-
Tuberculosis (TB) remains a significant global health challenge, with approximately 10.6 million cases reported and an estimated 1.3 million deaths in 2022[1-2]. The End TB strategy called for an 80% reduction in the global TB incidence rate by 2030 compared to the 2015 rates. However, from 2000 to 2018, the global TB incidence decreased at an annual rate of 1.6%[3-4]. Moreover, the COVID-19 pandemic had a detrimental impact on access to TB diagnosis and treatment, resulting in an increase in the number of people infected with and at risk of developing TB[1]. From these, achieving the goal of End-TB strategy by 2030 is challenging. The World Health Organization (WHO) reported that one quarter of the global population may carry latent TB infection (LTBI). Approximately 5% to 10% of individuals with LTBI would progress to active TB, constituting a potential reservoir of patients with TB, which is one of the biggest obstacles in achieving the goal of the End TB Strategy [5-6]. Providing TB preventive treatment (TPT) to people with LTBI, especially among high-risk groups is an essential component of the End-TB strategy until effective preventive vaccines become available[6].
TPT is consists of one or more anti-TB medicines to prevent people with LTBI from progressing to TB disease; the protective effect of TPT could be approximately 60%–90%[6-7]. Through mathematical models, conducting proactive screening on a large scale, and providing TPT to identified cases with LTBI could significantly reduce the incidence of TB[8]. However, the global promotion of TPT has been slow; 15.5 million people were initiated on TPT from 2018–2022, achieving 52% of the target set at the 2018 United Nations High-Level Meeting[1].
China represents one of the high TB-burdened countries worldwide. It is estimated that 350 million people live with LTBI; the LTBI rate is 18.08% among the population aged 5 years and above, and 20.34% among people aged 15 years and above[2,9-11]. The national guidelines[12-13] recommended TPT for high-risk group, including children < 5 years with LTBI who are in close contact of patients with etiologically positive TB, HIV/AIDS patients with LTBI, students who are in close contact with active TB cases, etc. However, TPT has not been systematically implemented nationwide. In 2022, only 1.2% of household contacts of bacteriologically-confirmed TB cases received TPT[1]. Understanding the acceptance levels of TPT and its influencing factors are helpful for the development of LTBI management strategies in China. A small number of studies have reported low acceptance of TPT, although these results were limited by sample size and population selection[14-17]. Here, we designed a study to understand the willingness and barriers to acceptance of TPT by people with LTBI in China.
-
The mainland of China has a population of approximately 1.4 billion, involving 31 provinces, autonomous regions, and municipalities, 333 units at prefecture level and 2,990 units at county level[18]. According to the geography and economy, the country is divided into eastern, central and western regions. Economic development is higher in the eastern regions and lower in the west. Moreover, the prevalence of TB is higher in the western region compared to the eastern and central regions. Considering TB burden, geographical and economic factors, 10 counties from eastern regions (Hebei Province, Guangdong Province), central regions (Henan Province, Hunan Province), and western regions (Chongqing Municipality) were selected as survey sites. The research was carried out under the routine TB program at survey sites from May 18, 2023 to December 31, 2023. According to the research implementation plan, each study site formulated a specific workflow and established a working group consisting of local CDCs (Center for Disease Control and Prevention, CDC) and designated TB hospitals.
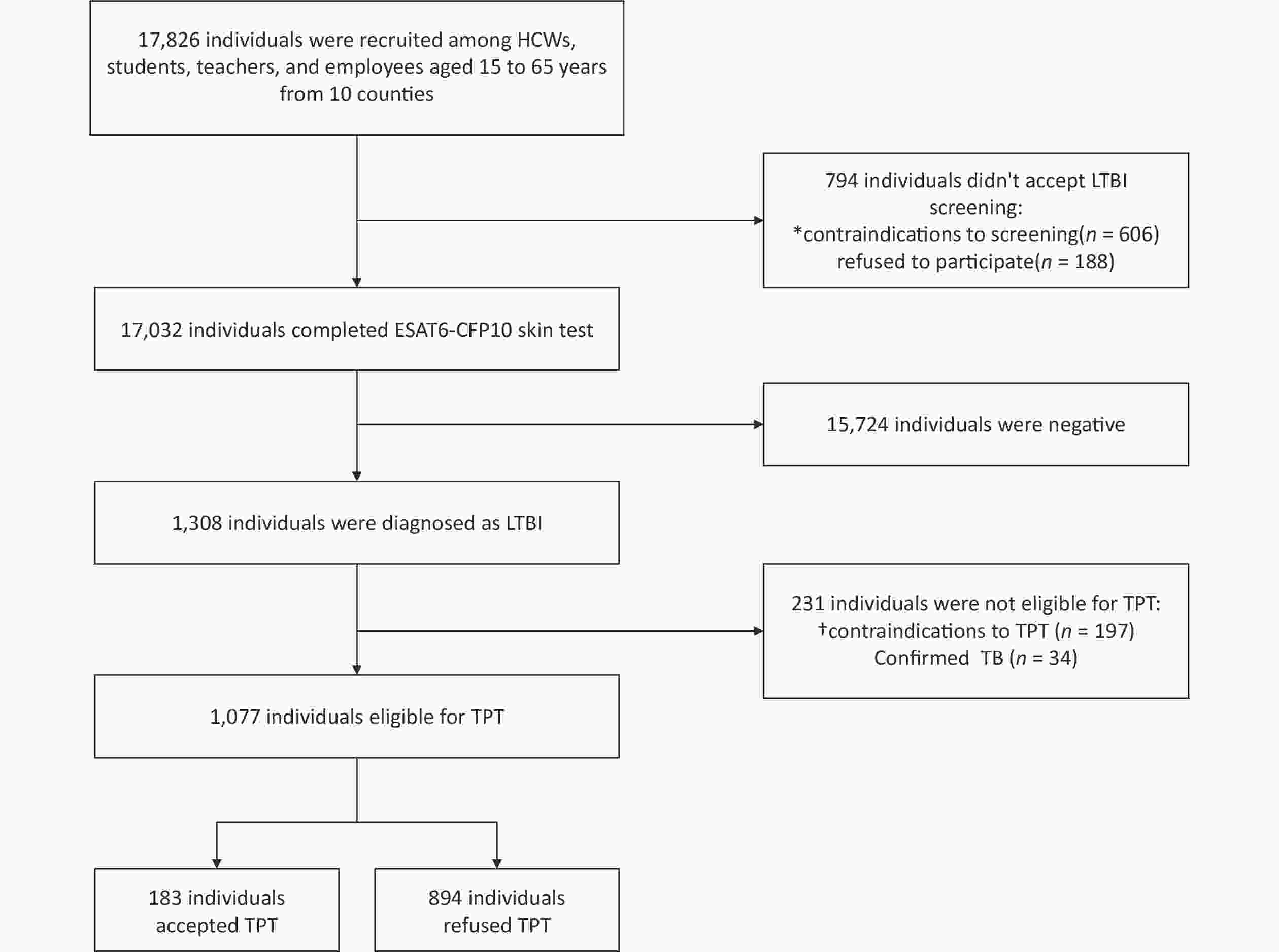
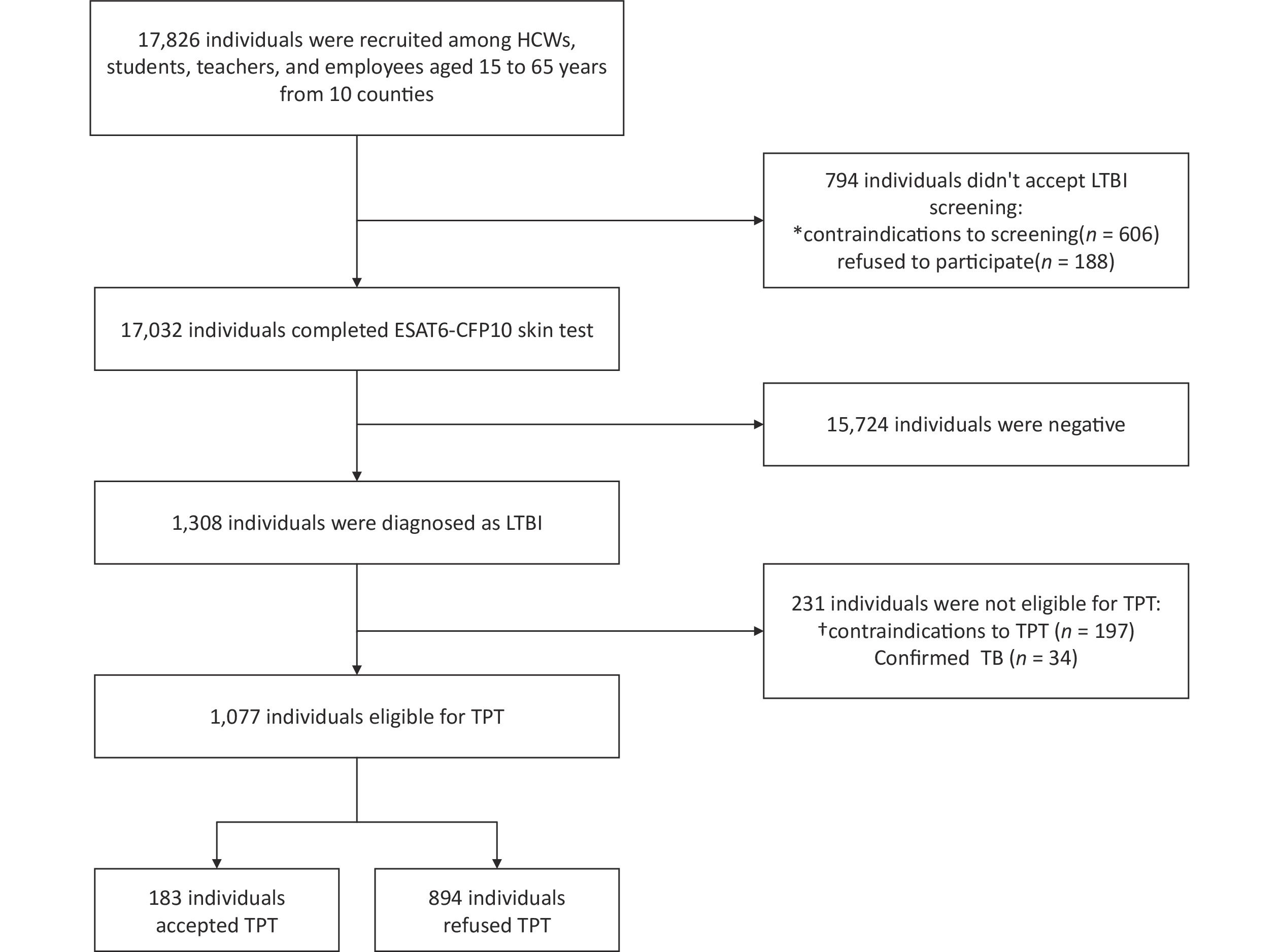
This study was approved by the Ethics Review Committee of the Chinese CDC (CCDC) (Approval number: 202316). TB-designated hospitals were responsible for LTBI screening. ESAT6-CFP10 skin test (EC) was used for LTBI screening because it is not affected by BCG vaccination and most non-TB mycobacterial infections; moreover, it has the advantages of being easy to use with high sensitivity and specificity. Those who met the criteria for TPT[12-13] were included in the study. All participants provided informed and voluntary consent to receive TPT from doctors at designated TB hospitals. Those who consented were provided treatment by TB-designated hospitals and the local CDCs were responsible for medication management. Those who declined to TPT were regularly followed-up by local CDCs according to national guidelines. Finally, 1,077 individuals were enrolled in the study. At enrollment, survey participants gave written informed consent. A flow chart of the inclusion criteria are presented in Figure 1.
-
A structured questionnaire was designed for data collection, and included sex, age, occupation, and education level, as well as reasons for TPT refusal (uncertain effect on prevention, fear of side effects, high economic burden, fear of discrimination, and non-adherence to treatment). All investigators had received training before conducting the questionnaires, and senior researchers provided technical support and supervision throughout the investigation. Quality control regarding the survey process was carried out and basic data were checked. The collected data were double-entered and logical validation, and the database was sorted by the research team. All questionnaires were checked for incompleteness and inconsistent or unclear information. We distributed 1,077 formal questionnaires and obtained 1,077 valid responses, with a 100% response rate.
Statistical analysis was performed using SPSS software v.26.0 (IBM, New York, USA). Continuous variables are expressed as means ± standard deviation, and categorical variables are described by frequency and percentage. Comparison of rates among groups were tested by Chi-squared tests and Fisher’s exact probability method. Multivariate binary logistic regression was performed to assess factors influencing acceptance of TPT among LTBI. P-values < 0.05 were considered statistically significant.
-
A total of 1,077 LTBI cases were included in this study, with a mean age of 37.5 ± 13.2 years. Among them, 61.6% (663/1,077) were females, 62.5% (673/1,077) were college graduates or higher, 57.9% (624/1,077) were healthcare workers (HCWs), and 21.5% (231/1,077) were students. The overall acceptance rate for TPT was 17.0% (183/1,077). There were statistically significant differences in the acceptance rate of TPT among different sexes, ages, educational levels, and occupations (P < 0.05). Compared to those having an education of primary school or lower, individuals with middle school education (adjusted odds ratio [aOR]: 7.384, 95% confidence intervals [95% CI ]: 3.092–17.636; P < 0.05), high school education (aOR:3.104, 95% CI:1.275-7.555; P < 0.05) and college or higher education (aOR: 5.416, 95% CI: 2.140–13.703; P < 0.05) were associated with lower acceptance of TPT. While comparing with other occupations, HCWs (aOR: 6.339, 95% CI: 3.458–11.620; P < 0.05), teachers (aOR: 6.253, 95% CI: 2.489–15.709; P < 0.05) and students (aOR: 2.920, 95% CI: 1.363-6.258; P < 0.05) were associated with lower willingness of TPT acceptance (Table 1).
Table 1. Factors influencing acceptance of TPT among LTBI in the 10 selected counties of China (N = 1,077)
Characteristics LTBI (n, %)* LTBI who accepted TPT (n, %)† Unadjusted OR (95% CI) P value Adjusted OR (95% CI) P value Sex 0.076 0.967 Male 414 (38.4) 81 (19.6) 1 1 – Female 663 (61.6) 102 (15.4) 1.338 (0.970–1.845) 0.992 (0.691–1.425) Age, years < 0.001 0.069 15–17 163 (15.1) 62 (38.0) 1 – 1 – 18–44 541 (50.2) 60 (11.1) 4.921 (3.250–7.450) < 0.001 2.346 (1.075–5.121) 0.032 45–65 373 (34.7) 61 (16.4) 3.140 (2.066–4.772) < 0.001 2.599 (1.135–5.952) 0.024 Education < 0.001 < 0.001 Primary school or lower 34 (3.2) 23 (67.6) 1 – 1 – Middle school 147 (13.6) 28 (19.0) 8.886 (3.882–20.340) < 0.001 7.384 (3.092–17.636) < 0.001 High school 223 (20.7) 73 (32.7) 4.296 (1.987–9.289) < 0.001 3.104 (1.275–7.555) 0.013 College or higher 673 (62.5) 59 (8.8) 21.760 (10.110–46.834) < 0.001 5.416 (2.140–13.703) < 0.001 Occupations < 0.001 < 0.001 Other occupations 134 (12.4) 54 (40.3) 1 – 1 – HCWs 624 (57.9) 48 (7.7) 8.100 (5.146–12.751) < 0.001 6.339 (3.458–11.620) < 0.001 Students 231 (21.5) 74 (32.0) 1.432 (0.920–2.229) 0.111 2.920 (1.363–6.258) 0.006 Teachers 88 (8.2) 7 (8.0) 7.811 (3.352–18.198) < 0.001 6.253 (2.489–15.709) < 0.001 Total (n, %)† 1,077 (100.0) 183 (17.0) Note. *Column percentage, †Row percentage. HCWs, healthcare workers; TPT, tuberculosis preventive treatment; LTBI, latent tuberculosis infection; OR, odds ratio; CI, confidence interval. As presented in Table 2, the main barriers to TPT acceptance among LTBI cases included the misconception that it had an uncertain effect on prevention (57.8%, 517/894), and concern regarding side effects (32.7%, 292/894). Among HCWs, 70.8% (408/576) cases had a misconception that TPT had uncertain effect on prevention, and 26.7% (154/576) expressed concerns regarding side effects of TPT. Among students, 50.3% (79/157) had misconceptions about the prevention effect and 24.2% (38/157) expressed concerns regarding side effects. Among teachers, 88.9% (72/81) expressed concern about side effects of TPT. In addition, 27.5% (22/80) of other occupations expressed concern regarding high economic burden.
Table 2. Main reasons for refusal TPT among people with LTBI in the 10 selected counties of China (N = 894)
Characteristics LTBI (n, %) * Uncertain effect on prevention
(n, %)†Fear of side effects (n, %)† High economic burden (n, %)† Fear of discrimination (n, %)† Nonadherence to treatment (n, %)† P value Sex Male 333 (37.2) 177 (53.2) 112 (33.6) 25 (7.5) 14 (4.2) 5 (1.5) 0.013 Female 561 (62.8) 340 (60.6) 180 (32.1) 30 (5.3) 9 (1.6) 2 (0.4) Age, years 15–17 101 (11.3) 42 (41.6) 24 (23.8) 13 (12.9) 16 (15.8) 6 (5.9) < 0.001 18–44 481 (53.8) 317 (66.0) 145 (30.1) 14 (2.9) 4 (0.8) 1 (0.2) 45–65 312 (34.9) 158 (50.6) 123 (39.4) 28 (9.0) 3 (1.0) 0 (0.0) Education Primary school or lower 11 (1.2) 8 (72.7) 1 (9.1) 2 (18.2) 0 (0.0) 0 (0.0) < 0.001 Middle school 119 (13.3) 53 (44.5) 39 (32.8) 22 (18.5) 2 (1.7) 3 (2.5) High school 150 (16.8) 57 (38.0) 58 (38.6) 12 (8.0) 19 (12.7) 4 (2.7) College or higher 614 (68.7) 399 (65.0) 194 (31.6) 19 (3.1) 2 (0.3) 0 (0.0) Occupations HCWs 576 (64.4) 408 (70.8) 154 (26.7) 11 (2.0) 3 (0.5) 0 (0.0) < 0.001 Students 157 (17.6) 79 (50.3) 38 (24.2) 15 (9.5) 18 (11.5) 7 (4.5) Teachers 81 (9.1) 1 (1.2) 72 (88.9) 7 (8.7) 1 (1.2) 0 (0.0) Other occupations 80 (8.9) 29 (36.3) 28 (35.0) 22 (27.5) 1 (0.1) 0 (0.0) Total (n, %)† 894 (100.0) 517 (57.8) 292 (32.7) 55 (6.1) 23 (2.6) 7 (0.8) Note.*Column percentage, †Row percentage. HCWs, healthcare workers; TPT, tuberculosis preventive treatment; LTBI, latent tuberculosis infection. -
TPT for people with LTBI has become a key measure to reduce the burden of TB disease[6-7]. Our study included insights from diverse populations with LTBI, and analyzed the acceptance of TPT. The study found that the acceptance rate of TPT among people with LTBI was low; the main barriers to TPT acceptance were misconceptions that it had uncertain effects on prevention and concern regarding side effects.
Compared to other populations, HCWs face a higher risk of LTBI owing to occupational exposure[17,19], making them a key group for implementing TPT. We observed that the acceptance rate of TPT among HCWs was only 7.7%; however, this was higher than another domestic study, where only one among 112 HCWs received TPT[17]. However, a systematic study reported that the acceptance rate of TPT among HCWs in low-income and middle-income countries was 48% to 63%[19-20], demonstrating that the acceptance rate of TPT among HCWs is typically low in China. In particular, the attitude of HCWs concerning TPT could have affected the acceptance of TPT among other people with LTBI, as HCWs were the key group involved in implementing TPT[16].
Schools are considered one of the high-risk public places for TB transmission. Introducing TPT and other interventional measures for individuals with LTBI in schools is of great significance for reducing the subsequent occurrence and transmission of TB[21-22]. In our study, 32.0% of students accepted TPT; the acceptance rate was higher than HCWs and teachers, although lower than the acceptance rate reported in a survey on LTBI among middle school and college students conducted in Jiangsu province in China, which was 47.3%[22]. Moreover, we found that the acceptance rate of TPT among teachers was only 8.0%. Teachers play a key role in in implementing TPT in school as their influence is crucial in health education and providing guidance to students.
Our study identified that 57.8% of participants refused to accept TPT owing to misconceptions about its effectiveness, which was the main barrier to TPT acceptance. Previous studies have reported that lack of knowledge around LTBI were factors influencing TPT acceptance[23-24]. TPT is overlooked as LTBI is asymptomatic and TPT does not produce any apparent therapeutic effects[16,25]. People who perceived the severity of TB could recognize the benefits of TPT and actively accepted it[26]. Hence, adequate health literacy concerning TB and TPT is vital in the decision-making process among people with LTBI. Meanwhile, another barrier to TPT acceptance was concerns regarding side effects, accounting for 32.7% of people with LTBI. Nevertheless, excessive awareness of TPT and its potential side effects could lead to the development of a fear of treatment that would be detrimental to proactive behavior[27], suggesting the importance of providing comprehensive and accurate counseling to people with LTBI.
Additionally, there were differences in reasons for refusing TPT among occupations. As for HCWs, students, and other occupations, the most important obstacle was distrust of TPT, whereas for teachers, the main barrier was concern about side effects of TPT. In addition, for other occupations, concerns regarding economic burden of TPT has become an important factor. These results indicate that targeted support is needed to promote TPT among different groups nationwide.
This study had certain limitations. First, despite this being a large sample, multi-center study, with five provinces from eastern, central and western regions selected based on levels of TB burden in China, the findings could not represent the current situation in China as only 10 counties were included in the study. Second, in-depth interviews involving focus groups were not conducted in the study; moreover, in future studies a mixed-methods approach is necessary to gain a deeper understanding on the reasons for TPT acceptance. Third, we know that older adults > 65 years of age represent a high-risk group for LTBI. However, owing to the restrictions on using the EC on older adults, this group was not assessed in the study. Despite these limitations, this study has some notable strengths. This was the first multi-center cross-sectional study to investigate willingness and barriers to TPT acceptance among LTBI populations. We observed that uncertainty concerning the effectiveness of TPT and excessive concerns regarding side effects were the main barriers to TPT acceptance. These findings could serve as a reference for developing intervention strategies among people who decline to accept TPT.
-
This study provided preliminary insights into the acceptance of TPT among different LTBI populations in China, providing theoretical support for implementing TPT on a larger scale nationwide. An enhanced and comprehensive understanding of LTBI and TPT is vital among people with LTBI. Moreover, targeted policies need to be developed to address obstacles faced by different groups of people with LTBI. Conducting TB screening and TPT of individuals with LTBI is of great public health significance among HCWs, teachers, and students.
-
Ni Wang and Yanlin Zhao were responsible for the study design. Jingjuan Ren and Fei Huang contributed to data analysis and article writing. Haifeng Chen, Huimin Zhang, Jianwei Sun, Ahui Zhao, Zuhui Xu, Liqin Liu, Huizhong Wu, Lanjun Fang, Chengguo Wu, Qingya Wang, Wenqian Zhang, Xinhua Sun, Xiaoping Liu, and Jizheng Yuan collected data from the survey. Bohan Chen contributed to data analysis. All authors have reviewed and approved the final manuscript.
doi: 10.3967/bes2024.150
Barriers to the Acceptance of Tuberculosis Preventive Treatment: A Multicenter Cross-sectional Study in China
-
Abstract:
Objective We aimed to understand the willingness and barriers to the acceptance of tuberculosis (TB) preventive treatment (TPT) among people with latent TB infection (LTBI) in China. Methods A multicenter cross-sectional study was conducted from May 18, 2023 to December 31, 2023 across 10 counties in China. According to a national technical guide, we included healthcare workers, students, teachers, and others occupations aged 15–65 years as our research participants. Results Overall, 17.0% (183/1,077) of participants accepted TPT. There were statistically significant differences in the acceptance rate of TPT among different sexes, ages, educational levels, and occupations (P < 0.05). The main barriers to TPT acceptance were misconceptions that it had uncertain effects on prevention (57.8%, 517/894), and concerns about side effects (32.7%, 292/894). Conclusion An enhanced and comprehensive understanding of LTBI and TPT among people with LTBI is vital to further expand TPT in China. Moreover, targeted policies need to be developed to address barriers faced by different groups of people. -
Key words:
- Latent tuberculosis infection /
- Tuberculosis preventive treatment /
- Acceptance /
- Healthcare workers /
- Students /
- Teachers
&These authors contributed equally to this work.
注释:1) CONFLICTS OF INTEREST: -
Figure 1. Study population flowchart.
HCWs, healthcare workers; LTBI, latent tuberculosis infection; TB, tuberculosis; TPT, tuberculosis preventive treatment. *Contraindications to screening LTBI involved: 1. Suffered from acute infectious diseases (such as measles, pertussis, influenza, pneumonia, etc.), acute conjunctivitis and acute otitis media. 2. People with a history of allergic reactions and hysteria with a variety of drugs. 3. Suffered from systemic skin diseases. 4. Other situations in which the clinician determine that TPT was not suitable. †Contraindications to TPT involved: 1. Those who are receiving treatment for active viral hepatitis or accompanied by hyper enzymopathy. 2. Those who have allergies, or whose bodies are in an allergic reactions. 3. Those who have epilepsy, psychopaths, or are receiving antipsychotic drugs. 4. Those who had clear close contact with multi-drug-resistant or extensively drug-resistant TB patients. 5. Those who suffer from blood system diseases. 6. Those who previously had TB and completed 5 years of standardized anti-TB therapy.
Table 1. Factors influencing acceptance of TPT among LTBI in the 10 selected counties of China (N = 1,077)
Characteristics LTBI (n, %)* LTBI who accepted TPT (n, %)† Unadjusted OR (95% CI) P value Adjusted OR (95% CI) P value Sex 0.076 0.967 Male 414 (38.4) 81 (19.6) 1 1 – Female 663 (61.6) 102 (15.4) 1.338 (0.970–1.845) 0.992 (0.691–1.425) Age, years < 0.001 0.069 15–17 163 (15.1) 62 (38.0) 1 – 1 – 18–44 541 (50.2) 60 (11.1) 4.921 (3.250–7.450) < 0.001 2.346 (1.075–5.121) 0.032 45–65 373 (34.7) 61 (16.4) 3.140 (2.066–4.772) < 0.001 2.599 (1.135–5.952) 0.024 Education < 0.001 < 0.001 Primary school or lower 34 (3.2) 23 (67.6) 1 – 1 – Middle school 147 (13.6) 28 (19.0) 8.886 (3.882–20.340) < 0.001 7.384 (3.092–17.636) < 0.001 High school 223 (20.7) 73 (32.7) 4.296 (1.987–9.289) < 0.001 3.104 (1.275–7.555) 0.013 College or higher 673 (62.5) 59 (8.8) 21.760 (10.110–46.834) < 0.001 5.416 (2.140–13.703) < 0.001 Occupations < 0.001 < 0.001 Other occupations 134 (12.4) 54 (40.3) 1 – 1 – HCWs 624 (57.9) 48 (7.7) 8.100 (5.146–12.751) < 0.001 6.339 (3.458–11.620) < 0.001 Students 231 (21.5) 74 (32.0) 1.432 (0.920–2.229) 0.111 2.920 (1.363–6.258) 0.006 Teachers 88 (8.2) 7 (8.0) 7.811 (3.352–18.198) < 0.001 6.253 (2.489–15.709) < 0.001 Total (n, %)† 1,077 (100.0) 183 (17.0) Note. *Column percentage, †Row percentage. HCWs, healthcare workers; TPT, tuberculosis preventive treatment; LTBI, latent tuberculosis infection; OR, odds ratio; CI, confidence interval. Table 2. Main reasons for refusal TPT among people with LTBI in the 10 selected counties of China (N = 894)
Characteristics LTBI (n, %) * Uncertain effect on prevention
(n, %)†Fear of side effects (n, %)† High economic burden (n, %)† Fear of discrimination (n, %)† Nonadherence to treatment (n, %)† P value Sex Male 333 (37.2) 177 (53.2) 112 (33.6) 25 (7.5) 14 (4.2) 5 (1.5) 0.013 Female 561 (62.8) 340 (60.6) 180 (32.1) 30 (5.3) 9 (1.6) 2 (0.4) Age, years 15–17 101 (11.3) 42 (41.6) 24 (23.8) 13 (12.9) 16 (15.8) 6 (5.9) < 0.001 18–44 481 (53.8) 317 (66.0) 145 (30.1) 14 (2.9) 4 (0.8) 1 (0.2) 45–65 312 (34.9) 158 (50.6) 123 (39.4) 28 (9.0) 3 (1.0) 0 (0.0) Education Primary school or lower 11 (1.2) 8 (72.7) 1 (9.1) 2 (18.2) 0 (0.0) 0 (0.0) < 0.001 Middle school 119 (13.3) 53 (44.5) 39 (32.8) 22 (18.5) 2 (1.7) 3 (2.5) High school 150 (16.8) 57 (38.0) 58 (38.6) 12 (8.0) 19 (12.7) 4 (2.7) College or higher 614 (68.7) 399 (65.0) 194 (31.6) 19 (3.1) 2 (0.3) 0 (0.0) Occupations HCWs 576 (64.4) 408 (70.8) 154 (26.7) 11 (2.0) 3 (0.5) 0 (0.0) < 0.001 Students 157 (17.6) 79 (50.3) 38 (24.2) 15 (9.5) 18 (11.5) 7 (4.5) Teachers 81 (9.1) 1 (1.2) 72 (88.9) 7 (8.7) 1 (1.2) 0 (0.0) Other occupations 80 (8.9) 29 (36.3) 28 (35.0) 22 (27.5) 1 (0.1) 0 (0.0) Total (n, %)† 894 (100.0) 517 (57.8) 292 (32.7) 55 (6.1) 23 (2.6) 7 (0.8) Note.*Column percentage, †Row percentage. HCWs, healthcare workers; TPT, tuberculosis preventive treatment; LTBI, latent tuberculosis infection. -
[1] World Health Organization. Global tuberculosis reports 2023. World Health Organization. 2023. [2] Houben RM, Dodd PJ. The global burden of latent tuberculosis infection: a re-estimation using mathematical modelling. PLoS Med, 2016; 13, e1002152. doi: 10.1371/journal.pmed.1002152 [3] World Health Organization. The end TB strategy. WHO. 2014. https://www.who.int/publications/i/item/WHO-HTM-TB-2015.19. [2024-06-03] [4] Xu CH, Zhao YL. China's countermeasures in the context of Global Tuberculosis Prevention Action. Chin J Tuberc Respir Dis, 2022; 45, 308−12. (In Chinese) [5] Cohen A, Mathiasen VD, Schön T, et al. The global prevalence of latent tuberculosis: a systematic review and meta-analysis. Eur Respir J, 2019; 54, 1900655. doi: 10.1183/13993003.00655-2019 [6] World Health Organization. WHO consolidated guidelines on tuberculosis: module 1: prevention: tuberculosis preventive treatment. World Health Organization. 2020. [7] Zenner D, Beer N, Harris RJ, et al. Treatment of latent tuberculosis infection: an updated network meta-analysis. Ann Intern Med, 2017; 167, 248−55. doi: 10.7326/M17-0609 [8] Houben RMGJ, Menzies NA, Sumner T, et al. Feasibility of achieving the 2025 WHO global tuberculosis targets in South Africa, China, and India: a combined analysis of 11 mathematical models. Lancet Global Health, 2016; 4, e806−15. doi: 10.1016/S2214-109X(16)30199-1 [9] World Health Organization. Latent tuberculosis infection: updated and consolidated guidelines for programmatic management. World Health Organization. 2018. [10] Gao L, Bai LQ, Liu JM, et al. Annual risk of tuberculosis infection in rural China: a population-based prospective study. Eur Respir J, 2016; 48, 168−78. doi: 10.1183/13993003.00235-2016 [11] Cui XJ, Gao L, Cao B. Management of latent tuberculosis infection in China: exploring solutions suitable for high-burden countries. Int J Infect Dis, 2020; 92S, S37−40. [12] Chinese Center for Disease Control and Prevention. Technical guide for tuberculosis prevention and control in China. People's Medical Publishing House. 2021. (In Chinese) [13] Chinese Center for Disease Control and Prevention. Technical guide for the preventive treatment of tuberculosis in China. People's Medical Publishing House. 2023. (In Chinese) [14] Zhang J, Fu RN, Wang SL, et al. Analysis of willingness of receiving preventive treatment in patients with latent tuberculosis infection among close contacts of pulmonary tuberculosis in high-burden areas. Chin J Antituberc, 2024; 46, 165−72. (In Chinese) [15] Li G, Xu H, Jing MY, et al. Reason analysis and countermeasure evaluation of latent tuberculosis infection refusing preventive treatment in a certain county. J Clin Pulm Med, 2022; 27, 1415−20. (In Chinese) [16] Fa LF, Xu CH, Cheng J, et al. Acceptability of tuberculosis preventive treatment strategies among healthcare workers using an online survey-China, 2021. China CDC Wkly, 2022; 4, 211−5. [17] Wang F, Ren YL, Liu K, et al. Large gap between attitude and action in tuberculosis preventive treatment among tuberculosis-related healthcare workers in eastern China. Front Cell Infect Microbial, 2022; 12, 991400. doi: 10.3389/fcimb.2022.991400 [18] National Bureau of Statistics. Major figures on 2020 population census of China. Office of the Leading Group of the State Council for the Seventh National Population Census. 2021. https://www.stats.gov.cn/sj/pcsj/rkpc/d7c/202303/P020230301403217959330.pdf. [2024-06-03] [19] Yuan YM, Li SX, Zhou CC. Acceptance and influencing factors of preventive treatment for latent tuberculosis infection: a review. Chin J Public Health, 2023; 39, 942−7. (In Chinese) [20] Almufty HB, Abdulrahman IS, Merza MA. Latent tuberculosis infection among healthcare workers in Duhok province: from screening to prophylactic treatment. Trop Med Infect Dis, 2019; 4, 85. doi: 10.3390/tropicalmed4020085 [21] Cao XL, Song ZX, He WC, et al. Tuberculosis screening characteristics amongst freshmen in Changping District, Beijing, China. BMC Infect Dis, 2023; 23, 869. doi: 10.1186/s12879-023-08802-y [22] Wang Z, Li ZQ, Ding XY, et al. The current situation of willingness to receive prophylactic treatment among students with latent tuberculosis infection and its influencing factors in Jiangsu Province. China Trop Med, 2024; 24, 244−51. (In Chinese) [23] Spruijt I, Haile DT, van den Hof S, et al. Knowledge, attitudes, beliefs, and stigma related to latent tuberculosis infection: a qualitative study among Eritreans in the Netherlands. BMC Public Health, 2020; 20, 1602. doi: 10.1186/s12889-020-09697-z [24] Gao J, Berry NS, Taylor D, et al. Knowledge and perceptions of latent tuberculosis infection among Chinese immigrants in a Canadian urban Centre. Int J Family Med, 2015; 2015, 546042. [25] Manoharan A, Siti Nur Farhana H, Manimaran K, et al. Facilitators and barriers for tuberculosis preventive treatment among patients with latent tuberculosis infection: a qualitative study. BMC Infect Dis, 2023; 23, 624. doi: 10.1186/s12879-023-08612-2 [26] Spence BC, Bruxvoort K, Munoz-Plaza C, et al. Patient-reported barriers to treatment initiation and completion for latent tuberculosis infection among patients within a large integrated health care system in Southern California. J Public Health Manag Pract, 2023; 29, 345−52. doi: 10.1097/PHH.0000000000001711 [27] Hagger MS, Orbell S. The common-sense model of illness self-regulation: a conceptual review and proposed extended model. Health Psychol Rev, 2022; 16, 347−77. doi: 10.1080/17437199.2021.1878050 -




 下载:
下载:



 Quick Links
Quick Links