-
As the acquired immune deficiency syndrome (AIDS) epidemic persists in China, the expansion of epidemic areas and the increasing number of people affected by AIDS in China present a scenario characterized by a combination of overall low and high levels of outbreaks in critical areas. The pandemic has spread from high-risk groups to the general population, posing formidable challenges to the prevention and treatment of AIDS. AIDS epidemics differ across China[1]. In 2015, 15 provinces in China had more than 10,000 people living with HIV/AIDS, with Sichuan Province ranking second following Yunnan.
The onset of AIDS in Sichuan dates back to 1991 when the first reported case emerged among laborers returning from East Africa (acquired through infection abroad). Subsequently, the first case of HIV/AIDS resulting from the sharing of injecting equipment was documented in 1995.
The first HIV/AIDS cases involving commercial and anal sex were reported in 1996 and 2002, respectively. By the end of 2002, HIV/AIDS was reported in 21 cities (states) in Sichuan. According to the Sichuan report, the number of people living with HIV/AIDS (PLWHA) reached 78,261, of whom 27,016 had AIDS, and the number of deaths from AIDS-related illnesses reached 23,037 at the end of 2015[2].
The developmental trajectory of the AIDS epidemic is a key factor affecting control strategies and measures. For a country or region, the prediction of the HIV/AIDS epidemic is particularly important, as it provides the basis for epidemic prevention and control efforts in the region. Are future trends in the HIV/AIDS epidemic increasing or decreasing? What is the trend in the HIV epidemic among high-risk groups? What is the prevalence of HIV in the general population? Which intervention is more effective? These urgent issues need to be addressed, and the HIV/AIDS prediction model stands out as the optimal solution. The AIDS Epidemic Model (AEM) version 4.13 is an updated version of the Asian Epidemic Model designed by Dr. Tim Brown’s research team at the East-West Center in the late 1990s. This model, crafted based on the epidemiological patterns predominantly observed in Asia, where most HIV transmissions occur through sex and injection-sharing practices, is versatile[3]. AEM 4.13 is designed for application in most low-level and concentrated epidemics, including those outside Asia, to assess past and future trends in HIV epidemics. This study is the first to apply the AEM model recommended by the Joint United Nations Programme on HIV/AIDS in Sichuan, China, to predict the provincial AIDS epidemic trend.
-
The AEM version 4.13 is an updated version of the Asian Epidemic Model designed by Dr. Tim Brown’s research team at the East-West Center in the late 1990s. This model was crafted based on the epidemiological patterns predominantly observed in Asia, where most HIV transmissions occur through sex and injection-sharing practices. AEM 4.13, designed for application in various low-level and concentrated epidemics, encompassing regions beyond Asia, is employed for the analysis of influencing factors in predicting future epidemics. The AEM is based on a semi-empirical process that replicates the key processes driving HIV transmission in Asia[4]. Using trends in risk behaviors among important Asian subpopulations as inputs, the model determines the necessary HIV transmission probabilities to align with the observed epidemiological patterns revealed by surveillance data. The AEM has several advantages over other HIV prediction models. First, owing to the annual serial nature of the AEM model input data, the dynamics of the HIV epidemic can be understood in a timely manner, and the authenticity of the model prediction results can be increased. The parameters and data were input and adjusted according to the actual local situation, resulting in a fitted epidemic curve that better reflects the local epidemic trend. Additionally, the AEM model can predict an epidemic scenario under different behavior levels, enabling the comparison of the effects of various interventions and providing a basis for decision-makers to formulate more effective intervention strategies. However, the AEM model has some shortcomings, the most significant being its substantial demand for data. In areas with low HIV prevalence where extensive data are unavailable, the AEM model is unable to generate predictions. Fortunately, the Sichuan Province met the forecast data conditions. Previous studies have applied AEM to Liangshan Prefecture in Sichuan Province[5]. In 1994, the Sichuan Province established a monitoring network for high-risk groups in 1994. This network serves as a valuable source of data for the application of the AEM. This is the first instance in which the AEM has been used to predict the provincial HIV/AIDS epidemic situation in China.
-
To maintain privacy, the following data collected from Sichuan Province in 1991–2015 were analyzed: (a) population data including demographic information (i.e., annual ratio of male and female patients aged ≥15 years and fertility rate) obtained from the Sichuan Statistical Yearbook, population size obtained from the Sichuan Census Bureau, and estimated size of high-risk populations obtained from the Chinese Center for Disease Control and Prevention; (b) behavioral data, including the proportion of condom use, injection practice, needle sharing, and sexual behavior from 146 behavioral surveillance sites; (c) HIV prevalence data, surveillance and epidemiological survey data obtained from 145 sentinel surveillance sites, and comprehensive surveillance data of 11 defined groups (i.e., injecting drug users (IDUs), men who have sex with men (MSM), female sex workers (FSWs), clients of FSWs, migrant workers, residents, entry-exit people, male patients attending sexually transmitted disease (STD) clinic, pregnant women, adolescents in school, and male coach driver) from the HIV surveillance systems of 21 cities and prefectures obtained from Sichuan Center for Disease Control and Prevention (CDC); and (d) reports and publications of HIV-related policies and public health/outreach projects obtained from local organizations (i.e., government, health-related sector, project management offices, and public security departments).
The accumulated data were checked, screened, sorted, and classified based on the standardized information system for portable diseases of AIDS cases (National Center for AIDS/STD Control and Prevention/STD, Chinese CDC, and Sichuan CDC). Experts were consulted to ensure the inclusion of high-quality data only, and any missing data were supplemented by referring to previous records or through interpolations.
-
AEM is based on epidemiological patterns commonly observed in concentrated epidemics, where the majority of HIV transmission occurs among several key populations and their sexual partners. These populations include MSM, male sex workers (MSWs), FSWs, clients of FSWs (CFSWs), people who inject drugs (PWID, men and women), transgender populations (TGs), and lower-risk members of the general population (both men and women). Based on the epidemiological patterns in China, the TGs were not fitted. Population dynamics were considered as individuals often move from one population group to another. The data were entered into the AEM, and modeling was performed following the previously described methodology[3,6]. Briefly, the AEM calculates the annual number of PLHIV, new HIV/AIDS cases, and HIV-related deaths based on an overall consideration of new infections and the natural course of HIV infection and AIDS. Consequently, the AEM facilitates the prediction of future HIV prevalence and transmission trends, as well as the estimation of the effects of different interventions on HIV prevalence.
-
Output fitting: The final curves of the model outputs for HIV/AIDS prevalence were fitted with the estimated prevalence rates from the data for all eight populations in Sichuan. This served as the baseline-fitted model for the projection under varying assumptions.
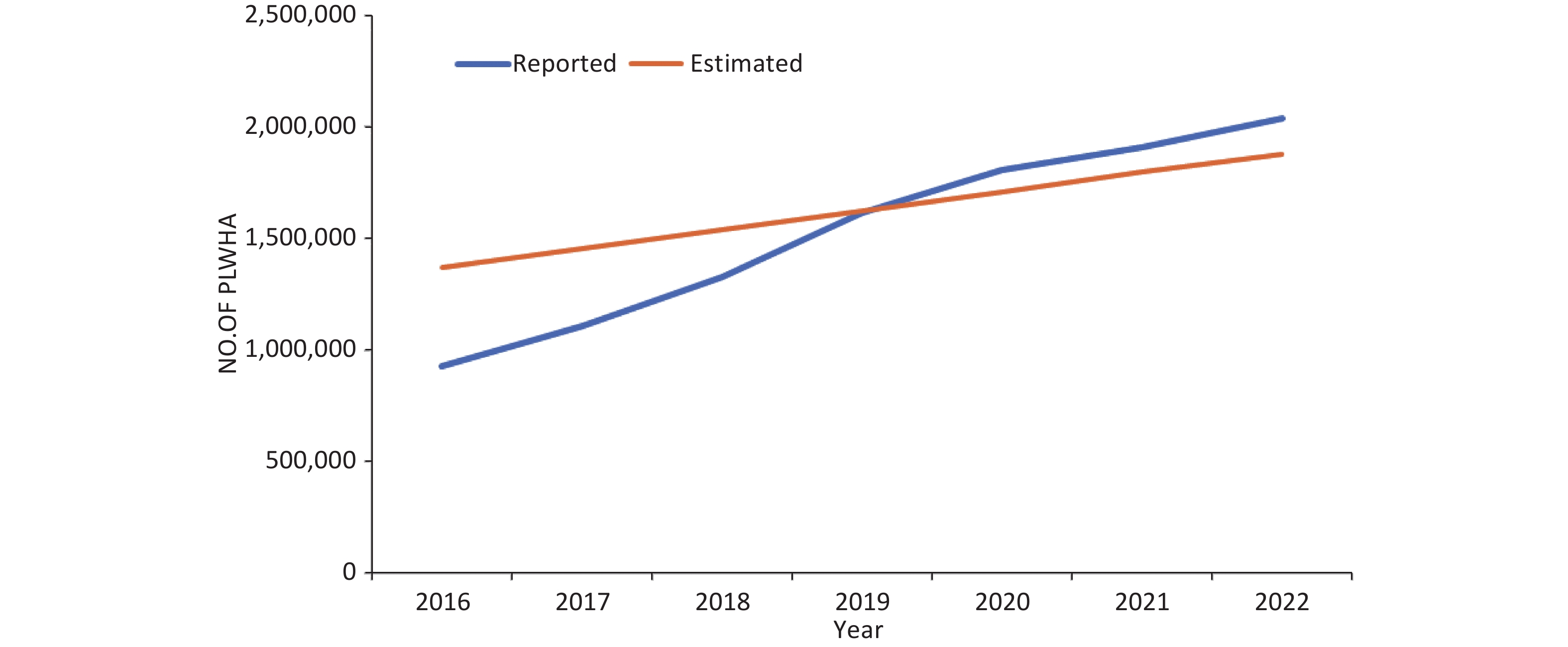
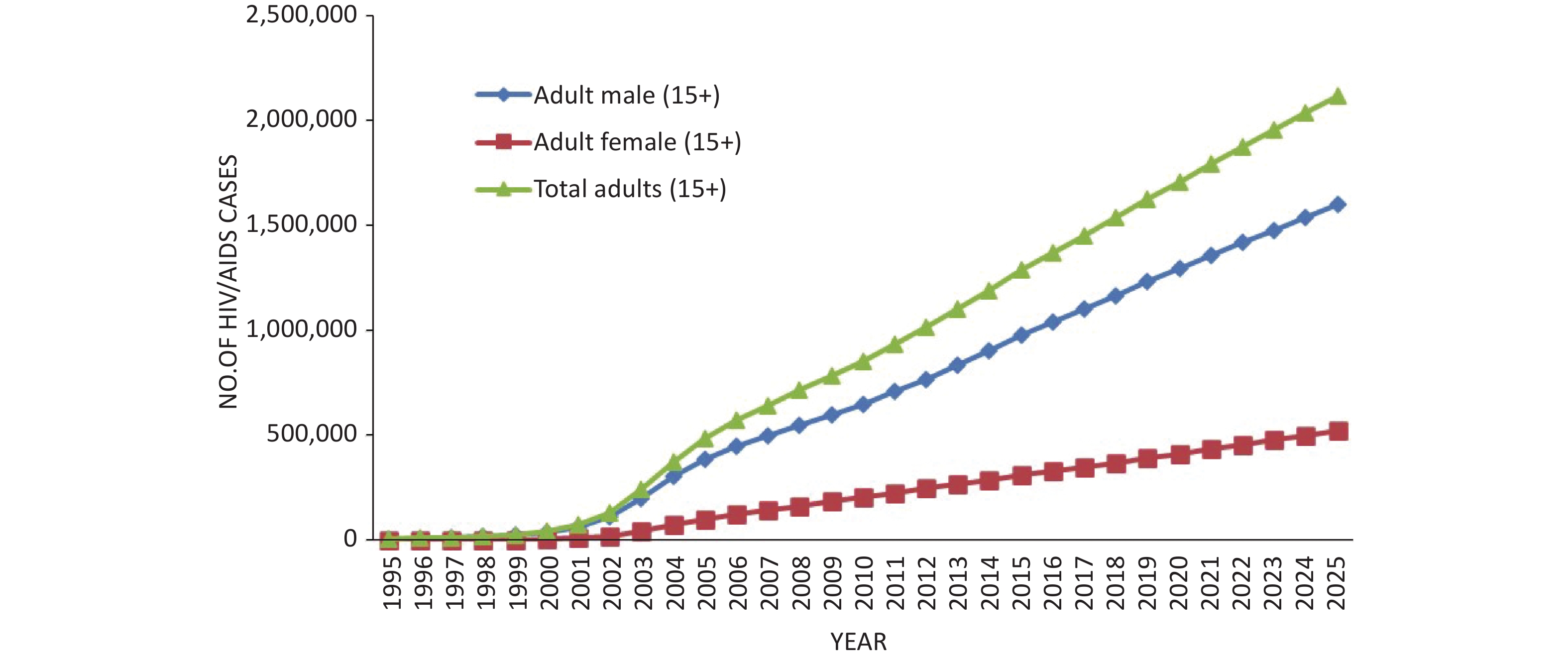
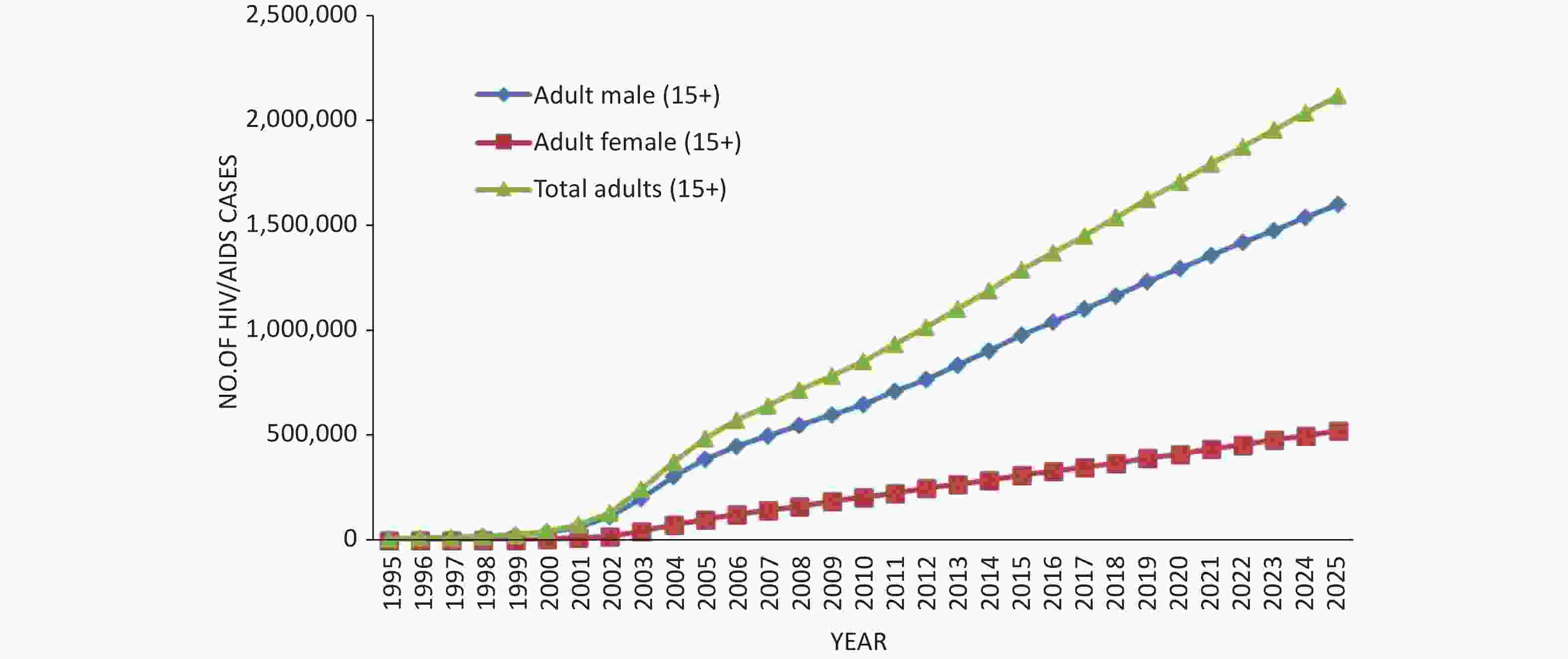
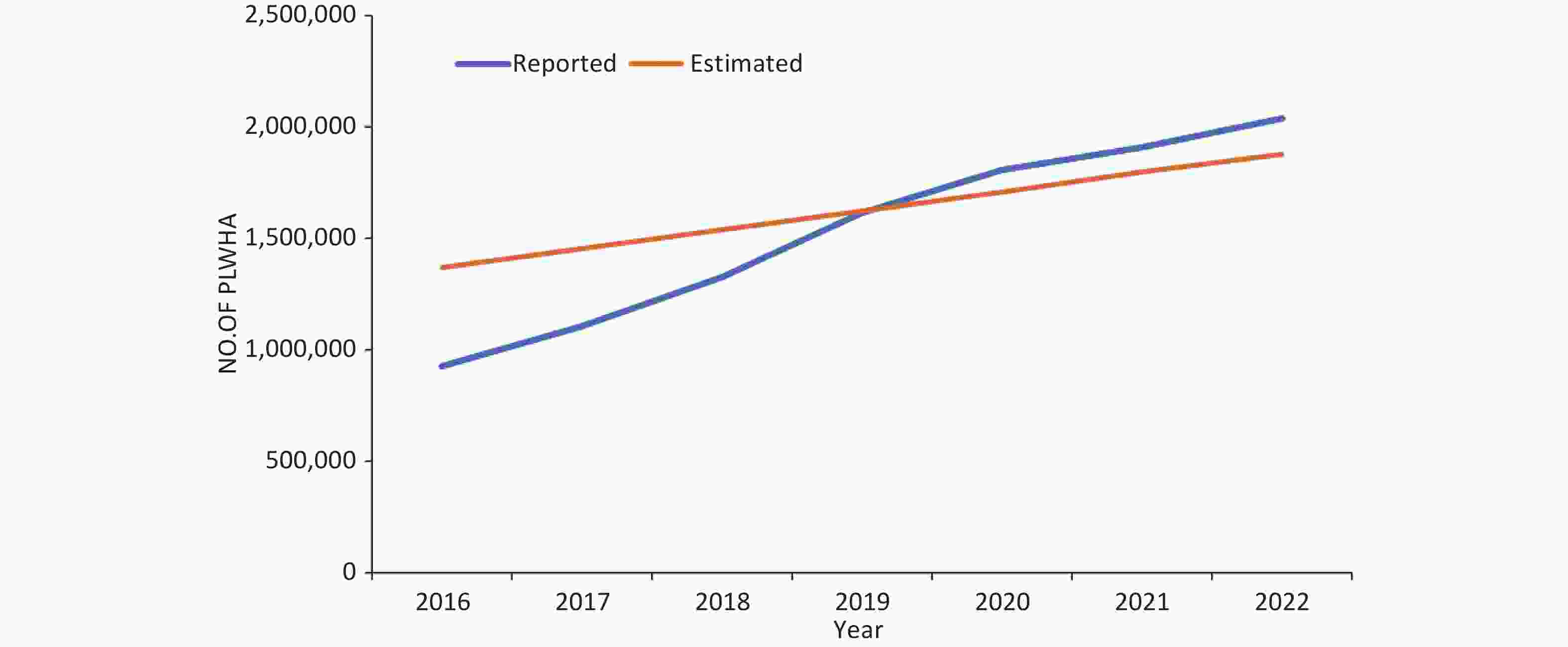
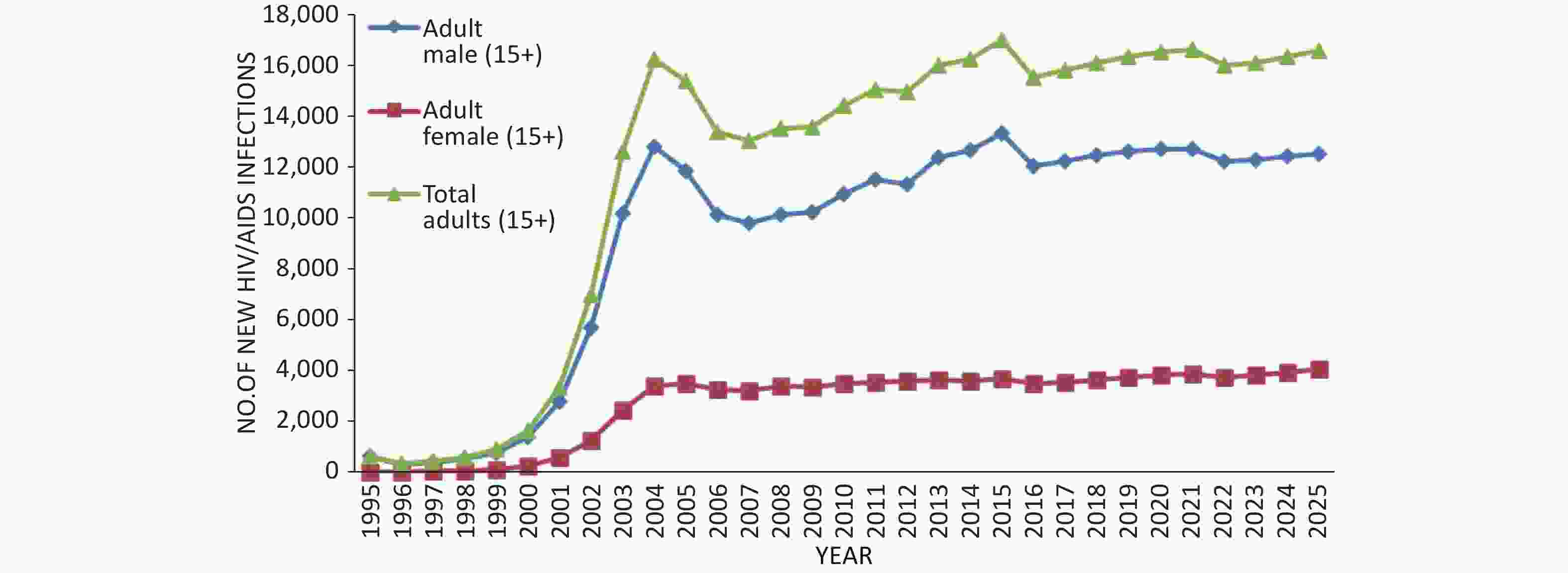
Dynamic HIV/AIDS trends with baseline prevention efforts induced behavioral changes: The onset of the HIV/AIDS epidemic in Sichuan is believed to have begun in the mid-1990s. The first HIV cases in this province were identified in 1995 among IDUs. In 2015, the prevalence of PLWHA in Sichuan increased to 0.191% (0.289% of men and 0.092% of women), with approximately 128,766 individuals (97,724 men and 31,042 women) identified as PLWHA. If behaviors are maintained at the current baseline levels, the prevalence of PLWHA is projected to increase to 0.306% by 2025 (0.460% for men and 0.150% for women). By 2025, the number of PLWHA is anticipated to reach 212,168 (159,970 men and 53,198 women) (Figure 1). The reported and estimated numbers of current HIV/AIDS infections in Sichuan Province are shown in Figure 2.
-
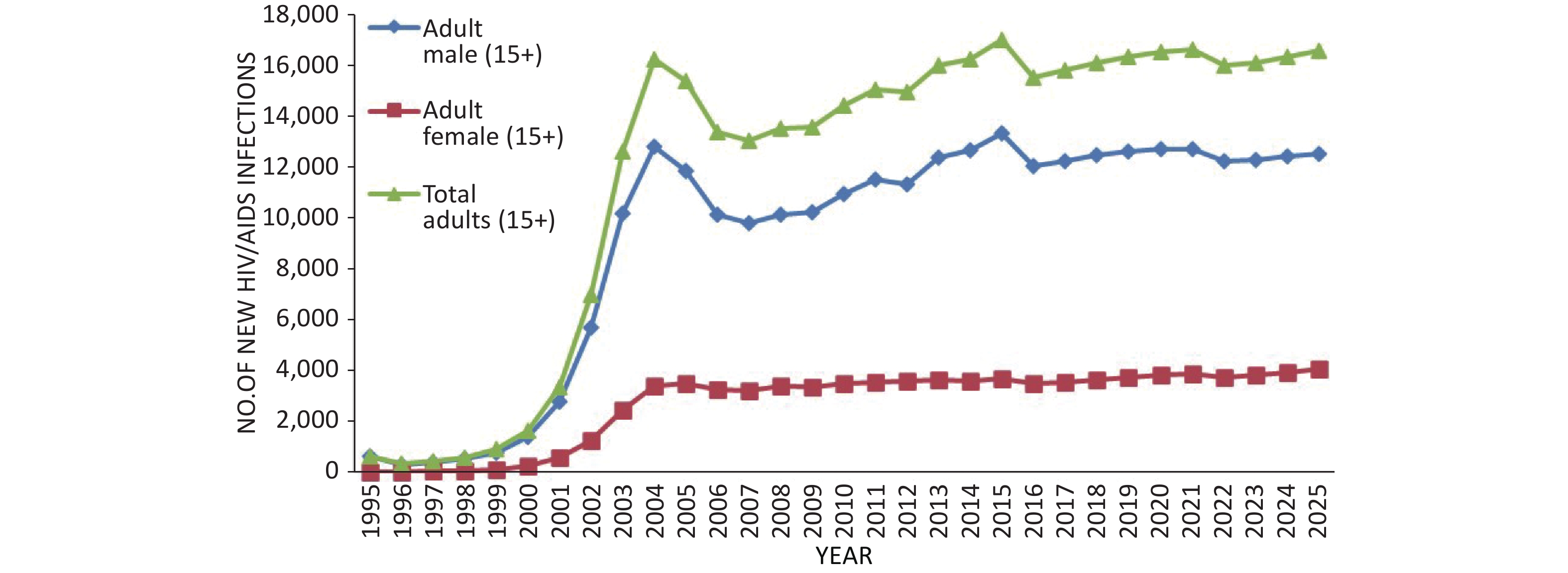
The number of new HIV infections in Sichuan Province rapidly increased from 1994, reaching a peak in 2004, followed by a slight decline. Subsequently, a slow rise occurred after 2007, followed by another gradual increase after 2015. Notably, the majority of patients with new infections were men (Figure. 3). According to the new infection rate of each population, the increase before 2004 was primarily attributed to the proliferation of injection drug use, while the subsequent gradual increase was mainly attributed to sexual transmission. The AEM predicted that the number of new HIV infections is expected to fluctuate from 2015 to 2025. By the end of 2025, 16,555 adults are anticipated to develop new HIV infections, including 12,507 men (75.55%) and 4,047 women (24.45%).
-
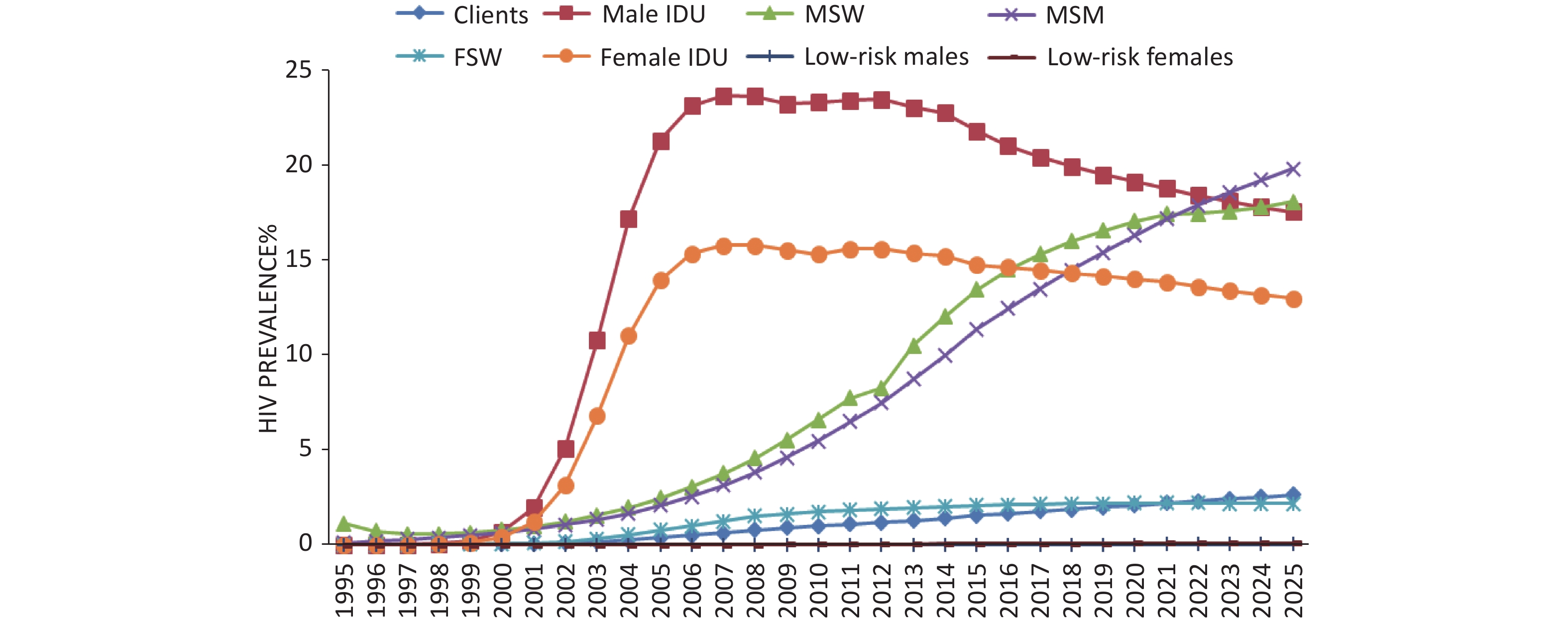
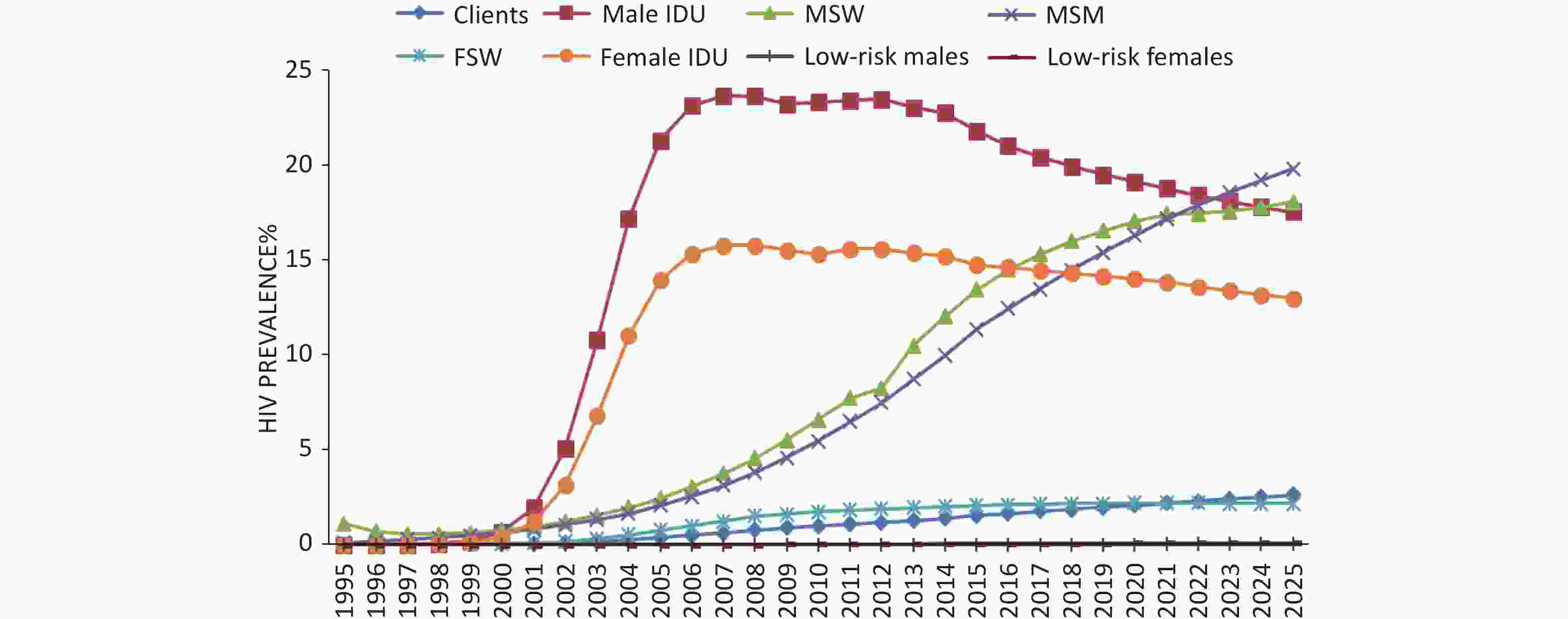
The HIV prevalence among male IDUs began to increase significantly in 1998, reaching approximately 21.82% in 2015. With current prevention efforts, the prevalence is predicted to decrease by 17.55% by 2025. The HIV prevalence rate among female IDUs reached an estimated 14.77% in 2015 and is predicted to gradually decline to 13.00% by 2025 (Figure 4).
Given the current rates of condom use, the HIV prevalence among MSM is expected to rise sharply from 11.38% in 2015 to 19.84% in 2025. Likewise, the HIV prevalence rate among clients of FSWs is expected to rapidly increase from 1.56% in 2015 to 2.64% in 2025. The prevalence rate among FSWs is predicted to slowly increase, from 2.08% in 2015 to 2.18% in 2025 (Figure 4).
-
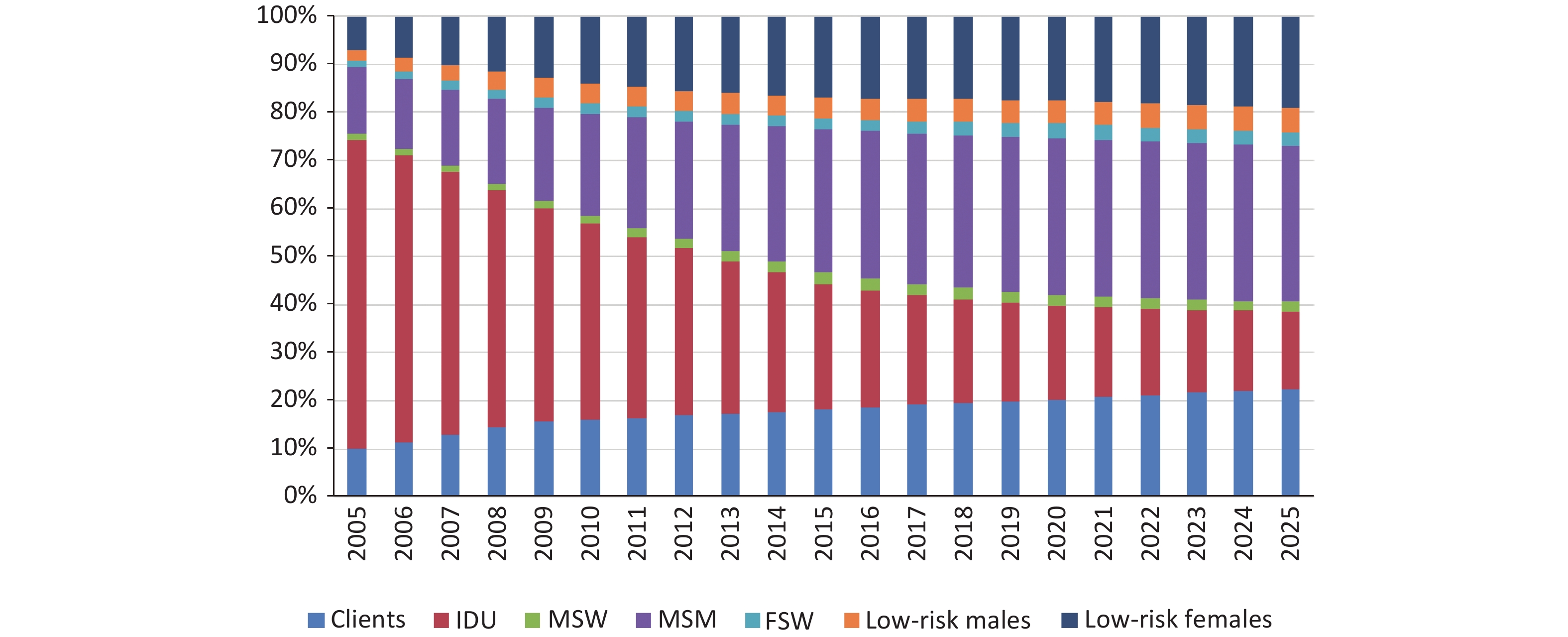
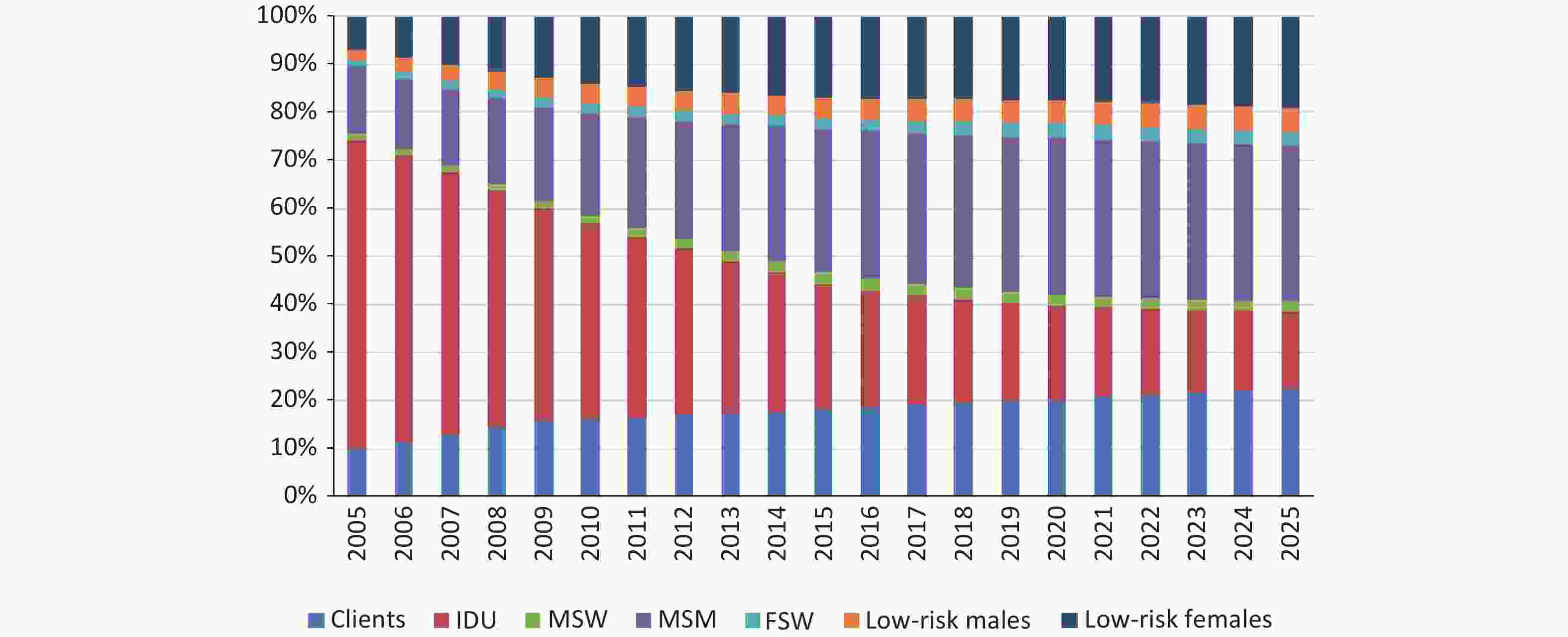
Within 20 years, the long-term trend of PLWHA in Sichuan indicated a gradual decrease in the prevalence of infections among IDUs (2025, 16.18%), while infections among MSMs sharply increased (2025, 32.44%). The prevalence of infections among FSWs exhibited a gradual increase (2.82%) in 2015, similar to that among the clients of FSWs (2025, 22.42%) and low-risk people (2025, 24.14%) (Figure 5). Heterosexual transmission, surpassing IDUs, is the predominant transmission route for HIV/AIDS, followed by homosexual transmission. HIV infection is spreading from high-risk groups to the general population.
In 2015, the AEM projected 16,983 new HIV infections, with MSM comprising the largest group (6,121, 36.04%), followed by IDUs (4,358, 25.65%), low-risk women (2,246, 13.22%), MSWs (1,645, 9.68%), clients of FSWs (1,590, 9.36%), FSWs (621, 3.65%), and low-risk men (404, 2.38%).
The AEM predicted a total of 16,555 new HIV infections by 2025. The primary group affected comprised MSM (4,625, 27.94%), followed by IDUs (4,150, 25.07%), low-risk women (2,269, 13.70%), MSWs (1,730, 10.45%), clients of FSWs (2,087, 12.60%), FSWs (1,151, 6.95%), and low-risk men (542, 3.27%).
The aforementioned results reveal distinct trends among MSM, FSW, and clients of FSWs. The number and proportion of new HIV infections among MSMs decreased, while those among FSWs and their clients increased. In low-risk populations, particularly among low-risk women, new HIV infections are predominant. The model shows that transmission is primarily attributed to sexual transmission between spouses, signifying the initiation of HIV infection spread from high-risk males men to low-risk women.
-
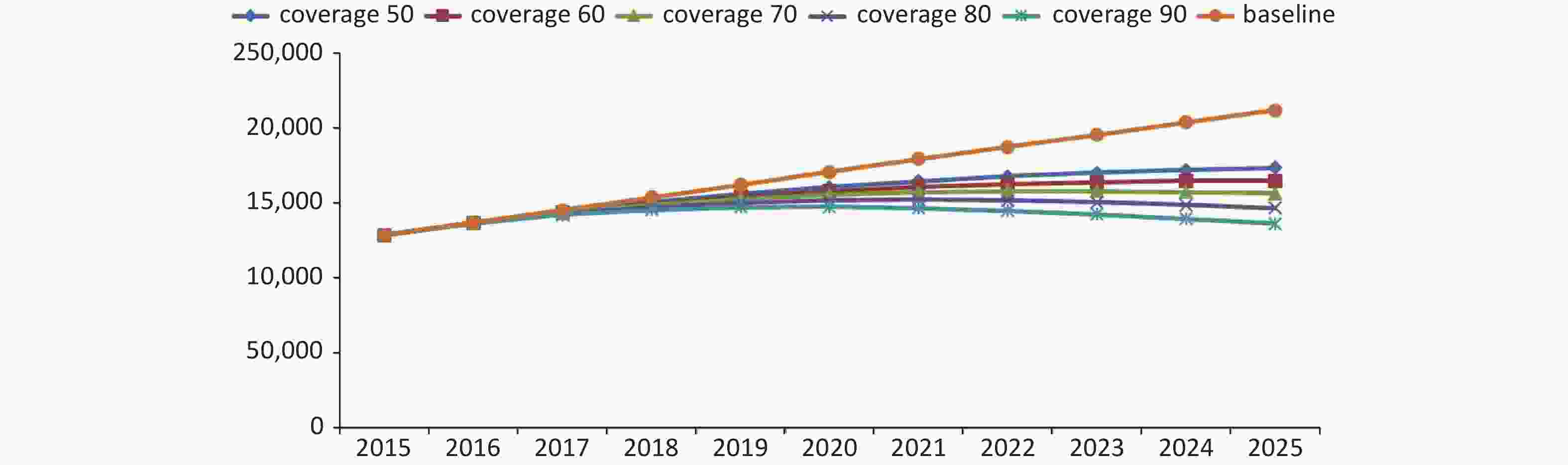
The existing intervention efforts will be intensified to make the comprehensive intervention coverage rates of all groups in Sichuan Province reach 50%, 60%, 70%, 80%, and 90% by 2025. This translates to increasing the rates of condom use to 75%, 80%, 85%, 90%, and 95%; the proportion of male IDUs who share needles to 25%, 20%, 15%, 10%, and 5%; the proportion of female IDUs who share needles to 15%, 10%, 10%, 5%, and 5%; the percentage of all injections shared (among those who share) to 50%, 40%, 30%, 20%, and 10%; and the STI% to 3%, 2.5%, 2%, 1.5%, and 1%.
Future scenarios with increased preventive efforts (comprehensive interventions): Assuming the current interventions remain unchanged, the model projects 16,555 new HIV infections by 2025. However, with a comprehensive intervention coverage rate of 50%, the model predicted a decrease in new HIV infections to 8,733, thereby preventing 7,822 new infections. At a comprehensive intervention coverage rate of 60%, the model predicted that the number of new HIV infections would stabilize at 7,016, avoiding 9,539 new infections. At a comprehensive intervention coverage rate of 70 %, the model predicted that the number of new HIV infections will decrease to 5,553, avoiding 11,002 new infections. At an 80% comprehensive intervention coverage rate, the model predicted that the number of new HIV infections will decline to 3,910, avoiding 12,645 new infections. At a 90% comprehensive intervention coverage rate, the model predicted that the number of new HIV infections would decline dramatically to 2,645, avoiding 13,910 new infections. Hence, elevating the comprehensive intervention coverage rate to more than 50% demonstrates a potential reduction in the trend of new HIV infections, with a more substantial decline as the intervention coverage rate increases (Figure 6).
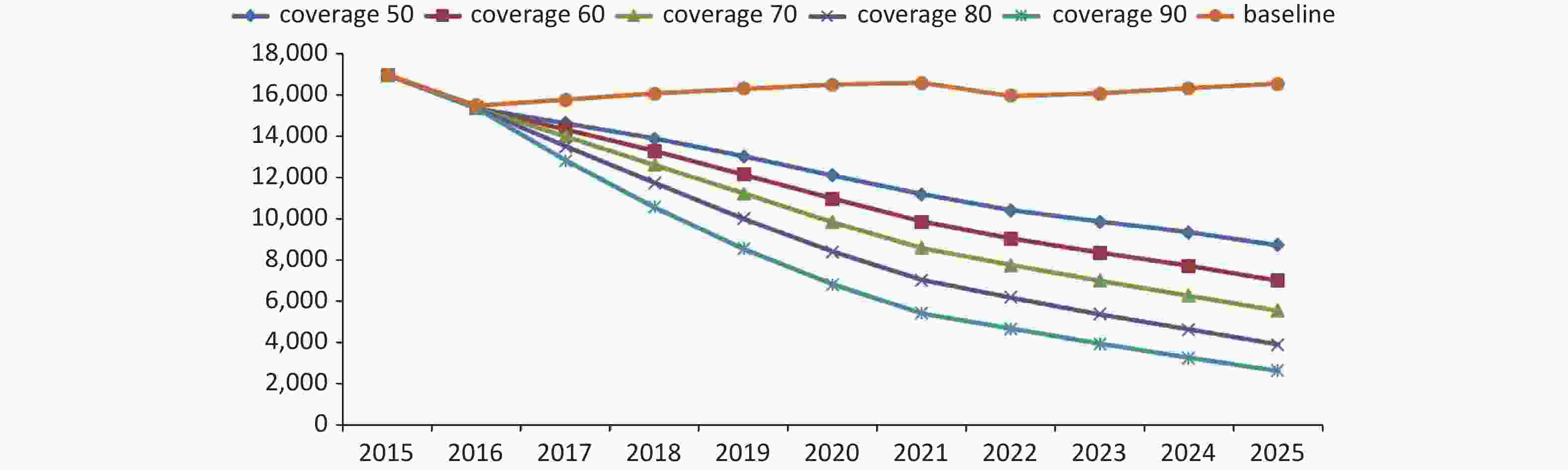
Figure 6. Changes in the number of HIV new infections under different intervention coverage from 2016 to 2025
According to the AEM model prediction, if the current interventions remain unchanged, the number of PLWHA will reach 212,168 by 2025 (Figure 7). At a comprehensive intervention coverage rate of 50%, the model predicted that the number of PLWHA will stabilize at 173,692, avoiding 38,476 PLWHA. At a 60% comprehensive intervention coverage rate, the model predicted that the number of PLWHA will stabilize at 164,923, avoiding 47,245 PLWHAs. At a comprehensive intervention coverage rate of 70%, the model predicted that the number of PLWHA will stabilize at 156,547, avoiding 55,621 PLWHAs. At an 80% comprehensive intervention coverage rate, the model predicted that the number of PLWHA will decline to 146,740, avoiding 65,428 PLWHAs. At a 90% comprehensive intervention coverage rate, the model predicted that the number of PLWHA will decline dramatically to 136,489, avoiding 75,679 PLWHAs, accompanied by a substantial reduction in HIV infection rates from 0.306% to 0.197%.
If the current intervention remains unchanged, the number of PLWHA in Sichuan Province will increase to 212,168 (prevalence: 0.306%) by 2025 according to the AEM model prediction. At a comprehensive intervention coverage rate of 50%, the number of PLWHA will continue to rise to 173,692 (prevalence: 0.250%). At a 60% comprehensive intervention coverage rate, PLWHA will reach an inflection point by 2025 (164,923, 0.238%) and then subsequently decline. At a comprehensive intervention coverage rate of 70%, the number of PLWHA will reach an inflection point in 2023 (158,200, 0.229%) and then subsequently decline. At an 80% comprehensive intervention coverage rate, the number of PLWHA will reach an inflection point in 2021 (164,923, 0.238%) and then decline.
In summary, achieving a comprehensive intervention coverage rate of more than 60% is needed to reverse the rising trend of PLWHA in Sichuan Province and reach a turning point of decline by 2025. To limit the number of PLWHA in Sichuan Province to 180,000 by 2025, the comprehensive intervention coverage rate should increase to more than 50%. To limit the number of PLWHA to 170,000 by 2025, the comprehensive intervention coverage should increase to more than 60%. To limit the number of PLWHA to 160,000 by 2025, the comprehensive intervention coverage rate should increase to more than 70%. To limit the number of PLWHA to 150,000 by 2025, the comprehensive intervention coverage rate must increase to more than 90%.
-
IDUs, FSWs, and MSMs are the main factors fueling the HIV/AIDS epidemics in various Asian countries and regions. As the disease progresses, FSWs contribute to the infection of clients, while IDUs transmit the infection to their heterosexual partners. This heterosexual transmission is a noteworthy component of the epidemic in this region[7]. According to the characteristics of the epidemic in Asia, Dr. Tim Brown and other foreign scholars developed the Asian AEM, which is suitable for the estimation and prediction of the HIV/AIDS epidemic in the clustered epidemic region of Asia[8].
At the end of 2015, data from the Sichuan report indicated the main transmission route of PLWHA was heterosexual, accounting for 57.06% of cases, followed by injection of drugs (25.31%) and homosexuality (12.31%). Since 2010, the newly reported rate of HIV/AIDS sexual transmission in Sichuan Province has surpassed that of drug injections as the primary transmission route. Therefore, the HIV epidemic in Sichuan Province is characterized by a clustered pattern with sexual transmission emerging as the main feature, which is suitable for the use of the AEM.
-
According to the AEM fitting results, the number of new HIV infections in Sichuan increased rapidly from 1994, peaked in 2004, experienced a slight decline, showed a gradual increase after 2007, and then declined again in 2015. By 2025, the number of PLWHA in Sichuan is projected to reach 212,168, while the HIV infection rate of the entire population in Sichuan is projected to increase to 0.306%. Analysis of the results revealed that the peak of new infections in 2004 was consistent with the peak of new infections among IDUs, while the peak of new infections in 2015 was consistent with the increase in new infections among MSMs, FSWs, and clients. The decline in the number of new infections after 2004 was largely due to the initiation of antiretroviral treatment. In Sichuan, free antiviral treatment was introduced in 2003, which has directly led to a decline in the number of new HIV infections in 2003. In 2004, the indication for free antiviral treatment was a CD4+T lymphocyte count of < 200; in 2012, the indication for treatment was changed to a CD4+T lymphocyte count of < 350; in 2015, the indication for treatment was further adjusted to a CD4+T lymphocyte count of < 500; and in 2016, the requirement for treatment based on CD4+T lymphocyte count was abolished. Treatment is now available for all individuals with HIV infection. Each change in the standard of care has led to a decline in the number of new infections. With the expansion of the coverage of antiviral treatment and the improvement in antiviral treatment effects in Sichuan, the viral load was effectively suppressed, the fatality rate of patients decreased, and the survival cycle was prolonged. Therefore, the number of new infections tended to stabilize; however, the number of PLWHA rapidly increased.
-
In 2015, the PLWHA population comprised 97,724 men (75.89%) and 31,042 women (24.11%). By the end of 2025, 159,970 men (73.51%) and 53,198 women (26.49%) are predicted to comprise the PLWHA population. The HIV infection rate in the entire population of Sichuan was higher in men than in women. Based on the projected infection rates for each population, the five groups with the highest HIV infection rates were male IDUs, MSMs, MSWs, female IDUs, and clients of FSWs, with four out of these five groups being men. As can be observed from the number of PLWHA, MSMs, IDUs, and clients of FSWs account for more than 70% of all infection cases. Therefore, we believe that HIV/AIDS infections primarily occur among men.
Based on the prediction results, the proportion of women infected is increasing, from 24.11% to 26.49%. Approximately 90% of new infections in women were observed among low-risk women, and more than 90% of new infections in low-risk groups occurred among women. According to the predicted results of transmission routes, the infection in newly infected low-risk women was primarily transmitted from one spouse to another. Based on these results, we believe that HIV infection in Sichuan is spreading from a high-risk male population to a low-risk female population.
-
The prediction results of the AEM show that among the PLWHA in Sichuan, the proportion of IDUs is decreasing, the proportion of MSMs is increasing, the proportion of FSWs and clients of FSWs is increasing, and the proportion of low-risk male and female heterosexual transmission is increasing. Therefore, heterosexual transmission has replaced the IDU as the primary route of infection.
-
If the comprehensive intervention coverage rates of FSW/IDU/MSM increase from the current situation to 50%, 60%, 70%, 80%, and 90%, respectively, in 2025, a total of 7,822, 9,539, 11,002, 12,645, and 13,910 new HIV infection and AIDS cases will be avoided, respectively. This could reduce the number of PLWHA to 38,476, 47,245, 55,621, 65,428, and 75,679, respectively, by 2025. If the intervention coverage rate is expanded to 90%, the HIV infection rates would be reduced from 0.306% to 0.197%.
If the coverage rates of clean needle exchange and methadone maintenance treatment increase to 14%, 18%, 22%, 26%, and 30% among IDUs, respectively, in 2025, a total of 1,486, 2,125, 2,606, 3,415, and 3,954 new HIV infections in the whole population could be avoided, respectively. Additionally, the number of PLWHA in Sichuan can be reduced by 5,576, 7,266, 8,381, 10,581, and 12,091, respectively, in 2025.
If the intervention coverage rates of MSM and MSW increase to 50%, 60%, 70%, 80%, and 90%, respectively, by 2025, and the condom utilization rates will increase to 75%, 80%, 85%, 90%, and 95%, respectively; hence, 4,260, 4,956, 5,604, 6,269, and 6,912 new HIV/AIDS infections in the whole population will be avoided, and 2,1841, 2,6482, 31,323, 36,602, and 42,860 PLWHA in Sichuan will be reduced.
In 2025, if the intervention coverage rates of FSW increase to 50%, 60%, 70%, 80%, and 90%, the condom use rates of FSWs and clients of FSWs will increase to 75%, 80%, 85%, 90%, and 95%, respectively. This will prevent 2,614, 3,034, 3,402, 3,797, and 4,175 new HIV infections in the whole population, and reduce 11,882, 14,502, 17,102, 19,811, and 22,821 PLWHA in the province, respectively.
In summary, improving the coverage rate of clean needle exchange and methadone maintenance treatment in IDUs and improving the condom utilization rate in MSMs, FSWs, and clients of FSWs are the most influential factors in predicting the continuous rising trend in the number of HIV/AIDS patients living in Sichuan Province from 2015 to 2025. Based on the above results, a comprehensive intervention targeting high-risk groups would yield the most significant impact if sufficient funds are available. In cases of limited funding, the primary focus should be on addressing male population behavior and implementing interventions for MSMs and MSWs. Strengthening interventions in these groups can effectively reduce the number of new HIV infections and cases of PLWHA. Following this, increased intervention among the FSWs is recommended; meanwhile, intensive intervention among the IDUs can reduce the number of HIV infections and cases. This analysis is rooted in the observation that HIV is primarily spread in Sichuan through sexual contact, making targeted interventions in this domain the most beneficial. Emphasizing the correct usage of condoms remains the most effective method of preventing the sexual transmission of AIDS.
-
According to the prediction results of the AEM, if the current intervention coverage rate remains unchanged, the number of PLWHA in Sichuan will continue to increase, reaching 212,168 (0.306%) by 2025. To alter the trajectory of increasing HIV prevalence in Sichuan Province and transition to a turning point of decline over the next decade, a comprehensive intervention coverage rate of more than 60% is essential for IDUs, MSMs, MSWs, and FSWs. If only the proportion of a single group increases, the intervention efforts will not be able to reverse the rising trend in Sichuan. To limit the number of PLWHA to 180,000 in Sichuan, it is imperative to either increase the comprehensive intervention coverage rate of the whole population to more than 50% or increase the condom use rate of the MSM/MSW population to more than 90%.
-
The results of this study underscore the potential impact of increasing the coverage of clean needle exchanges and methadone maintenance treatment among IDUs in reducing the number of new HIV infections and PLWHA in IDUs and the entire population. If the intervention coverage rate of needle exchange/methadone maintenance therapy among IDUs is increased to more than 14% (i.e., ensuring that the proportion of people who do not receive needle exchange or methadone treatment intervention is < 58%), 1,486 new HIV infections can be avoided, the number of PLWHA can be reduced to 5,576, and the number of new HIV infections in Sichuan will decrease annually.
Sichuan Province is close to the “Golden Triangle”. Drug traffickers have been using it as an important drug trafficking channel, a transit center, and an underground sales market from the “Golden Triangle” to the mainland due to its special geographical location. The results of this study also predicted that the largest proportion of new infections will continue to occur among drug users. Therefore, we suggest that Sichuan Province focus on IDUs, strengthen methadone maintenance treatment, improve the treatment coverage and maintenance rate of the IDU population, and improve community drug rehabilitation and referral mechanisms. Moreover, clean needles should be provided to drug users in areas where methadone replacement therapy is not available to reduce the risk of infection through needle sharing among drug users[9].
-
The prediction results show that the proportion of HIV infections among IDUs will decrease annually, whereas the proportion of HIV infections among MSM will increase annually. The majority of MSMs in Sichuan are young people, including male college and technical secondary school students[10]. They generally have a high willingness to accept AIDS prevention and intervention services and sufficient AIDS-related knowledge. In this population, after receiving a large number of AIDS awareness interventions, the condom utilization rate did not significantly improve[11], unsafe sex continued to exist among MSMs, and existing interventions failed to achieve the expected effect. Therefore, MSMs and MSWs will be key intervention groups in the future. Increasing the condom use rate in these groups will effectively control the number of newly infected HIV patients and PLWHA in Sichuan.
FSWs are a bridge group in the commercial sex service network, and the risk of HIV transmission is relatively high among IDUs, MSMs, clients of FSWs, and low-risk populations. Although the monitoring data show that the HIV-positive rate of FSW has remained low, ranging from 0.3% to 0.5%, the data may be more indicative of new infection rates rather than prevalence rates due to the influence of sampling points and the high mobility of the population sampled. After testing for HIV antibody positivity, FSWs choose to change prostitution venues or relocate to avoid potential isolation or the exposure of their privacy related to sexual services. The substantial mobility of this group presents challenges in monitoring. Thus, the annual rate of HIV infection detected at sentinel sites is likely reflective of the rate of new HIV infections among FSWs rather than its prevalence. BED capture-ELISA tests conducted by the Sichuan Center for Disease Control and Prevention[12] revealed fluctuating new infection rates of HIV-1 among FSWs between 0.09% and 0.51% from 2011 to 2015, a statistically significant difference. Similar results were confirmed by the new infection rate and sentinel monitoring of the incidence rate. Therefore, FSW should remain the focus of future interventions.
-
The results of the AEM in this study showed that the proportion of PLWHA (men and women) in Sichuan is increasing. At present, AIDS intervention work in Sichuan is mainly concentrated in the high-risk population; therefore, we believe that intervention work in the low-risk population needs to be strengthened. The primary infection routes in the low-risk population in Sichuan were through spousal and casual sexual transmission, often involving multiple sex partners.
The results of cohort studies in China showed that the transmission rate of HIV between couples of single-positive families was 30.0%, and the male-to-female transmission rate was higher than the female-to-male transmission rate[13]. Similar studies conducted both domestically and internationally have confirmed that the probability of sexually transmitted HIV from men to women is higher than that from women to men in couples of single-positive families[14,15]. This observation may be attributed to the higher HIV concentration in semen than in vaginal secretions or the differences in male and female genital anatomy, leading to more extensive and prolonged contact for women with the virus. AIDS prevention and control efforts should focus on male propaganda and interventions. The survey results of Sichuan Province indicate that the condom utilization rate of couples in single-positive families remains low. Only 32.35% of HIV-positive individuals consistently use condoms when engaging in sexual activities with a fixed partner or spouse, even after being informed of the infection[16]. Early notification of the spouse's infection is recommended. Some researchers have shown that spouses receiving notification services and HIV testing within 3 months can help reduce the risk of spousal transmission in couples with single-positive families[17]. In addition, regular follow-ups, guidance for infected people to use condoms correctly during sexual intercourse, and timely antiviral treatment of AIDS should be effective in reducing HIV transmission between spouses and sexual partners.
Liangshan Prefecture in Sichuan Province bears the most severe HIV/AIDS epidemic in the province and is home to the Yi ethnic minority group. In addition to Liangshan Prefecture, ethnic minorities such as Tibetans and Qiang in Ganzi and Aba Prefectures are prevalent in agricultural and pastoral areas, where non-commercial polysexual partners are more common. Owing to the relatively backward economy, limited healthcare infrastructure, low levels of public education, and language barriers in ethnic minority areas, it is difficult to implement effective public awareness campaigns and AIDS prevention efforts. Traditional health education has little effect on AIDS, and the public awareness rate of AIDS is relatively low. Some ethnic minority communities have relatively open attitudes toward sex. In some situations, such as ethnic traditional festivals, fairs, weddings, and funerals, people tend to have non-commercial and non-fixed sexual behaviors. The lack of condom availability and low utilization rates increase the risk of sexually transmitted diseases and AIDS transmission within these populations[18]. To address these challenges, it is recommended to engage local village doctors and community members as health education advocates in ethnic minority rural areas, conduct AIDS knowledge dissemination and promote the use of condoms among villagers, improve villagers’ awareness of AIDS and their self-protection ability, and strengthen awareness of condom use. In addition, the availability and accessibility of condoms should be ensured, and free condom self-collection points should be established in places where villagers gather, such as village activity rooms and clinics. Thus, condom access can be enhanced, condom use can be increased, and sexual transmission of AIDS can be reduced.
In addition, the active development of personalized intervention software is an important intervention measure for preventing HIV infection in the future, especially in low-risk groups. Combining the insights gained from the AEM with the development of personalized software based on different risk areas holds the potential for achieving enhanced and more comprehensive protection for low-risk groups.
-
The results of this study showed that the case fatality rate of AIDS will decrease annually from 2015 to 2025, which also reflects the effectiveness of current HIV antiviral treatment. Currently, highly active antiretroviral therapy (HAART) is the most effective AIDS treatment worldwide. Cohort studies[19] have shown that HAART effectively reduces mortality and prolongs survival. Clinical studies[20] have shown that HAART can effectively increase the number of CD4+T lymphocytes and reduce the viral load. Sichuan Province began implementing free antiviral treatments in 2003. The indications for receiving free treatment include a CD4+T lymphocyte count of < 200 in 2004, a CD4+T lymphocyte count of < 350 in 2012, and a CD4+T lymphocyte count of < 5 00 in 2015. The CD4+T lymphocyte criterion was eventually abolished in 2016, and the number of people receiving ART treatment increased. The results of the AEM also suggest that an increase in the number of people treated with ART and the treatment coverage rate can promote a decrease in the number of new HIV infections; the greater the number of people treated, the greater the decline. ART effectively suppresses the viral load and reduces infectivity, thereby reducing the number of new infections. With the change in CD4+T lymphocyte treatment standards, the number of people requiring treatment increases. In addition to newly infected people with HIV, PLWHA who do not meet the criteria for CD4+T lymphocyte treatment will become the target of antiviral treatment, underscoring the considerable treatment gap that persists. Therefore, it is necessary to strengthen the monitoring and testing in Sichuan Province to increase the proportion of HIV-infected persons and patients, strengthen departmental coordination, expand ART coverage of antiretroviral treatment, and increase the number of people receiving antiretroviral treatment.
-
Our study summarizes the current situation and dynamic trends of the AIDS epidemic in Sichuan Province. The AEM was used to fit the historical trend curve of the HIV epidemic as a baseline to explore future intervention options. Based on the current high-risk behaviors, heterosexual transmission will become the primary method of HIV transmission in Sichuan Province, the incidence of AIDS will remain stable, and the prevalence will increase in the future. This study has important implications for alleviating the spread of AIDS in Sichuan. Comprehensive intervention measures for high-risk groups are effective.
-
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
-
This work was funded by the Humanities and Social Sciences Research Project of Ministry of Education of China (Grant ID: 18YJA840018).
Projecting the Dynamic Trends of Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome: Modeling the Epidemic in Sichuan Province, China
doi: 10.3967/bes2024.080
- Received Date: 2023-11-23
- Accepted Date: 2024-02-26
-
Key words:
- HIV/AIDS /
- AIDS Epidemic Model /
- Heterosexual transmission /
- Sichuan province
Abstract:
The authors declare that they have no competing interests.
| Citation: | LI Yuan, LIU Qin Xi, LUAN Rong Sheng, YANG Yi, WU Tao, YANG Bi Hui. Projecting the Dynamic Trends of Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome: Modeling the Epidemic in Sichuan Province, China[J]. Biomedical and Environmental Sciences. doi: 10.3967/bes2024.080 |







 Quick Links
Quick Links
 DownLoad:
DownLoad: