disease status, i.e. disease cases and health controls. Shown in Figure 2 and Supplement Figure S3-S5 (e-f), stroke, CHD, diabetes and hypertension cases had very different performance of meat intake, drinking and weight changes compared with controls. These suggested that the LREMI had the ability to demonstrate distribution characteristics of cases and controls, and efficiently differentiated disease and health status. For our study (see Figure 2), the average meat intake per day was under recommendation in both males and females [8], though males' intakes were much higher. In this condition of malnourishment, meat intake seems to pose a potential risk factor for males but a potential protective factor for females. These different demonstrations in cases and controls indicated the effectiveness of LREMI in differentiating diseased and health status.
There were some limitations here. As a retrospective study design, the recall bias was unavoidable, although test-retest reliability analysis demonstrated moderate to high reliability. Further studies should be conducted in an already available prospective cohort or monitoring data of exposures to ascertain that these could match prospective data. In addition, the analysis of lifespan data was another challenge, for the number and timing of transitions in lifestyle habits differ between each individual. Therefore, it enquires statistical methods that can deal with time-varying longitudinal data to handle further analysis.
In conclusion, this study developed an effective and practical survey tool for use in life course epidemiology. This tool could provide valuable information on life course exposures (lifestyles, diet, physical activities, etc.) and their dynamic processes. We also demonstrated the reliability, feasibility and effectiveness of the LREMI tool.
HTML
-
Investigator (Inv): How old are you?
Respondent (Res): 60 years old.
Inv: draw a vertical line at the point of 60-year-old on the lifespan scale, and further require, do you smoke currently?
Res: No.
Inv: Write 'no' in the first row at left of vertical line, and further require, did you never smoke?
Res: no, I smoked cigarette before 55 years old.
Inv: draw a vertical line at the point of 55-year-old on the lifespan scale, write 'yes' in the first row at left of the vertical line, then require, at your 55 years old, what kind of cigarette did you smoke?
Res: Filtered-tipped cigarette.
Inv: Write '(2)' in the second row at left of the vertical line of 55, and further require, How often did you smoke (days per week)?
Res: 7 days per week.
Inv: Write '7 days/week' in the third row at left of the vertical line of 55, and further require, About how many cigarettes per day did you smoke?
Res: 10 cigarettes per day.
Inv: Write '10 cig/day' in the fourth row at left of the vertical line of 55, and further require, when did your above smoking status begin?
Res: From 40 years old.
Inv: draw a vertical line at the point of 40-year-old on the lifespan scale, and further require, at your 40 years old, what is your smoke status(yes/no, type, frequency and amount)?
Res: Yes, I smoked Unfiltered-tipped cigarette, 7 days per week and 3 cigarettes per day.
Inv: at left of line of 40, write 'no' in the first row, '(1)' in the second row, '7 days/week' in the third row, '3 cig/day' in the fourth row. and further require, when did your above smoking status begin?
Res: From 30 years old.
Inv: draw a vertical line at the point of 30-year-old on the lifespan, and further require, at your 30 years old,
what is your smoke status(yes/no, type, frequency and amount)?
Res: No. I didn't smoke. I start smoking at 30 years old.
Inv: Write 'no' in the first row at left of line of 30, finished.
More videos could be seen in https://www.dropbox.com/sh/ogr8r1hxr494gic/AAAdFiEUpKxXK5hGFV82wK5Ta?dl=0









 Quick Links
Quick Links
 DownLoad:
DownLoad: