-
Campylobacter surpassed Salmonella several years ago and has recently emerged as one of the most important foodborne pathogens even in high-income countries, bearing a significant economic burden[1]. In low- and middle-income countries, limited data indicate that the rate of Campylobacter infection has increased[2]. In China, between July 2005 and December 2006, 4.84% of 3,061 patients with diarrhea were positive for Campylobacter, and the highest prevalence was found among patients under 7 years of age[3]. On the basis of the detection rate of Campylobacter from raw chickens and the consumption of chicken products in China from 2007 to 2010, some researchers speculated that 1.6% of the urban population and 0.37% of the rural population are affected by Campylobacter every year[4]. However, these data are limited by detection method sensitivity, regional differences, monitoring range, and other factors. Few cases of Campylobacter infection have been detected by monitoring, but the reported cases of Campylobacter infection represented only a part of the burden. Therefore, the Campylobacter outbreak is rare, and incomplete cases of Campylobacter outbreak have been reported. On August 26, 2019, a Campylobacter outbreak linked to meal delivery was found in a factory of automotive parts in Shunyi District, Beijing, China. To provide effective control measures, Shunyi Center for Disease Control and Prevention surveyed additional cases, infection source, vehicle for infection, and mode of transmission.
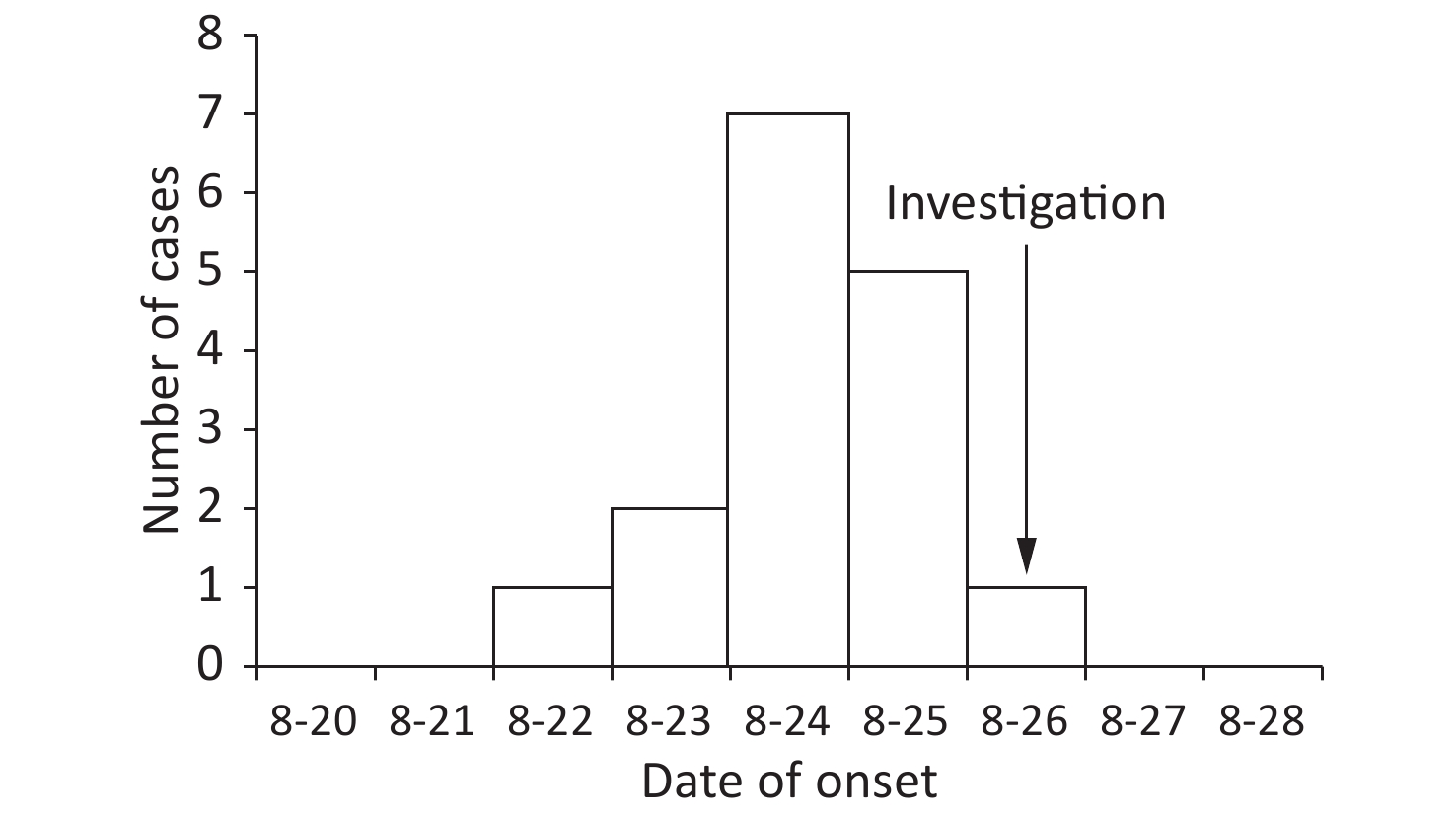
Self-designed questionnaires were used to collect basic personal information, illness information (if any), and exposure history to suspected food, water, and patients. Cases’ and cooks’ rectal swabs were collected and inserted with Cary-Blair transport medium for preservation. Food and environmental samples were collected in a sterile plastic bag or jar to avoid cross-contamination. All the samples were refrigerated and transported to Shunyi Center for Disease Control and Prevention for testing. Clinical feature analysis and space-time distribution of the population showed that 16 of 130 workers were identified to be suspected cases (had a history of common food exposure), and 12 of them were laboratory-confirmed cases. All the cases were workers at the factory of automotive parts, and their age ranged from 23 years to 42 years. The incidence rate was 12.3% (16/130). The main clinical symptoms were diarrhea (93.8%), abdominal pain (75.0%), dizziness (50.0%), nausea (43.8%), fever (31.2%), headache (31.2%), and vomiting (25.0%), which were consistent with the characteristics of lower gastrointestinal infections caused by intestinal bacteria. Furthermore, 63% (10/16) of the cases were male, and the median age of onset was 36 years (range of 23–42 years). The outbreak lasted 5 days, from August 22 to 26. The number of cases increased and decreased rapidly within a short period, and the peak was recorded on August 24 (Figure 1). The epidemic curve was compatible with a point source outbreak, indicating the possibility of foodborne contamination.
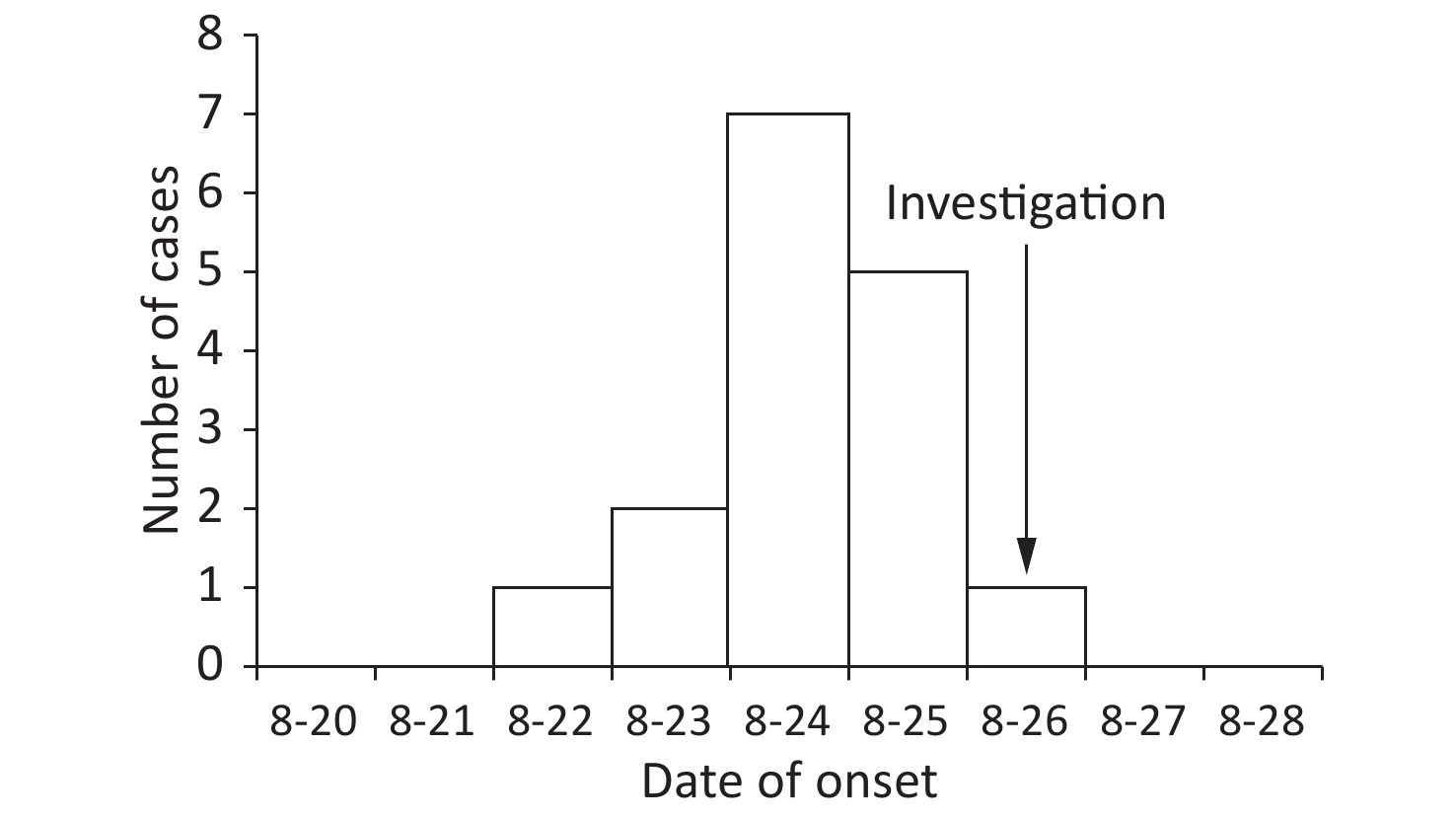
Figure 1. Epidemic curve of the probable outbreak cases of Campylobacter infection by 24 h intervals in a factory of automotive parts in Shunyi, Beijing, China, 2019.
All the factory workers who consumed the food supplied by their catering distribution company were subjected to a case-control study. A suspected case was defined by the onset of diarrhea (≥ 3 times or more loose stools per day) or other symptoms of gastrointestinal illness (e.g., abdominal pain, nausea, or vomiting) in the factory beginning August 19, 2019. A laboratory-confirmed case was identified on the basis of the stool or vomit specimen of a suspected case that tested positive for Campylobacter. Eventually, 10 laboratory-confirmed cases and 12 healthy controls were selected. The univariate analysis of all the food items from August 19 to 24 revealed that the cases were significantly more likely to be exposed to sautéed eel with duck blood curd (OR = 18.0, 95% CI = 1.7–196.3) and dried tofu slices (OR = 7.0, 95% CI = 1.1–45.9) than the controls (Table 1). A logistic regression model with all the statistically significant risk factors identified from univariate analysis was established. The results of the multivariable model showed that the consumption of sautéed eel with duck blood curd was the only statistically significant risk factor of illness (OR = 20.8, 95% CI = 1.2–352.2; Table 1).
Date Exposure N % Univariate
analysis
OR (95% CI)P value Multivariate
aanalysis
OR (95% CI)P value Case
(n = 10)Control
(n = 12)Case Control August 20,
2019Sautéed Eel with
Duck Blood Curd9 4 90.0 33.3 18.0 (1.7–196.3) 0.010 20.8 (1.2–352.2) 0.036 August 21,
2019Sautéed Shredded Pork
with Dried Tofu Slices7 3 70.0 25.0 7.0 (1.1–45.9) 0.046 7.4 (0.4–128.0) 0.168 Cucumber with Dried
Tofu Slices7 3 70.0 25.0 7.0 (1.1–45.9) 0.046 1.5 (0.1–20.5) 0.765 Note. OR, odds ratio; CI, confidence interval. Table 1. Relative risk of implicated food items
The kitchen of the catering distribution company was investigated to check whether kitchen utensils were unclean and placed disorderly. No independent cold food production room was available, and raw and cooked foods were not stored separately in refrigerators. Food was transported to customers via ordinary vehicles at room temperature. In the whole process of food packing to final consumption, food was stored in a delivery box for at least 1 h. Therefore, food could be potentially contaminated during food processing, storage, and transportation. In a study on the process of cooking sautéed eel with duck blood curd, about 70 kg of duck blood curd is blanched (cooked for a short time in boiling water or steamed). Along with bean sprout and ham, duck blood curd is boiled in a cauldron (added hot pot seasoning) without ensuring that adequate internal cooking temperatures are achieved. Lastly, hot oil is poured into the cauldron. About 70 kg of duck blood curd is cooked in a cauldron at a time, and cooking time is not more than 5 min to ensure the tenderness of duck blood curd. However, under such conditions, duck blood curd cannot be cooked completely. Campylobacter is inactivated after beef reaches an internal temperature of 70 °C for 10 min[5]. If the internal temperature does not reach 70 °C, then the survival rate of Campylobacter is predicted to be 48%–98%[6]. As recommended by the UK Food Standards Agency, food should be cooked at the minimum internal temperature of 65 °C for 10 min.
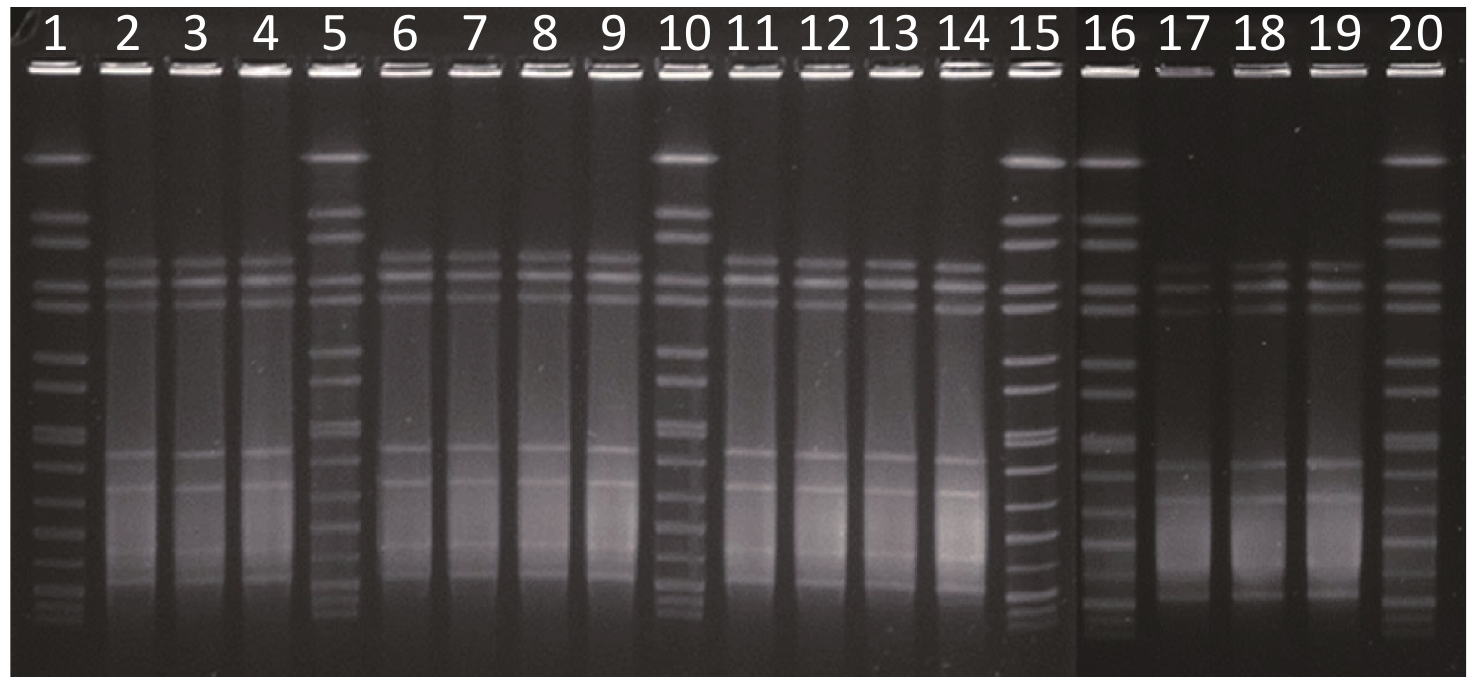
Rectal swabs from 16 cases and 7 food handlers, 18 retained food samples (between August 25 and 26), different batches of duck blood curd (the problem batch had been used up), 1 drinking water, and 4 swabs of environmental samples from the cookware and countertops were collected for microbiological examination. Intestinal bacteria, including Salmonella, Bacillus cereus, Vibrio parahaemolyticus, pathogenic Escherichia coli, Clostridium perfringens, and Campylobacter were tested via a culture method. If bacteria were isolated from the samples, isolates were further subjected to pulse field gel electrophoresis (PFGE) to analyze the genotype pattern through digestion with SmaI. PFGE cluster analysis was performed using the unweighted pair-group method with arithmetic means in BioNumerics v5.1 (Applied Maths). The strains were verified on the basis of their PFGE profile similarity to the outbreak isolate. The results showed that 12 of the 16 rectal swabs from the cases were positive for Campylobacter (positive rate of 75.0%). The rectal swabs from five cooks and two food handlers in the catering distribution company were tested, and the two handlers were positive (a positive rate of 28.6%).
PFGE analysis with SmaI was performed to examine 14 Campylobacter isolates from 12 cases and 2 food handlers. All the isolates had the same PFGE pattern (Figure 2), suggesting that this phenomenon was likely a single-source outbreak caused by a group of highly clonal Campylobacter. Two food handlers were found to be asymptomatic confirmed cases. However, no person-to-person infection with Campylobacter associated with an asymptomatic food handler was reported[7]. Indeed, undercooked chicken is a recognized risk factor of Campylobacter infection[8-9]. Therefore, asymptomatic food handlers were contaminated with Campylobacter while handling poultry food by touching contaminated raw food materials, such as duck blood curd, but they were not the likely source of infection. The specimens of 18 retained foods, duck blood curd, 4 environmental samples, and 1 drinking water tested negative for Campylobacter (Table 2).
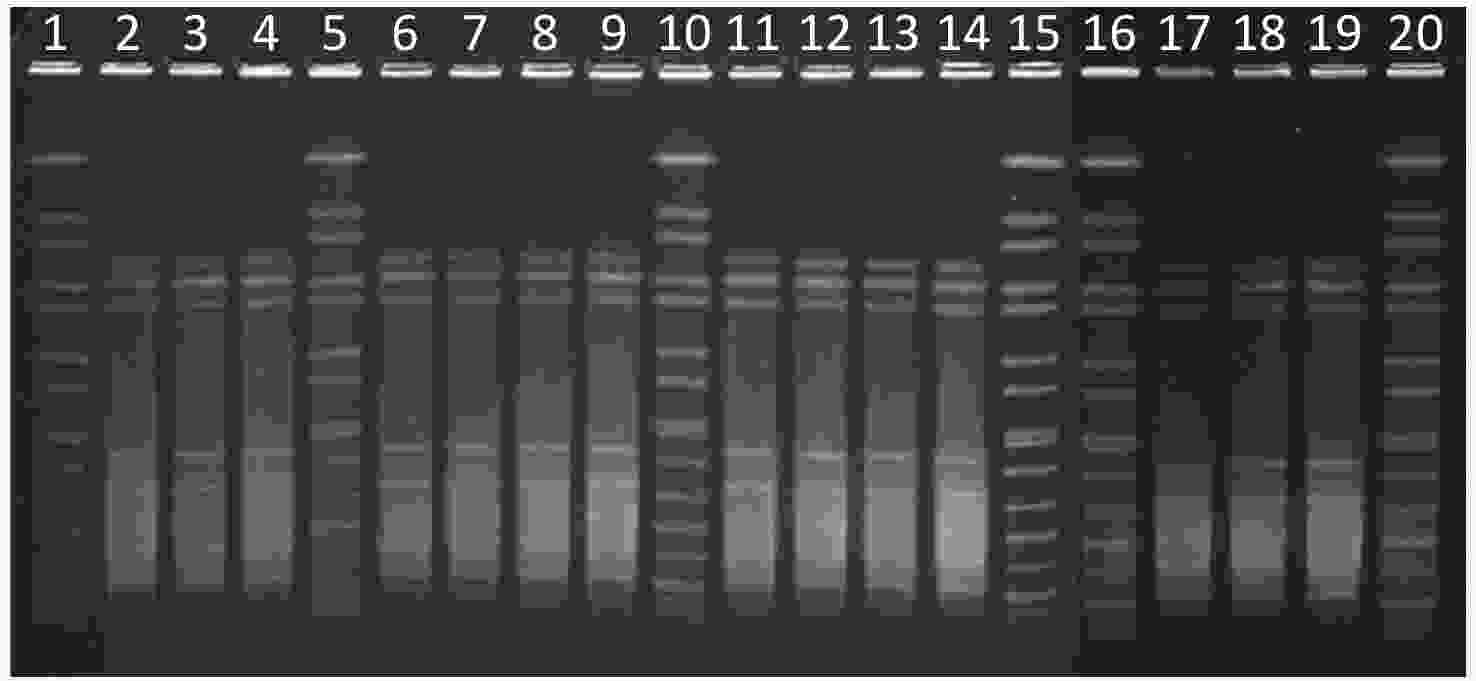
Figure 2. PFGE analysis with SmaI for 14 Campylobacter isolates from 12 cases and 2 food handlers. Lanes 1, 5, 10, 15, 16, and 20: H9812 reference standard. Lanes 2, 3, 4, 6, 7, 8, 9, 11, 12, 13, 14, and 17: Campylobacter isolates from 12 cases. Lanes 18 and 19: Campylobacter isolates from two food handlers. All of the 14 isolates had the same PFGE pattern. PFGE, pulse field gel electrophoresis.
Category N Positive Positive rate (%) Anal swab (case) 1,6 12 75.0 Anal swab (Kitchen staff) 7 2 28.6 Retained food∆ 18 0 0 Duck blood curd▲ 1 0 0 environmental sample 4 0 0 Drinking water 1 0 0 Note. ∆Retained foods from 25 to 26 August.
▲Different batches of duck blood curds.Table 2. Collection and test results of different types of samples
Some limitations were found in this study. First, the original source of infection was not identified, and microbiological evidence from high-risk food was lacking because it was not preserved. Second, although duck blood curd was a possible risk factor, accurately evaluating these associations was difficult because of the small size of the exposed population. Third, environmental samples tested negative for Campylobacter because of longer time intervals and difficulty in culturing bacteria from environmental samples[10]. Lastly, some cases might have failed to reveal any symptoms of gastroenteritis because of fear of adverse consequences. Therefore, the actual incidence rate might be higher than the reported value in this study.
Many Campylobacter outbreaks have been reported abroad, mostly because of exposure to or consumption of contaminated milk, mud, drinking water, chicken liver, and other factors. Duck blood curd as a risk factor of foodborne Campylobacter outbreak has Chinese characteristics, suggesting that this kind of food should be carefully prepared. Evidence has suggested that the cooking method used for poultry products is likely the cause of the outbreak. Based on the experience of the outbreak, our recommendation was to review the temperature and duration of cooking of poultry products. The Food Safety Regulatory Authority should emphasize prevention by providing more specific food preparation guidance that may help prevent future outbreaks. In addition, typical centralized outbreaks are difficult to detect because of the long incubation period of Campylobacter, so the construction of a foodborne disease surveillance system should be hastened, the sensitivity of surveillance should be improved, and scattered cases should be detected in the early stages.
In China, foodborne disease monitoring fully started only in 2010, which was later than that in developed countries and regions. Moreover, the current monitoring of Campylobacter is carried out voluntarily by regional laboratories, but it is not mandatory. For these reasons, further studies should be performed to determine how to actively monitor Campylobacter in food.
The authors declare that they have no competing interests.
We express our gratitude to the following: the staff of the factory of automotive parts involved in this outbreak for their cooperation with the collection of data for this study, the staff of the Center for Disease Control and Prevention and superior departments for guidance.
CHEN Dong Wan analyzed the data and drafted the manuscript. HE Chao, LV Jin Chang, LIU Xiu Feng, GAO Peng, and ZHEN Guo Xin collected the data. JING Hong Bo and LI Ying tested the specimens. All the authors read and approved the final manuscript.
Campylobacter Outbreak Associated with Duck Blood Curd in 2019 in Shunyi District, Beijing, China
doi: 10.3967/bes2021.067
- Received Date: 2020-08-07
- Accepted Date: 2021-01-21
| Citation: | CHEN Dong Wan, HE Chao, LYU Jin Chang, LIU Xiu Feng, GAO Peng, ZHEN Guo Xin, LI Ying, JING Hong Bo. Campylobacter Outbreak Associated with Duck Blood Curd in 2019 in Shunyi District, Beijing, China[J]. Biomedical and Environmental Sciences, 2021, 34(6): 489-492. doi: 10.3967/bes2021.067 |






 Quick Links
Quick Links
 DownLoad:
DownLoad: