-
Mental disorders (MDs) significantly impair cognition, mood, and social behavior, ranking among the top 10 leading causes of the global disease burden. Rising ambient temperatures are a critical factor triggering mental health-related conditions[1], especially under extreme temperature conditions[2]. Humidity further exacerbates these effects by inhibiting sweating and intensifying heat stress, making it a significant contributor to heat-related mental health impacts[3]. Existing evidence highlights an elevated risk of MDs associated with the combined effects of temperature and humidity[3,4]. However, current research lacks a comprehensive analysis of these combined effects on mental health.
We used individual-level, MDs-related emergency medical service (EMS) calls in Shenzhen as the outcome and two compound temperature–humidity indices (humidex and heat index) as exposures, employing a conditional logistic model within a time-stratified case-crossover design. This study aimed to (1) evaluate the nonlinear associations among humidex, heat index, and MDs-related EMS calls; (2) analyze the lagged effects of humidex and heat index extremes; and (3) identify the thresholds of high risk for MDs under specific temperature and humidity conditions. Findings from this study are intended to support early warning systems and preventive strategies addressing compound temperature–humidity extremes, thereby mitigating their mental health impacts and reducing related EMS calls.
The EMS call dataset was obtained from the Shenzhen Emergency Medical Center. MDs-related EMS calls were identified as those from patients with mental and behavioral disorders, diagnosed according to the 10th Revision of the International Classification of Diseases, with codes F01–F99. A total of 33,568 MDs-related calls from October 1, 2011, to June 30, 2023, were screened from 1,538,611 EMS calls.
Daily mean and maximum temperature, relative humidity, precipitation, and wind speed data were collected from the ERA5 reanalysis dataset (https://cds.climate.copernicus.eu/). We used two widely recognized indices to represent compound temperature and humidity: the humidex and heat index. Detailed calculations of these indices are provided in the Appendix (Technical Note 1 in Supplemental Materials).
To characterize compound temperature and humidity extremes, we defined humidex and heat index extremes as values exceeding the 90th percentile during the study period. Wind speed, precipitation, PM2.5, and O3 were used as covariates. Daily PM2.5 and O3 data were obtained from China High Air Pollutants. These covariates were extracted based on caller coordinates. We investigated the modifying effects of age (≤ 34 vs. > 34 years), sex (male vs. female), call location (workplace vs. residence), and seasonal variation (warm months: May–October; non-warm months: November–April). Age groups were determined based on the median age (34 years) of patients with MDs-related EMS calls.
A conditional logistic model with a time-stratified case-crossover design was used. In this design, the case day was defined as the day when a call occurred, and the control day was defined as the same day of the week in the same month and year, serving as a reference. The daily humidex and heat indices on the case and control days were compared. The odds ratio (OR) represents the change in risk when comparing exposure levels at the event time with typical exposure levels during the control periods for an individual. Time stratification simultaneously minimizes the influence of social and economic factors. First, we examined the nonlinear associations among humidex, heat index, and MDs-related EMS calls. The specific formula (1) is as follows:
$$ \begin{gathered}\text{logit}(P(Y_i=1|stratum))=ns(exposure,3)+\\ ns(windspeed,3)+ns(precipitation,3)+\\ ns(PM_{2.5},3)+ns(O_3,3) \end{gathered} $$ (1) where logit(P(Yᵢ = 1|stratum)) represents the conditional probability of the outcome (Yᵢ = 1) within the stratum. In formula (1), exposure denotes humidex and heat index as continuous variables. Wind speed, precipitation, PM2.5, and O3 levels were included as confounders in the model. The ns function represents natural cubic spline transformations. Based on the Bayesian Information Criterion,three degrees of freedom were determined for these variables, consistent with previous research[5].
Second, we examined the immediate and lagged effects of humidex and heat index extremes on the risk of MDs-related EMS calls. Formula (2) is as follows:
$$ \begin{gathered} {\text{logit}}(P({Y_i} = 1|stratum)) = exposur{e_{01lagk}} + wind spee{d_{lagk}}+\\ precipitatio{n_{lagk}} + P{M_{2.5lagk}} + {O_{3lagk}} \end{gathered} $$ (2) where lagk denotes the number of days before the call, including single-lag days (0, 1, 2, 3, 4, 5, 6, and 7) and cumulative lag days (moving averages: 0, 0–1, 0–2, 0–3, 0–4, 0–5, 0–6, 0–7). Lag days were selected based on previous research[4]. Exposure01 denotes the humidex and heat index as a binary variable (0 = no extreme, 1 = extreme, exceeding the 90th percentile). The results were compared for the overall population and subgroups stratified by sex, age, location, and call duration.
In the sensitivity analysis, we used a natural spline with six degrees of freedom for all factors in the nonlinear conditional logistic regression model to evaluate the stability of the nonlinear effects. We excluded wind speed, precipitation, PM2.5, and O3 to address potential interactions between air pollutants and weather factors.
All statistical analyses were performed using R software (version 4.4.1; R Foundation for Statistical Computing) with the “clogit” function from the “survival” package.
Figure 1A shows the overall increasing trend in MD-related EMS calls during the study period. The fitted curve of calls, maximum temperature, relative humidity, humidex, and heat index showed similar seasonal patterns, with peaks occurring between May and October (Figure 1B).
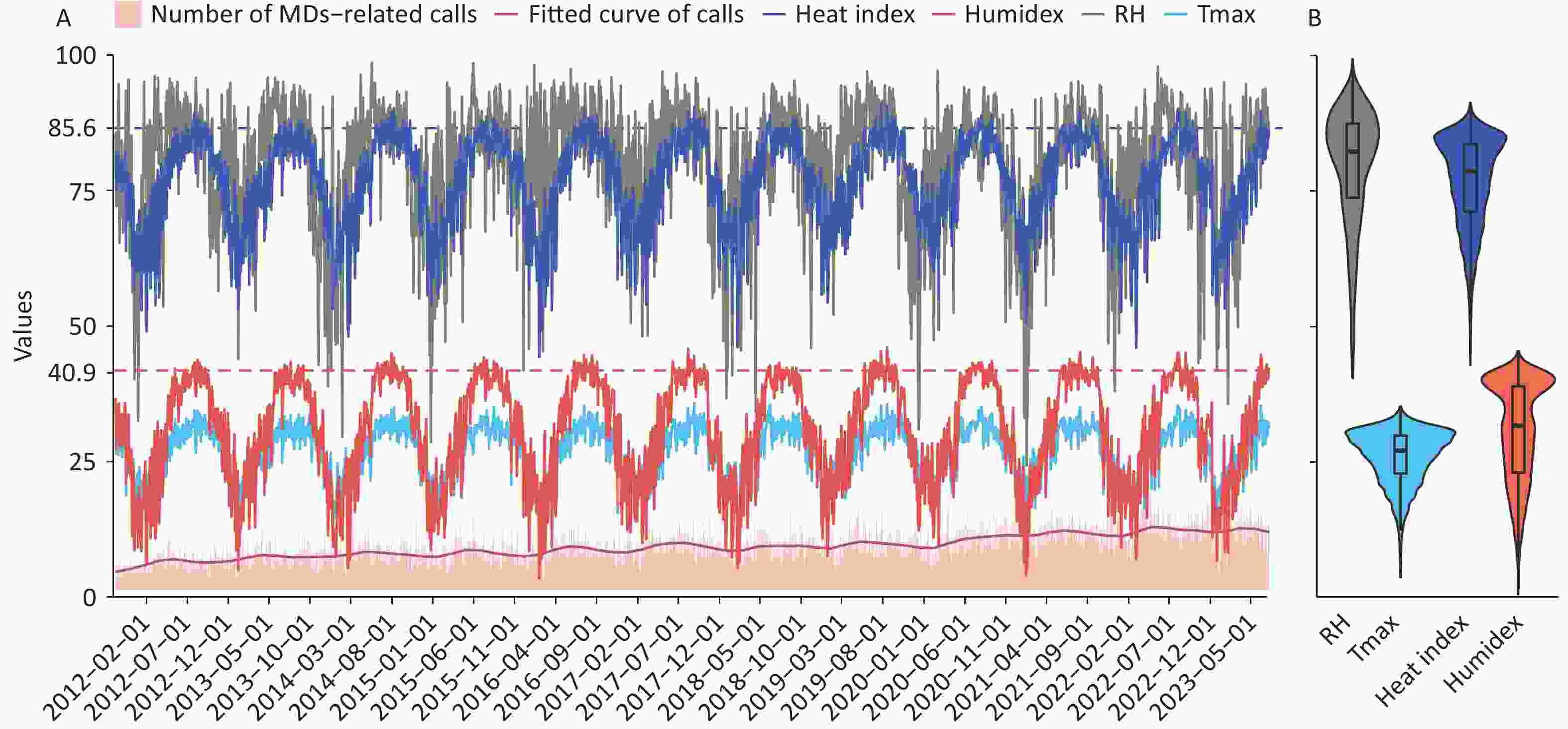
Figure 1. Characteristics of the variables used: temporal (A) and distribution trends (B). The y-axis represents the value of each variable. Two horizontal dashed lines depict the 90th percentile of the heat index (upper line) and humidex (lower line). The violin plot shows the data concentration trend. The band inside each box represents the median. The lower and upper boundaries of the box denote the 25th and 75th percentiles, respectively. The whiskers at the ends represent the 2.5th and 97.5th percentiles of each variable. MDs, mental disorders; RH, relative humidity (%); Tmax, maximum temperature (°C).
In total, 33,568 case days and 114,038 control days were included in the study period (Supplementary Table S1). The humidex and heat index for the case days were generally higher than those for the control days (Supplementary Table S2).
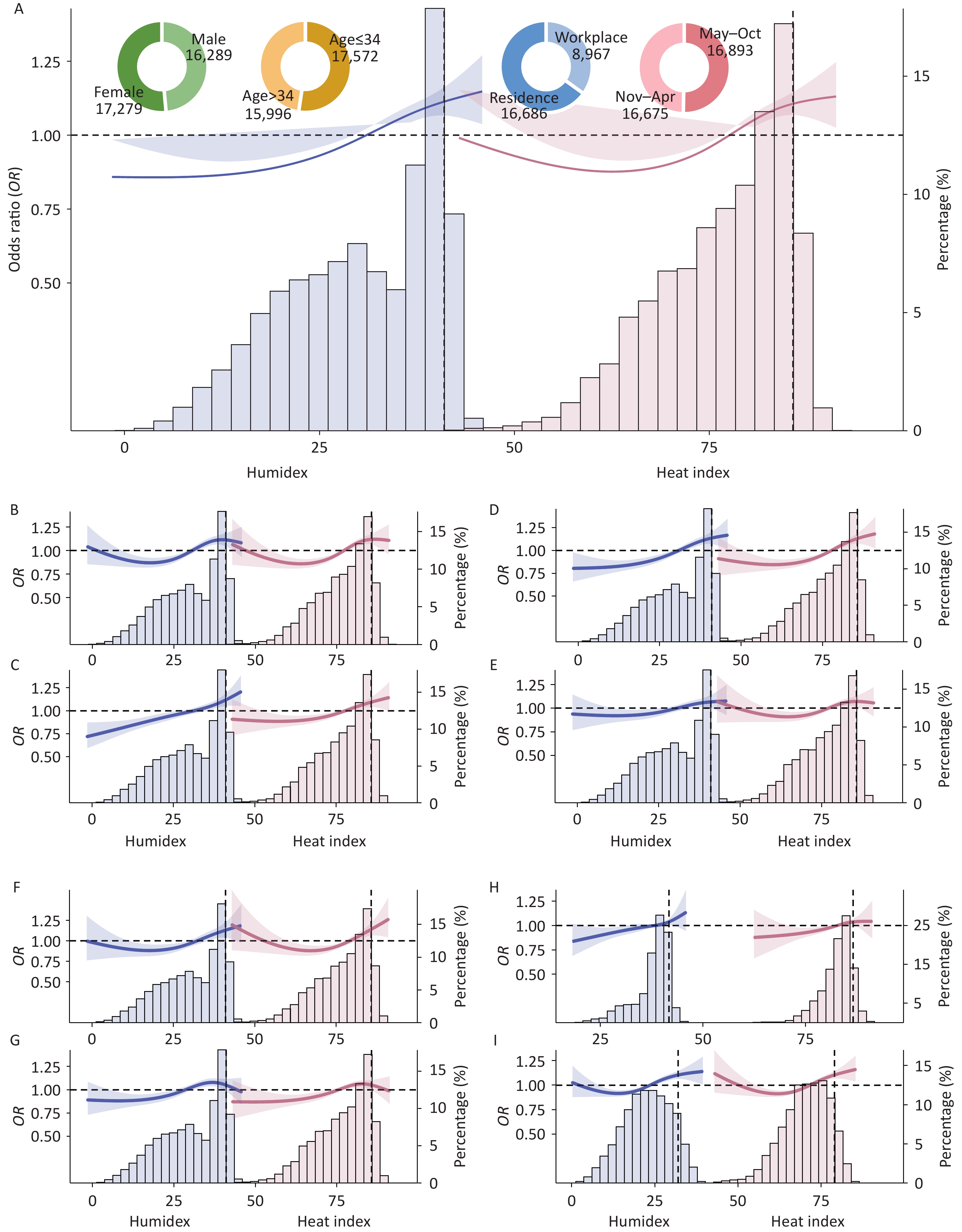
High humidex and heat index were found to significantly increase the risk of MDs-related EMS calls (Figure 2A), consistent with a previous study[4], which may be because of humidity under extreme temperature conditions that amplify heat stress[3].
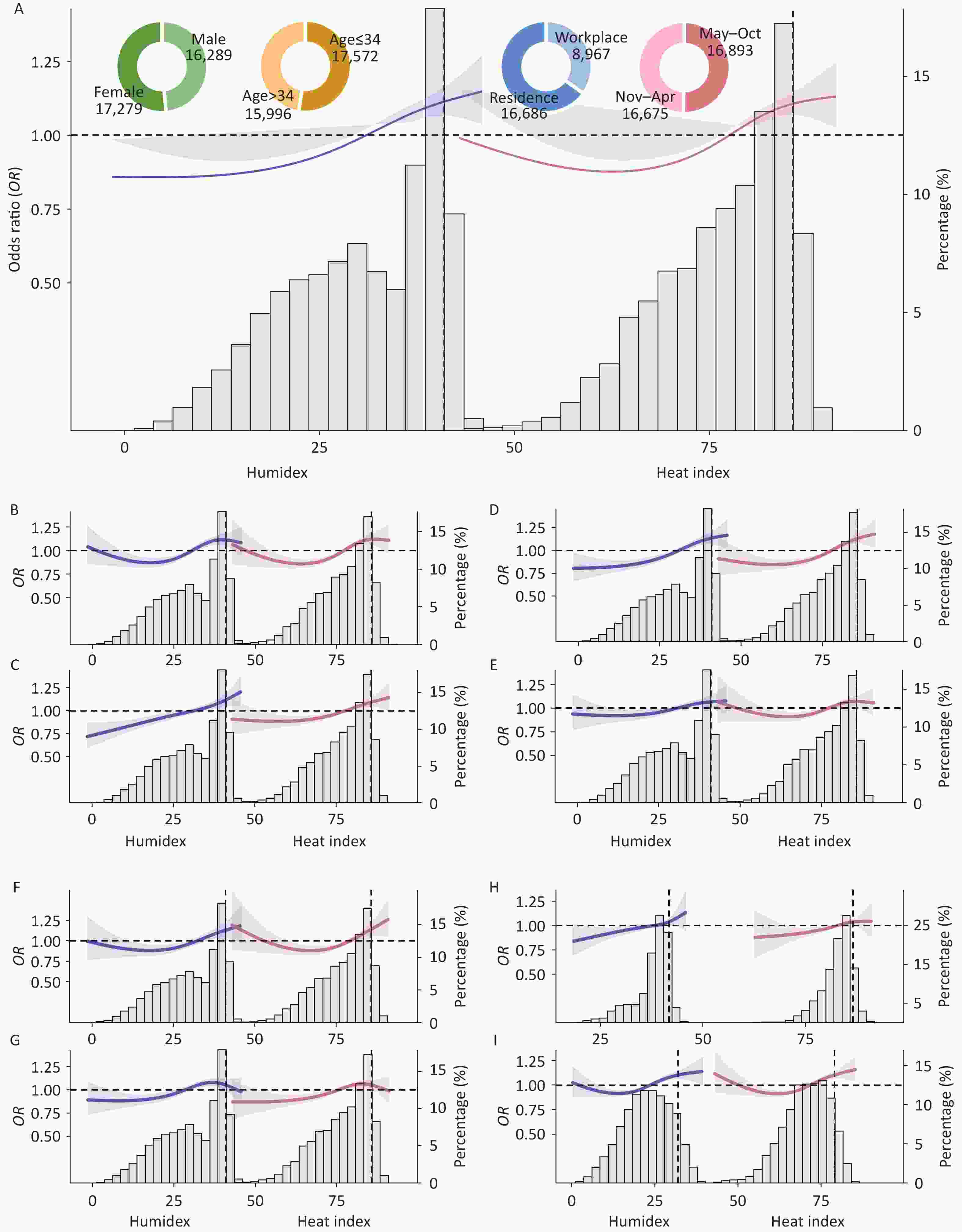
Figure 2. Exposure–response relations among humidex, heat index, and MDs-related EMS calls. The blue line represents humidex, and the red line represents the heat index. (A) Overall; (B) Men; (C) Women; (D) Age ≤ 34 years; (E) Age > 34 years; (F) Workplace; (G) Residence; (H) Warm months (May–October); and (I) Non-warm months (November–April). Four pie charts represent the proportions of case days across sex, age, location, and call month subgroups. The two vertical black dashed lines indicate the 90th percentiles of humidex and heat index. MDs, mental disorders; EMS, emergency medical services; OR, odds ratio.
Women appeared more susceptible to the effects of extremely high temperature–humidity conditions on acute mental health than males (Figure 2B and C). A potential explanation is that exposure to humid heat increases body thermal load[6], leading to greater heat intolerance and potentially reduced sweat responses in women[7]. These physiological changes negatively affect sleep quality, which is closely linked to mental health outcomes[8].
Individuals younger than 34 years appeared at greater risk for MDs-related EMS calls when exposed to extremely high compound temperature and humidity conditions (Figure 2D and E). Younger individuals tend to express heightened concern about hot weather, with high humidity intensifying perceived heat stress[3], which can provoke severe climate anxiety, potentially leading to emotional and cognitive mental health issues[9].
Furthermore, individuals in workplaces had a high risk of MDs-related EMS calls. This may be due to insufficient preventive measures in extremely hot and humid environments, such as limited access to air conditioning or cooling facilities[10]. A U-shaped relation between compound temperature–humidity indices and MDs-related EMS calls during the non-warm months was observed, suggesting that future studies should examine extremely low temperature–humidity conditions and their effects on MDs.
The main findings remained consistent when the degrees of freedom for natural splines were altered (Supplementary Figure S1), excluding wind speed, precipitation, PM2.5, and O3 (Supplementary Figure S2).
Overall, the OR for MDs-related EMS calls was 1.10 (95% confidence interval (CI): 1.05–1.15) for humidex extremes and 1.10 (95% CI: 1.06–1.14) for heat index extremes (Supplementary Tables S3 and S4). The risk of MDs-related EMS calls associated with humidex or heat index extremes was highest on lag day 1 for the overall population (Figure 3A and C). Similar single-day lag patterns were observed in women, individuals aged ≤ 34 years, and call months between May and October. The risk of MDs-related EMS calls remained significant over lag 0–7 d in the overall population, men, individuals aged ≤ 34 years, and during May–October (Figure 3B and D; Supplementary Tables S5 and S6).
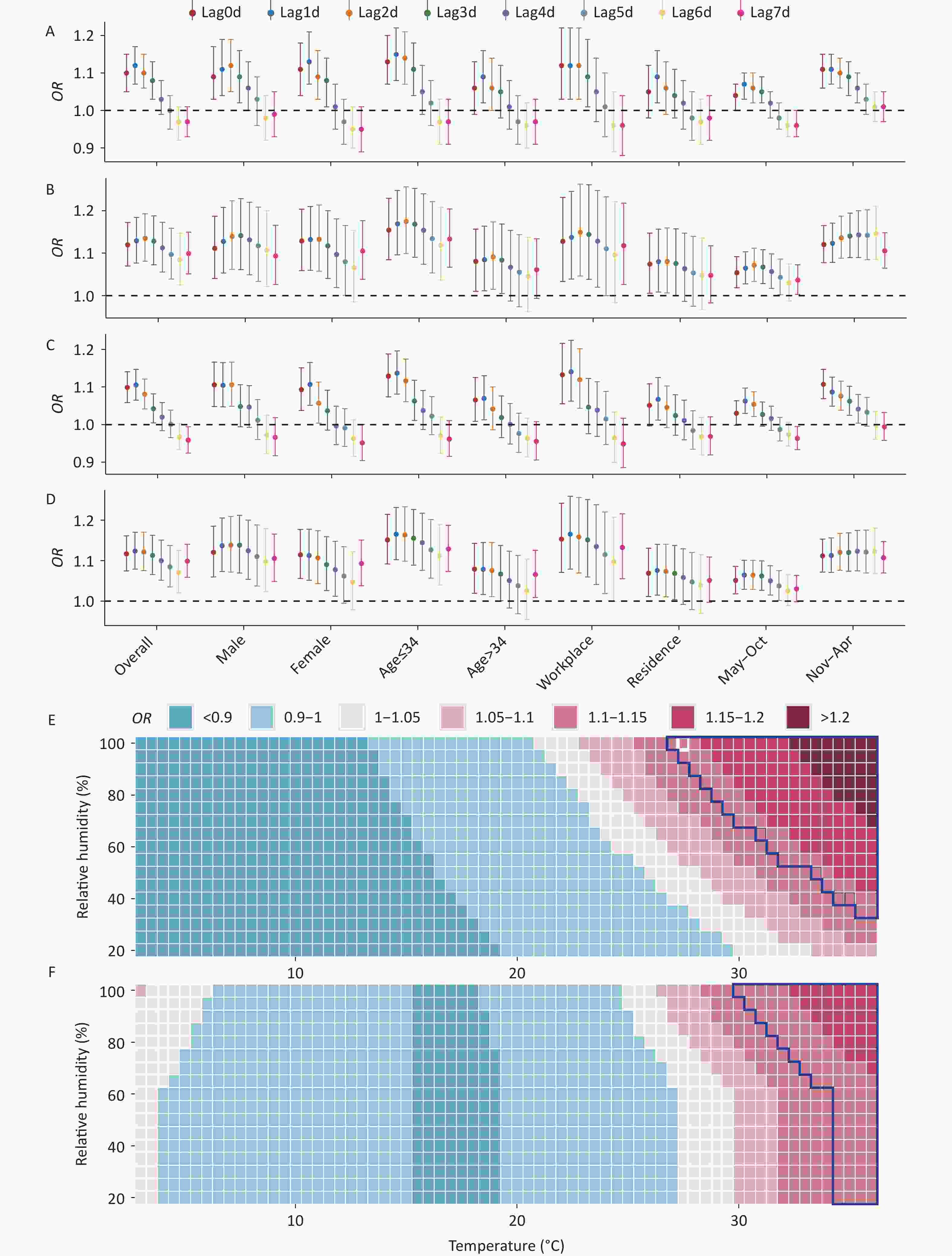
Figure 3. Risk of MDs-related EMS calls associated with compound temperature and humidity extremes and different temperature–humidity combinations. Panels A and B represent single-day and cumulative-day lag effects for humidex, respectively; panels C and D represent single-day and cumulative-day lag effects for the heat index, respectively; panels E and F represent humidex and heat index, respectively. Areas enclosed by dark blue lines represent compound temperature and humidity extremes (≥ 90th percentile). OR, odds ratio.
Figure 3E and F illustrate the risks of MDs-related EMS calls across different combinations of temperature and relative humidity. The threshold was defined as the humidex/heat index value at which the OR exceeded 1.15, and the threshold for high risk was identified when exposure to both indices was extreme (humidex > 43.09; heat index > 88.36). The numerical risk estimates for temperature, relative humidity, humidex, and heat index are presented in Supplementary Table S7. This finding reveals the potential risks under specific temperature and humidity conditions that may guide the development of early warning systems and mitigation measures.
This study had several limitations. First, we focused on the effects of compound temperature–humidity conditions on acute mental health outcomes, but an evaluation including patients with acute, mild, or moderate symptoms could be more informative. Second, given data availability, we could not analyze specific MD subtypes, such as schizophrenia and depression, and we could not consider individual factors, such as psychiatric history and occupation, when conducting a complete subgroup analysis. We also did not account for factors that could cause individual exposure bias, such as the use of air conditioners. Lastly, because the results are limited to the Shenzhen region, caution is warranted when extrapolating these relations to other study areas. Future analyses should focus on larger geographical areas with diverse climates and conduct multicenter studies to provide more comprehensive insights.
Compound Temperature–humidity Extremes Increase Acute Mental Health Outcomes: A 12-year Case-crossover Metropolitan Study
doi: 10.3967/bes2025.150
- Received Date: 2025-08-11
- Accepted Date: 2025-10-22
No potential conflicts of interest to disclose.
The study was ethically approved by the Medical Ethics Committee of the Southern University of Science and Technology (Approval No. 20240047).
&These authors contributed equally to this work.
| Citation: | Xin Liu, Xin Huang, Jingya Zhang, Haoran Li, Ning Zhang, Yingying Su, Yang Wang, Tongyan Liu, Rengyu Wu, Jincai Wei, Bin Zhu. Compound Temperature–humidity Extremes Increase Acute Mental Health Outcomes: A 12-year Case-crossover Metropolitan Study[J]. Biomedical and Environmental Sciences. doi: 10.3967/bes2025.150 |








 Quick Links
Quick Links
 DownLoad:
DownLoad: