-
Lumbar spondylolysis (LS) is a condition characterized by a defect or fracture in the pars interarticularis[1-3]. This defect can occur on one or both sides of the body. It is commonly believed to result from repetitive stress or trauma to the lumbar pars interarticularis, leading to fatigue fractures[4]. LS can lead to spinal instability, resulting in forward or backward slippage of the vertebra, known as Spondylolytic spondylolisthesis (SS)[5]. LS and SS are significant factors that contribute to lower back pain and symptoms related to lumbar nerve compression[2].
In the past, the diagnosis of LS relied mainly on plain X-ray films, but this often led to missed diagnoses owing to image overlap. Multidetector Computed Tomography (CT) can achieve multiplanar reconstruction and three-dimensional observation of the lumbar vertebral bone structure, effectively avoiding image overlap. It also provides a distinct advantage for distinguishing between SS and degenerative spondylolisthesis. Multidetector CT has shown significant advantages in the diagnosis of LS and SS[4,6].
LS has two peak incidence periods, occurring during childhood at ages 5-7 and during adolescence[7]. Its prevalence remains stable until adulthood[2]. LS is associated with genetic factors, leading to variations in prevalence among different ethnic groups[8]. Currently, there is a lack of data on the prevalence of LS and SS in mainland China. To address this issue, we aimed to diagnose LS and SS using lumbar spine CT images from community populations in mainland China. Thus, we determined the prevalence of LS in the mainland Chinese population and assessed the proportion of individuals with SS.
CT imaging not only serves as routine diagnostic imaging but also allows quantitative measurement of bone mineral density (BMD) and muscle parameters, thereby assessing musculoskeletal quality. Muscle cross-sectional area (CSA) measured by CT can represent muscle size, whereas CT attenuation values (Hounsfield units, HU) can indicate muscle density[9]. This study aimed to evaluate the prevalence of LS using CT imaging to quantitatively measure lumbar BMD, paraspinal muscle size, and density and further explore the musculoskeletal status of patients with LS and SS.
-
The cohort for this study was a subgroup of the China Action on Spine and Hip Status (CASH) study, a nationwide multi-center project. The main participants in this study were middle-aged and elderly individuals aged 40 and above from the community. It included 12 centers from one municipality directly under the central government and six provinces (two centers from Beijing, one from Liaoning, three from Sichuan, three from Jiangsu, one from Shanxi, one from Shaanxi, and one from Jiangxi). The study protocol and informed consent documents were reviewed and approved by the Institutional Review Board of Beijing Jishuitan Hospital (approval numbers 201210-01 and 201512-02). The inclusion and exclusion criteria for community volunteers have been described previously[10]. Details of data collection have been reported in previous studies conducted by our team[11]. The main baseline data included sex, age, height (H, m), weight (W, kg), waist circumference (WCF, cm), and hip circumference (HCF, cm), which were calculated using the following formulas for body mass index (BMI) and waist-hip ratio (WHR): BMI = W/H2, WHR = WCF/HCF.
-
A radiologist with over 6 years of experience in diagnosing musculoskeletal disease read axial and sagittal CT reconstructed images to diagnose LS and SS. SS was diagnosed when there was forward or backward slippage of the posterior margin of the vertebra relative to the adjacent lower vertebra in the mid-sagittal reconstructed images (Figure 1). The degree of slippage was classified into five grades using the Meyerding indexing method: Grade I (5%–25%), Grade II (26%–50%), Grade III (51%–75%), Grade IV (76%–100%), and Grade V (greater than 100%)[12].
-
Bone density measurements were performed using Mindways QCTPro Workstation (version 5.0; Mindways Software Inc., v5.0, Austin, TX, USA). Vertebrae L1 to L3 were routinely assessed for volumetric bone mineral density (vBMD), with the region of interest placed within the trabecular bone and excluding central venous structures and cortical bone of the vertebrae (Figure 2B). In cases where any of these three vertebrae exhibited fractures or other conditions that could potentially influence the results (such as severe endplate inflammation, degenerative changes, or internal fixation devices), adjacent normal vertebrae were selected for measurement. The average vBMD values of these three vertebrae were used to represent lumbar spine BMD.
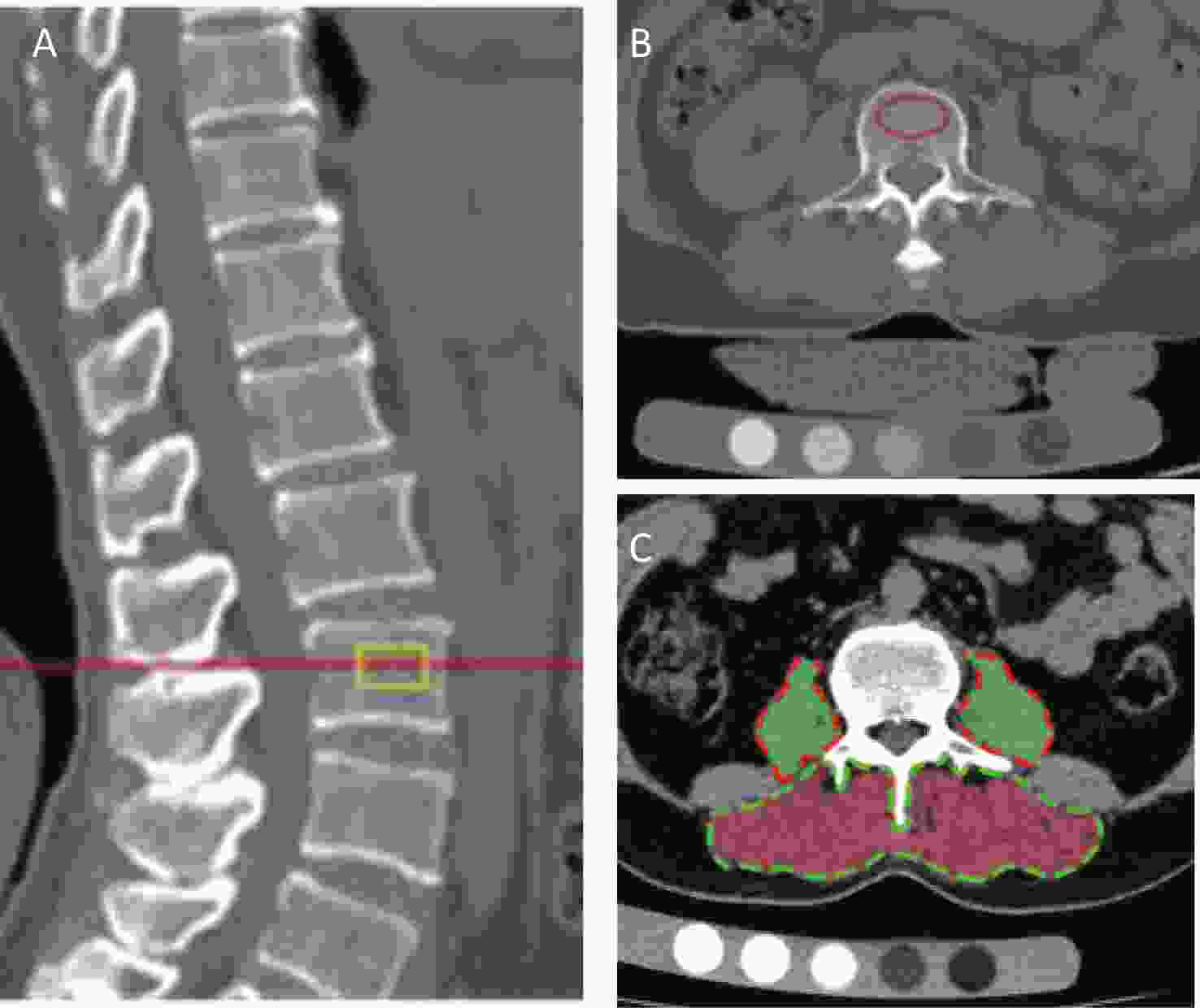
Figure 2. (A). Sagittal plane reconstructed CT image of the lumbar spine, centered at the L3 level. (B). Bone mineral density measurement: the red circle indicates the region of interest, avoiding cortical bone and the central venous structures of the vertebra. (C). Measurement of paraspinal muscle parameters: the green dashed lines outline the contours of the paraspinal extensor muscle group, with the inner red area representing muscle tissue of the paraspinal extensor muscles. The red dashed lines outline the contours of the bilateral psoas major muscles, with the inner green area representing muscle tissue of the bilateral psoas major muscles.
OsiriX software (Version 10.0.2; Pixmeo, Geneva, Switzerland) was used to measure the paraspinal muscle parameters. The measurement planes included the central planes of vertebrae L1, L3, and L5. Initially, sagittal reconstructed images from the CT scans were used to locate the central plane of each vertebra. Subsequently, on axial slices, measurements were taken of the cross-sectional area of the paraspinal extensor muscles (PEMS, cm²) comprising the multifidus and erector spinae, as well as their muscle density (PEMD, Hu). Measurements of the cross-sectional area of the psoas major muscle (PMMS, cm²) and muscle density (PMMD, HU) were also performed (Figure 2C). Tissues with CT attenuation values ranging from -30 to 150 HU were defined as muscle tissue[13].
-
Continuous variables were presented as mean ± standard deviation (SD). Categorical variables were presented as frequencies (n) and percentages (%). The comparison of frequencies was conducted using the χ2 test. The Student’s t-test was used to compare continuous variables between the two groups. One-way analysis of variance was used to compare continuous variables among multiple groups, and one-way analysis of variance (ANOVA) was used. If the variances were equal, Bonferroni post hoc tests were performed. If the variances were unequal, Tamhane’s T2 test was used. Covariance analysis was used to eliminate the effects of confounding factors. Statistical analysis was performed using IBM SPSS version 26.0, with a significance level (α) set at 0.05 (two-tailed), where p < 0.05 indicates statistical significance.
-
Out of a total of 3,457 sets of CT images, 140 sets were excluded for various reasons: ① six sets had discrepancies in sex and age compared to the database. ② 76 sets were detected for lumbar vertebral pedicle screws or poor image quality that affected the observation. ③ 48 sets did not contain complete L5 vertebrae. ④ Ten sets had severe spinal deformities that significantly affected the diagnosis. Ultimately, the analysis included 3317 individuals, with an age range of 40-82 years and a mean age of 62.00 ± 9.06 years. Among them, there were 1,214 males with a mean age of 62.91 ± 9.18 years and 2103 females with a mean age of 61.47 ± 8.95 years.
-
Among the 3,317 community-dwelling elderly individuals, there were 117 cases of LS, with a prevalence rate of 3.53%. Among the 1,214 males, 63 had LS, with a prevalence rate of 5.18%, whereas among the 2103 females, 54 had LS, with a prevalence rate of 2.57%. There was a statistically significant difference in the prevalence of LS between sexes (P < 0.001). The cohort was divided into four different age bands based on the age nodes of 50, 60, and 70 years. The prevalence rates in each age group were 3.07%, 4.09%, 3.52%, and 3.28%, respectively (Table 1). However, there was no statistically significant difference in the prevalence rates among the age groups (P = 0.860).
Age Total Non-LS LS Rate (%) All age 3317 3200 117 3.53 < 50 358 347 11 3.07 50-59 865 831 34 4.09 60-69 1364 1316 48 3.52 ≥ 70 730 706 24 3.28 Note. Non-LS, group without Lumbar spondylolysis. LS, group with Lumbar spondylolysis. Table 1. Prevalence rates of different age bands
The average age of the LS group was 61.71 ± 8.85 years, while it was 62.01 ± 9.07 years in the non-LS group. The difference in average age between the two groups was not statistically significant. The proportion of males in the LS group (53.85%) was higher than that in the non-LS group (35.97%) and the overall population (36.60%), and the proportion of females (46.15%) in the LS group was lower than that in the non-SL group (64.03%) and the overall population (63.40%). There was a statistically significant difference in the sex composition ratios among the groups (P < 0.001) (Table 2).
Variables Total (n = 3,317) Non-LS (n = 3,200) LS (n = 117) P Age, years 62.00 ± 9.06 62.01 ± 9.07 61.71 ± 8.85 0.727 Gender, n(%) < 0.001 Male 1214(36.60) 1151(35.97) 63(53.85) Female 2103(63.40) 2049(64.03) 54(46.15) Note. Non-LS, no lumbar spondylolysis; LS, lumbar spondylolysis Table 2. Gender and age information of cohort and groups divided by LS or not
-
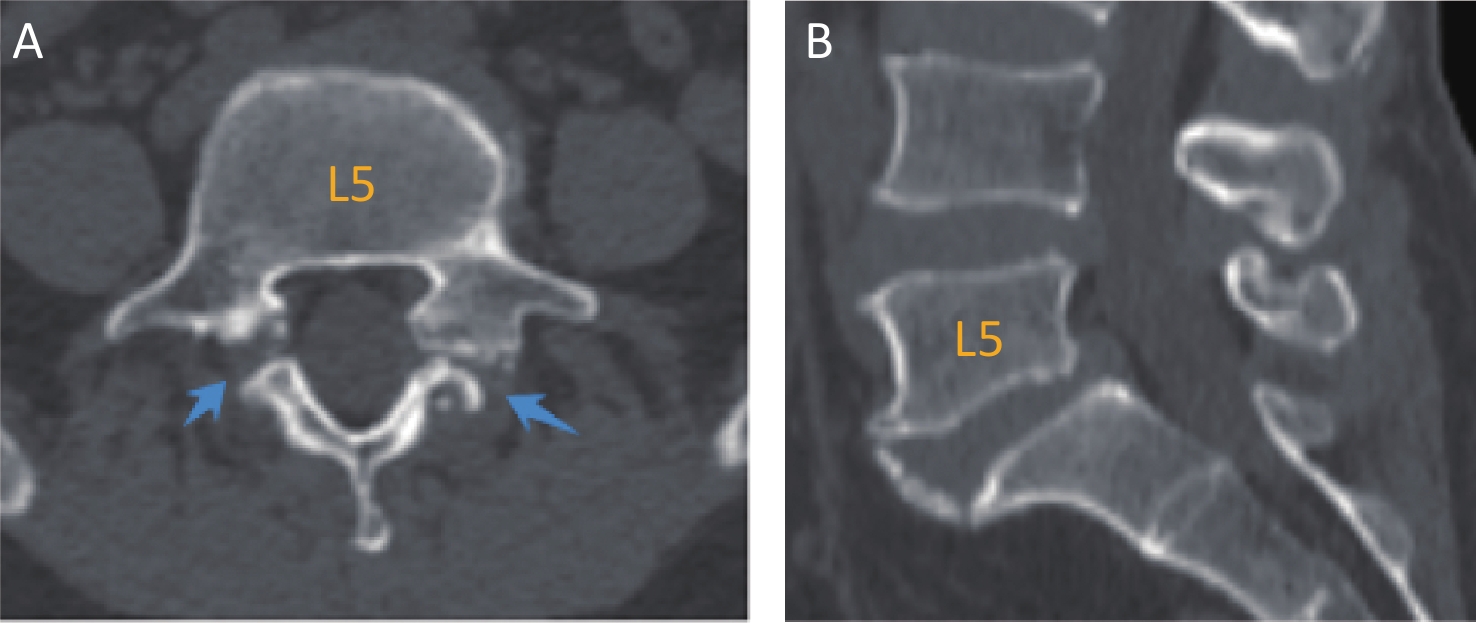
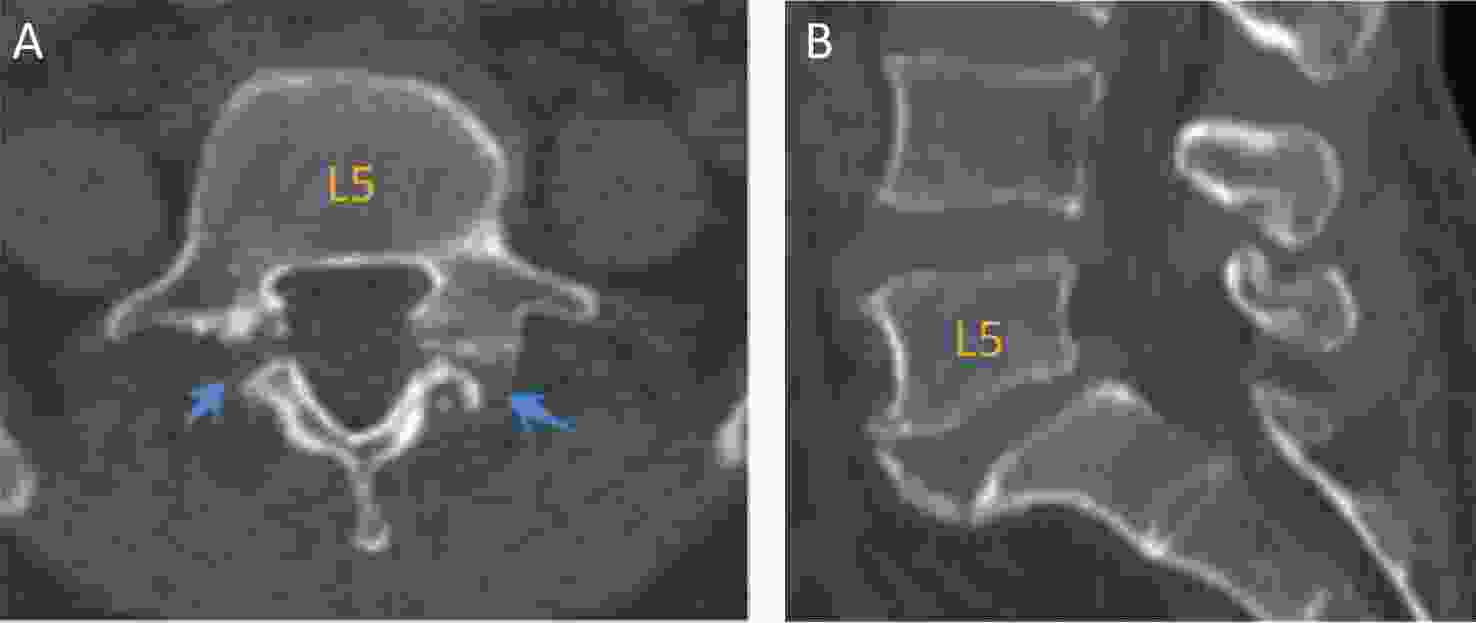
Among 117 patients with LS, 121 vertebrae had defects or fractures in the pars interarticularis. Four patients (3.42%) had spondylolysis in two vertebrae (L4 and L5). There were 102 cases of single-level spondylolysis at L5, accounting for 87.18% of all cases. Eight patients (6.84%) had single-level spondylolysis at L4. Additionally, there were 2 cases of spondylolysis at L3 (1.71%) and 1 case at L2 (0.85%). Spondylolysis was not observed at L1. L5 vertebrae were the most commonly affected by spondylolysis, followed by L4 vertebrae, with 106 cases at L5 (87.60%) and 12 cases at L4 (9.91%) out of all spondylolytic vertebrae.
Not all the patients had bilateral LS. Among the 121 spondylolytic vertebrae, 11 cases (9.09%) had only left-sided spondylolysis and 9 cases had only right-sided spondylolysis (7.44%), with unilateral spondylolytic vertebrae accounting for 16.53%. The remaining 101 (83.47 %) vertebrae exhibited bilateral spondylolysis.
-
Of the 121 LL, 64 cases were defined as SS (52.89%). Among them, 44 cases were classified as Grade I (36.36%), and 20 were classified as Grade II (16.53%). The remaining 57 patients (47.11%) with spondylolytic vertebrae did not exhibit vertebral slippage. No Grade III or higher slippages were observed. Among the spondylolytic vertebrae with SS, only one case had unilateral spondylolysis, whereas the rest had bilateral spondylolysis.
A comparison of the age and sex composition among the groups with no slippage (Grade 0), Grade I, and Grade II is shown in Table 3. There was no statistically significant difference in age among the three groups (P = 0.324). The proportion of males was higher in the Grade 0 group (70%), while the proportion of females was higher in the Grade II group (75%). There was a statistically significant difference in the sex composition between the Grade 0 group and the other two groups, but this difference was not observed between the Grade I and Grade II groups (P = 0.167).
Variables Grade 0 (n = 55) Grade I (n = 42) Grade II (n = 20) P0 P1 P2 P3 Age, years 61.20 ± 10.06 63.24 ±8.22 59.90 ± 5.94 0.324 0.619 0.872 0.208 Gender, n(%) Male 39 (70.91) 19 (45.24) 5 (25.00) < 0.001 0.013 0.001 0.167 Female 16 (20.09) 23 (54.76) 15 (75.00) Note. SS = spondylolytic spondylolisthesis. P0: Comparison among the three groups. P1, Grade 0 vs Grade I. P2, Grade 0 vs Grade II. P3, Grade I vs Grade II. Table 3. Comparison of age and gender composition among the groups divided by SS
-
The LS group had a smaller hip circumference (93.69 ± 6.78 cm) compared to the non-spondylolysis group (95.67 ± 8.77 cm), and this difference was statistically significant (P = 0.003). Even after adjusting for sex, the difference remained statistically significant (P = 0.013). There were no statistically significant differences between the two groups in terms of age, weight, height, BMI, or WHR. Comparing BMD between the two groups, the LS group (106.98 ± 39.40 mg/cm³) was slightly higher than the non-LS group (103.48 ± 39.03 mg/cm³), but the difference was not statistically significant (P = 0.341). When comparing paraspinal muscle parameters between the two groups, the LS group showed higher cross-sectional area and density of paraspinal extensor and flexor muscles compared to the non-LS group, and these differences were statistically significant, except for L5_PEMS, L5_PMMS, and L5_PMMD. However, after adjusting for sex, the only significant difference between the two groups was observed in L5_PEMD (P = 0.007) (Table 4).
Variables Total (n = 3,317) non-LS group (n = 3,200) LS group (n = 117) P P* Weight, kg 63.42 ± 11.76 63.39 ± 11.62 64.19 ± 14.95 0.473 − Height, m 159.64 ± 8.50 159.61 ± 8.52 160.65 ± 7.87 0.194 − BMI, kg/m2 24.89 ± 4.94 24.90 ± 4.94 24.80 ± 4.96 0.833 − WCF, cm 83.45 ± 10.18 83.49 ± 10.22 82.57 ± 8.67 0.268 − HCF, cm 95.60 ± 8.71 95.67 ± 8.77 93.69 ± 6.78 0.003 0.013 WHR 0.87 ± 0.07 0.87 ± 0.07 0.88 ± 0.06 0.226 − BMD, mg/cm3 103.61 ± 39.05 103.48 ± 39.03 106.98 ± 39.40 0.341 − L1_PEMS, cm2 38.53 ± 9.26 38.44 ± 9.26 40.70 ± 7.34 0.009 0.585 L1_PEMD, HU 39.94 ± 7.47 39.87 ± 7.46 41.7 ± 7.34 0.009 0.174 L3_PEMS, cm2 40.16 ± 8.91 40.04 ± 8.91 43.09 ± 8.12 < 0.001 0.077 L3_PEMD, HU 39.33 ± 7.47 39.27 ± 7.79 40.99 ± 8.12 0.019 0.299 L3_PMMS, cm2 15.62 ± 5.31 15.56 ± 5.27 17.12 ± 6.01 0.002 0.426 L3_PMMD, HU 43.19 ± 5.27 43.15 ± 5.27 44.27 ± 5.20 0.024 0.266 L5_PEMS, cm2 27.09 ± 6.39 27.08 ± 6.37 27.19 ± 6.87 0.852 0.548 L5_PEMD, HU 33.46 ± 7.85 33.36 ± 7.82 36.31 ± 8.40 < 0.001 0.007 L5_PMMS, cm2 19.88 ± 6.09 19.84 ± 6.06 20.67 ± 6.93 0.150 0.081 L5_PMMD, HU 45.01 ± 5.15 44.99 ± 5.13 45.36 ± 5.67 0.457 0.605 Note. Non-LS: group without lumbar spondylolysis; LS: lumbar spondylolysis. BMI: Body mass index. WCF: waist circumference. HCF: hip circumference. WHR: waist-hip ratio. BMD: bone mineral density. PEMS: paraspinal extensor muscle cross-sectional area. PEMD: paraspinal extensor muscle density. PMMS: psoas major cross-sectional area. PMMD: psoas major density. P, P-value before adjustment. *P value after adjusting for sex Table 4. Comparison between the LS and the non-LS group
-
In the baseline data, only height showed significant intergroup differences. The Grade 0 group had a significantly taller average height (163.47 ± 7.63 cm) compared to the Grade I group (158.20 ± 6.70 cm) and Grade II group (158.02 ± 8.48 cm), but these differences disappeared after adjusting for sex. BMD comparison revealed that the Grade II group had the lowest average BMD among the three groups (90.54 ± 39.40 mg/cm³), but there was no statistically significant difference in BMD among the three groups (P = 0.122).
Upon comparing the muscle parameter results, it was observed that as the spondylolisthesis grade increased, the values of the paraspinal muscle parameters tended to decrease. However, the difference in L3_PMMD (P=0.120) among the three groups was not statistically significant. For L1_PEMS, L1_PEMD, L3_PEMS, L5_PEMS, and L5_PMMD, statistically significant differences were found between the Grade 0 and Grade I groups as well as between the Grade 0 and Grade II groups, but no significant difference was observed between the Grade I and Grade II groups. Regarding L3_PEMD and L3_PMMS, statistically significant differences were noted only between the Grade 0 and Grade II groups. For L5_PEMD, Grade II group showed statistically significant differences compared to the Grade 0 and Grade I groups, but no significant difference was found between the Grade 0 and Grade I groups. The L5_PMMS group exhibited statistically significant differences among all the groups. However, after adjusting for sex, statistically significant differences were observed only for L5_PEMS among the aforementioned parameters (Table 5).
Variables Grade 0 (n = 55) Grade I (n = 42) Grade II (n = 20) P0 P1 P2 P3 P* Weight, kg 65.39 ± 15.80 64.15 ± 15.59 60.95 ± 10.69 0.528 0.688 0.260 0.434 − Height, m 163.47 ± 7.63 158.20 ± 6.70 158.02 ± 8.48 0.001 0.001 0.006 0.928 0.069 BMI, kg/m2 24.38 ± 4.94 25.50 ± 5.31 24.46 ± 4.25 0.517 0.272 0.950 0.442 − WCF, cm 82.91 ± 8.54 82.48 ± 8.75 81.86 ± 9.23 0.896 0.808 0.646 0.796 − HCF, cm 94.15 ± 6.84 93.04 ± 5.98 93.79 ± 8.29 0.729 0.430 0.840 0.688 − WHR 0.88 ± 0.60 0.89 ± 0.61 0.87 ± 0.05 0.712 0.673 0.602 0.413 − BMD, mg/cm3 110.27 ± 42.18 110.49 ± 33.95 90.54 ± 39.40 0.122 0.979 0.055 0.062 − L1_PEMS, cm2 42.95 ± 8.37 39.26 ± 9.47 37.65 ± 7.77 0.029 0.040 0.021 0.499 0.577 L1_PEMD, HU 43.60 ± 6.49 40.37 ± 7.84 39.28 ± 7.51 0.026 0.030 0.023 0.576 0.250 L3_PEMS, cm2 45.37 ± 7.86 41.48 ± 8.35 40.20 ± 7.88 0.015 0.020 0.015 0.559 0.290 L3_PEMD, HU 42.96 ± 6.57 40.25 ± 9,06 37.09 ± 8.62 0.015 0.097 0.005 0.144 0.243 L3_PMMS, cm2 18.46 ± 5.51 16.88 ± 6.63 13.99 ± 4.85 0.015 0.188 0.004 0.071 0.439 L3_PMMD, HU 45.28 ± 5.31 43.65 ± 5.10 42.80 ± 4.76 0.120 0.127 0.068 0.543 0.689 L5_PEMS, cm2 29.45 ± 5.96 26.07 ± 5.82 23.34 ± 9.00 0.001 0.019 0.028 0.535 0.003 L5_PEMD, HU 38.06 ± 6.29 36.28 ± 8.73 31.57 ± 11.03 0.011 0.288 0.003 0.036 0.183 L5_PMMS, cm2 23.11 ± 6.77 19.81 ± 6.74 15.78 ± 4.57 < 0.001 0.014 < 0.001 0.024 0.053 L5_PMMD, HU 46.82 ± 5.38 44.55 ± 5.52 43.01 ± 5.90 0.018 0.047 0.009 0.308 0.338 Note. SS: spondylolytic spondylolisthesis. BMI: Body mass index. WCF: waist circumference. HCF: hip circumference. WHR: waist-hip ratio. BMD: bone mineral density. PEMS: paraspinal extensor muscle cross-sectional area. PEMD: paraspinal extensor muscle density. PMMS: psoas major cross-sectional area. PMMD: psoas major density. P0: Comparison among the three groups. P1, Grade 0 vs. grade I; P2, grade 0 vs. Grade II P3: Grade I vs. Grade II. *P value after adjusting for sex Table 5. Comparison between groups based on the grading of SS
-
This study, based on a nationwide multi-center project, reported the prevalence of LS and the rate of SS in Chinese community-dwelling adults. The overall prevalence of LS in our study cohort was 3.53% and did not change significantly with age. The prevalence of LS was higher in males (5.18%) than in females (2.57%); however, females were more prone to SS than males among LS patients. L5 is the most common vertebra affected by spondylolysis. Although bilateral spondylolysis is the most common, it can also occur unilaterally, with the former being more likely to be associated with SS.
LS is believed to be associated with sex, family history, and ethnicity, resulting in varying prevalence rates across populations. Studies have indicated that the prevalence of lumbar spondylolysis in Caucasian populations is approximately 6%, which is 2–3 times higher than that in African Americans. Its prevalence rate in the Inuit population is as high as 25%[2]. The prevalence of lumbar spondylolysis in the Japanese population ranges from 5.9% to 6.4%[6,14], which is higher than that observed in the Chinese population in this study.
Reports suggest that the prevalence of LS in males is generally 2–3 times higher than in females[1,2,4,15]. In the present study, the prevalence of LS in males was approximately twice that in females. Lumbar spondylolysis typically occurs during childhood or adolescence, and its prevalence remains relatively stable in adults aged > 20 years old[16]. This study also found no significant age-related changes in the prevalence of lumbar spondylolysis. Therefore, although the study population mainly consisted of middle-aged and elderly individuals aged 40 and above, the prevalence derived from this cohort still reflects the epidemiological situation of LS in Chinese adults.
Previous studies reported that 85%–95% of lumbar spondylolysis cases occur at the L5 level, followed by L4 (10%–15%)[17,18]. The data from this study are consistent with these findings. Roche et al. found that unilateral spondylolysis accounts for approximately 1/6 of LS cases based on 4200 skeletons[19]. Aoki et al. found that the incidence of unilateral spondylolysis was approximately 15.6% in LS cases in a study of degenerative lumbar diseases in the Japanese population[14]. In this study, unilateral spondylolysis accounted for 16.53% of all cases, similar to the proportions reported in the aforementioned studies. However, some studies have reported different proportions; Belfi et al. and Sakai et al. found that unilateral spondylolysis accounted for approximately 1/5 of all LS cases[6,20]. Unilateral spondylolysis is more stable and less likely to lead to SS[6,14]. In this study, only one case of unilateral spondylolysis resulted in SS.
This study found that the occurrence of SS did not change with age, which differs from lumbar degenerative spondylolisthesis[21]. In a 45-year follow-up study in children, Fredrickson et al. found that most cases of SS occurred early, with subsequent slowing of progression every 10 years. By the end of the follow-up period, the proportion of cases without slippage had exceeded 40%, similar to the results of this study (47.11%)[22,23]. Although this study lacks early population data and cannot present the natural progression of secondary slippage due to spondylolysis, the results suggest that the risk of vertebral slippage due to spondylolysis in middle-aged and elderly individuals does not vary with age. However, it is important to note that a combination of degenerative spondylolisthesis and spondylolysis is possible. Females are more likely to develop SS, whereas males are more likely to experience LS[15]. The data of this study also support this observation.
Based on our investigation of the prevalence of LS and SS, we explored the skeletal and muscular characteristics of patients affected by these conditions. We found that patients with LS had smaller hip circumferences. Body circumference can reflect information about body composition, such as fat and muscle[24]. There is a correlation between the hip circumference and lumbar spine diseases[25]. However, we did not find any literature on the correlation between hip circumference and LS. Our study found that a small hip circumference may be a risk factor for lumbar spondylolysis, although it is also possible that lumbar spondylolysis leads to a smaller hip circumference. Our study revealed no statistically significant difference in the lumbar spine BMD between patients with and without LS. Moreover, the occurrence of SS was unrelated to BMD. In other words, the presence of lumbar spondylolysis did not affect the overall BMD.
After adjusting for sex, we found that the L5_PEMD was higher in the LS group than in the non-LS group. Additionally, individuals with SS exhibited lower L5_PEMS scores and lower grades of spondylolisthesis correlated with lower L5_PEMS values. There were no significant differences observed in muscle parameters at other planes, which may be attributed to LS predominantly affecting the L5 vertebrae. The paraspinal extensor muscles, particularly the deep multifidus fibers, play a crucial role in controlling intervertebral and segmental spinal movements, as well as maintaining spinal stability[26]. Following LS, the stability of the spinal bony structure diminishes, requiring greater muscular strength to compensate for and maintain spinal stability. This may explain why L5_PEMD was higher in the LS population than in the general population.
In the LS population, individuals with a reduced L5_PEMS are more prone to spondylolisthesis because insufficient muscle strength compromises the segmental stability of the spine. Park et al. also found that atrophy of the paraspinal extensor muscles (especially the multifidus muscle) correlated with SS progression[27]. In our study, when comparing L5_PMMS between the groups, we observed that as the degree of vertebral slippage increased, L5_PMMS decreased. Significant statistical differences were found in pairwise comparisons among the three groups (Table 5). However, after adjusting for sex, the statistical differences between the groups disappeared (P = 0.053). Park et al. reported a negative correlation between the cross-sectional area of the psoas major muscle and the severity of spondylolytic spondylolisthesis[27], which is in contrast to the findings of our study. Notably, this correlation does not exclude sex as a confounding factor.
This study of the paraspinal muscles may provide valuable guidance for functional rehabilitation and efficacy assessment of patients with LS. For patients with lumbar spondylolysis, it is important to focus on improving the quality of the lumbosacral muscles and engage in targeted exercises to maintain lumbar stability and prevent lumbar spondylolisthesis.
This study has several strengths: 1. It is based on a nationwide multi-center community project and provides a large sample size and a representative population for estimating the prevalence of LS. 2. CT imaging for multiplanar diagnosis of LS and SS offers higher accuracy than radiography and reduces the risk of missing unilateral spondylolysis. 3. Multilevel measurements of paraspinal muscle parameters provided a more detailed analysis. However, this study has some limitations to consider: 1. This study focused on middle-aged and elderly individuals in China aged 40 years and above, and being cross-sectional in nature, it does not reflect the natural progression of lumbar spondylolysis. 2. Some samples were excluded because of lumbar spine surgeries or image quality issues that may have included cases of spondylolysis, potentially affecting the results. Despite these limitations, the large sample size lends credibility to the findings.
-
The prevalence of LS in Chinese adults is 3.53% (5.18% in males and 2.57% in females. However, the prevalence did not change with age. Spondylolysis was most commonly observed at L5. The incidence of unilateral spondylolysis was 16.53% in all LS cases. Unilateral spondylolysis is less likely to result in SS than bilateral spondylolysis. The proportion of SS patients did not change with age. Female patients with spondylolysis are more likely to develop spondylolisthesis than male patients. Lumbar spondylolysis and spondylolytic spondylolisthesis are associated with the paraspinal extensor muscle density and area at the L5 level, respectively. Patients with spondylolysis exhibit higher paraspinal extensor muscle density at the L5 level, whereas those with spondylolytic spondylolisthesis show a smaller paraspinal extensor muscle area at the L5 level.
Lumbar Spondylolysis in Chinese Adults: Prevalence and Musculoskeletal Condition
doi: 10.3967/bes2025.043
- Received Date: 2024-08-21
- Accepted Date: 2024-12-02
-
Key words:
- Lumbar spondylolysis /
- Spondylolytic spondylolisthesis /
- Chinese /
- Prevalence /
- Musculoskeletal quantitative analysis
Abstract:
&These authors contributed equally to this work.
| Citation: | Dong Yan, Yandong Iiu, Ling Wang, Kai Li, Wenshuang Zhang, Yi Yuan, Jian Geng, Kangkang Ma, Fengyun Zhou, Zitong Cheng, Xiaoguang Cheng. Lumbar Spondylolysis in Chinese Adults: Prevalence and Musculoskeletal Condition[J]. Biomedical and Environmental Sciences. doi: 10.3967/bes2025.043 |







 Quick Links
Quick Links
 DownLoad:
DownLoad:
