-
Between 1990 and 2021, the proportion of global disability-adjusted life years attributed to mental disorders increased from 3.46% to 5.38%, making it one of the top 10 leading causes of the global burden[1]. The World Health Organization has listed anxiety disorders, including obsessive-compulsive disorder (OCD), as the sixth largest contributor to nonfatal health loss globally[2,3]. OCD is a mental and behavioral condition in which a person experiences intrusive thoughts (obsessions) and feels compelled to repeatedly perform certain rituals (compulsions) to alleviate the distress caused by the obsession[4]. Cognitive-behavioral theories suggest that OCD can often lead to an increase in anxiety or a sense of discomfort, resulting in a more extensive disease burden[5].
Previous observational studies suggested that body composition, such as body mass index (BMI), was linked to several psychiatric disorders[6-8]. Notably, individuals with OCD may tend to have lower rates of obesity and excess weight[9,10], and conversely, the prevalence of OCD is relatively low in obese individuals[11]. Several studies suggest that in addition to BMI, more attention should be given to indicators such as fat distribution, as these indicators may have superior predictive value[12,13]. However, the causal relationship and direction between fat mass (FM) and OCD remain unclear, and the results of observational studies may be influenced by confounding bias or reverse causality factors[9]. Fortunately, emerging genomics studies have allowed us to infer their causality by leveraging the Mendelian randomization (MR) approach. As the genetic variants are randomly allocated at conception, MR analysis could overcome the underlying reverse causation and confounding, similar to a randomized controlled trial.
In this study, we utilized the two-sample MR approach[14], which is based on publicly available summary statistics, to infer the causal association between genetically predicted FM and OCD, providing new insights into preventing psychiatric disorders.
-
We used summary statistics from publicly available genome-wide association studies (GWASs) to conduct two-sample MR analyses. We aimed to evaluate whether there was a causal association between FM and OCD. MR analysis relies on the following three assumptions: (1) instrumental variables (IVs) are strongly correlated with exposure; (2) IVs are not related to the confounding factors affecting the “exposure-outcome” pathway; and (3) IVs affect outcomes solely through the exposure variable.
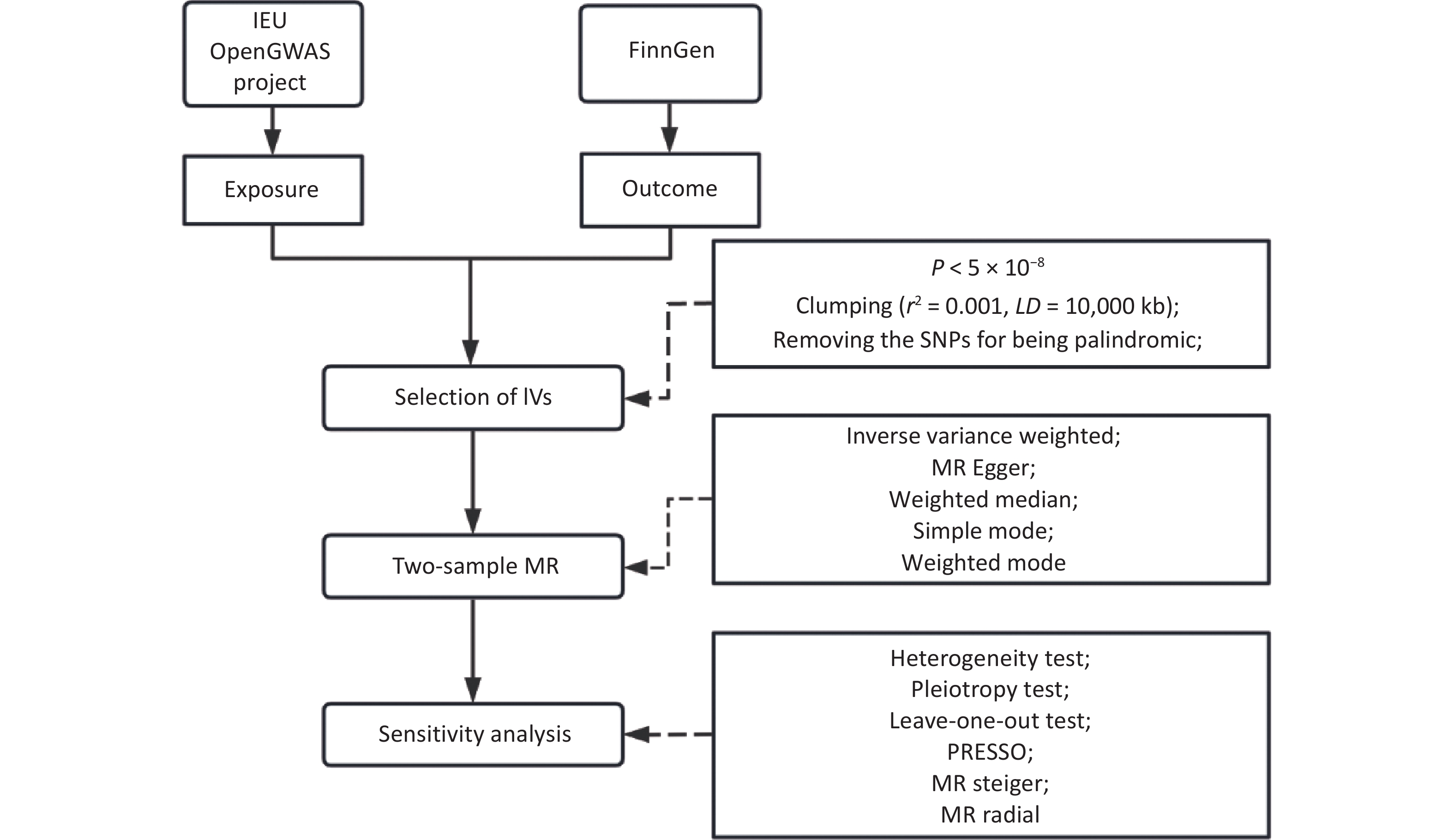
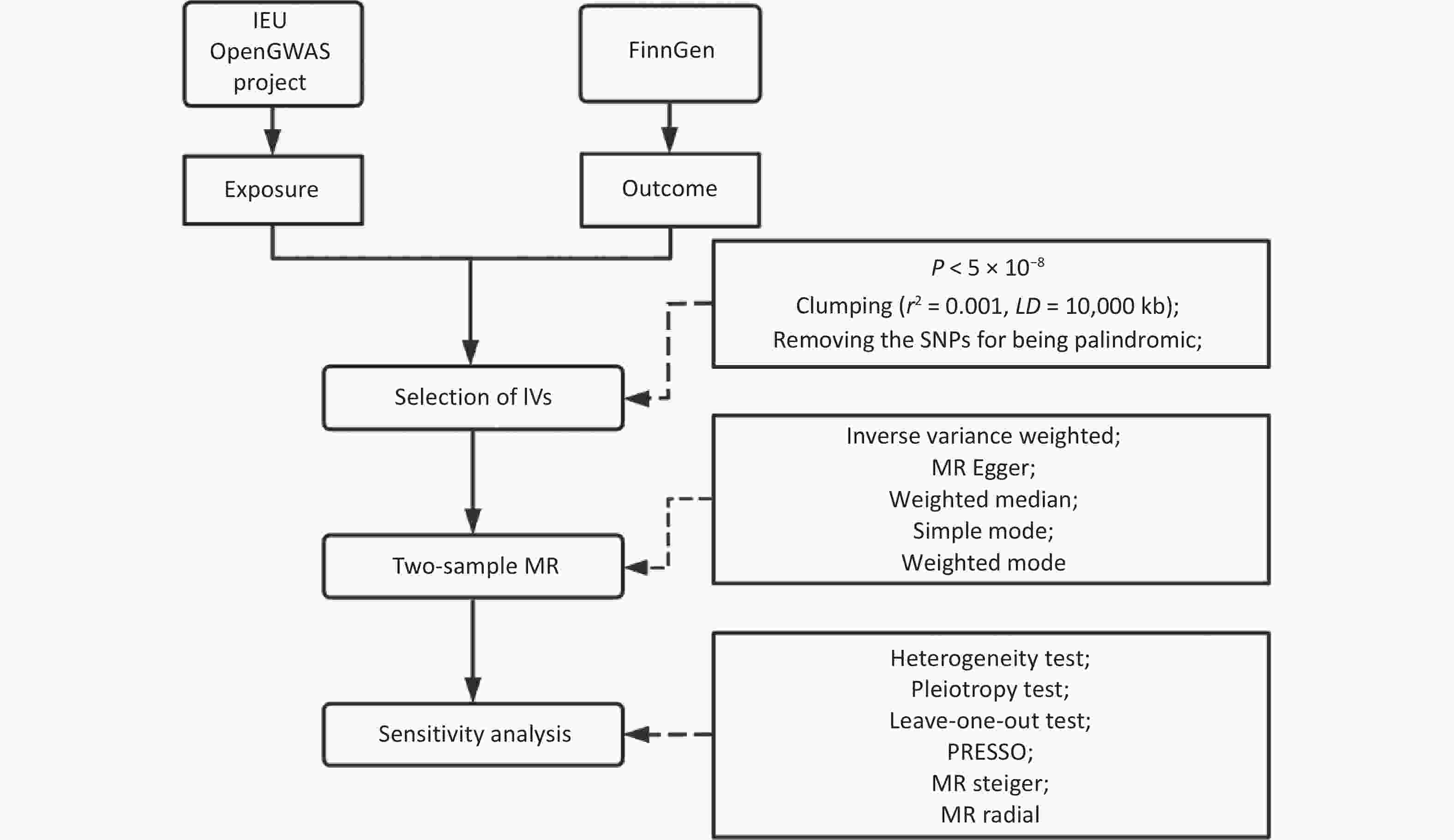
We searched for and retrieved the summary statistical data of the exposure and outcome variables from the IEU Open GWAS project and the FinnGen consortium. We selected single nucleotide polymorphisms (SNPs) that were independently associated with exposure at genome-wide significance levels (P < 5×10-8, r2 < 0.001 within a 10,000 k-base-pair window). Subsequently, palindromic SNPs were removed. Two-sample MR was then conducted using five methods to estimate causality. Multiple corrections were conducted for the primary analysis. Heterogeneity tests, pleiotropic tests, leave-one-out tests, MR pleiotropy residual sum and outlier (MR-PRESSO) tests, MR Steiger tests of directionality, MR radial tests, and sensitivity analyses were also performed to test the robustness of the causality results, as shown in Figure 1 for the technical roadmap. In addition, given that the education variable strongly predicted FM, fat-free mass (FFM), and body fat percentage (BF%), we performed sensitivity analyses after excluding SNPs associated with education (P < 5×10−8). The reverse causality between FM and OCD was further explored.
-
Our study obtained summary statistics from GWASs conducted by various international consortiums involving all participants of European ancestry. The available summary statistics for both sexes were combined. We chose the most recent GWAS with the largest sample size for the primary analysis and the other for the sensitivity analysis (Table 1).
Phenotype GWAS ID Consortium Sample size, n SNPs, n Year ICD-10 Total Case Control Exposure FM ukb-b-19393 MRC-IEU 454,137 − − 9,851,867 2018 − FM * ukb-a-265 Neale Lab 330,762 − − 10,894,596 2017 − FFM ukb-b-13354 MRC-IEU 454,850 − − 9,851,867 2018 − FFM * ukb-a-266 Neale Lab 331,291 − − 10,894,596 2017 − BF% ukb-b-8909 MRC-IEU 454,633 − − 9,851,867 2018 − BF% * ukb-a-264 Neale Lab 331,117 − − 10,894,596 2017 Education ebi-a-GCST90029012 − 470,941 − − 11,972,619 2018 Outcome OCD finn-b-F5-OCD FinnGen 339,539 1,962 337,577 16,380,384 2021 ICD-10 F42; ICD-9 3003; ICD-8 3003 OCD * ieu-a-1189 PGC 9,725 2,688 7,037 8,409,517 2017 DSM-IV Note. *: The summary statistical data were utilized for the sensitivity analyses. All the populations were of European ancestry and included males and females; SNP, single nucleotide polymorphism; FM, fat mass; FFM, fat-free mass; BF%, body fat percentage; OCD, obsessive-compulsive disorder; MRC-IEU, MRC Integrative Epidemiology Unit; PGC, The Psychiatric Genomics Consortium; ICD, The International Statistical Classification of Diseases and Related Health Problems. DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, 4th edition. Table 1. Summary of genome-wide association studies used in the present study
The selection of exposure-associated SNPs for genetic instruments was based on GWAS searches in the IEU Open GWAS project[15,16]. The GWAS data from the MRC-IEU and Neale Lab were output from the GWAS pipeline using Phesant-derived variables from the UK Biobank[17]. All three exposure phenotypes were continuous variables measured by a bioelectrical impedance analyser[18].
SNPs with genome-wide significant (P < 5×10-8) associations with exposure phenotypes were selected. The variants were subsequently pruned by linkage disequilibrium (r2 < 0.001 within 10,000 k-base-pair windows). The F-statistic was applied to evaluate the instrument strength. SNPs with an F-statistic greater than 10 were considered strong instruments[19]. No weak instrumental variables were found among the above. After excluding the palindromic sequence, 396, 512, and 367 independent SNPs were identified as IVs for FM, FFM, and BF%, respectively.
Genetic variants associated with OCD were obtained from the FinnGen consortium[20] and the PGC consortium[21]. In the FinnGen consortium, OCD was diagnosed according to the International Statistical Classification of Diseases and Related Health Problems 9th and 10th Revision. All patients from the PGC met the Diagnostic and Statistical Manual of Mental Disorders 4th edition[21]. The median age at first onset of OCD was 24.94 years. There was no overlap between the participants in the exposure and outcome studies.
We used publicly available summary data for which no additional ethical committee approval or participant informed consent was needed. The checklist for strengthening the reporting of observational studies in epidemiology using MR (STROBE-MR) was followed (Supplementary Table S1)[22].
-
After selecting the IVs, we implemented two-sample MR based on five analytical approaches: inverse variance weighted (IVW), MR-Egger, weighted median, simple mode, and weighted mode methods. IVW served as the primary estimator because it yields the most efficient pooled estimate under the assumption of either no directional pleiotropy or balanced pleiotropy across variants. The MR-Egger method incorporates an intercept term to identify and correct unbalanced pleiotropy, while it may be biased and inflated Type I error rates[23]. The weighted median method provides a consistent causal effect when at least 50% of the total weight derives from valid instruments, thereby tolerating a substantial proportion of invalid SNPs[24]. The simple and weighted mode estimators rely on the zero-modal pleiotropy assumption and provide a consistent causal estimation if the largest group of SNP-specific estimates originates from valid instruments[25]. Given its superior statistical power, IVW estimates were regarded as the primary results, with the other four methods serving as sensitivity analyses[25,26]. The Wald method and delta approach were utilized to estimate the causal ratio and confidence interval (CI) of the single IV, respectively. The effect of each SNP is weighted by the inverse of the variance of the ratio estimator. The results of the IVW method were corrected by the false discovery rate (FDR) and Bonferroni method. The association between the exposure variables and OCD with a P value < 0.05/3 = 0.0167 (Bonferroni correction for multiple testing) was considered significant.
Heterogeneity tests, pleiotropy tests, leave-one-out tests, and sensitivity analyses were performed to evaluate the robustness of the findings. The Cochran’s Q test was used to determine the heterogeneity between the causal estimates of different genetic variants[27]. The MR-PRESSO test and the slope of the MR‒Egger regression were applied to monitor the potential horizontal pleiotropy effect[28]. The MR Steiger test of directionality was performed to validate the direction of the association between exposure and OCD. The MR radial method[29] detected outliers, which were then excluded from the sensitivity analysis. In addition, the summary statistics of different data sources were used to examine the robustness of the primary results.
All analyses were performed using R software (version 4.2.3, R Foundation for Statistical Computing, Vienna, Austria). “TwoSampleMR”[15], “MR-PRESSO”[28], “RadialMR”[29], “ggplot2” and other software packages were utilized for statistical analysis and visualization. P < 0.05 was considered to indicate statistical significance.
-
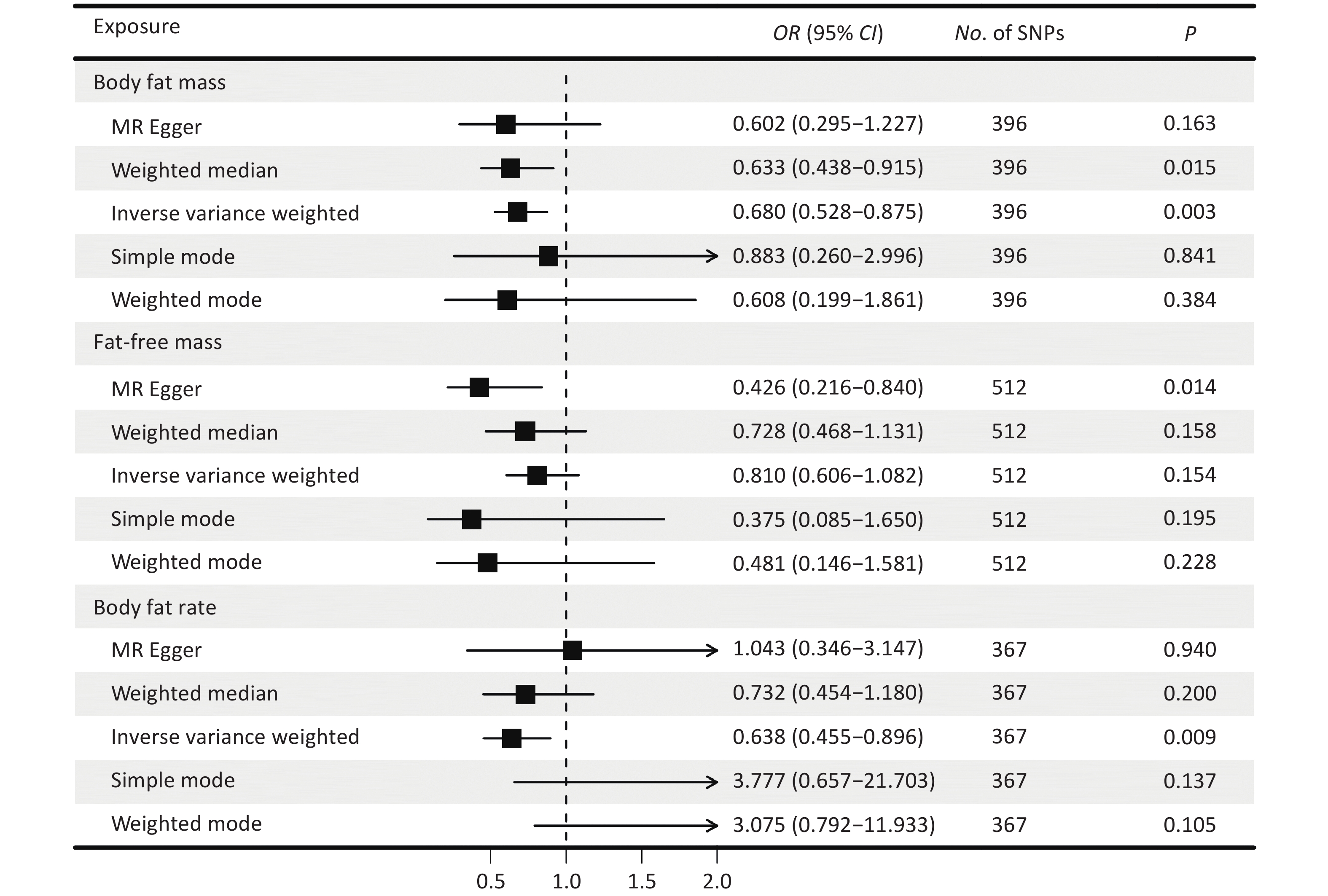
The F-statistic of each SNP was greater than 10 (Supplementary Table S2-S4). Figure 2 presents causal estimates across five MR methods, which collectively address heterogeneity and horizontal pleiotropy. The results of the IVW method showed that a genetically predicted decrease in FM was associated with an increased risk of OCD [odds ratio (OR) = 0.680, 95% CI: 0.528–0.875, P = 0.003] (Figure 2). Broadly consistent risk estimates were obtained using the weighted median approach (OR = 0.633, 95% CI: 0.438–0.915, P = 0.015), and the directionally same estimates were observed for the other methods. The causal effect of FM on OCD risk was consistent after Bonferroni correction and FDR correction (Table 2). The funnel plots and scatter plots for the causal effects of FM, FFM, and BF% on OCD are shown in Figure 3 and Supplementary Figure S1.
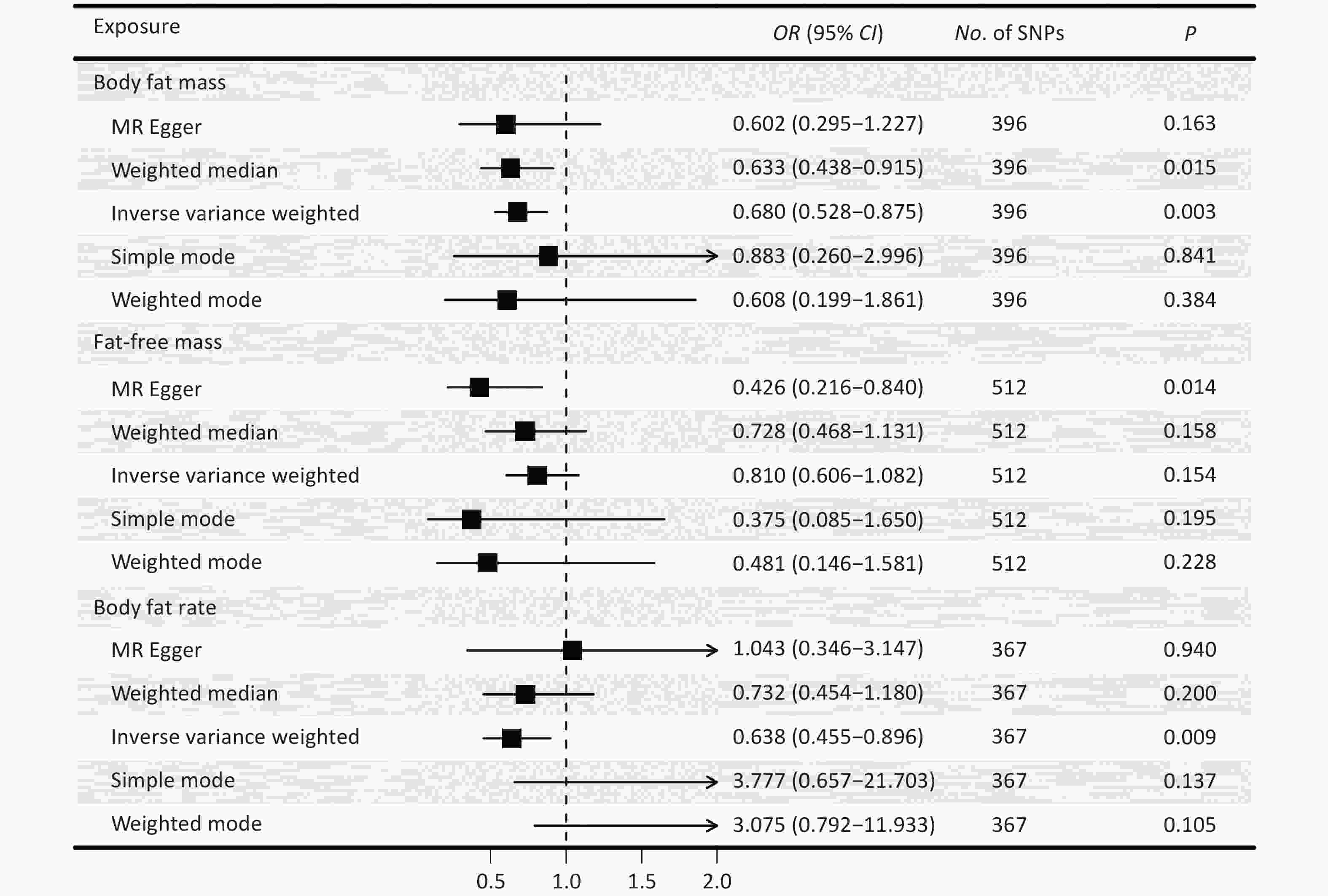
Figure 2. The causal effects of body fat mass, fat-free mass, body fat percentage and obsessive-compulsive disorder derived from five Mendelian-randomization methods. OR, odds ratio; CI, confidence interval; P, P value. SNP, single nucleotide polymorphism; MR, Mendelian randomization. The results of the IVW method were reported in the figure. The results of MR-Egger, weighted-median, simple mode, and weighted mode estimates provided as sensitivity checks for horizontal pleiotropy and instrument heterogeneity.
Exposure SNPs, n OR (95% CI) P value FDR P value Fat mass 396 0.680 (0.528, 0.875) 0.003* 0.008 Fat-free mass 512 0.810 (0.606, 1.082) 0.154 0.154 Body fat percentage 367 0.638 (0.455, 0.896) 0.009* 0.014 Note. IVW, inverse variance weighted; SNP, single nucleotide polymorphism; OR, odds ratio; CI, confidence interval; FDR, false discovery rate. *: The P value was still significant after Bonferroni correction. Table 2. The causal effects between body fat mass, fat-free mass, body fat percentage and obsessive-compulsive disorder (IVW method)
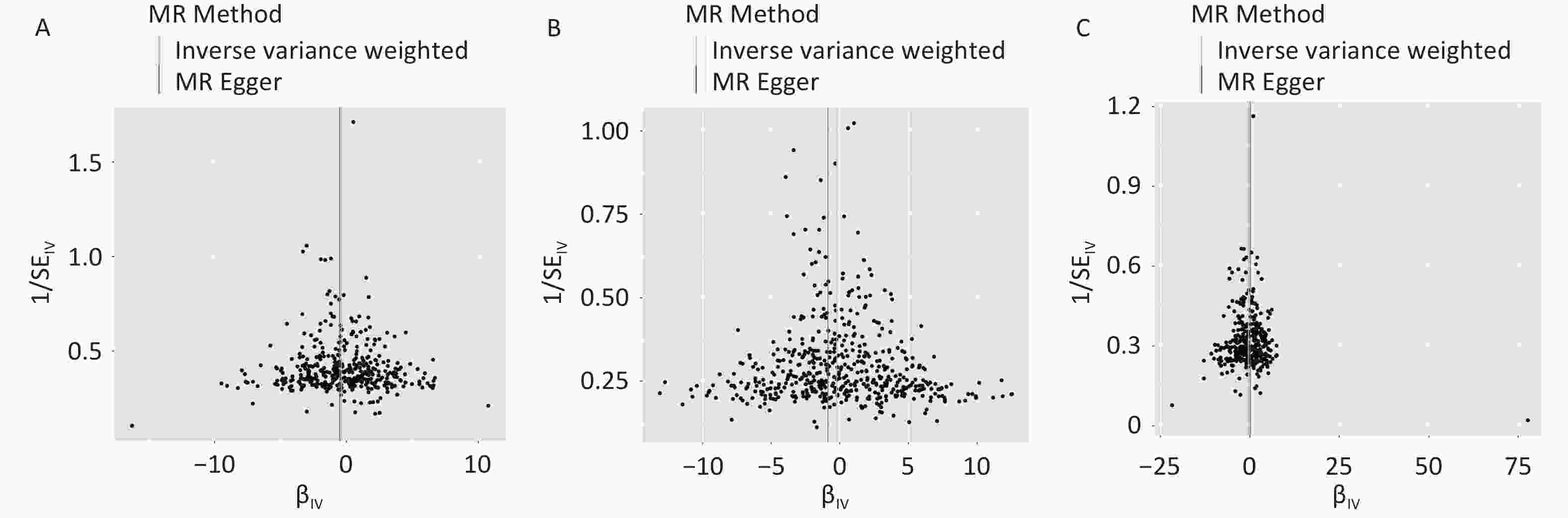
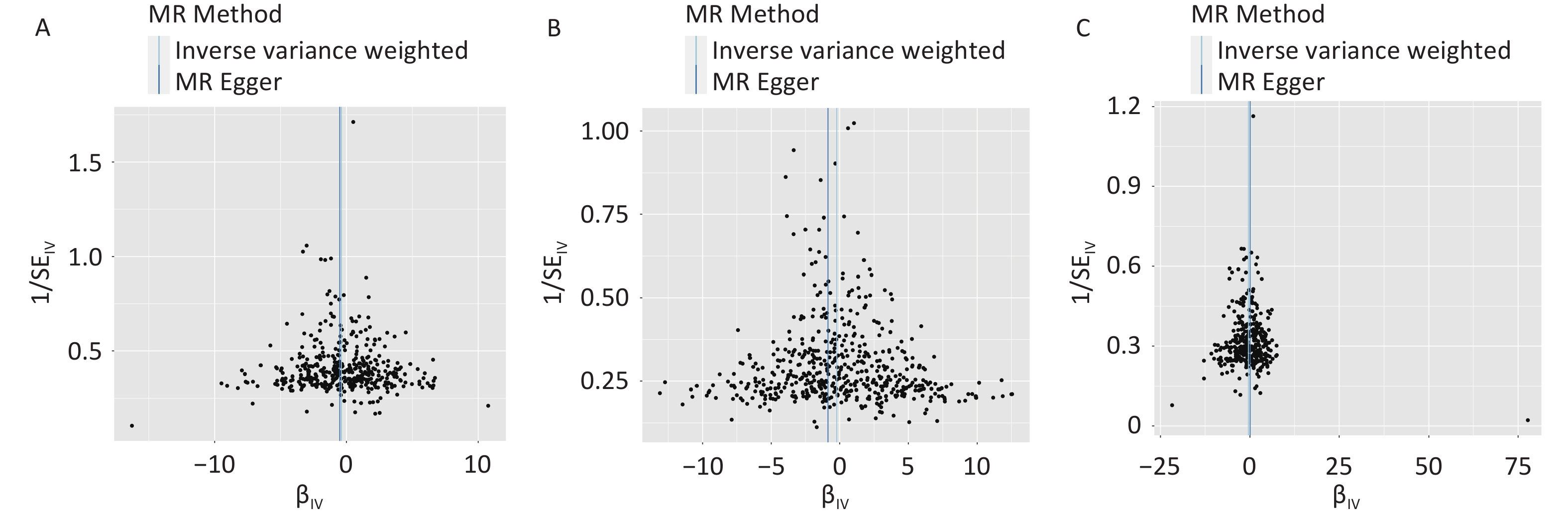
Figure 3. Funnel plot for the causal effects of (a) body fat mass, (b) fat-free mass, and (c) body fat percentage on obsessive-compulsive disorder. IV, instrumental variable; SE, standard error. MR, Mendelian randomization.
The results of MR‒Egger showed that a genetically predicted decrease in FFM was significantly associated with a greater risk of OCD (OR = 0.426, 95% CI: 0.216–0.840; P = 0.014). However, the other four methods showed no significant causal associations (Figure 2, Supplementary Table S5). According to the IVW estimate, with a per standard deviation (SD) increase in the genetically predicted level of BF%, the risk of OCD decreased by 36.2% (OR = 0.638, 95% CI: 0.455–0.896, P = 0.009). The estimates of the other four methods were not significant.
-
We conducted a series of sensitivity analyses to assess heterogeneity and pleiotropy (Supplementary Table S5). The Cochran’s Q test suggested the existence of heterogeneity in FM (P < 0.001), FFM (P = 0.003), and BF% (P = 0.002). Therefore, the random effect model was employed to estimate the effect size (Supplementary Table S6). Similar effect sizes as the primary finding were obtained from the random effects models (FM: OR = 0.680, 95% CI: 0.528–0,875, P = 0.003; BF%: OR = 0.638, 95% CI: 0.455–0.896, P = 0.009).
The pleiotropy test by MR‒Egger intercept suggested the existence of pleiotropy of FFM (P = 0.041). The intercepts from the MR‒Egger regression analysis of FM (P = 0.720) and BF% (P = 0.360) did not reach statistical significance, suggesting that there was no apparent evidence of pleiotropy.
According to the leave-one-out test, all the estimates had the same effect direction, indicating robust results (Supplementary Figures S2-4). The MR-PRESSO global test results showed horizontal pleiotropy; however, no outliers were detected. In addition, the correct causal direction was confirmed using the MR Steiger directionality test.
We obtained a comparable effect size as our primary finding after removing the outliers identified by the MR radial method (Supplementary Table S7). Our sensitivity analysis did not reveal any evidence of pleiotropy or heterogeneity.
We replaced the exposure and outcome dataset to verify whether the results of the primary analyses were robust (Supplementary Table S8). The results showed that the causal relationship between genetically predicted FM and OCD remained robust. For instance, a one-SD increase in genetically predicted FM decreased the risk of OCD, with an OR of 0.721 (IVW: 95% CI = 0.548–0.949, P = 0.019), after replacing the dataset with the FM. Similarly, the results after exchanging the OCD summary statistical data showed that a genetically predicted FM increase was significantly associated with a lower risk of OCD (IVW: OR = 0.656, 95% CI: 0.510–0.845, P = 0.001).
After excluding education-related SNPs, our results remained consistent with the main findings (Supplementary Table S9). For example, only one SNP (rs11245344) was strongly associated with FM and education. One SD increase in genetically predicted FM decreased the risk of OCD, with an OR of 0.682 (IVW: 95% CI = 0.530–0.878, P = 0.003) after removing rs11245344.
We conducted bidirectional MR by exchanging the exposure and outcome variables of the primary analyses. SNPs with genome-wide significant (P < 1 × 10−5) associations with OCD were selected since there were no SNPs with P values smaller than 5 × 10−8. Genetically predicted increases in OCD risk were significantly associated with decreased FM (IVW: OR = 0.992, 95% CI: 0.986–0.998, P = 0.010) (Supplementary Table S10).
-
We used a two-sample MR approach to explore the causal relationship between genetically predicted FM and OCD based on summary statistical data from the most recent GWAS with the largest sample size. For the first time, we found a negative causal relationship between genetically predicted FM and OCD.
The bidirectional causality between FM and OCD indicates that these two traits may share some common genetic predisposition. Few studies have investigated the effect of FM on OCD, and most of them found that people with OCD had a lower BMI, which supported our findings[9-11]. For instance, a cohort study from the Dutch Multicenter Clinical Consortiums revealed that the purer the OCD phenotype is, the stronger the protection against overweight and obesity[9]. An MR study by Hübel et al. revealed that OCD was significantly negatively associated with BF%[30]. Abramovitch et al.[31] proposed a model that illustrated how individuals with OCD tend to exhibit specific behaviors related to weight management. This may explain the negative association between genetically predicted OCD and FM. A causal relationship between reduced FM and increased risk of OCD was found for the first time in this study. This causal relationship between FM and OCD may provide a novel target for the prevention and treatment of OCD. Moreover, the reverse causal relationship between OCD and FM suggests that changes in FM levels may be considered an auxiliary indicator for assessing the severity of OCD progression. Further research is needed to elucidate the underlying mechanisms of this bidirectional causality. Moreover, while MR-Egger suggested a potential association between FFM and OCD (P = 0.014), the primary IVW analysis showed non-significance (P = 0.154). This discrepancy likely reflects MR-Egger’s sensitivity to residual pleiotropy, whereas IVW’s superior statistical power makes it more reliable, thus current evidence cannot substantiate causal claims. Future MR studies employing stronger FFM instruments and larger samples are warranted to clarify this relationship.
A multifactorial etiology of OCD is assumed, in which biological, psychological, genetic, and external factors interact[32-35]. Accordingly, we explored plausible mechanisms linked reduced FM to an increased risk of OCD from psychological, genetic, and biological perspectives.
From a psychological perspective, individuals with low FM may have a greater risk of developing OCD due to distorted beliefs and misconceptions within their cognitive and belief systems[36]. These individuals may excessively focus on weight, food, and dietary habits, leading to a skewed perception of their self-worth. Erroneously believing that satisfaction and self-acceptance can be achieved only through reducing body fat, individuals may become trapped in a cycle of obsessive thinking and compulsive behaviors[37]. For example, Levinson et al.[38] discovered that when individuals with anorexia nervosa reported greater concern over mistakes, they endorsed more severe OCD core dimensions (obsessions and compulsions). As participants' reported compulsions increased, their reported drive for thinness and body dissatisfaction also increased, suggesting a mutual influence between these factors. Previous studies have also attempted to explain the low BMI in OCD patients by repeated negative reinforcements resulting in alterations of positive reinforcement[39,40].
From a genetic perspective, a recent genetic analysis suggested that BMI may be a metabolic-behavioral trait[41]. BDNF[42] and FTO[43-45] were found to be associated with both obesity and psychiatric disorders. In addition, animal experiments have identified several candidate genes correlated with OCD, including SAPAP3 and SLITRK5[46,47]. Therefore, there may be shared genetic loci between FM and OCD that mediate the functional pathway. Further studies are warranted to investigate the genetic connection between FM and OCD.
From a biological perspective, serotonin (5-HT) deficiency has been implicated in OCD pathogenesis[48,49]. Although a recent systematic umbrella review revealed an inconsistent association between serotonin and depression[50], 5-HT3 antagonists are still used in clinical practice for the treatment of OCD[51]. Adipocytes in adipose tissue can synthesize and store tryptophan, an essential component of serotonin synthesis[52,53]. Thus, a decrease in FM may lead to an insufficient supply of tryptophan, affecting serotonin synthesis and release, thereby increasing the risk of OCD.
Moreover, disruptions in glutamate metabolism—particularly elevated glutamate levels in cortico-striato-thalamo-cortical circuits—are increasingly implicated in OCD pathophysiology[40,54-58]. Adipocytes regulate fatty acid synthesis pathways that intersect with glutamate metabolism, converting glutamate to α-ketoglutarate via adipocyte enzymes[59,60]. Thus, reduced FM may increase the risk of developing OCD through the glutamate system.
In summary, there is limited research on the causal association between reduced fat mass and increased OCD risk, possibly mediated through psychological distortions, shared genetic predispositions, altered serotonin synthesis, and dysregulated fatty acid-glutamate metabolism. This study is a data-driven causal exploration based on population-based GWAS data. Future studies are warranted to elucidate the underlying mechanisms involved.
Our study, based on the latest and largest publicly available European GWAS data and through comprehensive MR analysis and several sensitivity analyses, is the first to report the negative causality between genetically predicted FM and OCD, complementing previous correlational studies. However, limitations should also be noted. First, the generalizability of our findings is limited, given that only GWAS data from populations of European ancestry were used. Although the largest and most up-to-date GWAS data were selected for this study, our results may not fully extend to other ethnic groups. Further studies of diverse ancestral backgrounds are warranted to assess the robustness and cross-ethnic applicability of the observed FM-OCD causal relationship. Second, only summary-level data, not individual data, are available. Two-sample MR with the linear assumption is performed, which may result in the misestimation of the causality. Third, due to data limitations, we did not take into account the bimodal onset of OCD. By incorporating such detailed classifications, future studies can provide more valuable insights into the causality between FM and OCD. Fourth, the comorbidity of OCD with other disorders cannot be explored using MR methods. Subsequent studies can consider using alternative methods to investigate the causal relationship between FM and the comorbidity of OCD.
-
Based on the publicly available GWAS database, a negative causal relationship between genetically predicted FM and OCD was identified using the two-sample MR approach. This finding is informative for future research on the causal relationship between obesity and mental illness and provides new possibilities for targeted prevention strategies. The prevention or treatment of psychiatric disorders should include not only the control of BMI but also fat distribution and body composition. However, our findings should be interpreted with caution, as unmeasured pleiotropy or residual confounding could influence the causal estimates derived from MR.
Dissecting the Causal Association between Body Fat Mass and Obsessive-compulsive Disorder: A Two-sample Mendelian Randomization Study
doi: 10.3967/bes2025.069
- Received Date: 2025-03-10
- Accepted Date: 2025-05-27
-
Key words:
- Mendelian randomization /
- Body fat mass /
- Obsessive-compulsive disorder /
- Causal inference.
Abstract:
None.
We used publicly available summary data for which no additional ethical committee approval or participant informed consent was needed.
| Citation: | Meiling Hu, Zhennan Lin, Hongwei Liu, Yunfeng Xi, Youxin Wang. Dissecting the Causal Association between Body Fat Mass and Obsessive-compulsive Disorder: A Two-sample Mendelian Randomization Study[J]. Biomedical and Environmental Sciences. doi: 10.3967/bes2025.069 |







 Quick Links
Quick Links
 DownLoad:
DownLoad: