-
It is widely recognized that climate change is one of the greatest challenges humanity faces in the 21st century[1,2]. As the leading authority for the assessment of climate change, the Intergovernmental Panel on Climate Change (IPCC), in its special report on global warming of 1.5 °C, has concluded that human activities have caused approximately 1.0 °C of global warming above pre-industrial levels, with a likely increase of 1.5 °C between 2030 and 2052[3]. Climate-related risks for natural and human systems are projected to increase with global warming of 1.5 °C, and increase further with 2 °C or above. These risks depend on the magnitude and rate of warming, geographic location, levels of development and vulnerability, and on the choices and implementation of adaptation and mitigation options.
Levels of greenhouse gases (e.g., CO2, CH4, and N2O) continued to increase in 2020 despite the set-back from the pandemic of coronavirus disease-2019 (COVID-19)[4]. The temporary reduction in emissions in 2020 related to measures taken in response to COVID-19 is likely to lead to only a slight decrease in the annual growth rate of CO2 concentration in the atmosphere, which will be practically indistinguishable from the natural interannual variability driven largely by the terrestrial biosphere[4,5]. In fact, climate change is accelerating and has become the global health emergency[6].
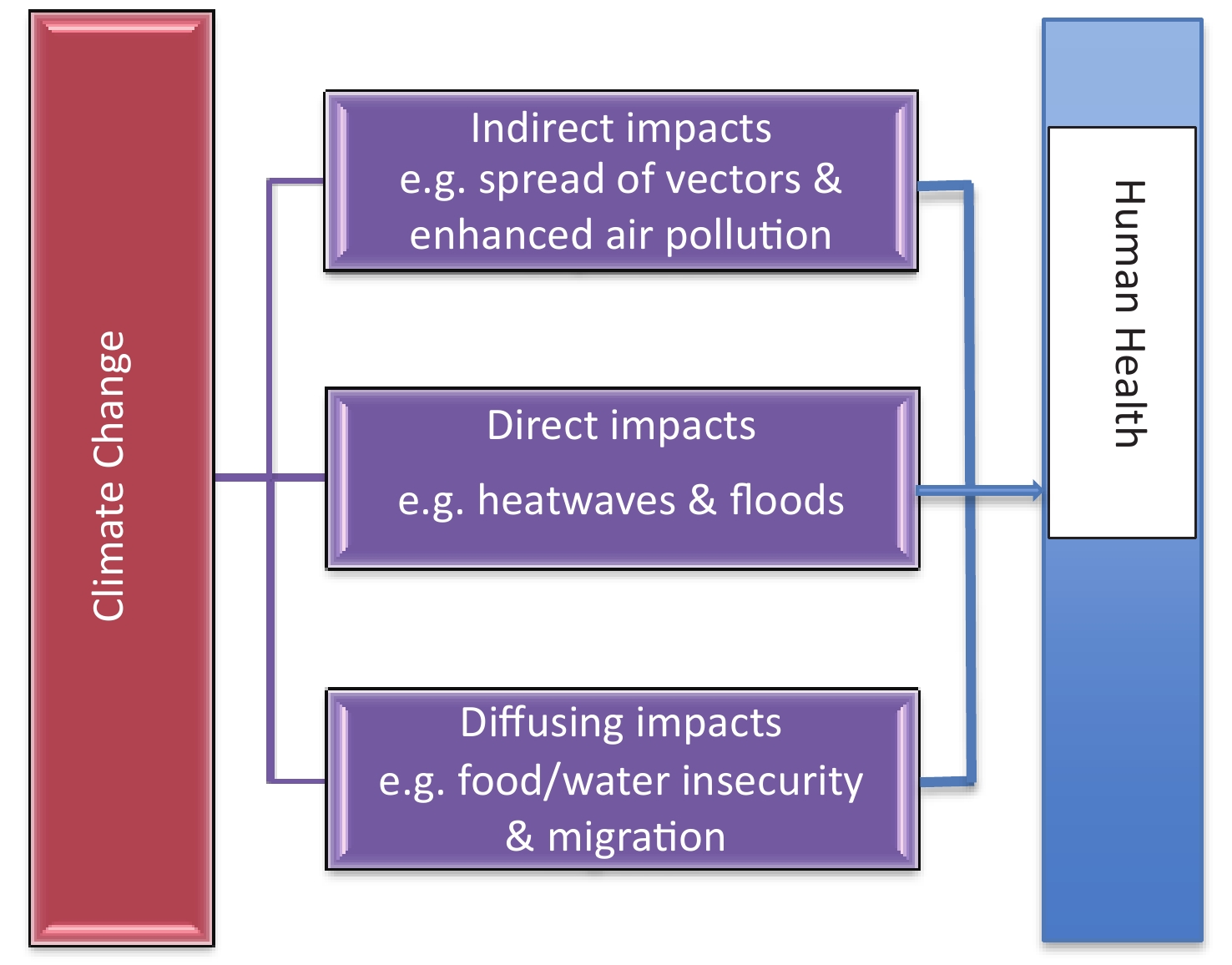
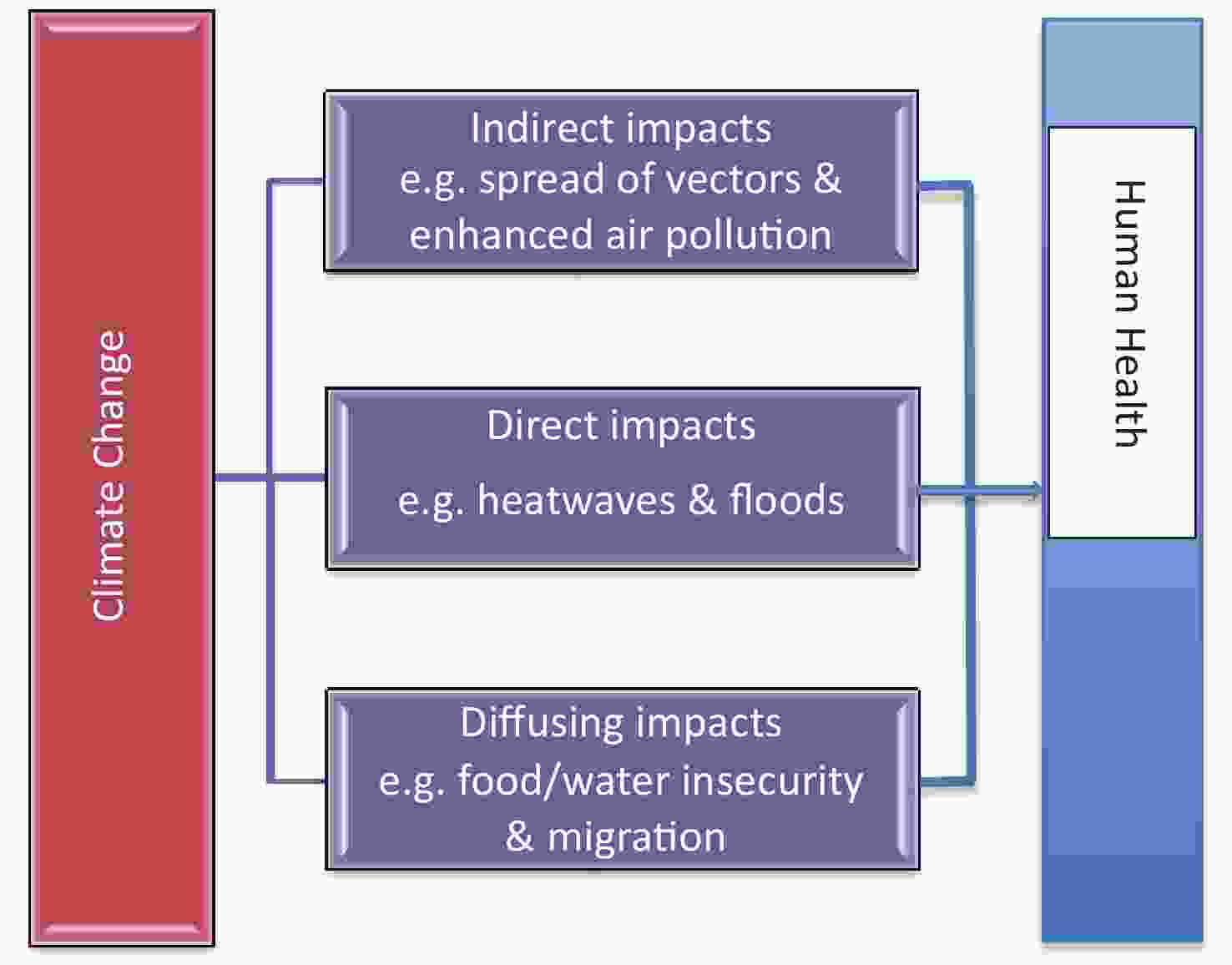
Climate change has already influenced and will increasingly affect human health through direct, indirect, and diffusing pathways[7,8]. The direct impacts include increasing mortality, morbidity and injuries caused by extreme weather events (e.g., heatwaves, storms, bushfires, droughts and flooding); the indirect effects comprise worsening air pollution, increases in vector-, food-, and water-borne diseases, and illnesses from reduced nutrition, due to changes in ecosystems which decrease air quality, result in the spread of disease vectors and reduce crop production; and the diffusing/delayed impacts refer to influences on socioeconomic infrastructure, natural resources and environment, which lead to worsening conditions in food and water security, migration, conflicts and wars as well as profound mental health harms from climate disasters (Figure 1). Among these effects, temperature-related health impacts may have been most extensively studied as these effects are direct and immediate[1,7]. However, health risks attributable to temperature vary with space and time due to different socio-environmental characteristics, population structure, public health systems and adaptation capabilities.
Several issues need to be addressed in evaluating the evidence on the direct impact of exposure to extreme temperatures at the global scale. First, what is the state-of-the-science knowledge on temperature-related health impacts? Second, to what extent might the decreases in cold-related mortality offset the increases in heat-related deaths? Third, what is the relative contribution of different temperature exposures (i.e., non-optimal temperatures and temperature variability) to mortality? Fourth, how much excess mortality is attributable to heatwaves and cold spells? Fifth, what are the compound health effects of temperature and air pollution? Finally, is the evidence available to date sufficient for developing coordinated and evidence-informed climate policies?
-
Heat is among the deadliest weather-related phenomena globally, and heat-related mortality may significantly increase as climate change proceeds. The 2020 report of The Lancet Countdown on health and climate change reveals that vulnerable populations were exposed to an additional 475 million heatwave events globally in 2019, which was, in turn, reflected in excess mortality and morbidity[1]. During the past 20 years, there has been a 53.7% increase in heat-related mortality in people older than 65 years, reaching a total of 296,000 deaths in 2018. Another international study examined the burden of heat-related mortality attributable to human-induced climate change over recent decades[9]. They found that recent climate change is already responsible for a considerable proportion of heat-related excess mortality burden. These results support the need for urgent global implementation of stronger mitigation strategies towards zero-carbon targets to reduce further heating and related health impacts.
A number of studies have examined temperature-related mortality, and have evaluated the potential direct health impacts of exposure to heat using scenario-based risk assessment approaches[10-13]. For example, a study projected future temperature-related mortality in New York City[10]. They modelled heat adaptation by incorporating an analysis of the observed population response to heat in New York City over the course of eight decades and estimated that the median number of projected annual heat-related deaths varied greatly by climate, adaptation and population change scenario, ranging from 167 to 3,331 in the 2080s compared with 638 heat-related deaths annually between 2000 and 2006. A European study found that high summer ambient temperatures have an important impact on population health, and this impact will significantly increase in the future, according to the projected increase of mean ambient temperatures and frequency, intensity and duration of weather events[11]. A study assessed the future impacts of climate change on heat-related mortality in 12 US cities[12]. Climate change was projected to result in an increase in heat-related fatalities over time throughout the 21st century in all of the cities included in the study. Nearly 200,000 heat-related deaths are projected to occur in the 12 cities by the end of the century due to climate warming. Another study estimated that for the period of 2041–2060, relative to 1970–2000, excess heat-related mortality in the 51 largest cities in China to be 37,800 (95% CI: 31,300–43,500), 31,700 (95% CI: 26,200–36,600) and 25,800 (95% CI: 21,300–29,800) deaths per year under high, medium and low emission scenario, respectively[13]. A recent study projected the excess cause-, age-, region-, and education-specific mortality attributable to future high temperatures in 161 Chinese districts/counties[14]. They found that heat-related excess mortality is projected to increase from 1.9% (95% CI: 0.2%–3.3%) in the 2010s to 2.4% (0.4%–4.1%) in the 2030 s and 5.5% (0.5%–9.9%) in the 2090 s under a high emission scenario. The projected slopes are steeper in southern, eastern, central and northern China. People with cardiorespiratory diseases, females, the elderly and those with low educational attainment could be more affected. Population ageing amplifies future heat-related excess deaths 2.3- to 5.8-fold under different shared socioeconomic pathways, particularly for the northeast region.
Current greenhouse gas mitigation ambition is consistent with 3 °C global mean warming above preindustrial levels. There is a clear need to strengthen mitigation ambition to stabilize the climate at the Paris Agreement goal of warming of less than 2 °C. Recently, a study examined the differences in city-level heat-related mortality between the 3 °C trajectory and warming of 2 °C and 1.5 °C, using the data from 15 US cities[15]. They found that ratcheting up mitigation ambition to achieve the 2 °C threshold could avoid between 70 and 1980 annual heat-related deaths per city during extreme events. Achieving the 1.5 °C threshold could avoid between 110 and 2,720 annual heat-related deaths. These results provide compelling evidence for the heat-related health benefits of limiting global warming to 1.5 °C in the United States.
An international collaborative team performed a multi-region analysis in 451 locations in 23 countries with different climate zones, and evaluated changes in temperature-related mortality under scenarios consistent with the Paris Agreement targets (1.5 and 2 °C) and more extreme temperature increases (3 and 4 °C)[16]. The results suggest that limiting warming below 2 °C could prevent large increases in temperature-related mortality in most regions worldwide. The comparison between 1.5 and 2 °C is more complex and characterized by higher uncertainty, with geographical differences that indicate potential benefits limited to areas located in warmer climates, where direct climate change impacts will be more discernible.
In general, all these studies have reported a significant increase in excess mortality associated with heat. Heat-related mortality is likely to pose a serious threat to population health within the context of global warming, but there will be substantial health benefits of limiting global warming to 1.5 °C.
-
Some studies have examined and compared variations in both cold- and heat-related deaths, and have consistently projected a decrease in cold-related health risks, with a concomitant increase in deaths directly associated with exposure to heat[17-23]. For example, a study found that temperature increases for Australia are expected to result in a significant increase in heat-related mortality and a decrease in cold-related mortality as climate change continues, but the balance of these differences varied by city. In particular, the seasonal patterns in temperature-related deaths will shift[17]. A study examined the total mortality burden attributable to non-optimum ambient temperature, and the relative contributions from heat and cold in 384 locations across 13 countries and regions[18]. They found that most of the temperature-related mortality burden was attributable to the contribution of cold. The effect of days of extreme temperature was substantially less than that attributable to milder but non-optimum weather. Another study investigated the mortality response to cold and heat in 18 French cities between 2000 and 2010, and observed that 3.9% (95% CI: 3.2%–4.6%) of the total mortality was estimated to be attributed to cold, and 1.2% (1.1%–1.3%) to heat[19]. However, there was a rapid increase in mortality risk at very high temperatures (above percentile 99).
A projection study estimated current and future seasonal patterns in temperature-related mortality in Manhattan, New York, using 16 downscaled global climate models and two emission scenarios[20]. All 32 projections yielded warm season increases and cold season decreases in temperature-related mortality, with steady increases in net annual temperature-related deaths in all cases. These results suggest that, over a range of models and scenarios of future greenhouse gas emissions, increases in heat-related mortality have been shown to outweigh reductions in cold-related mortality, with shifting seasonal patterns. A European study focused on long-term projections and acclimatization scenarios of temperature-related mortality, and observed a change in the seasonality of mortality, with maximum monthly incidence progressively shifting from winter to summer[21]. The results show that the rise in heat-related mortality will start to overtake the reduction of deaths from cold during the second half of the century, amounting to an estimated average drop in human lifespan of up 3–4 months in 2070–2100. There is also some literature questioning whether cold-season deaths will actually go down in a warming world[22,23]. Evidence in support of this contrarian view includes the presence of substantial cold-related mortality in both warm and cold cities in the current climate[24].
Nevertheless, human lifespan might indeed increase if a substantial degree of adaptation to warm temperatures takes place. Other researchers projected future temperature-attributable premature deaths in 209 U.S. cities, and found increasing future premature deaths but results varied by location, with some locations showing net reductions in premature temperature-attributable deaths with climate change[25]. An international study quantified the total mortality burden attributable to non-optimum ambient temperature, and projected excess mortality for cold and heat and their net change in 1990–2099 under climate change scenarios in 23 countries across nine regions of the world[26]. Results indicate, on average, a net increase in temperature-related excess mortality under high-emission scenarios, with disproportionately large impacts in the warmer and poorer regions of the world.
As noted, most literature suggests that there will be an increase in excess deaths during summer and a reduction in winter. In general, studies project a net increase of excess mortality with climate change, particularly under high-emission scenarios. However, estimates of the net impact on excess mortality depend on location and scenario.
-
Climate change not only increases average global surface temperature, but also enhances its variability and leads to increased frequency and intensity of temperature extremes[3]. Therefore, it is essential to evaluate excess mortality associated with temperature variability and extreme weather events. A number of studies have examined the mortality impacts of temperature variability. For example, a study assessed the association of temperature change between neighboring days (TCN), an indicator to reflect sudden temperature variation, with excess mortality[27]. They used daily mortality and meteorological data from 106 communities of United States and found that the relative risk for lag 0–21 days was 0.63 (95% CI: 0.59–0.68) for extremely negative TCN (1st percentile) and 1.46 (1.39–1.54) for extremely positive TCN (99th percentile) on non-accidental mortality. They also found prominent effects of extreme TCNs on mortality for cardiovascular, respiratory, pneumonia, and COPD diseases. People ≥ 75 years and those with respiratory disease, especially pneumonia-deaths, were identified as a particularly vulnerable population to TCN. The TCN-mortality association was modified by season and region.
An Australian study examined mortality risk and associated mortality burden from both non-optimal temperatures and temperature variability[28]. They collected daily time-series data on all-cause deaths and weather variables for the five most populous Australian cities (Sydney, Melbourne, Brisbane, Adelaide, and Perth), from 2000 to 2009. Temperature variability was calculated from the standard deviation of hourly temperatures between two adjacent days. It was observed that heat, cold and temperature variability together resulted in 42,414 deaths during the study period, accounting for about 6.0% of all deaths. 61.4%, 10.6%, and 28.0% of deaths were attributable to cold, heat and temperature variability, respectively. These findings suggest that, in addition to heat and cold, temperature variability needs to be considered in assessing and projecting the health impacts of climate change.
Recently, an international study projected the effect of diurnal temperature range (DTR) on future mortality across 445 communities in 20 countries and regions[29]. They found that, under the unmitigated climate change scenario (RCP 8.5), the future average DTR is projected to increase in most countries and regions (by −0.4 to 1.6 °C), particularly in the USA, south-central Europe, Mexico, and South Africa. The excess deaths currently attributable to DTR were estimated to be 0.2%–7.4%. Furthermore, the DTR-related mortality risk increased as the long-term average temperature increased; in the linear mixed model with the assumption of an interactive effect with long-term average temperature, they estimated 0.05% additional DTR mortality risk per 1 °C increase in average temperature. Based on the interaction with long-term average temperature, the DTR-related excess deaths are projected to increase in all countries or regions by 1.4%–10.3% in 2090–2099. This study suggests that globally, DTR-related excess mortality might increase under climate change, and this increasing pattern is likely to vary between countries and regions.
As climate change proceeds, many countries experience more and more intensified heatwaves, and increasing research attention has been paid to the health impacts of heatwaves. A systematic review indicates that heatwaves significantly increase mortality, but the magnitude of the effects varies under different heatwave definitions[30]. Heatwave intensity seems to play a relatively more important role than duration in determining heatwave-related deaths. A few studies have projected the impacts of heatwaves in the future[31,32]. For example, a study projected the heatwave trends in 82 US communities in 2061–2080 under two RCP (Representative Concentration Pathway) scenarios of climate change (RCP4.5, RCP8.5), two SSP (Shared Socioeconomic Pathway) scenarios of population change (SSP3, SSP5), and three scenarios of community adaptation to heat (none, lagged, on-pace)[31]. They defined a high-mortality heatwave as increases in mortality risk by ≥ 20%. More high-mortality heatwaves are expected under the RCP8.5 versus RCP4.5 scenario, and on-pace adaptation can significantly reduce the impact of high-mortality heatwaves. An international study projected excess mortality in relation to heatwaves in the future under different scenarios of greenhouse gas emissions, with two assumptions for adaptation (no adaptation and hypothetical adaptation) and three scenarios of population change (high, median, and low variant) in 412 communities within 20 countries/regions[32]. The mortality changes in 2031–2080 versus 1971–2020 range from approximately 2,000% in Colombia to 150% in Moldova under the highest emission and high-variant population scenario, without any adaptation. However, the increase would be much smaller if the scenario of lower emissions and hypothetical adaptation is adopted.
Compared with heatwaves, less research has focused on the impact of multi-day cold spells. A time-series study examined the relationship between cold spells and mortality in 31 capital cities across China[33]. They found that the relative risks (RR) of non-accidental mortality for cold spells were 1.03 (95% CI: 1.01–1.05), 1.27 (1.19–1.35) and 1.55 (1.40–1.70) at lag 0, lag 0–14 and lag 0–27 days, respectively. The greatest effect estimates of cold spells were found among total respiratory diseases and COPD, with RR of 1.88 (1.65–2.11) and 1.88 (1.58–2.19), respectively. The elderly, less-educated individuals and residents in southern China were more vulnerable to cold spells. Another study estimated and projected mortality attributable to cold waves during 1960–2050 in 209 US cities[34]. They reported that the cold waves were associated with an increased but small risk of mortality. The associations varied substantially across climate regions. The risk increased with the duration and intensity of cold waves. The projected mortality related to cold waves would decrease from 1960 to 2050. Such a decrease, however, is small and may not be able to offset the potential increase in heat-related deaths if the adaptation to heat is not adequate. A systematic review indicates that cold spells were associated with increased mortality rates but there was substantial heterogeneity in estimated effects among the studies[35].
Emerging evidence suggests that the increase in the frequency, intensity, and duration of extreme temperature events due to climate change will be more pronounced than expected[36]. This will affect human well-being and mortality more than that estimated in today's modelling scenarios. Thus, it is important to properly estimate the health impacts of extreme temperature events and develop improved weather/health early warning systems (WHEWSs). The application of WHEWSs is part of primary preventive measures. If WHEWSs are designed and implemented properly, they will likely reduce the public health risk at local, national, and international levels.
On the other hand, human populations have been adapting to heat, cold and the temperature variability. Several studies examined changes in temperature related mortality over the last century, and most of them reported a declining trend[37-39]. For instance, Carson et al. analysed weekly time series data in London, and found a decreasing vulnerability to temperature related mortality during the 20th century[37]. Another study investigated whether sensitivity to episodes of extreme heat and cold has changed in Stockholm, Sweden, for the period 1901–2009, and showed that the relative risk of mortality during extreme temperature events appears to have fallen[38]. The major reasons for such a trend include improved sanitation and healthcare, epidemiological transition (e.g., heat related deaths being caused by infectious diseases (such as diarrheal disease or septicaemia) in the first part of the century become less important), and the use of air conditioning. However, how people adapt to climate change varies with space and time. For example, a recent study analysed the historical relationship between weather fluctuations and mortality evolution in China for the 1964–2008 period[40]. The results show that an additional 1 °C rise in average temperature in a given year increased the annual mortality rate by an average of 3.2%. In contrast, cold days did not have these effects. In addition, by introducing interactions between temperatures and potential modifiers such as access to doctors, hospital beds, air conditioning and refrigerators, they determined that only residential air conditioning played an important role in mitigating the temperature-mortality relationship. However, the penetration of air conditioning in China is still relatively low. This may explain why there is little evidence of overall adaptation to high temperatures in China.
-
A number of studies have assessed interactive effects of temperature and air pollution on mortality[41-44]. Most of these studies have focused on a single city but a few studies have used multicity data. For example, a study examined whether the mortality effects of air pollution are modified by temperature and vice versa in eight European cities[45]. The results show that high temperature could modify the effects of air pollution on daily mortality and high air pollution might enhance the air temperature effects. Another study assessed whether temperature and community-level variables modify the association between long-term PM2.5 exposures and mortality across 207 US cities[46]. They found a higher association between long-term PM2.5 exposure and mortality in warmer cities. A stratified time-series analysis was conducted to examine whether the effects of particulate matter less than 10 μm in aerodynamic diameter (PM10) on mortality was modified by temperature across eight Chinese cities[47]. The results indicate that extreme high temperature increased the associations of PM10 with daily mortality. All these findings may have implications for the health impacts associated with both air pollution and global climate change.
-
Table 1 shows the agenda for formulating future health-related climate policy. The patterns of temperature-related mortality vary with space and time and it is essential to address this issue within the local context, while also considering relevant trends at the regional, national and global levels. Additionally, it implies that socio-environmental conditions at different scales should be taken into account in the development of adaptation strategies to cope with the increasing impacts of climate change.
Item Content Explore dynamics of temperature-related deaths The patterns of temperature-related mortality vary with space and time so that health-related climate policy should be developed within the local context. Quantify net balance between heat- and cold-related mortality Increases of heat-related mortality outweigh decreases of cold-related mortality, and there will be significant increase in temperature-related deaths across the globe, particularly in warmer and poorer regions. Evaluate health benefits of mitigation policies The increase in temperature-related mortality would be markedly reduced in scenarios involving mitigation strategies. Thus, it is imperative to develop coordinated and evidence-based climate and public health policies. Assess health gains of adaptation strategies It is vitally important to assess the best adaptation strategies to maximise the health gains as some of climate impacts are inevitable. Play a leadership role from advocacy to action Given a leading role in protecting population health from the impacts of climate change, medical professionals should take active action locally, regionally, nationally and globally. Examine the gap of adaptation It is also imperative to evaluate the gap of adaptation from time to time. Table 1. Agenda for formulating health-related climate policy
Even though more deaths are attributable to cold than heat in many parts of the world at the moment, this pattern will change as climate change proceeds[1,26,32]. Accumulating evidence indicates that, in high-emission scenarios, most regions are projected to experience a steep rise in heat-related mortality that will not be balanced by a reduction in cold-related deaths. As a result, it will result in a substantial net increase in mortality globally. However, the potential impact varies across areas, and populations living in warmer and poorer regions are expected to sustain an increased burden. Urban dwellers are likely to experience more heat exposures than rural counterparts due to heat island effects and densely population. Furthermore, the increase in temperature-related mortality would be substantially reduced in scenarios involving mitigation strategies to limit greenhouse gas emissions. This evidence is crucial for the development of coordinated and evidence-based climate and public health policies, and for informing the ongoing international discussion on the health impacts of climate change. Meanwhile, unintended consequences of mitigation policies should also be evaluated.
The negative health impacts of climate change would disproportionately affect poorer regions of the world[1,7,8]. Small island nations and countries in tropic and sub-tropic areas will be hurt most. Social and environmental inequality should be fairly addressed. Comparison with different emission scenarios highlights the importance and urgency of implementing mitigation policies for limiting global warming and reducing the associated health risks for both high and low income countries.
Thus, it becomes vitally important and exceedingly urgent to curb carbon emissions. However, even if carbon emissions were completely stopped today, global warming is inevitable over the next few decades due to the long atmospheric residence time of carbon and the inertia of the earth system. Therefore, it is necessary to call for an active adaptation in a context of climate change, and the strategies for mitigation and adaptation need to be developed in parallel. It is fundamentally important to design, develop and implement the best adaptation strategies.
The implications of the IPCC special report on global warming of 1.5 °C are indeed dire[3]. Rising seas, heatwaves, wildfires, floods, droughts and extreme storms will be happening at a higher frequency and a greater intensity than they are now. Thus, the next few years are probably the most important in our history. Evidence that climate change poses serious health risks is overwhelming but is being considered insufficiently in analyzing and developing climate policies to date. Greenhouse gas emissions have reached an all-time high and climate change is accelerating on a global scale[48]. Whether human health will continue to flourish or will instead deteriorate depends on actions we take now. Medical professionals have a leading role in protecting population health from the impacts of climate change. If no action is taken to mitigate carbon emissions, we may miss the last opportunity to tackle climate change. It is encouraging to see that Canada's municipalities are leading the efforts to stem the harmful effects of the climate emergency on human health and push for health-based climate action[49]. It is anticipated that more municipalities will follow the suit, and more concrete and decisive action (e.g., net zero carbon society in two-to-three decades or early) will take place.
-
Global patterns of temperature-related mortality are rapidly moving towards more heat-related and less cold-related deaths. Such a trend will become more apparent in the future if a high emission and no adaptation scenario is adopted. Through this scoping review, we believe that it is indispensably important to reduce carbon footprints from the individual to the globe (Table 2). It is also imperative to note that the “net zero carbon” climate policy will reduce air pollution and bring substantial health co-benefits. Meanwhile, governments at all levels need to develop and implement adaptation plans to cope with the increasing impacts of climate change. Urgent actions are required from the all walks of the society, particularly medical professionals as carers of patients, to prevent irreversible and catastrophic climate-induced health risks.
Highlights • Greenhouse gas emissions have reached an all-time high even with the pandemic of coronavirus disease-2019 (COVID-19). Climate change is accelerating and has become the global health emergency. Whether human health will continue to flourish or will instead deteriorate depends on actions we take now. Medical professionals have a leading role to play in protecting population health from the impacts of climate change. • Climate change poses serious risks to global health and the evidence is strong. The Intergovernmental Panel on Climate Change recently reported that climate-related risks for natural and human systems are projected to increase with global warming of 1.5 °C, and increase further with 2 °C and above. • Climate change has been increasingly affecting human health through direct, indirect, and diffusing pathways. Of these effects, temperature-related health impacts have been mostly studied. Global patterns of temperature-related mortality are rapidly moving towards more heat-related and less cold-related deaths. • It is vitally important to reduce carbon footprints from the individual to the globe. Actions are urgently required from the all walks of the society, particularly medical professionals as carers of patients, to prevent catastrophic climate-induced health risks. Table 2. Highlights box
-
The authors declare that there are no conflicts of interest.
-
ST conceived the study and wrote the original draft. JO and PK reviewed and edited the manuscript.
Climate Change and Temperature-related Mortality: Implications for Health-related Climate Policy
doi: 10.3967/bes2021.050
- Received Date: 2021-01-20
- Accepted Date: 2021-04-06
| Citation: | TONG Shi Lu, Jorn Olsen, Patrick L. Kinney. Climate Change and Temperature-related Mortality: Implications for Health-related Climate Policy[J]. Biomedical and Environmental Sciences, 2021, 34(5): 379-386. doi: 10.3967/bes2021.050 |






 Quick Links
Quick Links
 DownLoad:
DownLoad: