-
The benefits of peri-conceptional folic acid (FA) supplementation in preventing neural tube defects (NTDs) have been well established since the early 1990s[1,2]. A daily dose of 400 μg of FA is recommended worldwide[2,3]. In addition, 81 countries have introduced mandatory food fortification of grains with FA[4]. In these countries, risk reduction of NTDs has been reported[5-11]. In addition to the prevention of NTDs, maternal FA supplementation during the peri-conception period is associated with a reduced risk of other reproductive outcomes including congenital heart defects, small-for-gestational-age birth, and language delay[12-16]. However, emerging evidence suggests an association between increased exposure to FA and increased risk of several adverse health outcomes, including large-for-gestational-age, lower psychomotor scores, and asthma[17-21]. Although FA food fortification has not been introduced in China, the Ministry of Health launched a nationwide programme in 2009 to recommend the use of FA supplements (400 μg/d) among fertile women in rural areas[22], including the suburban districts in Shanghai[23]. However, there is a lack of recent estimates of FA supplementation of women at pre-conception and early pregnancy stages.
Additional evidences from animal models and population-based studies have shown that paternal FA deficiency may result in adverse outcomes in their offspring[24,25]. Moreover, there are limited population-based studies investigating FA supplementation in male pregnancy planners.
This study aimed to assess FA supplement use in populations planning a pregnancy, women at early pregnancy, and factors affecting FA supplement use in the peri-conception period.
-
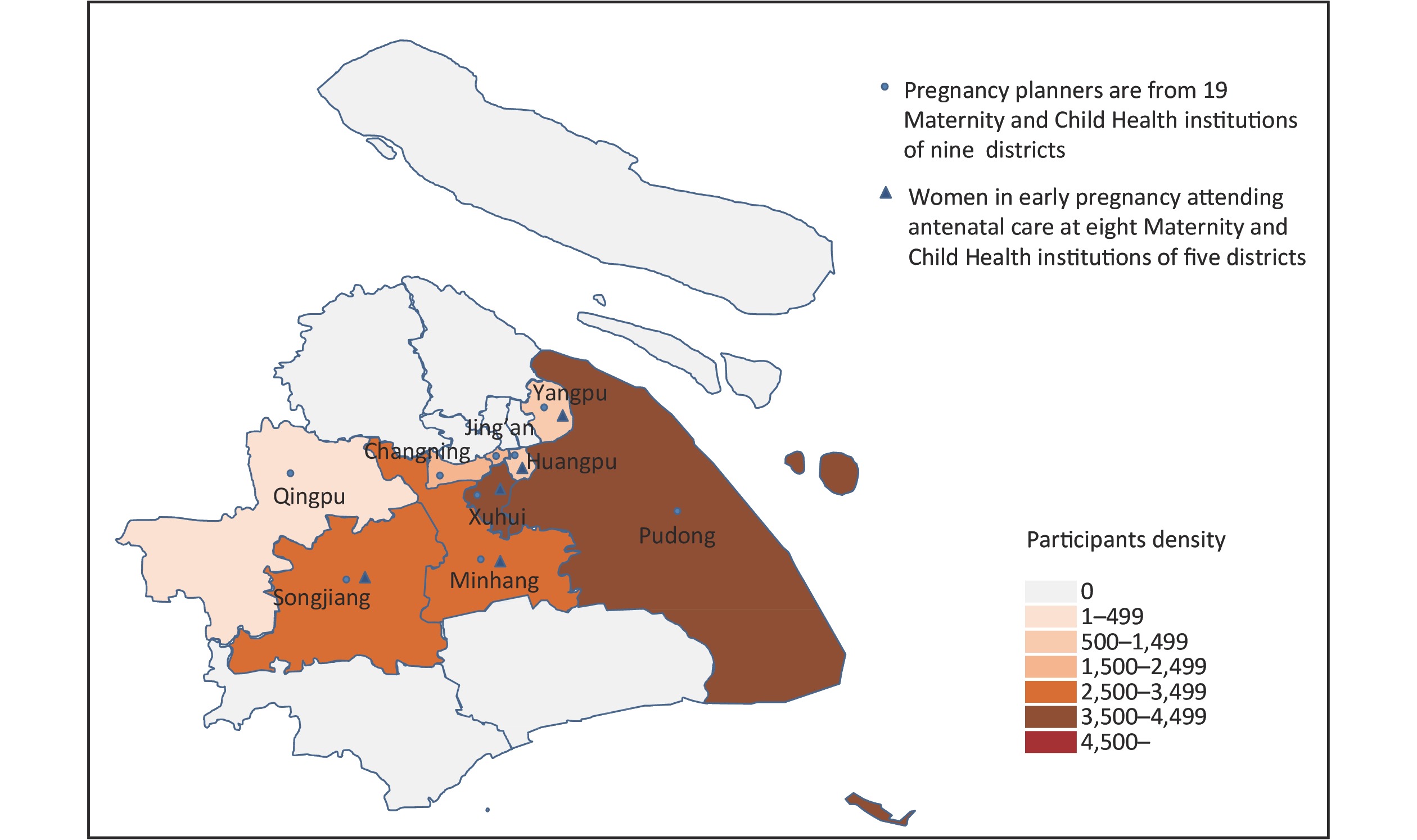
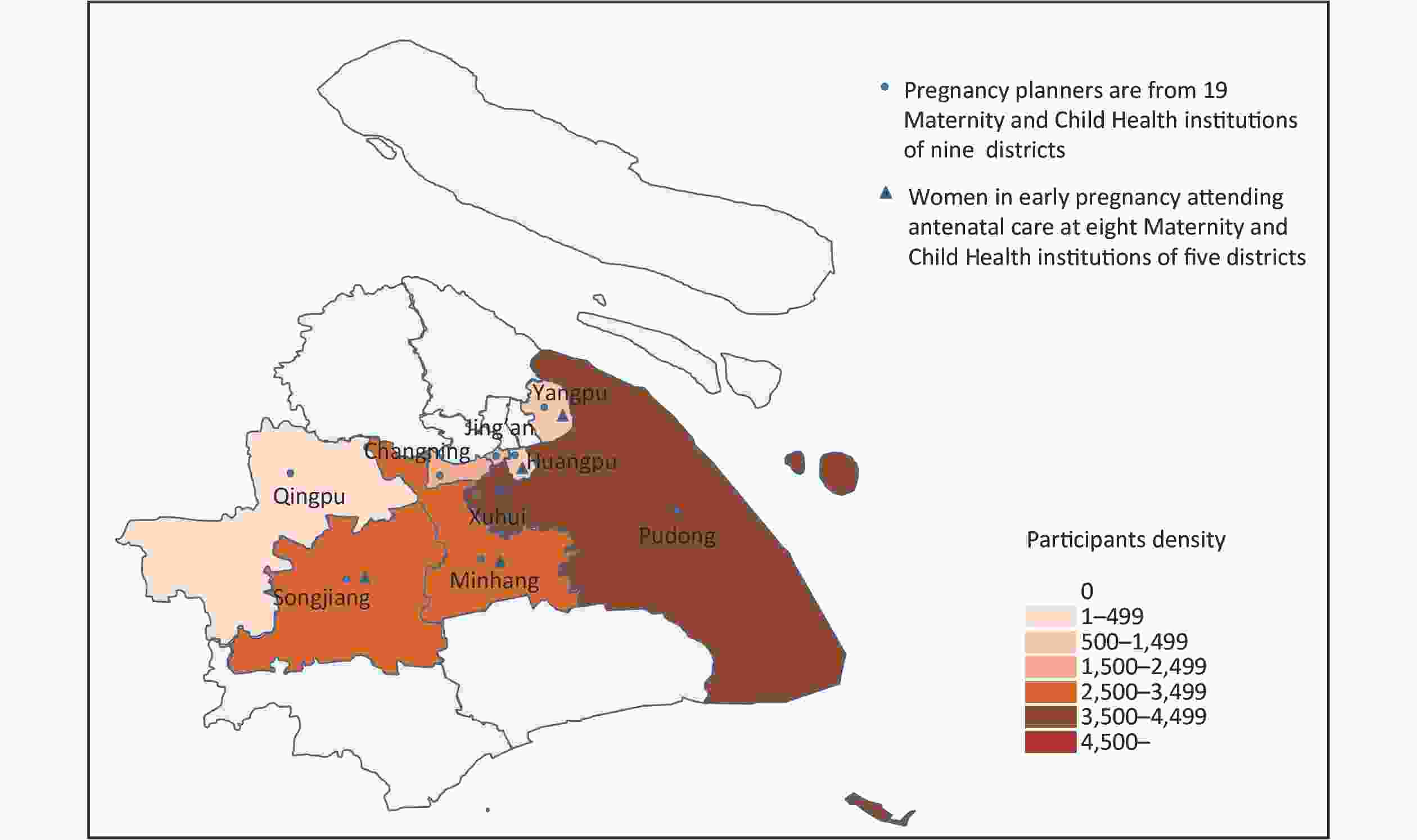
This was a cross-sectional study based on the Shanghai PreConception Cohort (SPCC) study[26]. The SPCC study is an ongoing multicentre, -government-funded study, investigating the association between peri-conception folate concentration and congenital heart defects in a prospective cohort, and recruitment of 20,000 pregnancies were expected. The baseline study population comprised couples preparing for pregnancy who visited their pre-pregnancy examination clinics and early-pregnant women at < 14 gestational weeks. The two samples were recruited separately without overlap. In the current study, the participants were baseline population of the SPCC prospective cohort[26]. From March 2016 to September 2018, we recruited couples or women alone at pre-pregnancy examination clinics in 19 maternity and child health care centres from 9 districts in Shanghai, who were residents of Shanghai, voluntarily presented at preconception examination clinical clinics and planned for pregnancy within a year (‘pregnancy planners’) (Supplementary Figure S1 available in www.besjournal.com). We also recruited pregnant women at their first antenatal examination who were within 14 weeks of pregnancy, planned to receive antenatal care until delivery from 8 maternity and child health institutions of 5 districts (Supplementary Figure S1). These two different groups of participants comprised the peri-conceptional population of our study. The study covered both urban and suburban districts of Shanghai. Since 2009, peri-conception FA supplementation promotion programmes have been implemented in the suburban districts.
The SPCC protocol was approved by the Institutional Review Board and the Ethical Committee of the Children’s Hospital of Fudan University (2016-49). All participants provided signed informed consent and could withdraw at any stage of the study.
-
In the SPCC study, all participants were invited to complete a questionnaire by themselves and the completeness was checked by trained physicians or research coordinators. Besides routine clinical information, we collected information of FA supplementation and related risk factors using questionnaires. Based on our knowledge and previous studies, we considered several factors that potentially influence the behaviour of taking FA supplements, including socio-demographic status (age, ethnicity, residence, education, and occupation), lifestyle (smoking and alcohol consumption) for participants. We also consider history of health care attendance of this population as possible risk factors, including attending pre-pregnancy examination and gravidity for early pregnant women.
-
FA supplement users were those who were taking an FA or multivitamin supplement containing FA. FA supplement non-users were those who did not take any supplement. Participants were asked to specify the brand names of the FA supplements and the frequency and time period of use. Pregnancy planners were categorised as FA users if they had taken FA or multivitamin supplements containing FA within three months before the pre-pregnancy examination (recruitment); those who did not were categorised as FA non-users. Pregnant women were categorised as FA users if they had taken any FA tablets after their last menstrual period; those who did not were categorised as FA non-users.
The dose of FA supplement was calculated from the label contents and the reported frequency of use. The dose could not be determined if the participants did not know the brand. According to the recommended dose of FA supplementation for the prevention of NTDs (400 μg/d) and the medicine’s recommended tolerable upper limit [(TUL) 1,000 μg/d)][3], we classified the FA intake into three categories (low: < 400 μg/d, normal: 400–1,000 μg/d, high: > 1,000 μg/d).
-
We estimated the proportion of participants reporting FA supplementation. Data following normal-distribution was reported as mean and standard deviation (SD). Multivariable log-binomial model was used for association analysis, by using GLM program based on binomial family and log for link function, with FA supplement use (0: no, 1: yes) as the dependent variable and the following exposure variables: age (0: < 30 years, 1: ≥ 30 years), ethnicity (0: Han, 1: other), education (1: high school, 2: college or above), district of residence (0: suburban, 1: urban), smoking (0: no, 1: yes), alcohol consumption (0: no, 1: yes), attending pre-pregnancy examination (0: no, 1: yes), gravidity (0: < 2 times, 1: ≥ 2 times), and a dummy variable created for occupation (1: blue collar, 2: white collar, 3: other).
Risk ratio (RR) and 95% confidence interval (95% CI) were reported the measure of associations. Participants with missing values for any of the covariates were excluded from the final multivariate model. All statistical analyses were performed using Stata version 15. Two-sided significance was determined at P < 0.05.
-
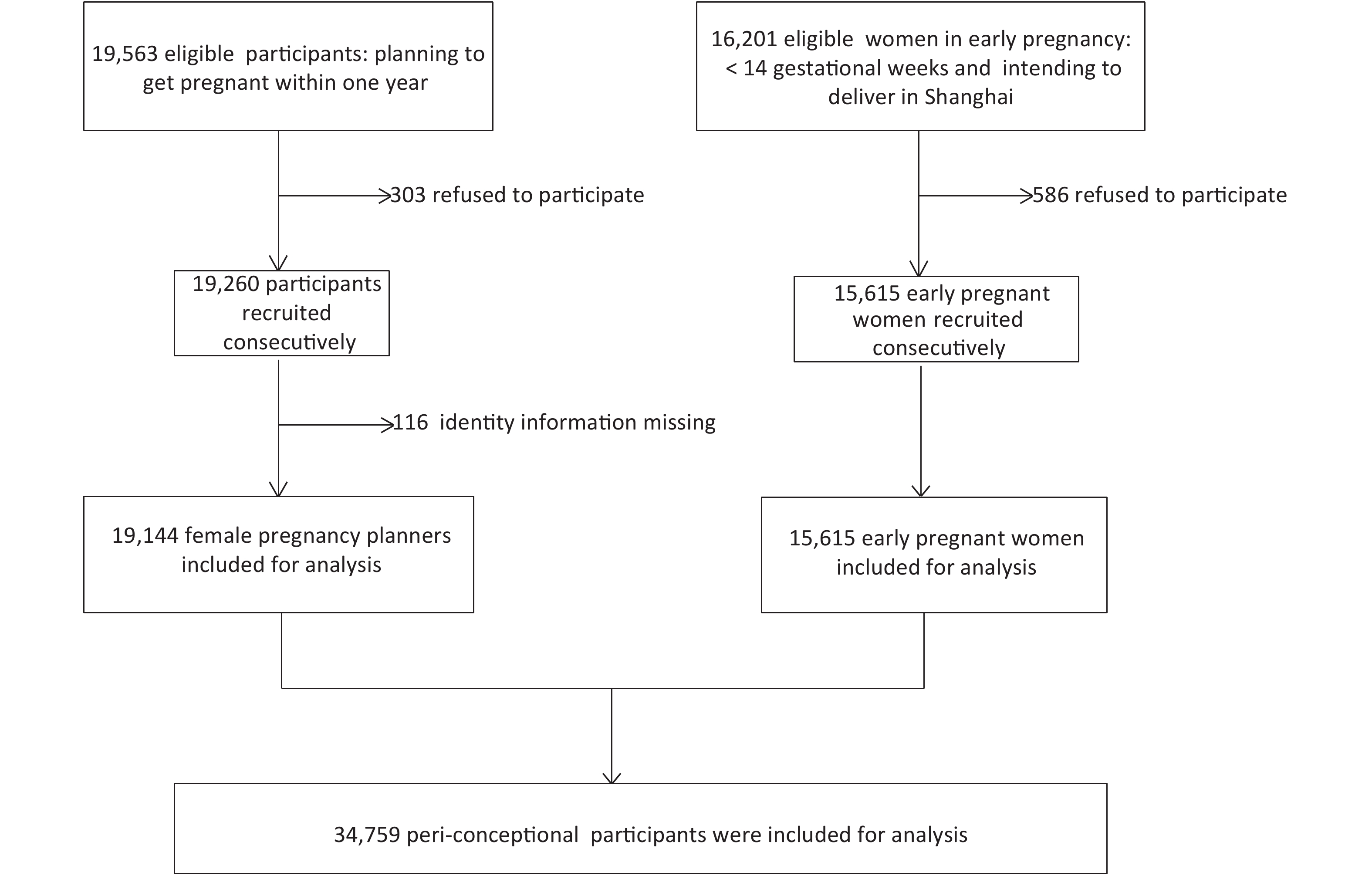
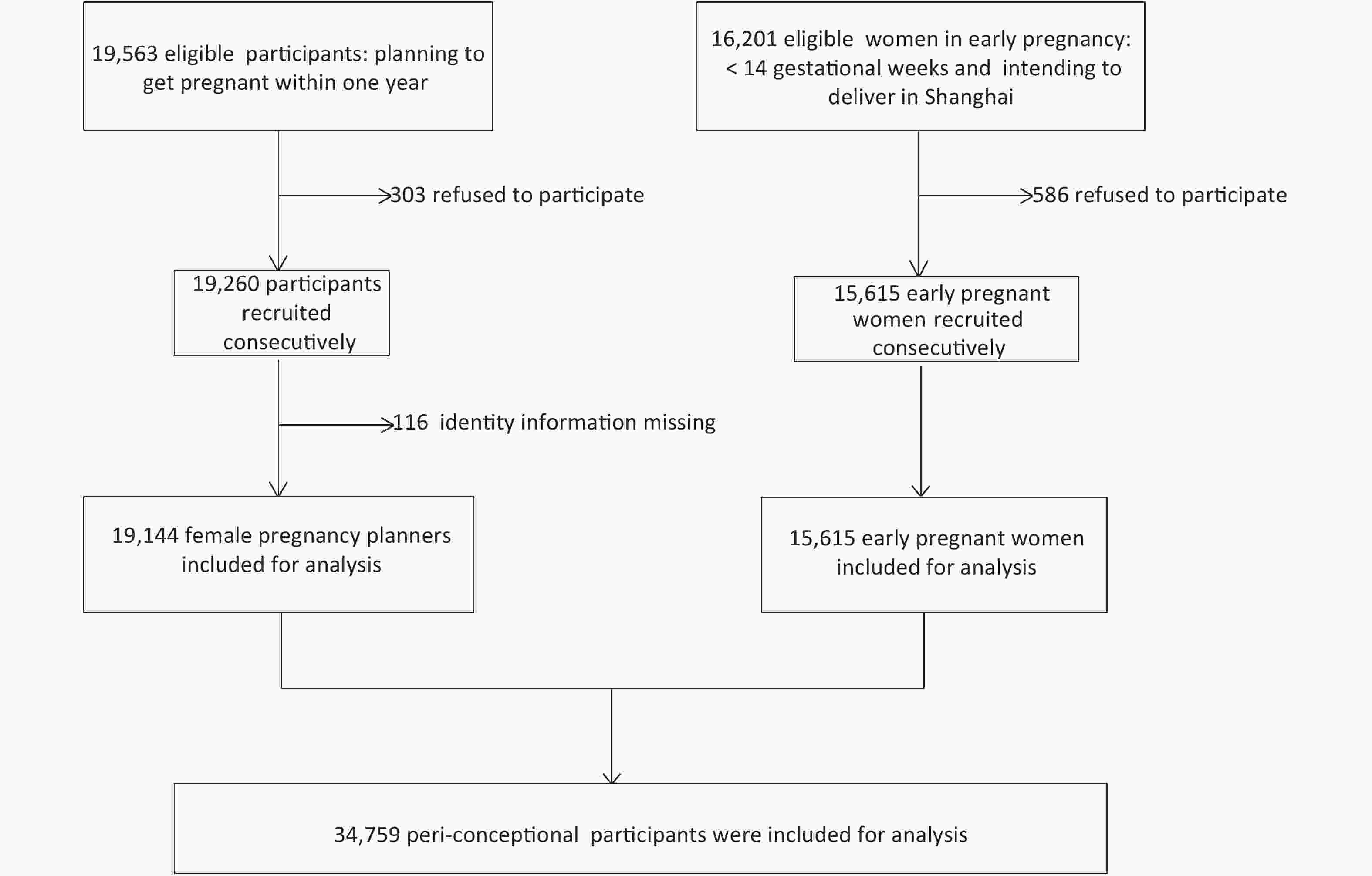
We consecutively-recruited 97.9% (19,144/19,563) wife/husband pregnancy planners who were eligible for the study, with a high participation rate across the districts; 96.4% (15,615/16,201) eligible women were recruited consecutively at early pregnancy (Figure 1).
The socio-demographic and lifestyle characteristics of the participants are presented in Table 1. The mean (SD) age was 29.9 (3.9) years, 31.4 (4.5) years, and 29.9 (4.0) years of female and male pregnancy planners and women at early pregnancy, respectively. The majority of the participants were of Han ethnicity, educated to college level or above, and employed. About half of the sample lived in suburban districts. Smoking was uncommon among women but common among men. Further, 1 in 3 women consumed alcohol before conception but only 1 in 10, during pregnancy; alcohol consumption was more common among men than women. Half of the women in early pregnancy were primigra-vidae.
Characteristics Couples completed questionnaires (a)
at pre-pregnancy examination clinics visit
(female = 11,099, male = 8,045)Pregnant women completed
questionnaires (b) at first antenatal
clinic visit (n = 15,615)Wife-pregnancy
planners, n (%)Husband-pregnancy
planners, n (%)Women in early
pregnancy, n (%)Age, years < 30 6,527 (58.8) 3,517 (43.7) 8,587 (55.0) ≥ 30 4,572 (41.2) 4,528 (56.3) 7,028 (45.0) Ethnicity Han 10,773 (97.1) 7,843 (97.5) 15,245 (97.6) Others 259 (2.3) 158 (2.0) 342 (2.2) Missing 67 (0.6) 44 (0.5) 28 (0.2) Educational level High school or less 947 (8.5) 613 (7.6) 2,117 (13.6) College or above 10,041 (90.5) 7,383 (91.7) 13,436 (86.0) Missing 111 (1.0) 49 (0.6) 62 (0.4) Occupation Blue collar 2,698 (24.3) 3,540 (44.0) 2,650 (17.0) White collar 3,499 (31.5) 2,413 (30.0) 2,403 (15.4) Others 4,661 (42.0) 1,954 (24.3) 5,366 (34.4) Missing 241 (2.2) 138 (1.7) 163 (1.0) Residencea Suburban districts 4,728 (42.6) 4,473 (55.6) 7,481 (47.9) Urban districts 6,371 (57.4) 3,572 (44.4) 8,134 (52.1) Smokingb No 10,816 (97.5) 5,501 (68.4) 15,410 (98.7) Yes 248 (2.2) 2,517 (31.3) 161 (1.0) Missing 35 (0.3) 27 (0.3) 44 (0.3) Alcohol consumptionc No 7,532 (67.9) 3,043 (37.8) 13,976 (89.5) Yes 3,374 (30.4) 4,840 (60.2) 1,599 (10.2) Missing 193 (1.7) 162 (2.0) 40 (0.3) Attending pre-pregnancy examination NA NA No 11,622 (74.4) Yes 3,374 (21.6) Missing 619 (4.0) Gravidity (times) NA NA < 2 7,804 (50.0) ≥ 2 7,782 (49.8) Missing 29 (0.2) Note. a Residence was classified according to administrative division of the Shanghai government. Suburban districts in this study were ‘rural areas’, where the national FA programme has been implemented since 2009.
bParticipants with a history of smoking.
cAlcohol consumption within three months.
FA, folic acid; NA, not applicable.Table 1. Characteristics of pregnancy planners and women in early pregnancy
-
In Table 2, among the pregnancy planners, 42.4% (4,710/11,099) of the wives and 17.1% (1,377/8,045) of the husbands reported current FA supplement use. The prevalence of FA supplementation in suburban districts was 40.6% (1,921/4,728) in the wives and 15.4% (688/4,473) in the husbands compared with 43.8% (2,789/6,371) and 19.3% (689/3,572), respectively, in the urban districts that were not included in the programme. Among women at early pregnancy, 93.4% (14,585/15,615) reported FA supplementation after their last menstrual period.
Description Before pregnancy At early pregnancy Female Male Early pregnant women Total prevalence of FA supplementation, n/N (%) 4,710/11,099 (42.4) 1,377/8,045 (17.1) 14,585/15,615 (93.4) Prevalence of FA supplementation in suburban districts, n/N (%) 1,921/4,728 (40.6) 688/4,473 (15.4) 6,951/7,481 (92.9) Prevalence of FA supplementation in urban districts, n/N (%) 2,789/6,371 (43.8) 689/3,572 (19.3) 7,634/8,134 (93.9) Respondent, n (%)a 2,866 (60.8) 648 (47.1) 10,033 (68.8) The percentage of single FA, n (%) 203 (7.1) 22 (3.3) 751 (7.5) The percentage of multi-vitamin, n (%) 2,663 (92.9) 626 (96.7) 9,282 (92.5) Dose of daily FA supplement (μg/d), n (%)b 2,781 (59.0) 614 (44.6) 10,033 (68.8) < 400, n (%) 613 (22.0) 135 (22.0) 1,072 (10.7) 400–1,000, n (%) 2,038 (73.3) 466 (75.9) 7,950 (79.2) > 1,000, n (%) 130 (4.7) 13 (2.1) 1,011 (10.1) Note. aNumber of participants who responded to ‘brand of product’; bNumber of participants who responded to both ‘brand of product’ and frequency of use. FA, folic acid. Table 2. Prevalence and dose of FA supplement use before and at early pregnancy
Based on the information on FA products, FA dose was calculated for 3,395 pregnancy planners (n = 614 husbands; n = 2,781 wives) and 10,033 women at early pregnancy. Insufficient FA intake (< 400 μg/d) was reported in 22.0% (613/2,781) of the wives, while 4.7% (130/2,781) of the wives went over the recommended TUL of 1,000 μg/d. At early pregnancy, 10.7% (1,072/14,585) of the women took a low dose of FA (< 400 μg/d), and 10.1% (1,011/14,585) exceeded the TUL.
-
In the multivariable log-binomial model analysis, factors that were statistically significantly associated with high FA supplement use in both male and female pregnancy planners were older age, high education level, and residence in an urban district. FA supplement use was lower in female pregnancy planners who consumed alcohol. High education level was also associated with high FA supplement use in early pregnancy women. In contrast to pregnancy planners, FA supplement use decreased in older early pregnant women. FA supplement use was low in pregnant women in multigravida. FA supplement use was high in early pregnant women who had attended a pre-pregnancy examination. The detailed results are presented in Table 3.
Characteristics Female pregnancy plannersa Male pregnancy plannersb Early pregnancy womenc RR (95% CI) P RR (95% CI) P RR (95% CI) P Age (years) < 30 1 1 1 ≥ 30 1.13 (1.08–1.18) < 0.001 1.22 (1.11–1.35) < 0.001 0.99 (0.98–0.99) 0.003 Ethnicity Han 1 1 1 Others 1.04 (0.90–1.20) 0.585 0.92 (0.65–1.31) 0.653 1.01 (0.99–1.03) 0.340 Education High school or less 1 1 1 College or above 1.71 (1.53–1.92) < 0.001 2.06 (1.55–2.75) < 0.001 1.04 (1.03–1.06) < 0.001 Occupation Blue collar 1 1 1 White collar 0.97 (0.92–1.02) 0.258 1.07 (0.95-1.21) 0.288 1.01 (0.99–1.02) 0.054 Other 1.02 (0.96–1.08) 0.473 1.03 (0.92–1.15) 0.634 1.00 (0.98–1.01) 0.697 Residing- districts Suburban districts 1 1 1 Urban districts 1.06 (1.01–1.11) 0.011 1.25 (1.11–1.41) < 0.001 1.00 (0.99–1.01) 0.828 Smoking No 1 1 1 Yes 0.94 (0.79–1.11) 0.444 0.91 (0.81–1.01) 0.081 0.95 (0.89–1.01) 0.101 Alcohol consumption No 1 1 1 Yes 0.95 (0.90–0.99) 0.035 0.98 (0.89–1.09) 0.719 0.99 (0.98–1.01) 0.291 Attending pre-pregnancy examination NA NA No Yes 1.02 (1.01–1.03) < 0.001 Gravidity (times) NA NAd < 2 ≥ 2 0.97 (0.96–0.98) < 0.001 Note. Multivariable log-binomial model was used. Missing data have not been included in the analysis. aModel performance: N = 10,612, Log likelihood = −7161.4269; bModel performance: N = 7,714, Log likelihood = −3511.2040; cModel performance: N = 14,769, Log likelihood = −3488.4899; dLacking of information due to the design limitation in questionnaires (a). RR, Risk ratio; FA, folic acid; 95% CI, 95% confidence interval; NA, not applicable. Table 3. Analyses of factors relate to FA supplement use among pregnancy planners and women in early pregnancy
-
The benefits of peri-conceptional FA supplementation in preventing NTDs have been well established since the early 1990s[1,2]. 81 countries have introduced mandatory food fortification of grains with FA, for example the U.S. adds 140 µg of FA per 100 g of enriched cereal grain product since 1998[4]. In China, we have not implemented FA food fortification policy. Instead the Ministry of Health launched a nationwide programme in 2009 to recommend the use of FA supplements (400 μg/d) among fertile women in rural areas, and provide FA supplement packs for free[22], including the suburban districts in Shanghai[23]. Owing to the lack of mandatory FA food fortification policies in China[22], the appropriate use of FA supplements is particularly important for women of childbearing age, especially those planning for pregnancy. There are very few studies on FA supplementation among pregnancy planners. Despite the programme to increase use of FA supplements in rural populations in China from 2009, we found a low prevalence of FA supplementation amongst pregnancy planners in rural areas; in the current study, only 42.4% of wife-pregnancy planners reported FA supplementation at the time of investigation. We believe that this prevalence is more reliable than the recall-based prevalence reported in retrospective studies. This prevalence was higher than that reported in several retrospective studies, such as 14.4% in China[27], 23.5% in Italy[28], 28%–35% in Denmark[29], and 13%–30% in Australia[30], in which data on FA supplement use before pregnancy were collected during the second or third trimesters or after birth. The prevalence in our study was lower than that reported in the USA (51%)[31].
Initiating FA supplementation at three months before conception is a critical requirement in the prevention of NTDs and other folate-sensitive defects, since they occur at the early stage of gestation[1]. Furthermore, supplementation for 6–9 months or more is recommended to achieve steady-state RBC folate in response to FA supplementation[32]. Although in our study, the prevalence of FA supplementation at early pregnancy markedly increased to 93.4%, the biological effect of FA supplementation in preventing birth defects may have been limited. The prevalence of FA supplementation in women at early pregnancy was similar to the 95.9% reported in Saudi Arabia[33], but higher than the 74% reported in Sweden[34] and 66%, in America[31], and higher than the 75.6% reported in the Chinese National Free Preconception Health Examination Project[35]. A previous study indicated that the risk of NTDs decreased throughout the continuum of RBC folate concentration until the threshold value of 906 nmol/L was attained, which would result in a 48% reduction in the risk of NTDs[36]. Only regular FA supplementation at the appropriate dose and for a sufficient time period before pregnancy can help achieve the benefit of FA supplementation in a population.
There is limited evidence on paternal FA deficiency and adverse outcomes in their offspring, so there is no universal agreement on FA supplementation in men during the pre-conception period[24, 25]. Animal studies indicated that paternal FA deficiency was related to adverse outcomes in their offspring[24]. High-dose FA supplementation can alter the human sperm epigenome and improve sperm parameters[37]. These findings indicate that paternal folate status has an impact on the offspring. However, we are not aware of any population-based studies involving male FA supplement users. In this study, 17.1% of male pregnancy planners reported FA supplement use. We reported the status of FA supplementation in male pregnancy planners to provide cues to future studies in this area. Further molecular and population-based studies are required to better understand the contribution of paternal folate status to conception, foetal development, and birth outcomes.
We also explored the factors associated with FA supplementation in the study population. Consistent with previous studies, we found that women of older age, with high education level, residing in an urban district were more likely to take FA supplement before conception than their younger peers, with low education, residing in rural areas[29, 38]. In contrast to a previous study[29], maternal smoking did not affect pre-conception FA supplement use in this study, probably because of the very low prevalence of maternal smoking in the Chinese population. Attendance to pre-pregnancy examination was significantly associated with FA supplement use in early pregnant women, similar to a study in Italy[28]. In China, pre-pregnancy check-ups are not mandatory, and there are no regulations that require doctors to provide education on FA supplementation to patients who come for pre-pregnancy check-ups. This means people who undergo pre-pregnancy check-ups are more health-conscious and thus more likely to take FA supplements than those who do not undergo check-ups. Although previous pregnancy or childbirth may increase awareness of peri-conceptional FA supplements use, we found a negative association between gravidity and FA supplement use. Similar to our study, having more than one baby was associated with decreased FA supplement use in other studies too[27, 30].
-
Our study has several strengths. To the best of our knowledge, this was the first report on FA supplementation in a population planning for pregnancy, based on a prospective cohort study. The sample size was large, and participants were recruited from both urban and suburban districts, so our findings could represent the status of FA supplementation in the south-eastern Chinese population. Additionally, our study is the first to report FA supplementation in male pregnancy planners, which may provide new insights into the relationship between paternal folate nutrition status and offspring outcomes.
This study has some limitations. Firstly, we did not investigate FA intake from foods; however, previous studies have found that the contribution of food sources to daily folate intake for prepare-for-pregnancy women may be limited[39, 40]. Secondly, the study population of the current study were from Shanghai, south-eastern China, the generalizability of our findings to other parts of China needs caution, such as the north and the west of China. Shanghai is one of the most developed cities whose population has the higher social economic levels of the country. The main findings of poor FA supplementation before pregnancy from this study sample may represent the best situation of folate levels in China, it may imply that the situation in other parts of the country, such as north and west of China, can be even worse. Finally, although multiple influential factors were considered for association analysis effect of some unknown or unmeasured factors were not included.
-
The majority of the pregnant women reported FA supplementation at early pregnancy, but more than half of the women planning for pregnancy did not take any FA supplements. Although the nationwide FA supplementation program was introduced in 2009, urgent strategies are needed to improve pre-conception FA supplementation, especially among women with lower educational level and those residing in suburban areas.
-
The authors are grateful to all of participants, nurses, doctors and staffs who contributed to this study. We are grateful to the Shanghai Municipal Commission of Health and Family Planning and the Department of Maternal and Child Health Care for their efforts on the project implementation. We would like to thank Editage (www.editage.cn) for English language editing.
-
No conflict of interest to declare.
-
HUANG Guo Ying and YAN Wei Li designed and implemented the SPCC study. WANG Ding Mei, ZHANG Yi, JIANG Yuan, YE Ying, LI Meng Ru, JI Mi, ZHAO Zheng Shan, CHEN Xiao Tian, SHENG Wei, MA Xiao Jing, and the Shanghai PreConception Cohort Group implemented the study. ZHANG Yi and WANG Ding Mei were the principal investigators and coordinators of the study. WANG Ding Mei and ZHANG Yi completed the data preparation and drafted the manuscript and ALLEN Stephen was the co-writer of the manuscript draft. WANG Ding Mei, ZHANG Yi, HUANG Xiang Yuan completed the statistical analysis and generated the tables and figures, and WANG Duo Lao was the guarantor of statistical analysis. HUANG Guo Ying, YAN Wei Li were the guarantors on the data preparation, statistical analysis and the manuscript draft, and had primary responsibility for final content. All individual authors critiqued the manuscript and approved the final report.
Folic Acid Supplementation in Chinese Peri-conceptional Population: Results from the SPCC Study
doi: 10.3967/bes2020.074
- Received Date: 2019-10-30
- Accepted Date: 2020-03-13
-
Key words:
- Folic acid supplementation /
- Peri-conception /
- Birth defects /
- China /
- Pregnancy
Abstract:
&Members of Shanghai PreConception Cohort Group are listed at the end of manuscript
| Citation: | WANG Ding Mei, ZHANG Yi, JIANG Yuan, YE Ying, HUANG Xiang Yuan, LI Meng Ru, JI Mi, ZHAO Zheng Shan, CHEN Xiao Tian, SHENG Wei, MA Xiao Jing, ALLEN Stephen, WANG Duo Lao, YAN Wei Li, HUANG Guo Ying, the Shanghai PreConception Cohort Group. Folic Acid Supplementation in Chinese Peri-conceptional Population: Results from the SPCC Study[J]. Biomedical and Environmental Sciences, 2020, 33(8): 557-565. doi: 10.3967/bes2020.074 |






 Quick Links
Quick Links
 DownLoad:
DownLoad: