-
The World Health Organization (WHO) launched the ‘End TB Strategy’, which aims to reduce the mortality and incidence rate of tuberculosis (TB) by 95% and 90% by 2035, respectively, compared with the levels in 2015. To achieve these targets and milestones, the strategy set three pillars and 10 indicators, one of which is systematic screening of contacts and high-risk groups[1].
China is one of the 14 high TB, TB/HIV, and multi-drug-resistant TB burdened countries. In 2018, the number of incident cases of TB in China was 866,000, equivalent to 61 cases per 100,000 population[2]. To attain the End TB targets, China must focus on high-risk groups, including close contacts, the very young or elderly, those in congregate settings, homeless persons, drug and alcohol users, inmates, and other marginalized populations. These high-risk groups still experience high incidence because of their special characteristics[3].
Close contact of TB is a definite-risk population according to TB guidelines from WHO and national TB programs (NTP) from most countries, including China[4]. Students are considered at high risk for TB according to China’s NTP[5]. In other words, close contacts of students with TB in universities are potentially at high risk in developing and later transmitting TB. Their clustering activities and environment render them susceptible when the learning institutions have TB cases[6].
We thus aimed to describe the detection of TB among close contacts of TB index cases in 27 universities in the Changping District of China. The specific aims were to establish the characteristics of the index cases and their contacts and yield of screening for TB among the close contacts in the universities between 2017 and 2018. The findings could help improve the strategies aimed at TB prevention and control in such settings.
This cross-sectional study utilized routine work data and investigation data. For this study, TB index cases were supplied by routine work data and were interviewed to provide a list of close contacts. When any index case was detected in the universities in Beijing, their close contacts were screened for TB and received face-to-face interviews within a week. All close contacts of an index case were screened using a symptom questionnaire [asking for cough (≥ 14 d), hemoptysis, chest pain, fever, fatigue, night sweats, loss of appetite, weight loss (≥ 10%)], a purified protein derivative (PPD) test, and a chest X-ray (only for students older than 15 years), all offered simultaneously. If the student had any of these symptoms or abnormal chest X-ray, smear microscopy and culture were performed for TB diagnosis. However, a positive PPD in the absence of symptoms or abnormal chest X-ray was not investigated further. The diagnosis of TB was based on the latest diagnostic criteria for TB.
Close contact: someone who comes close and directly with the index case in the living room for at least 7 d or in the same classroom/same office/the same place of activity for a cumulative at least 8 h (smear + index case) or 40 h (smear − index case) within 3 months before diagnosis in the study. PPD positive: After PPD injection for 72 h, average diameter of hardening ≥ 15 mm or blister or necrosis.
In total, 27 of the 36 universities in Changping District with data available were selected as the study sites. All pulmonary TB index cases and their close contacts in these universities were included in the study between 2017 and 2018.
Data collected from the interviews included 1) socio-demographic information of index cases and close contacts (e.g., age, gender, ethnicity, education, reported history of smoking, alcohol use), 2) clinical variables [e.g., TB symptoms, contact duration, reported diabetes, chronic kidney disease, chronic bronchitis, chronic gastritis/gastric ulcer, rheumatism, mental illness, use of immunosuppressive medications, and body mass index (BMI) as measured interviewer], 3) environmental variables related to index cases (e.g., index case’s room volume and air change per hour), and 4) examination and laboratory variables of the contacts (e.g., PPD test, smear microscopy, and culture). The index cases had been on treatment for varied durations of time at the time questions on symptoms of TB were elicited. All data were collected into structured questionnaire and double-entered from a paper-based pro forma into EpiData software, which was managed by the designed researchers. Cross-checking was performed before analysis.
The proportion of different categorical variables was analyzed and described among index cases and close contacts separately. The proportion was calculated by the number of TB cases diagnosed of all close contacts. The analysis was performed in SAS software (SAS Version 9.4).
A total of 101 index TB cases were notified in the 27 universities in Changping District, Beijing during the study period. All index cases were drug-sensitive pulmonary TB, including 39 (39.0%) with culture-confirmed TB and 62 (61.0%) with culture-negative TB. Almost all the index cases (99, 98.0%) were new cases of TB. Most 78 (77.0%) were students (the rest either teachers or other workers), 61 (60.0%) were males, 63 (62.0%) between 18 and 23 years of age, and of the students 65 (83.0%) were pursuing their bachelor degree courses (Table 1). Of the index cases, 34 (34.0%) lived in rooms of < 10 m3 volume per person while 82 (81.0%) lived in rooms with measured air exchange of < 12 air change per hour. Other clinical characteristics of the index cases are listed in Table 2.
Characteristic Index case Close contact N (%) N (%) Total 101 (100) 314 (100) Gender Male 61 (60.4) 197 (62.7) Female 40 (39.6) 117 (37.3) Age group (years) < 18 10 (9.9) 24 (7.6) 18–23 63 (62.4) 209 (66.6) > 23 28 (27.7) 81 (25.8) Ethnicity Han 94 (93.1) 285 (90.8) Others 7 (6.9) 29 (9.2) Job Students 78 (77.2) 244 (77.7) Teachers 18 (17.8) 58 (18.5) Other workers 5 (5.0) 12 (3.8) Education level* Bachelor 65 (83.3) 198 (81.2) Master or above 8 (10.2) 16 (6.6) Unknown 5 (6.4) 30 (12.3) Smoking Never 90 (89.1) 265 (84.4) Previous smoking 4 (4.0) 11 (3.5) Current smoking 7 (6.9) 38 (12.1) Alcohol user Never 90 (89.1) 234 (74.5) Previous alcohol use 4 (4.0) 40 (12.7) Current alcohol use 7 (6.9) 40 (12.7) BMI (kg/m2) < 18.5 12 (11.9) 35 (11.2) 18.5 to < 24.0 73 (72.3) 193 (61.5) 24.0 to < 28.0 16 (15.8) 66 (21.0) ≥ 28.0 0 (0.0) 20 (6.4) Exercise intensity# Heavy 49 (48.5) 152 (48.4) Medium or light 52 (51.5) 162 (51.6) Awareness of TB^ All correct answers 81 (80.2) 157 (50.0) At least 1 incorrect answer 20 (19.8) 157 (50.0) Note. BMI: body mass index, TB: Tuberculosis.
*Only to students in universities, not including staffs and teachers.
#Heavy exercise intensity: ≥ 3 times high-intensity exercise and ≥ 5 times medium-intensity exercise and ≥ 7 times Low-intensity exercise per week.
^Q1: What is the main transmission route of TB? Q2: Which symptoms do you think should be suspected of tuberculosis? Q3: If you suspect that you have tuberculosis, where will you go for diagnosis? Q4: Can covering mouth and nose and wearing a mask reduce the spread of TB when you cough or sneeze? Q5: Can TB be cured?Table 1. Socio-demographic characteristics of index TB cases and their close contacts in universities in Changping district, Beijing, 2017–2018
Characteristic Index case Close contact N (%) N (%) Total 101 (100) 314 (100) TB-related symptom Cough or bloody sputum 17 (16.8) 6 (1.9) Others 16 (15.8) 5 (1.6) No symptom 68 (67.3) 303 (96.5) Diabetes* Yes 1 (1.0) 0.0 (0.0) No 81 (80.2) 287 (91.4) Unknown 19 (18.9) 27 (8.6) Chronic kidney disease* No 82 (81.2) 286 (91.1) Unknown 19 (18.8) 28 (8.9) Chronic bronchitis* Yes 0 (0.0) 5 (1.6) No 82 (81.2) 281 (89.5) Unknown 19 (18.8) 28 (8.9) Chronic gastritis/gastric ulcer* Yes 0 (0.0) 3 (1.0) No 83 (82.2) 282 (89.8) Unknown 18 (17.8) 29 (9.2) Rheumatism* No 83 (82.2) 285 (90.8) Unknown 18 (17.8) 29 (9.2) Mental illness* No 83 (82.2) 285 (90.8) Unknown 18 (17.8) 29 (9.2) Immunosuppressant user* No 83 (82.2) 282 (89.8) Unknown 18 (17.8) 32 (10.2) Note. *As reported by the index case, TB: Tuberculosis. Table 2. Clinical characteristics of index TB cases and their close contacts in universities in Changping district, Beijing, 2017–2018
A total of 314 close contacts of the index cases were identified and screened, averaging three close contacts per index case. Majority of the contacts (197, 63.0%) were males and 209 (67.0%) were between 18 and 23 years of age. Of the contacts, 244 (78.0%) were students, of whom 198 (81.0%) were pursuing their bachelor degree courses (Table 1). The student contacts kept touch with the fellow student index cases for an average of 14 h per day (standard deviation, SD: 5.9), and the teachers and other staff kept in touch with their colleagues for an average of 7.4 h per day (SD: 4.7). With regard the risk factors for TB, 265 (84.0%) reported no history of ever smoking and only 35 (11.0%) were undernourished (BMI < 18.5). Only a few contacts reported chronic diseases (five chronic bronchitis and three chronic gastritis/gastric ulcer) (Table 2).
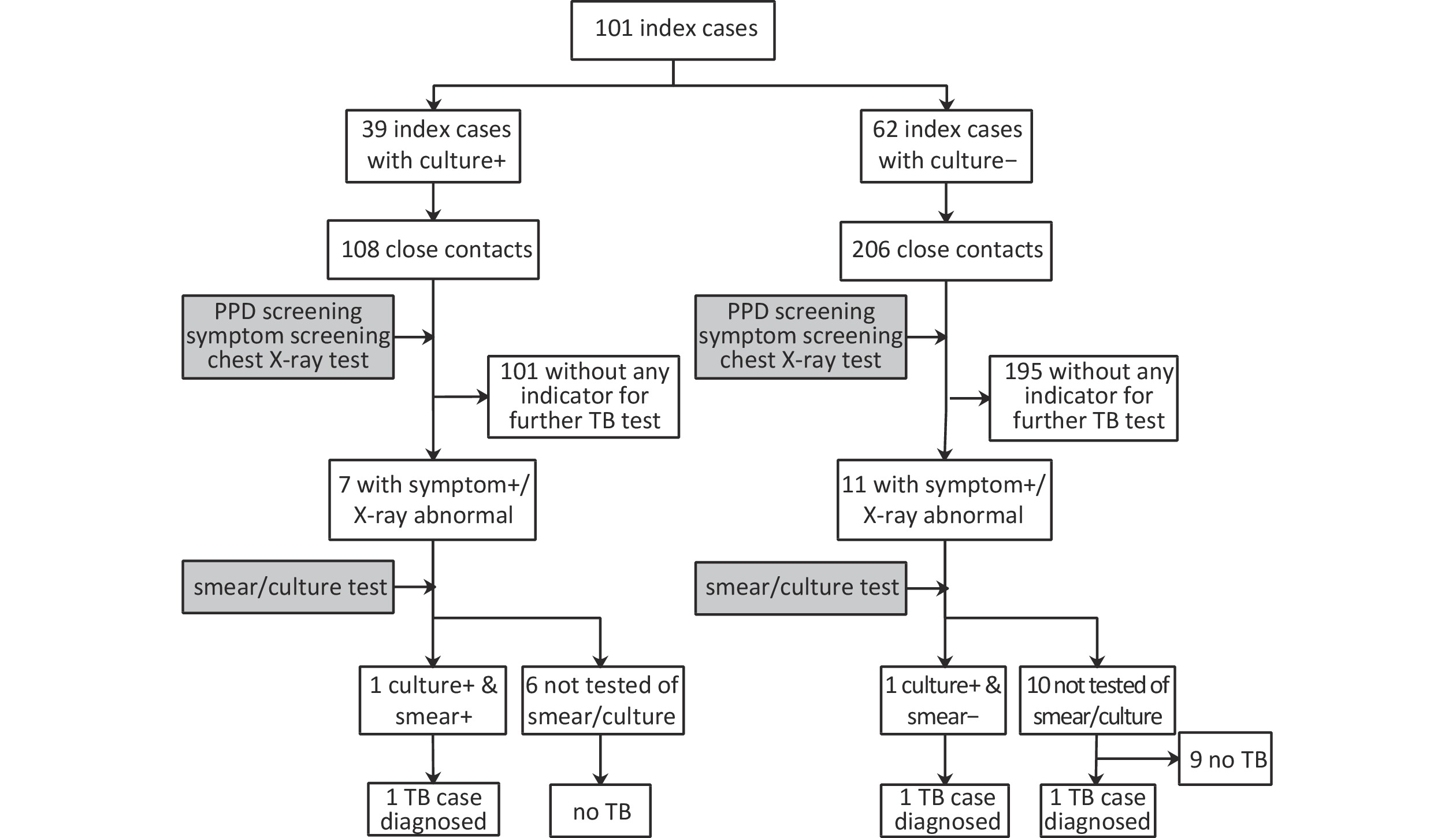
Of the contacts, 108 were from the culture-confirmed TB index cases and 206 from culture-negative index cases. The flow chart of the screening process is presented in Figure 1. Overall, 18 (6%) close contacts were symptomatic and/or had abnormal chest X-rays and were offered smear and culture tests, out of whom sputum was obtained from only two. Eventually, one contact of culture-confirmed index case was confirmed to have TB while two contacts of culture-negative index cases were diagnosed with TB (one with culture-confirmed, the other clinically diagnosed TB). Thus, three cases of TB among the contacts translated to an overall prevalence of 955 cases/100,000 population. The prevalence was 926/100,000 population and 971/100,000 population among contacts of culture-confirmed and culture-negative index TB cases, respectively. All three cases were students, of whom two had BMI < 18.5 kg/m2 and poor air exchange within the dormitory rooms of their respective index cases (air change per hour < 12).
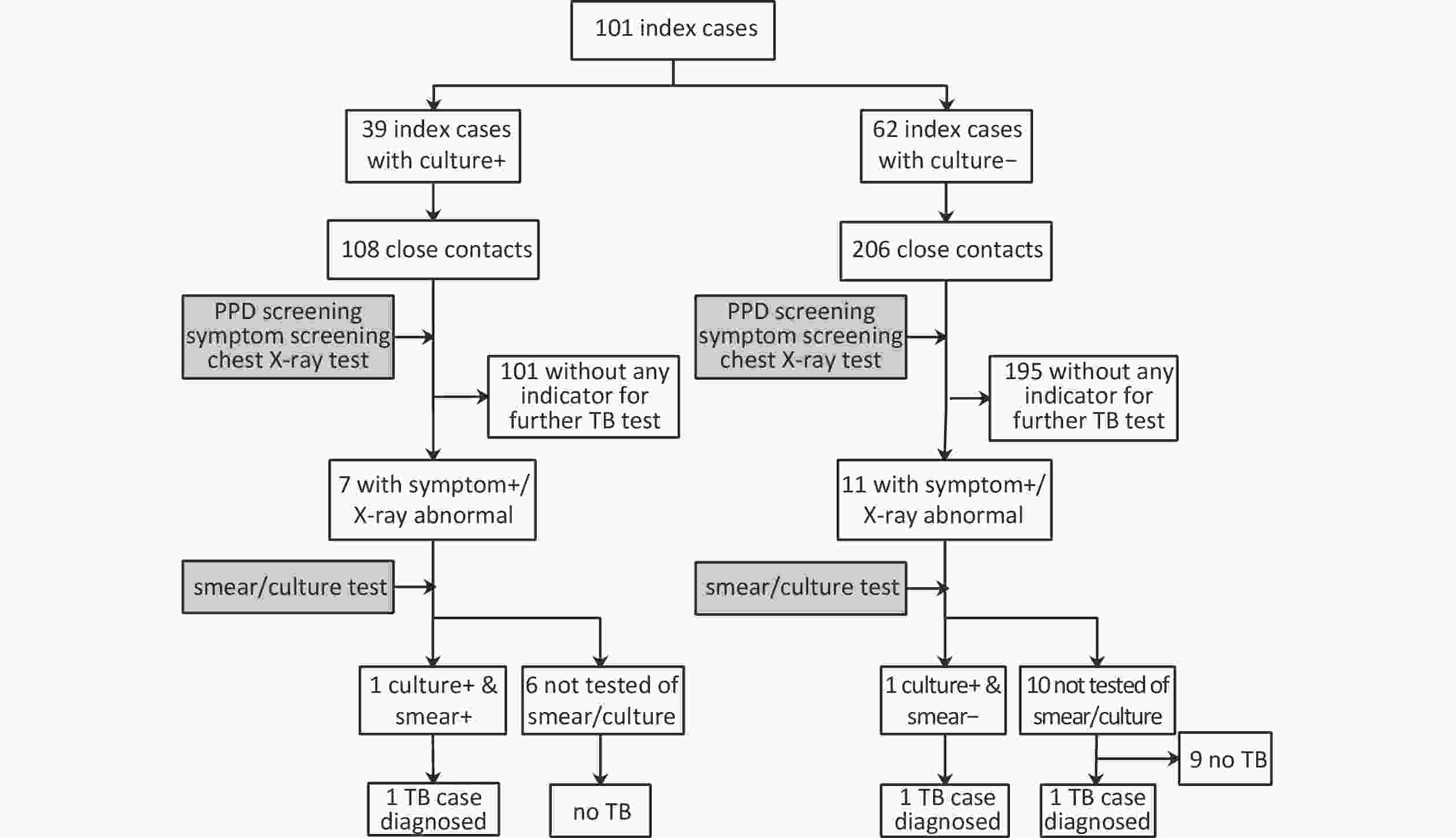
Figure 1. Flow chart of TB detection among close contacts of index cases in 27 universities in Changping District, Beijing, China, 2017–2018. PPD: purified protein derivative, TB: tuberculosis, symptom+: having presumptive TB symptoms, X-ray abnormal: chest X-ray test abnormal, smear+: smear microscopy positive, smear-: smear microscopy negative, culture+: culture positive
This study detected three TB cases out of 314 close contacts in the study sites. All the cases were among student contacts and none among the staff in this study. While in universities, students often have to live in crowded dormitories and share facilities with others. Some of these dormitories may also lack adequate ventilation, inhibiting efficient mycobacterial dilution. The students spend a lot of time together either in the classrooms or dormitories, thus increasing the risk of acquiring TB from fellow student index cases. The spread of TB is enhanced by crowding, poor ventilation, and increased duration of contact with an index case[7]. These scenarios may explain why the prevalence was higher than the general population. Compared with student contacts, the contacts of staff do not necessarily spend as much time with the index cases and they may not live in such congregate rooms as the dormitories. Even though the risk of TB among contacts of staff was lowered, screening programs in such congregate institutions still need to include them. Transmissions have been documented to occur from teachers to pupils/students in other settings[8].
By contrast, other similar studies in universities in Beijing showed lower prevalence rates of TB because contacts with presumptive TB were not offered culture test at that time and were tested by smear microscopy alone. Microscopy has a low sensitivity (39%–63%)[9], which may have resulted in missed cases of TB among the contacts. And this is one of strengths in this study. Moreover, these studies collected data for one year or less, including far fewer cases than necessary to make conclusions. Superior tests need to be performed to diagnose TB in this population. Although the sensitivity of Gene Xpert MTB/RIF is comparable to that of culture, it has a short turn-around-time for results. It also provides the status of rifampicin resistance in the same run.
The TB screening process in institutions of higher learning needs to be applied systematically with tact and skills. This process warrants advanced technology, considering that the smart phone ownership and usage in this population are high. Those presumed to have TB should be encouraged and educated on the best sputum collection techniques—thus increasing the uptake of laboratory testing—while those diagnosed with TB should be assured of confidentiality while handling their information. Patient education on cough etiquette, ventilation, and other infection control procedures also play a significant role in reducing the spread of TB in the dormitories and classrooms. The whole university population should also be included in the TB awareness campaigns to increase knowledge and reduce stigma.
This study has several strengths. First, compared with other studies in universities in China, this study used culture test for TB diagnosis aside from smear microscopy test among close contacts. This process could increase the sensitivity of TB detection among contacts and satisfy the latest criteria of TB diagnosis. Second, its implementation and reporting followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) and the Reporting of studies Conducted using Observational Routinely-collected health Data (RECORD) guidelines. Third, the inclusion of 27 (75%) of the total 36 universities in Changping district and over a two-year period provided broad and generalizable findings that could be applied even beyond the district. Forth, data were collected in a standardized and systematic manner across the universities and by trained staff overseeing TB activities in these institutions. Being part of a project, this procedure allowed similar applications of tools, systems, and criteria in all the study sites. Finally, the proportion with missing data in the key variables was also minimal.
The study also has limitations. Almost nine-in-ten eligible contacts (with symptoms or abnormal X-ray) did not have smear or culture results, possibly leading to underestimation of TB detection. Although the major reason given was lack of sputum, implementing the aforementioned procedure could improve this situation. In addition, some index cases might not have provided all their contacts for personal reasons. Only three contacts were diagnosed to have TB, thus not allowing us to conduct risk-factor analyses. Large-scale and long-term studies on this subject must be conducted to identify the risk factors (including social and environmental) for contacts developing TB in a systematic manner.
Prevalence of Tuberculosis among Close Contacts of Index Cases in 27 Universities in Beijing, China, 2017–2018
doi: 10.3967/bes2020.104
- Received Date: 2020-01-10
- Accepted Date: 2020-06-30
| Citation: | ZHAO Fei, ZHANG Zhi Guo, MA Shu Bo, YANG Zhen, HE Yan Ping, WANG Lu Qin, OWITI Philip, MA Chao, LI Tao, DU Xin, ZHANG Can You, CHENG Jun, WANG Li Xia, HE Guang Xue, ZHANG Hui, LI Ke Xin. Prevalence of Tuberculosis among Close Contacts of Index Cases in 27 Universities in Beijing, China, 2017–2018[J]. Biomedical and Environmental Sciences, 2020, 33(10): 780-784. doi: 10.3967/bes2020.104 |






 Quick Links
Quick Links
 DownLoad:
DownLoad: