-
To implement the national policy of focusing on grassroots and prevention, and to promote a shift from hospitals to the community as the main locus of cardiovascular disease (CVD) prevention and control efforts, the National Center for Cardiovascular Diseases organizes compilation of the Report on Cardiovascular Health and Diseases in China by experts in related fields nationwide every year, to provide detailed scientific information and support for health administrators and professionals. In 2019, CVD accounted for 46.74% and 44.26% of the causes of death in rural and urban areas, respectively: two of every five deaths were due to CVD. The burden of CVD will continue to increase as China faces the dual pressures of an aging population and the continued increasing of metabolic risk factors. These pressures will affect disease prevention and control strategies and resource allocation, such as primary prevention efforts to decrease CVD incidence. In addition, they will require greater allocation of medical resources to address the rapidly increasing number of cardiovascular emergencies, and to provide rehabilitation and secondary prevention medical services aimed at decreasing the risk of recurrence, rehospitalization and disability among CVD survivors. The number of people with hypertension, dyslipidemia or diabetes in China has reached hundreds of millions. Moreover, the number of people requiring lifelong treatment with multiple drugs to prevent CVD is increasing. Further research is necessary to formulate more effective strategies to improve CVD awareness, treatment and control. Because most of these elevated risk factors are insidious, by the time they are detected, they have often led to vascular lesions or even more serious events, such as myocardial infarction and stroke. Although subclinical atherosclerosis are prevalent, vascular injury and treatment have not been a priority for prevention. A growing body of evidence suggests that maintaining vascular health is an important foundation for preventing CVD and degenerative disease. Therefore, strengthening the primordial prevention strategy for hypertension, dyslipidemia, diabetes, obesity, and smoking is of utmost importance. In addition, the assessment of cardiovascular health status and the prevention and control of early pathological changes should be strengthened.
-
In 2017, smoking caused 2.6 million deaths in China, accounting for nearly one-third of all global deaths due to tobacco use (8.3 million)[1]. Tobacco use is far more harmful to the health of Chinese people than the global average. In 2018, the rate of second-hand smoke exposure was 68.1% in China, and the rate of exposure almost every day was 35.5%. At present, the rate of e-cigarette use is 0.9%. The smoking cessation rate among people ≥ 15 years of age in China was 20.1%[2].
A prospective cohort study of chronic diseases in China (China Kadoorie Biobank Collaborative Group, CKB) recruited more than 500,000 adults. After a 7-year follow-up, the results indicated that the hazard ratio (HR) for urban male smokers dying of CVD, compared with people who had never smoked, was 1.63, and that for rural male smokers was 1.24. Female smokers have been found to have a higher risk of dying from CVD than male smokers[3].
-
According to the data from the China National Nutrition Survey (CNNS) from 1982 to 2012 and the China Health and Nutrition Survey (CHNS) from 1989 to 2015, the intake of grains and vegetables by Chinese residents decreased, whereas the intake of animal food, mainly pork, increased (Figure 1). The intake of eggs, fish, and dairy products remained low. A significant increase in edible oil and decrease of household cooking salt was observed. However, the consumption of both edible oil and cooking salt far exceeded the recommended amounts.
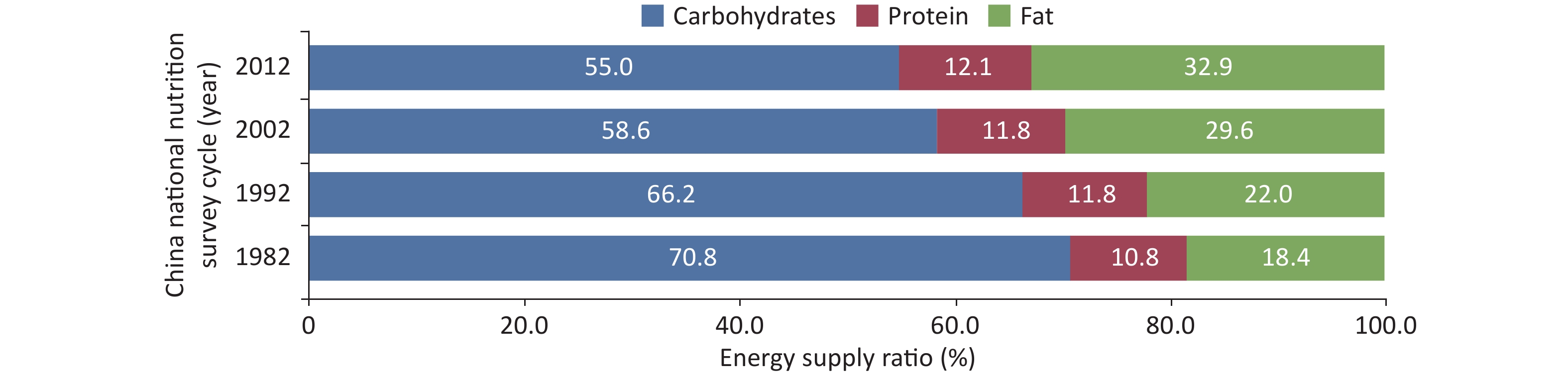
The total energy intake among Chinese residents showed a decreased trend. The protein intake remained stable, and the carbohydrate energy supply ratio significantly decreased. The fat energy supply ratio increased (Figure 2) and exceeded the upper limit recommended by the dietary guidelines (recommended range: 20%–30%). In rural areas, the fat energy supply ratio exceeded the upper limit recommended by 30% for the first time. The risk of inadequate intake of vitamins and minerals remains present.
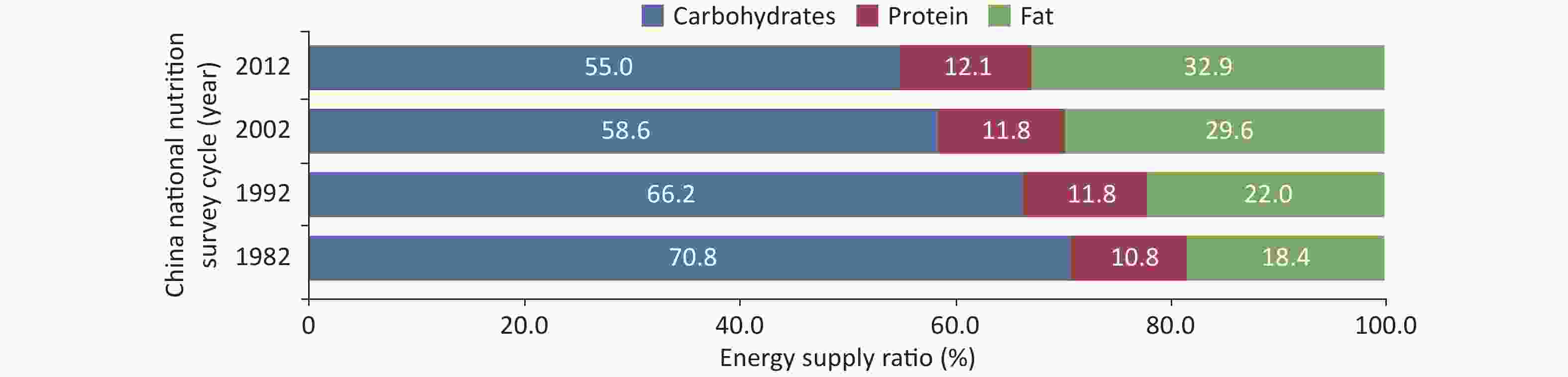
Figure 2. Trends in the energy supply ratio of carbohydrate, protein and fat among Chinese residents from 1982 to 2012.
According to data for 73,572 residents ≥ 2 years of age from the China National Nutrition and Health Surveillance (2015–2017), the average daily energy intake was 2,007.4 kcal, the carbohydrate intake was 266.7 g, the protein intake was 60.4 g, and the fat intake was 79.1 g[4]. An analysis of 8,777 children 6–11 years of age in the China Child and Lactating Mother Nutrition Health Surveillance (2016–2017) indicated daily intakes of energy, protein, fat and carbohydrates in this group of 1591.7 kcal, 50.0 g, 69.6 g, and 196.3 g, respectively[5]. An analysis of 7,265 Chinese people 12–17 years of age has reported a mean daily intake of dietary energy, carbohydrate, fat and protein per person were 1,995.0 kcal, 253.8 g, 84.5 g, and 61.4 g, respectively. The energy supply ratios of carbohydrate, fat and protein were 50.6%, 37.1%, and 12.3%, respectively[6].
CHNS data for 29,238 adults from 1991 to 2015 have indicated that China is experiencing a shift from traditional to Western dietary patterns[7]: the scores for the southern China dietary pattern (high intake of rice, vegetables and pork) have decreased, and those for the modern dietary pattern (high intake of fruits, dairy products, cakes, cookies and pastries) and the meat dietary pattern (high intake of offal, poultry and other livestock meat) have increased.
In 2014, a survey conducted among 27,485 people ≥ 3 years of age in 14 provinces (cities) in China reported an average daily intake of added sugar in carbonated beverages of 0.5 g, with an energy supply ratio of 0.11%. The average daily intake of added sugar was 13.4 g, with an energy supply ratio of 2.69%. Adolescents 13–17 years of age were the group with the highest consumption[8].
A survey on snack consumption among 27,374 primary and secondary school students in poor rural areas in central and western China from the Nutrition Improvement Program for Rural Compulsory Education Students (2019) has indicated that 14.0% of students ate snacks two or more times per day, and the top three main snack choices were vegetables and fruits (50.6%), cookies and bread (50.1%) and puffed food (40.0%)[9].
The China Adult Chronic Disease and Nutrition Surveillance 2015 reported that the proportion of Chinese residents 18–59 years of age who ate in restaurant in the past week was 36.1%, and 23.9% had eaten in restaurant seven or more times. Eating in restaurant was more common among men, people 18–44 years of age, people in urban areas, people with higher education and higher family incomes, and unmarried and employed people[10]. Compared with the data of 2010–2012, the proportion of people 18–44 years of age who ate in restaurant increased by 14.7%, and the proportion of people 45–59 years of age who ate in restaurant increased by 9.0% in 2015[11].
From 2015 to 2017, a survey conducted among 181,795 residents ≥ 18 years of age in the China National Nutrition and Health Surveillance has indicated that the alcohol consumption rate among adults in China was 43.7%, the average alcohol intake of alcohol consumers was 28.3 g/d, the hazardous alcohol consumption rate (average daily pure alcohol intake of 41–61 g for men and 21–41 g for women) was 9.4%, and the harmful alcohol consumption rate (average daily pure alcohol intake ≥ 61 g for men and ≥ 41 g for women) was 13.7%. All of these values were higher than those in 2010–2013[12].
According to the data from the Global Burden of Disease Study (GBD 2017), low dietary fiber intake contributed to 170,143 deaths from ischemic heart disease (IHD) in China in 2017. Dietary factors accounted for three of the top five risk factors associated with stroke: excessive sodium intake, inadequate fruit intake, and inadequate cereal intake, with population attributable fractions (PAF) of 38.5%, 24.2%, and 24.1%, respectively[13].
After a mean follow-up of 11.2 years in 461,047 residents 30–79 years of age, the CKB study found that an unhealthy diet (lack of vegetable, fruit and egg consumption daily, and red meat consumption daily or weekly in the past year) increased the risk of ischemic stroke (HR = 1.23). Excessive alcohol consumption (≥ 30 g of alcohol daily or stop drinking in the past year) increased the risk of ischemic stroke (HR = 1.21) and hemorrhagic stroke (HR = 1.30)[14].
The Study of the China Salt Substitute and Stroke Study (SSaSS) was an open-label, block-randomized trial that enrolled 20,995 residents with a history of stroke or residents ≥ 60 years of age with hypertension in 600 villages in China, with a mean follow-up of 4.74 years. A 14% lower risk of stroke was observed among those consuming low-sodium salt than regular salt (events per 1,000 person-years: 29.14 vs. 33.65; RR = 0.86). The incidence of serious adverse events due to hyperkalemia was not significantly higher in people who consumed low sodium salt rather than regular salt[15].
-
Physical Activity and Fitness in China—The Youth Study was conducted in Chinese school-children and adolescents. A multi-stage cluster sampling method was used to recruit 120,000 to 130,000 students from primary and secondary schools across all administrative provinces in mainland of China. The attainment rate of physical activity in 2017 was higher than that in 2016 for primary and middle school students, and did not change significantly for senior high school students.
In 2016, 85.2% primary and secondary school students participated in more than two physical education classes per week, 31.5% of whom participated in more than five times of extracurricular physical training per week. The prevalence of ≥ 2 h daily screen viewing time among primary and secondary school students was 8.7%, 11.5%, and 9.0% for television, mobile phones and computers, respectively, whereas these values increased to 23.7%, 27.7%, and 17.5%, respectively, on weekends.
National Physical Fitness Surveillance data has shown that, in 2014, the prevalence of regular physical activity was 33.9% among Chinese residents. Except for people older than 70 years of age, the lowest prevalence was in the group aged 20–39 years, while the highest in those aged 60–69.
According to CHNS, the total physical activity among Chinese adults fell decreased from 399 MET·h/7 d in 1991 to 213 MET·h/7 d in 2009. The occupational physical activity decreased by 31% in men from 1991 to 2011, and the trend in women was similar. From CHNS, Chinese adults’ time spent in sedentary behaviours increased from 15.1 hours per week in 1991 to 20.0 hours per week in 2009. According to the Report on Chronic Diseases Risk Factor Surveillance in China, the time spent in sedentary behaviours among adults ≥ 18 years of age increased from 2.7 h/d in 2010 to 3.3 h/d in 2013. The increase was greater in urban than rural areas, and was similar between men and women.
According to the physical activity data for 168 countries from 2001 to 2016 published by the World Health Organization (WHO) in 2016[16], among people 40–74 years of age, reaching the recommended physical activity goals could prevent 18.3% of premature deaths in China, which would be equivalent to avoiding 1.0165 million premature deaths in this age group every year.
The GBD 2016 study[17] has indicated that age standardized stroke mortality due to physical inactivity in China showed a downward trend from 1990 to 2016. The age standardized stroke mortality in men decreased from 6.0/100,000 to 1.8/100,000, and that in women decreased from 3.4/100,000 to 0.6/100,000. The annual net change rate in men was −1.3%, and that in women was −2.9%.
In the China Prediction of Atherosclerotic Cardiovascular Disease Risk Study (China-PAR), 100,560 individuals with no prior CVD history at baseline were examined for a median follow-up of 7.3 years [18], and a 26% (HR = 0.74) lower risk of CVD was observed among those who met than did not meet the recommended goal of moderate to vigorous physical activity at baseline. Moreover, those who were highly active had a 38% lower risk of CVD (HR = 0.62). Compared with those who were physically inactive at baseline and at follow-up, those who remained active had a 43% lower CVD risk (HR = 0.57).
In the CKB cohort study, more than 487,000 adults with no prior CVD history at baseline were followed up for an average of 7.5 years[19]. A significant negative correlation was observed between total physical activity and cardiovascular death. Compared with the lowest activity group (≤ 9.1 MET·h/d), the risk of cardiovascular death in the highest quintile (≥ 33.8 MET·h/d) decreased by 41% (HR = 0.59). For every 4 MET·h/d increase in physical activity, the risk decreased by 12%. Thus, increasing occupational or non-occupational activities can decrease the risk of cardiovascular death.
Data for more than 120,000 adults with long-term follow up in Shanghai[20] have indicated that, compared with people who did not participate in leisure activities, people who participated in moderate intensity leisure activities (such as Taijiquan, dancing or fitness walking) had a 14% (HR = 0.86) lower risk of cardiovascular death. Even people who did not reach the minimum recommended amount (approximately 7.5 MET·h/7 d) also had a significantly lower risk of cardiovascular death, and the relationship was dose-dependent.
The GBD study has estimated that, in 2013, the total health-care costs of physical inactivity were almost $4.86 billion in China, accounting for 10% of the global costs. The direct and indirect costs were $3.08 billion and $1.78 billion, respectively. The proportion of costs borne by households, and the public and private sectors was 33.90%, 55.80%, and 10.30%, respectively.
Comprehensive analysis of data from China Chronic Disease and Risk Factors Monitoring (2007) and the China Health Service Survey (2003) has indicated that the proportion of Chinese residents with coronary heart disease (CHD), stroke, hypertension, cancer or type 2 diabetes mellitus directly attributable to insufficient physical activity (below WHO recommendations) was 12.3%, 15.7%, 8.5%, 11.3%, and 13.5%, respectively. Simultaneously, overweight or obesity caused by a lack of physical activity further increased the risk. The lack of physical activity resulted in an economic burden of 6.7 billion US dollars in 2007, accounting for 15.2% of the total economic expenditure for major chronic diseases in that year. The direct medical economic burden accounted for more than 15.0% of the total direct economic burden due to major non-communicable diseases in China.
-
In 2013, the prevalence of overweight and obesity among Chinese children under 6 years of age was 8.4% and 3.1%, respectively. Compared with those in 2002, the overweight and obesity rates increased by 1.9% and 0.4%, respectively. The overweight rate among Chinese adults ≥ 18 years of age reached 30.1%, and the obesity rate reached 11.9% in 2012. Compared with those in 2002, the overweight and obesity rates of adults in China increased by 7.3% and 4.8%, respectively, and the growth rate in rural areas was higher than that in urban areas[21]. From 2014 to 2018, 2.70 million Chinese people 35–75 years of age were investigated in the China Patient-Centered Evaluative Assessment of Cardiac Events (China PEACE) study. The age-standardized abdominal obesity rate was 32.7% (32.6% to 32.8%) for women (waist circumference ≥ 85 cm) and 36.6% (36.5% to 36.8%) for men (waist circumference ≥ 90 cm). One of every three people in China has been estimated to have abdominal obesity[22].
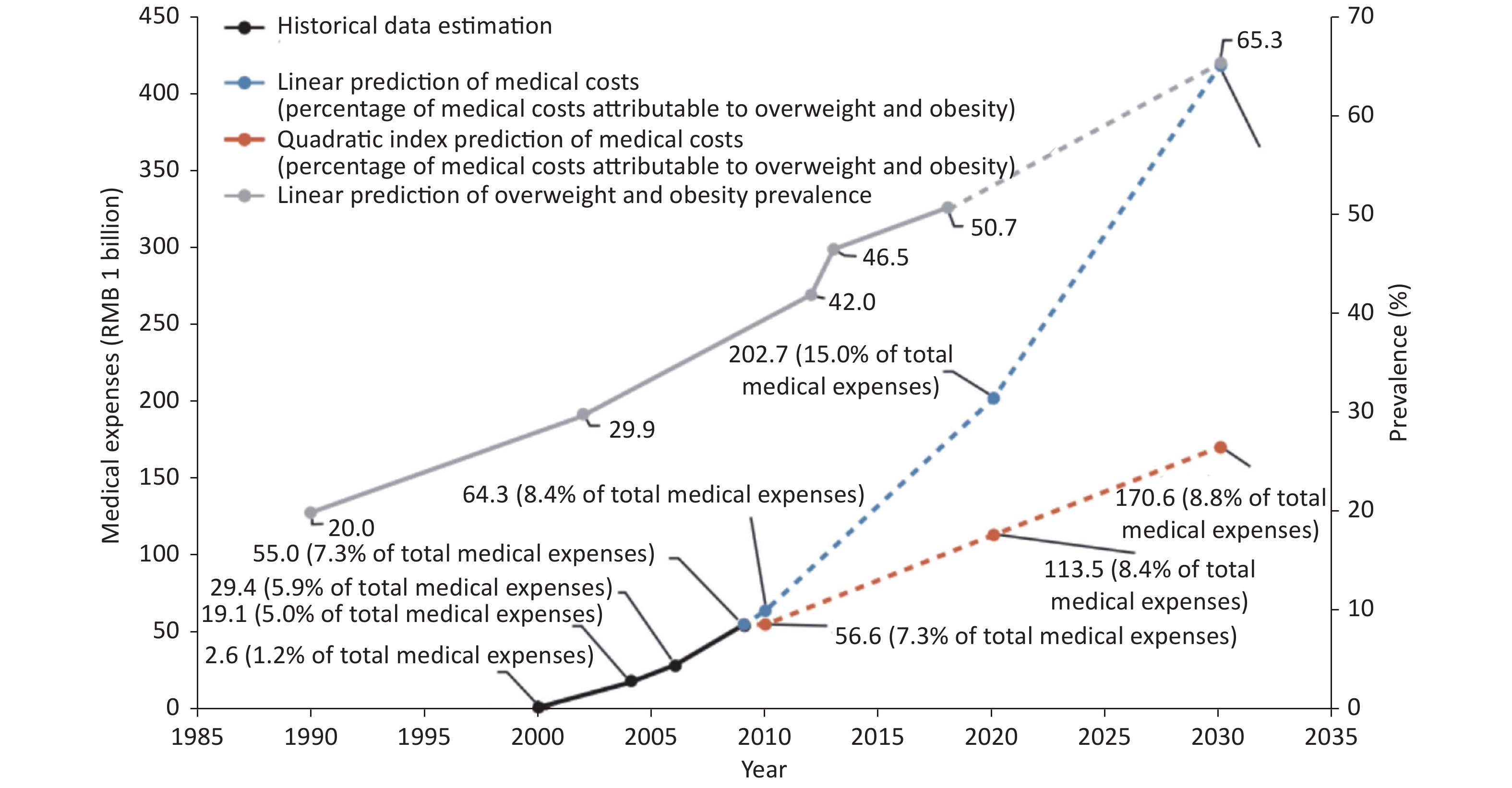
By 2030, the proportions of overweight and obesity in Chinese adults (Chinese standard), children and adolescents 7–17 years of age (Chinese standard) and children ≤ 6 years of age (WHO diagnostic standards) have been predicted to reach 65.3%, 31.8% and 15.6%, respectively. The number of overweight and obesity people may reach 789.95 million, 58.92 million and 18.19 million, respectively[23].
According to the GBD study, the number of CVD deaths due to high body mass index (BMI) in China was 549,500 in 2019. The age-standardized CVD mortality rate due to high BMI was 38.64 per 100,000, and 11.98% of CVD deaths were due to high BMI. The direct medical costs due to overweight and obesity in China ranged from $8.4 billion to $23.9 billion, and the indirect medical costs were $62.6 billion[24]. According to the trends in overweight and obesity rates, and the costs observed in the CHNS, the medical costs due to overweight and obesity have been estimated to be RMB 418 billion in 2030, without considering long-term increases in health care service costs (Figure 3)[23].
-
A meta-analysis of 23 hospital-based studies has indicated that the prevalence of depression among Chinese inpatients with coronary heart disease was 51%, and 0.5%–25.4% had major depression. In a study of community patients with coronary heart disease, the prevalence of depression was 34.6%–45.8%, and 3.1%–11.2% had major depression.
The INTERHEART study has indicated a prevalence of depression in China of 21.7% in patients with actue myocardial infarction (AMI)—a proportion significantly higher than that in the control group, at 10.4%; both values were lower than those in 51 other countries. However, depression was associated with a higher risk of AMI in China than in other countries (China: OR = 2.27, other countries: OR = 1.37).
According to data from the CKB study, the overall prevalence of major depression was 0.6% among 486,541 adults 30–79 years of age. Major depression was an independent risk factor for heart disease (HR = 1.32). The risk was significantly higher in urban residents (HR = 1.72).
The Shanghai Mental Health Center has analyzed 3,273 patients with depression from 32 hospitals in China and found that approximately 31.3% of patients with depression had a circulatory disorder as their first symptom. Other manifestations included insomnia, gastrointestinal disorders, trunk pain, sensory abnormalities, neurological disorders, loss of libido and physical pain[25].
-
According to the nationwide sampling surveys of hypertension conducted in 1958–1959, 1979–1980, 1991, and 2002, the crude prevalence rates of hypertension among people ≥ 15 years of age were 5.1%, 7.7%, 13.6%, and 17.6%, respectively, showing an increasing trend (Table 1). The results of the China Hypertension Survey (CHS)[26] indicated a crude prevalence rate of hypertension in Chinese adults ≥ 18 years of age of 27.9% from 2012 to 2015, and the weighted rate of 23.2%. The estimated number of adults with hypertension in China is 245 million. The crude detection rate of high normal blood pressure is 39.1%, and the weighted rate is 41.3%. A total of 435 million people in China have been estimated to have high normal blood pressure.
Study name Year Age (years) Sampling method Sample size (people) Prevalence (%) Key project of Chinese
Academy of Medical
Sciences: hypertension
research1958–1959 ≥ 15 Non-random sampling 739,204 5.1 National Hypertension
Sampling Survey1979–1980 ≥ 15 Random sampling 4,012,128 7.7 National Hypertension
Sampling Survey1991 ≥ 15 Stratified random sampling 950,356 13.6 China Health and
Nutrition Survey2002 ≥ 18 Multistage stratified cluster
random sampling272,023 18.8 Chinese Residents
Nutrition and Chronic
Diseases Survey2012 ≥ 18 Multistage stratified
random sampling− 25.2 China Hypertension Survey 2012–2015 ≥ 18 Multistage stratified
random sampling451,755 27.9 (weighted rate 23.2) China Chronic Disease
and Risk
Factor Surveillance2018 ≥ 18 Multistage stratified cluster
random sampling179,873 27.5 (weighted rate) Table 1. Sampling survey on the prevalence of hypertension in China
In 2018, the China Chronic Disease and Risk Factor Surveillance (CCDRFS) project investigated 298 counties in 31 provinces, autonomous regions and municipalities in mainland of China and recruited 179,873 adults ≥ 18 years of age with a multi-stage stratified cluster random sampling method[27]. The prevalence of hypertension was found to be 27.5%.
The CHNS prospective cohort study of 12,952 Chinese adults > 18 years of age[28] has indicated that the age-standardised hypertension incidence increased from 40.8 per 1,000 person-years in 1993–1997 to 48.6 per 1,000 person-years in 2011–2015. From 1991 to 2011, CHNS conducted eight cross-sectional surveys on adults ≥ 18 years of age in 8 provinces of China (which increased to 9 in 1997 and 12 in 2011). The age standardized detection rate of high normal blood pressure increased from 23.9% in 1991 to 33.6% in 2011.
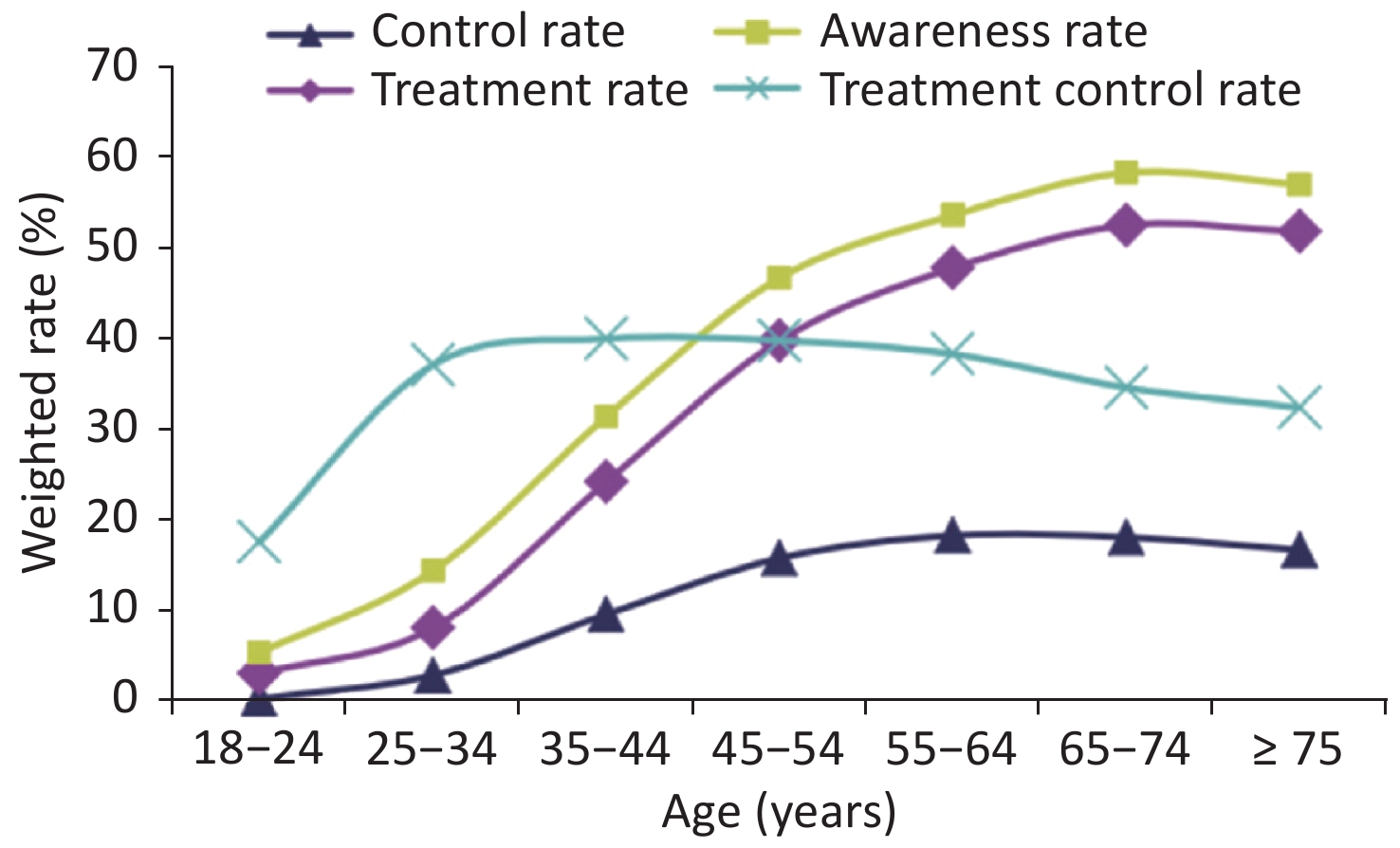
The CHS study[26] has found that the hypertension awareness, treatment and control rates (weighted rates) in Chinese adults ≥ 18 years of age generally increased with age, and the treatment control rate first increased and then decreased (Figure 4). In 2015, the hypertension awareness, treatment and control rates among adults ≥ 18 years of age in China were 51.6%, 45.8%, and 16.8%, respectively. All of these rates showed significant improvements with respect to those reported in previous surveys [26]. Studies of hypertension awareness, treatment and control rates in China over the years are shown in Table 2.
Study name Year Age
(years)Sampling method Sample size
(people)Awareness
rate (%)Prevalence
(%)Control
rate (%)National
Hypertension
Sampling Survey1991 ≥ 15 Multilevel random
sampling950,356 27.0 12.0 3.0 China Health and
Nutrition Survey2002 ≥ 18 Multistage stratified
cluster random
sampling272,023 30.2 24.7 6.1 Chinese Residents
Nutrition and Chronic
Diseases Survey2012 ≥ 18 Multistage Stratified
random sampling- 46.5 41.1 13.8 Chinese Residents
Nutrition and Health
Surveillance2010–2012 ≥ 18 Multistage stratified
cluster random
sampling120,428 46.5 41.1 14.6 Investigation of
the prevalence,
awareness, treatment
and control rates of
hypertension in the
Chinese working
population2012–2013 18–60 Multistage cluster
sampling37,856 57.6
(standardization
rate 47.8)30.5
(standardization
rate 20.6)11.2
(standardization
rate 8.5)China Hypertension
Survey2012–2015 ≥ 18 Multistage stratified
random sampling451,755 51.6
(weighted
rate 46.9)45.8
(weighted
rate 40.7)16.8
(weighted
rate 15.3)China Chronic Disease
and Risk Factor
Surveillance2013–2014 ≥ 18 Multistage stratified
random sampling174,621 31.9 26.4 9.7 Early screening and
comprehensive
intervention
program for
high-risk groups
of cardiovascular
disease2014 35–75 Convenience sampling 640,539 46.5 (standardization rate) 38.1 (standardization rate) 11.1 (standardization rate) China Chronic
Disease
and Risk Factor
Surveillance2018 ≥ 18 Multistage stratified
cluster random
sampling179,873 41.0
(weighted rate)34.9
(weighted rate)11.0
(weighted rate)Table 2. Awareness, treatment, and control rates of hypertension in various studies
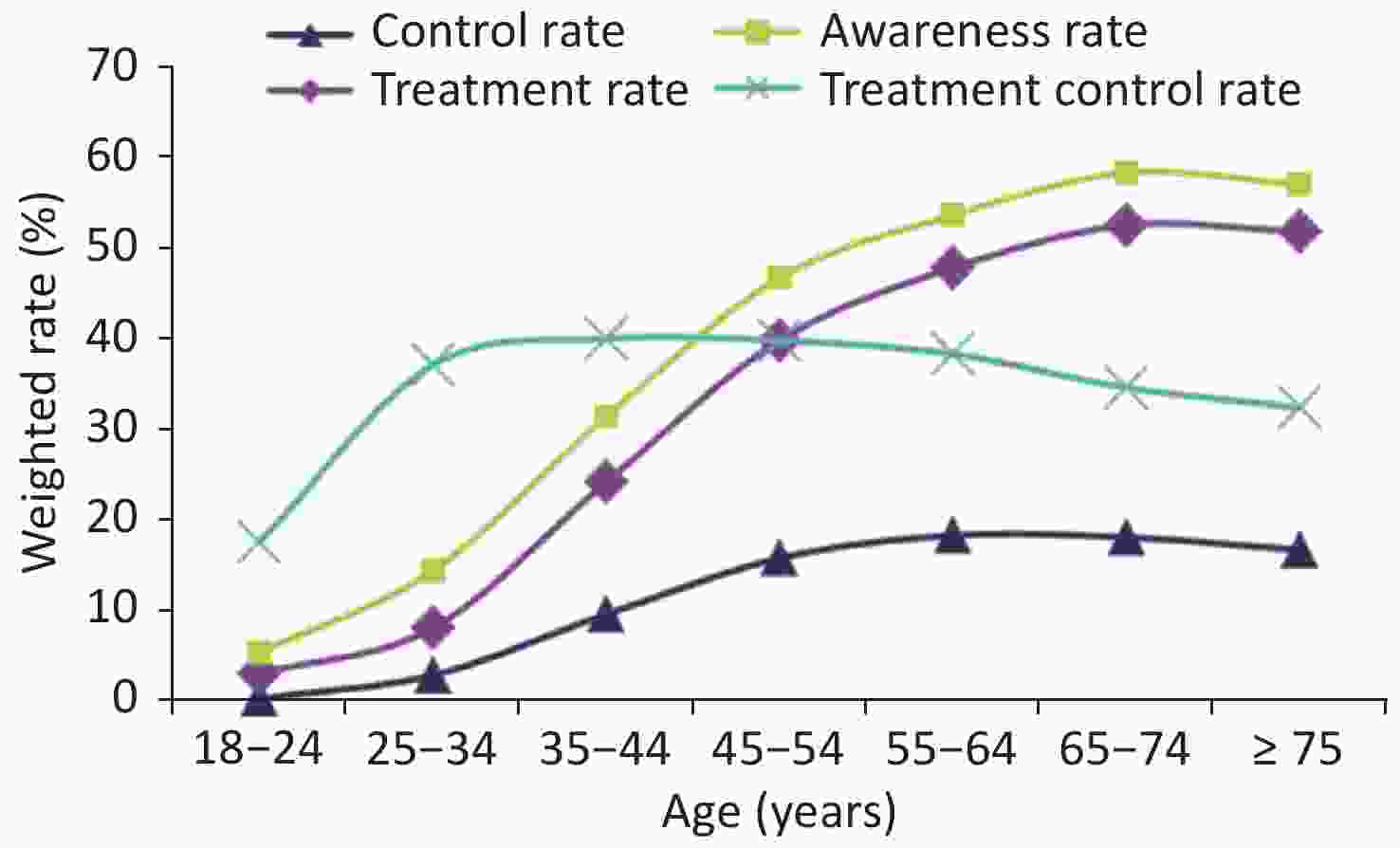
Figure 4. Awareness, treatment, control and treatment control rates regarding hypertension in different age groups in the China Hypertension Survey (CHS).
From 2005 to 2010, 12,497 adults were followed up for 5 years. After adjustment for other risk factors, the risk of hypertension in male drinkers was 1.236 times higher, and that in female drinkers was 1.409 times higher, than those in non-drinkers.
An investigation in eight provinces in China from 2007 to 2010, a cross-sectional study in 28 provinces from 2011 to 2012 and the China Health and Retirement Longitudinal Study (CHARLS) have all indicated that air pollution increases the risk of hypertension. The CHS has indicated that systolic blood pressure and diastolic blood pressure decrease by 0.74 mmHg (1 mmHg = 0.133 kPa) and 0.60 mmHg, respectively, for every 10 ℃ increase in ambient temperature.
A meta-analysis of 41 clinical studies on hypertension and depression has indicated a prevalence of depression in patients with hypertension of 28.5% in China.
A multicenter randomized controlled study published in the New England Journal of Medicine[29] has indicated that, during a median follow-up of 3.34 years among 8,511 elderly patients with hypertension, 147 (3.5%) of the 4,243 patients in the intensive treatment group had primary outcome events, compared with 196 (4.6%) of the 4,268 patients in the standard treatment group (RR = 0.74). The rate of primary outcome events in the intensive treatment group was significantly lower than that in the standard treatment group, with an absolute difference of 1.1%.
Another study[30] has found that, compared with standard hypertension control (targeting a blood pressure decrease to 140/90 mmHg), intensive hypertension control (targeting a blood pressure decrease to 133/76 mmHg) could avoid 2.209 million CHD events, 4.409 million stroke events and 75,100 cardiovascular deaths in 10 years. Compared to standard hypertension control, the intensive hypertension control could avert about 13% of stroke events, 17% of CHD events for males, and 11% of CHD events for females.
On the basis of China CVD policy modeling 2015–2025, if all patients with hypertension (with/without CVD, and stage I and II hypertension) were treated, as compared with the current treatment rates, 803,000 CVD events (690,000 cases of stroke and 113,000 cases of myocardial infarction) would be avoided, and 1.2 million quality adjusted life years (QALY) would be obtained.
For China, if the guidelines for the diagnosis and treatment of adult hypertension issued by the American College of Cardiology/American Heart Association in 2017 were adopted, to reach currently the treatment rate of hypertension. By preventing CVD events, the new guidelines will reduce the lifetime cost by US $3.77 billion and prevent the loss of 1.41 million life years due to disability[31].
A community multicenter prospective cohort study has evaluated the long-term antihypertensive efficacy, cost-effectiveness and cardiovascular outcomes of antihypertensive generic drugs and original drugs through propensity score matching and cost-effectiveness analysis[32]. The average annual cost per patient in the generic drug group was significantly lower than that in the original drug group ($220.4 and $472.7, respectively). The average annual savings per patient with use of generic drugs was $252.3, whereas the effect on decreasing systolic blood pressure was similar between groups [(7.1 ± 1.0) mmHg and (7.9 ± 1.0) mmHg, respectively]. The cost-effectiveness ratio (annual average cost of decreasing systolic blood pressure by 1 mmHg at follow-up) in the generic and original drug groups were 31.0 and 59.8, respectively. Compared with that of generic drug treatment, the cost of original drug treatment was US $315.4 greater for each additional 1 mmHg decrease in systolic blood pressure.
From 2012 to 2015, the China Children and Adolescents Cardiovascular Health Survey (CCACH) used a screening strategy with three time points on different days to evaluate the prevalence of hypertension in 44,396 children 6–17 years of age from six cities in China[33]. Although the prevalence of hypertension differed (17.1% vs. 15.4%) at a single time point screened according to the latest standards in China and the United States, the prevalence of hypertension after three consecutive blood pressure measurements on different days decreased by 79%, and the final prevalence of hypertension was similar (3.7% vs. 3.3%).
In a randomized controlled study of a nutrition and exercise intervention for hypertension prevention in children in grades 1–5 from 30 primary schools in five cities across the country, 15 schools served as the control group (3,333 people), and the other 15 schools served as the intervention group (3,431 people). The intervention group received population-based nutrition promotion (including nutrition courses, distribution of nutrition brochures and nutritional guidance provided to school cafeterias) and exercise promotion (at least 20 minutes of moderate- to high-intensity physical activity every day). One year later, children in the intervention group had a 0.9 mmHg lower systolic blood pressure and a 1.8% lower hypertension prevalence than the control group[34].
-
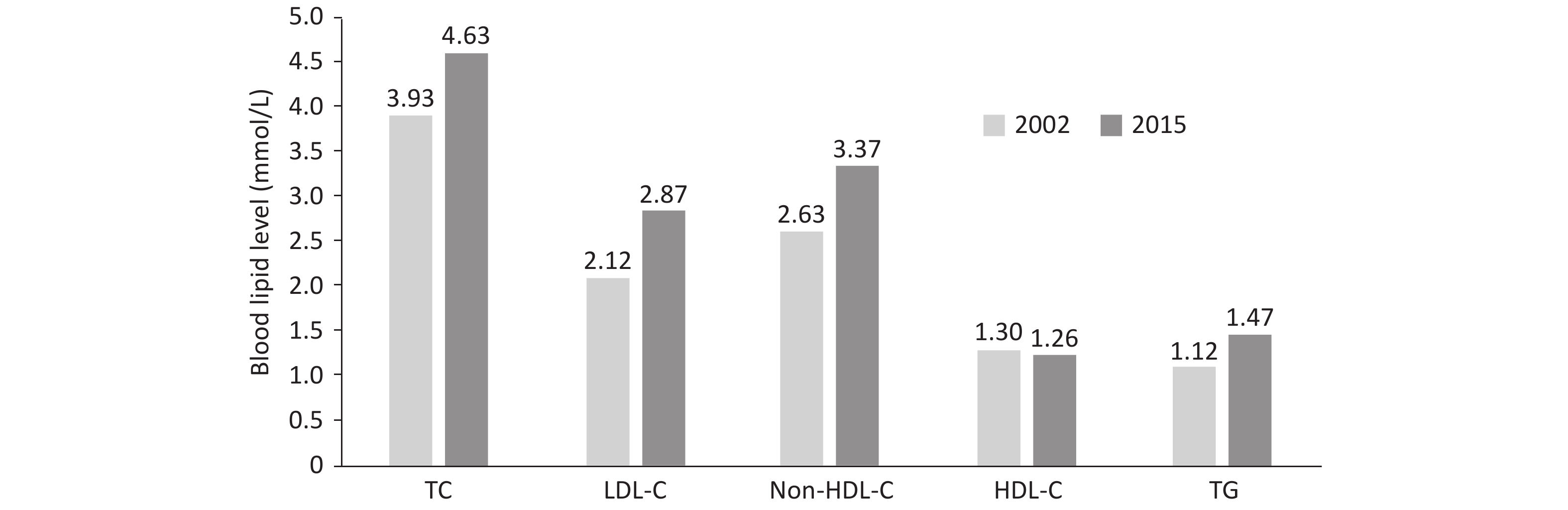
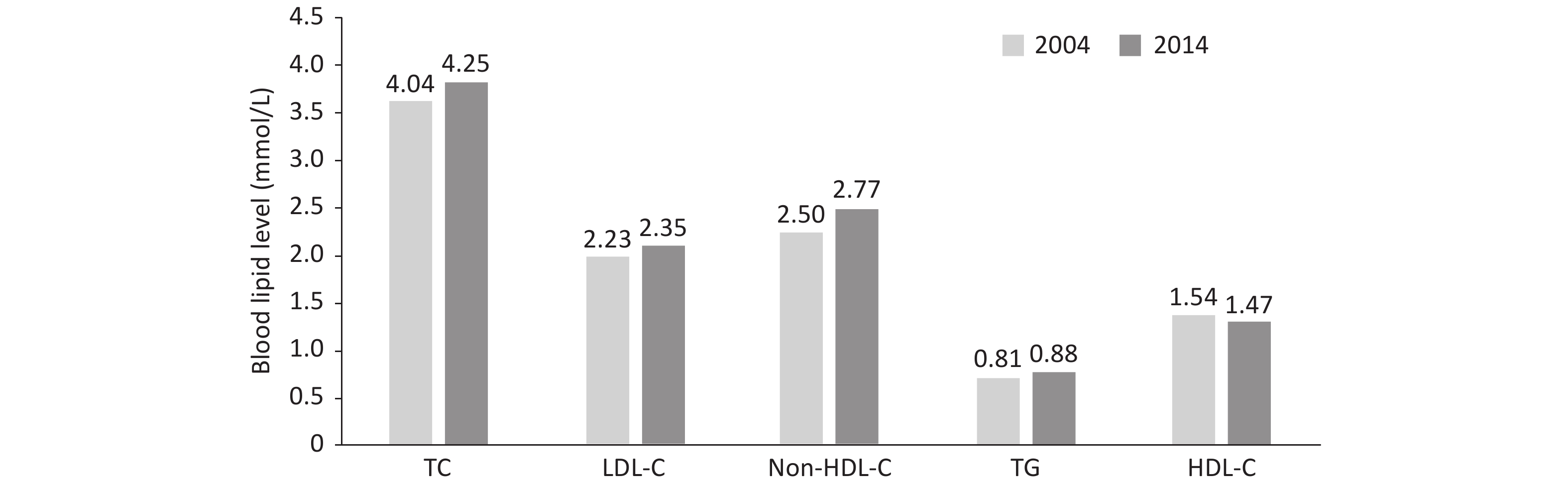
The results from 179,728 adults ≥ 18 years of age in the Chinese Adults Nutrition and Chronic Diseases Surveillance in 2015 have indicated that, the total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), non-high-density lipoprotein cholesterol (non-HDL-C) and triglyceride (TG) levels were higher than those in 2002 (Figure 5)[35].
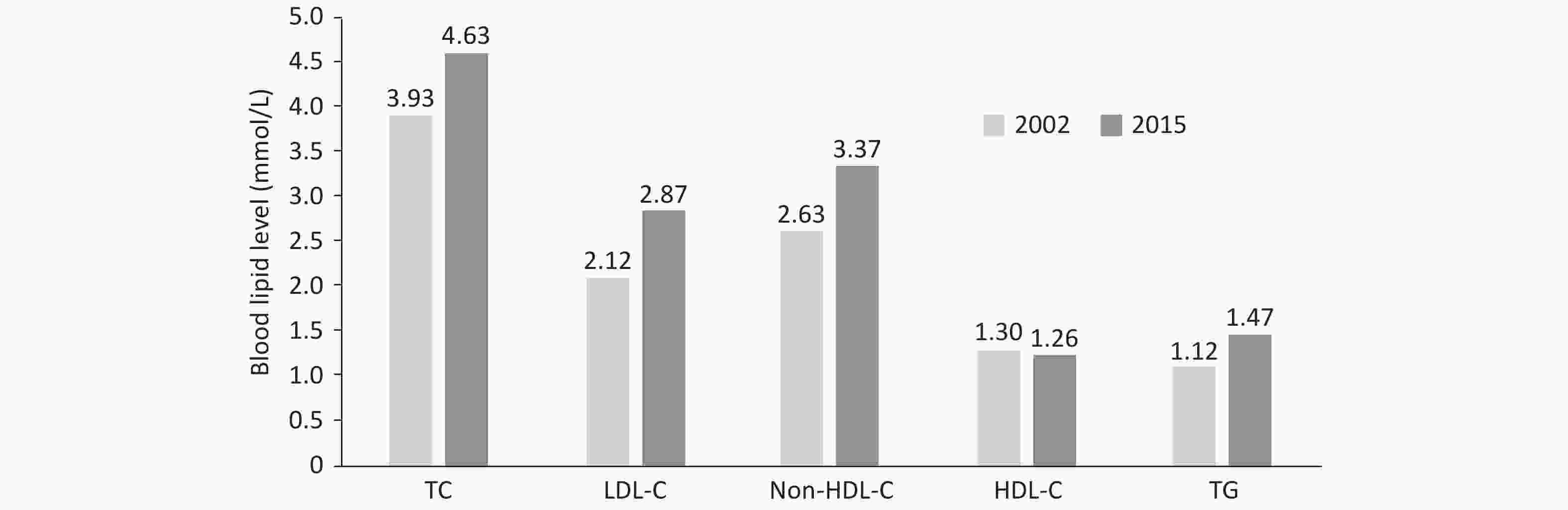
Figure 5. 13-year changes in blood lipid levels in Chinese adults ≥ 18 years of age. TC: total cholesterol; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol; TG: triglyceride.
An analysis by the Non-communicable Disease Risk Factor Collaborative Group has found that in 1980, the average non-HDL-C level in the Chinese population was one of the lowest worldwide, whereas by 2018, it was about 4 mmol/L, reached or exceeded the non-HDL-C level in many high-income western countries[36].
In 2004 and 2014, 1,660 and 1,649 children and adolescents 6–18 years of age in Beijing were recruited in the Beijing Children and Adolescent Metabolic Syndrome Study. The levels of TC, LDL-C, non-HDL-C, and TG in children and adolescents in 2014 were significantly higher than those 10 years prior (Figure 6).
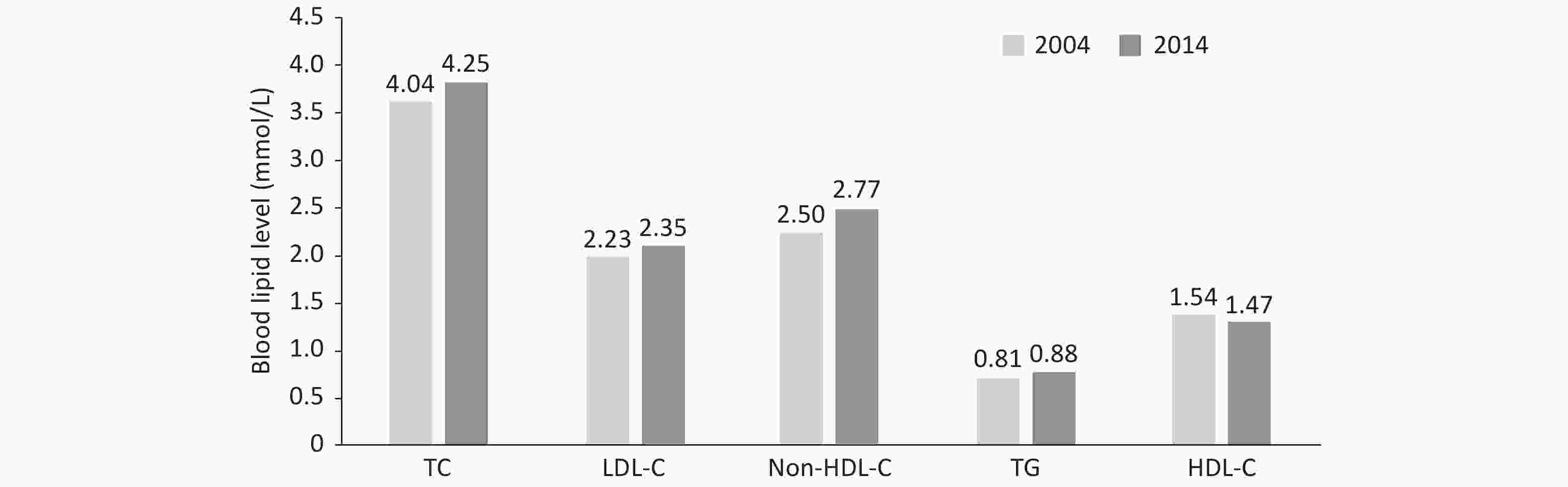
Figure 6. 10-year changes in blood lipid levels of children and adolescents 6–18 years of age in Beijing. TC: total cholesterol; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol; TG: triglyceride
The CHNS in 2002, the China National Survey on Chronic Kidney Disease (CNSCKD) in 2019[37], the CHNS in 2011[38] and the Chinese Residents Nutrition and Chronic Disease Survey in 2012 have indicated that the overall prevalence of dyslipidemia (defined as the presence of any type of dyslipidemia, including TC ≥ 6.22 mmol/L, LDL-C ≥ 4.14 mmol/L, HDL-C < 1.04 mmol/L, and TG ≥ 2.26 mmol/L) in Chinese people ≥ 18 years of age has increased significantly, from 18.6% in 2002 to 40.4% in 2012.
The CHS was conducted in 29,678 residents ≥ 35 years of age from 2012 to 2015[39]. The overall prevalence of dyslipidemia was 34.7%. The China National Stroke Screening and Prevention Project (CNSSPP) in 2014 indicated that the overall prevalence of dyslipidemia, standardized by age and sex, in Chinese residents ≥ 40 years of age was 43.0%[40]. According to the data from the fourth CCDRFS[41] 2013–2014 and the Chinese Adults Nutrition and Chronic Diseases Surveillance 2015[35], the main form of dyslipidemia in China are low HDL-C and high TG.
In 2012–2013, a survey was conducted on 16,434 children and adolescents 6–17 years of age from 93 primary and secondary schools in seven provinces, autonomous regions and municipalities in China. The total rate of dyslipidemia was 28.5% (cut points of TC > 5.18 mmol/L, LDL-C ≥ 3.37 mmol/L, HDL-C < 1.03 mmol/L, and TG > 1.7 mmol/L for dyslipidemia in children)[42].
The CHS results in 2012–2015 indicated that the awareness, treatment and control rates for dyslipidemia in Chinese adults ≥ 35 years of age were 16.1%, 7.8%, and 4.0%[39].
The fourth CCDRFS recruited 163,641 adults ≥ 18 years of age. Totally 15,382 people were in the high-risk of dyslipidemia (9.4% of the total population), of which, 74.5% didn't achieve their LDL-C goal (< 2.6 mmol/L). While 2,945 people were in the extremely high-risk of dyslipidemia (accounting for 1.8% of the total population), and the failure rate of LDL-C was as high as 93.2% (LDL-C < 1.8 mmol/L was the standard) [41].
A total of 25,317 outpatients ≥ 45 years of age who had taken lipid-lowering drugs for at least 3 months were included in the Dyslipidemia International Study-China (DYSIS-China). The LDL-C treatment compliance rates for those with high or very high risk of atherosclerotic cardiovascular disease (ASCVD) were 44.1% and 26.9%, respectively[43].
The Improving Care for Cardiovascular Disease (CCC) in China project, from November 2014 to June 2017, enrolled 6,523 patients with recurrent ACS who had a history of MI or coronary revascularization from 150 tertiary hospitals. The statin treatment rate was only 50.8%, and 36.1% attained the LDL-C goal (< 1.8 mmol/L). The previous patients with ASCVD ≥ 75 years of age with recurrent ACS had only a 33.9% statin treatment rate and 24.7% had LDL-C < 1.8 mmol/L at admission[44-45].
The GBD 2017 has indicated that among the deaths caused by high LDL-C, 81.76% died from ischemic heart disease (IHD), while the remaining 18.24% from ischemic stroke. The population attributable fractions of high LDL-C for IHD deaths was 40.30%, and that for ischemic stroke deaths was 18.49%. The rate of deaths attributable to high LDL-C was 61.08/100,000. The number of disability-adjusted life years (DALY) attributable to high LDL-C was 18,162,100 person-years, of which 13,941,500 person-years (76.76%) were attributable to IHD. The DALY rate was 1,285.83/100,000[46].
In the Kailuan prospective cohort study, 51,407 people were followed up for an average of 6.84 years. The cumulative exposure time to elevated LDL-C (≥ 3.4 mmol/L) and the cumulative exposure value of LDL-C measured multiple times significantly increased the risk of new onset AMI, thus suggesting that the cardiovascular hazards of LDL-C showed a cumulative exposure effect, independently of the single LDL-C measurement value [47].
The CKB study[48] has indicated that LDL-C levels are strongly positively correlated with ischemic stroke and strongly negatively correlated with cerebral hemorrhage (1 mmol/L decrease in LDL-C is associated with a 15% decrease in the relative risk of ischemic stroke and a 16% increase in the relative risk of cerebral hemorrhage). The above correlations have been further validated through Mendelian randomization analysis. The relative risk of ischemic stroke decreases by 25%, and the relative risk of cerebral hemorrhage increases by 13% with each 1 mmol/L decrease in LDL-C level associated with the genetic risk score. HDL-C levels are negatively associated with the risk of ischemic stroke (LDL-C and HDL-C are independently associated with ischemic stroke) and not with cerebral hemorrhage. TG levels are weakly positively associated with the risk of ischemic stroke and negatively associated with cerebral hemorrhage.
A study in 21,265 adults (35–64 years of age) without ASCVD in a multi-provincial cohort study in China, classified according to the 10-year ASCVD risk assessment of the Chinese Guidelines for the Prevention and Treatment of Dyslipidemia in Adults (2016 Revision), has indicated that low-dose statin intervention decreased the 10-year ASCVD incidence rate by 4.1%, 9.7%, and 15.5%, respectively in the low, moderate and high risk groups. Lowering statin prices to the level of the centralized procurement policy of the central government in 2019 could significantly decrease the incremental cost-effectiveness ratio (ICER) for all risk groups; thus, the cost-effectiveness of statins for primary prevention of ASCVD could be significantly improved[49].
-
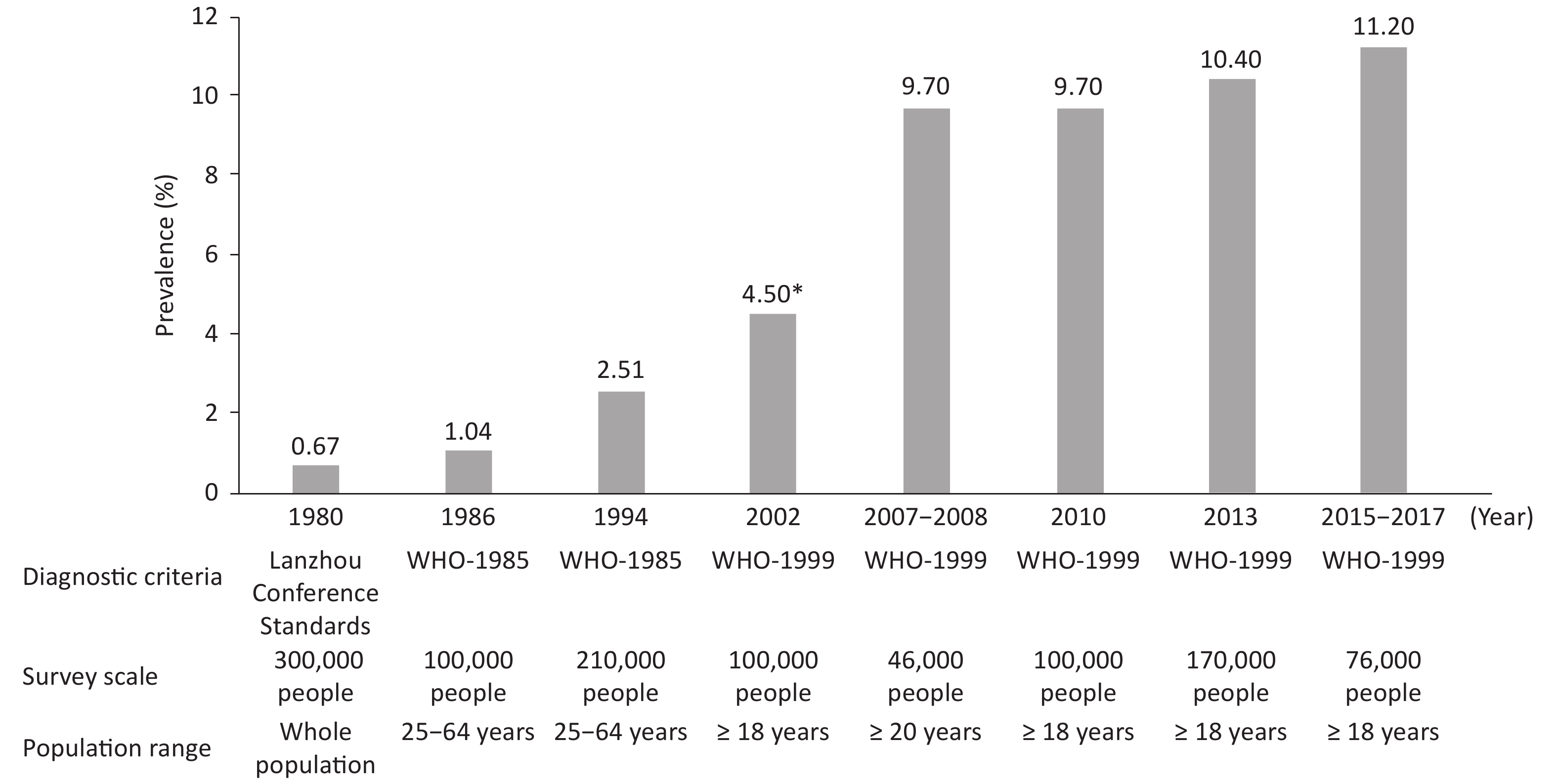
From 1980 to 2017, China conducted several surveys on the prevalence of diabetes (Figure 7). A population-based survey with 300,000 people in 1980 indicated a prevalence of diabetes of 0.67%. From 2015 to 2017, a cross-sectional survey of 75,880 adults over 18 years of age in 31 provinces, autonomous regions and municipalities has indicated that, on the basis of WHO diagnostic criteria, the prevalence rate of diabetes in Chinese adults was 11.2% (95% CI: 10.5%–11.9%), and the detection rate of prediabetes was 35.2% (95% CI: 33.5%–37.0%). According to the American Diabetes Association standard, the prevalence of diabetes was 12.8% (95% CI: 12.0%–13.6%): the prevalence of previously diagnosed diabetes was 6.0% (95% CI: 5.4%–6.7%), and the prevalence of newly diagnosed diabetes was 6.8% (95% CI: 6.1%–7.4%). An estimated 129.8 million adults have diabetes in China (70.4 million men and 59.4 million women)[50].
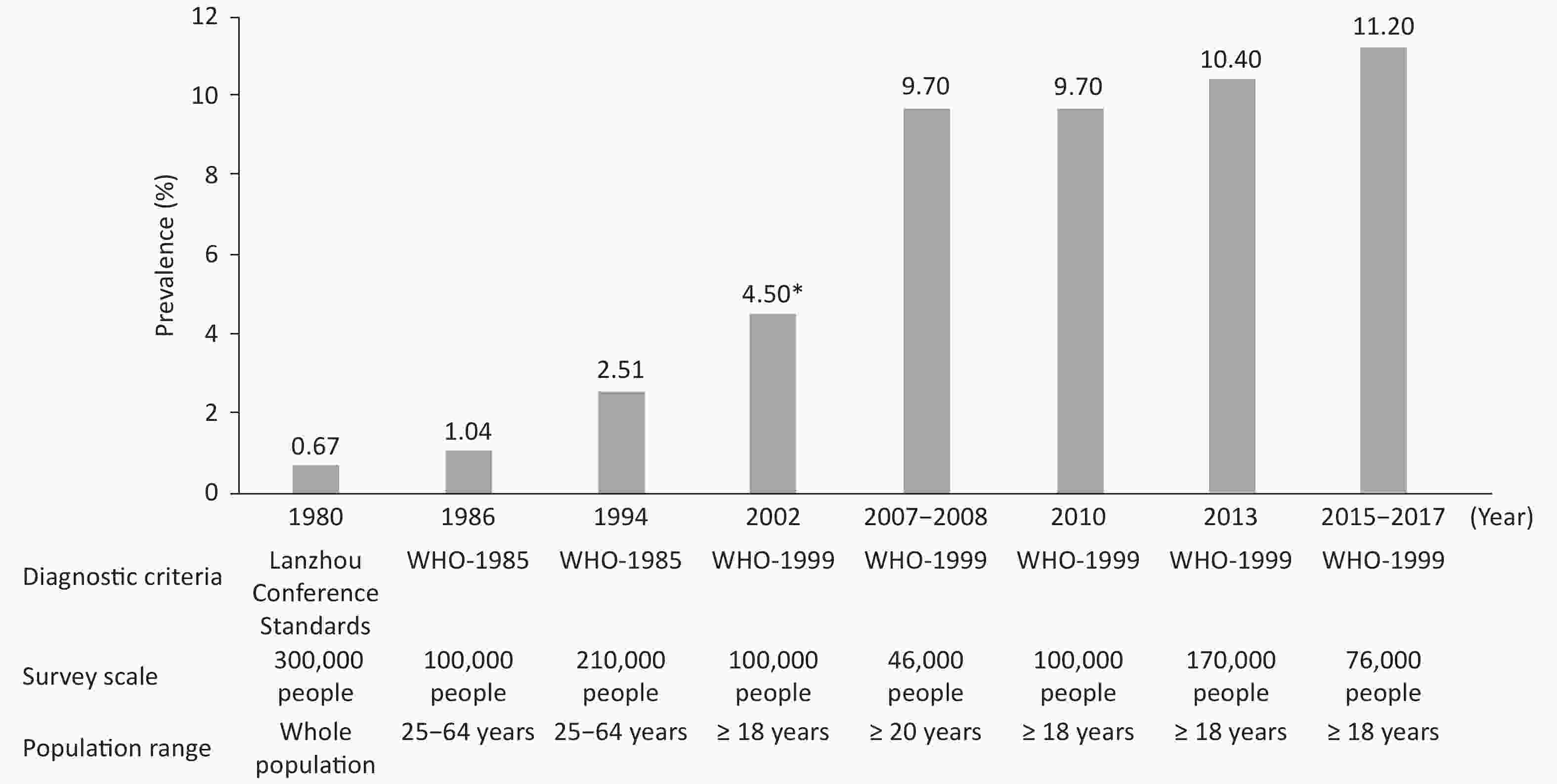
Figure 7. Investigation of the prevalence of diabetes in China. *: prevalence of diabetes in the urban population.
In a study based on the diabetes surveillance system in Zhejiang province, analysis of the data for 879,769 newly diagnosed cases of type 2 diabetes from January 1st, 2007 to December 31th, 2017 revealed an age standardized total incidence of type 2 diabetes of 281.73/100,000 person-years (95% CI: 281.26–282.20). The standardized annual incidence rate increased from 164.85/100,000 person-years in 2007 to 268.65/100,000 person-years in 2017, with an average annual increase of 4.01%, and a faster increase in men, young adults, and people in rural areas[51].
The Daqing Diabetes Prevention Study in China enrolled 577 adults with impaired glucose tolerance from 33 clinics, who were identified through oral glucose tolerance tests. The participants were randomly assigned to either a control group or one of three intervention groups (diet, exercise or diet plus exercise). Interventions were started in 1986 and completed in 1992. Subsequently, participants were followed for up to 30 years to assess the effects of the interventions. Compared with the control group, the combined intervention group had a median delay in diabetes onset of 3.96 years, a 39% lower incidence of diabetes, 26% fewer CVD events, a 35% lower risk of composite microvascular events, 33% fewer CVD deaths and a 26% lower risk of all-cause death. The incidence of stroke and severe retinopathy in the intervention group was also significantly lower than that in the control group. The average life expectancy of the intervention group was increased by 1.44 years compared with the control group[52].
Mathematical models estimated that a nationwide lifestyle intervention for the pre-diabetic population would be highly efficacious, resulting in a 9.53% decrease in cumulative diabetes incidence, an 0.82 year increase in mean life expectancy, a 0.52 year increase in QALY, a $700 decrease in mean total cost and an incremental cost-effectiveness ratio of -$1,339/QALY [53].
-
A national cross-sectional survey conducted from September 2009 to September 2010 among 47,204 adults > 18 years from 13 provinces, autonomous regions and municipalities in China has assessed the prevalence of chronic kidney disease (CKD). The overall prevalence of CKD was 10.8%. Therefore, the number of patients with CKD in China was estimated to be approximately 120 million. The adjusted prevalence of an estimated glomerular filtration rate (eGFR) < 60 mL/(min·1.73 m²) was 1.7%, and that of a urinary albumin to creatinine ratio > 30 mg/g was 9.4%.
The CHARLS from 2015 to 2016 included 6,706 participants ≥ 60 years of age with reduced renal function [eGFR < 60 mL/(min·1.73 m²)]. The overall prevalence of reduced renal function was 10.3% and increased with age (60–64 years: 3.3%; 65–69 years: 6.4%; 70–74 years: 11.4%; 75–79 years: 22.2%; and > 80 years: 33.9%)[54].
The China Kidney Disease Data Network (CK-NET) 2016 annual report indicated that the proportion of hospitalized patients with a comorbid CKD diagnosis was 4.86% of the total hospitalized patients in that year. The prevalence of CKD was 13.90% in patients with diabetes, 11.41% in those with hypertension, and 7.96% in those with CVD. A total of 18.82% of hospitalized patients with CKD had CHD, 16.91% had heart failure (HF), 13.22% had stroke, and 4.01% had atrial fibrillation (AF)[55].
In 2016, the median cost for inpatients with CKD was RMB 15,405 (IQR: RMB 8,435–RMB 29,542), which was higher than that for those without CKD RMB 11,182 (IQR: RMB 5,916–RMB 18,922). The average cost for patients with hemodialysis was RMB 89,257, and that for patients with peritoneal dialysis was RMB 79,653[55].
-
A total of 98,042 participants ≥ 18 years old were included in the analysis of the 2010–2012 China National Nutrition and Health Survey[56] in 31 provinces, autonomous regions and municipalities in mainland of China. Metabolic syndrome (MS) was defined according to the US National Cholesterol Education Program Adult Treatment Panel III criteria (NCEP ATP III). The prevalence of MS was 24.2%.
In the China National Nutrition and Health Survey 2010–2012, data were collected in 16,872 adolescents 10–17 years of age. According to the diagnostic criteria proposed by the Pediatric Branch of the Chinese Medical Association, the prevalence of MS was 2.4%. The prevalence of MS was 4.3% according to the Cook criterion.
-
Ambient air pollution and indoor air pollution are the 3rd and 13th greatest risk factors affecting DALY in China. Compared with 1990 values, the total number of deaths associated with indoor air pollution decreased by 72.7%, and DALY losses decreased by 80.2%, in 2019.
From 2000 to 2016, more than 30 million excess deaths in China have been attributed to long-term exposure to PM2.5, with annual excess deaths of 1.5 million–2.2 million[57].
A study on the evaluation of long-term PM2.5 exposure and related disease burden at the national level has shown that the number of deaths caused by PM2.5 pollution in China reached 30.08 million from 2000 to 2016. Since 2013, the total number of deaths caused by PM2.5 exposure in China has gradually decreased[57].
A series of studies based on data on air pollution and causes of mortality in 272 cities in China from 2013 to 2015 have reported that an increased risk of CVD mortality is associated with an increase in PM2.5 and coarse particulate matter (diameter 2.5–10.0 μm), O3, SO2, NO2, and CO. In addition, air pollution can increase the risk of CVD mortality and hypertension[58-61].
From a prospective cohort study in 226,000 urban residents in China, residents who used solid fuels rather than clean fuels (gas or electricity) for cooking had a 19% greater risk of all-cause mortality, a 24% greater risk of CVD mortality and a 43% greater risk of respiratory disease mortality. Moreover, kitchen ventilation decreased the risk of all-cause mortality by 19% and the risk of CVD mortality by 25%[62].
-
The National Demonstration Area for Comprehensive Prevention and Control of Non-communicable Diseases (hereafter referred to as "the demonstration area") is a pioneering project to implement the "Healthy China" concept and promote "health in all policies". By 2020, a total of 488 national demonstration areas were formed in 31 provinces, autonomous regions and municipalities, covering 17.1% of the counties in China[63]. The mid-term target of covering 15% of the demonstration area in 2020 required by the Medium and Long Term Plan for Chronic Disease Prevention and Control in China (2017–2025) has been achieved.
In the demonstration area of Tianjin, the "three reductions and three health" healthy lifestyle initiative was carried out to explore various innovative models such as community hypertension management and medical association construction. The analysis of whole population death surveillance data from 2008 to 2018 showed that the average life expectancy in the demonstration area increased from 81.48 years to 82.38 years. The average life expectancy of men increased from 79.66 to 80.31 years of age, and that of women increased from 83.44 to 84.51 years of age. In contrast, that of men in the non-demonstration area did not increase. Both the crude mortality and standardized mortality of AMI in the demonstration area showed a decreasing trend, and the annual percent change was greater than that in the non-demonstration area (crude mortality: −5.36% vs. −4.02%; standardized mortality: −6.27% vs. −5.41%).
In Chongqing and Guiyang, the probability of premature death from major chronic diseases in the demonstration area population was measured through the continual construction of a sound chronic disease surveillance system. The probability of premature death due to major chronic diseases in the demonstration area showed a significant decreasing trend, from 17.21% in 2012 to 15.38% in 2017, which was lower than those in the non-demonstration area in all years. The annual change was not significant in the non-demonstration area, with 16.79% and 17.05% in 2012 and 2017, respectively. According to the analysis in Guiyang, in 2018, the probability of premature death due to major chronic diseases in the demonstration area (including two national and three provincial demonstration areas) was 15.95%, and the probability of premature death due to CVD was 7.48%; that is, the overall probability of death due to CVD for people 30 years of age who were expected to survive to age 69 years of age was 7.48%.
-
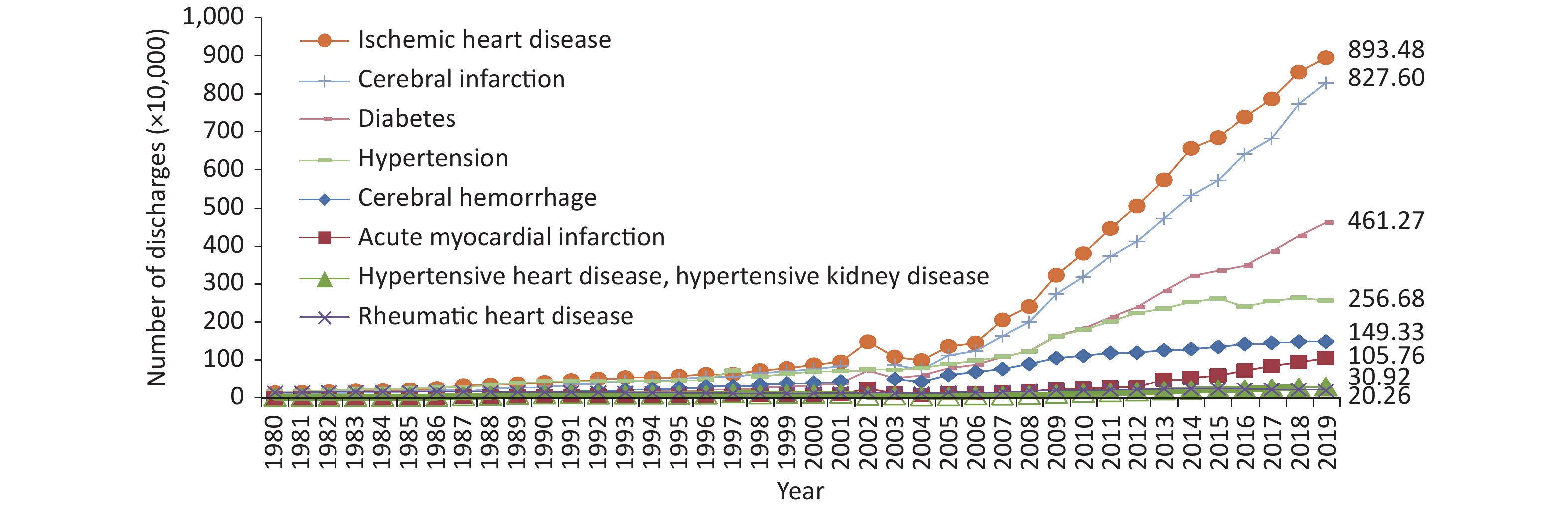
The prevalence of CVD in China is increasing. The number of patients with CVD is estimated to be 330 million: 13 million with stroke, 11.39 million with CHD, 8.9 million with HF, 5 million with pulmonary heart disease, 4.87 million with AF, 2.5 million with rheumatic heart disease, 2 million with congenital heart disease, 45.3 million with lower extremity arterial disease and 245 million with hypertension.
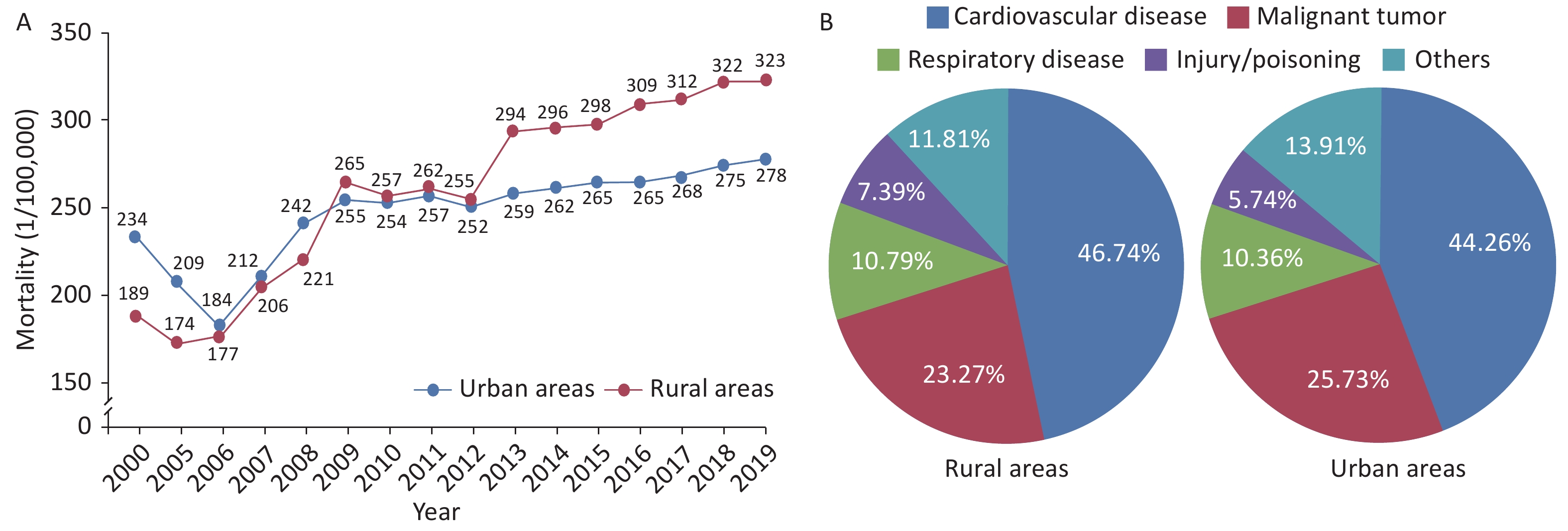
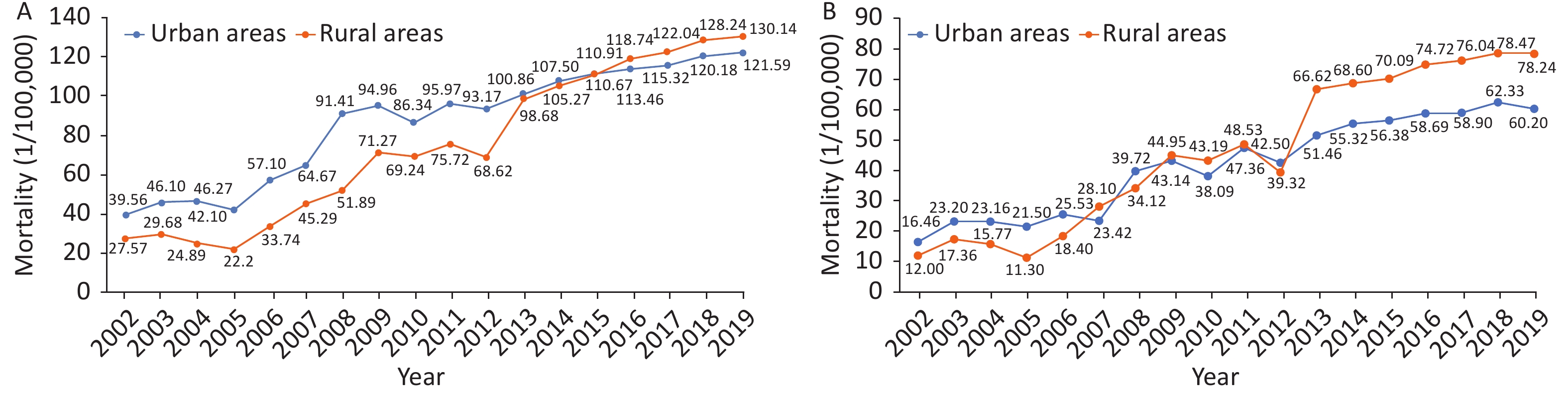
The mortality of CVD in rural areas has exceeded that in urban areas since 2009 (Figure 8A). CVD was the main cause of death[64] among rural and urban residents. In 2019, CVD accounted for 46.74% and 44.26% of deaths in rural and urban areas, respectively (Figure 8B). Two of five deaths were attributable to CVD.
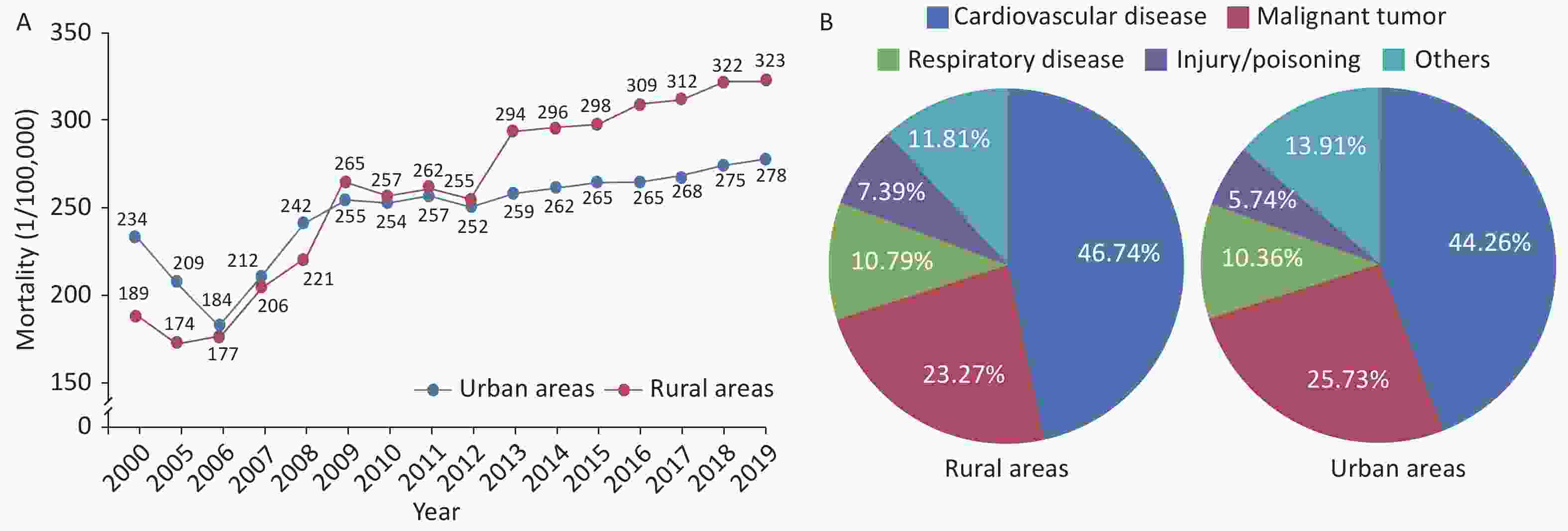
Figure 8. Changes in the mortality due to cardiovascular diseases among urban and rural residents in China from 2000 to 2019 (A) and the constituent ratios of major causes of death among urban and rural residents in China in 2019 (B).
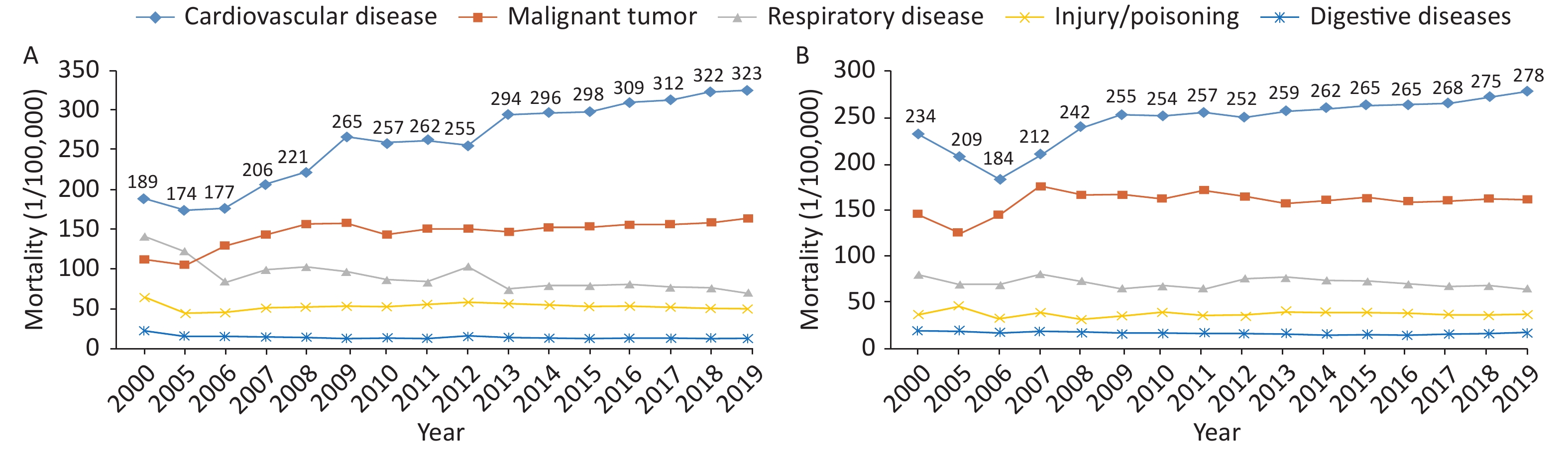
In 2019, the mortality due to CVD in rural areas was 323.29/100,000: 164.66/100,000 due to heart disease and 158.63/100,000 due to cerebrovascular disease (Figure 9A). The mortality due to CVD in urban areas was 277.92/100,000: 148.51/100,000 due to heart disease and 129.41/100,000 due to cerebrovascular disease (Figure 9B).
-
According to China Health Statistics Yearbook 2020[64], in 2019, the mortality due to CHD was 121.59/100,000 among urban residents and 130.14/100,000 among rural residents. The mortality due to CHD has been increasing since 2012. The mortality due to CHD in rural areas increased significantly and exceeded that in urban areas by 2016 (Figure 10A).
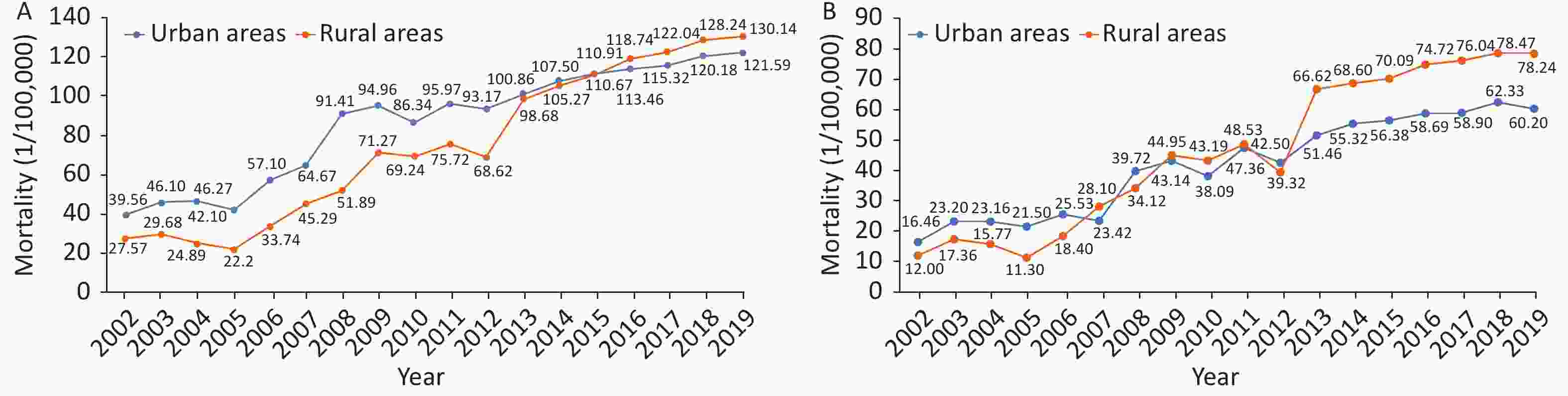
Figure 10. Trends in mortality due to coronary heart disease (CHD) (A) and acute myocardial infarction (B) in urban and rural areas of China from 2002 to 2019.
From 2002 to 2018, the mortality due to AMI showed an increasing trend, but a slight decrease was observed in 2019. The rate has increased rapidly since 2005. The mortality due to AMI in rural areas not only exceeded that in urban areas in 2007, 2009, and 2010, but also increased significantly since 2012. In 2013, the mortality of AMI in rural areas exceeded that in urban areas (Figure 10B).
According to the 5th National Health Services Survey in China, 2013, the prevalence of CHD among Chinese residents ≥ 15 years of age was 10.2‰, and that in people over 60 years of age was 27.8‰. Compared with that in the 4th data in 2008 (7.7‰), the total prevalence increased. There would be 11.40 million patients with CHD among Chinese residents ≥ 15 years of age. This number was 1.08 million more than the number of patients with CHD across all age groups in 2008, as calculated from the data from the 4th National Health Services Survey.
In the China PEACE study, 162 secondary and tertiary hospitals were randomly selected from 31 provinces, autonomous regions and municipalities in China, and 13,815 medical records were included in. In the 10 years from 2001 to 2011, the number of ST-segment elevation myocardial infarction (STEMI) inpatients increased each year per 100,000 people in China. In the general population, the hospitalization rate for STEMI increased from 3.7/100,000 in 2001 to 8.1/100,000 in 2006 and 15.8/100,000 in 2011. Significant geographical differences in the medical process and results for patients with AMI have been observed in China and found to persist at 2001, 2006, 2011, and 2015[65].
The China Acute Myocardial Infarction (CAMI) Registry study[66] has indicated significant differences in the treatment and outcomes of patients with STEMI in different levels of hospitals in China. Compared with that in provincial hospitals, the proportion of patients with STEMI receiving reperfusion treatment in prefectural and county-level hospitals was lower, and the proportion of in-hospital deaths was higher.
The China Clinical Pathway of Acute Coronary Syndrome study (CPACS)[67] enrolled 15,140 patients with ACS in 70 hospitals in 17 provinces, autonomous regions and municipalities in China. The application rate of standardized secondary preventive drugs in ACS patients after discharge decreased each year. The application rate at discharge was 86%, then decreased to 68% 1 year later and to 59.7% 2 years later.
A study of 3,387 patients within 24 h after AMI onset in 53 hospitals in various regions of the country[68] has reported a readmission rate within 30 days of 6.3%, nearly 50% of which occurred within 5 days after discharge. A total of 77.7% of patients were hospitalized because of cardiovascular events, including angina pectoris (31.2%), HF (16.7%), and AMI (13.0%).
China PEACE[69] has demonstrated that Chinese patients with AMI have a high recurrence rate of early myocardial infarction after discharge. The recurrence rate of myocardial infarction within 1 year is 2.5%, of which 35.7% of cases occur within 30 days after discharge. The 1-year mortality of patients with recurrent myocardial infarction increased by 25.42 times, and the 1-year mortality of patients with early recurrent myocardial infarction was highest (53.5%).
The China Acute Myocardial Infarction (CAMI) study analyzed data for 80 hospitals that admitted ≥ 50 patients with STEMI and were able to provide emergency percutaneous coronary intervention (PCI) from 2013 to 2016[70]. A total of 29,581 patients with STEMI were admitted to these hospitals, and the in-hospital mortality was 6.3%. Combined with the Chinese guidelines for STEMI diagnosis and treatment and the American myocardial infarction quality standard, the opportunity-based composite score (OBCS) indicated in-hospital mortality of patients with STEMI in lower OBCS (< 71.1%), moderate OBCS (71.1%–76.5%) and higher OBCS (> 76.5%) hospitals of 7.2%, 6.6%, and 5.4%, respectively.
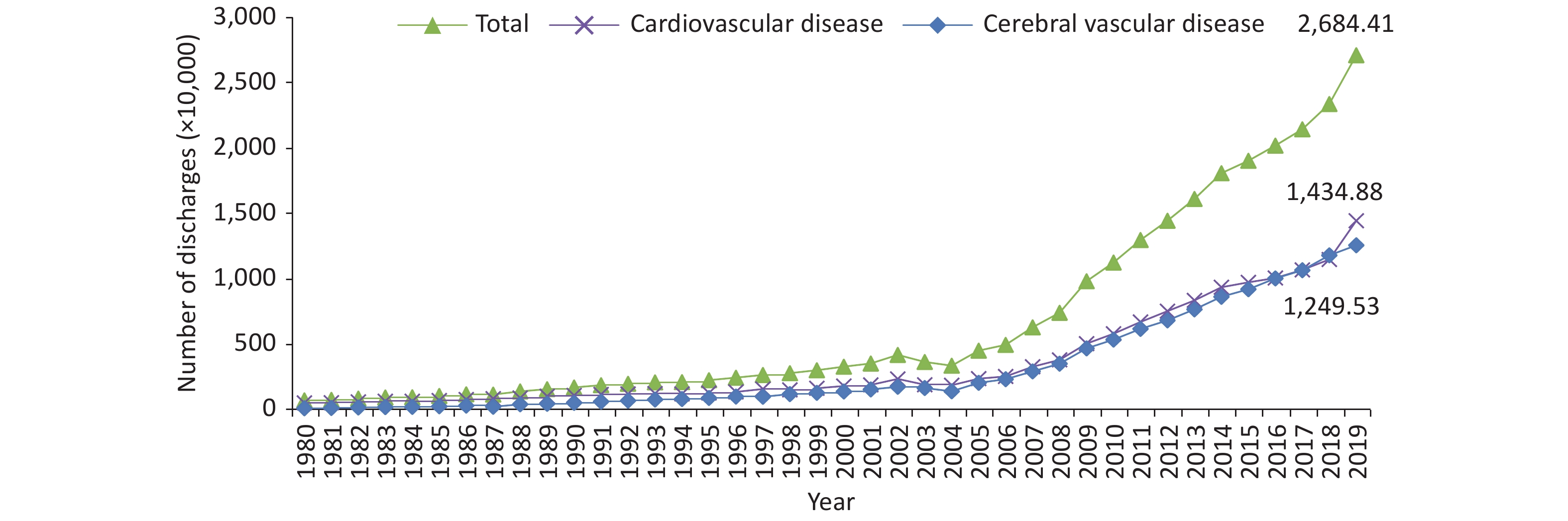
According to the data from hospital quality monitoring system (HQMS) for 10,259,521 CVD related inpatients (excluding those in military and traditional Chinese medicine hospitals) in 1,910 tertiary public hospitals (accounting for 79.5% of all tertiary public hospitals in China) and 2,124 secondary public hospitals (accounting for 35.9% of all secondary public hospitals in China) performed CVD diagnosis and treatment, there were 1,014,266 patients treated with PCI in China in 2020[71].
According to data from 87 heart centers nationwide enrolled in the China Cardiac Surgery Registration[72], a total of 56,776 patients received coronary artery bypass grafts from 2013 to 2016, and the total in-hospital mortality after the procedure was 2.1%.
From 2017 to 2019, a multi-center cross-sectional study, conducted in nine locations in China on more than 6,000 patients who underwent coronary angiography or CT angiography, has indicated that facial features are associated with an increased risk of CAD. The team has developed and verified a deep learning algorithm based on facial photos to detect CAD, which can assist in identifying CAD and is expected to be used in outpatient CAD probability assessment or community CAD screening[73].
-
Cerebrovascular disease is a major cause of death in China, reaching 2,189,175 cases in 2019. Compared with those in 2009, the number of deaths increased by 12.4%. In 2019, 3,935,182 new stroke cases and 28,760,186 patients with stroke in China were reported. Stroke was also the primary cause of DALY in 2019. The number of DALY reached 45,949,134, and the age standardized DALY rate was 2,412.52/100,000[74].
In 2019, the crude mortality due to cerebrovascular disease among Chinese residents was 149.56/100,000, accounting for 22.17% of total deaths, and ranking third among major causes of death, after malignant tumors (162.46/100,000) and heart disease (160.26/100,000).
The crude mortality due to cerebrovascular disease among urban residents in China was 129.41/100,000, accounting for 20.61% of the total urban deaths; that among rural residents was 158.63/100,000, accounting for 22.94%. The crude mortality rate due to cerebrovascular disease in men was higher than that in women, and that in rural areas was higher than that in urban areas[64].
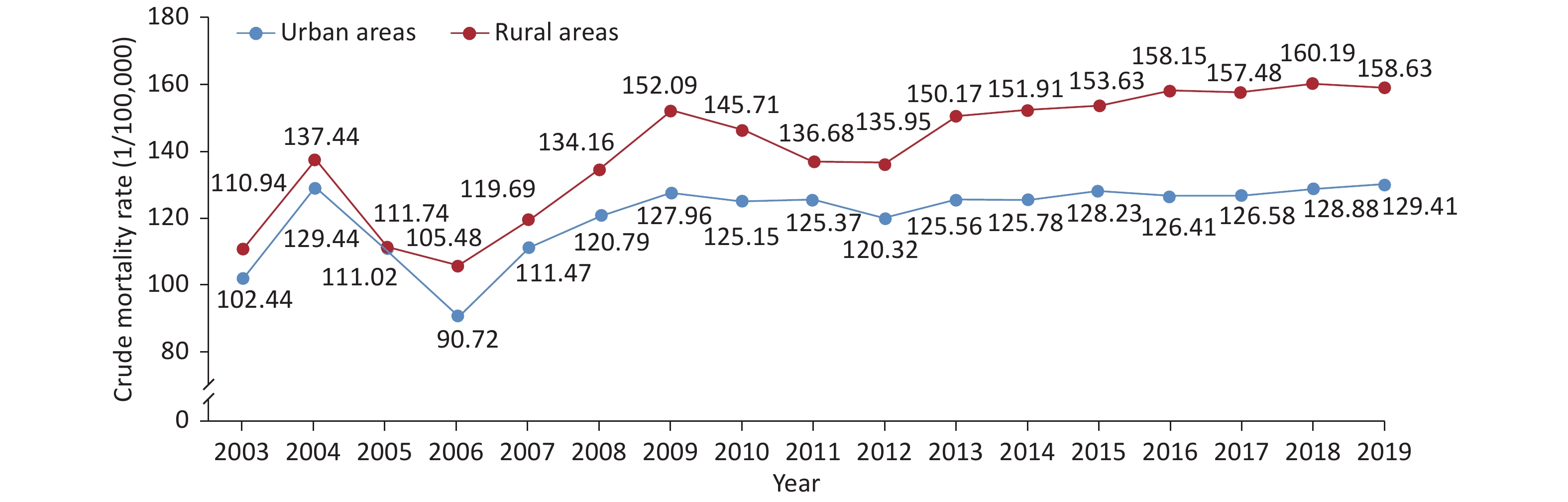
From 2003 to 2019, the crude mortality due to cerebrovascular disease in rural areas was higher than that in urban areas. Compared with the rate in 2006, the crude mortality due to cerebrovascular disease in 2009 increased by 1.41 times in urban areas and 1.44 times in rural areas. The crude mortality due to cerebrovascular disease showed a decreasing trend from 2009 to 2012, but increased slightly from 2013 to 2019, and was significant in rural areas (Figure 11).
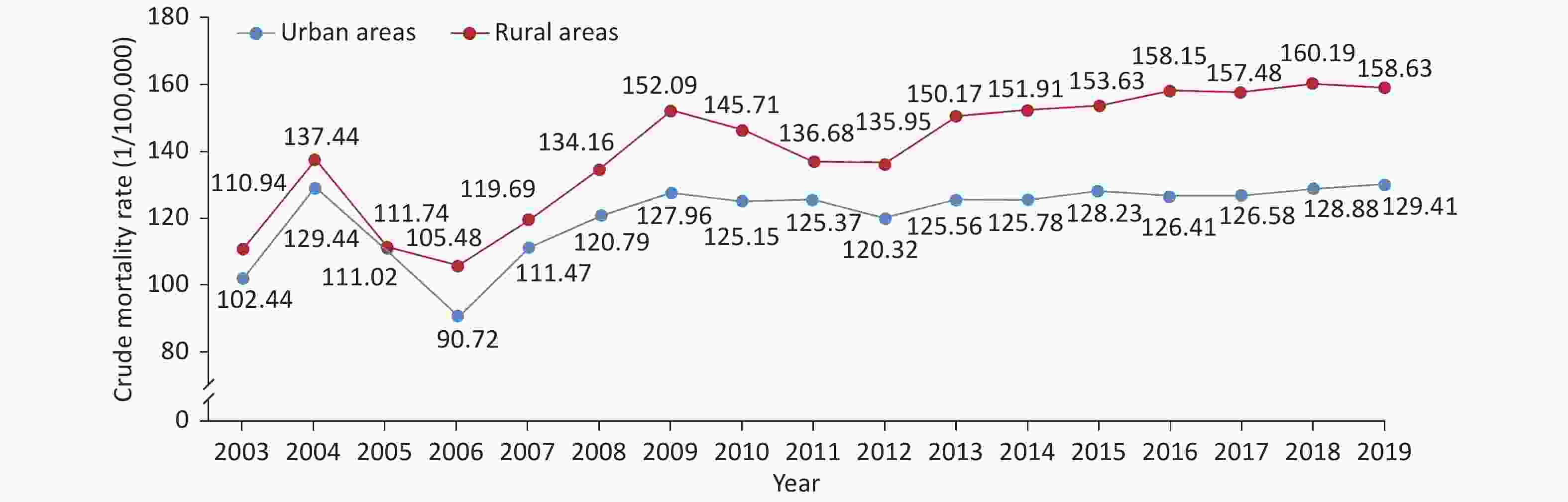
Figure 11. Trends in crude mortality of cerebrovascular disease in urban and rural residents in China from 2003 to 2019.
From 1997 to 2015, the CHNS analysis of 15,917 residents indicated an age standardized stroke incidence rate of 4.17/1,000 person-years in the north and was statistically significantly lower in the south, at 1.95/1,000 person-years. This difference was found in rural areas rather than urban areas. Hierarchical model analysis suggested that regional differences could be explained by differences in hypertension prevalence[75].
The transient ischemic attacks (TIA) epidemiological survey in 2013 involved face to face surveys of 178,059 families in 155 disease surveillance sites. A total of 595,711 people were analyzed for TIA incidence. The weighted incidence rate of TIA was 23.9/100,000: 21.3/100,000 in men and 26.6/100,000 in women. A total of 310,000 new TIA cases have been estimated to occur in China every year[76].
According to an epidemiological survey in 2013, the prevalence rate of stroke in China was 1,596.0/100,000, and the age standardized prevalence rate was 1,114.8/100,000; the rates were higher in rural areas (1,291.1/100,000) than in urban areas (814.4/100,000). The highest prevalence rate of stroke was in central China (1,549.5/100,000), followed by northeast China (1,450.3/100,000) and northern China (1,416.5/100,000), whereas the lowest rate was in South China (624.5/100,000)[77].
The 2019 annual cerebrovascular disease surveillance platform has identified a total of 291,632 inpatients with acute ischemic stroke in 31 provinces nationwide; intravenous thrombolysis rate of recombinant plasminogen activator for those who arrived within 4.5 h of onset was 30.4%, and the in-hospital mortality rate was 0.4% (Table 3).
Medical quality indicators n (%) Process indicators Thrombolytic rate of rt-PA in patients who came to the hospital within 4.5 hours of onset 22,400 (30.4) Prevention rate of deep venous thrombosis in patients unable to walk within 48 hours after admission# 9,266 (12.0) Dysphagia screening rate 231,089 (80.7) Rehabilitation evaluation rate 212,028 (74.0) Antithrombotic treatment rate at discharge 251,035 (88.7) Anticoagulation treatment rate for patients with atrial fibrillation at discharge 9,166 (45.9) Statin treatment rate for patients with non-cardiogenic cerebral infarction at discharge 248,258 (90.7) Antihypertensive treatment rate for patients with hypertension at discharge 143,232 (64.9) Hypoglycemic drug treatment rate for patients with diabetes at discharge 63,678 (78.4) Outcome indicators Hospitalization mortality 1,066 (0.4) Note. rt-PA, recombinant plasminogen activator. #The number of patients unable to walk on their own within 48 h after admission within a unit time who received prophylaxis for deep vein thrombosis (anticoagulants and/or combination intermittent inflation and compression) accounted for the proportion of hospitalized patients who could not walk by themselves in the same period. Table 3. Medical quality indicators for inpatients with acute ischemic stroke in 2019
-
According to the data statistics of the online registration system of the National Health Commission and the data reported by the provincial quality control center, during the COVID-19 pandemic, 86,181 cardiac pacemakers were implanted nationwide in 2020, representing a 4.8% decrease with respect to 2019, of which dual chamber pacemakers accounted for 73%. The indications for pacemaker implantation mainly included sick sinus syndrome (55.0%), atrioventricular block (41.5%) and other indications (3.5%). Clinical research on the feasibility, safety and effectiveness of His-Purkinje system pacing, including His bundle or left bundle branch pacing, in patients with bradyarrhythmia has rapidly progressed in China[78]. Left bundle branch pacing technology originated in China and has been described in more than 70 academic articles in international CVD related journals since 2019.
According to CHS, from 2012 to 2015[79], the prevalence of AF was 0.7% in Chinese residents ≥ 35 years of age, and was higher in rural (0.75%) than urban (0.63%) residents. A total of 34% of the patients were diagnosed with AF for the first time and were unaware of their condition.
A survey of 1,252,703 adults over 40 years of age by the China stroke screening survey from 2013 to 2014 has indicated that 12% of Chinese patients with ischemic stroke had AF. On the basis of this calculation, more than 2.15 million Chinese patients with ischemic stroke had AF, and the proportion of these patients receiving anticoagulation therapy was very low, at only 2.2%, of which 98.2% of patients used warfarin[80].
The Chinese Atrial Fibrillation Registry study analyzed 7,977 patients with non-valvular AF in 32 hospitals from 2011 to 2014. The proportions of oral anticoagulation use were 36.5%, 28.5%, and 21.4% for patients with CHA2DS2-VASc scores ≥ 2, 1, and 0, respectively. These proportions varied from 9.6% to 68.4% in tertiary hospitals and from 4.0% to 28.2% among nontertiary hospitals.
According to data from the AF registration research platform, the proportion of radiofrequency catheter ablation in patients with AF increased each year, accounting for 27.3%, 31.9%, 33.0%, and 32.2% of the total ablations in 2017, 2018, 2019, and 2020, respectively. Circumferential pulmonary vein isolation remained a major procedure, accounting for 60.2% of total ablations. The incidence of periprocedural ischemic stroke was 0.4%, and that of hemorrhagic stroke was 0.1%[81].
Radiofrequency catheter ablation has been widely used in more than 600 hospitals in China. According to the online registration system of the National Health Commission, the number of radiofrequency catheter ablation operations has continued to grow rapidly since 2010, with an annual growth rate of 13.2% to 17.5%. During the COVID-19 pandemic, the number of radiofrequency ablation operations in 2020 was 102,864, a number significantly lower than those in previous years. In 2020, the ablation rate for supraventricular tachycardia was 40.7%, and the radiofrequency ablation rate for AF was 32.2%—essentially the same as that in 2019.
A prospective study has monitored 678,718 participants from July 2005 to June 2006. At the 1-year follow-up, 284 (9.5%) sudden cardiac death (SCD) had occurred among 2,983 total deaths. The overall annual incidence of SCD was 41.8/100,000, and was higher in men than in women (44.6/100,000 vs. 39.0/100,000). On the basis of this project, SCD was estimated to account for more than 500,000 deaths in China annually.
According to the statistics of the online registration system of the National Health Commission and the data reported by the provincial quality control center, the implantation of implantable cardioverter defibrillators (ICD) decreased slightly in 2020 during the COVID-19 pandemic, compared with 2019 (4,800 cases vs. 5,031 cases). In 2020, single chamber accounted for 50% of ICD, while primary prevention accounted for 53% and secondary prevention accounted for 47%.
Among 230 patients with long QT syndrome (LQTS) from ten hospitals in China, LQT1 (KCNQ1 mutation, 37%), LQT2 (KCNH2 mutation, 48%) and LQT3 (SCN5A mutation, 2%) were the main subtypes.
The Chinese Ion Channelopathy Registry and International Project Collaborative Group Study have indicated that the probands’ mean age of onset was 17.3 ± 14.2 years; 60% had an onset before the age of 20 years, and 76% were women. Children with LQTS had a high degree of malignancy, with a clinical phenotype mostly presenting as complex arrhythmias and a pathogenic or likely pathogenic mutated gene detection rate of 71%[82]. In southwest China, 33.7% of patients with sudden unexplained death carried LQTS associated mutated genes (KCNQ1 and KCNH2)[83].
In a domestic health screening study among employed people 20–50 years of age, the detection rate of early repolarization ranged from 2.73% to 3.99% and was more frequent in men, with a higher occurrence in those with moderate or higher labor intensity. The detection rate of early repolarization in the ECG screening of 13,405 high school or college students was 1%, and was more frequent in men than women. Early repolarization occurred most frequently in inferior wall leads, followed by inferior and lateral wall leads, with a morphology of predominantly contusive and notch type. During a follow-up period of 12–36 months, no students experienced cardiovascular events, such as sudden cardiac death, or arrhythmia. An analysis of electrocardiograms of 1,215 students in competitive sports programs has indicated an early repolarization rate of 35.9%; early repolarization was more common in men, occurred most frequently in inferior wall leads and mostly showed contusive morphology.
-
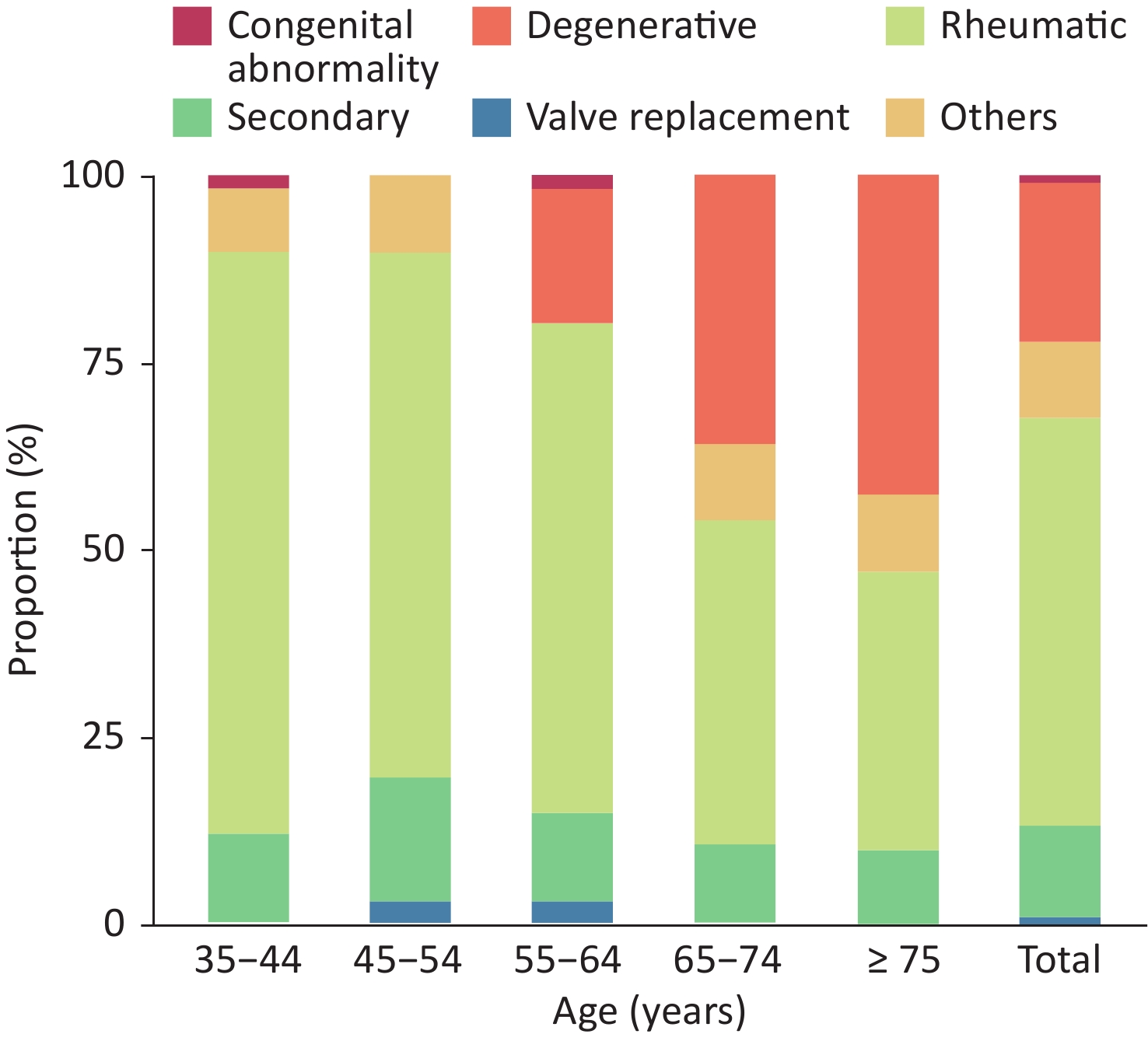
From October 2012 to December 2015, 31,499 residents ≥ 35 years of age received echocardiography in a study using a stratified multistage random sampling method. A total of 1,309 people had valvular heart disease, and the weighted prevalence of valvular heart disease was 3.8%. Approximately 25 million patients have been estimated to have valvular heart disease in China[84]. Rheumatic valvular disease remains the main cause of valvular heart disease in China, and the number of patients with degenerative valvular disease has significantly increased in recent years. Among Chinese patients with valvular heart disease, 55.1% had rheumatic valvular disease, and 21.3% had degenerative valvular disease (Figure 12).
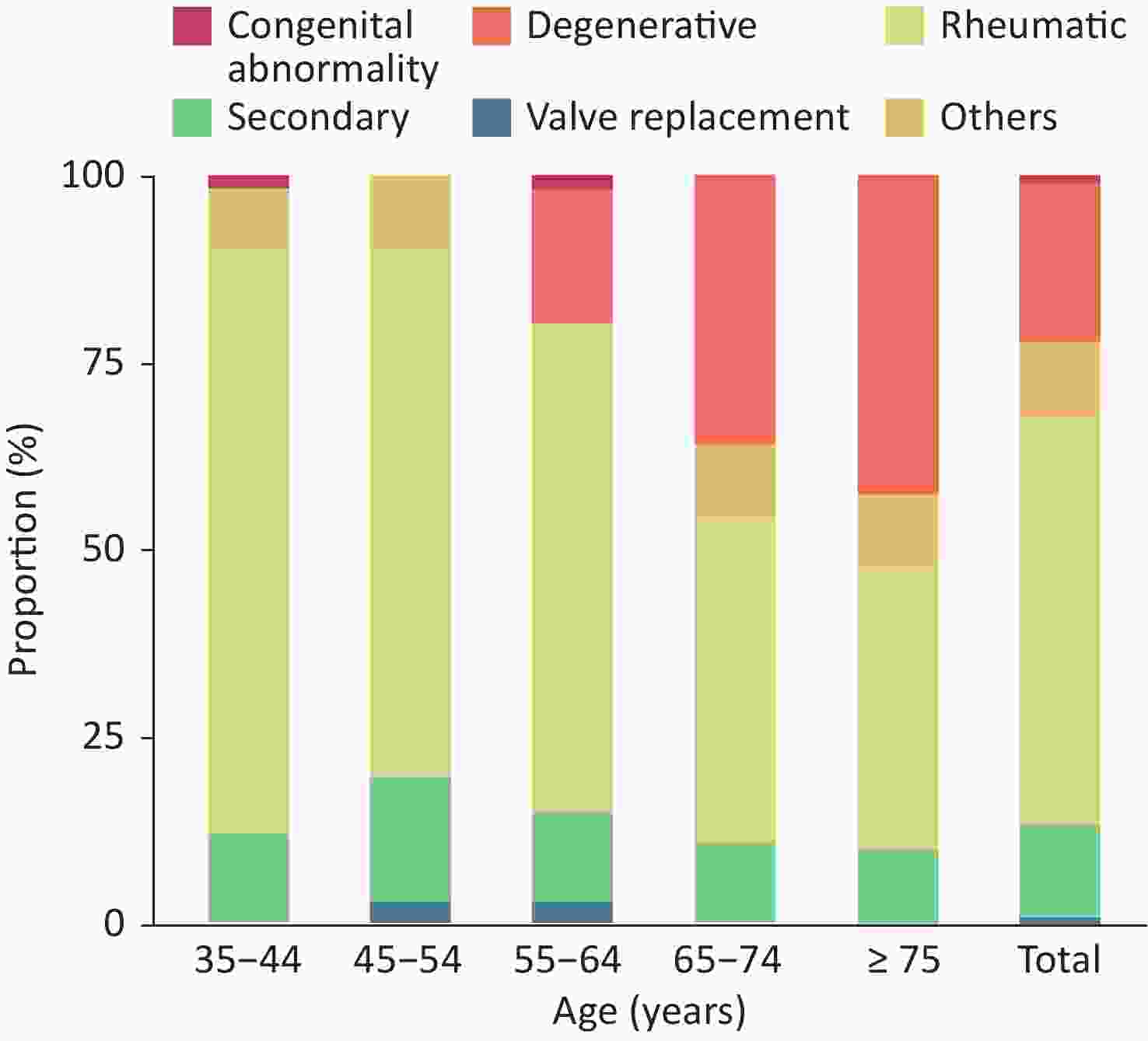
Figure 12. Proportion of valvular heart diseases due to different causes in the indicated age groups.
Researchers from Zhongshan Hospital Affiliation to Fudan University analyzed the data for 325,910 patients who underwent transthoracic echocardiography in the hospital from January 2011 to December 2015. A total of 3,673 patients (1.13%) were diagnosed with bicuspid aortic valve, accounting for 69.1% of men, 58.4% of patients with definite aortic valve insufficiency, 52.5% of patients with ascending aortic dilatation and 19.2% of patients with aortic root dilatation[85].
-
Congenital heart disease ranks first among neonatal birth defects in many areas of China. Regional differences exist in the detection rate of congenital heart disease, and rates vary primarily between 2.9‰ and 16‰.
A meta-analysis of the detection rate and spatial distribution characteristics of neonatal congenital heart disease in China[86] including data on 76,961,354 neonates in 617 studies from 1980 to 2019 has indicated that the detection rate of national neonatal congenital heart disease increased from 0.201‰ in 1980–1984 to 4.905‰ in 2015–2019. The detection rate of congenital heart disease increased gradually from the west to the east, and decreased gradually from the south to the north.
A survey of 122,765 newborns from 12 hospitals in eastern China and 6 hospitals in western China from August 2011 to November 2012[87] has indicated a detection rate of neonatal congenital heart disease in China of 8.98‰, with a higher rate in girls (11.11‰) than in boys (7.15‰).
According to China Health Statistics Yearbook 2020 [64], in 2019, the mortality rate due to congenital heart disease in urban residents in China was 0.76/100,000, and that in rural areas was higher, at 0.91/100,000.
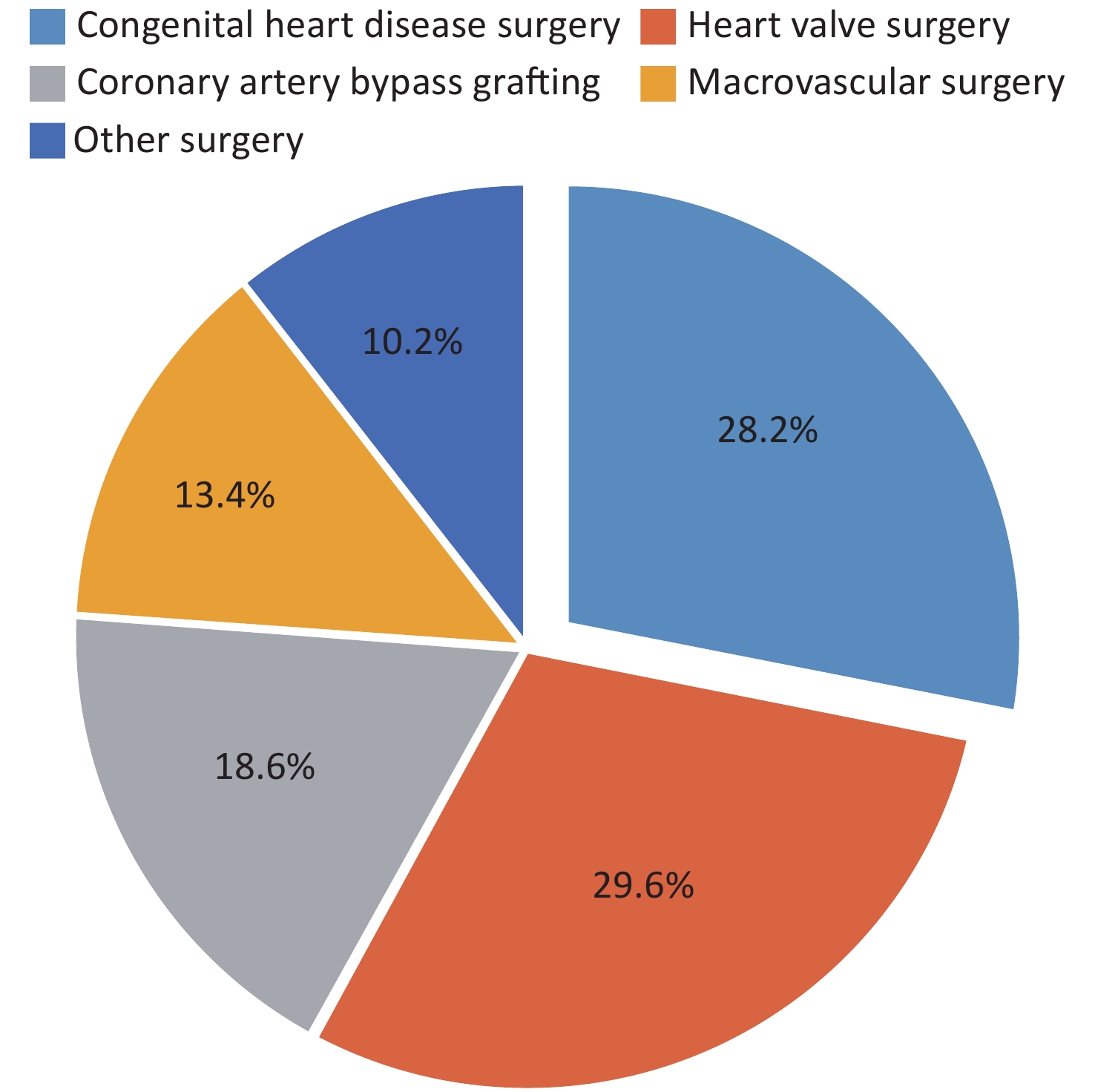
In 2020, according to the data from 714 hospitals performing cardiac surgery in China (including Hong Kong Special Administrative Region)[88] collected by the cardiopulmonary bypass branch of the Chinese Society of Biomedical Engineering, a total of 62,704 patients received surgery for congenital heart disease, accounting for 28.2% of all cardiac and aortic surgeries, and the proportion showed a decreasing trend, thus causing congenital heart disease to fall to second place among diseases receiving cardiovascular surgery treatment for the first time (Figure 13). This decrease might have been associated with the decline in the number of births and the birth rate every year, and the popularity of prenatal diagnosis and prenatal screening. The number of heart surgeries performed in patients under 18 years of age was 37,665, accounting for 60.1% of the total number of congenital heart disease surgeries in 2020, representing a decrease of 6.5% compared with 2019. Thus, adult congenital heart disease correction surgery is increasing each year, accounting for a high proportion of cardiovascular surgeries in China.
According to the data from the National Health Commission's network direct report system for interventional treatment of congenital heart disease and the military's network direct report system for interventional treatment of congenital heart disease, the total number of interventional treatments for congenital heart disease in mainland of China in 2019 was 39,027. Among them, the number of interventional treatments of congenital heart disease in local hospitals in mainland of China in 2019 was 34,758, representing an increase of 5.45% with respect to 2018. The treatment success rate was 98.41%, the incidence of serious complications was 0.12%, and the mortality was 0.01%. Overall, the number of cases of interventional treatment for congenital heart disease in local hospitals in China showed a slow increasing trend. In 2019, the number of local hospitals performing interventional treatment for congenital heart disease in mainland of China reached 313, and the number of physicians performing this treatment reached 483.
-
From October 2001 to February 2002, a stratified cluster sampling survey was conducted among 8,080 residents (including 4,064 men and 4,016 women) in nine provinces and cities of China. The crude prevalence rate of hypertrophic cardiomyopathy (HCM) was 0.16%. The prevalence of HCM in men (0.22%) was higher than that in women (0.10%). After adjustment for age and sex, the prevalence rate was 80/100,000. On the basis of these data, more than 1 million adult patients have been estimated to have HCM in China.
According to a survey of nine provinces (regions), the prevalence of dilated cardiomyopathy (DCM) in China is 19/100,000. From July 2011 to December 2011, a total of 49,751 residents were investigated in 120 villages in non-Keshan disease areas of seven provinces in northern China. A total of 6 DCM cases were detected, and the estimated prevalence rate was 1.2/10,000.
The Chinese Society of Cardiology analyzed 10,714 patients with HF from 42 hospitals in China in 1980, 1990, and 2000, and found proportions of DCM of 6.4%, 7.4%, and 7.6%, respectively.
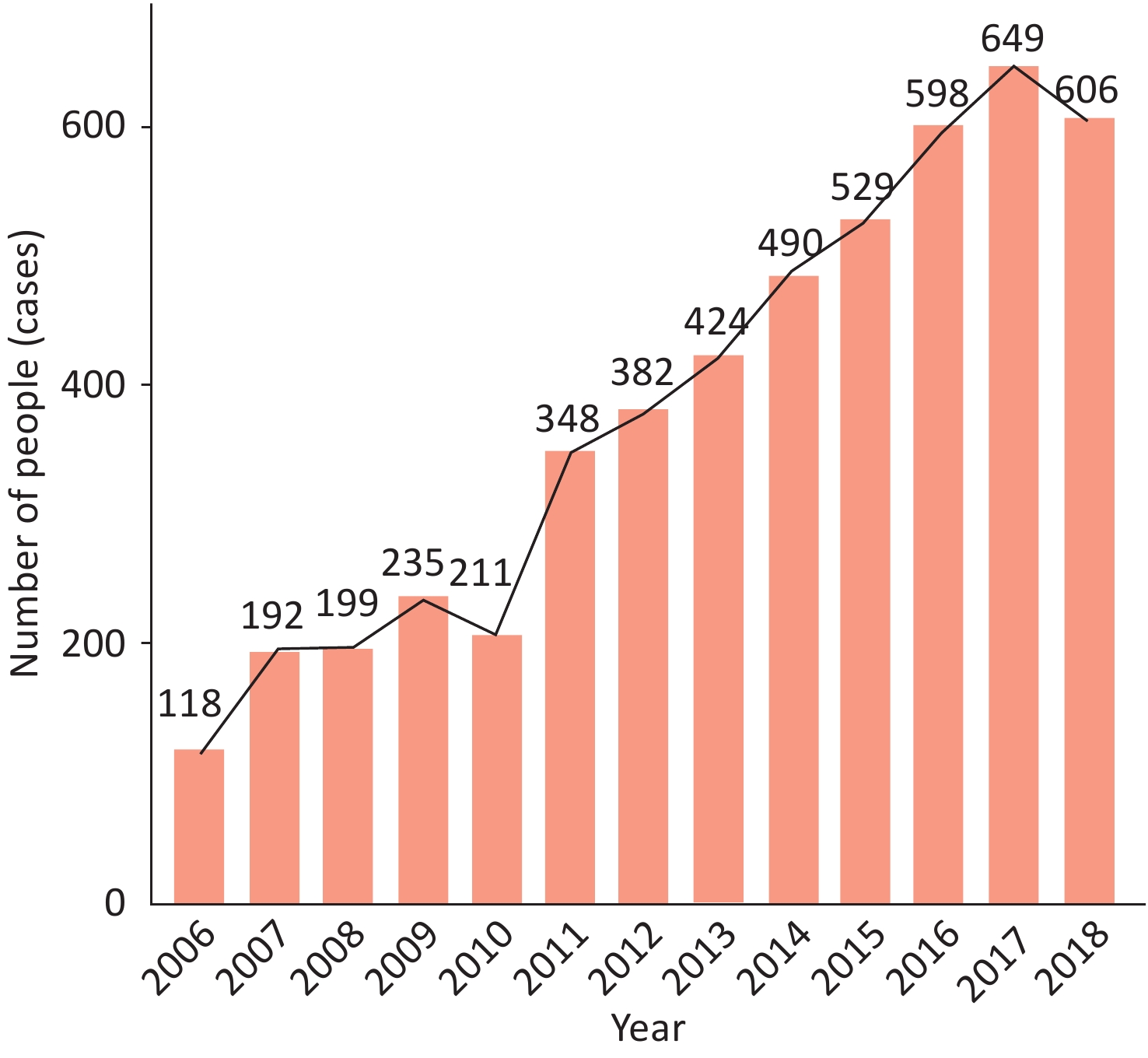
A survey by the Cardiovascular Group of the Pediatric Branch of the Chinese Medical Association[89] has reported that a total of 4,981 children with cardiomyopathy were admitted to 33 hospitals in China from July 2006 to December 2018, accounting for 0.079% (4,981/6,319,678 cases) of pediatric hospitalized children in the same period. DCM accounted for the most cases [1,641 (32.95%)], followed by endocardial fibroelastosis (EFE) [1,283 (25.76%)] and left ventricular non-compaction (LVNC) [635 (12.75%)]. The overall number of inpatients is increasing each year (Figure 14).
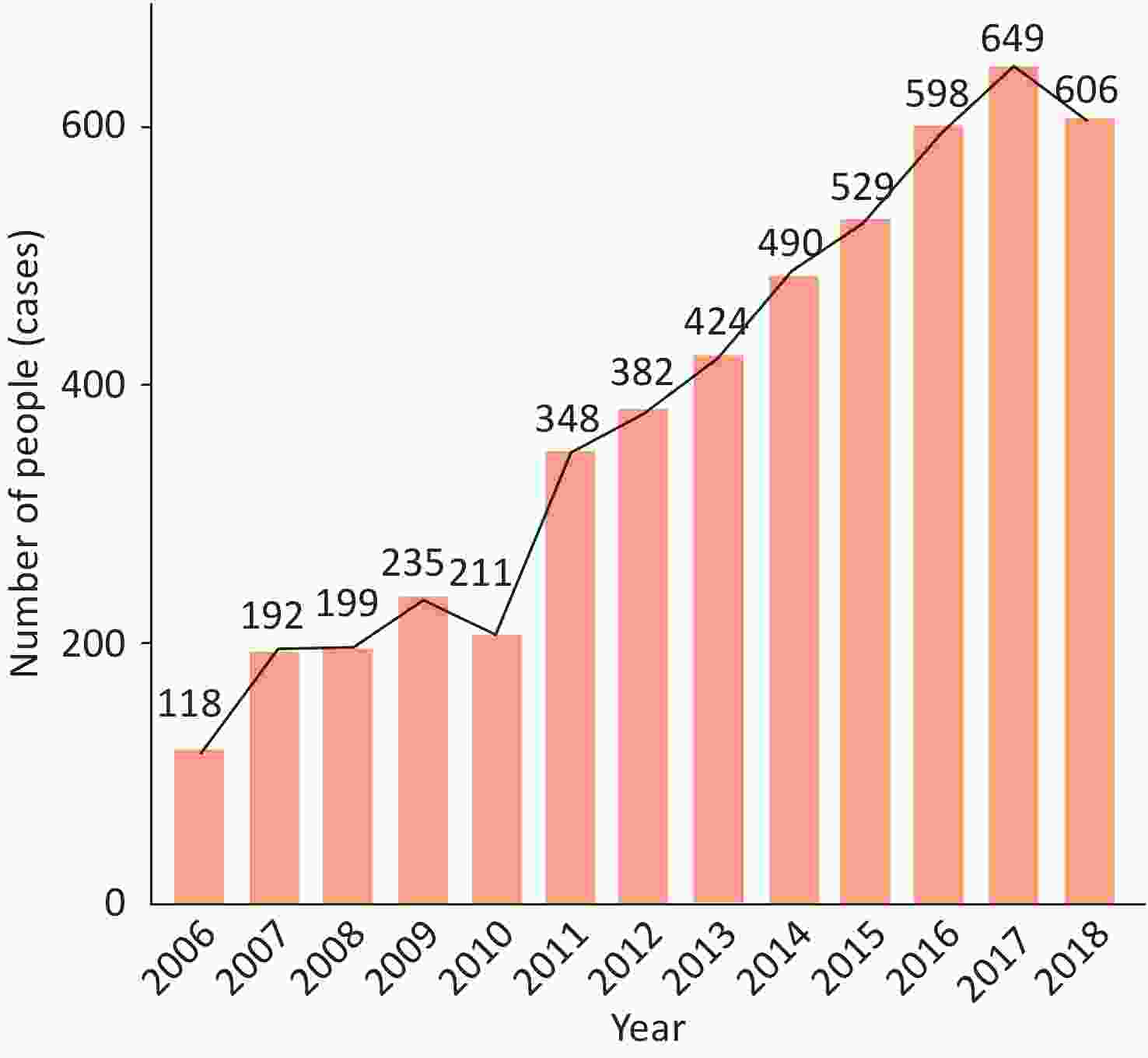
Figure 14. Annual number of pediatric inpatients with cardiomyopathy in 33 hospitals in China from 2006 to 2018.
In a domestic study, 529 patients with HCM were subjected to gene detection. It was found that 43.9% of the patients could be detected definite pathogenic mutations, among which, MYH7 and MYBPC3 genes accounted for the largest proportion. In 2020, a study at the Fuwai Hospital of the Chinese Academy of Medical Sciences found that common genetic variants are also important contributors to HCM, thus suggesting a non-Mendelian inheritance pattern with ethnic specificityy[90].
Arrhythmogenic cardiomyopathy (ACM) is mainly caused by mutations in the gene encoding desmoglein. Domestic studies have shown that pathogenic mutations can be detected in 63.3% of patients with ACM, of which PKP2 accounted for the largest proportion[91]. It was found that the founder mutation p.Phe531Cys of the homozygous DSG2 gene was a risk factor for China ACM, which was at a frequency of 8% with a full penetrance[92]. Homozygous c.245G > A/p.G82D mutation in the PNPLA2 gene is associated with the phenotypic penetrance of ACM[93].
A study has retrospectively analyzed all fetuses with non-compaction of ventricular myocardium (NCCM) diagnosed antenatally from October 2010 to December 2019. A total of 37 cases of NCCM were identified in 49,898 fetuses, and the detection rate of NCCM was 0.07%. Among them, 47% had positive gene testing results, most of which were non-sarcomere gene mutations. No mutations were found in the three sarcomere genes most common in children and adults (MYH7, TTN, and MYBPC3)[94].
-
A survey among 15,518 residents from 20 urban and rural areas in China showed that the prevalence of chronic HF was 0.9% in the population aged 35–74 years in 2000.
CHS analyzed 22,158 participants [95], and found that the prevalence rate of HF was 1.3% among adults aged 35 years or older. The prevalence of left ventricular systolic dysfunction (LVEF < 50%) was 1.4%, and that of moderate/severe diastolic dysfunction was 2.7%.
China Heart Failure (China-HF) Registry Study[96] enrolled 13,687 patients with HF from 132 hospitals in China from January 2012 to September 2015, and the in-hospital mortality was 4.1%. In the China Heart Failure Medical Quality Control Report in 2020[97], an analysis of 33,413 patients with HF with recorded hospital outcomes, who were treated at 113 hospitals nationwide from January 2017 to October 2020, has indicated a mortality of 2.8% among hospitalized patients.
From January 2011 to September 2012, 3,335 patients with acute HF in 14 hospitals in Beijing were followed up for 5 years[98]. The 5-year all-cause mortality rate was 55.4%, the CVD mortality rate was 49.6%, and the median survival time was 34 months.
According to the China Heart Failure Medical Quality Control Report in 2020 [97], the average age of patients with HF was 67 ± 14 years, and men accounted for 60.8%. The proportion of valvular disease in patients with HF has decreased each year. Hypertension (56.3%) and CHD (48.3%) have become the main causes of HF in China. Infection is the primary cause of HF, followed by myocardial ischemia and fatigue. HF with decreased ejection fraction, with intermediate ejection fraction and with preserved ejection fraction accounted for 40.2%, 21.8%, and 38.0%, respectively.
The overall usage rate of diuretics in hospitalized HF patients in China had not changed significantly. The usage rate of digoxin had shown a downward trend due to the influence of international clinical studies. In the meantime, the usage rate of aldosterone receptor antagonists and β-receptor blockers had increased significantly. The overall usage rate of renin angiotensin system (RAS) blockers showed an upward trend, but because of the advent of angiotensin receptor enkephalinase inhibitor (ARNI), the usage rate of angiotensin-converting enzyme inhibitor (ACEI) and angiotensin II receptor antagonist (ARB) decreased (Table 4)[97].
Research source Investigation year Sample size
(cases)Utilization rate of therapeutic drugs (%) Nitrate Diuretics Digitalis ARB ACEI ARNI MRA β receptor
blockerCalcium
antagonist42 hospitals in China 1980 1,756 44.7 73.7 51.7 0.4 14.0 − 10.0 8.5 6.1 1990 2,181 36.0 70.2 45.5 1.4 26.4 − 8.4 9.5 16.4 2000 6,777 53.0 48.6 40.3 4.5 40.4 − 20.0 19.0 10.5 Hubei 2000−2010 16,681 − 69.1 46.2 18.7 51.6 − − 46.6 − 10 hospitals 2005−2009 2,154 53.2 74.4 57.6 Total 66.0 − 74.6 68.3 46.1 Kunming 2008−2012 2,106 − 84.8 28.2 Total 82.8 − 76.6 72.2 − Xinjiang Uygur
Autonomous Region2011−2012 5,357 − 45.5 26.8 Total 72.8 − 46.6 66.8 − China-HF study 2012−2015 13,687 41.4 72.2 − 28.8a 71.7b − 74.1b 70.0b − 51.3c 49.4c 48.7c 52.2c Heart failure quality
control report2007−2020 33,413 − 75.0 29.3 Total 44.0 36.9 87.8 82.2 − Note. a, Intravenous medication during hospitalization; b, Oral drugs used in patients with HFrEF after discharge; c, Oral drugs used in patients with HFpEF after discharge; ACEI: Angiotensin-converting enzyme inhibitor; ARB: Angiotensin II receptor antagonist; MRA: Mineralocorticoid receptor antagonist; ARNI: Angiotensin receptor enkephalinase inhibitor. −: Not reported. Table 4. Drug application in patients with heart failure
According to statistics from the online registration system of the National Health Commission of China and the data reported by the provincial quality control center, the number of cardiac resynchronization therapy (CRT) implants in 2020 was 3,896, representing a decrease of 13.9% with respect to 2019. The proportion of CRT-D implantations increased each year, because patients who met CRT-P indications also met CRT-D indications. From 2013 to 2015, 454 cases of CRT-P/D from 22 centers in China were included in a study, and 52.2% of the patients chose CRT-D. The proportion of CRT-D in patients treated with CRT in 2019 further increased to 64%. The ratio of CRT-D was higher in hospitals with an annual number of implants exceeding 40 and lower in areas with lower GDP.
To date, nearly 100 implantable left ventricular assist device operations have been performed in 16 hospitals in China. Among them, the National Medical Products Administration has approved only three registration clinical trials on the evaluation of the safety and effectiveness of artificial heart treatment of end-stage HF.
The first was the EVAHEART I clinical trial study, led by the Fuwai Hospital of the Chinese Academy of Medical Sciences, produced by Chongqing Yongren Heart. From January 2018 to January 2021, 17 EVAHEART I implantations were performed, and no patients died during the perioperative period. During the long-term follow-up, two patients received heart transplantation 156 days and 1,035 days postoperatively, respectively, and the other 15 patients survived for 350–1,100 days with the artificial heart.
The second was the CH-VAD clinical trial study, led by the Fuwai Hospital of the Chinese Academy of Medical Sciences, produced by Suzhou Tongxin. From January 2019 to December 2020, 33 CH-VAD implantations were performed at five centers. Three patients died during the perioperative period, and the remaining 30 patients had recovered to NYHA I or II by 1 month postoperatively. During the long-term follow-up, one patient had the device removed 166 days after cardiac function recovery, one patient had the device removed and received heart transplantation 190 days postoperatively, and the other 28 patients survived for 360–1,600 days with the device.
The third was a clinical trial on the safety and effectiveness of "rocket heart" in the treatment of end-stage HF, produced by Hangtian Taixin. A total of 50 cases have been enrolled, and the specific data remain to be published.
According to data from the China heart transplantation registration system, a total of 56 medical institutions in China were qualified to perform heart transplantation as of 2020. From 2015 to 2020, the annual numbers of heart transplant procedures implemented and reported by transplantation centers in China were 279, 368, 446, 490, 679, and 557, respectively. A total of 2,819 procedures were completed and reported in 6 years (excluding Hong Kong, Macao, and Taiwan, China). In 2020, non-ischemic cardiomyopathy was present in 74.4% of heart transplantation recipients in China and 84.9% of pediatric heart transplant recipients. In 2020, the in-hospital survival rate among Chinese heart transplant recipients was 88.5%, and multiple organ failure and transplant HF accounted for more than 60% of the early causes of death. From 2015 to 2020, the 1-year survival rate after heart transplantation in China was 85.3%, and the 3-year survival rate was 80.4%. The 1-year survival and 3-year survival rates after heart transplantation in adults were 85.3% and 80.4%, respectively, and those in children were 91.0% and 84.0%, respectively.
-
4.9.1 Pulmonary Hypertension From May 2007 to October 2010, 551 adult patients with pulmonary hypertension (PH) were enrolled in a national multicenter study, including 487 patients (88.4%) with pulmonary arterial hypertension (PAH) and 64 patients (11.6%) with chronic thromboembolic pulmonary hypertension (CTEPH). The PAH subtypes comprised 273 cases (56.1%) of congenital heart disease-related PAH (PAH-CHD), 64 cases (13.1%) of connective tissue disease-related PAH (PAH-CTD) and 150 cases (30.8%) of idiopathic pulmonary hypertension (IPAH).
According to the data from the Chinese Systemic Lupus Erythematosus (SLE) Treatment and Research group (CSTAR) in 2014, with PH defined as a resting pulmonary artery systolic pressure ≥ 40 mmHg, as measured by echocardiography, the prevalence of PAH was 3.8% (74/1,934) in patients with SLE[99].
Before 2006, no targeted drug for PAH was available in China. The 1-, 3-, and 5-year survival rates of IPAH and familial PAH were 68.0%, 38.9% and 20.8%, respectively. In the era of targeted drugs, the survival status of IPAH has improved significantly, with 1- and 3-year survival rates for IPAH of 92.1% and 75.1%, respectively[100].
4.9.2 Pulmonary Thromboembolism and Deep Venous Thrombosis From 1997 to 2008, 18,206 of the 16,972,182 hospitalized patients in more than 60 tertiary hospitals in China were diagnosed with pulmonary embolism (PE), accounting for 0.11% of hospitalized patients. The PE mortality in China in 1997–2008 decreased significantly, from 25.1% in 1997 to 8.7% in 2008.
In a study on venous thromboembolism (VTE) hospitalization and mortality rates in China, a total of 105,723 patients with VTE were enrolled from 90 hospitals in mainland of China from January 2007 to December 2016; 43,589 (41.2%) of the cases were PE combined with DVT, and 62,134 cases (58.7%) were simple deep venous thrombosis (DVT). The age and sex adjusted hospitalization rate increased from 3.2/100,000 in 2007 to 17.5/100,000 in 2016. The in-hospital mortality rate decreased from 4.7% in 2007 to 2.1% in 2016 (Figure 15), and the hospitalization time decreased from 14 days to 11 days[101].
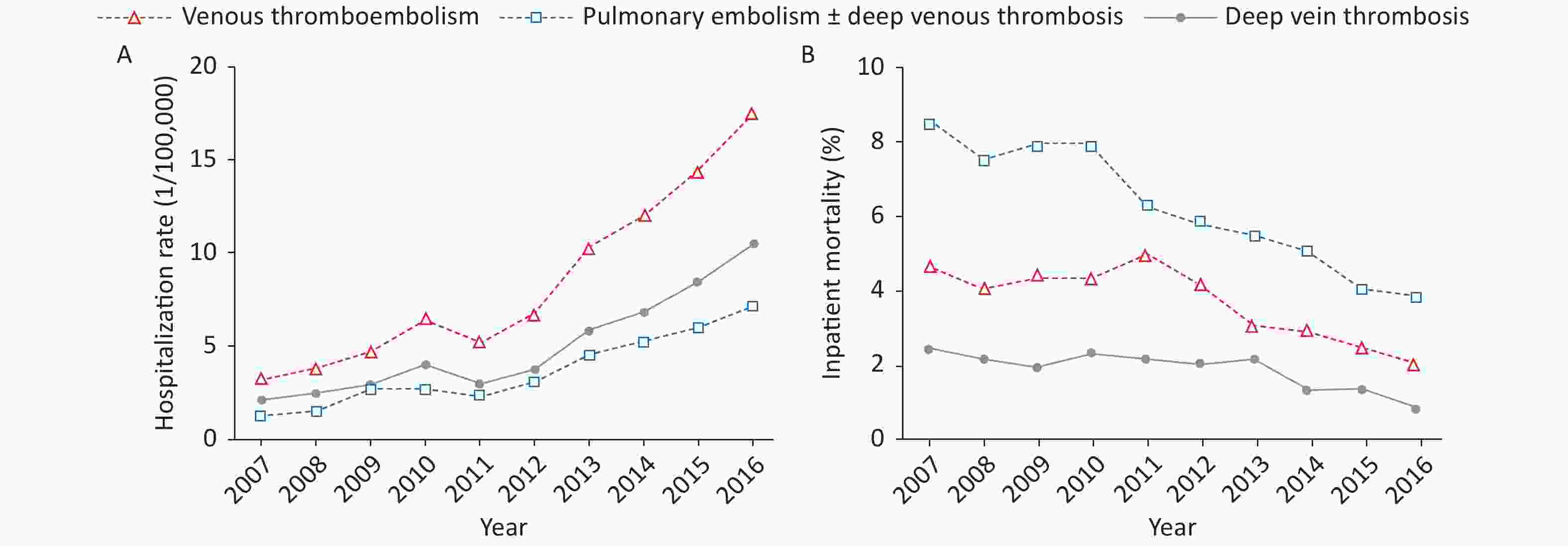
Figure 15. Inpatient rate (A) and inpatient mortality rate (B) for venous thromboembolism in China from 2007 to 2016.
In the China Pulmonary Thromboembolism Registry Study (CURES)[102] from 2009 to 2015, a total of 7,438 adult hospitalized patients with acute symptomatic pulmonary embolism treated at medical institutions in 31 provinces, autonomous regions and municipalities were included. High-risk (hemodynamic instability), moderate-risk [simplified pulmonary embolism severity index (sPESI) ≥ 1] and low-risk (sPESI = 0) patients accounted for 4.2%, 67.1%, and 28.7%, respectively. CT pulmonary angiography was the most commonly used diagnostic method (87.6%), and anticoagulation therapy was the most commonly used initial treatment method (83.7%). The proportion of initial systemic thrombolytic therapy decreased from 14.8% to 5.0%, and the mortality of acute pulmonary embolism decreased from 3.1% to 1.3%.
The Identification of Chinese Hospitalized Patients' Risk Profile for Venous Thromboembolism (Dissolve-2) study[103] enrolled a total of 13,609 patients—6,623 (48.7%) from internal medicine departments and 6,986 (51.3%) from surgical departments—who were hospitalized for more than 72 hours due to medical or surgical emergencies from 60 tertiary hospitals in China from March to September in 2016. According to the 9th version of the CHEST Guidelines, the risk of VTE among medical inpatients was divided into low-risk (63.4%) and high-risk (36.6%) groups, and the risk of VTE among surgical inpatients was divided into low-risk (13.9%), moderate-risk (32.7%) and high-risk (53.4%) groups. The main VTE risk factor for surgical inpatients was open surgery (52.6%), whereas the main VTE risk factor for medical inpatients was acute infection (42.2%). The proportion of all patients receiving the preventive measures recommended in the 9th version of the CHEST Guidelines was 14.3% (19.0% of surgical patients and 9.3% of medical patients), whereas 10.3% (11.8% of surgical patients and 6.0% of medical patients) received appropriate preventive measures.
-
4.10.1 Aortic Disease According to Chinese health insurance data in 2011, the annual incidence of acute aortic dissection in the mainland of China was approximately 2.8/100,000, and was significantly higher in males than in females (3.7/100,000 vs. 1.5/100,000)[104].
The results of a domestic registration study of aortic dissection (Sino-RAD) have indicated that the average age of Chinese patients with aortic dissection is approximately 51.8 years—an age approximately 10 years younger than that in Europe and America. For type A aortic dissection, the open surgery treatment rate was 89.6%, the drug treatment rate was 7.8%, the endovascular treatment rate was 1.6%, the hybrid treatment rate was 1.3%, and the in-hospital mortality rate was 5.5%. For type B aortic dissection, the rate of drug therapy alone was 21.3%, and the mortality rate was 9.8%. The surgical treatment rate was 4.4%, and the mortality rate was 8.0%. The intracavitary treatment rate was 69.6%, and the mortality rate was 2.5%.
Different types of aortic dissection require different surgical methods, and their hospitalization days and hospitalization costs are also different. According to HQMS, in 2020, the averagestay length of thoracic endovascular aneurysm repair (TEVAR) in China was 15.9 days, and the average hospitalization cost was RMB 157,500. The average stay length of simple graft replacement of ascending aorta with aortic valve (Bentall surgery) was approximately 23.4 days, and the average hospitalization cost was RMB 211,600. The average stay length of patients undergoing total aortic arch replacement was approximately 23.2 days, and the average hospitalization cost was RMB 274,100.274,100.
Screening of 5,402 people ≥ 40 years of age with relevant risk factors in three urban and two rural communities in central China has indicated a prevalence of abdominal aortic aneurysm of 0.33% in people 55–75 years of age—a value higher than those in the other age groups (0.51% vs. 0.11%)[105]. A cross-sectional survey conducting abdominal aortic ultrasound screening on a total of 3,560 people > 60 years of age in four cities in Liaoning province has reported a positive detection rate of abdominal aortic aneurysm of 0.9%[106].
A meta-analysis on the growth rate of Chinese abdominal aortic aneurysms [107] showed that the annual growth rate of abdominal aortic aneurysms in the Chinese population is 0.18–0.75 cm. The larger the diameter of the aneurysm, the faster the growth rate was.
According to HQMS, in 2020, the average stay length of abdominal aortic prosthesis replacement surgery in China was 22 days, and the average hospitalization cost was RMB 123,000. The average stay length of endovascular abdominal aortic repair (EVAR) was 14 days, and the average hospitalization cost was RMB 178,400.
4.10.2 Peripheral Arterial Disease
4.10.2.1 Lower Extremity Arterial Disease (LEAD)
A stratified random sampling survey in mainland of China has indicated a prevalence rate of LEAD in the general population ≥ 35 years of age of 6.6%. On the basis of these data, the number of patients with LEAD in China has been inferred to be approximately 45.3 million[108]. Among them, 1.9% of the patients received revascularization. A total of 860,000 patients in China have been estimated to receive revascularization.
4.10.2.2 Carotid Atherosclerotic Disease
In 2018, the results of carotid ultrasonography in 106,918 urban and rural community residents ≥ 40 years of age were collected and analyzed in the Chinese Stroke Prevention Program (CSPP). The data show that the prevalence rate of moderate and above carotid stenosis was 0.5% [109].
According to the China Stroke Prevention and Control Report in 2019, the number of reported cases of carotid endarterectomy (CEA) in 2018 was 4,910, and the rate of serious complications of the operation was 2.79%. In 2018, a total of 15,801 carotid artery stenting procedures were performed, and the incidence of serious complications was 1.92%[110].
4.10.2.3 Renal Artery Stenosis
A single center study[111] involving 2,905 patients with renal artery stenosis (RAS) for 18 years has found that the main causes of RAS in Chinese population are atherosclerosis (82.4%), Takayasu arteritis (11.9%), fibromuscular dysplasia (4.3%) and other causes (1.4%). AS increased from 50% in 1999–2000 to 85% in 2015–2016. Non-AS causes were more common in patients below less than 40 years old.
4.10.2.4 Subclavian Artery Stenosis
An inter-arm systolic blood pressure difference ≥ 15 mmHg is a powerful index for predicting subclavian artery stenosis > 50%, and can be used for epidemiological screening and diagnosis of subclavian artery stenosis. A study of 3,133 elderly people with an average age of 69 years in a community in Shanghai has indicated that 1.7% of the population had an inter-arm systolic pressure difference ≥ 15 mmHg. A single center study has investigated the etiological composition of subclavian artery stenosis in hospitalized patients and found that AS accounted for 95.9% in patients above 40 years of age, whereas the main cause in patients younger than 40 years of age was Takayasu arteritis (90.5%)[112].
-
A large cohort study of 710,000 cancer patients has reported that 18% of patients had CVD risk factors or CVD: 13% of patients with cancer had at least one CVD risk factor, and 5% had one type of CVD. After adjustment for age, sex, tumor stage and treatment received, patients with HF had the poorest prognosis, with a 79% increase in all-cause mortality, followed by myocardial infarction, with a 50% increase in all-cause mortality[113].
-
In 2016, a survey on the current situation of cardiac rehabilitation work in hospitals across the country[114] included 124 tertiary hospitals in seven regions of mainland of China. Only 30 (24%) hospitals provided cardiac rehabilitation services, and only 2.2 hospitals in an average population of 100 million were able to perform cardiac rehabilitation. Among the 13 hospitals that completed 36 surveys and performed cardiac rehabilitation, 3 (23%) performed in-hospital phase I rehabilitation, 3 (23%) performed phase II rehabilitation, and 7 (54%) performed phase I and phase II rehabilitation simultaneously.
-
In 2016, compared with previous years, the number of rehabilitation hospitals and rehabilitation beds in China increased significantly[115]. A sampling survey of the national medical quality management and control information system in 2018 included data from 7,544 hospitals in 32 provinces, autonomous regions and municipalities, including Xinjiang Production and Construction Corps. A total of 2,147 hospitals were equipped with rehabilitation medical wards, with a ward allocation rate of 28.46%; the average number of beds in the 1,897 rehabilitation wards included in the statistics was 41.17. In 2018, the average number of person-times discharged from the rehabilitation medicine departments of general hospitals nationwide was 753.25, including 241.56 person-times with stroke. The implementation rate of early rehabilitation (within 24–48 hours of hospitalization) in neurology wards was 11.79%, and the rate of implementation of early rehabilitation for acute ischemic stroke was 25.25% [116].
A survey in 2009 indicated there were 16,000 rehabilitation doctors, 14,000 therapists and 12,000 nurses in China. In 2018, the numbers of rehabilitation doctors and nurses increased to 38,000 and 15,000, respectively. Approximately 70% of rehabilitation therapists graduated from rehabilitation training programs, and approximately 15% graduated from traditional Chinese medicine training programs[115-116].
In 2018, the average hospitalization cost for patients in rehabilitation medicine departments was RMB 11,222, and the drug cost was RMB 2,286, accounting for 20.37% of the cost. The cost of rehabilitation treatment was RMB 5,567, accounting for 49.61% of the cost[116]. The rehabilitation medicine department of the Third Hospital of Peking University analyzed 1,552,248 samples from 462 tertiary hospitals equipped with rehabilitation medicine wards. The average stay length in the rehabilitation medicine department from 2013 to 2018 was 21.53 days, and the average daily hospitalization cost was RMB 810. The proportion of rehabilitation related costs (rehabilitation costs and physical therapy costs) increased each year. The proportion of discharge fees comprising drug costs, including Western medicine fees, Chinese patent drug fees, and Chinese herbal medicine fees, has decreased each year[117].
-
High-level cardiovascular disease basic research in China started in 2005, with influential papers published in two major journals, Circulation and Circulation Research. From the data of Cell, Nat Med, Circulation, J Am Coll Cardiol, Eur Heart J, Circ Res and Nat Commun, we can observe the rapid development of high-level basic research on CVD in China in recent years (Figure 16).
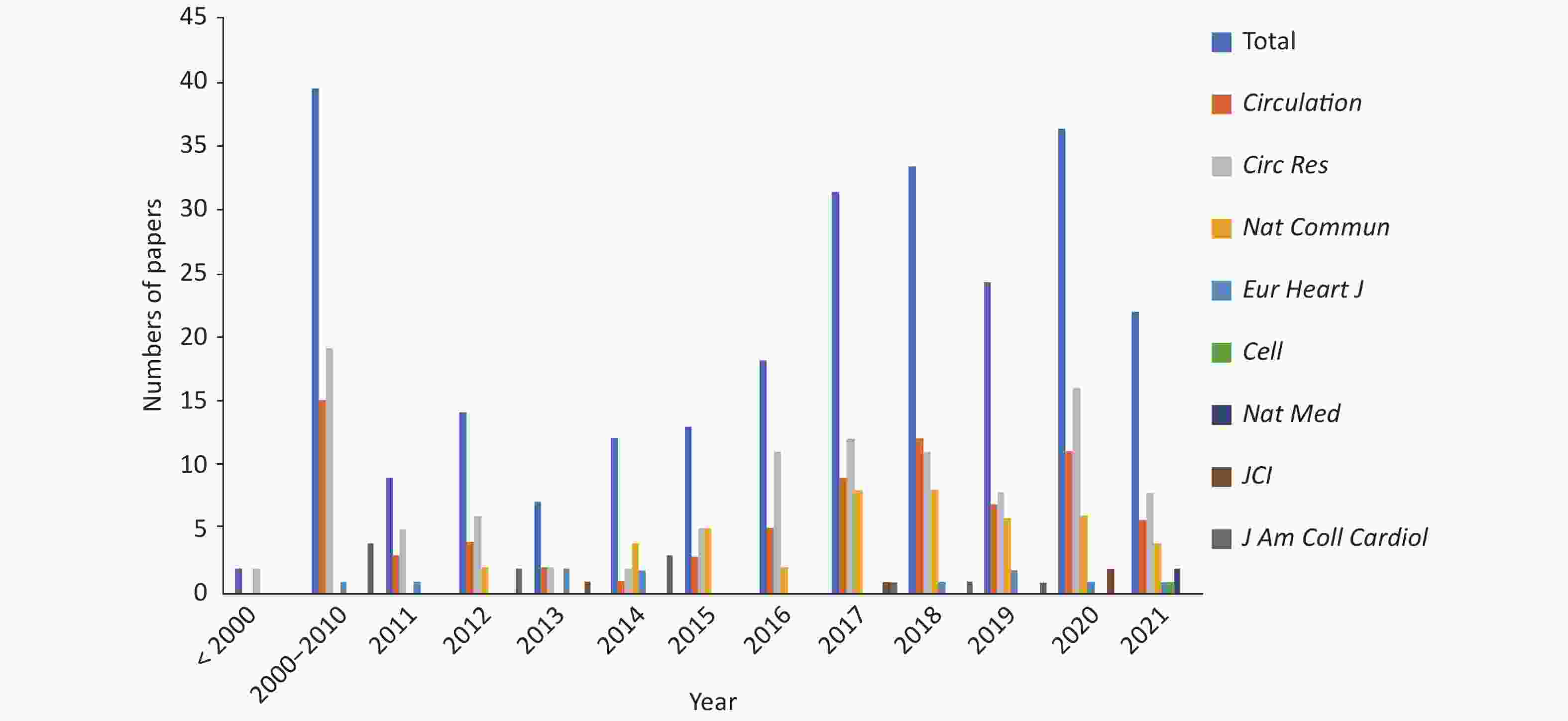
Figure 16. Basic research paperarticles on cardiovascular diseases published by the first author/ corresponding author in China from 2000 to 2021
From 2020 to 2021, 48 basic research articles with first authors and corresponding authors from Chinese institutions were published on heart and vascular anatomy, development and functional pathogenesis, involving IHD, cardiomyopathy, myocarditis, HF, arrhythmia, atherosclerosis, and growth and development. The main research topics included heart protection and regeneration, single cell sequencing technology, gene therapy and device learning.
-
From September 1st, 2020 to August 31th, 2021, the National Medical Products Administration approved entry of a total of 68 medical devices into the evaluation channel for innovative medical devices. Among them, 31 were cardiovascular products, accounting for 45.6%, thus indicating that cardiovascular technology is the dominant medical device innovation type in China. In addition, 58 domestic original products, accounting for 85.3%, were included. In the same period, the National Medical Products Administration approved entry of 15 medical devices into the priority medical device evaluation channel, two of which were cardiovascular products.
From September 1st, 2020 to August 31th, 2021, the National Medical Products Administration approved 142 class III medical device registration certificates in the cardiovascular field. Among them, 101 were domestic products, and 11 products have entered the evaluation channel for innovative medical devices. As compared with the data from September 1st, 2019 to August 31st, 2020 (including 141 approved registration certificates and 96 approved domestic products, 5 of which entered the evaluation channel for innovative medical devices), the speed of approval of cardiovascular devices by the National Medical Products Administration has continued to accelerate, and the proportion of approved innovative medical devices has significantly increased. Simultaneously, the current industrialization development in the field of cardiovascular medical devices in China has entered a rapid stage of progress. The 101 domestic products comprise 90 interventional products, 4 imaging products, 3 blood flow measurement systems, 2 open surgery products, 1 active surgery product and 1 artificial intelligence software.
-
In 2019, the total number of discharged patients with cardiovascular and cerebrovascular diseases in Chinese hospitals was 26.8441 million (Figure 17), accounting for 14.03% of the total number of discharges in the same period (including all diseases associated with hospitalization). Among them there were 14.3488 million with CVD, accounting for 7.50%, and 12.4953 million with cerebrovascular disease, accounting for 6.53%.
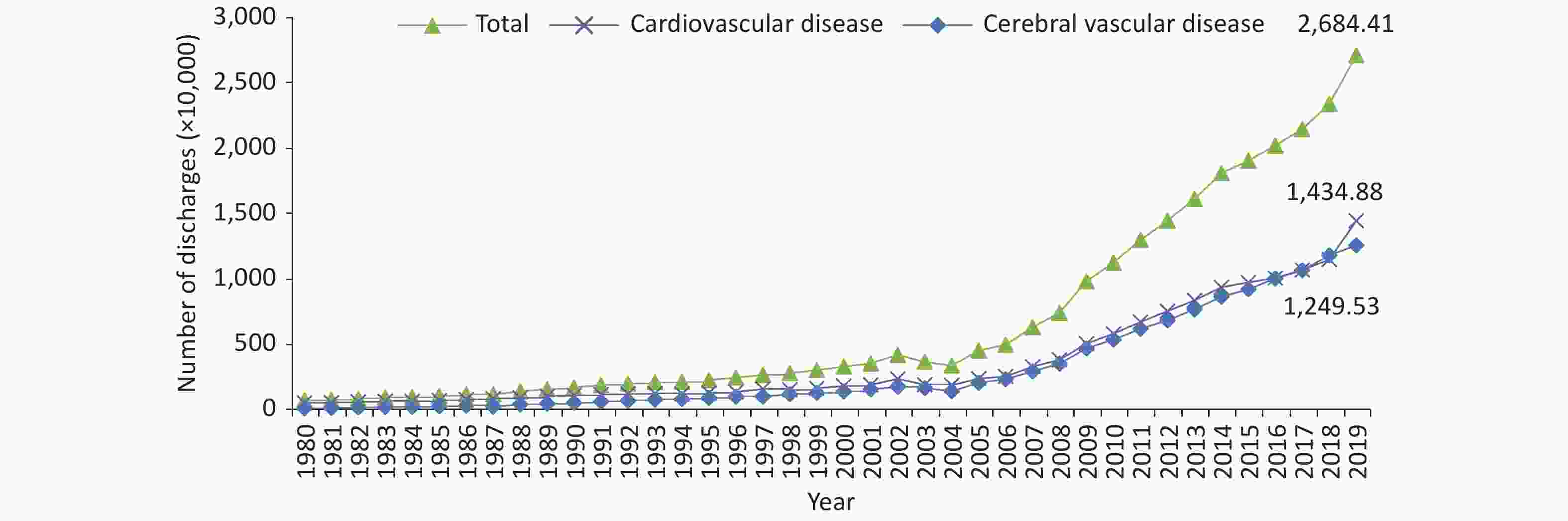
Figure 17. Trends in the number of Chinese patients discharged with cardiovascular diseases from 1980 to 2019. Cardiovascular diseases include ischemic heart disease (angina pectoris, acute myocardial infarction and other ischemic heart diseases), chronic rheumatic heart disease, acute rheumatic fever, pulmonary embolism, arrhythmia, heart failure and hypertension (including hypertensive heart disease and hypertensive kidney disease). Before 2002, ischemic heart disease in the annual report of health statistics was recorded as CHD.
Among all the discharged patients with CVD, IHD (8.9348 million) and cerebral infarction (8.2760 million) were the main diseases, accounting for 36.92% and 34.20%, respectively. In 2019, the number of discharged patients with diabetes was 4.6127 million (Figure 18).
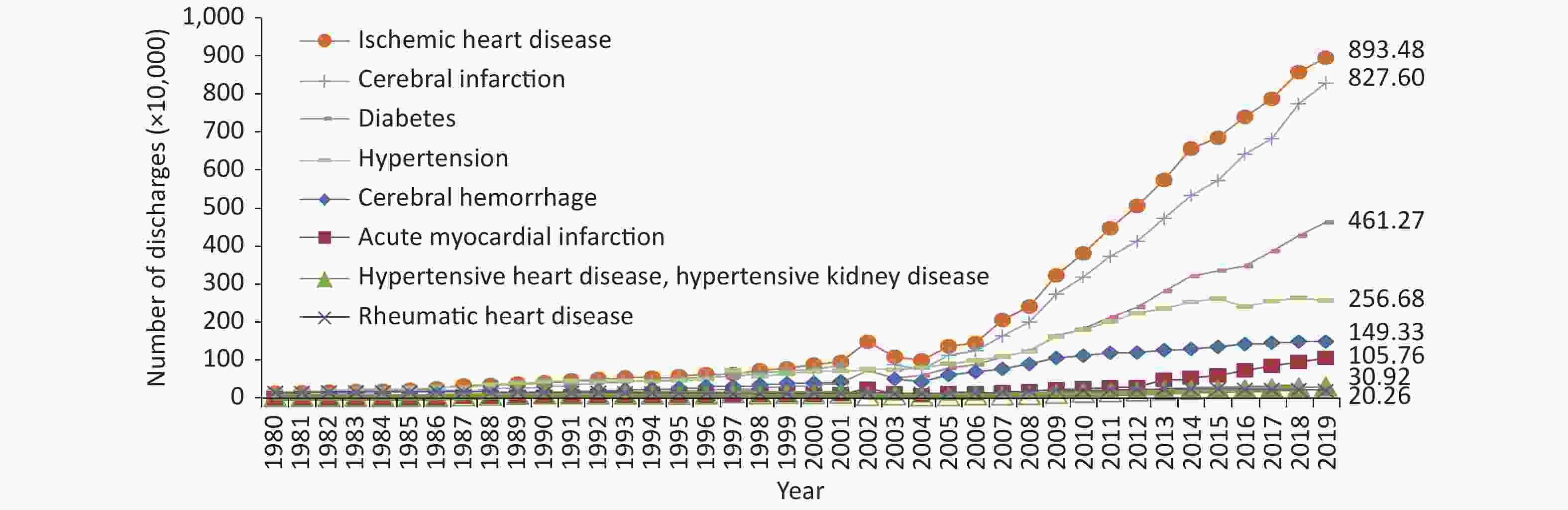
Figure 18. Trends in the number of discharged patients with major cardiovascular diseases and diabetes in China from 1980 to 2019.
From 1980 to 2019, the average annual growth rate of the number of discharged patients with CVD in China was 9.59%, a rate faster than the average annual growth rate of the number of discharged patients with all diseases in the same period (6.33%). The average annual growth rate of discharges for various CVD diseases ranked as follows: HF (20.66%) > angina pectoris (13.02%) > cerebral infarction (11.91%) > pulmonary embolism (11.45%) > IHD (11.04%) > AMI (10.94%) > cerebral hemorrhage (8.84%) > hypertension (7.04%) > arrhythmia (6.15%) > hypertensive heart disease and hypertensive kidney disease (5.95%) > chronic rheumatic heart disease (0.70%) > acute rheumatic fever (−11.98%). The average annual growth rate of diabetes discharge was 13.31%.
-
In 2019, the total cost of hospitalization for cardiovascular and cerebrovascular diseases in China was RMB 313.366 billion. The total hospitalization cost for CVD was RMB 177.338 billion, including RMB 125.625 billion for IHD (including RMB 42.784 billion for angina pectoris and RMB 32.118 billion for AMI), RMB 18.099 billion for arrhythmia, RMB 16.721 billion for hypertension (including RMB 2.761 billion for hypertensive heart disease and hypertensive kidney disease), RMB 13.064 billion for HF, RMB 1.930 billion for rheumatic heart disease, RMB 1.809 billion for pulmonary embolism and RMB 90 million for acute rheumatic fever. The total hospitalization cost for cerebrovascular disease was RMB 136.028 billion, including RMB 81.197 billion for cerebral infarction and RMB 29.633 billion for cerebral hemorrhage (Figure 19). In addition, the total cost of hospitalization for diabetes was RMB 36.592 billion.
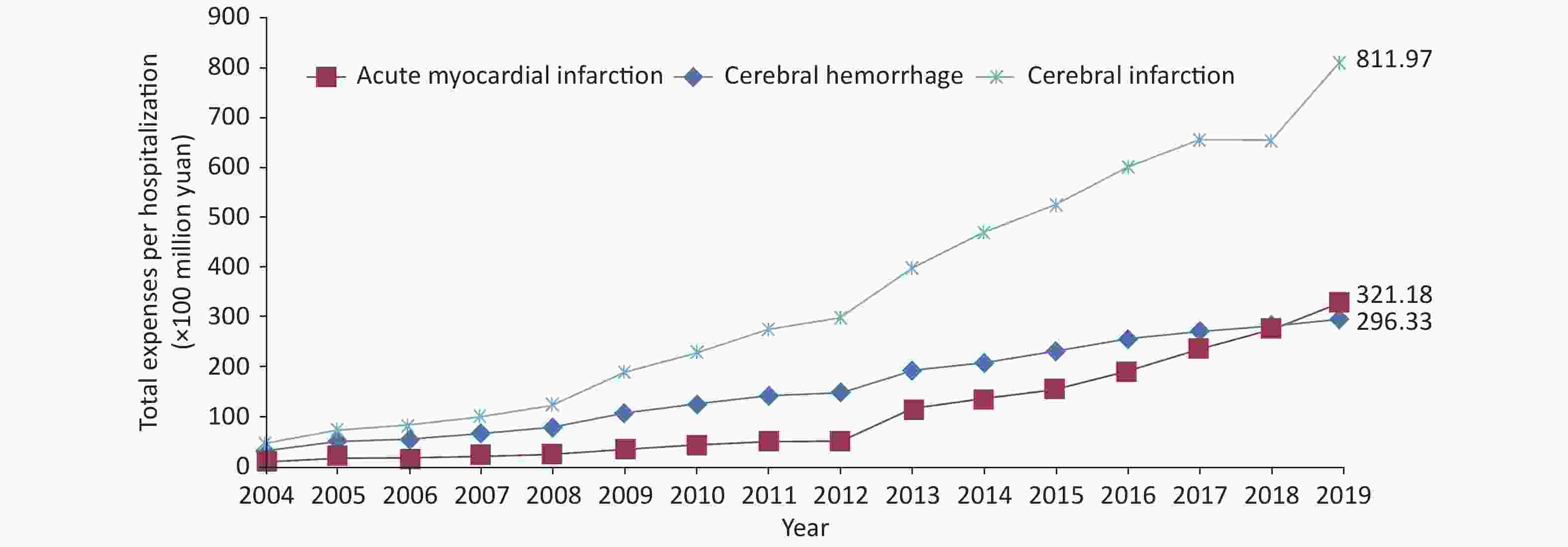
Figure 19. Trends in total expenses per hospitalization for three cardiovascular diseases from 2004 to 2019 (current year price).
After correction for the influence of price factors, since 2004, the average annual growth rate of total hospitalization expenses for AMI, cerebral infarction and cerebral hemorrhage has been 25.99%, 18.82%, and 13.51%, respectively (Figure 20). Compared with that in 2018, the total hospitalization cost in 2019 changed by 9.55% for IHD (angina pectoris 14.41%), −2.03% for hypertension (hypertensive heart disease or hypertensive kidney disease 7.91%), 11.53% for pulmonary embolism, 15.59% for arrhythmia, 24.04% for HF, −10.18% for chronic rheumatic heart disease and −9.46% for acute rheumatic fever. In addition, that for diabetes increased by 7.72%.
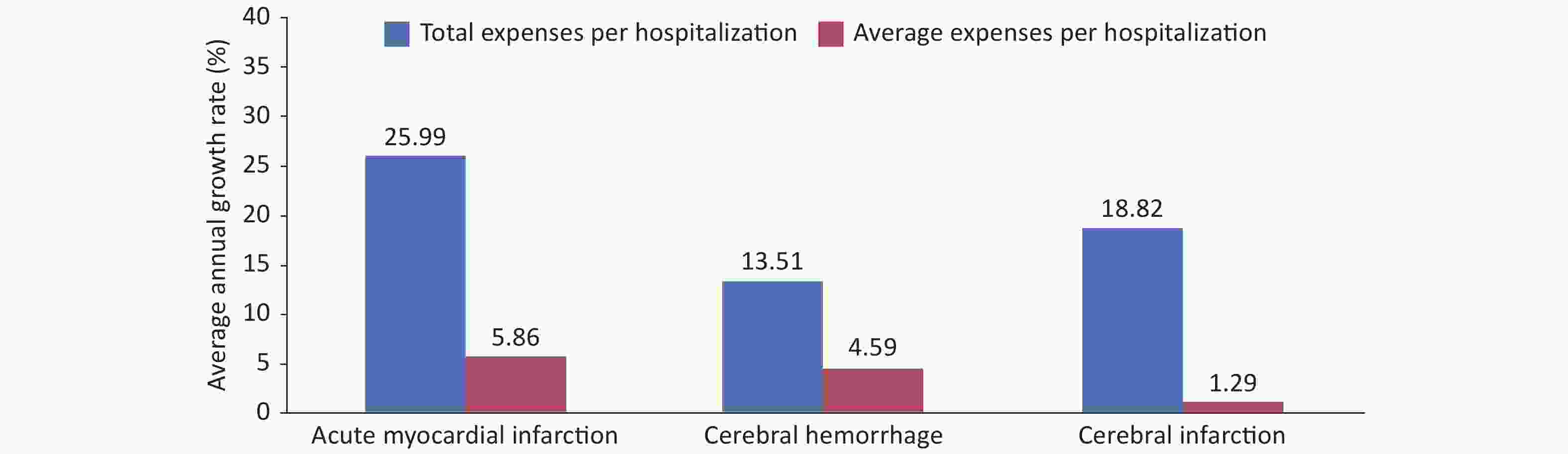
Figure 20. Average annual growth rate of total and average expenses per hospitalization for three cardiovascular diseases from 2004 to 2019
The average expenses per hospitalization for IHD was RMB 14,060.20 (RMB 15,486.51 for angina pectoris and RMB 30,368.54 for AMI), RMB 9,811.18 for cerebral infarction, RMB 19,843.37 for cerebral hemorrhage (Figure 21), RMB 6,514.19 for hypertension (RMB 8,929.68 for hypertensive heart disease and hypertensive kidney disease), RMB 17,169.01 for pulmonary embolism, RMB 16,028.28 for arrhythmia, RMB 9,368.51 for HF, RMB 9,525.63 for chronic rheumatic heart disease and RMB 5,780.11 for acute rheumatic fever. In addition, the expense for diabetes was RMB 7,932.88.
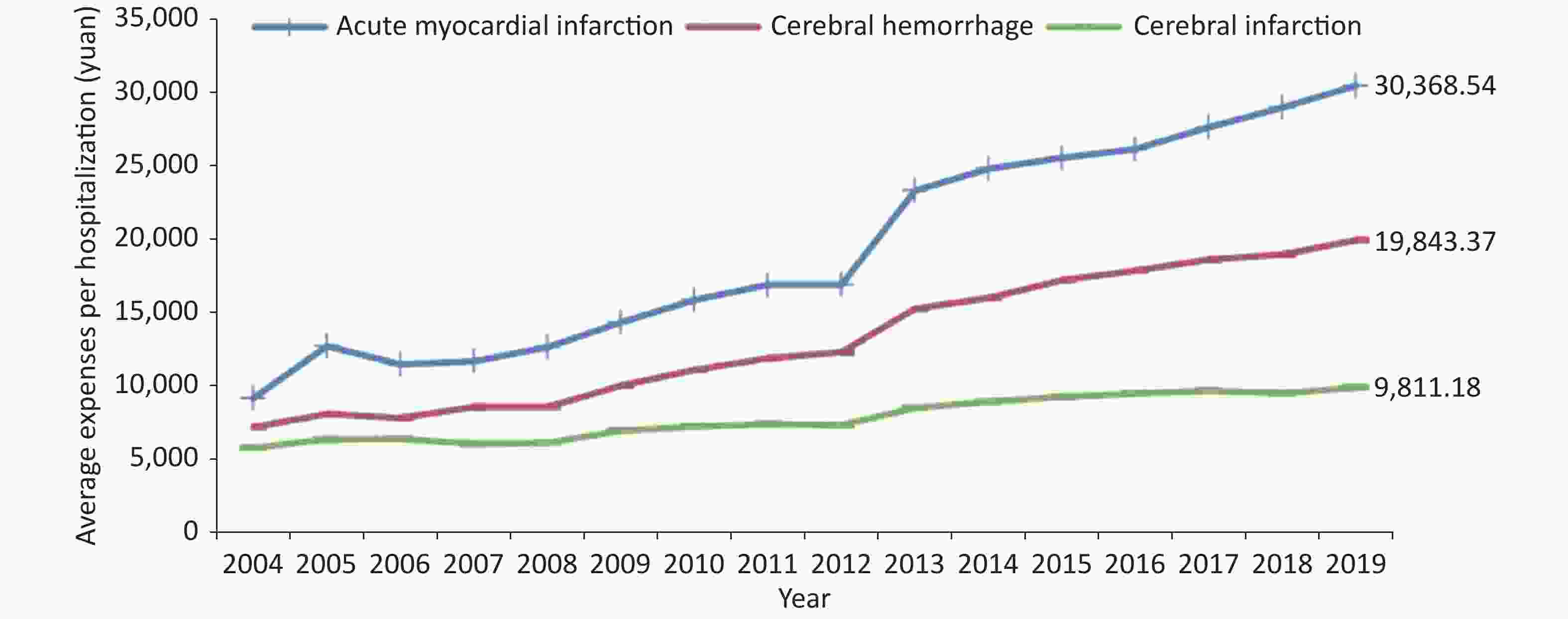
Figure 21. Trends in average expenses per hospitalization for three cardiovascular diseases from 2004 to 2019 (current year price).
After correction for the influence of price factors, since 2004, the average annual growth rate of average expenses per hospitalization for AMI, cerebral infarction and cerebral hemorrhage has been 5.86%, 1.29%, and 4.59%, respectively. Compared with those in 2018, the average expenses per hospitalization in 2019 for IHD increased by 4.94% (angina pectoris 1.23%), those for hypertension increased by 0.62% (hypertensive heart disease, hypertensive kidney disease 1.62%), those for pulmonary embolism increased by 0.07%, those for arrhythmia increased by 8.89%, those for HF increased by 2.80%, those for chronic rheumatic heart disease increased by 1.53%, and those for acute rheumatic fever increased by 2.87%. In addition, those for diabetes increased by –0.35%.
Acknowledgements We thank all experts who participated in the preparation of the Annual Report on Cardiovascular Health and Diseases in China 2021. A list of members of the preparation team is provided in the references[118].
Conflicts of Interest All authors declare that there are no conflicts of interest.
Report on Cardiovascular Health and Diseases in China 2021: An Updated Summary
doi: 10.3967/bes2022.079
- Received Date: 2022-06-28
- Accepted Date: 2022-07-13
-
Key words:
- Cardiovascular disease /
- Epidemiology /
- Health influencing factors /
- Risk factors /
- Prevalence /
- Mortality /
- Community-based prevention and control /
- Rehabilitation /
- Basic research /
- Medical device development
Abstract: In 2019, cardiovascular disease (CVD) accounted for 46.74% and 44.26% of all deaths in rural and urban areas, respectively. Two out of every five deaths were due to CVD. It is estimated that about 330 million patients suffer from CVD in China. The number of patients suffering from stroke, coronary heart disease, heart failure, pulmonary heart disease, atrial fibrillation, rheumatic heart disease, congenital heart disease, lower extremity artery disease and hypertension are 13.00 million, 11.39 million, 8.90 million, 5.00 million, 4.87 million, 2.50 million, 2.00 million, 45.30 million, and 245.00 million, respectively. Given that China is challenged by the dual pressures of population aging and steady rise in the prevalence of metabolic risk factors, the burden caused by CVD will continue to increase, which has set new requirements for CVD prevention and treatment and the allocation of medical resources in China. It is important to reduce the prevalence through primary prevention, increase the allocation of medical resources for CVD emergency and critical care, and provide rehabilitation services and secondary prevention to reduce the risk of recurrence, re-hospitalization and disability in CVD survivors. The number of people suffering from hypertension, dyslipidemia and diabetes in China has reached hundreds of millions. Since blood pressure, blood lipids, and blood glucose levels rise mostly insidiously, vascular disease or even serious events such as myocardial infarction and stroke often already occured at the time of detection in this population. Hence, more strategies and tasks should be taken to prevent risk factors such as hypertension, dyslipidemia, diabetes, obesity, and smoking, and more efforts should be made in the assessment of cardiovascular health status and the prevention, treatment, and research of early pathological changes.
| Citation: | The Writing Committee of the Report on Cardiovascular Health and Diseases in China. Report on Cardiovascular Health and Diseases in China 2021: An Updated Summary[J]. Biomedical and Environmental Sciences, 2022, 35(7): 573-603. doi: 10.3967/bes2022.079 |




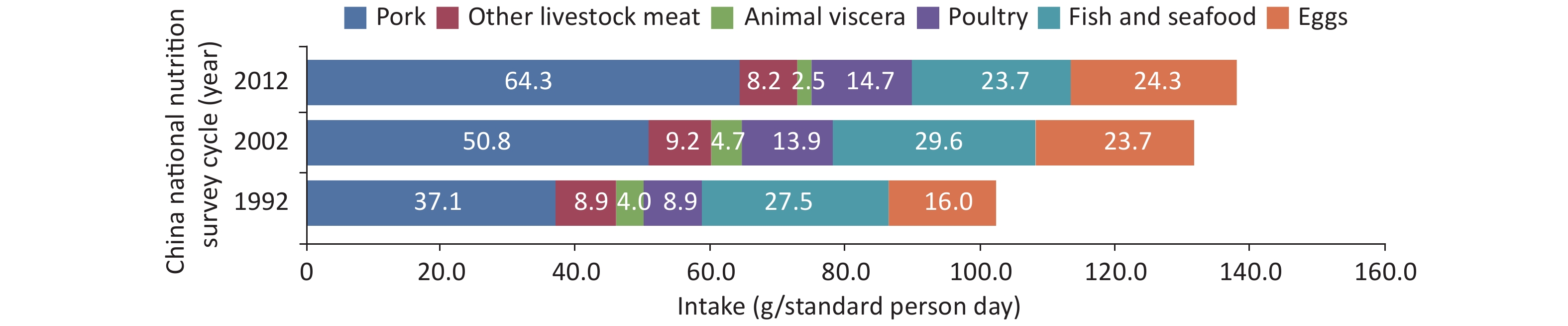

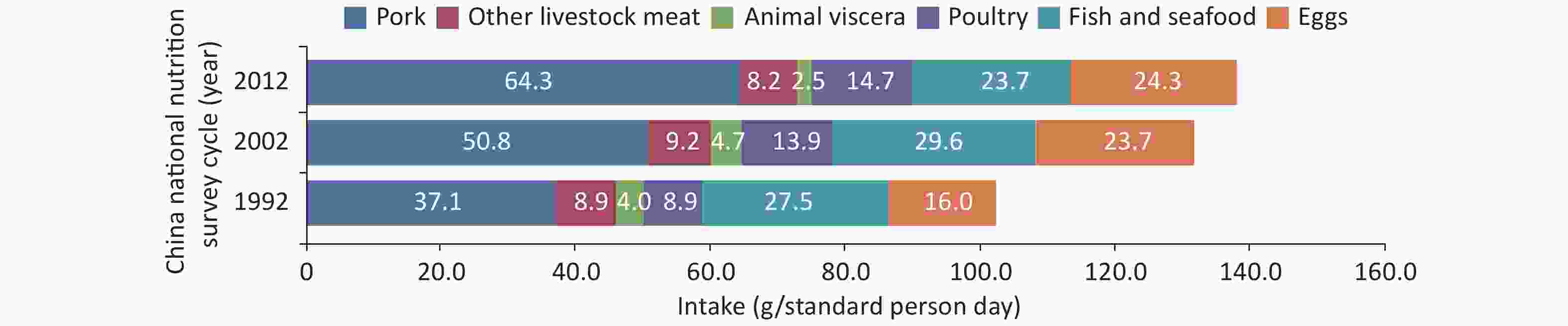
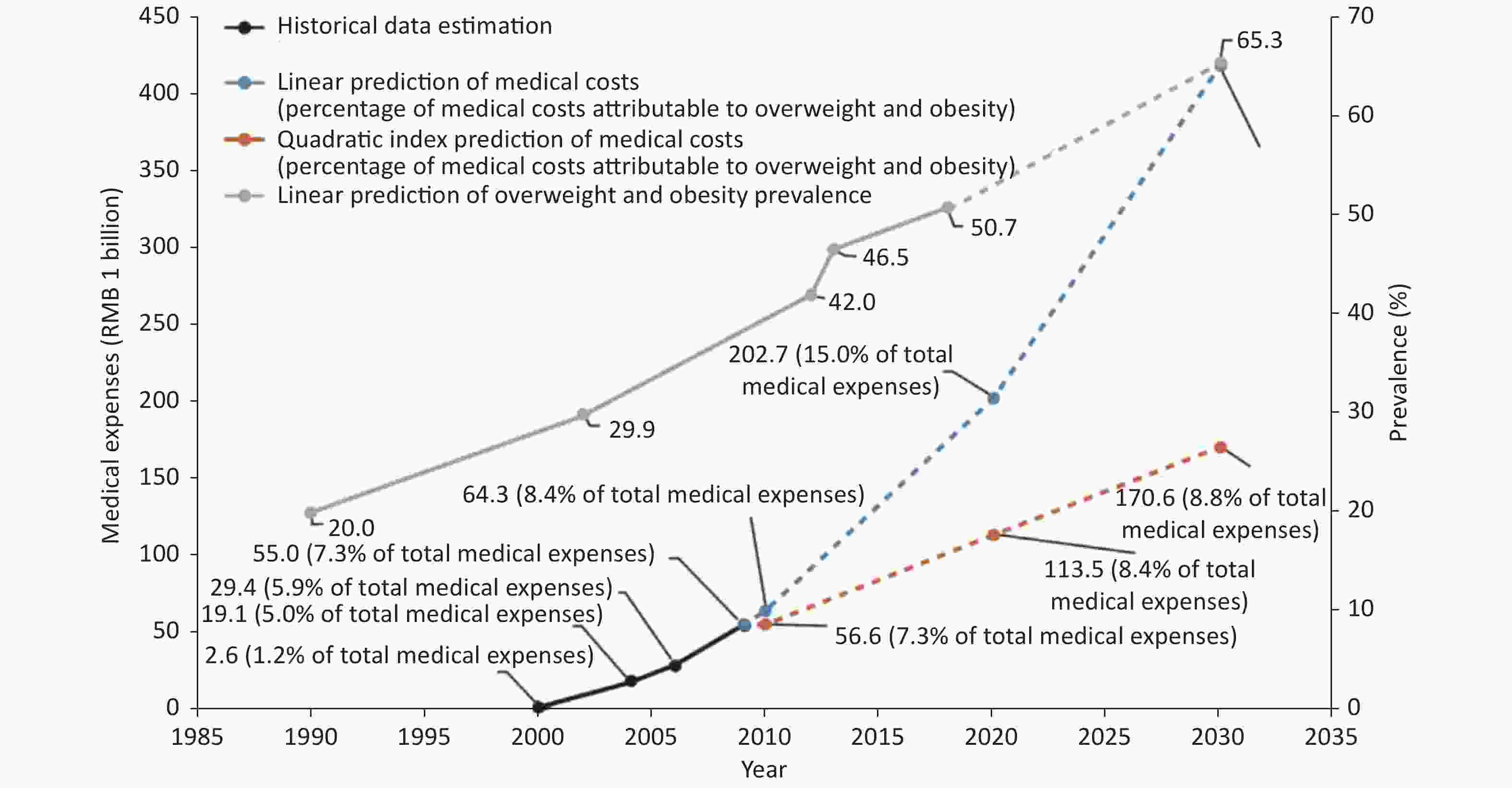
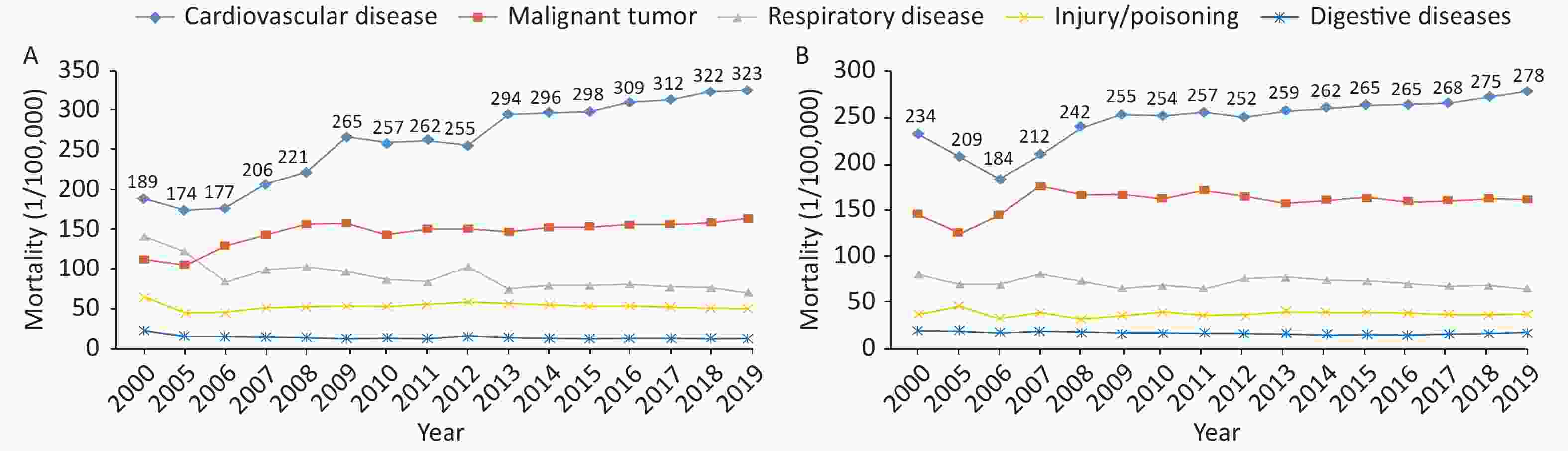
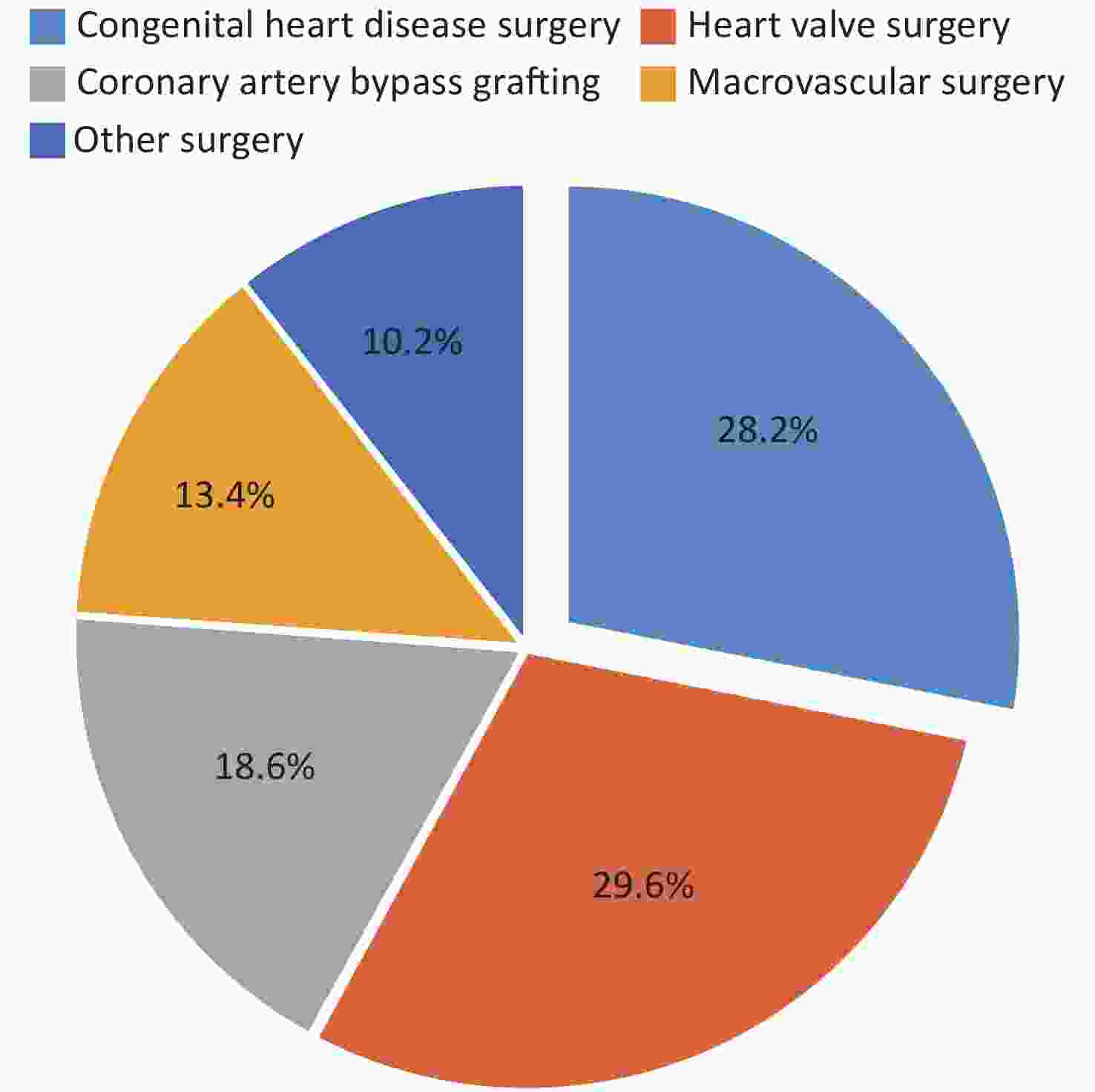

 Quick Links
Quick Links
 DownLoad:
DownLoad: