-
Clostridium difficile infection (CDI) is a major global public health concern, accounting for 15–25% of antibiotic-associated diarrhea, 50%–75% of antibiotic-associated colitis, and nearly all cases of pseudomembranous colitis. Over the past decade, CDI outbreaks have become increasingly prevalent in North America and Europe, with rising incidence and mortality rates. In 2019, the Centers for Disease Control and Prevention (CDC) in the United States classified CDI as a “critical” public health threat in their report on antibiotic resistance threats[1]. CDI incidence varies widely across countries, healthcare settings, and age groups, with cumulative incidence rates ranging from 1.12 to 631.80 per 100,000 people annually[2]. As the epidemiology of CDI continues to evolve and our understanding of the disease advances, reassessing its burden remains essential. The Global Burden of Disease, Injury, and Risk Factors Study (GBD2021) database offers new insights into this issue.
Data for this study were obtained from the GBD2021 database (http://ghdx.healthdata.org/gbd-results-tool). First, we describe overall trends and regional variations. Piecewise regression was performed using the Joinpoint Regression Program (version 5.2.0.0) to calculate annual percentage changes (APCs) and average annual percentage changes (AAPCs), which reflect temporal trends in mortality burden. Next, using the sociodemographic index (SDI) as an indicator of overall social development, we applied Pearson correlation analysis to assess the relationship between mortality burden and SDI, thereby exploring potential influencing factors. Finally, we used the age-period-cohort (APC) analysis tool (https://analysistools.cancer.gov/apc/) to examine the independent effects of age, period, and birth cohort on mortality burden. All data processing, statistical analyses, and visualizations were conducted in R (version 4.3).
Our results and discussion are as follows:
1. Overall Trends (1990–2021): The global number of deaths due to CDI increased from 3,047 cases (0.11% of all-cause mortality) in 1990 to 15,598 cases (1.37% of all-cause mortality) in 2021. The CDI-related mortality rate was 0.06 per 100,000 in 1990 and 0.20 per 100,000 in 2021, with an AAPC of 2.3%, indicating an increasing trend (Supplementary Table S1). No significant difference was observed in the age-standardized mortality rate between male and female patients (t = 1.009, P = 0.317) (Supplementary Table S2).
2. Regional Trends: CDI-related mortality exhibited substantial geographic disparities across the 21 GBD regions and 204 countries or territories analyzed. In 2021, the highest mortality rates among the 21 GBD regions were recorded in high-income North America (1.16 per 100,000), Central Europe (0.36 per 100,000), and Western Europe (0.33 per 100,000). Pearson correlation analysis indicated a positive correlation between mortality rate and SDI (R = 0.543, P = 0.011). The greatest increases in AAPC were observed in high-income North America (6.0%), tropical Latin America (2.3%), and Central Europe (2.1%) (Supplementary Table S2). However, no statistically significant correlation was found between AAPC and SDI at the regional level (R = 0.397, P = 0.075). At the national level, the highest CDI-related mortality rates in 2021 were reported in the United States (1.22 per 100,000), Norway (0.92 per 100,000), and Greenland (0.85 per 100,000). Pearson correlation analysis demonstrated a significant positive correlation between mortality rate and SDI (R = 0.466, P < 0.001). The highest AAPC values for mortality rate were observed in the United States (6.3%), Sweden (5.0%), and Poland (4.3%). AAPC across the 204 countries and territories was positively correlated with SDI (R = 0.232, P < 0.001) (Supplementary Table S3).
Both mortality rate and AAPC exhibited a positive correlation with SDI, although the association was not strong. Possible explanations include: (1) limited epidemiological data on CDI burden in Latin America, South America, Africa, and Asia due to inadequate surveillance and diagnostic resources; and (2) the predominance of highly virulent strains such as ribotype 027 in high-SDI regions (e.g., Europe, North America, and Australia), whereas less virulent strains such as ribotypes 017, 001, and 014 are more prevalent in Asia, Africa, and South America[3].
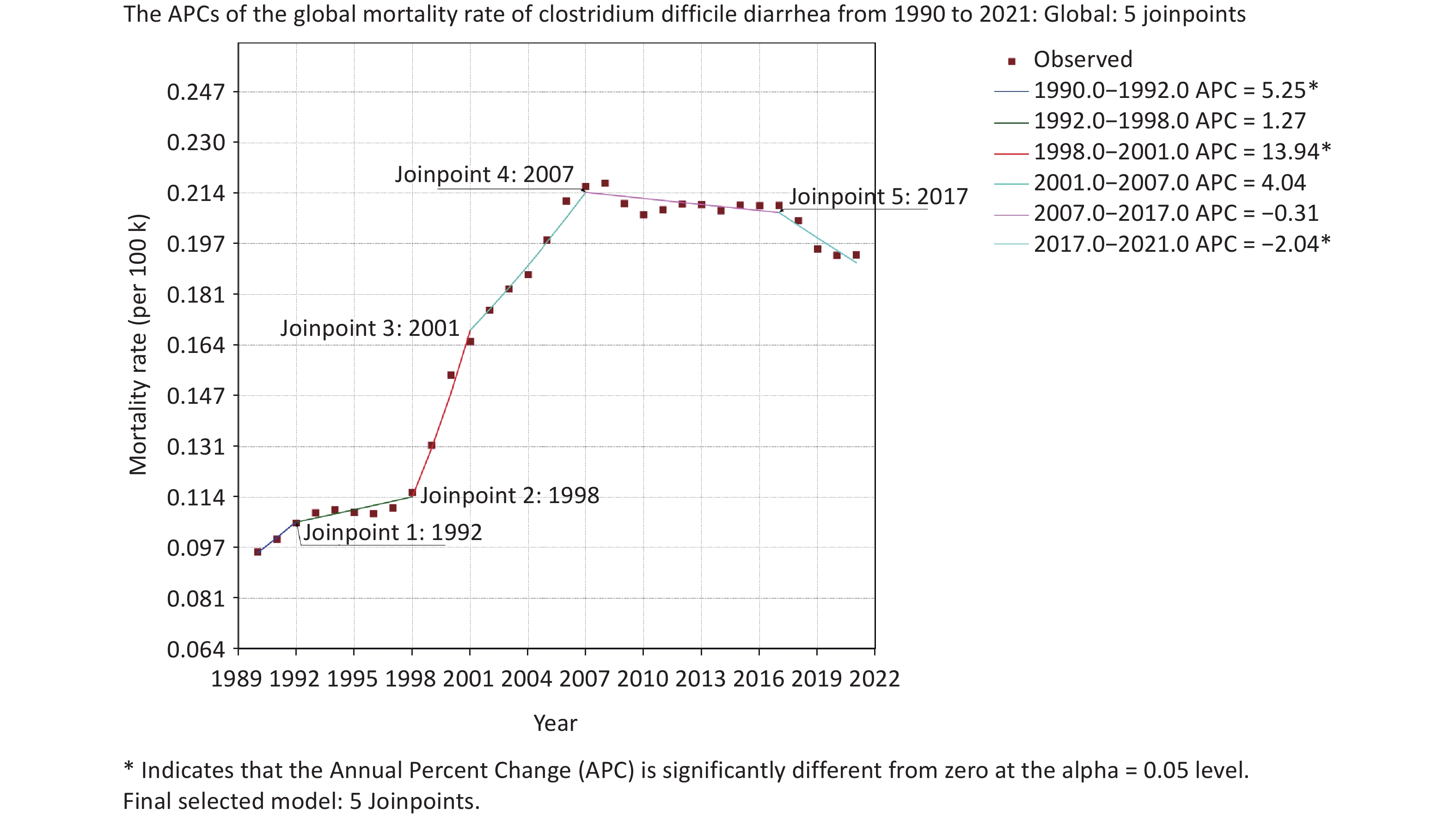
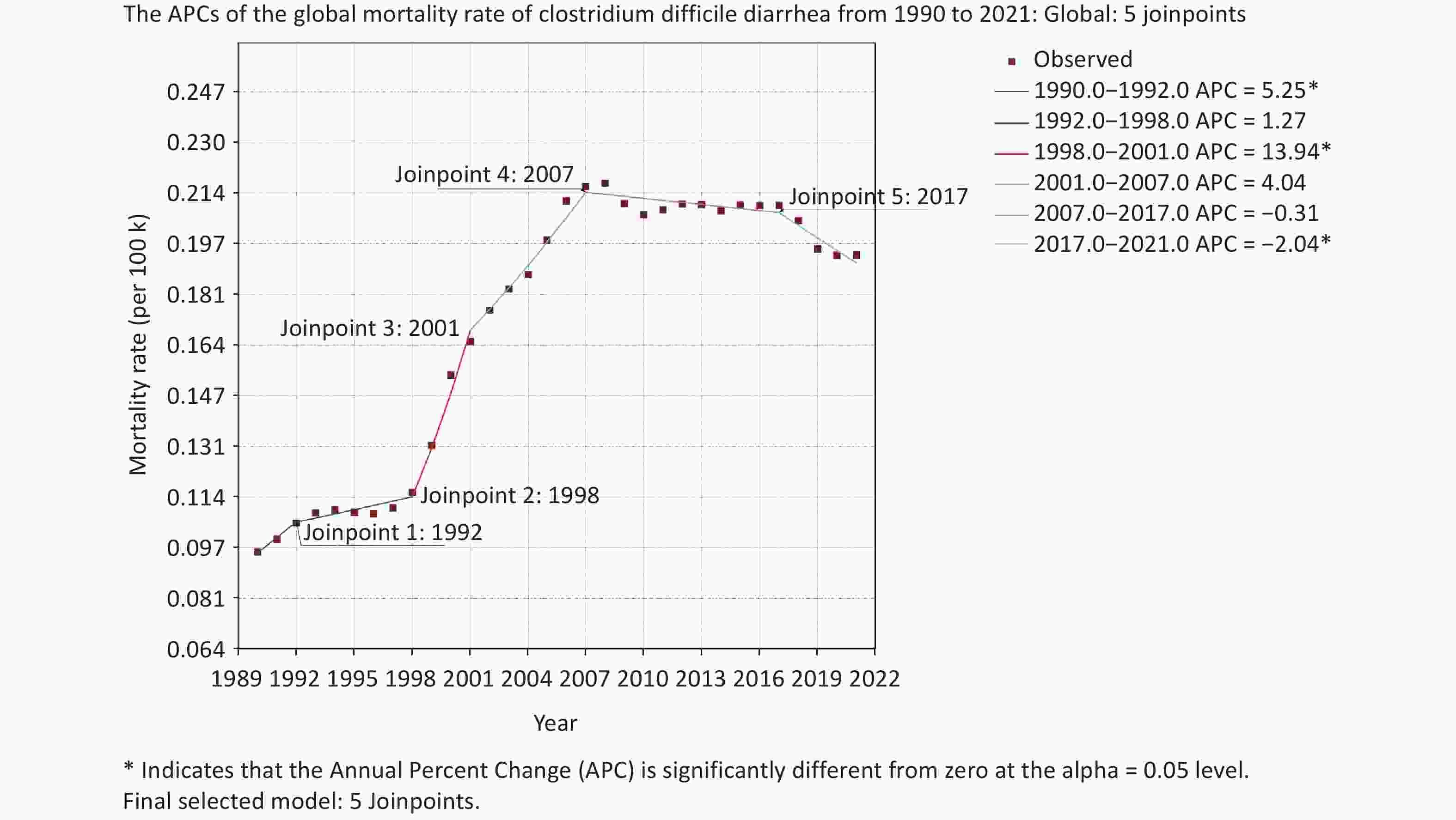
3. APC Trends: A joinpoint regression model was used to analyze temporal trends in global CDI-related mortality from 1990 to 2021. Five significant inflection points were identified: 1992, 1998, 2001, 2007, and 2017. The APC values for each period were as follows: 1990–1992: 5.25% (P < 0.05); 1992–1998: 1.27% (P > 0.05); 1998–2001: 13.94% (P < 0.05); 2001–2007: 4.04% (P > 0.05); 2007–2017: −0.31% (P > 0.05); 2017–2021: −2.04% (P < 0.05). The overall AAPC was 2.3% (P < 0.05). These results indicate a general upward trend in CDI-related mortality from 1990 to 2007, with a particularly sharp increase from 1998 to 2001, followed by a declining trend after 2007 (Figure 1, Supplementary Tables S4 and S5).
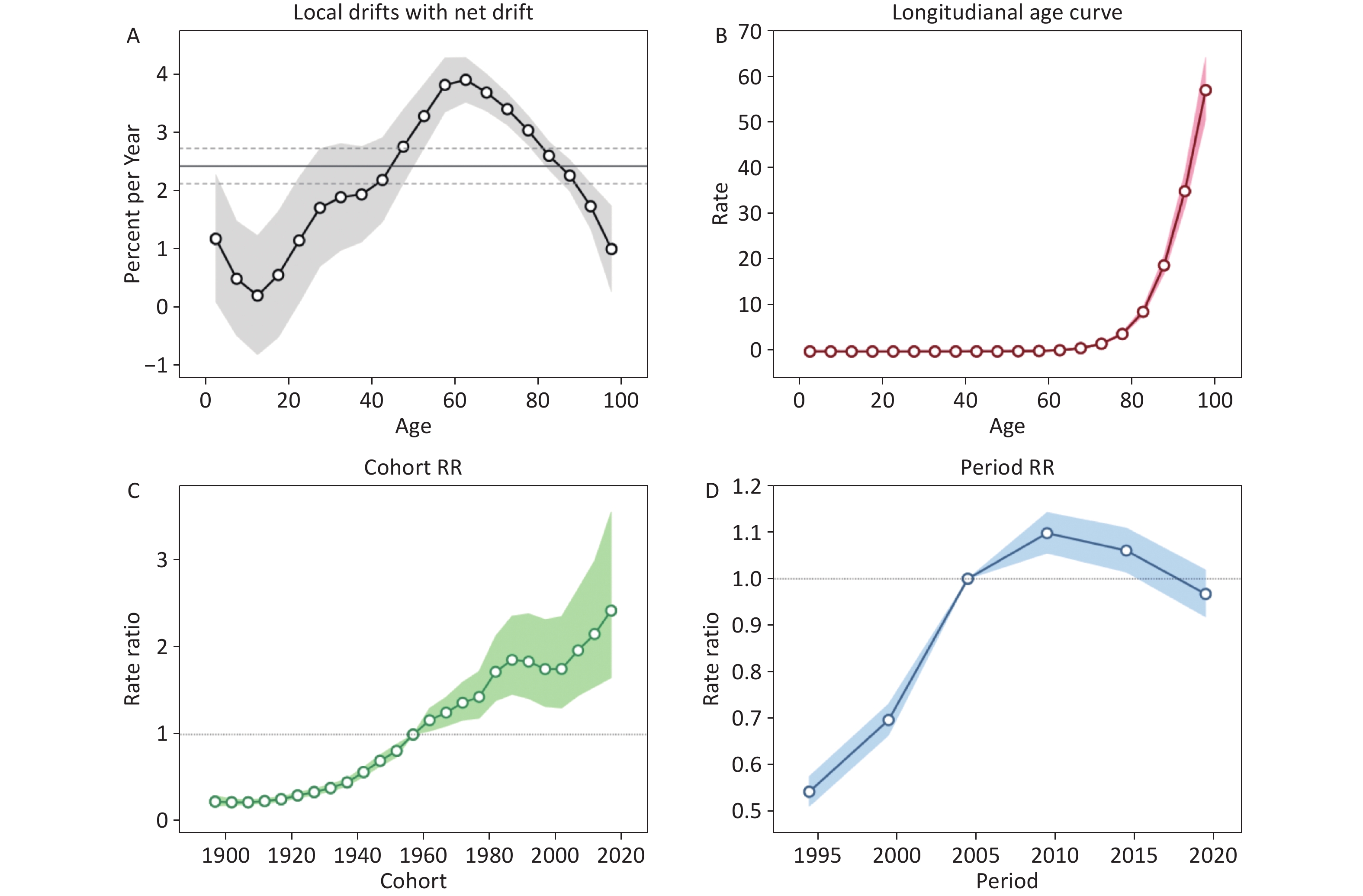
4. Age-Period-Cohort Analysis: The age-period-cohort model (Supplementary Table S6) showed that net drift, local drift, period deviations, cohort deviations, age deviations, period rate ratios (RR), and cohort RR were all statistically significant (P < 0.001). These findings suggest that CDI-related mortality was independently influenced by age, period, and cohort factors.
Net Drift: The global net drift in CDI diarrheal mortality from 1992 to 2021 was 2.44%, closely aligning with the Joinpoint model result of 2.3%. As both values exceeded 1%, they indicate a significant upward trend in mortality. Several factors may contribute to this increase: 1) The emergence of highly virulent strains, particularly ribotype 027, in Europe and North America in the early 21st century has led to higher disease severity and mortality rates[4]. 2) CDI outbreaks in Europe and North America have spread globally due to population movement. 3) The increased prevalence of livestock-associated strains, such as ribotypes 014 and 078, has contributed to a rise in human CDI incidence and severity[5]. 4) Rising resistance of C. difficile to metronidazole and vancomycin[6]. 5) Increased recognition and detection of community-acquired CDI. While CDI has traditionally been regarded as a common hospital-acquired infection, studies indicate that community-acquired CDI (CA-CDI) now accounts for approximately 40% of all CDI cases[7].
Local drift: Local drift analysis revealed that local drift values were greater than zero across all age groups, indicating a general upward trend in mortality. Among these, the local drift values for the 5–9, 10–14, and 15–19-year age groups were below 1%, suggesting a relatively mild increase. In contrast, the 0–4 and ≥ 20-year age groups exhibited values exceeding 1%, indicating a more pronounced rise, peaking at 3.9% in the 60–64-year age group. Among individuals aged 45–84 years, local drift values exceeded the net drift, contributing significantly to the overall increase in mortality (Figure 2A).
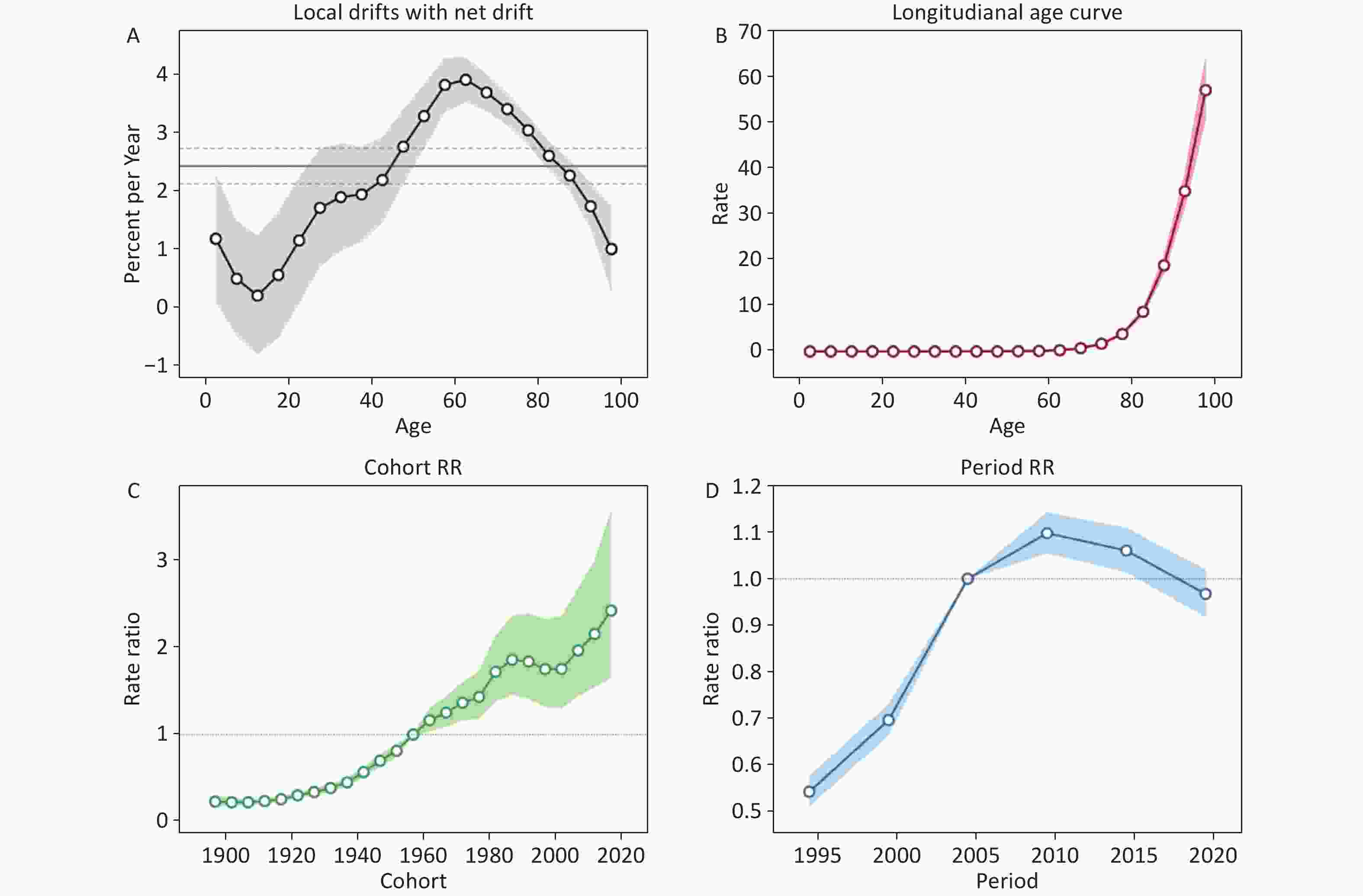
Figure 2. Age-Period-Cohort Analyses of CDI-Related Diarrhea Mortality. (A) Local drift with net drift. (B) Longitudinal age curve. (C) Cohort effect. (D) Period effect.
The effect of CDI-related diarrhea mortality was influenced by age. The longitudinal age curve showed that, after adjusting for period and cohort effects, mortality among the 0–4, 5–9, 10–14, and 15–19-year age groups exhibited slight decreases, declining from 0.0078 per 100,000 to a minimum of 0.0036 per 100,000. After the 20–24-year age group, mortality increased with age. Previous studies have shown that more than 80% of CDI-related diarrheal deaths occur in individuals over 65 years of age. Our study revealed a significant increase in mortality among older age groups, with rates rising from 1.69 per 100,000 in the 70–74-year age group to 56.87 per 100,000 in those aged 95 years and older (Figure 2B). In combination with the local drift results, we found that, from the perspective of mortality growth rate, local drift values for the 50–54 (3.3%), 55–59 (3.8%), 60–64 (3.9%), 65–69 (3.7%), 70–74 (3.4%), and 75–79 (3.0%) age groups all exceeded 3%. Among these, the 60–64-year age group exhibited the fastest growth rate. These findings suggest that while the majority of CDI-related deaths occurred in individuals over 80 years of age, the most rapid increase in mortality was observed in those aged 55–69 years. Therefore, enhanced surveillance and prevention efforts are necessary for these age groups.
After adjusting for age and period, a birth cohort effect on mortality was observed between 1992 and 2021. Using the 1957–1961 birth cohort (median group) as a reference (RR = 1.000), the mortality risk exhibited an upward trend from the 1897–1902 birth cohort to the 1992–1996 cohort. A slight decline was observed in the 1997–2006 cohort, followed by a marked increase in the 2007–2012 cohort, with the 2017–2021 birth cohort reaching a peak RR of 2.42 (95% CI: 1.65–3.54) (Figure 2C). This suggests a notably high risk ratio for cohorts born between 2007 and 2021. The increase may be attributed to the high susceptibility of children to CDI, who were previously considered to have high carrier rates but low pathogenicity[8]. However, the emergence of hypervirulent strains has led to increased mortality and a higher detection rate of CDI in children.
The period effect on CDI-related diarrhea mortality, after adjusting for age and cohort effects, showed a significant increase from 1992 to 2011. Using the median period of 2002–2006 as the reference (RR = 1.000), the period effect peaked between 2007 and 2011 (RR = 1.1, 95% CI: 1.06–1.14) before gradually declining (Figure 2D). The decline observed after 2012 is likely attributable to proactive measures implemented by various countries, including infection prevention programs, hand hygiene practices, contact precautions, disinfection protocols, and financial incentives or penalties aimed at improving CDI management[9]. Additionally, increased emphasis on CA-CDI, identification of recurrent CDI, and optimized testing protocols have improved diagnostic sensitivity and specificity[10]. Furthermore, the introduction of fidaxomicin and the monoclonal antibody bezlotoxumab for CDI treatment and prevention[6] has provided new options for reducing adverse effects and addressing antimicrobial resistance. Collectively, these measures have contributed to a reduction in CDI-related mortality.
In summary, the global burden of CDI-related diarrhea deaths has increased over the past three decades, although a slight decline has been observed since 2007. Individuals aged 80 years and older represent the largest proportion of CDI-related deaths, with mortality rates rising exponentially with age. The most rapid increase in mortality was observed in individuals aged 55–69 years, and the highest RRs were recorded in birth cohorts from 2007 to 2021. Therefore, strengthening surveillance and prevention strategies for middle-aged and elderly populations, as well as children, is essential. Marked regional disparities persist, with CDI burden likely underestimated in underdeveloped regions due to limited awareness and diagnostic resources. To address these gaps, efforts should focus on education, surveillance, and new drug development, which hold promise for reducing the global burden of CDI.
Global Burden of Clostridium difficile Infection-Related Diarrhea Mortality from 1990 to 2021: A Study Based on the 2021 Global Burden of Disease Database
doi: 10.3967/bes2025.039
- Received Date: 2024-10-08
- Accepted Date: 2025-03-10
The authors declare no conflicts of interest.
| Citation: | Ying Li, Jie Li, Hesheng Chang, Yuehua Hu, Chengdong Xu. Global Burden of Clostridium difficile Infection-Related Diarrhea Mortality from 1990 to 2021: A Study Based on the 2021 Global Burden of Disease Database[J]. Biomedical and Environmental Sciences. doi: 10.3967/bes2025.039 |







 Quick Links
Quick Links
 DownLoad:
DownLoad: