-
As one of the 30 countries with the highest burdens of tuberculosis (TB) and multidrug-resistant tuberculosis (MDR-TB), China has the third largest number of TB patients in the world. Thus, TB control and prevention is an ongoing serious social health concern in China. To achieve the aim of ending the global TB epidemic, the recent World Health Organization (WHO) END TB Strategy requires accelerated reduction in the number of TB cases in the post-2015 era[1]. Therefore, enhancing the ability to identify TB cases in the National TB Control Program (NTP) has become particularly important.
According to the Fifth National TB Epidemiological Survey in China[2], presumptive TB patients usually visit non-NTP health-care facilities for their initial diagnosis; these are centers not designated medical facilities (DMFs) authorized by the Centers for Disease Control (CDCs), which include designated hospitals and TB dispensaries. Therefore, these non-NTP health-care facilities play an important role in the screening and referral of presumptive TB patients in China. To facilitate early diagnosis and standardized treatment, especially for presumptive TB patients without confirmed lab testing results, China has issued many public-public mix (PPM) measures via enactment of national laws and regulations, which dictate that all health-care facilities are obligated to report all presumptive TB cases in the national Infectious Disease Reporting System (IDRS) and to refer these cases to DMFs. In turn, DMFs are responsible for tracing patients who are lost to follow-up during the transfer process, conducting further evaluation, and registering confirmed cases with the national Tuberculosis Information Management System (TBIMS)[3]. Due to successful execution of these PPM measures, the rate of proper referral of TB cases from non-NTP health care facilities to DMFs has been substantially increased[4].
Although these PPM referral strategies have proved efficient, a gap remains for presumptive patients who do not arrive at DMFs for further diagnosis and treatment. This implies that there are barriers to collaboration between the DMFs and non-NTP health-care facilities, and some presumptive TB patients may not be managed within the NTP. Using national TBIMS records, we can assess the number of presumptive TB cases who have not been properly referred to DMFs. However, to the best of our knowledge, there are limited national data in China regarding the characteristics of these patients and the reasons for their loss to follow-up. This retrospective study aimed to describe referred cases and the factors related to their loss to follow-up during referral and tracing processes among all presumptive TB cases reported by non-NTP health-care facilities in 2015, and to use the results to further improve TB case identification in China.
This study retrospectively investigated all case reports in the IDRS of presumptive TB cases reported by non-NTP health-care facilities from January 1 to December 31, 2015. Data of the general sociodemographic characteristics of this population, their referral status, and diagnosis results were collected from the IDRS and TBIMS. Cases reported by NTP DMFs were excluded and all duplicated records were removed. Factors affecting unsuccessful referral were the key analytic output. The reasons for loss to follow-up during the referral and/or tracing processes were also obtained from the TBIMS database. Frequency and percentage were used to summarize the data.
According to national tuberculosis diagnostic criteria (WS288-2008)[4], patients meeting one of the following criteria are defined as presumptive TB patients. A) Children under 5 years old who have pulmonary TB (PTB) symptoms and have close contact with smear-positive PTB patients or a strongly positive Purfied Protein Derivatives Tuberculin Test (PPD) reaction; B) chest radiography findings of active PTB lesions consistent with clinical manifestations of primary PTB, disseminated hematogenous PTB, secondary PTB or tuberculous pleuritis.
All data were processed using Microsoft Access 2007, and statistical analyses were performed using SPSS 17.0 (SPSS Inc., Chicago, Il, USA). Logistic regression modeling was used to carry out univariate and multivariate analysis; variables with P value less than 0.1 were included in the multivariate analysis. P < 0.05 was considered statistically significant.
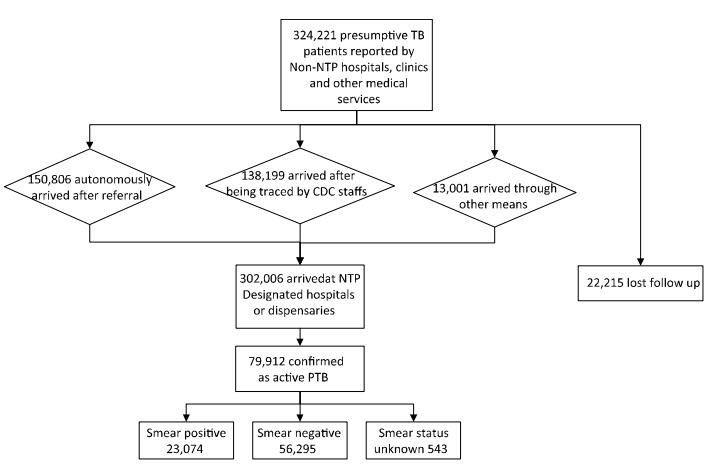
In 2015, there were 324, 221 presumptive PTB cases reported by non-NTP health-care facilities. Among them, 302, 006 cases successfully arrived at DMFs for further diagnosis and treatment, whereas 22, 215 cases were lost to follow-up, yielding a general arrival rate of 93.1%. In addition, 150, 806 patients (49.9%) visited DMFs themselves, after being transferred by non-NTP health-care facilities; 138, 199 (45.8%) patients passively arrived at DMFs after being urged to do so by health care workers (HCWs); 13, 001 (4.3%) patients completed the transfer process but not by the means mentioned above. Of 302, 006 presumptive cases, 79, 912 patients were finally diagnosed with PTB, including 23, 074 (28.9%) smear-positive cases, 56, 295 (70.4%) smear-negative cases, and 543 (0.7%) cases with unknown results (Figure 1).
As shown in Table 1, the rate of arrival at DMFs of presumptive cases was slightly lower among male patients (92.9%) than that among female patients (93.7%), and this difference is statistically significant. For different age groups, we found that children (0-14 years old), adults (15-64 years old), and older adults (65 years old or older) accounted for 1.4%, 73.3%, and 25.3%, respectively, of all reported presumptive cases; multivariate analysis revealed that there were no statistically significant differences when children were set as reference. In addition, most (73.3%) reported cases were local permanent residents, followed by migrants (19.1%) from the same province but a different county; the remaining cases were migrants (7.5%) from other provinces. Univariate analysis showed that rates of loss to follow-up were significantly different among these groups [unadjusted odds ratio (OR) = 11472.4, P < 0.001]; multivariate analysis results also indicated that migrants have a higher risk of loss to follow-up compared with local residents (adjusted ORs = 4.126 and 5.003, respectively). When comparing different occupations, more than half of presumptive patients were farmers or herdsmen (53.5%), followed by unemployed laborers (14.7%); all other occupations together accounted for less than 8%. There were significant differences by occupation (unadjusted OR = 2983.7, P < 0.001). Compared with farmers and herdsmen, pre-school children (adjusted OR = 2.361), unemployed laborers (adjusted OR = 1.274), retirees (adjusted OR = 1.068), and people with other occupations (adjusted OR = 1.993) had higher rates of loss to follow-up during the referral and tracing processes. We also observed that 57.8% of cases went to health-care facilities within a week of symptom onset, 24.2% within a month, 14.9% within 6 months, and 3.1% delayed the visit for 6 months or longer. Compared with those patients who immediately sought medical care, the remaining three groups had lower rates of loss to follow-up (adjusted ORs = 0.835, 0.667, and 0.836, respectively).
Item Unsuccessful Transfer Successful Transfer Univariate Analysis Multivariate Analysis Cases Percentage(%) Cases Percentage(%) Wald P Exp(B) 95%CI of Exp(B) Wald P Exp(B) 95%CI of Exp(B) Lower Upper Lower Upper Sex < 0.001 46.0 < 0.001 Male 15, 732 7.1 205, 049 92.9 ref ref Female 6, 483 6.3 96, 957 93.7 81.3 0.872 0.846 0.898 0.899 0.871 0.927 Age (years) 203.8 < 0.001 90.9 < 0.001 0-14 520 11.5 3, 994 88.5 ref ref 15-65 16, 584 7.0 221, 182 93.0 136.0 0.576 0.525 0.632 2.7 0.098 0.865 0.764 1.094 > 65 5, 111 6.2 76, 830 93.8 189.3 0.511 0.464 0.562 0.1 0.728 1.110 0.924 1.333 Residency 11472.4 < 0.001 9842.0 < 0.001 Permanent residents 8, 998 3.8 228, 789 96.2 ref ref Migrants from other counties in the same province 9, 007 14.5 52, 973 85.5 8733.8 4.323 4.193 4.458 7829.9 < 0.001 4.126 3.998 4.257 Migrants from other provinces 4, 210 17.2 20, 244 82.8 6892.0 5.288 5.084 5.500 5676.6 < 0.001 5.003 4.798 5.217 Occupation 2983.7 < 0.001 1105.0 < 0.001 Farmers and herdsmen 8, 956 5.2 164, 420 94.8 ref ref Pre-school children 320 17.7 1, 487 82.3 482.1 3.951 3.495 4.466 62.1 < 0.001 2.361 1.907 2.924 Students 745 7.0 9, 916 93.0 66.3 1.379 1.277 1.490 3.3 0.070 1.089 0.993 1.194 Industrial workers 1, 643 7.0 21, 920 93.03 132.0 1.376 1.303 1.453 3.2 0.074 0.949 0.895 1.005 Unemployed laborers 4, 173 8.8 43, 453 91.2 845.3 1.763 1.697 1.832 138.3 < 0.001 1.274 1.223 1.326 Medical staff 54 5.2 985 94.8 0.002 1.006 0.765 1.325 0.3 0.583 0.925 0.699 1.223 Employees 399 6.5 5, 790 93.6 19.8 1.265 1.141 1.403 0.9 0.355 0.951 0.855 1.058 Retirees 1, 491 7.5 18, 508 92.5 181.8 1.479 1.397 1.566 4.7 0.031 1.068 1.006 1.134 Non-fixed occupation 1, 352 7.5 16, 590 92.5 176.9 1.496 1.410 1.588 2.6 0.107 0.950 0.892 1.011 Other 3, 082 14.0 18, 937 86.0 2420.3 2.988 2.860 3.121 851.7 < 0.001 1.993 1.903 2.088 Delay in seeking medical care 615.6 < 0.001 348.1 < 0.001 < 1 week 172, 877 92.3 14, 484 7.7 ref ref < 1 month 73, 561 93.8 4, 827 6.2 202.0 0.783 0.757 0.810 104.4 < 0.001 0.835 0.806 0.864 < 6 months 45, 989 95.2 2, 318 4.8 489.1 0.602 0.575 0.629 296.2 < 0.001 0.667 0.637 0.698 ≥6 months 9, 579 94.2 586 5.8 52.4 0.730 0.671 0.795 16.3 < 0.001 0.836 0.766 0.912 Table 1. Distribution and Factors of Presumptive Tuberculosis Patients Reported in 2015 by Non-NTP Health Facilities in China
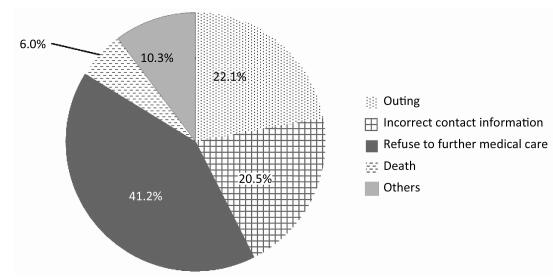
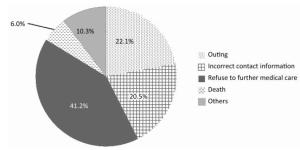
The main reason for loss to follow-up was that presumptive PTB cases refused to go to DMFs for further medical care, accounting for 41.2% (9, 157/22, 215) of all cases lost to follow-up. Of 22, 215 presumptive PTB cases lost to follow-up, 4, 907 (22.1%), 4, 546 (20.5%), and 1, 325 (6.0%) were due to outing, incorrect contact information, and death, respectively. In addition, among 9, 157 (41.2%) patients who refused to go to DMFs for further medical care, 1, 934 directly rejected the referral, and 7, 223 cases did not verbally reject the referral but never reached a DMF (Figure 2).
The general arrival rate of presumptive TB cases from non-NTP health-care facilities to DMFs was 93.1% in 2015, suggesting great improvement in comparison with the situation 10 years ago (82.6%)[5]. Despite great efforts made to improve the current referral strategy, a very large number of presumptive TB cases at non-NTP facilities result in staff experiencing a heavy workload. In view of insufficient compensation for these staff, the quality of patient referral is unsatisfactory, leading to a potentially increased rate of loss to follow-up. While the PPM strategy makes up for this to a large degree, 45.8% of referred cases were traced to DMFs after home visits or telephone tracing by NTP HCWs. In addition, our data revealed that 79, 912 (26.5%) presumptive TB cases were diagnosed as new PTB patients after being referred to DMFs; therefore, there were an estimated 6, 000 PTB patients from 22, 215 presumptive TB cases that were lost to follow-up in 2015. In view of the nature of TB as a serious infectious disease, missed opportunities to identify TB patients may result in transmission of the disease within the community. Greater effort should be made in China to strengthen its PPM strategy and to resume the management of lost patients within the NTP. Notably, a significantly low proportion of presumptive pediatric cases were identified in the TBIMS database, accounting for 1.4% of all presumptive TB cases, which was lower than an estimated 15% of the global TB burden[6]. This underreporting may reflect that the current medical care system in China still must strengthen its diagnostic capability for childhood TB[7], and our TBIMS may not reflect the true pediatric TB incidence. Female presumptive cases had lower risk of being lost to follow-up, which might be related to a greater willingness and ability to comply among female patients[8]. Our results showed that patients who sought medical care within a week were more likely to be lost to follow-up. Delays in seeking medical care might be associated with a patient's perception and knowledge of disease. When TB patients are at early stage with mild symptoms, they are likely to ignore the diagnosis and do not seek hospital health services. In addition, migrant populations had significantly higher risk of being lost to follow-up than local permanent residents. On one hand, migrant populations usually have unstable work and poor living conditions; therefore, they often conceal health problems in order to keep their job and income. Additionally, owing to unstable health insurance, they prefer to go to small private clinics or return to their hometown for medical care. On the other hand, migrants frequently change their workplace and contact information, which could also influence their compliance with referral[9]. In terms of occupation, farmers and herdsmen accounted for the highest percentage of all presumptive TB cases whereas they had the lowest risk of loss to follow-up. The high referral rate may be associated with favorable compliance among this population. In contrast, unemployed laborers and retirees had a high risk for loss to follow-up, which is attributable to their unstable income and health insurance. Given the unsatisfactory referral rates of these presumptive cases, further targeted strategies should be formulated to improve the compliance of presumptive TB cases among these high-risk groups.
Among 22, 215 presumptive cases that were lost to follow-up, outing, and incorrect contact information were the most frequent causes, indicating that non-NTP health-care facilities should strengthen health education for patients and get patients information recorded correctly. In addition to factors affecting the referral of presumptive TB cases, the unsatisfactory conditions at DMFs is another likely important contributor to the loss to follow-up. Fortunately, the NTP has turned its attention to this underlying concern and a number of general hospitals have been included as DMFs, which might help to effectively reduce patients' psychological resistance towards being referred to DFMs[10].
Our findings of the reasons and risk factors for loss to follow-up can help in the design of strategies and interventions to improve identification of presumptive TB cases. The new modeling of PPM, with the inclusion of more general hospitals rather than TB dispensaries, may also help to improve the situation. Other specialized policies aimed at migrants and other high-risk populations or high-incidence areas are also under exploration. Furthermore, we should learn from the best practices and experiences of other counties including Vietnam[11] and Indonesia[12], among others. These countries have implemented various policies and activities to strengthen cooperation between NTP and other health-care facilities, and have thus reduced the risk of loss to follow-up during the referral process[13]. Some countries have extended the scope of referral agencies by working with pharmacies and other health service providers who can provide diagnosis and treatment for presumptive TB patients[14]. To facilitate the tracing process, researchers in Pakistan match medical record data with laboratory records[15]. China can implement some of the strategies being used in other countries with high TB burdens.
In conclusion, this study demonstrated the high referral rate of presumptive TB cases from non-NTP health-care facilities to DMFs in China owing to implementation of effective active case identification strategies. In addition, migrant populations, pre-school children, unemployed laborers, and retirees were identified as groups at high risk for loss to follow-up, which highlights that further targeted strategies should be formulated to improve the compliance of presumptive TB cases among these populations.
HTML
-
The authors would like to thank Dr. GUO Hui from the US Centers for Disease Control and Prevention for her help in editing the language of this manuscript.
-
DU Xin collected the data. LI Tao collected and analyzed the data and wrote the paper. WANG Li Xia and ZHANG Hui participated in the conception and design of the study. PANG Yu, DU Xin, and ZHANG Hui reviewed the protocol. LI Tao, DU Xin, and ZHANG Hui analyzed and interpreted the data. PANG Yu, DU Xin, ZHANG Hui, and WANG Li Xia critically reviewed the paper for intellectual content. ZHANG Hui and Du Xin contributed equally to the article.
-
The authors have no other funding or conflicts of interest to declare.






 Quick Links
Quick Links
 DownLoad:
DownLoad: