-
To determine the reason for the different mortality trends of ischemic heart disease (IHD) for China between Global Burden of Disease (GBD) 2010 and GBD2013, and to improve garbage code (GC) redistribution. All data were obtained from the disease surveillance points system, and two proportions for assigning chronic pulmonary heart disease (PHD) as GC to IHD were from GBD2010 and GBD2013, which were different for years before 2004. By using the GBD2013 approach, the age-standard mortality rate (ASMR) increased by 100.21% in 1991, 44.81% in 1996, and 42.47% in 2000 in comparison with the GBD2010 approach. The different methods of chronic PHD redistribution impacted the trend of IHD mortality, which elevated it in the earlier 1990s by using the GBD2013 approach. Thus, improving the redistribution of GC as a key step in mortality statistics is important.
According to World Health Organization (WHO) estimates, ischemic heart disease (IHD) is one of the leading causes of mortality[1]. The disease also resulted in substantial long-term morbidity and is one of the leading causes of overall disease burden [as measured in disability-adjusted life-years (DALYs) lost][1]. The challenge for IHD mostly comes from the developing countries. Over the past three decades, IHD mortality has been estimated to decrease by more than 50% in many developed countries such as Finland, England, the United States, Canada, Australia, New Zealand, France, and Japan[2], but accounts for more than 60% of the global disease burden in developing nations[3].
However, recently, in China, one of the largest developing countries, claims on the trend of IHD mortality at the national level over the past two decades were divergent. The Global Burden of Disease (GBD) 2010 study result showed that the age-standard mortality rate (ASMR) of IHD increased from 55.7 per 100, 000 population in 1990 to 70.1 per 100, 000 population in 2010[4]. However, the newly published GBD2013 result showed that the ASMR of IHD remained stable in the past two decades, with 115.40 per 100, 000 population in 1990 and 115.89 per 100, 000 population in 2013[5]. The sources of the cause-of-death data for China in GBD2010 and GBD2013 were both the disease surveillance points (DSP) system, but the results were different. Thus, this evoked a controversy among experts in China and abroad[6]. In China, the mortality trend of IHD is especially an important and sensitive issue. Meanwhile, the mortality trend of IHD is the key indicator closely related to the global target of prevention and control of non-communicable disease (NCD). Thus, whether the ASMR of IHD is increasing or stable in China should be clarified.
Mortality analysis is a complicated process in the GBD study, and the detailed information for China in GBD2010 and GBD2013 can be found in previous studies[4-5]. Generally speaking, first, the mortality envelope was calculated to adjust underreport of cause of death for each country. Second, the codes for various ICD tabulation lists were mapped to the GBD cause list. Third, the un-underlying causes of death, which were called garbage code (GC) in the GBD study, were redistributed by using a series of statistical methods and models[7]. Finally, the burden of disease for different diseases was systematically analyzed. To determine the cause of the difference in IHD ASMR trend between GBD2010 and GBD2013, the original DSP data were used to compare the cause-of-death analysis methods for IHD with similar GC redistribution approaches separately in both studies. The discussion also is important to improve the redistribution of GC as a key step in mortality statistics.
HTML
-
All these mortality and population data from 1991 to 2013 were from the DSP system. The DSP system for recording causes of death was established in China in 1991, covering a population of 10 million people in 145 locations in all provinces by utilizing multiple-stratified random sampling. The system was expanded in 2004 to cover 71.4 million people, which increased about 6 times from that before. The expanded DSP system was adjusted to cover 161 locations, which included 103 of the original locations and 58 new locations[8]. The new DSP system expanded to cover the whole district of a city or county, instead of one or two residential district(s) or town(s) at each location.
A uniform cause-of-death certification procedure, based on the international format of the medical certificate of cause of death, has been run in the DSP system of China after legislation in 1992, by using verbal autopsy (VA) tool for the deceased at home. At that time, local medical workers and personnel death statisticians could not understand the underlying cause of death (UCD) clearly, including ill-defined death, complicated chain of death causes, and so on. Hence, when they filled out the death certification, sometimes they regarded the un-underlying causes of death as UCD, including chronic pulmonary heart disease (PHD). In addition, an effective tool to control the quality of underlying cause of death (UCD) in the data entering system was lacking during the 1990s. Thus, the database contains a corresponding proportion of chronic PHD as a UCD, although chronic PHD has been assigned to COPD in the DSP annual report. Chronic PHD was called GC in the GBD study [7]. After the outbreak of severe acute respiratory syndrome (SARS), the Chinese government strengthened the infrastructure of the public health system, including setting up a national public health information network for countrywide coverage in 2004. The individual certifications with ICD10 codes were reported through the computer-assistance information net work, which improved the quality of death certification, especially the accuracy of the UCD coding by using automatic coding software. For example, in the death certificate, disease A is pulmonary heart disease (I27.9), disease B is emphysema (J43.9), and disease C is chronic bronchitis (J42). The computer would automatically regard chronic obstructive pulmonary disease (COPD; J44.8) as the UCD[9], which means that after 2004, all chronic PHDs were redistributed to COPD automatically and no chronic PHD was regarded as UCD in the database. In general, the quality of data collection in the DSP system is high, which have been validated in previous studies[10].
Owing to the increase in the surveillance population by more than 6 times after 2000, the death cases increased from 50, 000 to 430, 000 annually after the system expanded. Thus, approximately 6 million deaths cases were recorded from 1991 to 2013. Before 2004, approximately 6%-9% all death cases from chronic PHDs were reported in death certifications annually, but not one case of chronic PHD was recorded after 2004 because of the automatic coding system adjustment to COPD. Table 1 shows the reported death cases for selected death causes in selected years.
Diseases Name ICD-9 Code ICD-10 Code 1991 1996 2000 2005 2010 Total - - 52, 763 53, 866 50, 659 434, 244 453, 211 Cardiovascular diseases 390-459 I00-I99 18, 778 19, 665 20, 671 165, 853 187, 558 Rheumatic heart disease 390-398 I01-I09 890 701 570 4, 182 2, 688 Hypertensive heart disease 401-405 I10-I13 2, 051 1, 715 1, 648 6, 946 9, 445 Ischemic heart disease 410-414 I20-I25 2, 171 2, 996 3, 553 48, 153 64, 221 Chronic pulmonary heart disease 416 I27.9 4, 687 2, 988 3, 411 0 0 Cerebra-vascular disease 430-438 I60-I69 7, 252 9, 732 9, 681 97, 466 10, 3638 Chronic respiratory diseases 470-478, 490-519 J30-J98 5, 223 7, 848 5, 674 59, 831 55, 769 COPD 490-492, 495-496 J40-J44 5, 023 7, 688 5, 482 55, 980 51, 093 Table 1. Reporting Death Cases for Selected Causes of Death in the DSP System in the Selected Years
-
Between GBD2010 and GBD2013, the great difference in mortality analysis for IHD was GC chronic PHD redistribution. Thus, in this study, two redistribution approaches of GC were used for IHD mortality analysis: one was similar with GBD2010, in which 100% chronic PHD was redistributed to COPD, and the other was similar to GBD2013, where chronic PHD was assigned to IHD, COPD, and hypertension heart disease (HTD) before the year 2004. Since after 2004, 100% chronic PHDs were redistributed to COPD by the automatic coding software during data collection, and no chronic PHD cases could be redistributed during data cleaning. The redistribution fractions of chronic PHD from some selected years in GBD2010 and GBD2013 from the GBD team are shown in Table 2. These two approaches were simply called GBD2010 and GBD2013. Owing to the 2.5% ill-defined categories[10] and the fixed fraction of the other GCs for IHD, we just focused the redistribution of chronic PHD as GC in GBD2010 and GBD2013, which might have led to a few underestimations of the mortality level of IHD in this study. Compared with GBD2010, before 2004, more than 45% IHD cases yearly were reported in GBD2013 because of the redistribution of chronic PHD cases, especially for females.
Years Items GBD2010 GBD2013 Total Male Female Total Male Female 1991 to COPD 100.0 100.0 100.0 45.0 59.8 26.3 to IHD 0.0 0.0 0.0 46.0 35.3 59.6 to HTD 0.0 0.0 0.0 9.0 4.9 14.2 1996 to COPD 100.0 100.0 100.0 46.8 62.6 26.5 to IHD 0.0 0.0 0.0 44.1 32.6 58.9 to HTD 0.0 0.0 0.0 9.0 4.7 14.5 2002 to COPD 100.0 100.0 100.0 46.8 63.4 26.5 to IHD 0.0 0.0 0.0 44.0 31.9 58.7 to HTD 0.0 0.0 0.0 9.3 4.7 14.8 Table 2. Comparison of Redistribution Fraction of Chronic PHD in GBD2010 and GBD2013
-
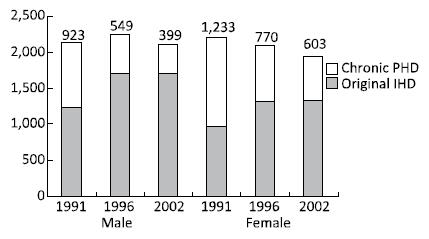
The IHD cases were calculated by using original data from the DSP database and adding different chronic PHD redistribution fractions from two GBD studies. The original IHD death cases increased with time, which were the same as the cases in GBD2010 (grey bar in Figure 1). In the DSP system, the number of deaths from chronic PHD decreased with the improvement of the death registration quality, from 4, 687 cases in 1991 to 3, 411 in 2002 (Table 1). Thus, in GBD2013, owing to the fraction of chronic PHD as GC to IHD, the highest increase in the number of deaths from IHD was in 1991 (43% for males and 56% for females), but the increment number of deaths was reduced in the following years before 2004. After 2004, no chronic PHD cases have been assigned to IHD (Figure 1).
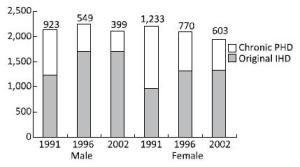
Figure 1. The original IHD death cases and added deaths from the assigned fraction of chronic PHD from GBD2013 in the period 1991-2002, according to sex.
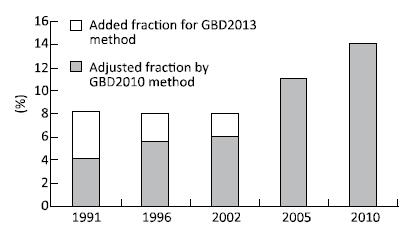
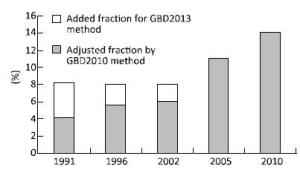
The difference in the proportion of IHD in all death cases and the mortality trend of IHD with different redistribution from chronic PHD were quantitatively analyzed by using ASMR based on the 2010 census population structure in China. The fraction for IHD cases increased from 4.1% in 1991, 5.6% in 1996, and 6.1% in 2002 without PHD to be adjusted to IHD in GBD2010. However, after using the chronic PHD redistribution fraction from GBD2013, owing to a fraction of IHD cases redistributed to IHD before 2004, the number of IHD cases increased and the fractions remained at approximately 8% from 1990to 2002 (Figure 2). Therefore, by using the GBD2013 approach, the ASMRs increased by 100.21% in 1991, 44.81% in 1996, and 42.47% in 2000, in comparison with the GBD2010 approach. The increase was faster for females than for males (Table 3). Thus, the mortality rates for IHD were elevated in the early 1990s.

Table 3. The Number and ASMR for IHD after Adjuted Assigned Fraction of Chronic PHD from GBD2010 and GBD2013 in Selected Years
-
Pulmonary heart disease, as a popular term in the medical literature, is the enlargement and failure of the right ventricle of the heart in response to increased vascular resistance (e.g., from pulmonic stenosis) or high blood pressure in the lungs[11]. Thus, the redistribution methods for PHD cases in GBD 2013 were not reasonable for the pathological and physiological mechanisms of PHD. COPD is the major cause of chronic PHD, probably accounting for 80%-90% of the causes in the Western literature[12]. A study in China indicated that the proportion was even higher for Chinese. Fu et al. investigated that 96.6% of chronic PHD cases were from COPD in Beijing[13]. Therefore, the primary disease of chronic PHD is not from IHD or HTD, so the redistribution of approximately 50% of death cases of PHDs to IHD and HTD is not reasonable.
Most chronic PHDs develop from chronic bronchitis, blocking the development of emphysema, which means COPD, but a few PHD cases develop from bronchial asthma, tuberculosis, bronchiectasis, pneumoconiosis, and so on[11]. Thus, a few (approximately 5%) of mortality levels of COPD were overestimated with the GBD2010 method. The method of redistribution of GC needs to be further improved. The key procedure should be to improve the reporting quality of medical death certificates. After 2004, no chronic PHD has been recorded as UCD in the DSP system and the quality of death certification has improved, as the DSP system follows a strict data collection procedure, including training of local staff and using a computer-assisted coding system.
Thus, we believe that the method in GBD2010 was relatively reasonable, and the result on the mortality trend of IHD in GBD2010 was similar with other research studies. Most studies showed that the trend of the ASMR of IHD has been increasing[14-15]. Some international studies showed that IHD is the main cause of mortality and morbidity in most developing countries, including China, and this pattern will probably be unchanged in 2020[16]. Meanwhile, the trend of IHD mortality is consistent with the lifestyles change and increasing behavior risk factors in Chinese, such as smoking, unhealthy diet, hypertension, and overweight/ obesity.
In March 2015, the Institute of Basic Medical Sciences at the Chinese Academy of Medical Sciences, Chinese Center for Disease Prevention and Control, National Center for Cardiovascular Diseases of China, and the Institute for Health Metrics and Evaluation of the University of Washington jointly held a ‘symposium on Chinese cardiovascular disease burden and health policy.' More than 100 Chinese and international scientists reviewed the findings on the cardiovascular disease (CVD) burden of GBD2010 and GBD2013, and other studies on CVD in China discussed the risk factors related to the mortality trend of CVD, and realized that results in GBD2013 may lead to an overestimation of IHD and underestimation of COPD, especially for provinces with high proportions of PHDs as GC, which may also lead to a false description of the mortality trend of IHD and COPD for the Chinese population[6]. The symposium promoted the consensus on the redistribution of PHD as GC, and the approach redistribution of PHD would be corrected in GBD2015.
-
Based on the above-mentioned description, the difference in the trend of IHD mortality between GBD2010 and GBD2013 can be easily understood. The main reason is the different methods of chronic PHD redistribution in the two GBD studies. In GBD2010, the deaths from chronic PHD were redistributed to COPD from 1991 to 2010, and none of them were redistributed to IHD, which was the same as the original methods in the DSP system. However, in GBD2013, before 2004, the cases were redistributed to COPD, IHD, and HTD by different fractions based on the module. After 2004, all chronic PHD cases were redistributed to COPD by using the automatic coding software mentioned in the methodology section of this paper. By using the GBD2013 approach, owing to changing the redistribution fraction of chronic PHD, more IHD cases were adjusted in the early 1990s, which led to high mortality rates during the period.
The GBD approach is a systematic, scientific effort to quantify the comparative magnitude of health loss due to diseases, injuries, and risk factors according to age, sex, and geography for specific time points. The GBD study in China has a substantial impact on the Chinese policy orientation. To better promote the transformation of the findings of the GBD study to translate the policy, whether the GBD results are in line with the actual situation of China should be determined. Careful evaluation and validation of the GBD results is an important component of the GBD study. Our study will promote the allocation of GC in a manner that is more scientific and closer to reality. Moreover, evaluation and verification are important processes to promote the dissemination and policy.






 Quick Links
Quick Links
 DownLoad:
DownLoad: