-
Hepatitis A virus (HAV) is transmitted via the fecal-oral route, causing not only self-limited infectious hepatitis, but also epidemics through close personal contact(s). HAV infection is prevalent worldwide, and it is estimated that HAV infections account for 1.4 million sporadic or epidemic cases per year worldwide [1]. Due to the globalization of trade and travel, middle-income countries play an important role in global HAV infection control because they are more likely to switch to becoming non-endemic countries with continued economic development [2]. Given this, more attention should be devoted to China, since it is a middle-income country with the largest population in the world.
The trends in the incidence of HAV infection among different age groups have been reported to have decreased from 2004 to 2013 in China [3]. However, sex differences in the incidence of HAV infection in China among different age groups and their time variations have seldom been reported. Given that identifying the significant time periods in which the incidence of age- and sex-specific hepatitis A may contribute to future hepatitis A prevention and control programs, relevant data were collected.
Hunan Province, which has an intermediate economic level in China, is in the south-central region of the country. The incidence rate of hepatitis A in this province is close to the national average [4]. We therefor estimated significant time trends in incidence rates of HAV infection according to age and sex in Hunan, from 2004–2020, to reassess the hepatitis A profile for ongoing policymaking and to clarify the long-term impact of the implemented measures in the management of HAV infection in the nation.
We obtained the data from the web-based China Information System for Disease Control and Prevention (CISDCP). The HAV infection cases were diagnosed according to the diagnostic criteria GB 17010-1997 (before 2008) and WS 298-2008 (after 2008), which were issued by the National Health Commission. CISDCP is a routine reporting surveillance system established in 2003 for selected infectious diseases, whose morbidity, mortality, and population data for all provinces in China according to year, age, sex, and place of residence are recorded. Data extraction, cleaning, sorting, and calculations were performed using spreadsheet software (Excel, Microsoft Corporation, Redmond, WA, USA) and statistical analyses were performed using SPSS version 24.0 (IBM Corporation, Armonk, NY, USA). Ethics approval was not required given the lack of interaction or intervention with human participants in this study.
Incidence is expressed as the number of reported cases per 100,000 individuals. The age-adjusted incidence rates of HAV infection were calculated using the World Health Organization World Standard Population 2000. We compared the HAV incidence rate across 2004–2020 between groups by Kruskal-Wallis test and tested the difference in the median between groups by Dunn’s post-hoc test. The differences with P < 0.05 were considered statistically significant.
Joinpoint regression analysis was adopted to determine incidence trend(s) (stationary, upwards, or downwards) and to identify points at which linear trends changed significantly. At least two time points, including the beginning and ending points, were observed in the study period and a maximum of two joinpoints were searched for using the grid search algorithm and permutation test at an overall alpha level of 5%. This joinpoint regression analysis also enabled the calculation of the annual percentage change (APC) and average APC (AAPC) in the HAV infection rate over the entire study period. Additionally, corresponding 95% confidence intervals (CIs) were calculated. These analyses were performed using the Joinpoint Regression Program version 4.8.0.1 (Statistical Research and Applications Branch, National Cancer Institute, USA).
According to joinpoint regression, the HAV infection count was found to increase in individuals aged 0–14 years [APC, 25.21% (95% CI: 16.0 to 35.2); P < 0.05] and decrease in individuals aged 15–64 years [APC, –0.58% (95% CI: –2.6 to 1.5); P = 0.600] and ≥ 65 years [APC, –11.77% (95% CI: –17.9 to –5.2); P < 0.05] in the study period. Based on this result, individuals were classified into three age groups: 0–14, 15–64, and ≥ 65 years.
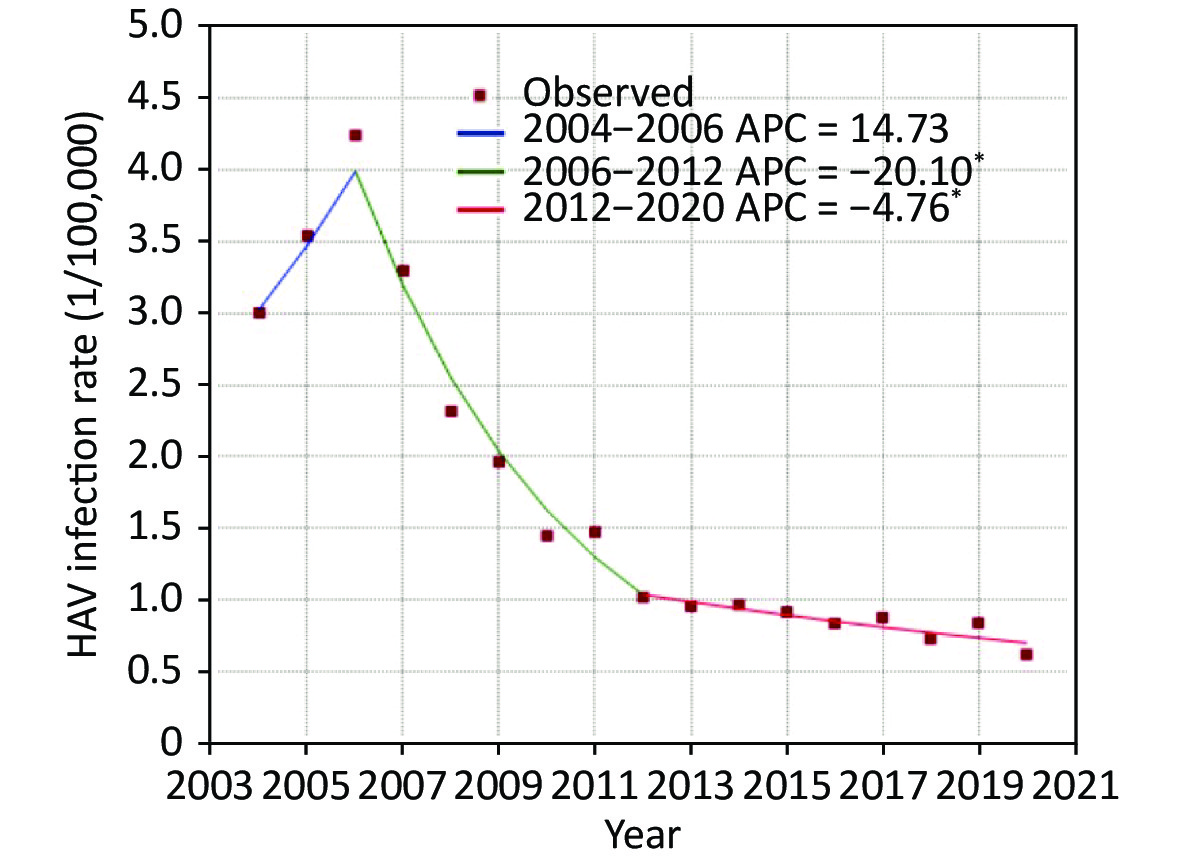
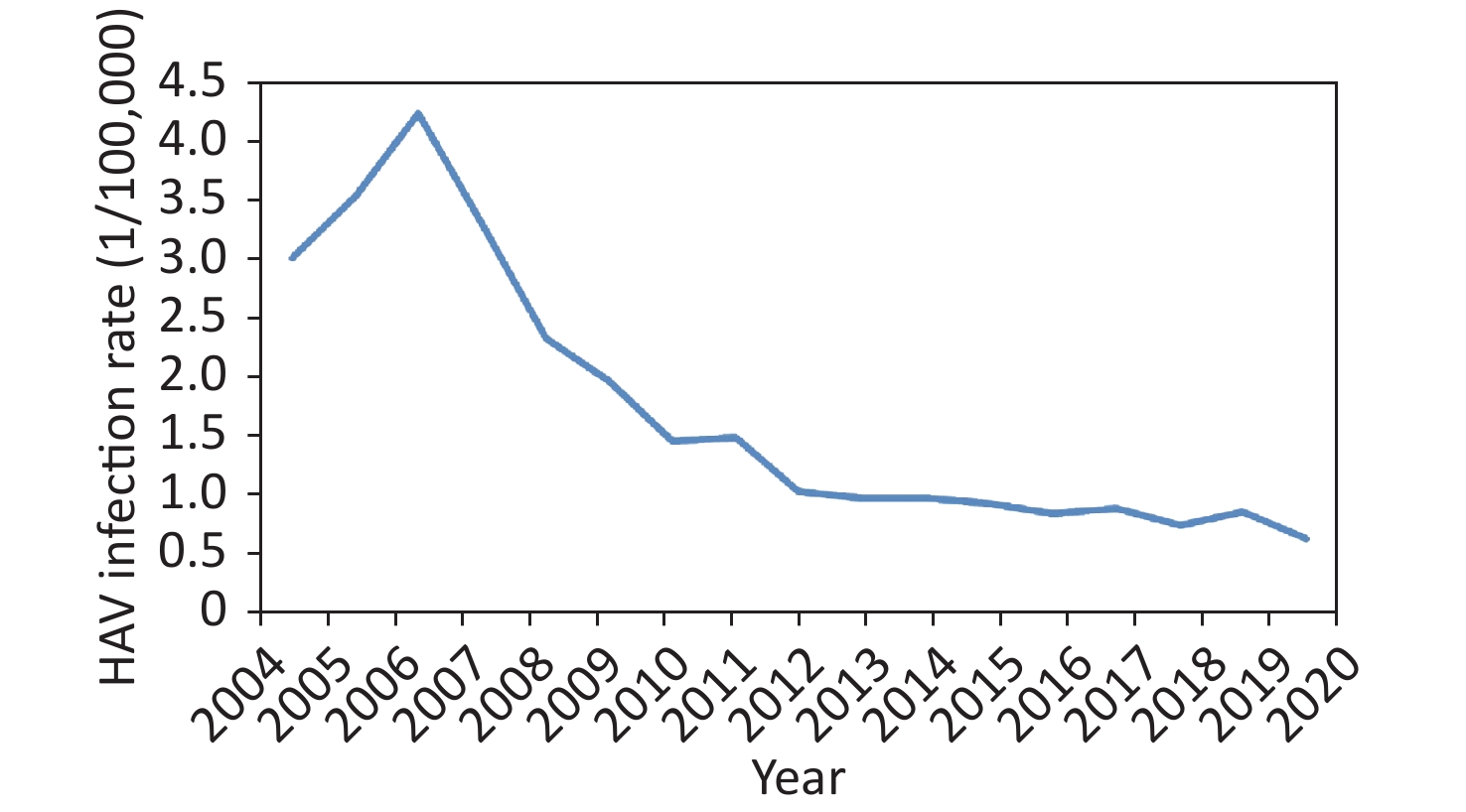
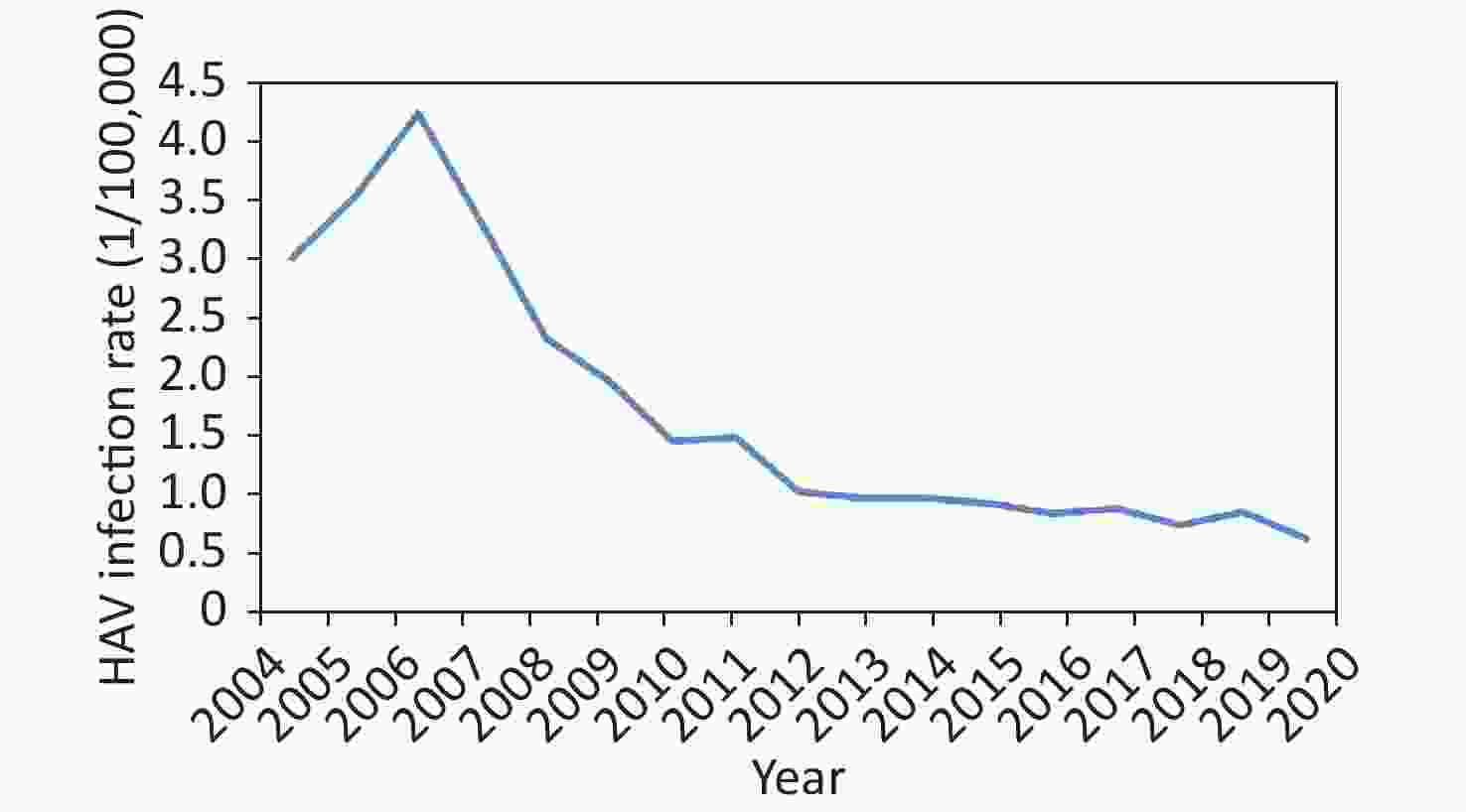
During the 17-year period from 2004 to 2020, a total of 18,893 cases (12,742 male, 6,151 female) of HAV infection were reported to CISDCP, corresponding to a mean annual incidence rate of 1.68/100,000. Six deaths were recorded during the study. The reported incidence of HAV infection increased from 2004 (3.00/100,000) to 2006 (4.24/100,000) and continued to decline until 2020 (0.62/100,000) (Supplementary Figure S1, available in www.besjournal.com).
The overall yearly incidence of HAV infections exhibited a decreasing trend from 2004 to 2020, and the AAPC for HAV infection from 2004 to 2020 was –8.70% (95% CI:
–12.5 to –4.8; P < 0.05). Specifically, the HAV infection rate first increased from 2004 to 2006 [APC, 14.73% (95% CI: –15.3 to 55.5); P = 0.300], and then decreased significantly from 2006 to 2012 [APC, 20.10% (95% CI: –25.4 to –14.5); P < 0.05], after which a more modest change was observed from 2012 to 2020 [APC, –4.76% (95% CI: –7.9 to –1.5); P < 0.05] (Supplementary Figure S2, available in www.besjournal.com). 
Figure S2. Annual percentage change in the rate of hepatitis A virus infection in Hunan, China, 2004–2020.
Improved socio-economic and living conditions may have contributed to the first drop in the incidence of hepatitis A after 2006. Wen et al. reported that, in Hunan Province, improvement in latrine sanitation in rural areas helped to reduce pollution caused by excrement in soil, water, and the surrounding environment and purified the rural environment. The incidence of intestinal infectious diseases in these rural areas was reduced by 42.62% [5]. Furthermore, elevated sanitation awareness and standards can also help decrease the number of HAV outbreaks. Studies have shown that HAV outbreaks are typically caused by water pollution and inadequate sewage treatment in developing and developed countries, and contaminated food and water in higher-income countries [1]. A previous study from Hunan reported that outbreak-associated HAV infections waned after 2006 when the case load dropped from 13,330 in 2006 to 7,815 in 2007; the main factors causing HAV outbreaks between 2005 and 2008 were water contamination and person-to-person contact [6].
Moreover, after 2003, when the severe acute respiratory syndrome (i.e., SARS) epidemic broke out in China, the government established a sound disease prevention and control system and the world’s largest reporting system for infectious disease with increased financial support from national and local governments [7]. During this period, China’s economy rapidly developed, health-related facilities were reinforced, clean and safe drinking water was generally provided, and the treatment rate of garbage and excrement gradually increased, promoting an epidemiological transition. The epidemiological transition is known as the transition of endemicity patterns, a transition from a high-endemicity pattern to a low-endemicity pattern, for example, because of socioeconomic development, improved hygiene, etc. Epidemiological transition may account for most of the first drop in HAV infections.
In addition, the incidence of HAV infection has consistently decreased with the introduction of the HAV vaccine. However, the 2012 joinpoint marked a new trend (2012 to 2020) that differed significantly from 2006 to 2012. This may be because before the Expanded Program on Immunization (EPI) in May 2008, the HAV vaccine was first introduced into the private market and was only available to children whose parents were willing to pay out-of-pocket. After 2008, when the HAV vaccine was included in the EPI, it enabled access to all newborns free of charge. The HAV vaccine initially prioritized the needs of Western countries and was finally expanded to nationwide use in China by 2010. Research has shown that hepatitis A vaccine coverage was > 90% among children born between 2008 and 2012 in China [8]. Thus, the HAV vaccine could account for the second drop in infection rates in 2012, after which a more moderate descending line was observed with < 1 case per 100,000 individuals. The HAV vaccine is beneficial for decreasing HAV infection rates and its effectiveness is evident with long-term immunization.
Overall, the observed descent between 2004 and 2020 was probably due to the combined effects of the aforementioned factors. The accumulation of these rich experiences could provide some lessons for other regions in eliminating HAV and other infectious diseases. For example, in South Asia, the age-adjusted rate of HAV infection was similar to that in East Asia in 1990 but higher than that in East Asia in 2019 [9], especially during the coronavirus disease 2019 pandemic, which may trigger renewed attention by governments to promote a sound disease surveillance system.
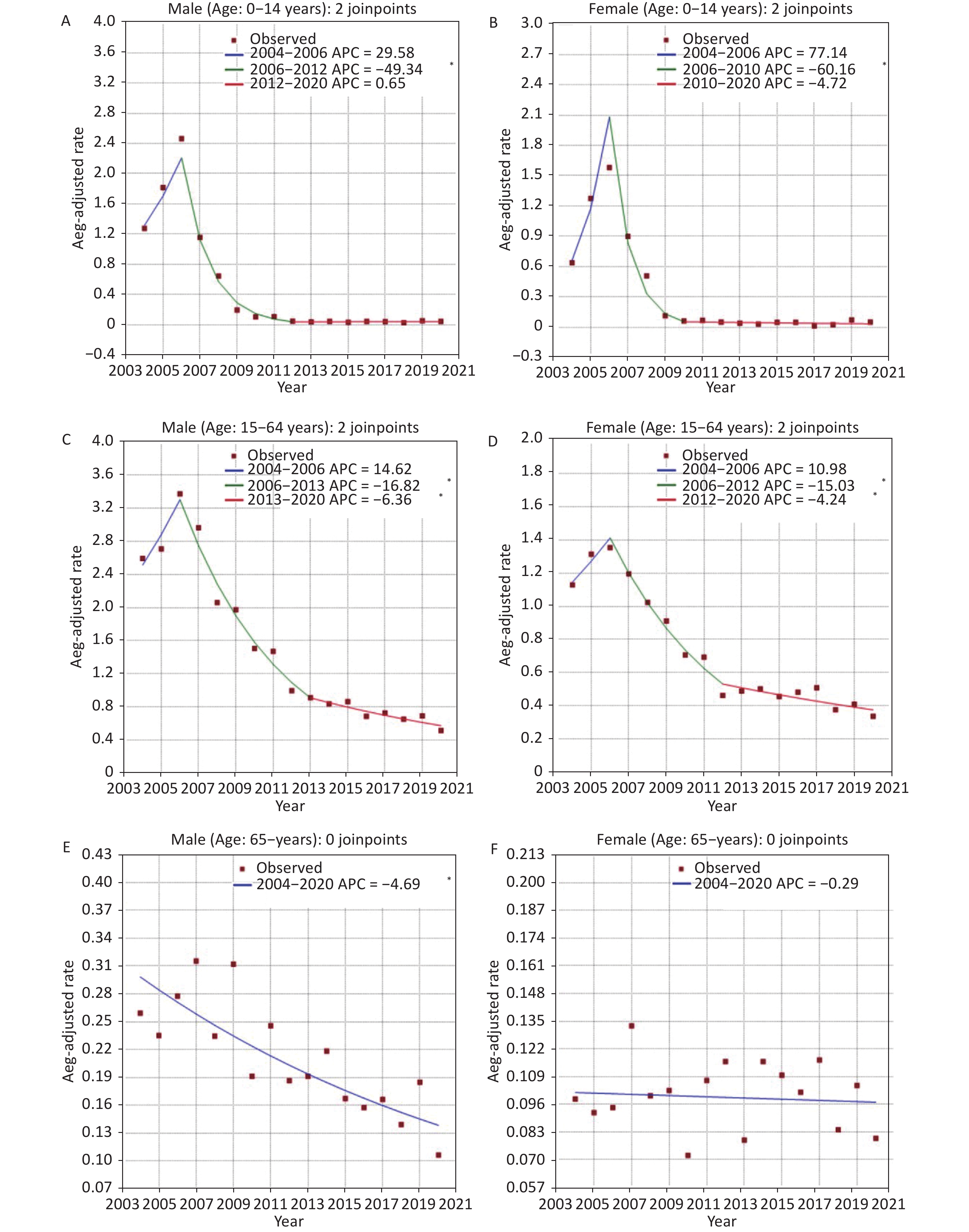
The joinpoint analysis performed for the two sexes revealed that males and females shared two joinpoints: at 2006 and 2012; and 2006 and 2010, respectively. The AAPC was –9.5% (95% CI: –13.6 to –5.3; P < 0.05) among males and –7.4% (95% CI: –12.4 to –2.1; P < 0.05) among females. Moreover, a significant difference was found between the sexes, indicating that the HAV infection rate in males was higher than that in females during the study period. More specifically, sex differences in HAV infection rates were observed in individuals aged 15–64 and ≥ 65 years. Furthermore, according to the Kruskal–Wallis test, incidence in individuals aged 0–14 years was found to have a significant difference comparing to those > 64 years of age (P < 0.05) (Table 1). Joinpoint analysis was also performed on males and females in the three age groups. Using this model, three-segmented trends were identified in individuals between 0–14 and 15–64 years of age in both sexes (Figure 1, Table 2).
Variable Variable abbreviations HAV infection, n HAV infection rate (1/100,000) H P value Post hoc test Gender 229.00 0.003** Male 0 12,742 3.74 Female 1 6,151 1.92 0–14 years 149.00 0.892 Male 0 1,932 2.98 Female 1 1,147 2.05 15–64 years 229.00 0.003** Male 0 9,440 3.87 Female 1 4,301 1.86 ≥ 65 years 283.00 < 0.001** Male 0 1,370 4.28 Female 1 703 2.13 Age 7.19 0.027* 0–14 years Y1 3,079 2.55 Y1–Y3 (P = 0.026*) 15–64 years Y2 13,741 2.89 Y1–Y2 (P = 0.233) ≥ 65 years Y3 2,073 3.18 Y2–Y3 (P = 1.000) Age (Male) 8.24 0.016* 0–14 years Y1 1,932 2.98 Y1–Y3 (P = 0.015*) 15–64 years Y2 9,440 3.87 Y1–Y2 (P = 0.175) ≥ 65 years Y3 1,370 4.28 Y2–Y3 (P = 1.000) Age (Female) 6.64 0.036* 0–14 years Y1 1,147 2.05 Y1–Y3 (P = 0.033*) 15–64 years Y2 4,301 1.86 Y1–Y2 (P = 0.297) ≥ 65 years Y3 703 2.13 Y2–Y3 (P = 1.000) Note. IQR: Inter Quartile Range; Post hoc test for groups: Dunn–Bonferroni pairwise comparison followed by Kruskal–Wallis; *P < 0.05; **P < 0.01. Table 1. Comparison of hepatitis A virus infection rate in Hunan, China, according to sex and age, 2004–2020

Figure 1. Joinpoint regression analysis of the age-adjusted rate of hepatitis A virus infection in Hunan, China, according to sex and age, 2004–2020.
Age group
(years)Period 1 Period 2 Period 3 AAPC (95% CI) Years APC 95% CI Years APC 95% CI Years APC 95% CI AAPC 95% CI All population 2004–2006 14.7 (–15.3, 55.5) 2006–2012 –20.1* (–25.4, –14.5) 2012–2020 –4.8* (–7.9, –1.5) –8.7* (–12.5, –4.8) 0–14 Male 2004–2006 29.5 (–47.2, 217.9) 2006–2012 –49.3* (–58.5, –38.1) 2012–2020 0.6 (–8.7, 11.0) –19.7* (–29.1, –9.1) Female 2004–2006 77.14 (–66.7, 841.0) 2006–2010 –60.2* (–82.7, –8.2) 2010–2020 –4.7 (–16.3, 8.5) –17.2 (–36.5, 7.9) Total 2004–2006 33.7 (–55.1, 298.3) 2006–2012 –48.5* (–59.6, –34.2) 2012, 2020 2.3 (–9.2, 15.3) –18.2* (–29.7, –4.8) 15–65 Male 2004–2006 14.6 (–15.6, 55.6) 2006–2013 –16.8* (–21.0, –12.4) 2013–2020 –6.4* (–10.1, –2.5) –8.8* (–12.5, –5.0) Female 2004–2006 11.0 (–15.8, 46.3) 2006–2012 –15.0* (–20.1, –9.6) 2012–2020 –4.2* (–7.1, 1.3) –6.7* (–10.2, –3.1) Total 2004–2006 14.3 (–10.3, 45.7) 2006–2013 –17.1* (–21.4, –12.5) 2013–2020 –6.3* (–8.7, –3.8) –8.2* (–11.3, –5.1) 65– Male 2004–2020 –4.7* (–6.3, –3.0) –4.7* (–6.3, –3.0) Female 2004–2020 –0.3 (–2.0, 1.5) –0.3 (–2.0, 1.5) Total 2004–2020 –3.2* (–4.7, –1.7) –3.2* (–4.7, –1.7) Note. APC: annual percentage change; AAPC: average annual percentage; CI: confidence interval; *P < 0.05; Periods 1, 2 and 3 are time intervals determined by joinpoint analysis. Table 2. Annual percentage change and average annual percentage change in age–adjusted rate of hepatitis A infection in Hunan, China, according to sex and age, 2004–2020
From 2004 to 2020, the incidence of HAV infection decreased in the three age groups, and the reduction in individuals aged 0–14 was more striking. In addition, we found that similar incidence change curves could be detected in both sexes that demonstrated an initial rising trend and subsequent decline in individuals aged 0–14 and 15–64 years. For the older age group (≥ 65 years), a significant and continuously declining trend in males and a stable trend in females were identified. Although the EPI only targeted the population born after 2008, a decline was observed in all age groups including the male group aged ≥ 65 years. This was probably due to better socioeconomic development, social hygiene awareness, and sanitation situations (improved sewage treatment and water quality) and could be further evidence of gain in herd immunity by routine HAV immunization programs.
In general, the incidence of HAV infection was found a significant difference between the older adults (≥ 65 years of age) and the young (0–14 years) in both sexes. Some possible supporting points were identified. First, the observed difference was mostly a result of EPI implementation, which greatly reduced the rates of HAV infection among individuals aged 0–14 years. Moreover, the fact that older adults with a high rate of hepatitis A were not included in the target population of the EPI until now, may have increased the difference between the two groups. In addition, the infection detection rate is one of the reasons. Because most acute HAV infections are self-limiting and the clinical symptoms are determined primarily by patient age, they are usually silent or subclinical in early childhood and are more likely to cause jaundice and abdominal pain in late childhood, adolescence, and adulthood [2, 10]. The case detection rate in the older adults was higher than that in the young, leading to a higher incidence of HAV infection among the older adults. Additionally, we found that individuals aged 0–14 years reached the third period earlier (2012) than those aged 15–65 years (2013), which was probably caused by the nationwide routine vaccination program.
In our study, the HAV infection rate among males was found to be higher than that among females. However, there is no published evidence on the possible biological mechanism of higher susceptibility to HAV infection among males. This difference may be caused by sex disparities in the access to health resources. It is a common belief that females have poorer access to health resources than males due to their comparable situation in education and paid labor. Moreover, males with outgoing personalities who mostly prefer to go out for drinking, meals or travel, usually have poorer hygiene habits than women. For example, they drink raw water and skip handwashing before meals and after defecation, increasing the possibility of HAV infection. In addition, travelers and men who have sex with men (MSM) are considered risky for a higher rate of HAV infection[1]. These could also explain why males in our study reached the third joinpoint later than females in the age groups 0–14 and 15–64 years. More specifically, there was a sex difference in all age groups except those aged 0–14 years as a result of universal vaccination, which has narrowed the sex differences in the incidence of HAV infection.
Underreporting was a major limitation of our research; data collection in our study was based on a passive surveillance system that can be affected by the accuracy of diagnosis and reporting. However, this web-based “reporting of incidence” still serves as a good estimation of the disease burden of hepatitis A. In addition, certain characteristics (trips data, transmission ways, etc.) were not provided in this surveillance system; therefore, deeper analysis for underlying reasons of the incidence curve of hepatitis A could not be ascertained. Finally, our data were confined to the Hunan area and nationwide data should be collected to accurately describe trends in hepatitis A conditions across China.
In conclusion, this study showed a higher HAV infection incidence in males and old age (≥ 65 years), and a more significant improvement between the study period in individuals aged 0–14 years. Moreover, this study examined different sex- and age-dependent trends in HAV infection from 2004 to 2020 in Hunan, China. The incidence trends among demographic groups may not only inform and guide the management of HAV infection in this region but also advise the control of similar viral hepatitis epidemics in other areas of the country.
HTML
 22235Supplementary Materials.pdf
22235Supplementary Materials.pdf
|

|






 Quick Links
Quick Links
 DownLoad:
DownLoad: