-
Leishmania is a parasitic disease caused due to infection with Leishmaniasis, which is prevalent in 88 countries across the globe [1]. Clinically, Leishmaniasisis is divided into 3 types: visceral leishmaniasis (VL), mucosal cutaneous leishmaniasis (MCL), and cutaneous leishmaniasis (CL) [2]. VL, which is known as kala-azar, is caused by Leishmania donovani specie (L. donovani); and the infected patient's skin often shows dark pigmentation and fever, hence the name kalaazar. In China, VL is considered as the most serious disease and is prevalent in Xinjiang, Inner Mongolia, Gansu, Sichuan, Shaanxi, and Shanxi provinces [3]. CL is rarely reported in China, as there were only 3 reported cases of CL in China since 2010, while the imported CL cases were caused by L. major [4, 5].
CL is mainly caused by Leishmania tropicalis or Leishmania gigantica, which is related to the bite of infected female phlebotomine sandflies. CL is an epidemic disease, with India, North Africa, and Mediterranean coastal countries representing the endemic regions [6, 7]. In China, CL is only found in Shawan and Karamay in Jungar basin, as well as in Northern Tianshan Mountains, Xinjiang. Since 1949, a large-scale diagnosis and control of important parasitic diseases that endanger human health have been carried out in China. However, with the increase in number of overseas workers, the number of imported CL cases has increased sharply and the sources of infection are mainly countries with relatively high prevalence of CL, such as North Africa, as well as Middle East and Central Asia[12]. After 1984, except in Zhengzhou in 2011, a case with unknown source of infection was found and there were no local cases of leishmania infection in Henan Province. In the past 50 years, the incidence of CL is low and many clinicians lacked the knowledge of its clinical manifestations, which often led to misdiagnosis.
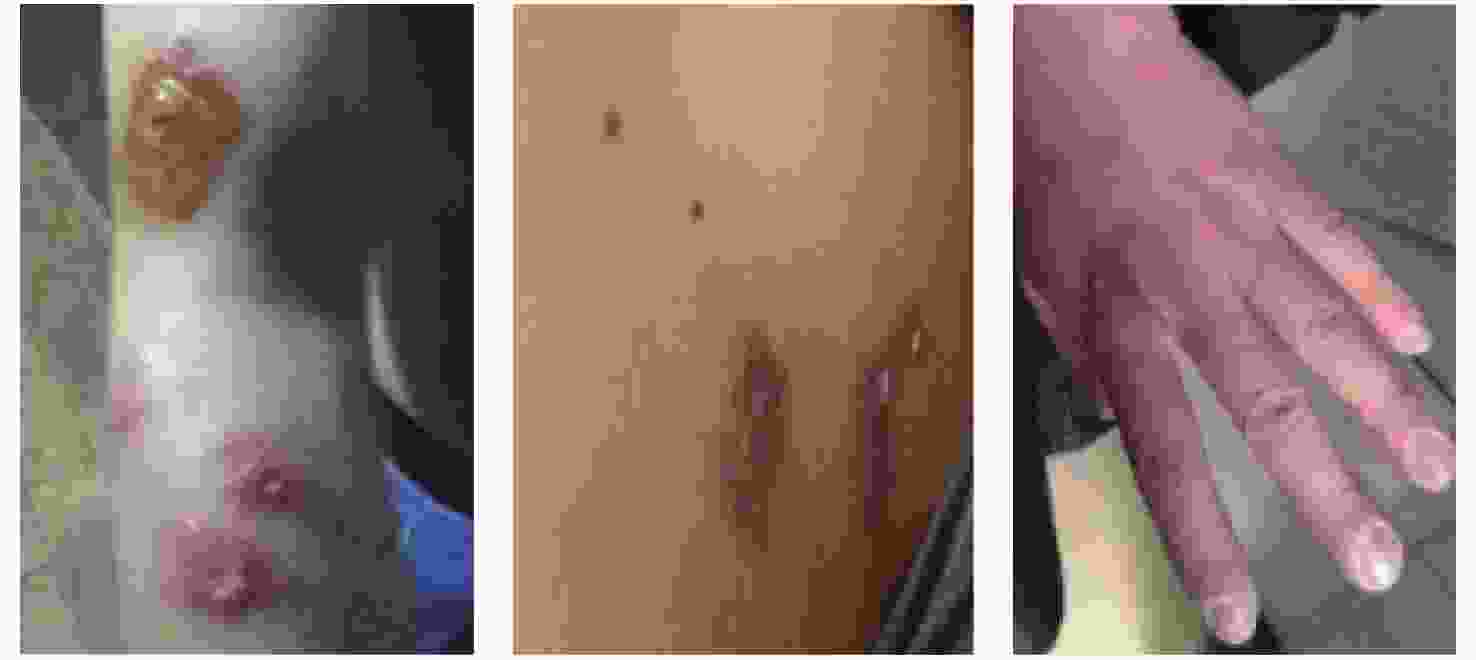
The Republic of Uzbekistan is a landlocked country located in Central Asia. In October 2017, an employee (Bai XX) who returned from the construction site of Uzbekistan was diagnosed with CL in Zhengzhou Sixth People’s Hospital. This is the first case of CL reported in Zhengzhou City in the past 50 years. In July 2017, Bai XX’s arms, back, dorsum of hands, and other parts showed swelling, ulceration, and pigmentation spots on the skin. In Karakuri, Uzbekistan, patients were diagnosed with CL in a local hospital. After hospitalization and treatment, he was discharged from the hospital on October 16, 2017. Later, some other employees showed similar symptoms. By January 2018, 9 people had skin damage. After returning to China, Bai XX visited the Zhengzhou Sixth People’s Hospital on October 30 due to skin swelling, erosion, and ulcers; and was diagnosed with CL. In addition, in December 2017, Zhang XX had scabby which exuded under the scab on the left clavicle. Yu XX had brown inflammatory spots on the popliteal fossa of his left leg (Figure 1). The other 6 people had skin damage but were not seriously infected. After treatment in foreign countries, the skin was not completely cured.
Henan Center for Disease Control (CDC) and Prevention paid close attention to these imported cases and handled the epidemic situation by pathogen diagnosis, treatment of patients, and vector investigation. According to the information reported by the network of epidemics of infectious diseases, the infection was traced back to the time of exposure. From December 2017 to January 2018, we conducted screening and etiological diagnosis of leishmaniasis for 180 migrant workers of the same construction project. The basic information of these workers were collected.
Blood test, skin lesions examination, and rK39 test were performed for 180 workers. For Leish rK39 test, in brief, 20 μL of serum was added to Leish rK39 dipstick paper card and then 2–3 drops of chase buffer solution was added to a test tube followed by addition of the dipstick into the test tube containing the chase buffer and readings were taken after 10 minutes. Among the 180 subjects, 18 had abnormal findings; whereas 9 had varying degrees of skin damage, including 3 with severe skin lesions. Three out of the 9 cases were positive on rK39 dipstick test. Five cases had hepatomegaly and splenomegaly, and one case had superficial lymph node enlargement.
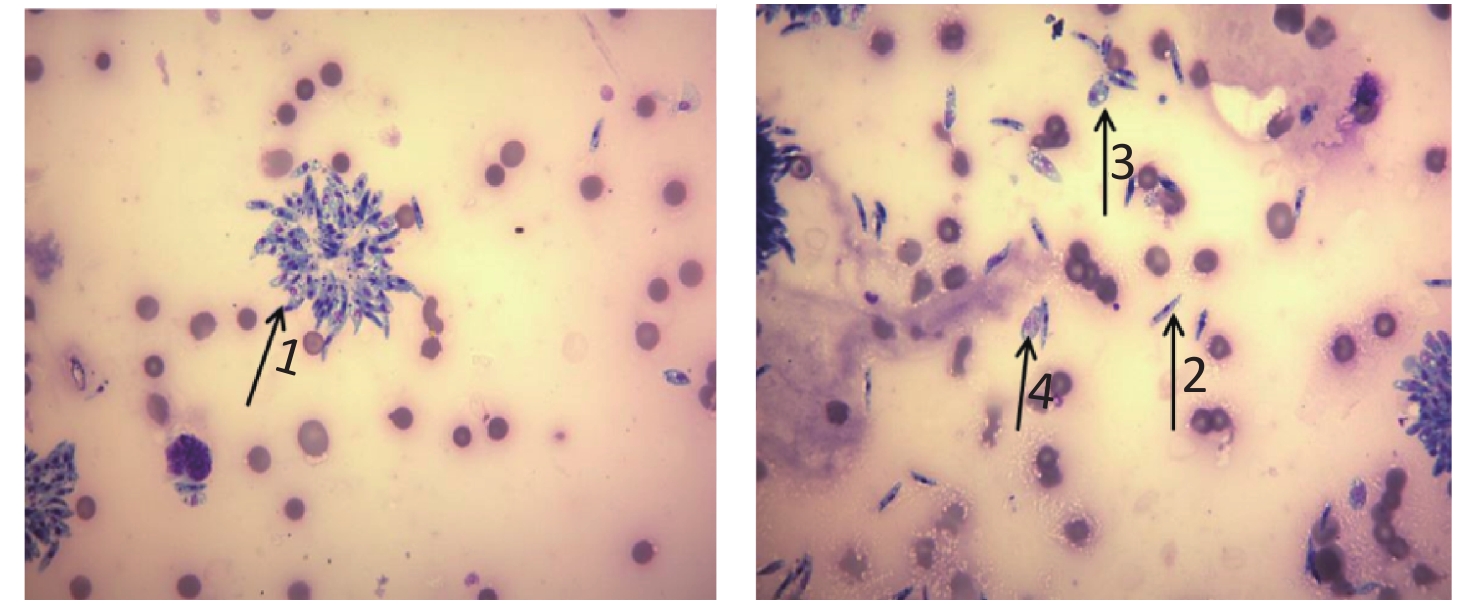
The tissue samples of typical skin lesions were collected for smear and culture. 75% alcohol was used to disinfect the skin lesions and marginal skin of the patients and a sterile scalpel was used to cut open the skin lesion and marginal skin of the patients. A part of the skin lesion tissue was directly smeared and stained with Giemsa and no amastigotes was observed under an oil microscope. The skin tissues specimens were collected and cultured in a sterile NNN medium (Novy-Macneal-Nicolle culture medium) at 25 ℃. A small amount of medium was taken every 2–3 days and Giemsa staining was performed to observe the presence of promastigotes and amastigotes under an oil microscope (Figure 2).
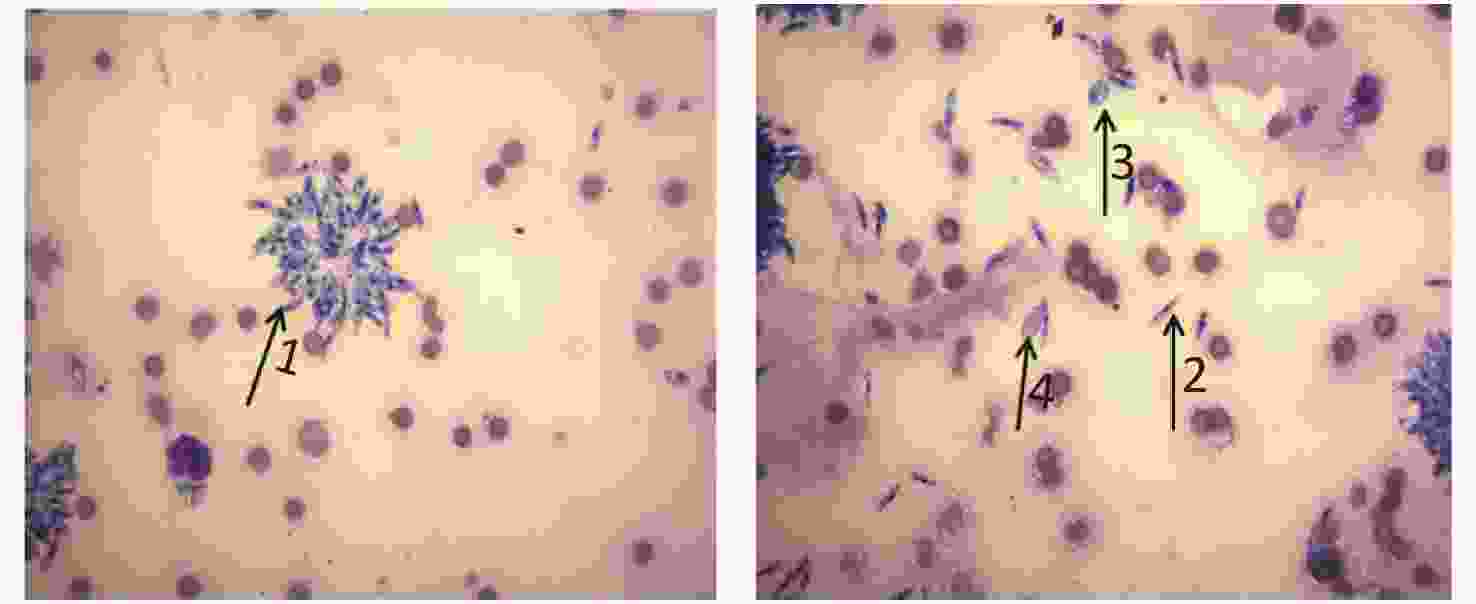
Figure 2. Leishmania amastigotes and promastigotes in NNN culture solution (Giemsa staining, × 1,000)
Nucleic acid was extracted from positive culture with Qiagen nucleic acid extraction kit according to the manufacturer’s instruction. The nucleic acid obtained was stored at 20 ℃ for until further use. Primers K13A-K13B and L5.8S-LITSR were used for kDNA and ITS1 amplification in ribosomal DNA, respectively (Table 1) [8, 9].
Gene name Kinetoplast DNA Internal transcribed spacer of rDNA Forward primer K13A: 5′ -GTGGGGGAGGGGCGTTCT-3′ LITSR: 5′-CTGGATCATTTTCCGATG-3′ Reverse primer K13B: 5′-ATTTTACACCAACCCCCAGTT-3′ L5.8S: 5′ -TGATACCACTTATCGCACTT-3′ Product length(bp)120 120 350 Table 1. Primer sequences of PCR
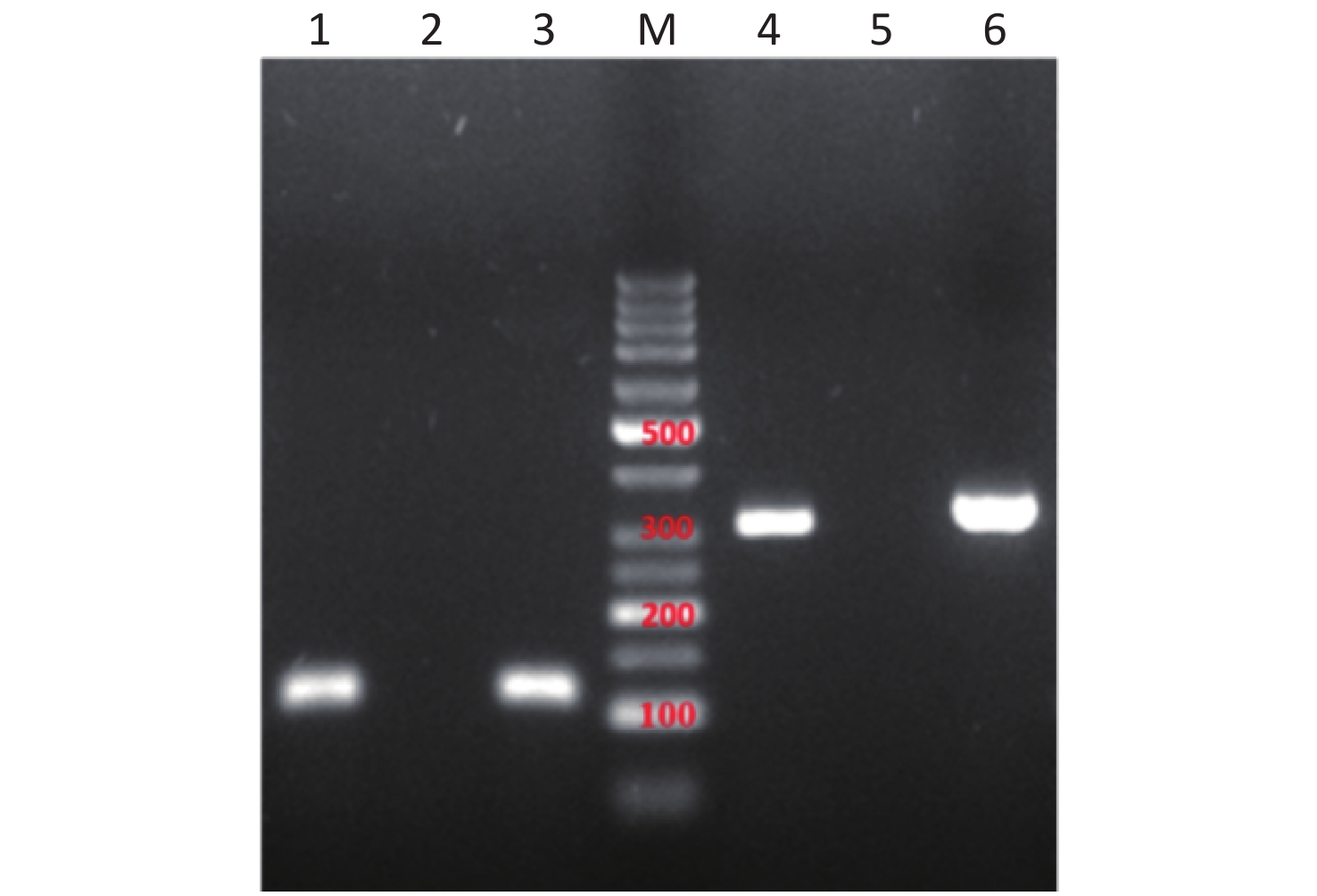
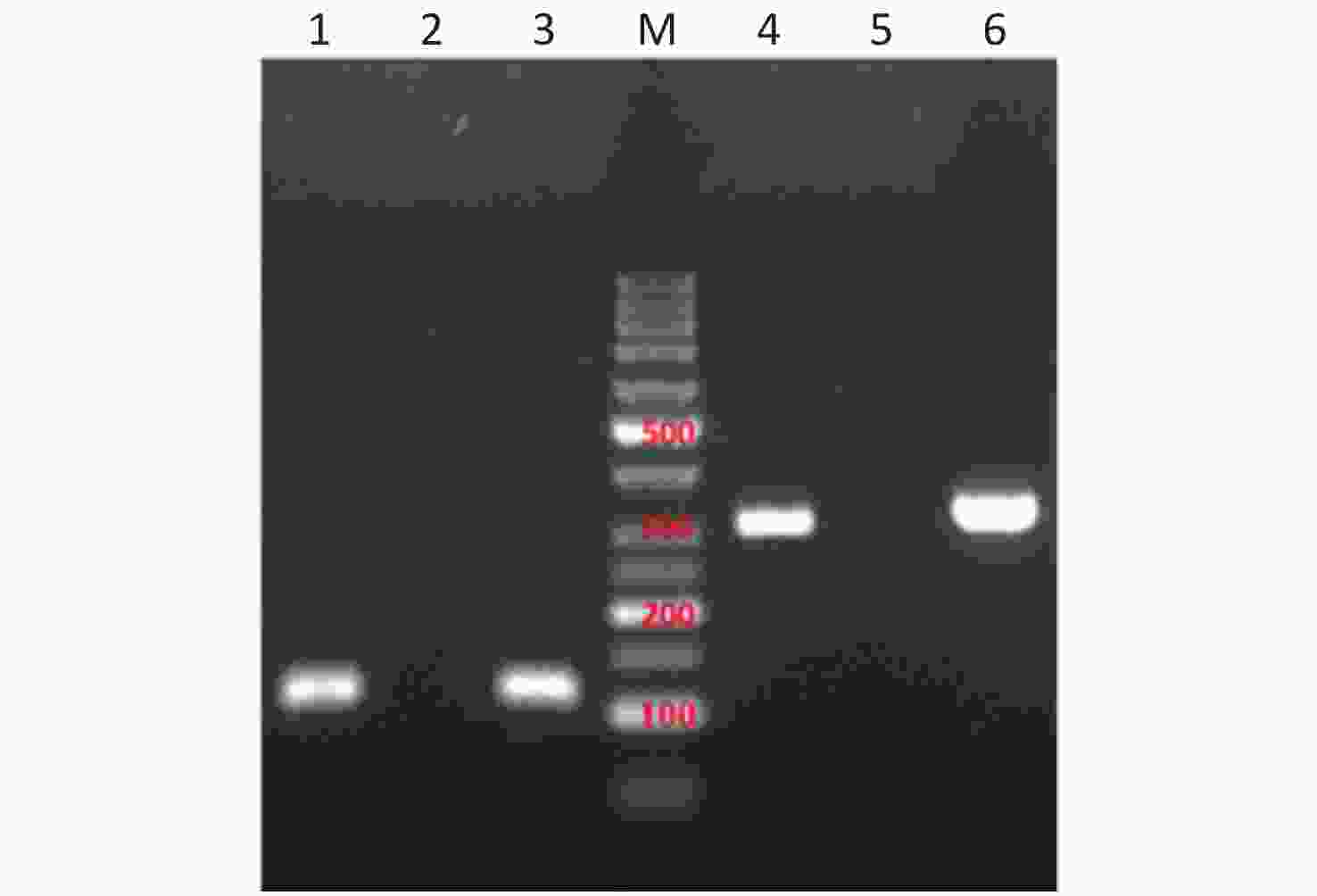
The polymerase chain reaction (PCR) system (50 µL) is as follows: 2× PCR Master Mix 25 µL; forward and reverse primers (1.5 µL each); DNA template of 5 µL (50 ng/µL); and ddH2O supplemented to 50 µL. The reaction conditions were: 94 ℃ for 3 min; 94 ℃ for 30 s; 58 ℃ for 30 s (52 ℃ for L5.8S-LITSR); 72 ℃ for 1 min (45 s for L5.8S-LITSR); (35 cycles L for 5.8S-LITSR); and 72 ℃ for 5 min. 5 µL amplification products were subjected to 2% agarose gel electrophoresis. In the results, there were about 120 BP and 350 BP fragments that were amplified out, which are consistent with those reported by Doudi M and Hejazi SH, et al. [10] (Figure 3). The amplified products of K13A-K13B and L5.8S-LITSR were sequenced by Shanghai Biotechnology Co. Ltd and the sequences were aligned using NCBI database. The two amplification products were 90% and 98% homologous to the corresponding sequences of L. major, respectively.
Luoyang Center for Disease Control and Prevention organized the surveillance and investigated sandflies in its jurisdiction. From April to July, sandflies were collected from various districts and counties and the parasites species were identified as Phlebotomus chinensis using molecular assays in parasitological positive specimens.
At present, there are four known species of sandflies that transmit leishmaniasis in China: P. chinensis, P. longiductus, P. Wui, and P. alexandri. Since 1970, no Phlebotomushas been found in the plain areas of Henan province; however, there are some Phlebotomus in the mountain and hilly areas. The remnants of sandflies are mainly Phlebotomus chinensis and scaly-beak Sergentomyia.
According to the monitoring results of sandflies in Linzhou City, P. chinensis, Phlebotomus, and scaly-beak Sergentomyia were the main species in Henan. Luoyang CDC conducted a sandfly surveillance from April to July 2018 in Luoning county and other jurisdictions and reported that all the sandflies were P. chinensis. However, the main vectors of CL are Phlebotomus papatasi and Phlebotomus sergenti. There is low of risk cutaneous leishmaniasis transmission in our province, due to the difference and blocking of the transmission link of the media.
Dermatologically, this disease is diagnosed as biting dermatosis. As Leishmania propagates into the lesion tissues, the absence of solustibosan causes delayed healing of the lesion and causes great psychological pressure on patients. All cases were cured and improved after undergoing wound treatment, systemic application of solustibosan, and topical application of amphotericin B and miltefosine. The lesions were gradually healed and prognosis remained good.
Up till date, although it is not clear whether the sandflies in Henan can serve as the vector of leishmaniasis, the imported leishmaniasis has become a potential threat to people's health, with the aggravation of population mobility in China. Therefore, the relevant departments must attach great importance to it. The possibility of CL should be suspected in migrant workers with skin injury who return from the endemic regions of leishmaniasis.
Acknowledgement Institute of Parasitic Diseases of the Chinese Center for Disease Control and Prevention, Luoyang Entry-Exit Inspection and Quarantine Bureau, Luoyang Health and Family Planning Commission and Luoyang Centerfor Disease Control and Prevention.
Investigating the Aggregation of Imported Cutaneous Leishmaniasis in Henan, Central China
doi: 10.3967/bes2021.032
- Received Date: 2020-05-31
- Accepted Date: 2020-09-21
| Citation: | ZHAO Yu Ling, LI Su Hua, ZHU Xin, ZHOU Rui Min, YANG Cheng Yun, LIU Ying, NIU Yuan Na, LU De Ling, ZHANG Hong Wei, ZHAO Dong Yang. Investigating the Aggregation of Imported Cutaneous Leishmaniasis in Henan, Central China[J]. Biomedical and Environmental Sciences, 2021, 34(3): 247-249. doi: 10.3967/bes2021.032 |







 Quick Links
Quick Links
 DownLoad:
DownLoad: