-
Cancer stands as a prominent contributor to mortality from non-communicable diseases (NCDs) worldwide[1]. According to the latest GLOBOCAN 2022 estimates, the global cancer death toll surpassed 9.7 million in 2022, with 11.4% occurring in individuals younger than 50 years (early-onset cancer) and 51.9% in those under 70 years (premature mortality)[2]. In 2015, the United Nations (UN) issued a political declaration urging all member states to reduce premature mortality from NCDs by a third by 2030[3]. However, most countries have made little progress in achieving this ambitious target[4]. Coordinated global efforts aimed at enhancing cancer care are imperative to maximize health outcomes and make tangible progress towards this global health priority.
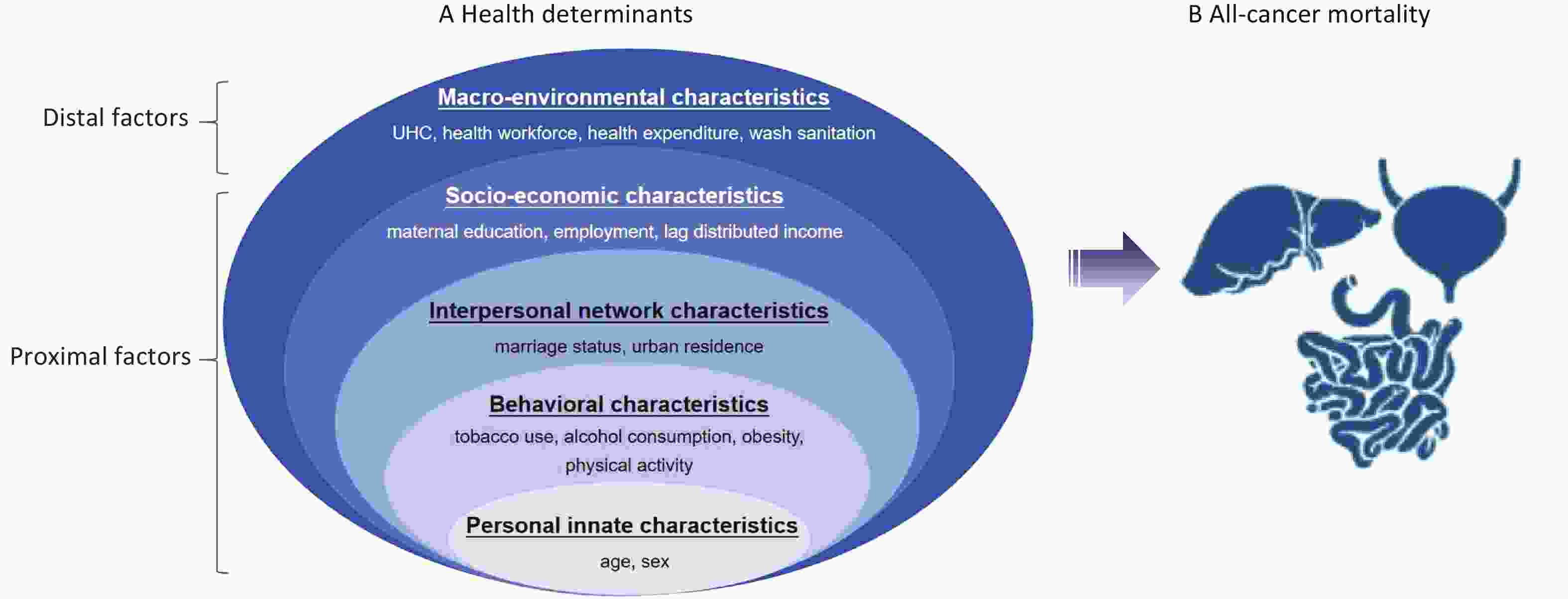
The health ecology framework, advocated by Collins[5], underscores that individual health outcomes are a composite of both distal and proximal factors, ranging from innate personal etiology to behavioral, interpersonal, socioeconomic, and political characteristics. By adopting a health ecology perspective to comprehend the intricate nature of health, public health professionals can gain valuable insights into devising and delivering targeted interventions that transcend traditional disciplinary boundaries[6,7]. According to the health ecology theory, health determinants that impact cancer outcomes are multifaceted. Among the most recognized modifiable risk factors, tobacco use, dietary risks, alcohol consumption, and obesity accounted for 21.5%, 6.8%, 3.5%, and 3.3% of global total cancer deaths in 2021, respectively[8]. Notably, the newly proposed “5 x 5 NCD agenda” at the Third High-level Meeting of the UN General Assembly on the Prevention and Control of NCDs in 2018[9], significantly broadened the scope of collective actions beyond the traditional four primary risk factors to incorporate air pollution, reflecting the expanding attention on a multidimensional approach to addressing risk factors. Moreover, certain socioeconomic determinants, including healthy housing conditions featuring appropriate ventilation and standard insulation to mitigate indoor air pollution, are positively correlated with a decreased risk of developing cancer[10]. Importantly, a supportive national health system characterized by a high degree of universal health coverage (UHC) and an increasing number of public cancer centers is more likely to reduce specific cancer mortality[11,12].
Incorporating health determinants to enhance cancer outcomes is an indispensable step towards achieving equitable and affordable cancer prevention and control on a global scale. Despite previous studies exploring individual factors correlated with all-cancer or cancer-specific mortality[13-15], a comprehensive framework that embraces multidimensional dominance remains insufficient. In this study, we examined the key health determinants influencing cancer outcomes from a health-ecological perspective by drawing on nationally representative data from global sources. Understanding the roles played by these health determinants is pivotal, as it will not only facilitate the identification of national-level health priorities for a comprehensive cancer control strategy but also illuminate pathways towards enhancing health equity.
-
We gathered the incidence and mortality data for all cancers in 185 countries from the 2022 GLOBOCAN estimates, which is considered the most reliable source of information on cancer outcomes set by the International Agency for Research on Cancer (https://gco.iarc.fr/en). Data on behavioral, interpersonal network, socioeconomic, and macroenvironmental factors were obtained from the WHO Global Health Observatory, the 2021 Global Burden of Disease (GBD) Study, the UN, and World Bank. A total of 153 of the 185 countries with complete data available for all relevant variables were included in this study. The development level of a country was assessed using the Human Development Index (HDI) devised by the UN, which is a summary measure of average achievement in the key dimensions of a long and healthy lifespan, intellectual prowess, and a decent standard of living. The HDI is the geometric mean of the normalized indices corresponding to each of these three vital aspects. A detailed list of the definitions, data sources, and estimated years of the 15 specific health determinants is provided (Table 1). Details on each matched health determinant are provided (Supplementary Table S1). This study conforms to the guidelines for accurate and transparent health estimate reporting. Ethical approval and patient consent were not required as the data were publicly available.
Health determinants Indicator definition Data source Estimate year Personal innate characteristics Age All ages (0 to > 85 years), < 50 years (early-onset), 30–69 years (Premature mortality) GLOBOCAN 2022 2022 Sex Male, Female GLOBOCAN 2022 2022 Behavioral characteristics Tobacco use (both, by sex) Current tobacco use prevalence (%) (age-standardized rate) The Global Health Observatory 2022 Alcohol consumption (both, by sex) Alcohol, total per capita (15 +) consumption (in liters of pure alcohol) The Global Health Observatory 2016–2018 Obesity (both, by sex) Prevalence (%) of obesity among adults, body mass index ≥ 30 (age-standardized rate) The Global Health Observatory 2022 Physical activity Age-standardized summary exposure value (SEV) (%) for low physical activity Global Burden of Disease Study 2021 Interpersonal network characteristics Marital status Married or in a union women age 15–49 years (age-standardized rate) The United Nations 2022 Urban residence Urban population (% of total population) Global Burden of Disease Study 2021 Socio-economic characteristics Maternal education Mean level (years) of maternal education attainment Global Burden of Disease Study 2021 Employment status (both, by sex) Employment in agriculture (% of total employment) the World Bank 2022 Lag-distributed income Lag-distributed income per capita (I$): gross domestic product per capita that has been smoothed over the preceding 10 years Global Burden of Disease Study 2021 Macro-environmental characteristics Universal health coverage Measure of coverage of essential health services on a scale of 1–100 The Global Health Observatory 2021 Health workforce Health workers per 10,000 population Global Burden of Disease Study 2021 Health expenditure Current health expenditure as percentage of gross domestic product (%) The Global Health Observatory 2021 Unsafe sanitation Age-standardized SEV for unsafe sanitation Global Burden of Disease Study 2021 Table 1. Definitions and data sources of health determinant indicators
-
The primary outcome of this study was the age-standardized mortality rate (ASMR) for all cancers. Additionally, we considered the age-standardized incidence rate (ASIR) as a secondary outcome. The code of death for all cancers was C00–C97, as defined according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD–10)[2].
-
According to the health ecology theory proposed by Collins[5], we comprehensively incorporated the diverse health determinants of cancer mortality into a multilevel health ecological model. We subsequently organized these factors into five domains: (1) Two personal innate characteristics, the core level, representing age and sex. With heightened attention paid to the distinctive features of early-onset and premature forms of cancer mortality over the past several decades, we focused on two specific age subgroups: individuals aged < 50 years (classified as early-onset) and those aged 30–69 years (who experience premature mortality due to cancer). (2) Four behavioral characteristics, the second level, representing tobacco use, alcohol consumption, obesity, and physical activity. (3) Two interpersonal network characteristics, the third level, representing marital status and urban residence. (4) Three socio-economic characteristics, the fourth level, representing maternal education level, employment status, and lag-distributed income. (5) Four macro-environmental characteristics, the fifth level, representing UHC, health workforce, health expenditure, and unsafe sanitation (Figure 1). The rationale for selecting each health determinant is provided in Supplementary Table S2.
-
To characterize the epidemiological profiles of health determinants, we presented continuous variables using medians and quartiles. We then employed the chi-square test to compare the differences in proportions of categorical characteristics across countries with different HDI levels. A multivariate linear regression model was used to estimate the association between health determinants and ASMR for all cancers. Subsequently, dominance analysis was conducted to assess the relative significance of each variable in contributing to the overall regression model. Sensitivity analyses were performed using these two approaches. First, we reconstructed a multivariable linear regression model using the mean years of schooling (obtained from Our World in Data) as an alternative indicator of maternal educational level. Second, we fit an additional multivariable linear regression model with ambient particulate matter pollution (obtained from GBD 2021), further adjusted as a covariate. Additionally, we examined the relationship between health determinants and the ASIR as an exploratory analysis.
All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA). The statistical test was two-sided, and the significance level of α was 0.05.
-
A total of 153 countries were included in this study, with 24, 33, 35, and 61 countries categorized as having low, medium, high, and very high HDI levels, respectively. In 2022, the global median (interquartile range) ASMR for total cancers was 90 (76, 108) per 100,000 population. The median ASMR was lowest in low HDI countries (80 [73, 95] per 100,000) and highest in very high HDI countries (98 [82, 112] per 100,000). The median ASMR for those aged < 50 years decreased as the HDI level increased, from 24 (20–27) per 100,000 people in low-HDI countries to 11 (9–15) per 100,000 people in very high-HDI countries. Among males, there was a notable increase in median ASMR as the HDI level increased, whereas females from countries with low HDI levels exhibited the highest median ASMR across all HDI hierarchies (Table 2). The crude mortality rates for all cancers stratified by HDI levels showed a trend comparable to that observed in ASMR, with the exception of females (Figure 2A–C).
Health determinants World
(n = 153)Low HDI
(n = 24)Medium HDI
(n = 33)High HDI
(n = 35)Very High HDI
(n = 61)P value* Personal innate characteristics Age ASMR for all ages (1/100,000) 90 (76, 108) 80 (73, 95) 81 (67, 97) 92 (80, 113) 98 (82, 112) 0.003 ASMR for < 50-year-old age group (early-onset cancer) (1/100,000) 17 (12, 21) 24 (20, 27) 21 (15, 25) 18 (15, 21) 11 (9, 15) < 0.001 ASMR for 30–69-year-old age group (premature mortality) (1/100,000) 134 (112, 161) 131 (115, 153) 135 (114, 161) 139 (122, 172) 130 (104, 159) 0.655 Sex ASMR for males (1/100,000) 100 (77, 124) 77 (68, 93) 80 (68, 106) 107 (83, 133) 113 (93, 149) < 0.001 ASMR for females (1/100,000) 81 (69, 91) 84 (71, 96) 83 (63, 96) 79 (71, 88) 80 (70, 90) 0.830 Behavioral characteristics Current tobacco use (%) 19 (11, 26) 9 (8, 14) 15 (11, 24) 21 (11, 26) 22 (16, 29) < 0.001 Alcohol consumption (per capita, in liters) 6 (3, 10) 3 (2, 7) 4 (2, 6) 6 (3, 7) 10 (7, 12) < 0.001 Obesity (%) (age-standardized prevalence) 22 (12, 30) 11 (7, 13) 16 (9, 23) 27 (22, 33) 24 (19, 32) < 0.001 Low physical activity (%) 17 (13, 24) 12 (8, 17) 15 (11, 19) 21 (14, 29) 19 (16, 26) < 0.001 Interpersonal network characteristics Married or in a union status for women aged 15–49 years (%) 57 (53, 63) 63 (57, 68) 58 (56, 63) 58 (55, 66) 54 (51, 57) < 0.001 Urban residence (%) 41 (29, 54) 28 (22, 34) 30 (24, 40) 45 (35, 56) 52 (41 ,60) < 0.001 Socio-economic characteristics Maternal educational level (years) 11 (8, 13) 5.1 (3, 7) 7 (7, 9) 11 (10, 12) 13 (12, 14) < 0.001 Employment in agriculture (%) 17 (4, 35) 53 (39, 67) 33 (22, 42) 17 (11, 26) 4 (2, 7) < 0.001 Lag-distributed income per capita 12,190
(4,705, 28,883)1,770
(1,432, 2,264)4,705
(3,512, 7,299)11,559
(9,962, 14,228)33,306
(23,696, 45,058)< 0.001 Macro-environmental characteristics Universal health coverage index 72 (55, 80) 42 (38, 47) 56 (52, 63) 72 (66, 76) 82 (78, 85) < 0.001 Health workforce per 10,000 population 129 (55, 247) 32 (22, 42) 57 (44, 71) 129 (86, 162) 302 (221, 387) < 0.001 Current health expenditure as percentage of GDP 7 (5, 9) 5 (4, 8) 5 (4, 7) 7 (5, 8) 9 (7, 11) < 0.001 Unsafe sanitation (%) 0 (0, 1) 1 (1, 1) 0 (0, 1) 0 (0, 0) 0 (0, 0) < 0.001 Note. HDI, human development index; GDP, gross domestic product; SEV, summary exposure value; ASMR, age-standardized mortality rate. Data are presented as median (interquartile range, IQR). Level of data: national data. *Differences between variables across HDI levels were tested using the non-parametric Kruskal-Wallis test. Table 2. Characteristics of health determinants and cancer mortality in 153 countries by HDI level
Figure 2. Crude mortality rate (1/100,000) for all cancers in 2022. Definition of abbreviations: HDI, human development index. Early-onset cancer: cancer diagnosed before the age of 50 years. Premature death: death occurring between the ages of 30 and 69 years.
As the HDI hierarchy increased, there was a significant increase in the median prevalence of several key characteristics, including current tobacco use, alcohol consumption, urban residence, maternal education level, lagged-distributed income per capita, UHC index, health workforce density, and current health expenditure as a percentage of GDP (all P < 0.01). However, the median proportion of women aged 15–49 years who were married or in a union, engaged in agricultural employment, and resided in unsafe sanitation conditions exhibited a declining trend as the HDI level increased (all P < 0.01) (Table 2).
-
In the multivariate analyses, ASMR for total cancers demonstrated independent positive correlations with current tobacco use [OR: 2.26, 95% CI (1.55, 3.28)], alcohol consumption [5.23 (1.78, 15.31)], obesity [1.59 (1.09, 2.31)], employment in agriculture [1.54 (1.12, 2.12)], and lag-distributed income [1.00 (1.00, 1.00)]. Conversely, a negative association was observed between ASMR and being married or in a union among women aged 15–49 years [0.63 (0.41, 0.97)] (Figure 3A). When stratified by age, a positive correlation was observed between ASMR for early-onset all-cancer and employment in agriculture [1.14 (1.04, 1.24)]. Furthermore, a marginal association was found with lag-distributed income [1.00 (1.00, 1.00)] and unsafe sanitation [1.08 (1.00, 1.17)] (Figure 3B). Notably, the associations between health determinants and ASMR in individuals aged 30–69 years were similar to those observed in all age groups (Figure 3C).
Figure 3. Association between health determinants and ASMR for all cancers. Definition of abbreviations: ASMR, age-standardized mortality rate; OR, odds ratio; UHC, universal health coverage. The health determinants included in the health-ecological model were presented in the format of continuous variables.
We also noted a pronounced sex disparity in health determinants linked to all-cancer ASMR. Among males, there were notable positive associations between current tobacco use [2.54 [1.77, 3.64)], alcohol consumption [8.69 (3.44, 21.95)], obesity [2.13 (1.22, 3.72)], and all-cancer ASMR. In females, current tobacco use [1.57 (1.05, 2.34)], obesity [1.56 (1.14, 2.12)], and employment in agriculture [1.27 (1.02, 1.59)] were positively associated with all-cancer ASMR. Notably, being married or in a union among women aged 15–49 years [0.63 (0.42, 0.93)] was negatively associated with ASMR (Figure 3D–E).
-
Dominance analysis revealed that current tobacco use, the most prominent contributor, accounted for 24.3% of the variations in all-cancer ASMR, followed by alcohol consumption (23.4%), lag-distributed income (7.4%), and agricultural employment (6.2%). Similarly, current tobacco use (28.6%) was most strongly associated with premature mortality, followed by alcohol consumption (18.4%) and lag-distributed income (14.9%). For early-onset cancer, employment in agriculture, unsafe sanitation, and lag-distributed income demonstrated associations of 17.9%, 16.0%, and 15.7% with ASMR. Among males, alcohol consumption (25.8%) had the highest association with ASMR, whereas for females, the strongest association was noted for being married or in a union among those aged 15–49 years (15.2%) (Table 3).
Health determinants Total Age Sex < 50 years
(Early-onset)30–69 years
(Premature mortality)Male Female Standard dominance
statistic, %P value Standard dominance
statistic, %P value Standard dominance
statistic, %P value Standard dominance
statistic, %P value Standard dominance
statistic, %P value Behavioral characteristics Current tobacco use 24.3 < 0.01 0.7 0.59 28.6 < 0.01 20.1 < 0.01 10.3 0.03 Alcohol consumption 23.4 < 0.01 1.6 0.88 18.4 < 0.01 25.8 < 0.01 11.4 0.19 Obesity 4.6 0.02 2.4 0.28 4.7 0.01 5.9 < 0.01 12.8 < 0.01 Low physical activity 3.2 0.88 3.3 0.71 4.6 0.89 5.4 0.50 2.4 1.00 Interpersonal network characteristics Being married or in a union status for women aged 15–49 years 5.3 0.04 2.2 0.07 1.1 0.32 2.0 0.18 15.2 0.02 Urban residence 0.5 0.74 4.0 0.70 2.0 0.66 1.0 0.95 1.4 0.64 Socio-economic characteristics Maternal educational level 14.3 0.20 8.6 0.07 8.7 0.14 14.4 0.37 9.6 0.10 Employment in agriculture 6.2 0.01 17.9 0.01 7.9 0.02 3.4 0.11 9.4 0.04 Lag-distributed income 7.4 0.02 15.7 0.04 14.9 < 0.01 5.5 0.01 5.0 0.26 Macro-environmental characteristics Health expenditure 1.8 0.08 2.0 0.51 1.3 0.11 1.6 0.13 2.5 0.14 UHC index 3.8 0.45 12.6 0.92 2.0 0.95 7.5 0.15 7.3 0.29 Health workforce 2.9 0.18 13.2 0.34 3.8 0.78 3.1 0.34 2.6 0.22 Unsafe sanitation 2.3 0.61 16.0 0.05 2.0 0.58 4.3 0.91 10.2 0.11 Table 3. The standard dominance statistic of health determinants using dominance analysis
-
After incorporating mean years of schooling as a substitute for maternal educational level or accounting for ambient particulate matter pollution, the associations between health determinants and ASMR for all ages, individuals aged < 50 years and 30–69 years, males, and females, remained consistently robust (Supplementary Tables S3–S4).
-
There was a notable surge in the crude incidence rate of total cancers as HDI levels increased, irrespective of age and sex. In high and very high HDI countries, males exhibited notably higher incidence rates than females, whereas the opposite was true for females from low and medium HDI countries (Supplementary Figure S1A–C). Notably, current tobacco use, alcohol consumption, and the health workforce displayed positive correlations with all-cancer ASIR among the entire population and subgroups. Furthermore, our analysis revealed significant positive associations between urban residency and ASIR in the whole population [1.93 (1.15, 3.23)], in individuals aged < 50 years [early-onset cancer, 1.30 (1.09, 1.54)], and 30–69 years [premature mortality, 2.88 (1.15, 7.21)], and specifically among females [2.07 (1.29, 3.31)] (Supplementary Table S5).
-
To the best of our knowledge, this study offers a comprehensive and insightful examination of the health determinants that correlate with cancer outcomes from a health-ecological perspective. Our findings demonstrated a persistent disparity in the mortality burden of all cancers across countries with varying HDI levels. Notably, we identified a range of factors, including age, sex, tobacco use, alcohol consumption, obesity, being married or in a union, agricultural employment, and unsafe sanitation conditions as having a significant association with all-cancer mortality. Overall, by leveraging nationally representative data from reputable sources such as GLOBOCAN 2022, the WHO Global Health Observatory, the GBD 2021, the UN, and the World Bank, our ecological estimates provide policymakers and public health professionals with a robust foundation to gain a deeper understanding of the challenges facing cancer prevention and control in the global health landscape.
Our study revealed distinct patterns in all-cancer mortality and the prevalence of risk factors across countries with varying HDI levels. Specifically, countries with higher HDI levels exhibited a disproportionately greater burden of all-cancer mortality, particularly premature death, in line with previous studies[11,16]. This phenomenon could potentially stem from the elevated incidence of cancer in high-HDI countries with increased access to healthcare resources, including advanced screening and early detection. Our exploratory analysis, as well as previous research, supports this hypothesis[11]. However, our findings indicate that early-onset cancer exhibits the most significant mortality burden in low HDI countries. A growing body of research suggests that exposure to certain dietary, lifestyle, and environmental factors during early life and among young adults could significantly elevate the risk of developing cancer in later life[17]. Its predominantly high mortality burden associated with early-onset cancer is likely attributable to poorly regulated exposure patterns. Additionally, an inadequate health insurance system that fails to cover the costs of cancer screening, along with shifting demographics[18,19], could also be contributing factors.
Among the 15 enrolled health determinants related to cancer mortality, current tobacco use, alcohol consumption, and obesity were crucial behavioral factors that significantly elevated the risk of all-cancer mortality (Supplementary Table S6) and premature death, regardless of sex. The pivotal roles of these risk factors in cancer onset and progression have been confirmed through large-scale population-based studies[14,20-22]. Currently, extensive global efforts are underway to mitigate these risk factors. Since the WHO’s endorsement of the Global Action Plan for the Prevention and Control of NCDs 2013–2020, there has been a renewed focus on implementing the renamed “Best Buys” interventions[23]. These core interventions encompassed bolstering the efficient execution of the WHO Framework Convention on Tobacco Control, fostering heightened awareness about the detrimental consequences of harmful alcohol use, and executing the global strategy on diet and physical activity, with the aim of expediting national responses in preventing and managing NCDs[23]. Continuous interventions hold significant promise for alleviating the cancer burden. Nonetheless, our findings revealed no discernible association between behavioral patterns and mortality risk in early-onset cancer. Given that the data on behavioral risk exposure and cancer outcomes utilized in this study originated from global epidemiological surveys conducted within the past five years, it is plausible that the inadequate duration of cumulative exposure may contribute to a lack of statistical power in detecting any substantial association. To validate these potential effects, extensive population-based studies involving large cohorts of young adults are warranted.
Numerous studies have investigated the intricate associations between interpersonal networks, social determinants, and cancer outcomes. It has been observed that cancer patients who are married experience a heightened all-cancer mortality [1.57 (1.56–1.59)] compared with unmarried patients among males. This disparity could potentially stem from the positive impact of marital status on access to social support and the availability of medical insurance, all of which may contribute to lower cancer mortality rates[24]. Furthermore, previous studies have found a positive association between marital status and cervical cancer screening. The potential causes could be the motivating influence of familial support and the fostering of social connections, which may encourage preventive healthcare behaviors among married individuals[6,25]. The transgenerational importance of education for enhancing child survival has been firmly confirmed through an exhaustive global systematic review and meta-analysis[26]. Similarly, a case-control study drawing participants from the Italian census cohort demonstrated that individuals whose parents possessed higher levels of education experienced a lower mortality rate ratio for total cancers[27]. However, our primary findings and sensitivity analysis did not reveal similar correlations. Further population-based studies are needed to validate these associations. It is noteworthy that agricultural employment was positively correlated with a heightened mortality risk from cancer among all ages, those aged < 50 and 30–69 years, and females. One cohort study utilizing data linkage between population censuses and registers in Belgium, found that agricultural and fishery workers faced a significantly elevated risk of ovarian cancer [1.63 (1.20, 2.21)] compared with women in managerial and professional roles, while male workers in these sectors demonstrated a higher mortality risk for multiple myeloma [1.55 (1.09, 2.22)] and leukemia [1.33 (1.01, 1.74)][28]. Occupational status intricately intertwines with social networks, exposure to occupational hazard substances, and work-related psychological factors, ultimately influencing the accessibility and utilization of healthcare. Additionally, a case-control study in rural agricultural communities in Northern India suggested that pesticide use, such as heptachlor, ethion, and chlorpyrifos, may play a role in the higher prevalence of cancer cases[29]. Addressing these health disparities necessitates multifaceted and collaborative strategies across multiple sectors[30].
Previous studies have revealed a correlation between the characteristics of national health systems, specifically increased national public health expenditure on healthcare, UHC, and the health workforce, and a decrease in cancer mortality[31,32]. Our findings indicated a notable enhancement in macro-environmental performance as HDI levels increased. However, we failed to uncover a substantial association between these factors and a decline in cancer mortality. A plausible rationale is that the limited sample size of the enrolled countries, which may not have been sufficient to establish a definitive ecological association within the scope of this study. Consequently, there is a need for further exploration of the intricate interplay between pivotal characteristics, with a broader spectrum of countries and subnational health system variables being incorporated.
-
From a health-ecological perspective, this study provides the first systematic quantification of health determinants and all-cancer mortality using nationally representative data on epidemiological variables and cancer outcomes sourced from multiple reputable datasets. It provides a comprehensive overview of the health determinants associated with the overall cancer burden within the proposed health- ecological framework. Our findings provide policymakers with well-informed evidence, enabling them to devise comprehensive strategies that holistically address both proximal and distal factors to effectively alleviate the overarching burden of cancer.
This study has some limitations. First, the risk-outcome relationships were interpreted through data linkage between cancer outcomes from GLOBOCAN 2022 and health determinants from diverse global sources. However, it is imperative to note that a potential selection bias arises when assessing the global impacts of multifaceted health determinants owing to the insufficiency of input data from cancer registries, disease surveillance systems, and original epidemiological studies in some low-income countries. Additionally, the national estimates of risk exposure in the GBD study relied heavily on predictors derived from standard models. The reliability of these country-level estimates could be improved if the limitations of the input data are adequately addressed. Second, given the primary focus of the present study and space constraints, we refrained from investigating the association between health determinants and cancer-specific mortality. A more detailed examination of specific cancer types and their associated mortality estimates will be the focus of our future research. Third, this study adopted an ecological approach utilizing national-level matched data from 153 countries. Additionally, we did not account for some important variables, such as differences in dietary behaviors, (including animal- or plant-based product consumption across countries) due to data unavailability. Further studies should incorporate more well-established risk factors to enable a more comprehensive exploration[33]. As such, future population-based studies should strive to collect more intricate individual-level data to provide a more nuanced understanding of the topic.
-
The profiles of health determinants, including innate personal factors, behavioral patterns, interpersonal networks, socioeconomic status, and macroenvironmental characteristics, exhibit substantial heterogeneity across countries with varying HDI levels. Notably, ecological associations were predominantly observed between behavioral and socioeconomic attributes and all-cancer mortality. Our findings underscore the crucial need to incorporate cross-sectoral interventions within a resilient healthcare system to effectively mitigate the cancer mortality burden.
Health Determinants in Association with Cancer Mortality from a Health Ecological Perspective
doi: 10.3967/bes2025.152
- Received Date: 2025-08-03
- Accepted Date: 2025-11-04
-
Key words:
- Health determinants /
- Cancer mortality /
- Health ecological model /
- Dominance analysis
Abstract:
The authors declare that they have no conflict of interest.
Ethical approval was not required for this study because the data were publicly available.
| Citation: | Chenran Wang, Zilin Luo, Jiaxin Xie, Xiaolu Chen, Yadi Zheng, Zeming Guo, Xiaoyue Shi, Xinyue Zhu, Wei Cao, Fei Wang, Xuesi Dong, Ni Li, Jie He. Health Determinants in Association with Cancer Mortality from a Health Ecological Perspective[J]. Biomedical and Environmental Sciences. doi: 10.3967/bes2025.152 |







 Quick Links
Quick Links
 DownLoad:
DownLoad: