-
The application of radiation for medical examination and treatment has increased rapidly since the 1980s. In contrast to other radiation-based imaging and medical treatment, medical staff working in fluoroscopic-based procedures have to suffer radiation exposure. Its harm is well known not only for the deterministic effects causing cataract or dermatitis[1], but also for the stochastic effects with increased risks of chromosomal damage or malignant tumors[2].
Although challenges in interventional cardiology still exist in term of device developments such as X-ray tube, online monitoring chambers, etc, radiation protection is a key issue that has direct impact on physicians’ health. Currently, traditional lead clothing (TLC) is the main form of protection from radiation. However, TLC has limitations including lack of protection efficacy and increased risk of orthopedic injuries attributable to its heavy weight[3]. Problems including low mechanical strength, low quality of sterilization and secondary radiation production have also been reported[4]. In this study, we developed a new protection device (NPD) and compared its effects on the reduction of radiation exposure compared with the TLC. In addition, we observed the effects of the new X-ray protector on complications associated with the radiation and heavy body-load.
The NPD (WLXP-006, Yingnuoweite Medical Science and Technology, Co., Ltd., Nanjing, China) is a floor-standing medical radiation protection device mainly composed of a barrel-like frame and protective lead rubber (0.5 mm lead equivalent) (Supplementary Figure S1 available in www.besjournal.com). The barrel-like frame includes an upper frame and a lower frame. These two frames are integrated by a lifting apparatus, which can be moved up and down along the lower frame by pressing two buttons on the top panel of the NPD. Besides, both the upper and lower frames consist of two semi-ring frames. The posterior ends of the two semi-ring frames are connected to a rotating rod with a motor, so that the frame can be opened and closed (by pressing another two buttons on the top panel of the NPD). The anterior ends of the two semi-rings overlap about 20 cm to avoid cracks for radiation. For safety, an anti-pinch device is installed on the anterior end of the right semi-ring frame to prevent the operator from being pinched by the device. The inside and outside of the frame are covered by lead rubbers. The bottom of the device is equipped with four universal wheels for convenience of movement.
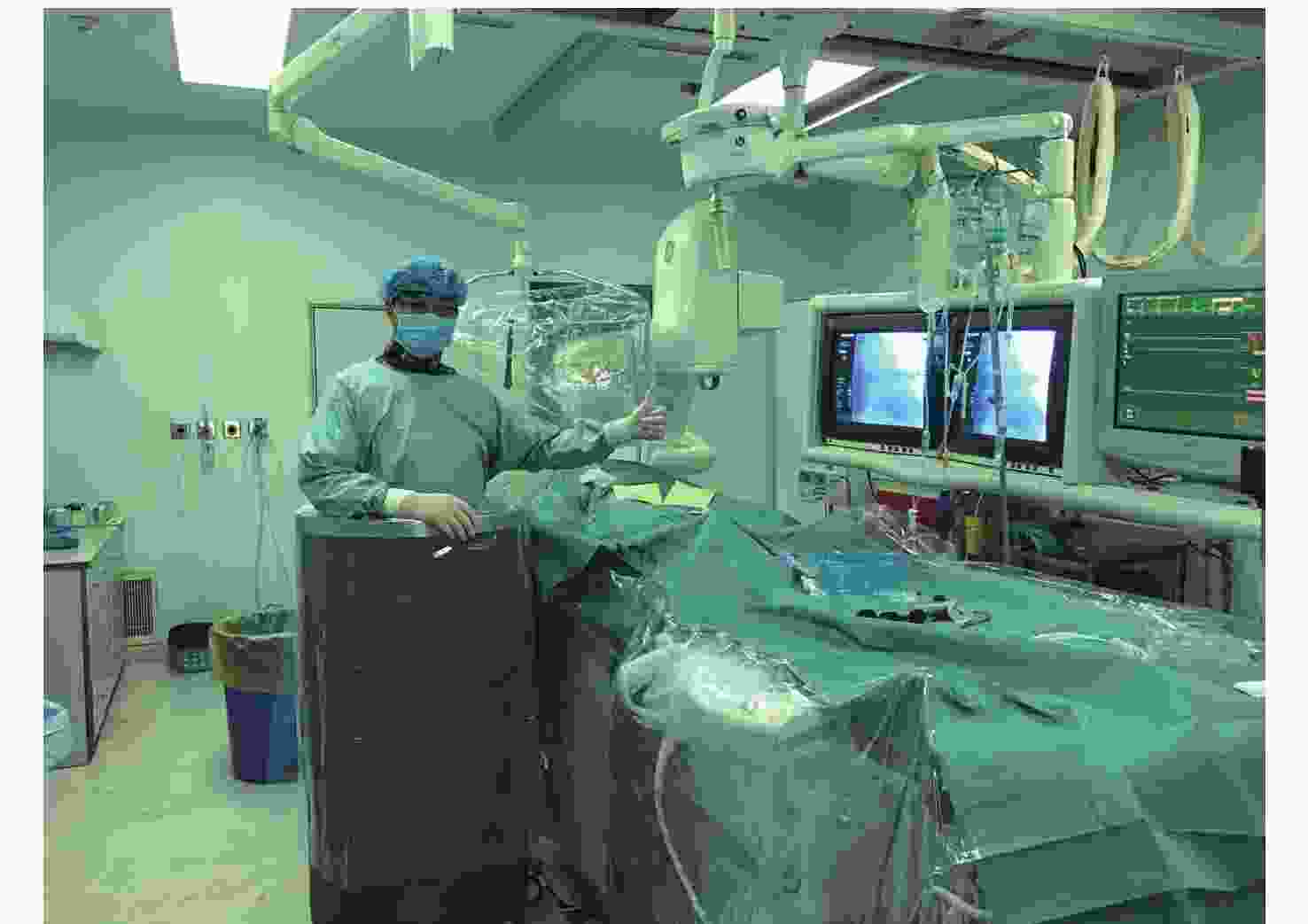
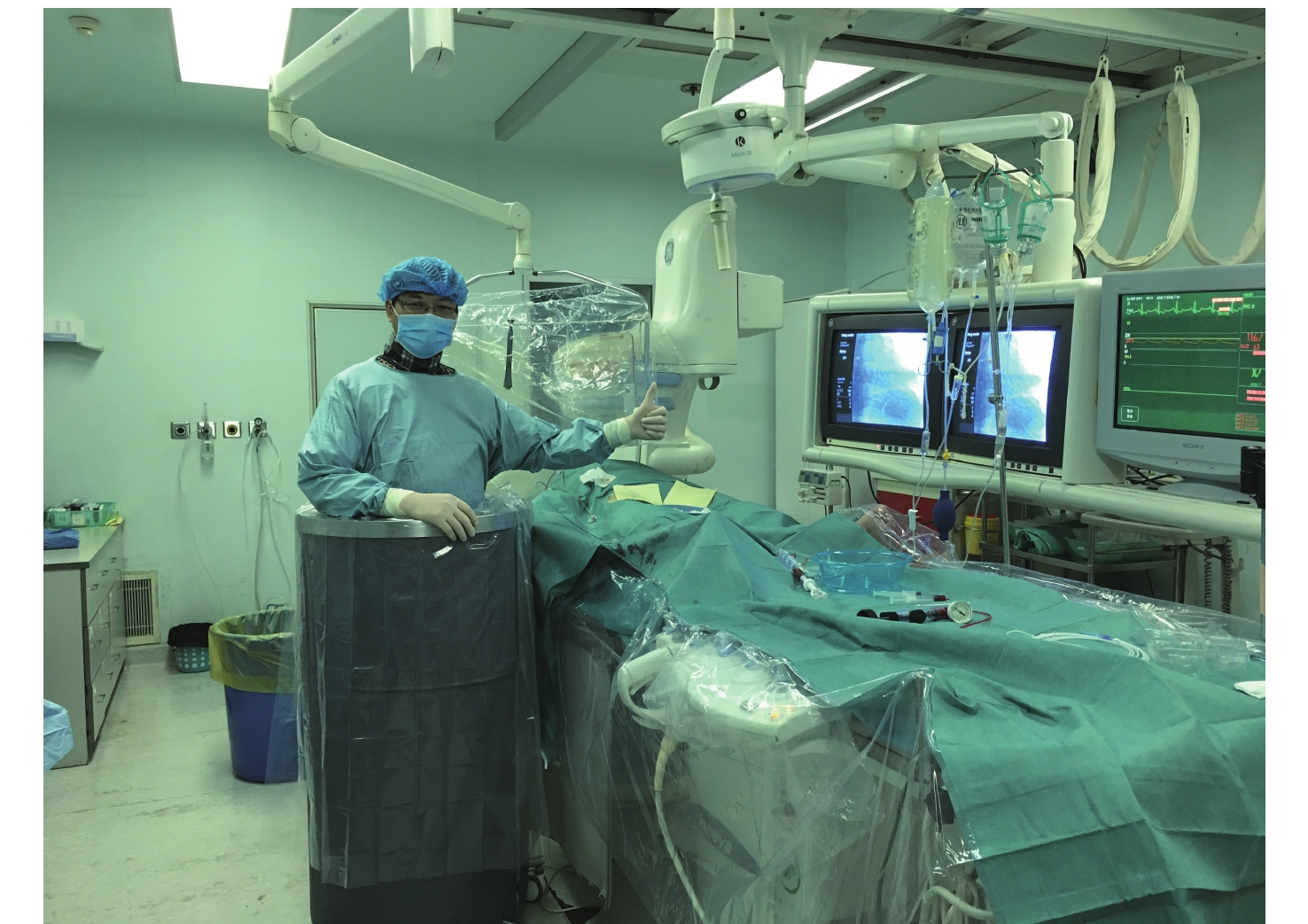
Figure S1. New X-ray protection device Photograph shows the scene while using NPD in the catheterization laboratory. NPD, new X-ray protection device.
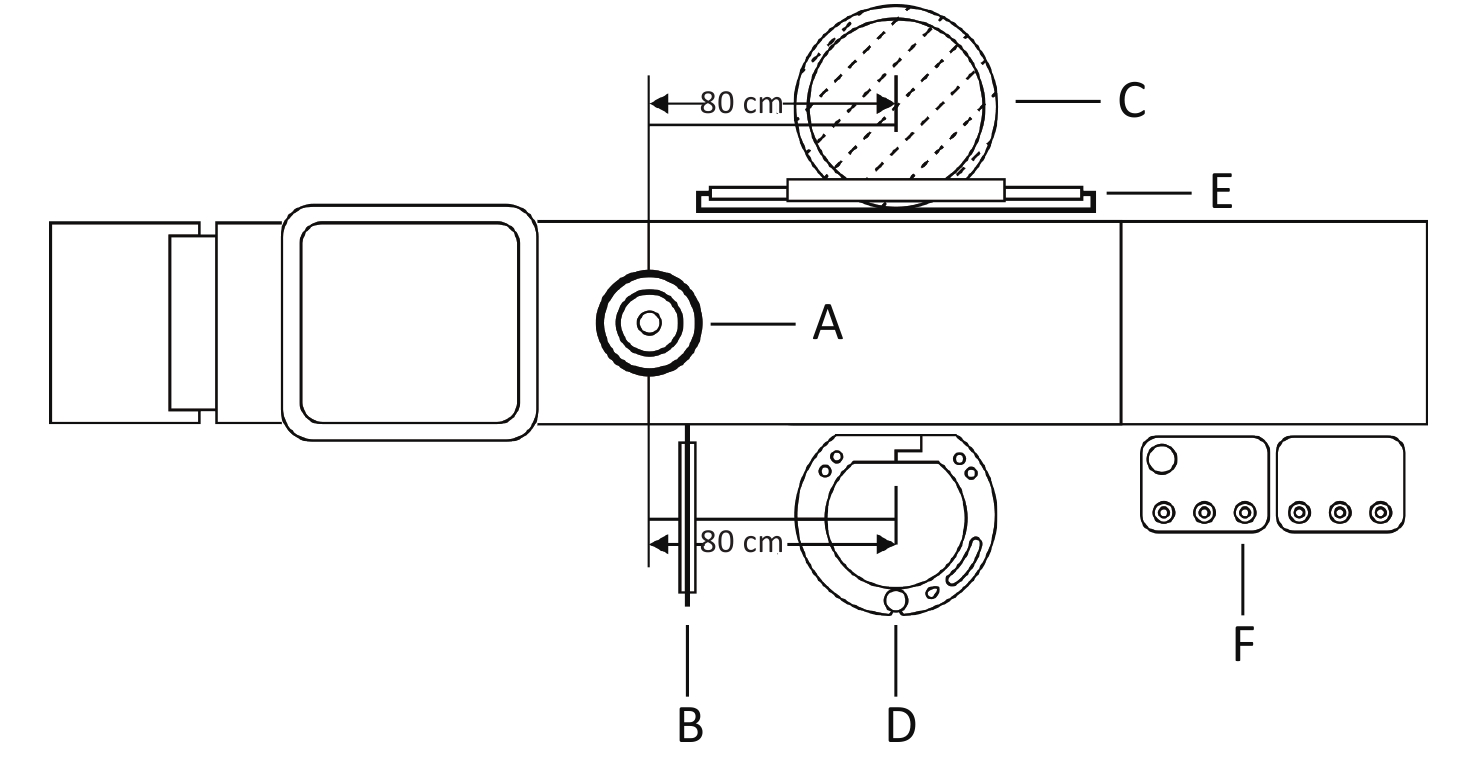
Firstly, the ambient dose equivalent rates (ADER) inside and outside of the NPD and TLC were tested in an off-work catheter lab. A movable ceiling-suspended lead shield and a table-mounted side lead shield were kept at the operation table to simulate the real surgical environment. The NPD or TLC was successively set in the operator position (The TLC was set on a barrel-like wooden frame). ADER was measured inside and outside of NPD and TLC at six height levels, i.e. 5, 10, 30, 60, 90, 120 cm from the ground and each test was performed three times with a dosimeter (AT1121, ATOMTEX, Belarus). The measurements were performed using a digital angiography unit (Artis zee, Siemens, Germany) with an x-ray tube under the tabletop at a magnification of 20 cm and a frame rate of 15 frames/s.
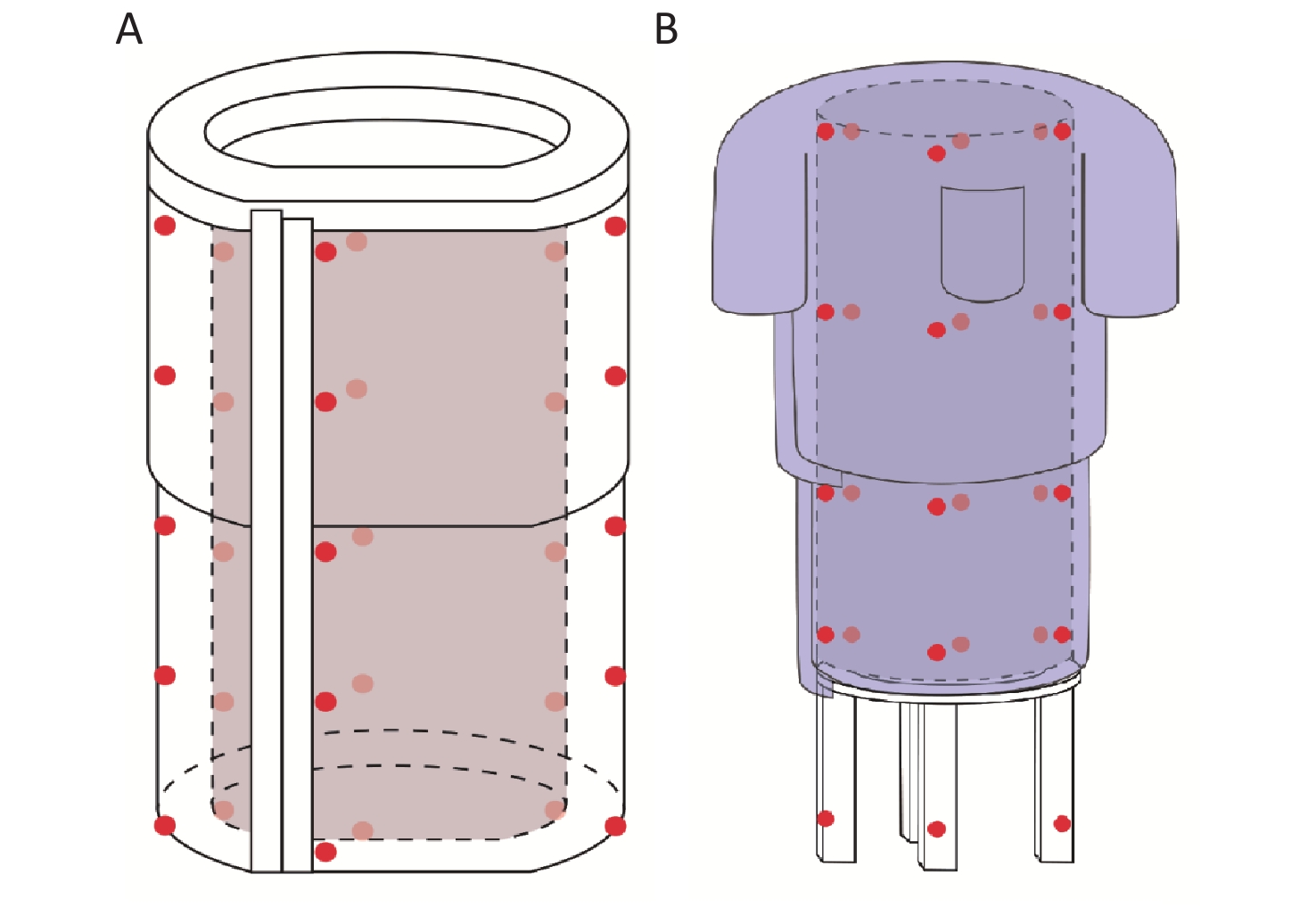
Secondly, the cumulative absorbed doses inside and outside of the NPD and TLC were determined during 121 coronary interventions. Patients referred for CAG or PCI were successively included in the First Affiliated Hospital of Nanjing Medical University from December 2017 to February 2018. The procedures involved access from either radial artery or femoral artery or both. The characteristics of the patients and the parameters of the procedures are shown in Table 1. The NPD was set in the operator position, while the TLC was simultaneously and symmetrically set at the opposite position of the tabletop (Supplementary Figure S2 available in www.besjournal.com). Forty thermoluminescent dosimetries (TLDs) were attached at five height levels (10.0, 37.5, 65.0, 92.5, 120.0 cm from the ground, respectively), in four directions, inside and outside of the NPD during the procedures. Another 40 TLDs were attached at the corresponding positions of the TLC (Supplementary Figure S3 available in www.besjournal.com). Procedures were performed at 3 catheter labs using different digital angiography units (Artis zee, Siemens Germany; UNIQ FD20, Phillips, Netherlands; or Innova 2000, GE, United States). Parameters were set at a magnification of 17–20 cm and a frame rate of 7.5 frames/s for each digital angiography unit[5]. The cumulative absorbed dose was analyzed by a TLD reader (Harshaw 5500, ThermoFisher, US) and the X-ray shielding efficiency was compared between the NPD and TLC.
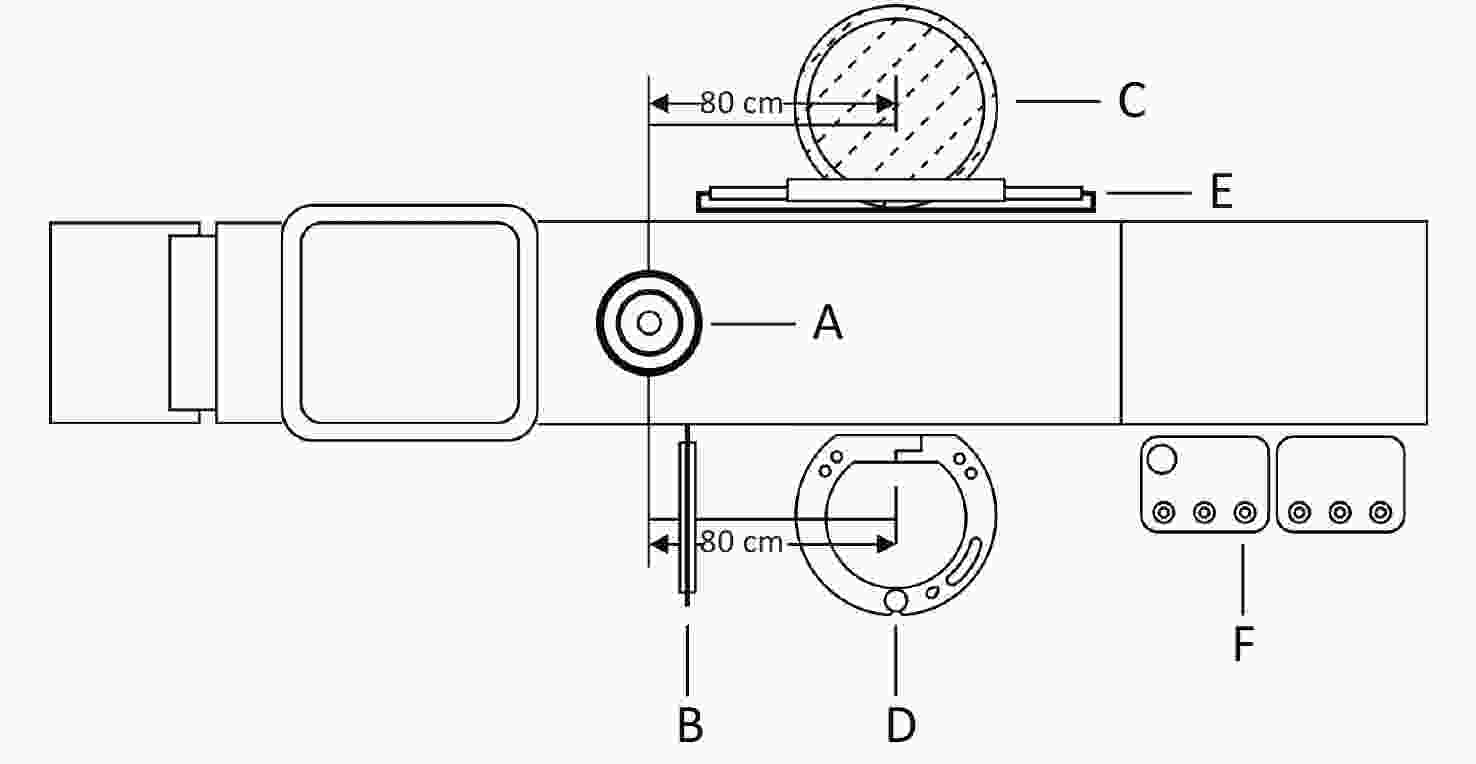
Figure S2. Positions of NPD and TLC in the catheterization laboratory during cumulative dose measurement. (A) X-ray tube; (B) Ceiling-suspended lead shield and table-mounted side lead shield; (C) Position of the TLC; (D) Position of the NPD; (E) Screen; (F) Control panel. NPD, new X-ray protection device; TLC, traditional lead clothing.
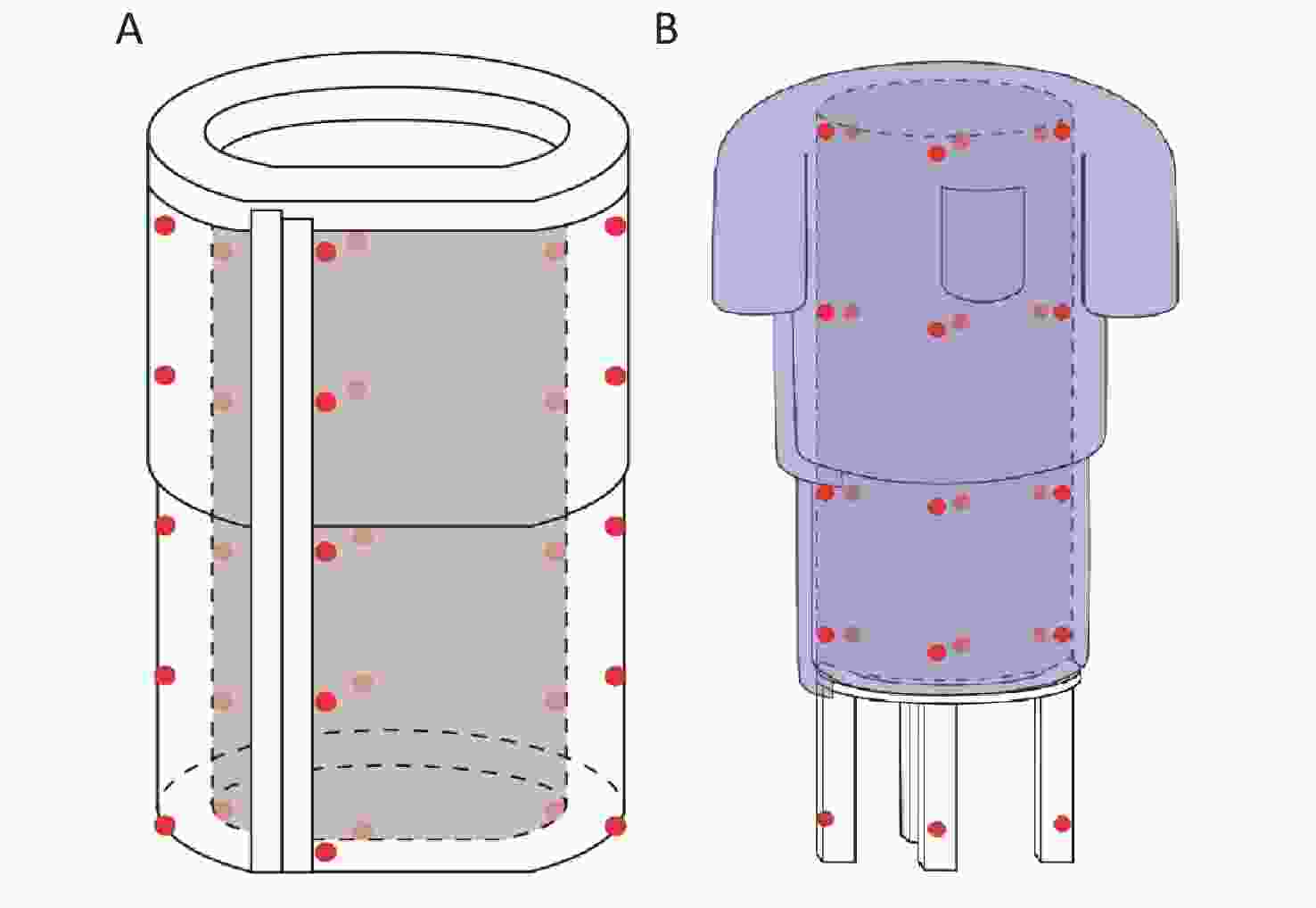
Figure S3. Placements of TLDs attached on NPD and TLC. (A) Anterior side of the NPD; (B) Posterior side of the NPD. Crimson dots indicate that the TLDs were attached to the outside of the NPD or TLC, and light-red dots indicate that the TLDs were attached to the inside of the corresponding positions. TLDs, thermoluminescent dosimetries; NPD, new X-ray protection device; TLC, traditional lead clothing.
Item Overall (n = 121) Gender, male 89 (73.6%) Age, yrs 66.8 ± 9.3 BMI, kg/m2 24.3 ± 2.5 Clinical diagnosis Stable angina 25 (20.7%) Unstable angina 57 (47.1%) NSTEMI 12 (9.9%) STEMI 25 (20.7%) Access site Radial only 83 (68.6%) Femoral only 1 (0.8%) Femoral and Radial 37 (30.6%) CAG 61 (50.4%) PCI 60 (49.6%) Single vessel lesion 36 (29.8%) Multivessel lesion 24 (19.8%) Calcification 19 (15.7%) Chronic total occlusion 9 (7.4%) Syntax Score 25.3 ± 6.9 Air kerma radiation exposure, Gy 1.7 ± 1.5 Fluoroscopy time, min 15.0 ± 14.8 Procedure time, min 52.8 ± 41.2 Contrast volume, mL 125.8 ± 69.7 Note. Values are presented as mean ± SD or number (percentage). BMI = body mass index; STEMI = ST-segment elevation myocardial infarction; NSTEMI = non-ST-segment elevation myocardial infarction; CAG = coronary artery angiography; PCI = percutaneous coronary intervention. Table 1. Baseline characteristics of the patients and parameters of the procedures
All procedures were performed by Dr. C. Li, who was required to stand inside the NPD without wearing the lead apron. On the basis of ensuring successful completion of the procedure, the first operator tried to minimize the fluoroscopy time to reduce unnecessary radiation dose. Other medical staff were trained to stay next to the NPD and cooperate with the first operator to complete the procedure.
The routine measures to reduce radiation exposure, including lead lenses, lead collar, lead vest, movable ceiling-suspended lead shield, and a table-mounted side lead shield, were used as per usual practice. All operators besides the first author were required to wear the lead apron during the procedure.
The TLD2000C lithium fluoride LiF: Mg, Cu, P round element with a diameter of 4.5 mm and a thickness of 0.8 mm was selected for the determination of the cumulative absorbed dose. The same batch was selected and screened to ensure a dispersion of < 5.0%. In total, 80 TLDs compositions of LiF: Mg, Cu, P were analyzed by a TLD reader (Harshaw 5500, ThermoFisher, United States) and the detailed methods were as follows.
The TLDs were first placed in a self-developed annealing pan for the thermal treatment processes. Then two-stage temperature ramps were performed with the first stage of 135 ℃ for 8 s and a second stage of 240 ℃ for 20 s. The heating rate was set at 15 ℃/s[6]. Readings were carried out by a TLD reader equipped with a micro-tip vacuum needle and a readout software ‘Winrems’ (ThermoFisher Scientific Inc.; Waltham, Massachusetts, US). The reader is capable of reading 50 TLDs automatically at one time. The signal definition of the detector was defined as the time integral of the thermoluminescence curve after subtracting the background value.
All statistical analyses were performed using SPSS21.0 (SPSS Inc.; Chicago, Illinois, US). Continuous variables are presented as mean ± standard deviation (SD). Categorical variables are presented as frequencies and percentages. Comparison between the two groups was performed using the t test for normally distributed variables. A two-tailed P value of < 0.05 was considered as a statistically significant difference.
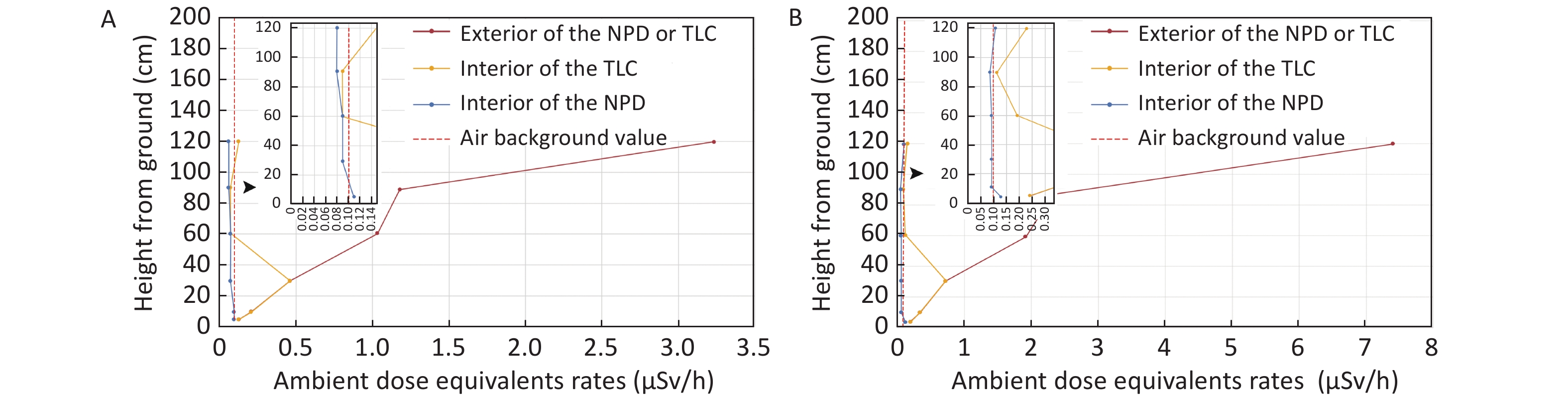
The TLC does not cover the lower leg segment, thus this part receives no protection under the traditional protection condition. As a result, the maximum ADER reached (0.46 ± 0.17) µSv/h during fluoroscopy, and (0.74 ± 0.03) µSv/h during cineradiography at the level of 30 cm from the ground. By comparison, while using the NPD, similar protection effects were detected no matter within or beyond 30 cm from the ground level. Besides, at all detected levels, the inner ADERs of the NPD in fluoroscopy and cineradiography were comparable to or even numerically lower than the baseline air background. NPD showed significantly lower inside ADERs than that of the TLC at levels of 5, 10, 30, 60, and 120 cm from the ground under fluoroscopy, and at levels of 5, 10, 30, 90, and 120 cm from the ground under cineradiography, though the corresponding ADERs were comparable outside the NPD and TLC (Figure 1A–B, Supplementary Table S1 available in www.besjournal.com).
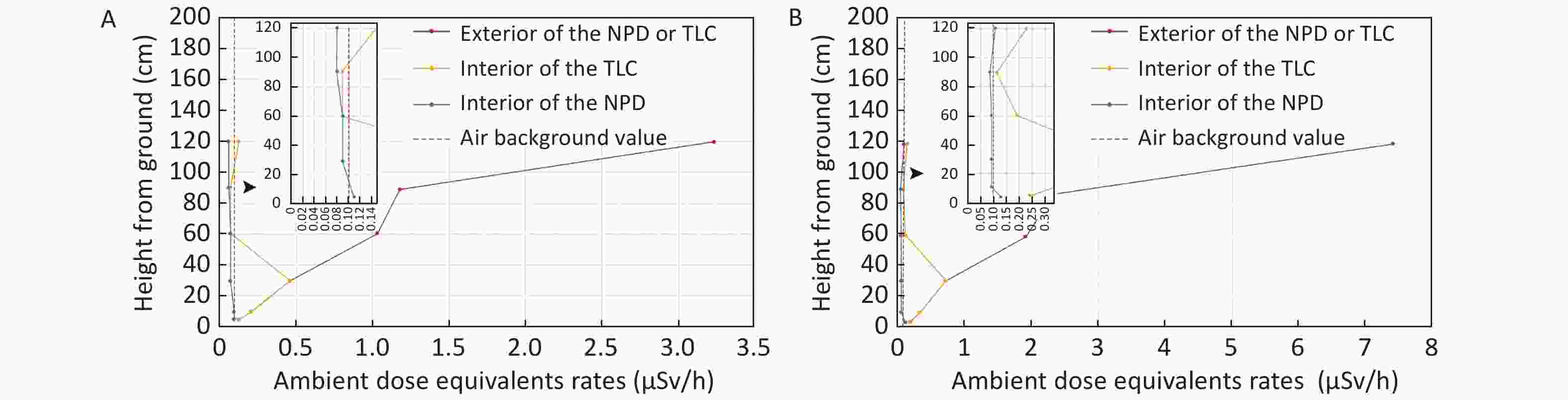
Figure 1. Comparisons of ADER between NPD and TLC in fluoroscopy and cineangiography. (A) Comparisons of ADER between NPD and TLC in fluoroscopy. (B) Comparisons of ADER between NPD and TLC in cineangiography. ADER, ambient dose equivalent rates; NPD, new X-ray protection device; TLC, traditional lead clothing.
Location NPD TLC NPD vs. TLC Outside Inside P Outside Inside P Outside P Inside P ADER-FLORO Level 6 (120 cm) 3.333 ± 0.306 0.082 ± 0.000 0.0001 3.361 ± 0.317 0.146 ± 0.033 0.0001 0.918 0.028 Level 5 (90 cm) 1.217 ± 0.075 0.082 ± 0.001 < 0.0001 1.221 ± 0.041 0.094 ± 0.020 < 0.0001 0.939 0.358 Level 4 (60 cm) 1.043 ± 0.060 0.086 ± 0.000 < 0.0001 1.011 ± 0.101 0.093 ± 0.003 < 0.0001 0.662 0.010 Level 3 (30 cm) 0.457 ± 0.168 0.086 ± 0.002 0.019 − 0.457 ± 0.168* − − 0.019 Level 2 (10 cm) 0.264 ± 0.032 0.109 ± 0.012 0.001 − 0.264 ± 0.032* − − 0.001 Level 1 (5 cm) 0.153 ± 0.005 0.113 ± 0.009 0.003 − 0.153 ± 0.005* − − 0.003 ADER-CINE Level 6 (120 cm) 7.400 ± 0.346 0.114 ± 0.002 < 0.0001 7.269 ± 0.174 0.234 ± 0.034 < 0.0001 0.590 0.004 Level 5 (90 cm) 2.336 ± 0.055 0.083 ± 0.001 < 0.0001 2.185 ± 0.063 0.118 ± 0.019 < 0.0001 0.035 0.032 Level 4 (60 cm) 1.910 ± 0.035 0.085 ± 0.001 < 0.0001 1.693 ± 0.250 0.189 ± 0.098 < 0.0001 0.211 0.139 Level 3 (30 cm) 0.737 ± 0.031 0.087 ± 0.001 < 0.0001 − 0.737 ± 0.031* − − < 0.0001 Level 2 (10 cm) 0.387 ± 0.047 0.087 ± 0.002 0.0004 − 0.387 ± 0.047* − − 0.0004 Level 1 (5 cm) 0.242 ± 0.048 0.130 ± 0.016 0.018 − 0.242 ± 0.048* − − 0.018 Note. *There is no protection here. NPD, new X-ray protection device; TLC, traditional lead clothing; ADER, ambient dose equivalent rates. Table S1. Comparisons of ADER between NPD and TLC in fluoroscopy and cineradiography (μSv/h)
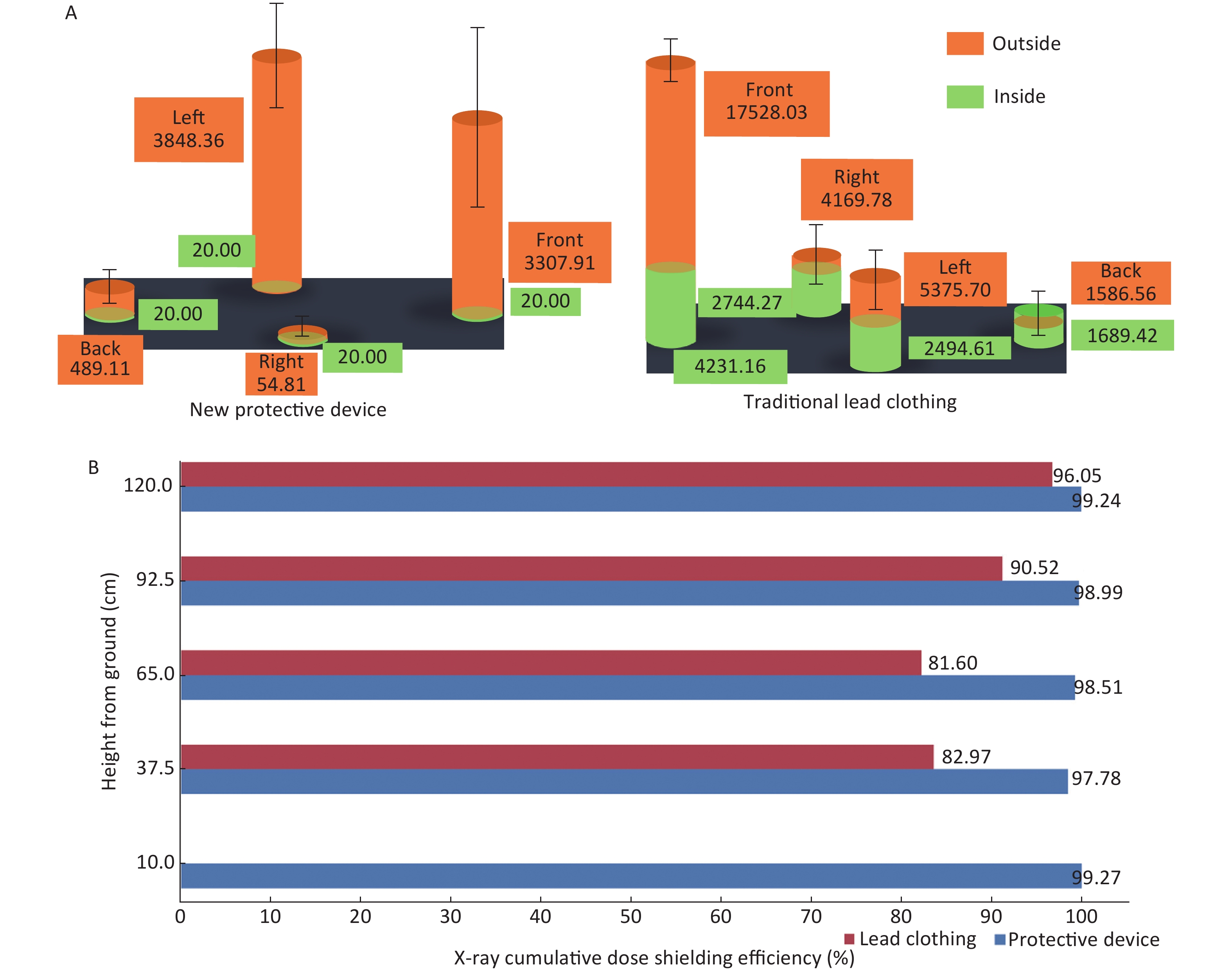
The corresponding cumulative dose distributions were comparable outside the NPD and TLC. All cumulative doses measured inside the NPD were below detection threshold of 40 μSv, calculated as the lower limiting value/2 (20 μSv) as recommended[7], which were significantly lower than that of the corresponding doses inside the TLC (Figure 2A, Supplementary Table S2 available in www.besjournal.com). Based on the results of cumulative doses, we calculated the shielding efficiencies of the NPD and TLC at the 5 investigated height levels. As a result, the shielding efficiencies of TLC were found to be between 81.60%–96.05% at different levels; By comparison, the corresponding shielding efficiencies of NPD were between 97.78%–99.27%, which was significantly superior to that of the TLC (Figure 2B, Supplementary Table S2 available in www.besjournal.com).
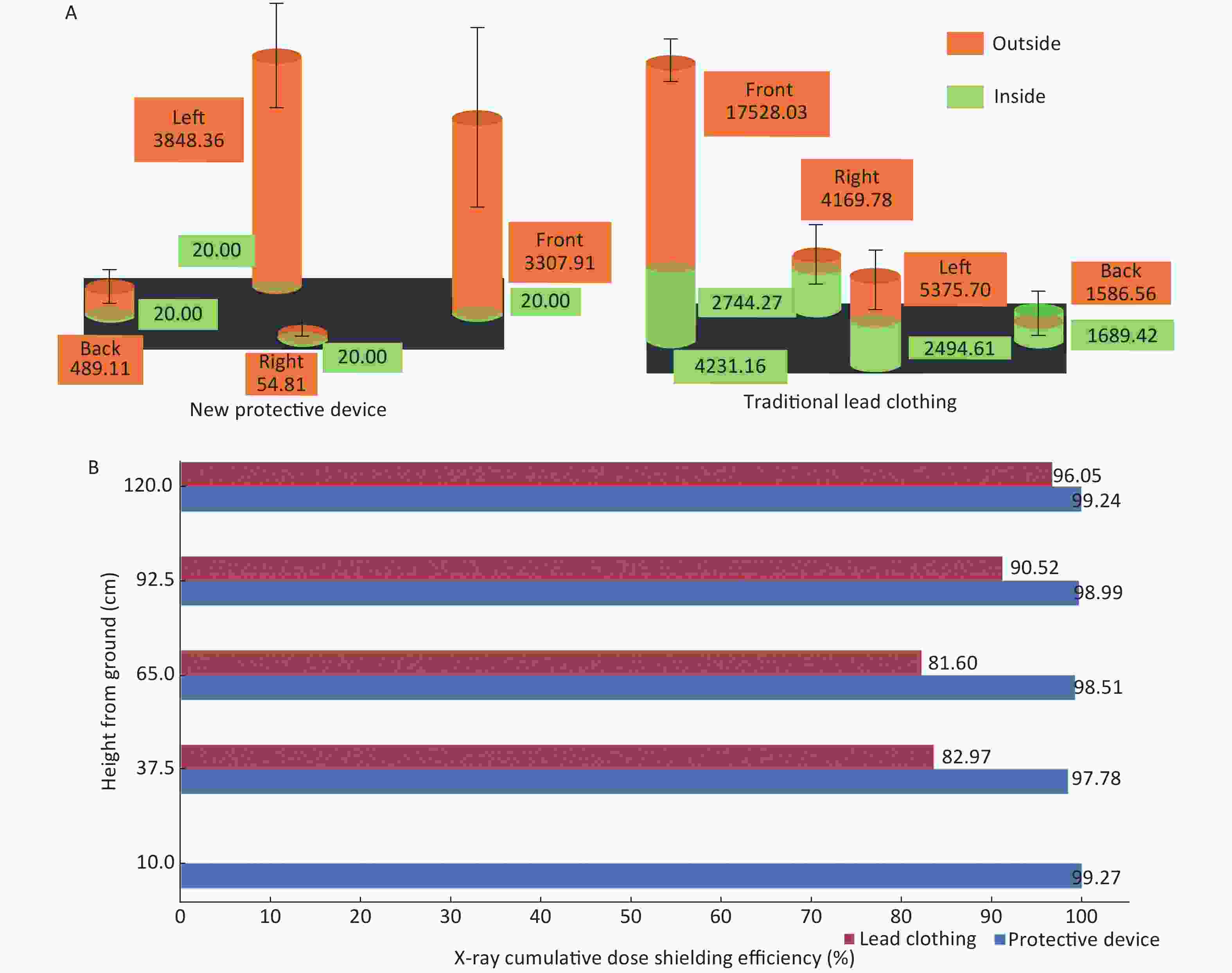
Figure 2. Cumulative dose distribution and shielding efficiency of NPD and TLC. Cumulative dose distribution of NPD and TLC. (B) Comparison of shielding efficiency between NPD and TLC. NPD, new X-ray protection device; TLC, traditional lead clothing.
Location NPD TLC Outside Inside Efficiency (%) Outside Inside Efficiency (%) Level 5 (120.0 cm) 11015.62 80 99.24 19788.17 781.84 94.71 Level 4 (92.5 cm) 3606.94 80 98.99 28183.66 2671.11 90.52 Level 3 (65.0 cm) 5377.41 80 98.51 21797.63 4009.73 81.60 Level 2 (37.5 cm) 7937.08 80 97.78 30368.29 5171.95 82.97 Level 1 (10.0 cm) 10563.88 80 99.27 − 43162.61* − Note. *There is no protection here. NPD, new X-ray protection device; TLC, traditional lead clothing. Table S2. Cumulative dose distribution and shielding efficiency of NPD and TLC (μSv)
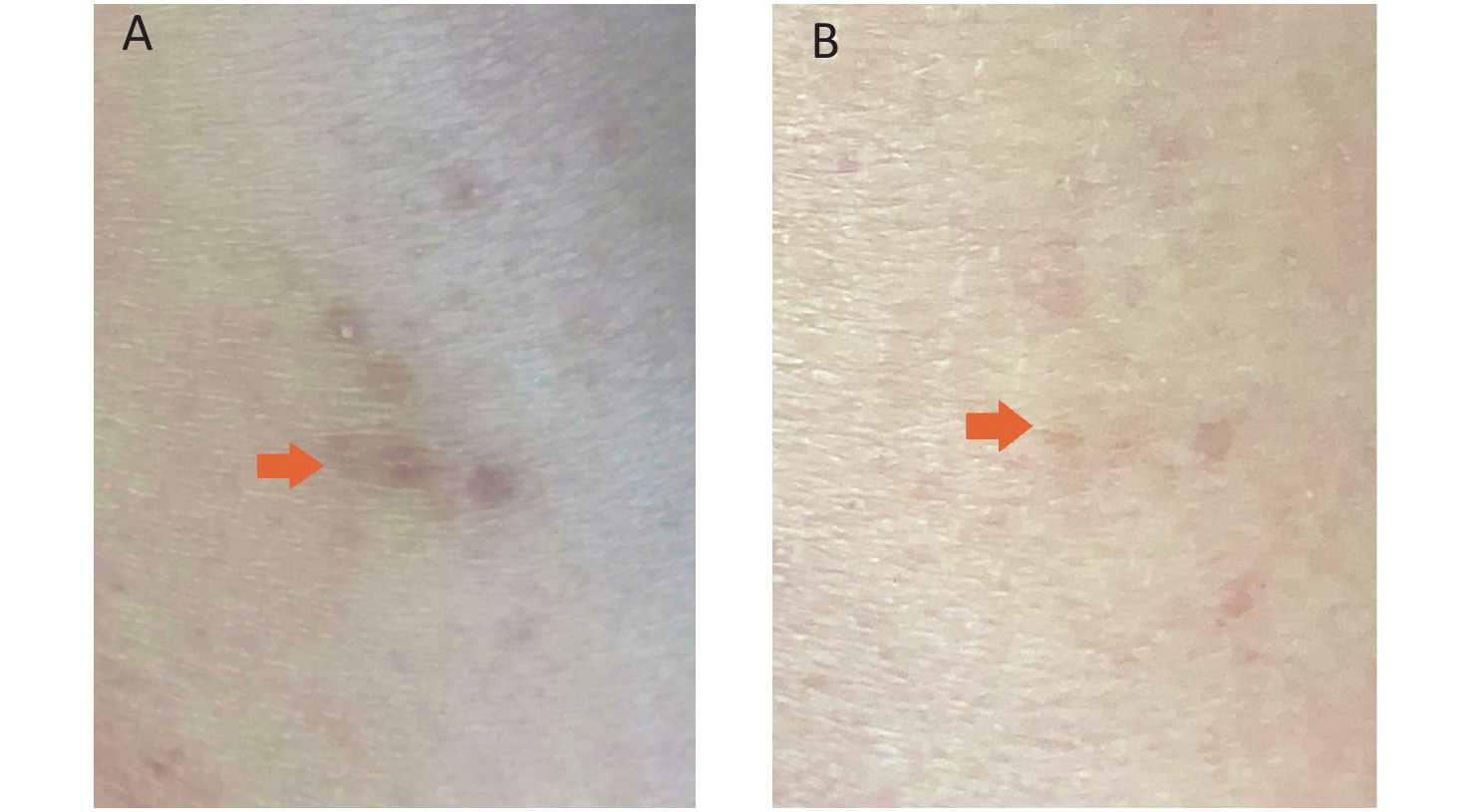
In our catheter lab, the operators regularly wear TLC while doing interventional procedures, which includes 5.3 kg of lead vest and 4.4 kg of lead apron. By comparison, the first operator (C. Li) used the NPD instead of lead apron in this study, which significantly lowered the extra load on his body. As a result, his back pain due to lumbar disc protrusion completely disappeared without any medical treatment during the 3-month study period. Besides, his initial diagnosis of left lower limb radiodermatitis at the beginning of this study which caused severe itching after daily procedures significantly recovered by the end of the study (Supplementary Figure S4 available in www.besjournal.com).
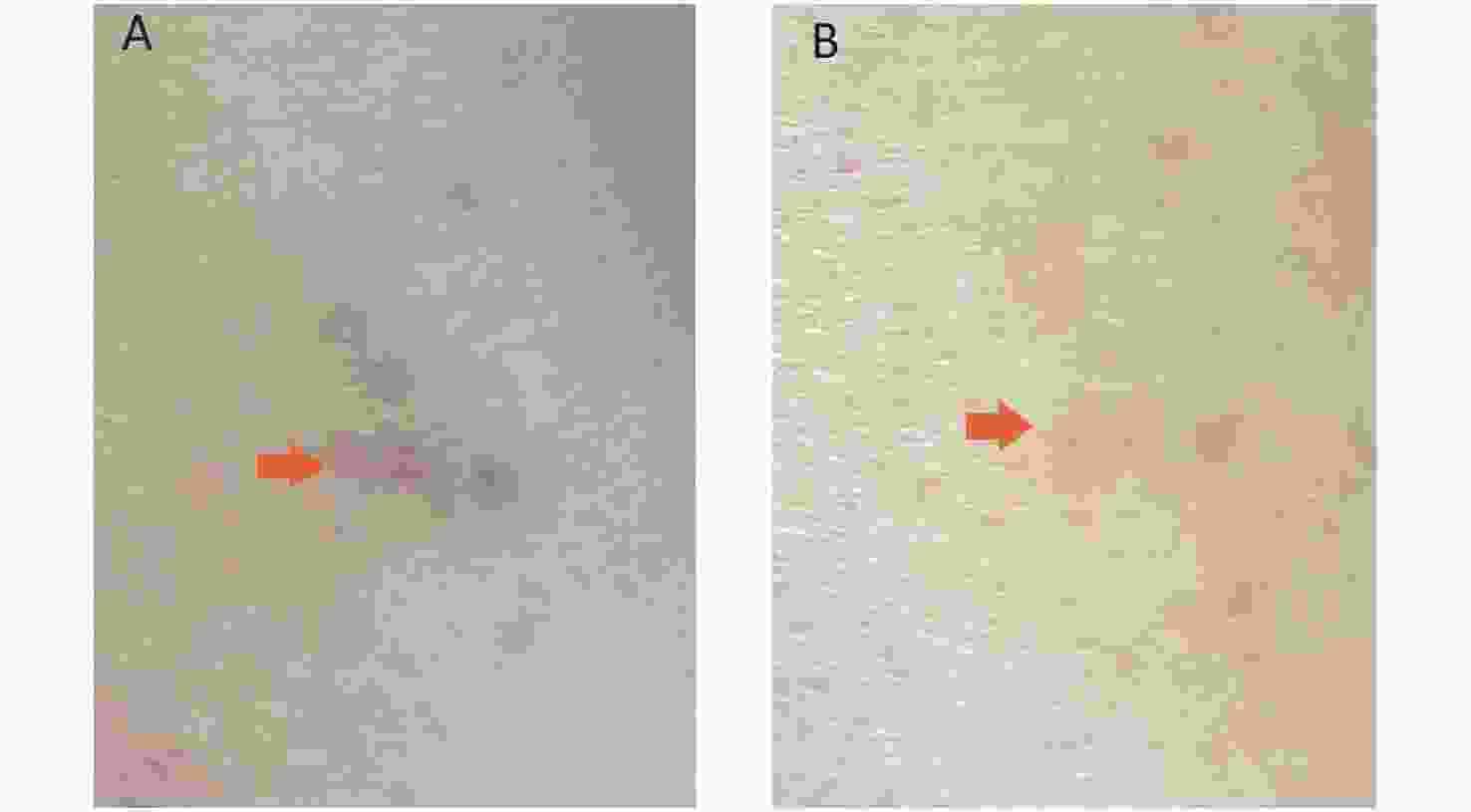
Figure S4. Recovery of the Lower Limb Radiodermatitis. (A) Arrow shows the baseline left lower limb skin injury due to the radiodermatitis; (B) Arrow shows recovery of the radiodermatitis.
Our study showed that the NPD was superior to the TLC in the following aspects: 1) the NPD provided an ADER similar to the baseline background of the air in both fluoroscopy and cineradiography conditions; 2) The excellent shielding efficacy of NPD was also verified by the study of cumulative dose in the real interventional procedure environment; 3) The NPD is beneficial to reduce the complications associated with radiation and body-load (e.g. left lower limb radiodermatitis, lumbar disc protrusion). The superior shielding efficacy of NPD should attribute to its dual layer lead rubber as well as all-round protection especially for a height of approximately 30 cm from the ground, where the TLC does not cover.
Several endeavors have been made to improve the shielding efficacy as well as alleviate the body-load for the interventionists[8-10]. However, shortcomings including inablility to cover the lower limb, inconvenient to move around and lower protection efficacies were reported[10]. To the best of our knowledge, this NPD is the first zero-load protection device that meets the requirements of coronary intervention, which fully covers the operator’s lower limb, increases the shielding efficacy, enables the operators to move around during the procedure, and liberates their lower body from wearing heavy lead apron.
Two limitations of this NPD should be pointed out: 1) it does not protect a range above the breast level where we still need to wear a lead vest during the procedure; 2) The radio-protective effect is generally confined to the first operator, although other operators staying next to the NPD may also be protected to some extent, personnels such as circulating nurses as well as patients may not receive any protection from the device.
In summary, this preliminary study of the NPD revealed that it significantly improved the shielding efficiency, lowered the body load, and relieved the radiation and body-load associated complications, which indicated its significant superiority to the TLC for coronary intervention.
LU Yi contributed to data collection, statistics and article writing; Abdus Samee contributed to article writing; WANG Jin and WANG Fu Ru contributed to sample detection; TANG Shao Wen contributed to statistics; YANG Ming Wen and YE Sen contributed to sample collection; LI Jin Shuang, GONG Xiao Xuan and LI Yong contributed to data collection and article writing; LI Chun Jian contributed to the design of the study, data analysis and the revision of the article. All authors reviewed and approved the final version of the article for publication.
The authors declare that they have no conflicts of interest.
HTML
Reference






 Quick Links
Quick Links
 DownLoad:
DownLoad: