-
Rescuers, who form the main group that helps citizens respond to emergencies, play an irreplaceable role in disaster relief operations. Rescue workers need to deal with various situations such as working across different time zones, changing patterns of work and rest, and overwhelming work intensity, to name but a few. Notably, rescuers are prone to over-excitement, anxiety, and restlessness and insomnia, which can have serious consequences. There have been reports about the insomnia burden suffered by rescue workers in China, such as in a paper by Liu et al.[1], who found that escort workers in the Gulf of Aden demonstrated insomnia symptoms. More specifically, the incidence of insomnia symptoms of the four batches of escort officers and soldiers investigated in their study were 44 (5.30%), 43 (4.63%), 37 (4.77%), and 47 (5.54%) respectively; a U-shaped distribution was present. The number of insomnia patients in each batch was highest during the early stage of the escort mission and decreased gradually, reaching its lowest level during the middle stage of the mission and rising again during the late stage. Only the epidemic characteristics were described and no prediction model was reported.
Meanwhile, Mollayeva et al.[2] reports that different types of traumatic events and various risk factors may lead to acute sleep disorders. Considering differences in behavioral and environmental factors, it is helpful to understand and identify the susceptibility factors of long-term sleep disorders after traumatic events; however, no assessment tool or model has yet been found-nevertheless, the burden of sleep disorders caused by disasters remains serious. A cross-sectional survey of typhoon disasters in Wenzhou, Zhejiang province in 2019 showed that participants were affected by unprecedented terror and were reminded of the disaster every day after it[3]. Notably, 41.2% of villagers were found likely to be carriers of mental disorders. The most common symptoms were tension or worry (66.2%), unhappiness (64.7%), vulnerability to shock (61.8%), and sleep disorders (33.8%). While some studies have been done on the factors of insomnia specific to the rescuer population, they are rare and imperfect—to date, no reliable evaluation tool exists for early insomnia screening and, as Hughes et al.[4] notes, no theoretical model exists to explain increasing and chronic insomnia. Other research has found that predeployment sleep complaints (e.g., insomnia and shortsleep duration) predict downstream behavioral health problems (e.g., anxiety, aggression, substance use, depression, and PTSD)[5]. However, no work has yet been done to consider how best to apply such findings to the unique case of rescuers.
In response to this gap in scholarship, we conducted a cross-sectional survey of 1,133 rescuers to identify the influencing factors of insomnia and establish a targeted early warning model to create effective tools for improving rescuer sleep.
-
A cross-sectional survey involving psychological questionnaires was conducted among all rescuers in one military unit, and a total of 1,133 valid questionnaires were collected. Exclusion criteria were as follows: (1) under 16 years old; (2) listening comprehension disorder or expressive disorder; (3) intelligence disorder or poor mental status that precludes cooperation with the examination; (4) insomnia secondary to other mental or physical disorders; (5) past or present drug consumption (such as sedative, anti-anxiety, or anti-depression drugs); and (6) non-compliance. All respondents gave informed consent (Clinical research registration no. chictr1900023441; hospital ethics no. 2019-108).
-
Cluster sampling was adopted and verified by a group of investigators trained in epidemiology and psychology. The questionnaire survey is organized by the subjects in collaboration with each other and arranged in a special place. Before the survey, the investigator explains the purpose and content of the survey to each subject, and the subject fills in the questionnaire independently.
Among the 1,133 valid questionnaires, there were 31 active reports of diagnosed insomnia or anti-insomnia drug consumption. The positive rate of screening was 2.74%. Basic information in the questionnaire included age, gender, religious belief, respiratory rate (times/min), height, weight, systolic and diastolic blood pressure, educational background, marital status, family per capita monthly income (CNY), enlistment time, smoking, drinking, past history, and family history.
-
We took ‘rescuer’ to signify an individual who participates in various special tasks such as earthquake relief, flood relief, anti-terrorism and stability maintenance, search and rescue, and military exercises and trainings. In 1997, the WHO defined ‘smokers’ as people who smoke continuously or cumulatively for 6 months or more in their lifetime and ‘drinkers’ as people who consume at least 12 glasses of alcoholic beverages a year (1 glass is equivalent to 355 mL of beer, 150 mL of wine, or 45 mL of 40-proof spirits).
The definition of insomnia is based on the explanation provided by the Chinese Classification and Diagnosis Criteria for Mental Disorders (CCMD-3)[3, 6], according to which patients actively report having been diagnosed with insomnia or having consumed relevant anti-insomnia drugs. Diagnoses of insomnia were made by hospitals above grade II ranking. Diagnostic criteria were as follows: (1) sleep disorder is the only symptom, and other symptoms are secondary to insomnia; (2) difficulty with falling asleep, propensity to light sleep, occurrence of multiple dreams, early awakening tendency, difficulty in falling asleep after waking up, post-waking discomfort, fatigue, and daytime sleepiness; (3) the aforementioned sleep disorders occur ≥ 3 times a week and last ≥ 1 month; (4) insomnia causes significant distress or some symptoms of mental disorders and decreases activity efficiency or hinders social functioning; and (5) the insomnia is not related to any type of physical or mental illness[6].
-
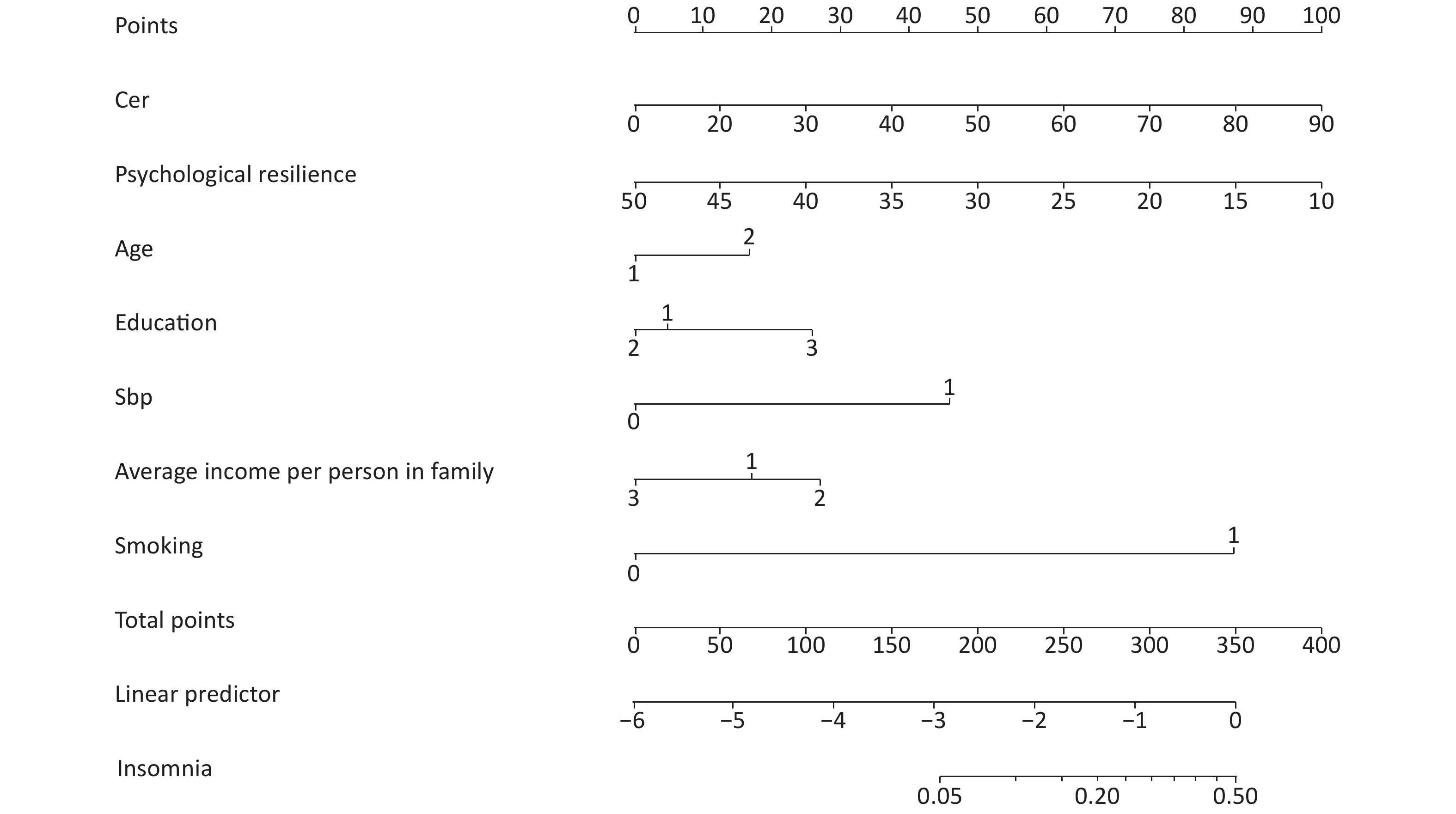
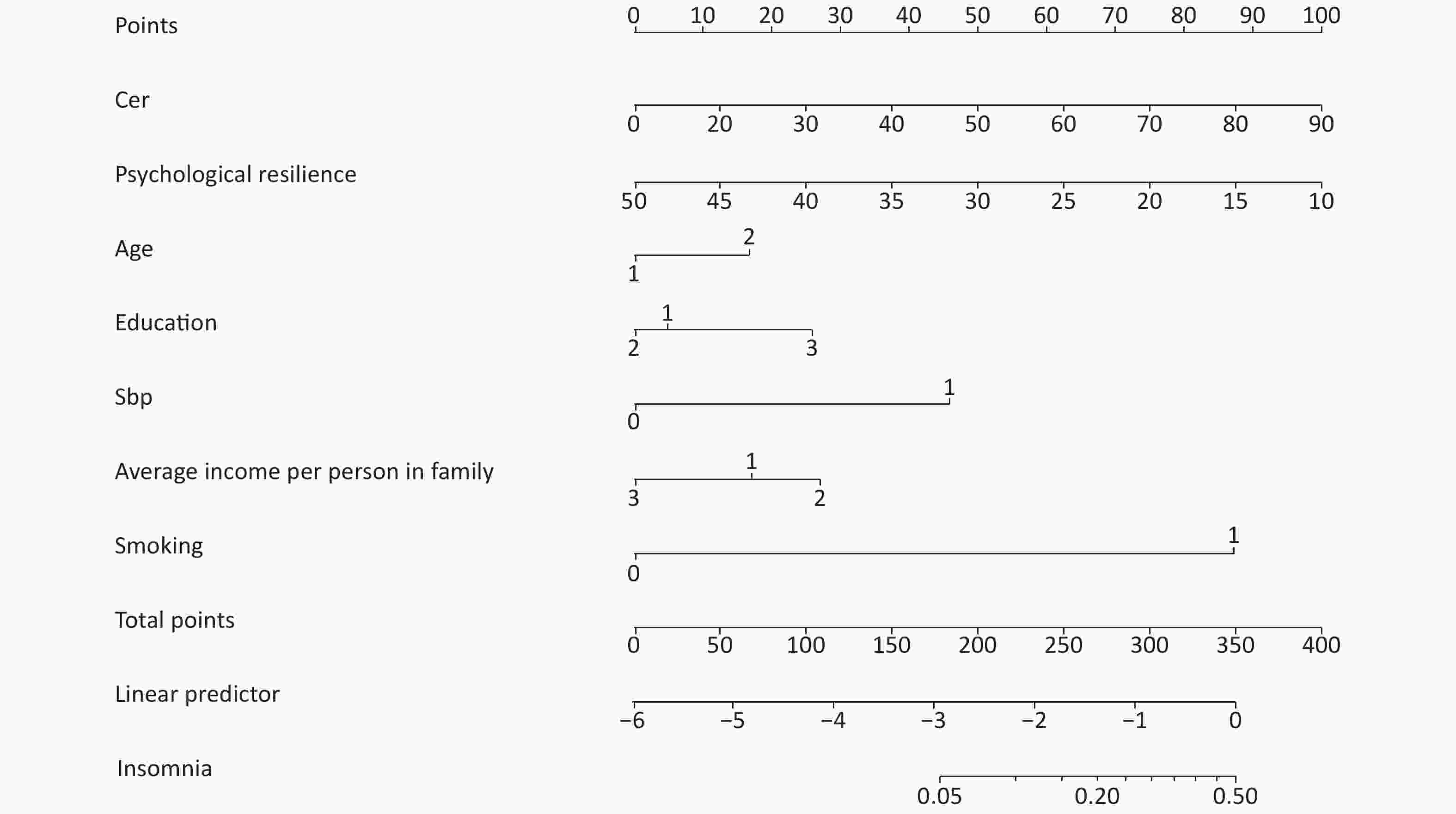
An array diagram was completed with Empower Stats. A PRISM model was used to predict the population’s risk of insomnia. The scores corresponding to the indicators of the model were added to obtain the total score corresponding to the rescuers’ probability of insomnia (Figure 1).
-
Participants were grouped by educational level (1: middle school and below, 2: high school, 3: university and above), smoking (0: no, 1: yes), insomnia (0: no, 1: yes), and family history of insomnia (0: no, 1: yes).
-
Epidata 3.0 software was used for data sorting and input and verifying the validity and reliability of the data. The data of the questionnaire were checked logically. All the questionnaires were entered by two persons. SPSS 23.0 software (Authorization No.6b4543b2xxxxf3c69a68) was used for statistical analysis. The measurement data were analyzed with a t-test, with P < 0.05 considered significant, and binary logistic regression analysis was used for correlation analysis, with P < 0.05 considered significant.
-
A total of 1,133 male rescuers aged 17–36 years old (20.49 ± 1.855) with systolic blood pressure between 100–170 mmHg (118.16 ± 8.287) participated in this study. Family per capita monthly incomes were < 3,000, 3,000–4,999, and ≥ 5,000 CNY for 46%, 32%, and 22% of participants, respectively. Further, 3.6%, 43.4%, and 53.0% of participants reported having an education level of middle school and below, high school, and university and above, respectively. In addition, 19.6% and 80.4% of participants were smokers and nonsmokers, respectively. Cognitive emotion regulation was set at 18–90 points (47.04 ± 14.33) and psychological resilience at 10–50 points (41.50 ± 10.43) (Table 1). Finally, 2.74% of patients voluntarily reported that they were either diagnosed with insomnia or had taken anti-insomnia drugs in the hospital above a grade II ranking.
Item Cases (n = 1,133) Insomnia cases (n = 31) Non-insomnia cases (n = 1,102) Age ($\bar {\rm{x} }$ ± s, years old) 1,133 21 ± 2 20 ± 2 Educational background [n (%)] Middle school and below 41 1 (3.2) 40 (3.6) High school 492 11 (35.5) 481 (43.7) University and above 600 19 (61.3) 581 (52.8) Systolic blood pressure ($\bar {\rm{x} }$ ± s, mmHg) 1,133 122 ± 11 118 ± 8 Per capita family monthly income (CNY) < 3,000 521 10 (32.3) 511 (46.4) 3,000–4,999 363 5 (16.1) 358 (32.5) ≥ 5,000 249 16 (51.6) 233 (21.1) Smoking [n (%)] No 911 16 (51.6) 895 (81.2) Yes 222 15 (48.4) 207 (18.8) Cognitive emotional regulation ($\bar {\rm{x} }$ ± s) 1,113 51 ± 17 47 ± 14 Psychological resilience ($\bar {\rm{x} }$ ± s) 1,113 37 ± 15 42 ± 10 Table 1. Comparison of basic data between two groups
-
Univariate analysis was conducted with insomnia as the dependent variable and factors such as age, educational background, systolic blood pressure, family per capita monthly income, smoking, cognitive emotional regulation, and psychological resilience as independent variables. Results showed that systolic blood pressure and per capita family monthly income significantly (P < 0.05) affected insomnia; notably, the Cochran-Armit age trend test revealed a linear trend between family per capita monthly income and insomnia (P = 0.003). While no significant relationship between insomnia and education level was observed, it is notable that insomnia tended to increase in step with education level: participants with university degrees or higher had the highest rates of insomnia (61.3%); meanwhile, participants holding only a middle school qualification had the lowest rates (3.2%).
After adjusting for the effects of age, educational background, systolic blood pressure, and cognitive emotion regulation, binary logistic regression analysis was used for multivariate analysis. Family per capita monthly income, smoking behavior, and psychological resilience all proved statistically significant. Table 2 presents the relevant OR and 95% CI values. Ultimately, smokers were 4.124 times more likely to suffer from insomnia than nonsmokers; meanwhile, results revealed that increases in psychological resilience lower the probability of insomnia.
Item OR 95% CI P value Age (years) ≤ 22 1.000 > 22 1.336 0.598–2.985 0.480 Education background Middle school and below 1.000 0.760 High school 1.128 0.136–9.338 0.911 University and above 1.495 0.186–12.010 0.705 Systolic blood pressure (mmHg) < 140 1.000 ≥ 140 1.662 0.198–13.973 0.640 Per capita family monthly income (CNY) < 3,000 1.000 3,000–4,999 0.622 0.208–1.865 0.397 ≥ 5,000 2.998 1.307–6.879 0.010 Smoking No Yes 4.124 1.954–8.706 0.000 Cognitive emotional regulation 1.019 0.993–1.046 0.162 Psychological resilience 0.960 0.933–0.988 0.005 Note. Age, educational background, systolic blood pressure, per capita family monthly income, smoking, cognitive emotional regulation and psychological resilience were taken into account. P < 0.05 is considered to have significant difference. Table 2. Analysis of influencing factors of insomnia
-
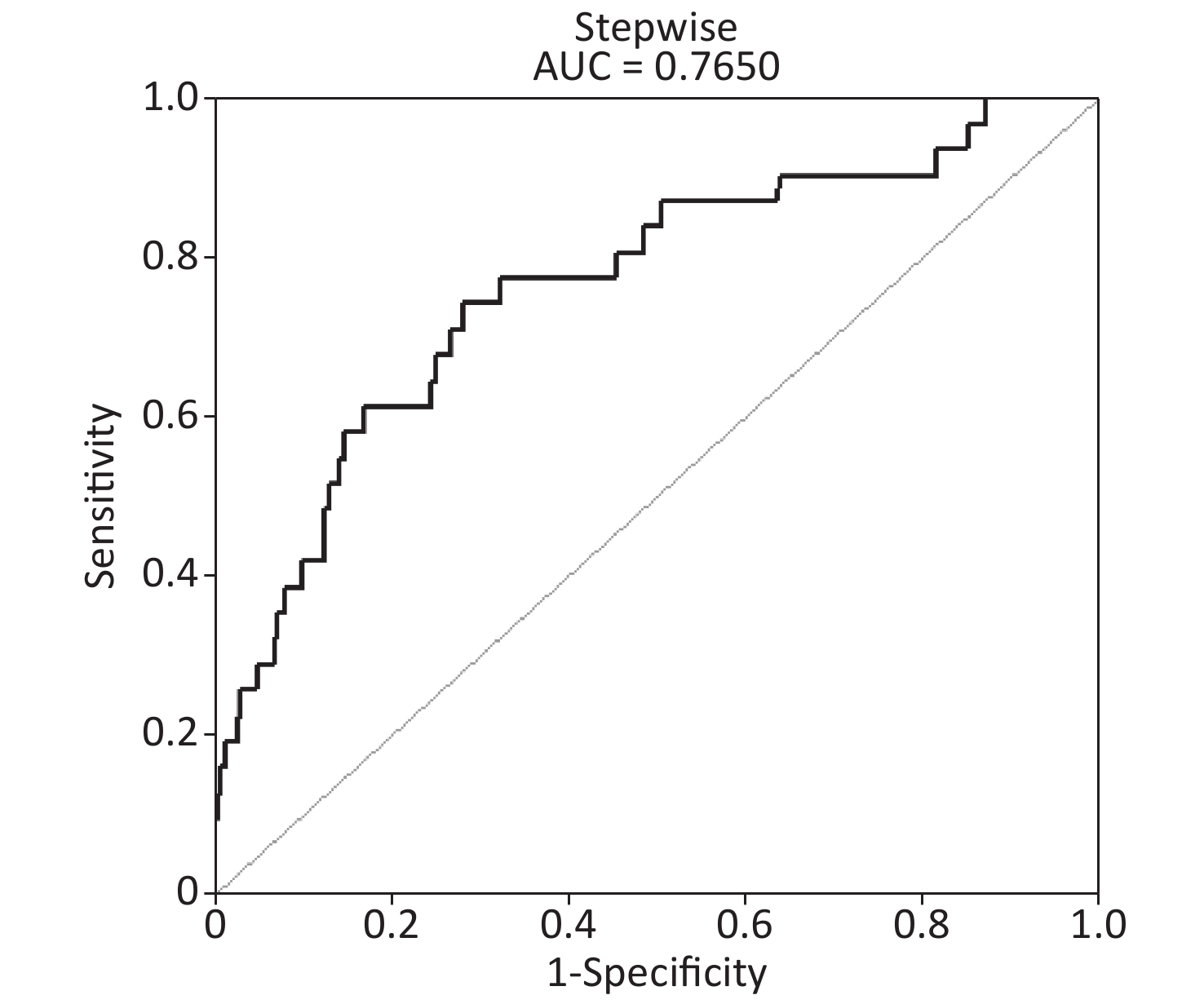
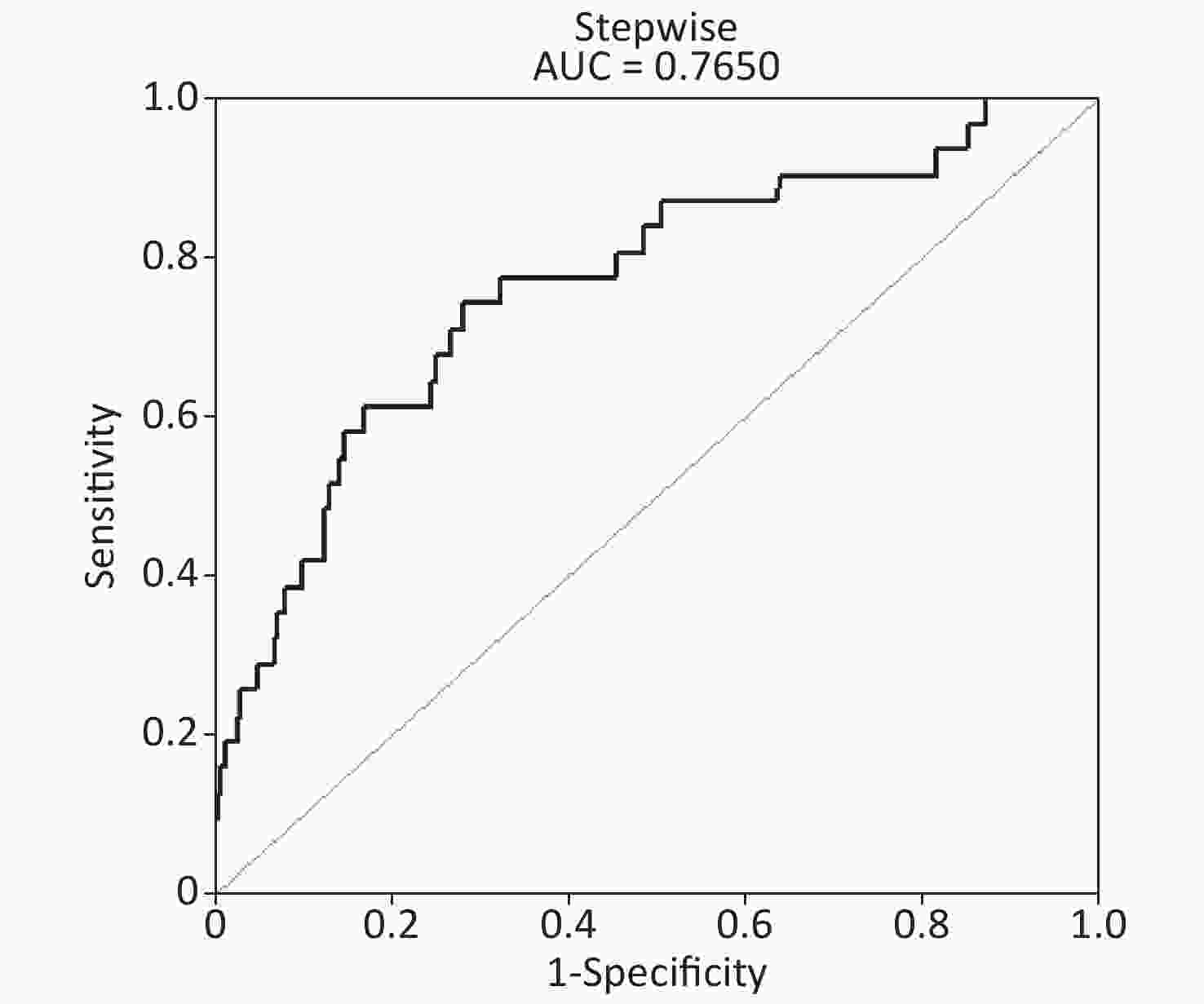
The ROC area (AUC) of the predictive model of ROC curve analysis nomogram = 0.7650, specificity = 0.7169, and sensitivity = 0.7419 (Figure 2). Ultimately, the PRISM model had good diagnostic value.
-
In short, this study found that family per capita monthly income, smoking, and psychological resilience are related to insomnia in rescue workers. Below, we discuss each of these relations in detail.
-
Insomnia incidence increased in step with family per capita monthly income. An earlier study[7] revealed that people from poor socioeconomic backgrounds are more likely to experience mental stress and develop symptoms of chronic insomnia. The problems related to sleep quality and time are more common among low-income or highly educated people[8, 9]. Further, sleep deprivation is often thought to be causally connected to low income and socioeconomic status, as well as an increased risk of disease[10]. According to the current study, the higher participant family per capita monthly income, the higher their risk of insomnia; notably, this correlation may be related to high work intensity and pressure. Also important to note here is that these results of the current study are not consistent with the findings of earlier studies, perhaps because few studies have examined the mechanism of sleep effects in low-income populations. Hence, further research is necessary to verify the results of our work.
-
Smoking may cause diseases in multiple physical systems, including respiratory, cardiovascular, nervous, and reproductive systems. Our study results showed that 50.9% of male participants were smokers[11]. Earlier studies found that, after adjusting for age and gender, smoking is associated with sleep disorders and, moreover, the greater the impulse to smoke, the worse the quality of sleep[12, 13]. To be sure, the relationship between insomnia and smoking is complex and bidirectional—smoking may lead to insomnia and insomnia may promote continued smoking. Despite the association between insomnia and smoking, only limited research has been conducted on their relationship. Helpful to note here is that emotional disorders may strengthen the relation between insomnia and smoking and clinically exacerbate smoking behavior. In theory, smokers experiencing insomnia may have inadaptable reactions, such as somatic agitation associated with sleep disorders, subjective expression of agony, and a tendency to adopt more frequent smoking behavior to control discomfort. Further, one report wagered that emotional regulation may link insomnia to cognitive-emotional smoking processes by enhancing negative feelings [14]. Our research results support this finding.
-
Psychological resilience is the ability to manage stressful events. Individuals with low psychological resilience have high incidences of personality crises and are prone to psychological crises, which may result in a series of psychological problems. High psychological resilience enables individuals to reduce psychological crisis in stressful situations. Further, reflection, as a mechanism, can explain the relationship between stressful events and poor sleep quality. The degree of individual reflection after a stressful event may affect the quality of sleep. In people with high individual resilience, reflection may not significantly affect sleep quality; however, in people with low individual resilience, reflection increases resilience’s impact on sleep quality. Our results are consistent with those of Zhang et al.[15] and Huang et al. [16]. An increase in psychological resilience can reduce the direct and indirect effects of stressful events on sleep quality. Since psychological resilience serves as a buffer between stressful events and sleep quality and the relation between reflection and sleeping problems, sleep problems may reasonably be solved by improving individuals’ psychological resilience[17].
At present, only limited diagnostic strategies and tools are available to predict rescuer sleep disorders at home and abroad. Although insomnia has a high prevalence and serious consequences, the theoretical model that can be applied to rescue workers still needs to be studied in depth. The currently available models for insomnia include the location-scale hybrid model[18], structural equation model[19], and 3R model[20]; further, to date, reliable insomnia prediction models for rescuers have not been reported. Ultimately, the PRISM model provides an operational assessment tool to diagnose insomnia in the rescuer population; to be sure, this is an important step toward overcoming the aforementioned research gap. According to the sleep-related stress response theory, individuals with high levels of baseline stress responses (i.e., high basal cortisol levels and several negative/anxious psychological tendencies) are more likely to suffer from insomnia than those with low levels[21]. Although insomnia is highly prevalent in society and has serious consequences, relatively few theoretical models exist that can be applied to rescuers.
Literature[22] reveals that the rate of insomnia occurrence among active duty personnel is more than five times that of government officials and more than twice that of the general population[23]. Further, our research group reported that 49.2% of the investigated 122 helicopter pilots had difficulty falling asleep or would easily wake up without enjoying deep sleep in 2004[24]. Compared with soldiers without insomnia, those with insomnia have a weaker ability to cope with stress after service. Moreover, a significant difference exists between military morale and intentions between people with and without insomnia[25].
Significant relationships have been observed between insomnia and PTSD that offer a deeper sense of the nuances of insomnia in rescuers. Insomnia is the main symptom of PTSD; along these lines, studies evidence the occurrence of traumatic insomnia, which may occur before the complete onset of PTSD or may be a precursor to the subsequent development of PTSD[26]. To be sure, disaster environments and scenes can cause rescuers to experience huge sensory shocks; they may experience tension, danger, and cruelty during disasters and often bear all-round and high-intensity psychological pressure. Although professional training provides rescuers with strategies to protect themselves and reduce stress, such disaster exposure can still cause rescuers tosuffer acute and long-term agony and dysfunction related to acute stress disorder (ASD) and PTSD. An earlier study revealed that the higher the frequency of rescuer participation in rescue work, the higher the probability that they will experience such elevated levels of occupational stress[27]. Further, sleep-related motional and respiratory disorders are closely related to PTSD[28] and depression[29] and, as a commonly occurring post-traumatic reaction, sleep disorder is considered a common characteristic of combat-related PTSD[30]; along these lines approximately 60%–90% of patients with PTSD suffer from insomnia[31] and, accordingly, insomnia is one of the most frequently reported sleep disorders in patients with PTSD and severe PTSD is highly likely to occur in people with insomnia. Further, insomnia is related to a decline in quality of life, impaired psychosocial functions (including cognitive impairment), negative emotional fluctuations, cardiovascular complications, and the increased use of medical services. Therefore, a clear understanding of insomnia’s role in PTSD may help prevent trauma-related psychiatric disorders and inform more effective and targeted interventions. Notably, analysis reveals that veterans are more likely to seek treatment for insomnia than PTSD or depression[32]. Happily, early identification and treatment of traumatic insomnia can prevent the development of PTSD[33]—combining the findings of this study with the above points may help optimize treatment.
Although our study used cluster sampling with a certain level of representativeness, it still has three limitations: (1) due to the nature of rescue tasks, all study subjects were men; hence, our research results can only be extrapolated to a limited extent. (2) Since it was restricted by the survey content, our study did not analyze other factors related to insomnia incidence, such as social relations, lifestyle, dietary habits, and whether the subject has siblings. (3) Finally, insomnia was measured using a self-reporting scale and previous medical records rather than by structured clinical interviews; we thus advise that follow-up studies be carried out to obtain higher-level evidence.
-
Our study revealed the important factors affecting insomnia in rescuers and established an early warning model to help improve rescuer physical and mental health and enhance their working efficiency. Ultimately, we found that insomnia in rescue workers was related to per capita family monthly income, smoking habits, and psychological resilience. We found that the developed PRISM model has good diagnostic value, may be applied to screen rescuer early sleep quality, and should be tested. Further, to ensure good rescuer sleep quality and raise battle effectiveness, rescuers should engage in psychological resilience training and quit smoking.
Analysis of Factors Influencing Insomnia and Construction of a Prediction Model: A Cross-sectional Survey on Rescuers
doi: 10.3967/bes2020.067
- Received Date: 2020-03-16
- Accepted Date: 2020-06-28
-
Key words:
- Rescuers /
- Insomnia /
- Influencing factors /
- Cross sectional survey /
- Prediction model
Abstract:
| Citation: | SAI Xiao Yong, CHEN Qiao, LUO Ting Gang, SUN Yuan Yuan, SONG Yu Jian, CHEN Juan. Analysis of Factors Influencing Insomnia and Construction of a Prediction Model: A Cross-sectional Survey on Rescuers[J]. Biomedical and Environmental Sciences, 2020, 33(7): 502-509. doi: 10.3967/bes2020.067 |






 Quick Links
Quick Links
 DownLoad:
DownLoad: