-
Cognitive impairment, especially dementia, is common in elderly individuals and seriously affects life quality. Dementia is the most severe expression of cognitive impairment characterized by a progressive functional decline in one or more cognitive domains. The prevalence of dementia has increased dramatically, and the number of patients with dementia will reach 130 million in 2050[1]. The worldwide prevalence of dementia among elderly individuals is approximately 5.0%[2]. In China, more than 220 million people aged over 60 years in 2016. As aging intensifies and the number of patients increases, dementia will become a significant public health problem[3].
Vascular disorders have been identified as modifiable risk factors for cognitive impairment. Hypertension (HTN) plays an essential role in vascular diseases. To reduce the risk of cognitive impairment, the World Health Organization (WHO) set a global target, which was reducing the prevalence of HTN to 25% in 2025[4]. Hyperhomocysteinemia (HHcy), elevated levels of plasma homocysteine, were associated with an increased risk of chronic disease, especially among elderly individuals. Many studies have examined the relationship between hyperuricemia and cognitive impairment, but the findings are conflicting. Hypertension with hyperhomocysteinemia (HTN-HHcy) has recently received increasing attention. However, few studies have examined the efforts of HTN-HHcy on cognitive impairment. Our study aimed to explore the relationship between HTN-HHcy and the risk of cognitive impairment based on the cross-sectional Asymptomatic Polyvascular Abnormalities Community (APAC) Study.
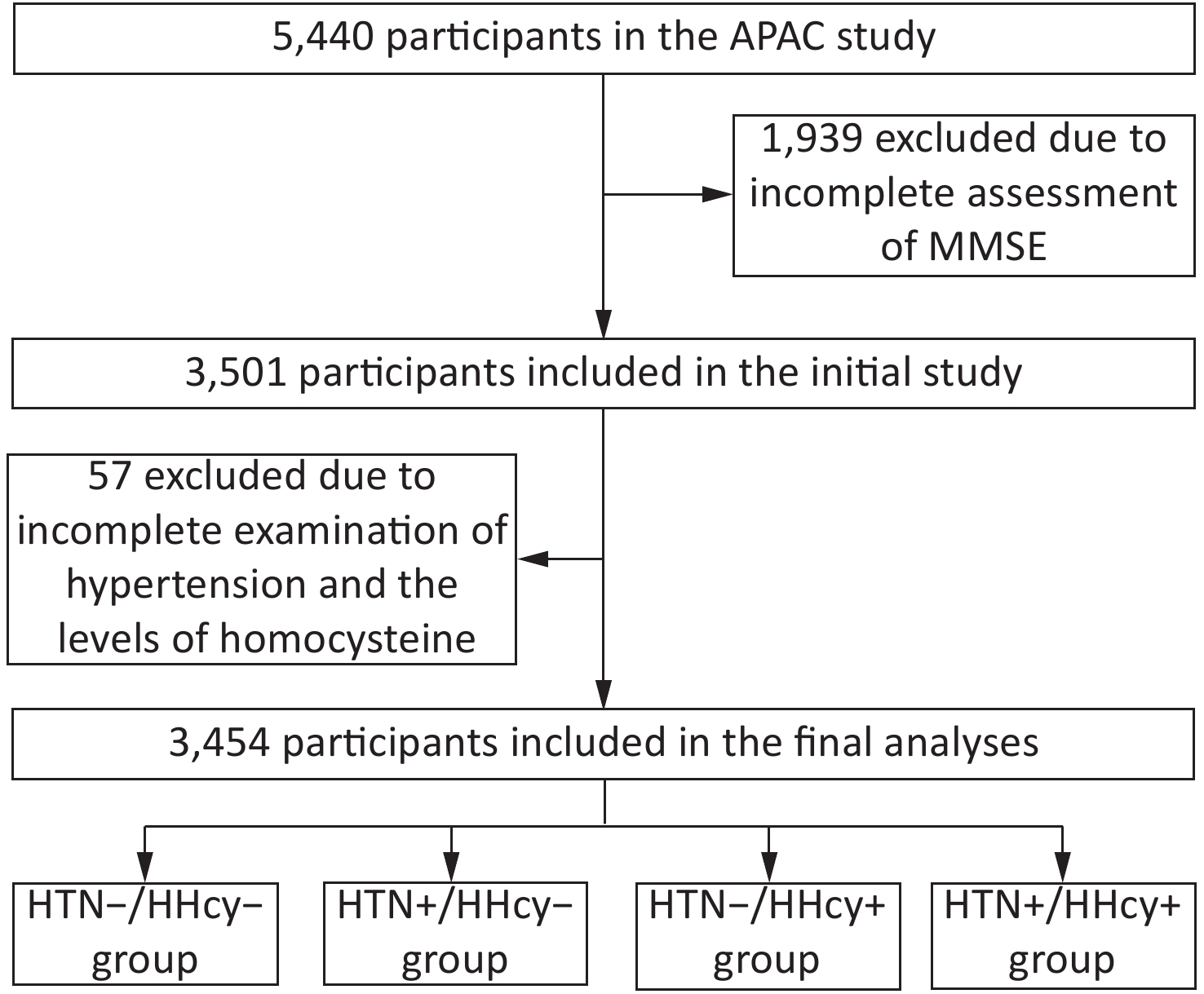
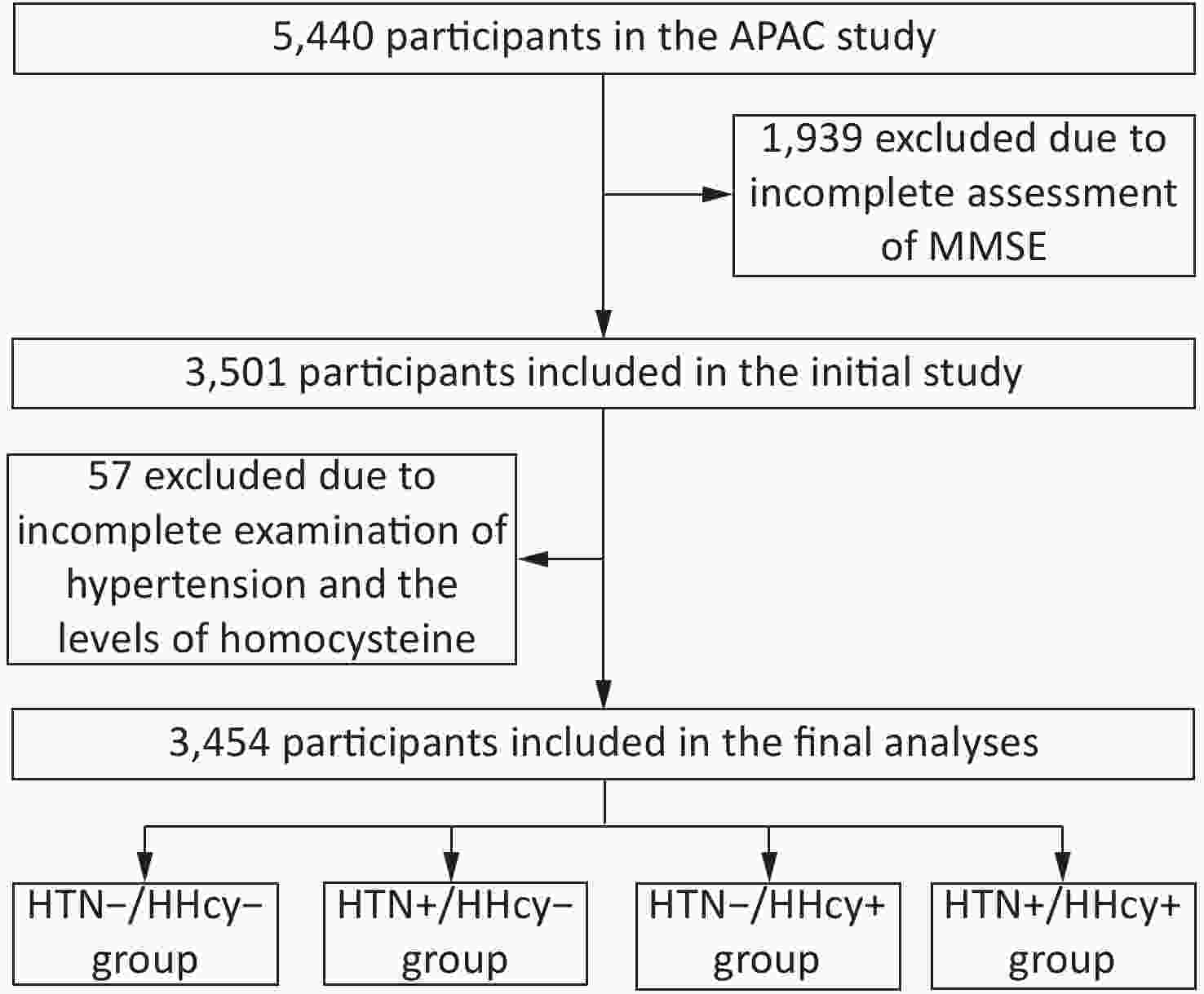
Participants in the present study were recruited from the APAC study. The inclusion criteria for the APAC study were 1) ≥ 40 years old; 2) complete and available basic information; and 3) free of stroke, myocardial infarction, transient ischaemic attack, coronary heart disease, and neurological deficits. Among the 5,440 participants, we finally identified 3,454 observers who had complete data on the Mini-Mental State Examination (MMSE), blood pressure, and levels of homocysteine (Supplementary Figure S1 available in www.besjournal.com). The study was conducted according to the guidelines of the Helsinki Declaration and was approved by the ethics committee of Kailuan General Hospital of Tangshan City. Written informed consent was obtained from all study subjects.
HTN was defined as systolic blood pressure (SBP) ≥ 140 mmHg or a diastolic blood pressure (DBP) ≥ 90 mmHg, a history of hypertension, or taking antihypertensive drugs. The blood pressure of each participant was measured twice by a mercury sphygmomanometer, and the average of the two readings was calculated. Plasma total homocysteine (tHcy) concentration was measured by sandwich enzyme-linked immunosorbent assay (Quantikine ELISA, R&D Systems Inc.). HHcy was defined as a plasma homocysteine level greater than 15 µmol/L[5].
MMSE was used as a cognitive screener to assess respondents’ abilities with respect to time, place, language, construction, learning, calculation, attention, delayed recall, and memory. The MMSE comprises 30 items, and the total score ranges from 0 to 30 points, with a lower score reflecting greater cognitive impairment. Cognitive impairment was defined as MMSE scores ≤ 24. In this study, cognitive impairment was defined as a score ≤ 24 for junior school graduates or above (≥ 9 years of education); a score ≤ 20 for primary school graduates (≥ 6 years of education); and a score ≤ 17 for illiterate individuals[6].
Demographic information including age, sex, marital status, education level, per capita monthly income, physical activity, current smoking status, and current alcohol consumption was collected from questionnaires. The body mass index (BMI) was calculated as the weight (kg) divided by the height squared (m2). All participants were measured for the levels of fasting blood glucose (FBG), total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C). All blood samples were tested with a Hitachi 747 autoanalyzer (Hitachi; Tokyo, Japan). Diabetes mellitus was defined as a fasting blood glucose ≥ 126 mg/dL or treatment with diabetes medication. Dyslipidaemia was defined as having either TC ≥ 200 mg/dL, or HDL-C < 40 mg/dL, or LDL-C ≥ 130 mg/dL, or TG ≥ 150 mg/dL, or the presence of a history of hyperlipidemia, or drug treatment for dyslipidemia.
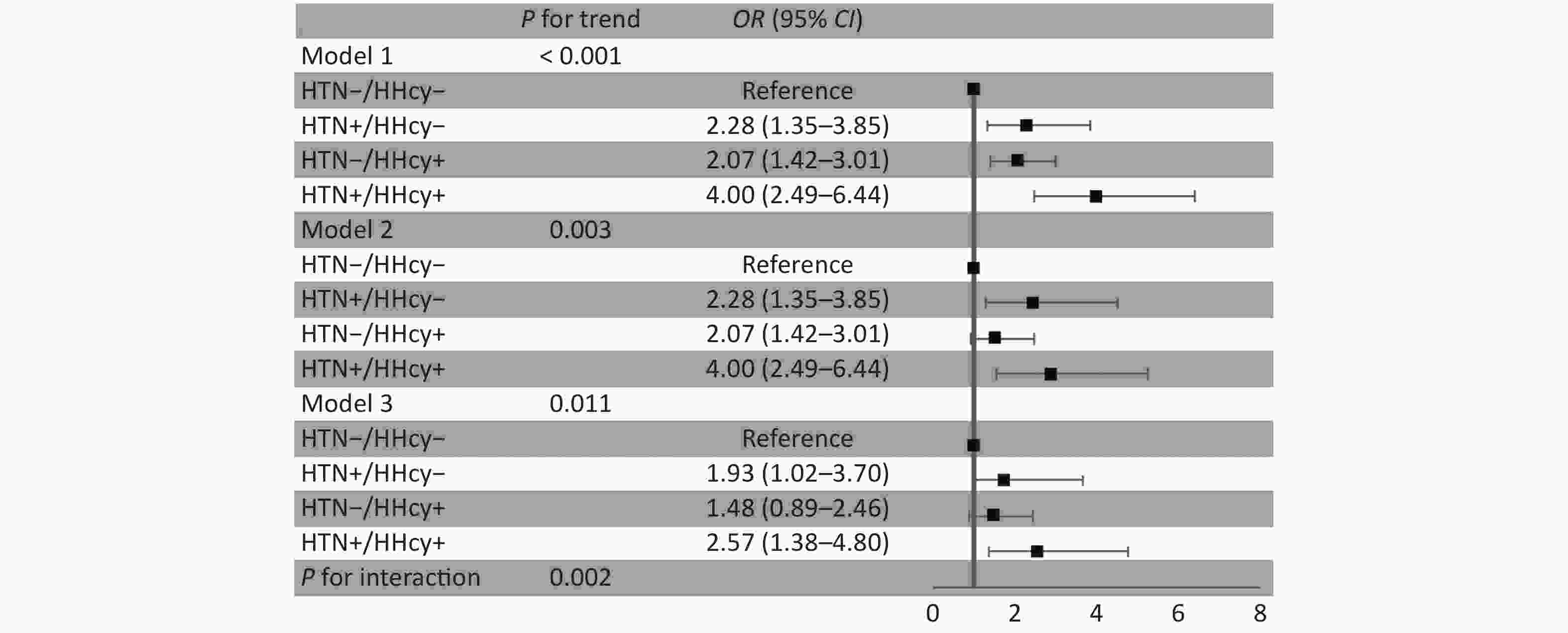
Subjects were divided into the following four groups according to whether they had HTN and HHcy: normal (no HTN and no HHcy, HTN-/HHcy-), isolated HTN (HTN but no HHcy, HTN+/HHcy-), isolated HHcy (no HTN but HHcy, HTN-/HHcy+), and HTN-HHcy (HTN with HHcy, HTN+/HHcy+). All continuous variables were normally distributed and tested using the Shapiro-Wilk test. Means and standard deviations were calculated for continuous variables. Categorical variables were described with frequencies and percentages and tested with Chi-square tests. Differences among groups were tested by one-way ANOVA for normally distributed variables. Logistic regression was used to analyze the associations between HTN, HHcy and cognitive impairment with odds ratios (ORs) and 95% confidence intervals (CIs). The model's adjustment variables were age, sex, education level, per capita monthly income, current smoking status, alcohol consumption, BMI, diabetes, and dyslipidemia. Statistical significance was set as a P value < 0.05. All statistical analyses were performed by SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Out of a total of 5,440 individuals enrolled in the study, 3,454 participants had measurements for blood pressure and tHcy: 16.8% of subjects were elderly (≥ 65 years old), and the mean age was 53 years (range: 40–89 years). The characteristics of the participants in our study are summarized in Table 1. Significant differences were found in age, gender, education level, physical activity, current smoking, drinking, dyslipidemia, diabetes, BMI, and LDL-C levels among the different groups (all P < 0.05). There were no significant differences in marital status, income, TC levels, or HDL-C levels among the different groups (all P > 0.05). The proportion of cognitive impairment in the HTN-HHcy group (10.7%) was higher than that in the normal, isolated HTN and isolated HHcy groups (2.9%, 6.4%, and 5.9%, respectively), and the difference was statistically significant (P < 0.05). In the present study, a higher prevalence of cognitive impairment was noted in the HTN-HHcy group than in the other group, which implied that HTN-HHcy might be associated with cognitive impairment.
Characteristics Total HTN-/HHcy- HTN+/HHcy- HTN-/HHcy+ HTN+/HHcy+ P Number of subjects (n, %) 3,454 1,747 (50.6) 327 (9.5) 1,110 (32.1) 270 (7.8) Age, years (n , %)* 53.9 ± 10.7 51.5 ± 9.3 54.5 ± 9.1 56.3 ± 12.1 58.9 ± 11.3 < 0.001# < 65 2,874 (83.2) 1,567 (54.5) 280 (9.7) 843 (29.3) 184 (6.4) < 0.001# ≥ 65 580 (16.8) 180 (31.0) 47 (8.1) 267 (46.0) 86 (14.8) < 0.001# Male (n, %) 1,961 (56.8) 715 (40.9) 178 (54.4) 845 (76.1) 223 (82.6) < 0.001# Education level (n, %) < 0.001# Illiteracy 16 (0.6) 1 (0.1) 2 (0.8) 7 (0.8) 6 (2.8) Primary 115 (4.1) 39 (2.6) 16 (6.0) 46 (5.3) 14 (6.5) Middle 2,294 (81.2) 1,208 (81.9) 203 (75.8) 704 (81.0) 179 (83.6) College 401 (14.2) 227 (15.4) 47 (17.5) 112 (12.9) 15 (7.0) Marital status (n, %) 0.255 Married 2,816 (98.2) 1,471 (98.6) 266 (97.8) 865 (97.5) 214 (98.6) Unmarried 52 (1.8) 21 (1.4) 6 (2.2) 22 (2.5) 3 (1.4) Physical activity (n, %) 0.017# Inactive 995 (34.4) 540 (36.0) 83 (30.1) 313 (35.0) 59 (26.9) Moderately 1,531 (53.0) 773 (51.5) 165 (59.8) 458 (51.2) 135 (61.6) Active 364 (12.6) 188 (12.5) 28 (10.1) 123 (13.8) 25 (11.4) Income,¥/month (n, %) 0.094 ≤ 1,000 823 (31.5) 453 (33.8) 85 (34.3) 229 (27.9) 56 (27.6) 1,000–3,000 1,234 (47.2) 608 (45.3) 113 (45.6) 409 (49.8) 104 (51.2) ≥ 3,000 557 (21.3) 281 (20.9) 50 (20.2) 183 (22.3) 43 (21.2) Current smoking (n, %) 672 (24.1) 246 (16.9) 51 (19.2) 297 (34.7) 78 (37.3) < 0.001# Current drinking (n, %) 593 (21.6) 244 (16.8) 64 (24.2) 226 (27.3) 59 (29.2) < 0.001# Dyslipidemia (n, %) 245 (8.5) 119 (7.9) 35 (12.7) 69 (7.7) 22 (10.1) < 0.001# Diabetes (n, %) 198 (6.9) 82 (5.5) 36 (13.0) 55 (6.2) 25 (11.4) < 0.001# BMI (kg/m2)* 24.9 ± 3.3 24.7 ± 3.1 25.9 ± 3.7 24.7 ± 3.2 25.7 ± 3.3 < 0.001# TC (mmol/L)* 5.2 ± 1.6 5.2 ± 1.0 5.3 ± 1.0 5.2 ± 2.4 5.2 ± 1.0 0.741 TG (mmol/L)* 1.7 ± 2.2 1.6 ± 1.8 1.9 ± 1.9 1.7 ± 2.9 1.9 ± 1.8 0.092 HDL-C (mmol/L)* 1.4 ± 0.5 1.4 ± 0.5 1.4 ± 0.5 1.4 ± 0.4 1.4 ± 0.8 0.208 LDL-C (mmol/L)* 2.5 ± 1.2 2.6 ± 1.0 2.7 ± 1.6 2.4 ± 1.4 2.5 ± 0.8 0.008# HCY (µmol/L)* 15.5 ± 9.3 9.9 ± 3.3 10.6 ± 2.9 23.7 ± 9.2 24.0 ± 9.5 < 0.001# SBP (mmHg)* 129.8 ± 19.7 124.2 ± 17.6 144.9 ± 19.8 129.5 ± 17.7 148.6 ± 19.7 < 0.001# DBP (mmHg)* 82.8 ± 11.1 80.2 ± 10.2 90.4 ± 11.7 82.7 ± 10.4 90.9 ± 10.6 < 0.001# Cognitive impairment (n, %) 166 (4.8) 51 (2.9) 21 (6.4) 65 (5.9) 29 (10.7) < 0.001# Note. HTN, hypertension; HHcy, homocysteinemia; BMI, body mass index; TC, total cholesterol; TG, total cholesterol; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; HCY, Homocysteine; SBP, Systolic blood pressure; DBP, Diastolic blood pressure.
*Mean ± standard deviation; #P < 0.05.Table 1. Baseline characteristics of subjects in the study groups
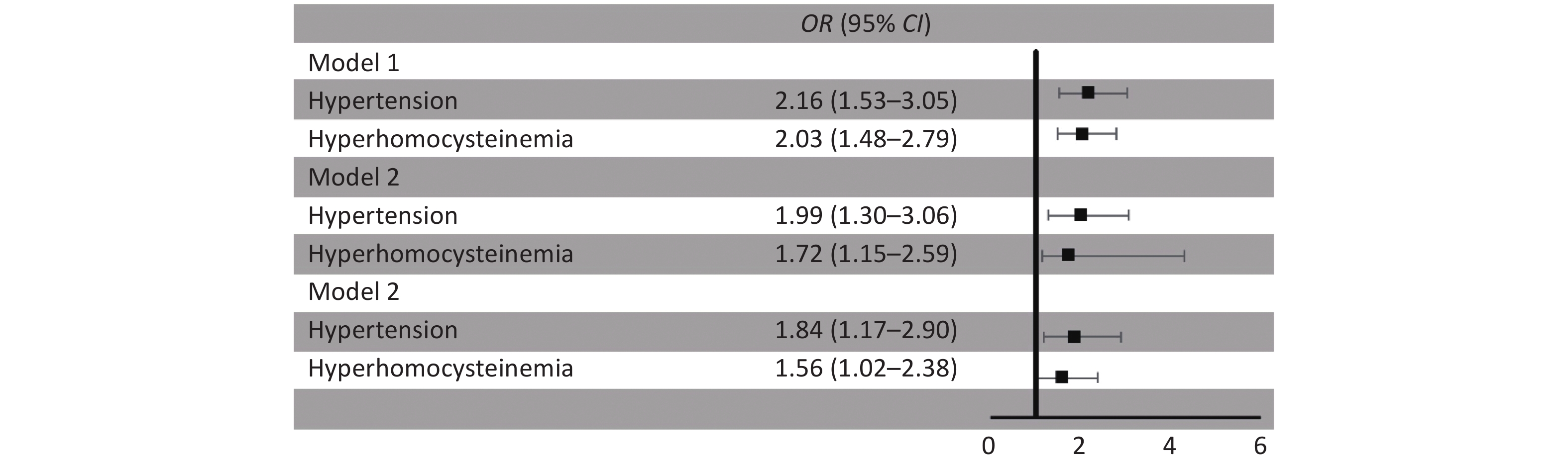
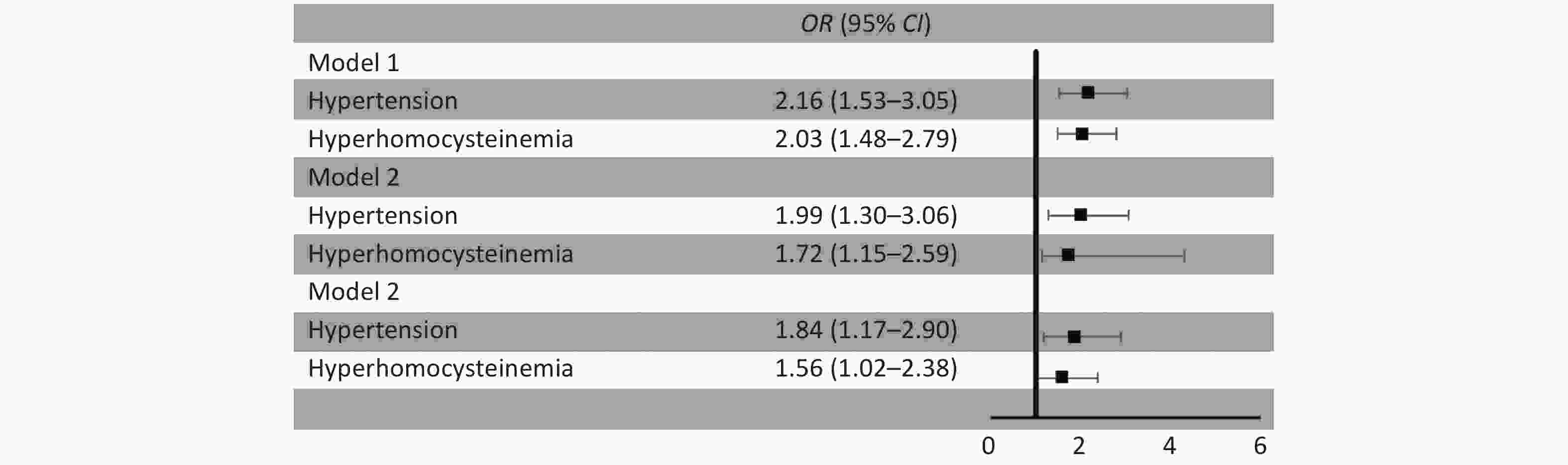
Multiple logistic regression analyses showed that participants with HTN had a higher risk of cognitive impairment (OR = 1.84, 95% CI: 1.17–2.90; P < 0.001), with non-hypertensive participants as a reference, after adjusting for multiple variables in model 3. A similar association was observed in the participants with HHcy (OR = 1.56, 95% CI: 1.02–2.38; P < 0.001) (Figure 1). In addition, while numerous studies show associations between HTN and HHcy with cognitive impairment, the interaction between HTN and HHcy was not considered. We drew the same conclusion in unisolated HTN, HHcy, and cognitive impairment, but after adjusting for the interaction, the analysis revealed that the results were inconsistent.
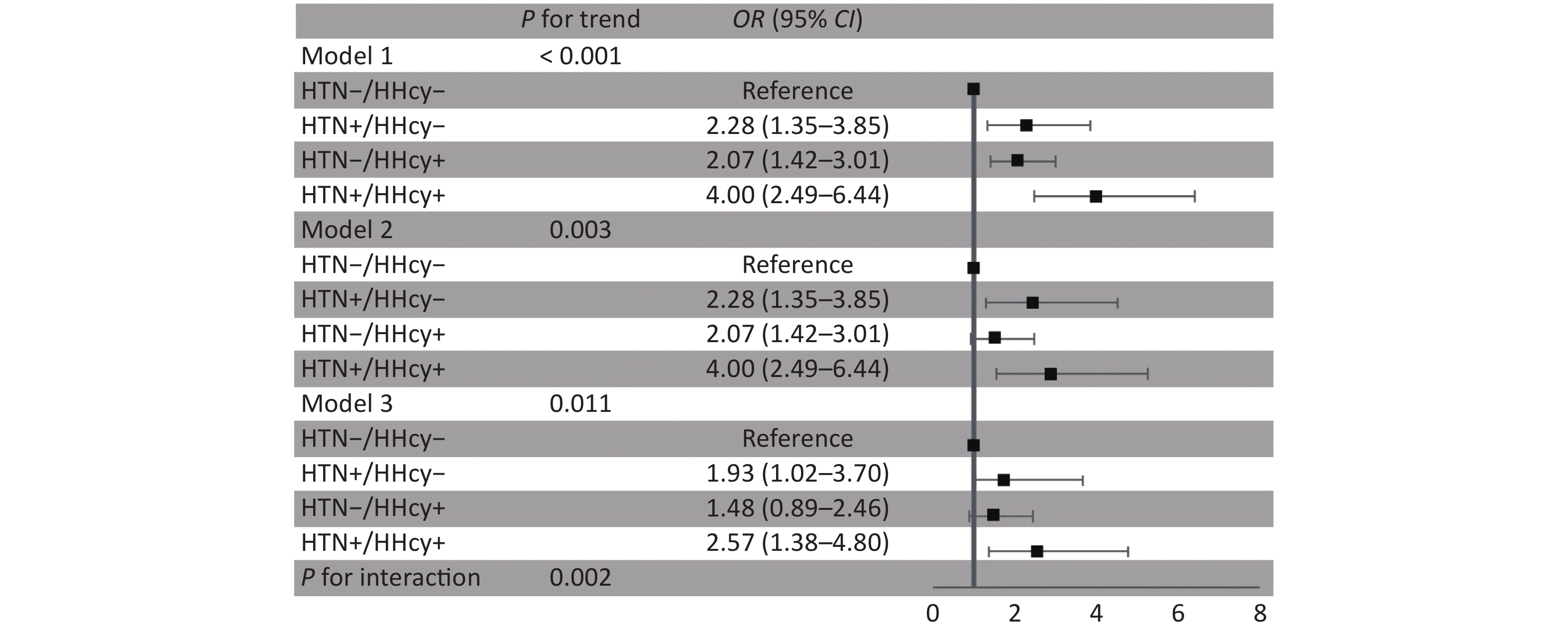
Our results showed that HTN-HHcy was associated with the risk of cognitive impairment (OR = 4.00, 95% CI: 2.49–6.44; P < 0.001). After adjusting for confounding factors, HTN-HHcy was still associated with cognitive impairment (OR = 2.57, 95% CI: 1.38–4.80; P value for interaction: 0.002). The HTN-HHcy group had a higher risk of cognitive impairment than the isolated HTN group (OR = 1.93, 95% CI: 1.02–3.70; P < 0.001) when the normal group was regarded as the reference. However, isolated HHcy was not significantly associated with cognitive impairment (OR = 1.48, 95% CI: 0.89–2.46; P > 0.05) (Figure 2).
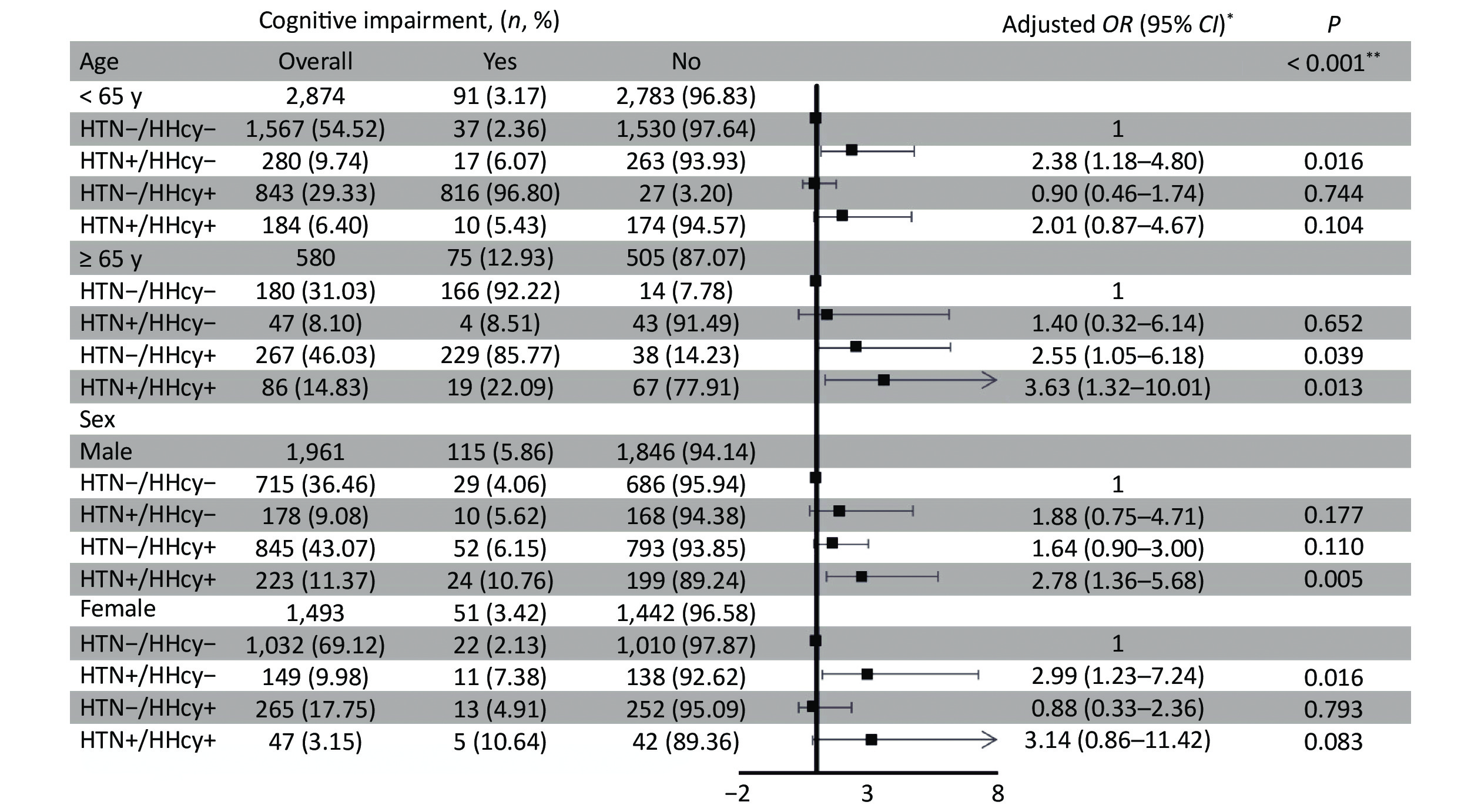
We also found that older people over 65 are at higher risk of cognitive impairment. Stratified analyses showed that the risk of cognitive impairment is higher in elderly patients with HTN-HHcy over 65 years old (OR = 3.63, 95% CI: 1.32–10.01). The adjusted OR and 95% CI of HTN-HHcy for cognitive impairment among participants younger than 65 were 2.01 (0.87–4.67) (Supplementary Figure S2 available in www.besjournal.com).
Figure S2. Association of hypertension and hyperhomocysteinemia with cognitive impairment between different ages and genders in our study.
The synergistic effects of HTN and HHcy may be explained by the fact that HHcy activates the angiotensin-converting enzyme by inhibiting the production of endogenous hydrogen sulfide from leading to or aggravate HTN[7]. The predictive role of HTN for cognitive impairment has been widely proven, and chronic conditions of HTN lead to deterioration of cognitive impairment in the test that assesses hippocampal functions. HTN can cause damage to the hippocampus and produces typical features such as hypoperfusion, brain amyloid deposition, and neuroinflammation[8]. Although the direct association between HHcy and cognitive impairment is controversial, there have been studies demonstrating the potential mechanisms by which Hcy may induce cerebral arteriosclerosis and catalyze the development of cognitive impairment, such as increased oxidative stress of body tissue, alterations of lipid metabolism, impaired endothelial function, increased adhesion of platelets and induced thrombosis[9, 10]. Therefore, when HTN and HHcy are combined, the effects on cognitive impairment may be increased, especially in elderly individuals (≥ 65 years old) at high risk of neurodegenerative disease.
Although our study includes a large sample size and adjustments for a variety of potential confounders, some limitations should be noted. First, we measured the Hcy concentration but not the Hcy activity in the 2012 participant, which might produce a positive bias to evaluate the effect of Hcy. Second, the study was performed based on participants in China who were 40 years old or older. Therefore, it may not be generalizable for young people who were under 40 years old. In addition, the sample size of participants age ≥ 65 was relatively small. Finally, in this cross-sectional study, we cannot make causal inferences and obtain more convincing results.
In conclusion, we suggest that HTN-HHcy was positively associated with the risk of cognitive impairment. Our findings indicated that HTN-HHcy might be a useful marker for cognitive impairment risk assessment.
The authors confirm that there are no conflicts of interest.
The authors would like to thank Prof. LI Dong, Prof. LI Xiao Dong, and Prof. JI Long for their kind assistance in proofreading the manuscript and discussion.
All authors critically reviewed and edited the manuscript and approved the final version for submission. CHEN Xue Yu, YANG Yao, DING Guo Yong, TANG Zhao Yang undertook the statistical analysis and drafting of the manuscript. Field surveys and data collection were performed by SHI Feng Xue, CHEN Yan Ru, WANG Xiao Hui, TAN Tan, XING Wei Jia, HOU Hai Feng. We thank all of the participants and their relatives who were enrolled in our study.
HTML
Reference






 Quick Links
Quick Links
 DownLoad:
DownLoad: