-
Hepatitis C infection is a serious public health threat. The World Health Organization (WHO) estimated that in 2019, approximately 58 million people were living with hepatitis C virus infection and 290,000 people died from hepatitis C worldwise[1]. Approximately 7.6 million people have been infected by hepatitis C virus in China, and 4.56 million people are currently living with chronic HCV infection[2].
In 2016, WHO approved the goal and the framework of strategy to eliminate hepatitis infections, aiming to diagnose 90% of hepatitis C patients and reduce the number of new infections by 80%[3]. In 2021, China launched the National Action Plan (2021–2030) to realize HCV-free by 2030[4]. It is especially important to analyze associated factors to achieve introduced goals and better estimate HCV prevalence in different populations.
Many countries made efforts to detect hepatitis C patients through screening. Japan started a five-year national program to test for HBV and HCV infections among people aged 40 and above in 2002[5]. The US Centers for Disease Control and Prevention provided a one-time screening for “baby boomers”, to people who were born between 1945 and 1965[6]. Offering HCV screening to emergency department (ED) attendees could effectively identify patients and limiting onward transmission[7-10]. A research project was conducted in different regions in China and proved that an age-targeted screening strategy for inpatients aged 40 and above would help to find the missing millions of the unaware patients[11]. Most previous research mainly focused on HCV prevalence and associated factors among ED patients, along with small samples[12-13]. Limited information was found regarding the prevalence of HCV antibody among a large sample of patients as well as data from diverse hospitals in China.
In China, hospitals are recommended to provide HCV antibody testing for auxiliary diagnosis, before surgery, blood transfusion, endoscopy, invasive operation, etc.[4]. Although the patients who received HCV antibody testing in hospitals could not represent the general population, the surveillance data based on those populations could provide useful information to estimate the HCV epidemic. Thus, we analyzed the HCV antibody test data from 77 HCV sentinel hospitals in China. The results could provide references for HCV epidemic estimates and developing screening strategies.
-
The research team slected sentinel hospitals nationally from counties (districts) in the pilot provinces. Sentinel hospitals collected outpatient and inpatient information on epidemiological data, laboratory tests and outcomes of clinical treatment actively and continuously. This study was conducted between January 2017 and December 2019. Seventy-seven hospitals were selected from 30 cities in 12 regions (Jilin, Liaoning, Gansu, Henan, Hubei, Zhejiang, Hunan, Sichuan, Guangdong, Tianjin, Guangxi, Yunnan), which covered the Eastern coastal area, the Northeast, the Central, and the West China. The Eastern coastal area includes Tianjin, Zhejiang, and Guangdong. The Northeast contains Jilin, and Liaoning. The Central involves Henan, Hubei, and Hunan. The West indicates Sichuan, Guangxi, Gansu, and Yunnan.
The selection of study sites, hospitals, and departments included four criteria, 1) 2–4 counties (districts) were selected from each area, including ten provinces, one municipality, and one autonomous region; 2) cases reported by the local CDCs ranked among the top 10 in the province last year or the number of cases reported should not be less than 50; 3) hospitals were capable of hepatitis C diagnosis, treatment, and infectious disease reporting; 4) all departments, which issued HCV antibody test sheets, were included in sentinel hospitals, such as Department of Surgery, Internal Medicine, Department of Obstetrics and Gynecology, liver disease-related departments, Department of Pediatrics, invasive diagnosis and treatment-related departments, etc.
-
The study team collected data on HCV antibody testing from outpatient and inpatient in 77 sentinel hospitals. Sentinel hospitals perform HCV antibody testing among patients with two main methods. First, patients received HCV antibody testing for obvious liver symptom in Liver disease-related departments. HCV antibody detection is a mandatory item before hospitalization and invasive operation in non-Liver disease-related departments. Second, the Department of Surgery and the invasive diagnosis and treatment-related departments conduct blood-borne virus screening for patients (particularly those who will undergo invasive examination, surgery and transfusion) to prevent iatrogenic infections.
Data on demographic characteristics and diagnosis-related information were collected from electronic case records. HCV antibody test results were obtained from the database of the laboratory information system. The variables included specimen number, gender, age, departments of specimen delivery, reasons for testing, HCV antibody results, date of testing, etc. For those who had only multiple negative HCV antibody tests throughout the time, the study team only collected their first test results. For those who had positive HCV antibody test, only the first positive result were selected. The proposal was approved by the Institutional Review Board of the Chinese Center for Disease Control and Prevention (Beijing, China; No. X170308449).
-
HCV antibody examinations were performed at the Department of Clinical Laboratory of 77 sentinel hospitals. Also, 36 hospitals used enzyme immunoassays, 20 utilized chemiluminescence assays, and four employed colloidal gold immunochromatographic assays to test for HCV antibodies. Besides, 17 hospitals used any two of these three methods. Each sentinel hospital selected different reagents according to different detection methods. All the reagents were approved by the State Food and Drug Administration of China, and assays were performed based on the manufacturers’ instructions.
-
All categorical variables were summarized as frequencies and percentages. The research group applied the univariate logistic regression analysis to identify the potential factors. The candidate variables were included in the multivariable logistic regressions based on the univariate logistic regressions and literature reviews. The candidate variables included gender, age group, hospital level, hospital type, regional distribution, and departments of specimen delivery. The final results were presented as crude and adjusted odds ratios (cOR, aOR), along with their corresponding 95% confidence intervals (CIs) and P-values. All P-values were based on two-tailed tests, and P < 0.05 was considered to be statistically significant. Data analysis was performed in SPSS (version 24.0, SPSS Inc, Chicago, IL, USA).
-
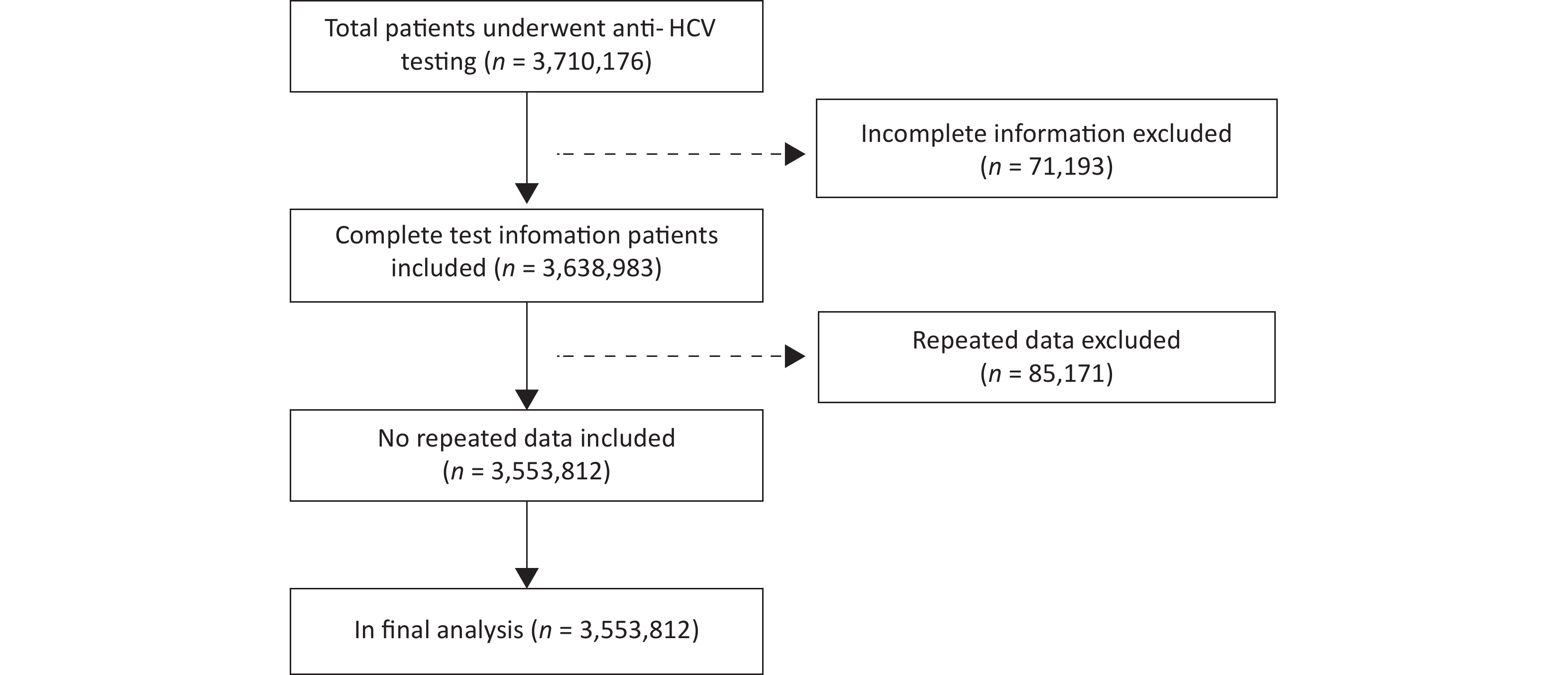
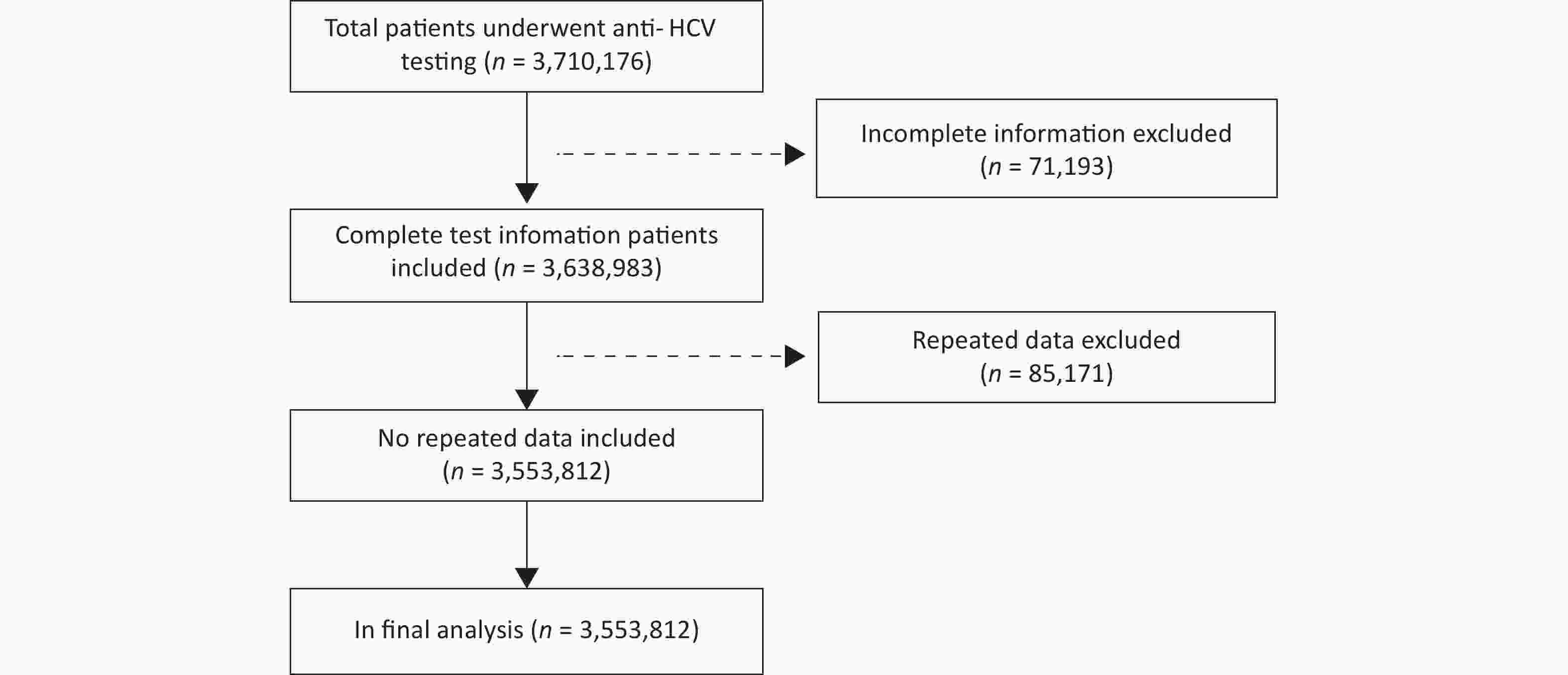
A total of 3,710,176 subjects in 77 sentinel hospitals were collected in this study. The study group excluded 156,364 subjects from the final analysis because of incomplete questionnaire information and repeated data. The study profile was described in Figure 1.
Nearly half of the 3,553,812 subjects who underwent the HCV antibody testing (49.16%) were over 45 years old. More than half of the subjects were female (55.61%); 92.51% of subjects were from the Eastern coastal area, the Central, and the West China; 95.91% of subjects were found in non-communicable disease hospitals; and 72.38% of subjects were in tertiary hospitals. Most subject data (74.21%) were from the Internal Medicine, Department of Surgery, and Department of Obstetrics and Gynecology (Table 1).
Characteristics Total n % Gender Female 1,976,181 55.61 Male 1,577,631 44.39 Age group (years) 0−45 1,806,827 50.84 > 45 1,746,985 49.16 Hospital level Secondary hospitals 981,664 27.62 Tertiary hospitals 2,572,148 72.38 Hospital type Non-communicable disease hospitals 3,408,345 95.91 Infectious disease hospitals 145,467 4.09 Regional distribution* Eastern coastal area 1,062,118 29.89 Northeast 266,301 7.49 Central 1,078,436 30.35 West 1,146,957 32.27 Departments of specimen delivery Department of Surgery 985,727 27.74 Internal Medicine 870,159 24.49 Department of Obstetrics and Gynecology 781,175 21.98 Liver disease-related departments 216,207 6.08 Department of Pediatrics 110,311 3.10 Invasive diagnosis and treatment-related departments 32,937 0.93 Other departments 557,296 15.68 Note. *Eastern coastal area: Tianjin, Zhejiang, Guangdong; Northeast: Jilin, Liaoning; Central: Henan, Hubei, Hunan; West: Sichuan, Guangxi, Gansu, Yunnan. Table 1. HCV antibody characteristics of patients in 77 hospitals (N = 3,553,812)
-
HCV antibody prevalence rates among patients were distinct in different non-viral hepatitis departments. The highest rates of HCV antibody among the patients were found in Internal Medicine (3.77%), invasive diagnosis and treatment-related departments (2.25%), and the Department of Surgery (1.52%). Except in invasive diagnosis and treatment-related departments, the rate of HCV antibody in non-communicable disease hospitals was higher than the prevalence in infectious disease hospitals. The HCV antibody prevalence in Internal Medicine, invasive diagnosis and treatment-related departments, and the Department of Surgery was higher in males, aged 45 or above, secondary hospitals, and infectious disease hospitals compared with females, under 45 years old, tertiary hospitals, and non-communicable disease hospitals, respectively. Except in invasive diagnosis and treatment-related departments, the prevalence rates of HCV antibody in the Central and the West China were lower than the prevalence in the Eastern coastal area. The rates in Internal Medicine, invasive diagnosis and treatment-related departments and Department of Surgery were higher in the Northeast, the Central, and the West China, comparing with the Eastern coastal area, respectively (Table 2).
Characteristics Internal Medicine Department of Surgery Invasive diagnosis and
treatment-related
departmentsTotal (n) Positive (n) % Total (n) Positive (n) % Total (n) Positive (n) % Gender Female 400,992 13,637 3.40 409,006 5,713 1.40 17,257 328 1.90 Male 469,167 19,132 4.08 576,721 9,297 1.61 15,680 412 2.63 Age group (years) 0−45 203,019 3,014 1.48 390,910 2,639 0.68 12,419 99 0.80 > 45 667,140 29,755 4.46 594,817 12,371 2.08 20,519 641 3.12 Hospital level Tertiary hospitals 592,090 11,347 1.91 740,642 7,844 1.06 16,804 225 1.34 Secondary hospitals 278,069 21,422 7.70 245,085 7,166 2.92 16,133 515 3.19 Hospital type Non-communicable disease hospitals 844,557 31,565 3.74 970,333 14,456 1.49 32,085 722 2.25 Infectious disease hospitals 25,602 1,204 4.70 15,394 554 3.60 852 18 2.11 Regional distribution* Eastern coastal area 153,956 1,273 0.83 293,206 1,327 0.45 768 24 3.13 Northeast 123,762 19,646 15.87 62,553 5,899 9.43 3,394 426 12.55 Central 293,124 6,092 2.08 306,436 3,539 1.15 10,696 147 1.37 West 299,317 5,758 1.92 323,532 4,245 1.31 18,079 143 0.79 Note. *Eastern coastal area: Tianjin, Zhejiang, Guangdong; Northeast: Jilin, Liaoning; Central: Henan, Hubei, Hunan; West: Sichuan, Guangxi, Gansu, Yunnan. Table 2. Characteristics of socio-demographic and health seeking in non-viral hepatitis departments
-
HCV antibody prevalence rates among patients were distinct in different departments, with a range of 0.33%–6.93%. Additionally, 6.93% of patients presented in liver disease-related departments, 3.77% in the Internal Medicine, 2.25% in invasive diagnosis and treatment-related departments, 1.83% in other departments, 1.52% in the Department of Surgery, 0.54% in the Department of Pediatrics, and 0.33% in the Department of Obstetrics and Gynecology. The prevalence of HCV antibody varied among hospital patients in different regions of China. Overall, hospital patients in the Northeast (12.95%), the Central (1.59%), and the West (1.52%) China had higher HCV prevalence than those who were in the Eastern coastal area (0.74%) (Table 3).
Characteristics Positive Crude OR 95% CI P-value Adjust OR 95% CI P-value n % Gender Female 32,421 1.64 1.00 1.00 Male 44,489 2.82 1.74 1.72−1.77 < 0.001 1.22 1.20−1.24 < 0.0001 Age group (years) 0−45 14,280 0.79 1.00 1.00 > 45 62,630 3.59 4.67 4.58−4.75 < 0.001 2.74 2.69−2.80 < 0.0001 Hospital level Tertiary hospitals 36,661 1.43 1.00 1.00 Secondary hospitals 40,249 4.10 2.96 2.92−3.00 < 0.001 1.72 1.69−1.75 < 0.0001 Hospital type Non-communicable disease hospitals 69,029 2.03 1.00 1.00 Infectious disease hospitals 7,881 5.42 2.77 2.71−2.84 < 0.001 2.33 2.26−2.40 < 0.0001 Regional distribution* Eastern coastal area 7,854 0.74 1.00 1.00 Northeast 34,480 12.95 19.97 19.47−20.47 < 0.001 12.75 12.40−13.11 < 0.0001 Central 17,193 1.59 2.18 2.12−2.23 < 0.001 1.65 1.61−1.70 < 0.0001 West 17,383 1.52 2.07 2.01−2.12 < 0.001 1.78 1.73−1.83 < 0.0001 Departments of specimen delivery Department of Obstetrics and Gynecology 2,595 0.33 1.00 1.00 Liver disease-related departments 14,991 6.93 22.35 21.43−23.31 < 0.001 10.76 10.27−11.28 < 0.0001 Internal Medicine 32,769 3.77 11.74 11.28−12.22 < 0.001 2.87 2.75−3.00 < 0.0001 Invasive diagnosis and
treatment-related departments740 2.25 6.90 6.35−7.49 < 0.001 1.91 1.76−2.09 < 0.0001 Other departments 10,208 1.83 5.60 5.36−5.85 < 0.001 2.58 2.47−2.70 < 0.0001 Department of Surgery 15,010 1.52 4.64 4.45−4.84 < 0.001 1.95 1.87−2.04 < 0.0001 Department of Pediatrics 597 0.54 1.63 1.49−1.79 < 0.001 1.24 1.13−1.35 < 0.0001 Note. *Eastern coastal area: Tianjin, Zhejiang, Guangdong; Northeast: Jilin, Liaoning; Central: Henan, Hubei, Hunan; West: Sichuan, Guangxi, Gansu, Yunnan. Table 3. Associations between variables and prevalence of HCV antibody among patients in 77 hospitals
The results showed that the prevalence of HCV antibody among patients was associated with gender, age, hospital level, hospital type, regional distribution, and departments of specimen delivery (P < 0.05). The prevalence of HCV antibody among patients was higher in males, over 45 years old, secondary hospitals and infectious disease hospitals compared with females, under 45 years old, tertiary hospitals, and non-communicable disease hospitals, respectively. Participants in the Northeast, the Central and the West China were more likely to receive positive testing results than those who were in the Eastern coastal area. HCV antibody prevalence was higher among patients who were admitted to liver disease-related or invasive diagnosis and treatment-related departments, Internal Medicine, Department of Surgery, and the Department of Pediatrics than those in the Department of Obstetrics and Gynecology (Table 3).
In multivariable analysis, HCV antibody testing of admitted patients at the liver disease-related departments, Internal Medicine, and Department of Surgery were associated with positive HCV antibody status. HCV antibody prevalence was associated with 45 years old and older, testing in infectious disease hospitals and secondary hospitals. Patients in sentinel hospitals of the Northeast, the Central, and the West China had higher HCV prevalence than those who were in the Eastern coastal area (Table 3).
-
The study findings document several important features of hospital patients who had received HCV antibody. The prevalence rates of HCV antibody among patients were higher in males, over 45 years old, secondary hospitals, and infectious disease hospitals compared with females, under 45 years old, tertiary hospitals, and non-communicable disease hospitals. Participants in the Northeast, the Central, and the West China were more likely to be tested for HCV antibody than those who were in the Eastern coastal area. The HCV antibody prevalence was higher among patients who were admitted to the liver disease-related department, invasive diagnosis and treatment-related departments, Internal Medicine, Department of Surgery, and Department of Pediatrics than the Department of Obstetrics and Gynecology. Tailored HCV antibody screening and testing strategies targeting hospital patients are recommended to locate priority populations and increase relative testing rates.
The findings revealed that the HCV antibody prevalence among patients, and the results were varied greatly in different departments. According to previous studies, HCV antibody prevalence in the Department of Obstetrics and Gynecology approximately represented the general population[14]. Whereas, our study results showed different findings. To be specific, a Chinese national epidemiological survey indicated that the HCV antibody prevalence was at 0.43% among people aged 1–59. According to our study, the prevalence of patients in the Department of Obstetrics and Gynecology was 0.33%, and it was lower than the rate among people aged 1–59 back in 2006[15]. There are two possible reasons for the stated inconsistency. First, the subjects in the Department of Obstetrics and Gynecology would not be generalizing to all age groups since those patients might be generally younger than those surveyed in the 2006 study, and the HCV antibody prevalence was higher in the elders compared to young women[16]. Second, those patients would represent the general population since the HCV antibody prevalence had decreased from 2006 to 2019. One possible reason might be the effective implementation of the national HCV control and prevention programs in China[17]. Additionally, the Chinese government issued a technical standard for nosocomial infection control to prevent HCV transmission. A study demonstrated that the HCV antibody prevalence among pregnant women in 32 hospitals was 0.23%[18]. Pregnant women are more optimally representative of the Chinese population based on our study findings compared to the population of general patients in hospitals. The prevalence in the Department of Obstetrics and Gynecology (0.33%) was lower than the rates that were indicated in previous studies from other countries. For example, the HCV antibody prevalence rate of urban-based pregnant women who attended antenatal care in the hospitals in the Amhara national regional state, Ethiopia[19] was higher than the prevalence in the Department of Obstetrics and Gynecology in our study, as well as pregnant women who were screened for HCV at a single tertiary-care center in the US[20]. Furthermore, the prevalence is comparable to the rate of pregnant women in an urban area of Mwanza city, Tanzania[21]. The prevalence of HCV antibody in our survey differs from the meta-analysis among the general population in Mainland China. Meta-analysis data collected between 1991 and 2015, while the data of our survey was collected between 2017 and 2019. In recent years, with the implementation of various prevention and control strategies and measures, the hepatitis C infection rate has been reduced. The HCV antibody prevalence in Department of Obstetrics and Gynecology is comparable to the report in volunteer blood donors in China and overall population in Hong Kong, China, which is an important reference for understanding the infection of the general population.
It was not surprising that the highest prevlence of hospital patients has been observed in liver disease-related departments[22]. This result was attributable to patients who had symptoms of liver infections and saw doctors in the liver disease-related departments for help. Additionally, the HCV antibody prevalence of patients in invasive diagnosis and treatment-related departments and the Department of Surgery was higher than those were in the Department of Obstetrics and Gynecology and the Department of Pediatrics. Several studies demonstrated that HCV infection was more prevalent in surgical interventions and invasive operations[23-24]. These patients were more susceptible to hepatitis C infection than others since they might receive surgery interventions or invasive operations before invasive diagnosis and treatment. Those procedures may increase patients’ risk of HCV infections because the virus is transmitted via blood. Thus, promoting HCV antibody testing among patients was essential in the invasive diagnosis and treatment-related departments. The prevalence of HCV antibody among patients in Internal Medicine was relatively high for several reasons. The liver disease-related departments and the Department of Gastroenterology were classified as Internal Medicine in some sentinel hospitals, which might lead to a high positive rate in Internal Medicine. Future studies are encouraged to explore the subdivision of hospital departments further.
Results from non-viral hepatitis departments and multivariate logistic regression indicated that the prevalence of HCV antibody among patients was higher in males, over 45 years old, secondary hospitals, and infectious disease hospitals compared with females, under 45 years old, tertiary hospitals, and non-communicable disease hospitals. Our study results also suggest a reference for further detection in non-viral departments.
HCV antibody prevalence rates among patients also varied geographically. Compared with other regions, the East coastal area of China had a relatively lower prevalence of HCV antibody. The result was similar with the previous epidemiological survey[25], and this may be associated with better implementation of preventive measures (better health care systems and better health education, etc.). In the East coastal area of China, where the economy is more developed than other regions of China. Moreover, as most paid blood donors were in the Northeast and the Central China before 1998, the reservoir of HCV infection may be larger than that in other regions of China. More efforts in hepatitis C control and prevention were needed to devote in the West, the Northeast, and the Central regions of China[26].
We also found that some factors were associated with the prevalence of HCV antibody among patients. Compared to patients under 45 years old, the prevalence of HCV antibody was higher among patients aged 45 years or older. This was in line with previous findings[27-29]. Literature[24] suggested that patients aged 40 or above who engaged in risky behaviors, such as tattoos, blood transfusion, and unclean injections, were at increased risk for hepatitis C. Furthermore, middle age people and the elders with insufficient health education and literacy accounted for a large proportion of HCV positivity that might have fewer opportunities to learn about HCV knowledge[11]. Contrary to previous findings[30], the prevalence of HCV antibody among patients in secondary hospitals was higher than the rate in the tertiary hospitals. The reason may be related to the selection of sentinel hospitals. In several areas with serious hepatitis C epidemic, such as Jianping County in Liaoning Province, there were no tertiary hospitals during our data collection period. If sentinel hospitals of Jianping County were removed, the prevalence of HCV antibody among patients was higher in tertiary hospitals (1.43%) than in secondary hospitals (0.99%). HCV antibody prevalence occurred higher in males than in females[31-33]. Previous studies had reported that men had an increased chance of HCV through unhealthy lifestyles or behaviors, including sharing of equipment for drug injection, male homosexuality, etc [34].
Our study has several limitations. First, we only selected 77 sentinel hospitals in China. The prevalence of HCV antibody only illustrated the relevant rates of patients in sentinel hospitals, not representing the whole Chinese population. Second, due to the shortcomings of passive surveillance, a well-designed, active surveillance system may imply collecting more convincing information in the future. Third, HCV antibody testing strategies among patients in Chinese hospital settings were distinct in different departments. Future studies are recommended to launch in-depth explorations on HCV antibody screening strategies (universal, risk-based, etc.) in China, since those may influence the differences in estimated prevalence.
-
The study results suggest that the prevalence of HCV antibody varied in different populations. Hospitals might be a uniquely, important venues to encourage patients to receive HCV screening. Effective screening strategies need to target the priority population in hospitals and indicate characteristics of patients, including those who were males, over 45 years old, and saw doctors in departments of liver disease, invasive diagnosis and treatment. The priority population should be referred to have HCV antibody tests.
-
The views expressed herein are those of the authors and do not represent the official policy, or endorsement, of their affiliated institutions.
Prevalence of HCV Antibody and its Associated Factors: A Study from Sentinel Hospitals in China
doi: 10.3967/bes2023.039
- Received Date: 2022-07-03
- Accepted Date: 2022-11-04
-
Key words:
- Hepatitis C virus /
- HCV antibody test /
- Prevalence of HCV antibody /
- Sentinel hospital
Abstract:
We declare that we have no conflicts of interest.
| Citation: | XU Peng, DING Guo Wei, WANG Xiao Chun, YE Shao Dong, HEI Fa Xin, YU Jie Jun, YUAN Qing, LIU Zhong Fu, LI Jian. Prevalence of HCV Antibody and its Associated Factors: A Study from Sentinel Hospitals in China[J]. Biomedical and Environmental Sciences, 2023, 36(4): 334-342. doi: 10.3967/bes2023.039 |






 Quick Links
Quick Links
 DownLoad:
DownLoad: