-
An estimated 40% of people living with HIV (PLHIV) were unaware of their HIV-positive status in 2016 at a global level, suggesting that as an international community, we are not on track to meet the first of the Joint United Nations Programme on HIV and AIDS (UNAIDS) 90-90-90 targets-having 90% of infected individuals diagnosed by 2020[1-2]. Performance toward this target varies at the individual country level[3]. In China, official joint estimates conducted by UNAIDS, WHO, and China's National Health and Family Planning Commission place the country's estimated total number of PLHIV at 850, 000 as of the end of 2015. China's National Center for AIDS/STD Control and Prevention (NCAIDS) reported a total of 550, 000 cases nationwide indicating a 65% diagnostic rate[4]. Although these estimates place China at a similar level with the international community as a whole, the figures are off track to meet the 'First 90' with less than four years to go.
To hit the First 90, China must introduce new methods to increase testing rates. HIV voluntary counseling and testing (VCT) has been available nationwide since 2002 and provider-initiated counseling and testing (PICT) since 2007[5]. However, these services have clearly not been enough and new strategies must be explored and embraced. Sexual contact has become the dominant route of transmission, with men who have sex with men (MSM) being the population making the most substantial contribution to the annual tally of new infections. Among newly diagnosed cases in 2014 in China, 26% were MSM, a substantial increase from the 2.5% reported in 2006. In addition, HIV prevalence among MSM increased from 2% in 2007 to 8% in 2015[6-7]. However, the testing rate among MSM has historically been low despite national guidelines that recommend testing every six months[7-8].
There are well-documented barriers to HIV testing in Chinese MSM, including inconvenience (testing facility locations or house), concern over confidentiality and privacy, fear of stigma and discrimination (both socially and by medical personnel at testing facilities), poor service quality, and long waiting times to obtain the results[7, 9-11]. However, worldwide evidence[12-14] as well as recent experience in China[7, 15-16] suggest that HIV self-testing may help reach key populations who do not choose to access conventional facility-based testing services such as VCT or PICT or do not access them frequently enough. HIV self-testing kits provide a non-discriminatory and highly confidential way to test for HIV.
In China, a very broad variety of HIV test products are easily accessible for purchase online and at HIV/AIDS clinics, hospitals, pharmacies, and Chinese Centers for Disease Control and Prevention (CDC) offices. These products are not regulated by the State Food and Drug Administration (SFDA) and they are not officially promoted nor restricted[7, 17-18]. Although several studies have recently examined HIV self-testing among MSM in China[9-11, 16-21], further characterization is required to better inform the development and broad-scale implementation of HIV self-testing programs for MSM in China. Therefore, the primary aim of this study was to examine self-testing uptake among a large sample of online MSM in Beijing, China as well as factors associated with self-test use.
-
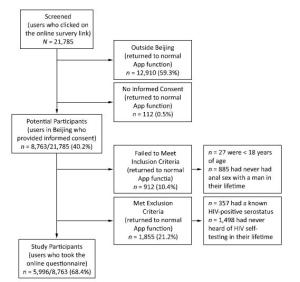
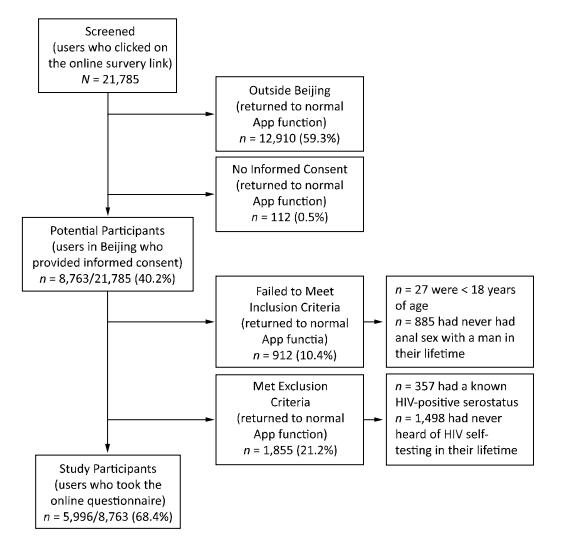
A cross-sectional study design was used to conduct an online survey among MSM in Beijing from May 14th to May 17th 2016. Figure 1 contains a flow diagram showing the study design as well as the development of the final study population.
-
Potential participants were users of a popular gay networking smart phone application (App) who met the following geographical criteria: (a) had previously registered in the App with their region being Beijing; (b) had a smart phone global positioning satellite (GPS) signal located in Beijing; and (c) had answered the question 'Currently, which city do you live in?' as Beijing. Each user identified as being located in Beijing was given a unique identifier based on their IP address. Potential participants were then required to provide informed consent. Only those who did so were further selected if were ≥ 18 years old and had had anal sex with a man at least once during their lifetime. Lastly, potential participants were excluded if they had a known HIV-positive status or had never heard of HIV-self testing.
-
The questionnaire was adapted from that of Wong et al.[20] and consisted of the following sections: (a) demographics, (b) sexual behavior, (c) history of HIV VCT, (d) knowledge of and attitudes toward HIV self-testing, (e) personal HIV self-testing experience, (f) drug use, and (g) sexual health history. HIV self-testing was defined for participants as the use of an HIV testing kit on oneself without supervision from a professional medical worker, where the user chooses the time and place for testing and completes the whole testing process without any professional consultation, inclusive of sample collection, testing, and result interpretation[14, 18, 20].
Participants were presented with each question one at a time and were allowed to select from a finite number of provided scripted answer choices. For most questions, participants were only allowed to select one answer. There were two questions for which participants could choose to select multiple answers, including 'How do you find information on HIV self-testing?' and 'What factors are most important when choosing an HIV self-test kit?' Furthermore, some sections of the survey were adaptive such that only participants who answered affirmatively moved on to more specific questions on that topic. These sections included lifetime drug use, lifetime HIV self-test kit use, and lifetime VCT attendance.
-
The characteristics of the participants were described using categorical variables and presented as numbers and percentages. Participants were stratified according to their personal HIV self-testing experience into two groups: those who had performed HIV self-testing ('self-testers') and those who had never done so ('non-self-testers'). Differences between categories within variables were assessed by Chi-square analysis.
Univariate and multivariate logistic regression was used to assess determinants of HIV self-testing. Having performed HIV self-testing was given a value of 1 and having never per formed an HIV self-test was given a value of 0. Variables with P < 0.05 in the univariate analysis were used as candidate independent variables for multivariate analysis. The final multivariate model was determined by automatically forward selection of the candidate independent variables based on its significant contribution to the model.
P values < 0.05 were considered statistically significant. All confidence intervals (CIs) presented were 95% CIs. Analyses were performed using the SPSS software Version 18.0 (IBM, New York, USA).
-
The study was reviewed and approved by the Institutional Review Board of the Chinese CDC. Informed consent was obtained electronically for all participants prior to the start of the online survey. No personal identifier information was collected, all survey respondents remained anonymous, and no compensation was provided.
-
A total of 21, 785 App users clicked on the link for the online survey. However, 12, 910 (59.3%) returned to normal App function because they were outside Beijing and a further 112 (0.5%) exited from the survey after declining to provide informed consent. Thus, 8, 763 potential participants (40.2%) were screened. A total of 912 over 8, 763 participants (10.4%) failed to meet inclusion criteria and a further 1, 855 (21.2%) met exclusion criteria. This led to a final study population of 5, 996 (of 8, 763, 68.4%), all of whom completed the online survey and were included in the analysis (Figure 1).
-
Characteristics of the participants are presented in Table 1. Most participants were less than 30 years of age (18-24 years: 29.1%; 25-29 years: 32.7%), of Han ethnicity (92.1%), had at least some college-level education (college: 63.3%; ≥ graduate school: 15.9%), were full time employed (79.1%), had monthly incomes above 5, 000 CNY (5, 001-10, 000: 33.9%; > 10, 000: 21.2%), lived in Beijing for at least 2 years (70.9%), were unmarried (85.2%), were cohabitating (67.4%), and self-identified as homosexual (72.0%).
Table 1. Characteristics of the Participants
Items All Participants [N = 5, 996] n(%) 'Self-Testers' [N = 2, 383] n(%) 'Non-Self-Testers' [N = 3, 613] n(%) P-value Demographic Characteristics Age (years) 0.001 18-24 1, 746 (29.1) 649 (27.2) 1, 097 (30.4) 25-29 1, 961 (32.7) 841 (35.3) 1, 120 (31.0) ≥ 30 2, 289 (38.2) 893 (37.5) 1, 396 (38.6) Ethnicity 0.12 Han 5, 524 (92.1) 2, 199 (92.3) 3, 325 (92.0) Minority 472 (7.9) 184 (7.7) 288 (8.0) Education level 0.76 ≤ High schoola 1, 247 (20.8) 499 (20.9) 748 (20.7) College 3, 795 (63.3) 1, 515 (63.6) 2, 280 (63.1) ≥ Graduate school 954 (15.9) 369 (15.5) 585 (16.2) Employment status 0.007 Unemployed or part-time 291 (4.9) 114(4.8) 177 (4.9) Student 962 (16.0) 339 (14.2) 623 (17.2) Full-time 4, 743 (79.1) 1, 930 (81.0) 2, 813 (77.9) Monthly Income (CNY) < 0.001 ≤ 1, 500 554 (9.3) 183 (7.7) 371 (10.3) 1, 501-5, 000 2, 139 (35.7) 814 (34.2) 1, 325 (36.7) 5, 001-10, 000 2, 034 (33.9) 810 (34.0) 1, 224 (33.9) > 10, 000 1, 269 (21.2) 576 (24.2) 693 (19.2) Duration of residence in Beijing (years) 0.30 < 2 1, 746 (29.1) 676 (28.4) 1, 070 (29.6) ≥ 2 4, 250 (70.9) 1, 707 (71.6) 2, 543 (70.4) Marital status 0.004 Married 885 (14.8) 313 (13.1) 572 (15.8) Unmarried 5, 111 (85.2) 2, 070 (86.9) 3, 041 (84.2) Cohabitation status < 0.001 Alone 1, 956 (32.6) 851 (35.7) 1, 105 (30.6) Cohabitatingb 4, 040 (67.4) 1, 532 (64.3) 2, 508 (69.4) Sexual orientation < 0.001 Homosexual 4, 318 (72.0) 1, 775 (74.5) 2, 543 (70.4) Bisexual 1, 643 (27.4) 604 (25.3) 1, 039 (28.8) Unknown/unsure 35 (0.6) 4 (0.2) 31 (0.9) Sexual Behavior Characteristics Method for finding sex partners 0.11 Internet or mobile Apps 5, 255 (87.6) 2, 088 (87.6) 3, 167 (87.7) Parties 288 (4.8) 129 (5.4) 159 (4.4) Other 453 (7.6) 166 (7.0) 287 (7.9) Age at sexual debut with male (years) 0.17 < 18 1, 209 (20.2) 498 (20.9) 711 (19.7) 18-29 4, 328 (72.2) 1, 719 (72.1) 2, 609 (72.2) ≥ 30 459 (7.7) 166 (7.0) 293 (8.1) Role in sexual intercourse 0.02 Anal receptive 1, 396 (23.3) 511 (21.4) 885 (24.5) Anal insertive 1, 338 (22.3) 553 (23.2) 785 (21.7) Both 3, 262 (54.4) 1, 319 (55.4) 1, 943 (53.8) Number of male sex partnersc < 0.001 0 1, 856 (31.0) 600 (25.2) 1, 256 (34.8) 1 2, 091 (34.9) 797 (33.4) 1, 294 (35.8) ≥ 2 2, 049 (34.2) 986 (41.4) 1, 063 (29.4) Condom use with latest male sex partner 0.001 Yes 3, 157 (76.3) 1, 406 (78.9) 1, 751 (74.3) No 983 (23.7) 377 (21.1) 606 (25.7) Missing (no male sex partners) 1, 856 - - Condom use with male sex partnersc < 0.001 Never 410 (9.9) 140 (7.9) 270 (11.5) Ever 1, 208 (29.2) 538 (30.2) 670 (28.4) Always 2, 522 (60.9) 1, 105 (62.0) 1, 417 (60.1) Missing (no male sex partners) 1, 856 - - Number of commercial male sex partnersc < 0.001 0 5, 572 (92.9) 2, 182 (91.6) 3, 390 (93.8) 1 271 (4.5) 114 (4.8) 157 (4.3) ≥ 2 153 (2.6) 87 (3.7) 66 (1.8) Condom use with latest commercial male sex partner 0.68 Yes 336 (79.2) 161 (80.1) 175 (78.5) No 88 (20.8) 40 (19.9) 48 (21.5) Missing (no commercial male sex partners) 5, 572 - - Condom use with commercial male sex partnersc 0.22 Never 43 (10.1) 18 (9.0) 25 (11.2) Ever 97 (22.9) 40 (19.9) 57 (25.6) Always 284 (67.0) 143 (71.1) 141 (63.2) Missing (no commercial male sex partners) 5, 572 - - Number of female sex partnersc 0.33 0 5, 265 (87.8) 2, 089 (87.7) 3, 176 (87.9) 1 656 (10.9) 258 (10.8) 398 (11.0) ≥ 2 75 (1.3) 36 (1.5) 39 (1.1) Condom use with latest female partner 0.002 Yes 404 (55.3) 183 (62.2) 221 (50.6) No 327 (44.7) 111 (37.8) 216 (49.4) Missing (no female sex partners) 5, 265 - - Condom use with female partnerc 0.002 Never in lifetime 263 (36.0) 83 (28.2) 180 (41.2) Ever in lifetime 153 (20.9) 69 (23.5) 84 (19.2) Always 315 (43.1) 142 (48.3) 173 (39.6) Missing (no female sex partners) 5, 265 - - Sexual Health Characteristics Sought healthcare for STI symptomsd 0.006 Yes 541 (9.0) 245 (10.3) 296 (8.2) No 5, 455 (91.0) 2, 138 (89.7) 3, 317 (91.8) Results of the latest STI testing 0.48 Gonorrhea 34 (6.3) 16 (6.5) 18 (6.1) Syphilis 164 (30.3) 82 (33.5) 82 (27.7) Chlamydial trachomatis 29 (5.4) 16 (6.5) 13 (4.4) Condyloma acuminate 128 (23.7) 54 (22.0) 74 (25.0) Herpes progenitalis 31 (5.7) 14 (5.7) 17 (5.7) Other 155 (28.7) 63 (25.7) 92 (31.1) Missing (did not seek healthcare) 5, 455 - - Drug Use Behavior Characteristics Drug use ever in lifetime < 0.001 Yes 2, 171 (36.2) 1, 082 (45.4) 1, 089 (30.1) No 3, 825 (63.8) 1, 301 (54.6) 2, 524 (69.9) Anal sex after drug use 0.63 Yes 1, 852 (85.3) 927 (85.7) 925 (84.9) No 319 (14.7) 155 (14.3) 164 (15.1) Missing (no drug use) 3, 825 - - Condom use after drug use 0.03 Never 127 (6.9) 54 (5.8) 73 (7.9) Ever 477 (25.8) 260 (28.0) 217 (23.5) Always 1, 248 (67.4) 613 (66.1) 635 (68.6) Missing (no drug use) 3, 825 - - History of HIV VCT HIV VCT attendance < 0.001 Ever in lifetime 3, 772 (62.9) 1, 914 (80.3) 1, 858 (51.4) Never in lifetime 2, 224 (37.1) 469 (19.7) 1, 755 (48.6) Time since latest HIV VCT (months) < 0.001 ≤ 3 1, 379 (36.6) 786 (41.1) 593 (31.9) 4-6 740 (19.6) 360 (18.8) 380 (20.5) 7-12 539 (14.3) 258 (13.5) 281 (15.1) ≥ 13 1, 114 (29.5) 510 (26.6) 604 (32.5) Missing (never in lifetime) 2, 224 - - Consultation during latest HIV VCT 0.005 Yes 2, 123 (56.3) 1, 101 (57.5) 1, 022 (55.0) No 1, 037 (27.5) 483 (25.2) 554 (29.8) Can't remember 612 (16.2) 330 (17.2) 282 (15.2) Missing (never in lifetime) 2, 224 - - Site of the latest HIV VCT < 0.001 CDC 1, 343 (35.6) 696 (36.4) 647 (34.8) Hospital 1, 328 (35.2) 559 (29.2) 769 (41.4) Blood donation station 111 (2.9) 70 (3.7) 41 (2.2) NGO 792 (21.0) 423 (22.1) 369 (19.9) Others 198 (5.2) 166 (8.7) 32 (1.7) Missing (never in lifetime) 2, 224 - - HIV Self-testing Knowledge and Attitudes Sources of information on HIV self-testinge Mobile Apps 3, 670 (61.2) 1, 269 (53.3) 2, 401 (66.5) Posters 1, 552 (25.9) 617 (25.9) 935 (25.9) Consultation with medical professionals 1, 090 (18.2) 555 (23.3) 535 (14.8) Friends 1, 556 (26.0) 787 (33.0) 769 (21.3) Websites 2, 668 (44.5) 1, 026 (43.1) 1, 642 (45.4) Other 79 (1.3) 43 (1.8) 36 (1.0) Willingness to use an HIV self-test kit in the future < 0.001 Willing 5, 535 (92.3) 2, 310 (96.9) 3, 225(89.3) Unwilling 461 (7.7) 73 (3.1) 388 (10.7) Best feature of HIV self-testing < 0.001 Easy to purchase 151 (2.5) 79 (3.3) 72 (2.0) Simple operation 967 (16.1) 449 (18.8) 518 (14.3) Protection of privacy 3, 307 (55.2) 1, 203 (50.5) 2, 104 (58.2) Convenient 1, 538 (25.7) 643 (27.0) 895 (24.8) Other 33 (0.6) 9 (0.4) 24 (0.7) Disadvantages of HIV self-testinge Difficult to obtain 2, 143 (35.7) 772 (32.4) 1, 371 (37.9) Lack of consultation 1, 765 (29.4) 584 (24.5) 1, 181 (32.7) Difficult operation 1, 004 (16.7) 365 (15.3) 639 (17.7) Difficult results interpretation 1, 507 (25.1) 491 (20.6) 1, 016 (28.1) High price 1, 385 (23.1) 631 (26.5) 754 (20.9) Quality concerns 3, 438 (57.3) 1, 269 (53.3) 2, 169 (60.0) Other 187 (3.1) 76 (3.2) 111 (3.1) Note.CNY: Chinese Yuan; CDC: Centers for Disease Control; NGO: non-government organization; STI: sexually-transmitted infection; VCT: voluntary counseling and HIV testing. aThe category 'High School' includes also vocational or technical school. bThe category 'Cohabitating' includes those who live with their spouse, roommate, or other. cThese sexual behavior characteristics were limited to the prior 3 months. dSeeking healthcare for STI symptoms was limited to the last year. eFor these two variables, more than one response was allowed in the survey. No statistical comparison was performed for these variables. 'Self-testers' indicates those who had used HIV self-testing and 'non-self-testers' those who had never used HIV self-testing. Most of the participants reported finding their sex partners via the internet or mobile Apps (87.6%). In the preceding 3 months, 34.9% reported having had one male sex partner and 34.2% reported having two or more male sex partners. The majority of the participants reported using condoms with their latest male sex partner (76.3%) and always using condoms with male sex partners (60.9%). Only 9.0% reported having sought healthcare for symptoms of sexually transmitted infection (STI) during the last year. Lifetime drug use was reported by 36.2% of the participants, the majority of them reporting having had anal sex after drug use (85.3%).
The majority of the participants reported having attended VCT (62.9%). Among those who had attended VCT, 36.6% reported attending at least once in the past three months while 29.5% reported that it had been at least 13 months since they last attended. The most frequently selected source of information on HIV self-testing was mobile Apps (61.2%). A large majority reported willingness to use HIV self-testing kits (92.3%) and most participants selected either privacy (55.2%) or convenience (25.7%) as the best features of these products.
-
Among all 5, 996 participants, 2, 383 (39.7%) reported having used an HIV self-test kit before ('self-testers'), while 3, 613 (60.3%) reported never having self-tested ('non-self-testers'). As shown in Table 1, a larger proportion of 'self-testers' were aged between 25 to 29 years (35.3% vs. 31.0% for 'non-self-testers', P = 0.001), employed full-time (81.0% vs. 77.9%, P = 0.007), had monthly incomes > 10, 000 CNY (24.2% vs. 19.2%, P < 0.001), were unmarried (86.9% vs. 84.2%, P = 0.004), lived alone (35.7% vs. 30.6%, P < 0.001), and self-identified as homosexual (74.5% vs. 70.4%, P < 0.001).
A larger proportion of 'self-testers' had two or more male sex partners in the prior 3 months (41.4% vs. 29.4%, P < 0.001). Among those who had had at least one male sex partner in the prior 3 months, a larger proportion of 'self-testers' used condoms with their latest male sex partner than 'non-self-testers' (78.9% vs. 74.3%, P = 0.001) and always used condoms with male sex partners (62.0% vs. 60.1%, P < 0.001). Among those who had had at least one female sex partner, a greater proportion of 'self-testers' also used condoms with their latest female sex partner (62.2% vs. 50.6%, P = 0.002) and always used condoms with female sex partners (48.3% vs. 39.6%, P = 0.002) than 'non-self-testers'.
A greater proportion of 'self-testers' had sought healthcare for symptoms of STIs (10.3% vs. 8.2%, P = 0.006) and had used drugs in their lifetimes (45.4% vs. 30.1%, P < 0.001). A larger proportion of 'self-testers' had attended VCT in their lifetimes (80.3% vs. 51.4%, P < 0.001). Among those that had attended VCT, a greater proportion of 'self-testers' reported that their most recent visit to VCT had been within the prior 3 months (41.1% vs. 31.9%, P < 0.001), had included a consultation (57.5% vs. 55.0%, P = 0.005), and that the VCT site they attended was located at sites other than hospitals [CDC: 36.4% vs. 34.8%, blood donation station: 3.7% vs. 2.2%, non-governmental organization (NGO): 22.1% vs. 19.9%, or other: 8.7% vs. 1.7%, P < 0.001].
A larger proportion of 'self-testers' reported obtaining knowledge about HIV self-testing from medical professionals (23.3% vs. 14.8%) and friends (33.0% vs. 21.3%) and reported being willing to use HIV self-test kits in the future (96.9% vs. 89.3%, P < 0.001). A greater proportion of 'self-testers' selected simple operation (18.8% vs. 14.3%) and convenience (27.0% vs. 24.8%, P < 0.001) as the best features of HIV self-testing. The only disadvantage that 'self-testers' selected more frequently that 'non-self-testers' was high price (26.5% vs. 20.9%).
-
Results of univariate and multivariate regression assessing determinants of HIV self-testing are presented in Table 2. After controlling for confounding factors, elements associated with HIV self-testing uptake included age ≥ 30 years (adjusted OR = 0.69, CI = 0.57-0.83, P < 0.001), monthly income > 10, 000 CNY (adjusted OR = 1.49, CI = 1.10-2.02, P = 0.010), self-identifying as bisexual (adjusted OR = 0.85, CI = 0.73-0.99, P = 0.034), having ≥ 2 male sex partners in the prior 3 months (adjusted OR = 1.24, CI = 1.09-1.43, P = 0.002), having ≥ 2 commercial male sex partners in the prior 3 months (adjusted OR = 1.94, CI = 1.34-2.82, P = 0.001), having history of VCT (adjusted OR = 3.62, CI = 3.11-4.22, P < 0.001), and being unwilling to use an HIV self-test kit in the future (adjusted OR = 0.20, CI = 0.15-0.28, P < 0.001).
Table 2. Determinants of HIV self-testing as assessed by univariate and multivariate regression
Items Unadjusted OR(CI) P-value Adjusted OR(CI) P-value Age (years) 18-24 1.00 1.00 25-29 1.27 (1.11-1.45) < 0.001 0.94 (0.78-1.13) 0.495 ≥ 30 1.08 (0.95-1.23) 0.233 0.69 (0.57-0.83) < 0.001 Employment status Unemployed or part-time 1.00 - Student 0.84 (0.64-1.11) 0.221 - - Full-time 1.07 (0.84-1.36) 0.609 - - Monthly income (CNY) ≤ 1, 500 1.00 1.00 1, 501-5, 000 1.25 (1.02-1.5) 0.029 1.18 (0.89-1.55) 0.245 5, 001-10, 000 1.34 (1.10-1.64) 0.004 1.13 (0.85-1.50) 0.403 > 10, 000 1.69 (1.37-2.08 < 0.001 1.49 (1.10-2.02) 0.010 Marital status Married 1.00 - Unmarried 1.24 (1.07-1.44) 0.004 - - Cohabitation status Alone 1.00 - Cohabitating 0.79 (0.71-0.89) < 0.001 - - Sexual orientation Homosexual 1.00 1.00 Bisexual 0.83 (0.74-0.94) 0.002 0.85 (0.73-0.99) 0.034 Unknown/unsure 0.18 (0.07-0.52) 0.002 0.36 (0.11-1.21) 0.098 Role in sexual intercourse Anal receptive 1.00 1.00 Anal insertive 1.22 (1.05-1.42) 0.011 1.37 (1.12-1.68) 0.002 Both 1.18 (1.03-1.34) 0.014 1.34 (1.13-1.59) 0.001 Number of male sex partners 0 1.00 - 1 1.29 (1.13-1.47) < 0.001 1.00 ≥ 2 1.94 (1.70-2.21) < 0.001 1.24 (1.09-1.43) 0.002 Condom use with latest male sex partner Yes 1.00 - No 0.77 (0.67-0.90) 0.001 - - Condom use with male sex partner Always 1.00 - Ever 1.03 (0.90-1.18) 0.678 - - Never 0.66 (0.53-0.83) < 0.001 - - Number of commercial male sex partner 0 1.00 1.00 1 1.13 (0.88-1.44) 0.339 1.18 (0.88-1.59) 0.258 ≥ 2 2.05 (1.48-2.83) < 0.001 1.94 (1.34-2.82) 0.001 Sought healthcare for STI symptoms No 1.00 - Yes 1.28 (1.07-1.53) 0.006 - - Drug use ever in lifetime No 1.00 1.00 Yes 1.93 (1.73-2.15) < 0.001 1.42 (1.23-1.62) < 0.001 HIV VCT attendance Ever in lifetime 3.85 (3.42-4.35) < 0.001 3.62 (3.11-4.22) < 0.001 Never in lifetime 1.00 1.00 Willingness to use an HIV self-test kit in the future Willing 1.00 1.00 Unwilling 0.26 (0.20-0.34) < 0.001 0.20 (0.15-0.28) < 0.001 -
Our study revealed a nearly 40% rate of HIV self-testing uptake among MSM in Beijing. Furthermore, although not a primary aim of the study, we found a very high rate of willingness to use HIV self-test kits in the future -92% among all participants and 97% among those who had never used self-test kits in their lifetimes. Factors associated with increased odds of HIV self-test kit use were higher monthly income, greater number of male sex partners and commercial male sex partners, lifetime drug use, and lifetime HIV VCT attendance. Factors associated with decreased odds of self-testing uptake were older age and being unwilling to use an HIV self-test kit in the future.
These findings add to a small, but growing literature on HIV self-testing among MSM in China. Two recent qualitative studies of HIV testing barriers and facilitators among Chinese MSM have suggested that rapid HIV self-testing would be considered very desirable for this key population[9-10]. An online survey of MSM in Guangdong and Chongqing found that 20% had taken an HIV self-test in their lifetime. Factors associated with lifetime self-testing were being married, having at least six male sex partners in the prior three months, having tested for HIV in the last year, having an annual income greater than 16, 000 USD, and having a history of STI testing[18]. A subsequent study in Guangdong and Chongqing conducted by the same research team found that in-home testing was highly preferred-57% of participants rated it 'very acceptable' and 75% 'very important' or 'quite important'[17]. A study in Beijing found more than 80% of participants to be willing to use oral fluid HIV self-test kits[16]. A study among MSM in Jiangsu Province, found that 27% had used HIV self-test kits and factors associated with having self-tested were having had more than two male sexual partners in the prior six months, having tested for HIV before, and having friends who had self-tested[19]. Lastly, an online survey of MSM in Hong Kong, China found only a 6% rate of HIV self-test kit uptake and a moderate 44% rate of acceptability, with factors associated with use and acceptability being knowledge of and attitudes toward HIV self-testing[20].
The rate of HIV self-testing uptake and willingness observed in our study was higher than in prior studies, which may be an indication of a growth in knowledge of and experience with these products among MSM in China. However, the very low uptake and acceptability observed in the Hong Kong, China study[20] was likely due to HIV self-testing kits not having been authorized for sale over the counter. Like the Guangdong and Chongqing study[18] as well as the Jaingsu study[19], we found greater odds of self-testing uptake among those who engaged in higher risk behavior, had prior testing experience, and had higher incomes.
Our results are further supported by evidence from settings outside of China. A recent literature review of HIV self-testing among key populations found a high degree of acceptability of HIV self-testing among MSM across a range of mostly high-income country (HIC) settings[22]. The review also found higher willingness to pay for HIV self-testing kits among studies conducted in HIC compared to low-and middle income countries (LMIC)[22]. This, together with the findings presented here that higher income is associated with increased odds of test uptake and high price as a determinant of uptake suggests that kit cost may be an important factor to consider in the development of interventions meant to drive HIV self-testing uptake. Another important factors to be considered are quality and reliability of the kit and the impact of user's errors on the results[23]. Although other studies found that the majority of self-test kit users were able to use the products correctly with little or no support[23] and that participants could successfully perform the HIV self-test procedure after watching an online instructional video[22], the participants in our study identified difficult operation (17%), difficult result interpretation (25%), and quality concerns (57%) as major disadvantages to HIV self-testing[11].
HIV self-testing can be the key to moving China toward meeting the UNAIDS 90-90-90 targets[2]. Self-testing can provide the convenient, confidential, and cost-effective solution to the current testing coverage gaps, particularly for stigmatized and hidden populations like MSM. However, barriers (or perceived barriers) to HIV self-testing uptake, including high cost, concerns about quality and reliability, and difficulty of kit operation and results interpretation, will need to be quickly and effectively addressed.
-
This study had several limitations. Firstly, the participants were all users of a gay networking App. While there were fifteen million registered users of the App in 2015, it did not cover all MSM in Beijing and thus affecting the generalizability of the study. There is also the possibility that the App users were not MSM. Secondly, despite implemented quality control measures, the online nature of the survey leaves for possibility of incomplete or untruthful information. Thirdly, since this was a cross-sectional study, causality could not be assessed.
-
Our study provides evidence of a nearly 40% rate of uptake of HIV self-testing among MSM in Beijing. It is very encouraging that over 92% of MSM in our sample and 96% of those who had never used HIV self-test kits in the past reported willingness to use them in the future. HIV self-testing could become a major contributor to improving testing rates in China, particularly among vulnerable and hidden populations like MSM. We call on HIV self-testing kit manufacturers to simplify testing procedures and instructions of use and on Chinese authorities to regulate HIV self-testing kits, so consumers can be more confident in product quality and reliability.
doi: 10.3967/bes2017.054
Uptake of HIV Self-testing among Men Who have Sex with Men in Beijing, China:a Cross-sectional Study
-
Abstract:
Objective To examine HIV self-testing uptake and its determinates among men who have sex with men (MSM) in Beijing, China. Methods A cross-sectional online survey was conducted in Beijing, China in 2016. Participants were users of a popular Chinese gay networking application and had an unknown or negative HIV status. Univariate and multivariate logistic regression analyses were conducted to examine factors associated with HIV self-testing based on adjusted odds ratio (AOR) and 95% confidence interval (CI). Results Among the 5, 996 MSM included in the study, 2, 383 (39.7%) reported to have used HIV self-testing kits. Willingness to use an HIV self-test kit in the future was expressed by 92% of the participants. High monthly income (AOR=1.49; CI=1.10-2.02; P=0.010), large number of male sex partners (≥ 2:AOR=1.24; CI=1.09-1.43; P=0.002), sexual activity with commercial male sex partners (≥ 2:AOR=1.94; CI=1.34 -2.82; P=0.001), long-term drug use (AOR=1.42; CI=1.23-1.62; P < 0.001), and long-term HIV voluntary counseling and testing (VCT) attendance (AOR=3.62; CI=3.11-4.22; P < 0.001) were all associated with increased odds of HIV self-testing uptake. Conclusion The nearly 40% rate of HIV self-testing uptake among MSM in our sample was high. In addition, an over 90% willingness to use kits in the future was encouraging. HIV self-testing could be an important solution to help China achieve the global target of having 90% of all people living with HIV diagnosed by 2020. -
Key words:
- Men who have sex with men /
- HIV self-testing; Associated factors /
- Beijing
注释:1) COMPETING INTERESTS: 2) AUTHOR CONTRIBUTIONS: -
Table 1. Characteristics of the Participants
Items All Participants [N = 5, 996] n(%) 'Self-Testers' [N = 2, 383] n(%) 'Non-Self-Testers' [N = 3, 613] n(%) P-value Demographic Characteristics Age (years) 0.001 18-24 1, 746 (29.1) 649 (27.2) 1, 097 (30.4) 25-29 1, 961 (32.7) 841 (35.3) 1, 120 (31.0) ≥ 30 2, 289 (38.2) 893 (37.5) 1, 396 (38.6) Ethnicity 0.12 Han 5, 524 (92.1) 2, 199 (92.3) 3, 325 (92.0) Minority 472 (7.9) 184 (7.7) 288 (8.0) Education level 0.76 ≤ High schoola 1, 247 (20.8) 499 (20.9) 748 (20.7) College 3, 795 (63.3) 1, 515 (63.6) 2, 280 (63.1) ≥ Graduate school 954 (15.9) 369 (15.5) 585 (16.2) Employment status 0.007 Unemployed or part-time 291 (4.9) 114(4.8) 177 (4.9) Student 962 (16.0) 339 (14.2) 623 (17.2) Full-time 4, 743 (79.1) 1, 930 (81.0) 2, 813 (77.9) Monthly Income (CNY) < 0.001 ≤ 1, 500 554 (9.3) 183 (7.7) 371 (10.3) 1, 501-5, 000 2, 139 (35.7) 814 (34.2) 1, 325 (36.7) 5, 001-10, 000 2, 034 (33.9) 810 (34.0) 1, 224 (33.9) > 10, 000 1, 269 (21.2) 576 (24.2) 693 (19.2) Duration of residence in Beijing (years) 0.30 < 2 1, 746 (29.1) 676 (28.4) 1, 070 (29.6) ≥ 2 4, 250 (70.9) 1, 707 (71.6) 2, 543 (70.4) Marital status 0.004 Married 885 (14.8) 313 (13.1) 572 (15.8) Unmarried 5, 111 (85.2) 2, 070 (86.9) 3, 041 (84.2) Cohabitation status < 0.001 Alone 1, 956 (32.6) 851 (35.7) 1, 105 (30.6) Cohabitatingb 4, 040 (67.4) 1, 532 (64.3) 2, 508 (69.4) Sexual orientation < 0.001 Homosexual 4, 318 (72.0) 1, 775 (74.5) 2, 543 (70.4) Bisexual 1, 643 (27.4) 604 (25.3) 1, 039 (28.8) Unknown/unsure 35 (0.6) 4 (0.2) 31 (0.9) Sexual Behavior Characteristics Method for finding sex partners 0.11 Internet or mobile Apps 5, 255 (87.6) 2, 088 (87.6) 3, 167 (87.7) Parties 288 (4.8) 129 (5.4) 159 (4.4) Other 453 (7.6) 166 (7.0) 287 (7.9) Age at sexual debut with male (years) 0.17 < 18 1, 209 (20.2) 498 (20.9) 711 (19.7) 18-29 4, 328 (72.2) 1, 719 (72.1) 2, 609 (72.2) ≥ 30 459 (7.7) 166 (7.0) 293 (8.1) Role in sexual intercourse 0.02 Anal receptive 1, 396 (23.3) 511 (21.4) 885 (24.5) Anal insertive 1, 338 (22.3) 553 (23.2) 785 (21.7) Both 3, 262 (54.4) 1, 319 (55.4) 1, 943 (53.8) Number of male sex partnersc < 0.001 0 1, 856 (31.0) 600 (25.2) 1, 256 (34.8) 1 2, 091 (34.9) 797 (33.4) 1, 294 (35.8) ≥ 2 2, 049 (34.2) 986 (41.4) 1, 063 (29.4) Condom use with latest male sex partner 0.001 Yes 3, 157 (76.3) 1, 406 (78.9) 1, 751 (74.3) No 983 (23.7) 377 (21.1) 606 (25.7) Missing (no male sex partners) 1, 856 - - Condom use with male sex partnersc < 0.001 Never 410 (9.9) 140 (7.9) 270 (11.5) Ever 1, 208 (29.2) 538 (30.2) 670 (28.4) Always 2, 522 (60.9) 1, 105 (62.0) 1, 417 (60.1) Missing (no male sex partners) 1, 856 - - Number of commercial male sex partnersc < 0.001 0 5, 572 (92.9) 2, 182 (91.6) 3, 390 (93.8) 1 271 (4.5) 114 (4.8) 157 (4.3) ≥ 2 153 (2.6) 87 (3.7) 66 (1.8) Condom use with latest commercial male sex partner 0.68 Yes 336 (79.2) 161 (80.1) 175 (78.5) No 88 (20.8) 40 (19.9) 48 (21.5) Missing (no commercial male sex partners) 5, 572 - - Condom use with commercial male sex partnersc 0.22 Never 43 (10.1) 18 (9.0) 25 (11.2) Ever 97 (22.9) 40 (19.9) 57 (25.6) Always 284 (67.0) 143 (71.1) 141 (63.2) Missing (no commercial male sex partners) 5, 572 - - Number of female sex partnersc 0.33 0 5, 265 (87.8) 2, 089 (87.7) 3, 176 (87.9) 1 656 (10.9) 258 (10.8) 398 (11.0) ≥ 2 75 (1.3) 36 (1.5) 39 (1.1) Condom use with latest female partner 0.002 Yes 404 (55.3) 183 (62.2) 221 (50.6) No 327 (44.7) 111 (37.8) 216 (49.4) Missing (no female sex partners) 5, 265 - - Condom use with female partnerc 0.002 Never in lifetime 263 (36.0) 83 (28.2) 180 (41.2) Ever in lifetime 153 (20.9) 69 (23.5) 84 (19.2) Always 315 (43.1) 142 (48.3) 173 (39.6) Missing (no female sex partners) 5, 265 - - Sexual Health Characteristics Sought healthcare for STI symptomsd 0.006 Yes 541 (9.0) 245 (10.3) 296 (8.2) No 5, 455 (91.0) 2, 138 (89.7) 3, 317 (91.8) Results of the latest STI testing 0.48 Gonorrhea 34 (6.3) 16 (6.5) 18 (6.1) Syphilis 164 (30.3) 82 (33.5) 82 (27.7) Chlamydial trachomatis 29 (5.4) 16 (6.5) 13 (4.4) Condyloma acuminate 128 (23.7) 54 (22.0) 74 (25.0) Herpes progenitalis 31 (5.7) 14 (5.7) 17 (5.7) Other 155 (28.7) 63 (25.7) 92 (31.1) Missing (did not seek healthcare) 5, 455 - - Drug Use Behavior Characteristics Drug use ever in lifetime < 0.001 Yes 2, 171 (36.2) 1, 082 (45.4) 1, 089 (30.1) No 3, 825 (63.8) 1, 301 (54.6) 2, 524 (69.9) Anal sex after drug use 0.63 Yes 1, 852 (85.3) 927 (85.7) 925 (84.9) No 319 (14.7) 155 (14.3) 164 (15.1) Missing (no drug use) 3, 825 - - Condom use after drug use 0.03 Never 127 (6.9) 54 (5.8) 73 (7.9) Ever 477 (25.8) 260 (28.0) 217 (23.5) Always 1, 248 (67.4) 613 (66.1) 635 (68.6) Missing (no drug use) 3, 825 - - History of HIV VCT HIV VCT attendance < 0.001 Ever in lifetime 3, 772 (62.9) 1, 914 (80.3) 1, 858 (51.4) Never in lifetime 2, 224 (37.1) 469 (19.7) 1, 755 (48.6) Time since latest HIV VCT (months) < 0.001 ≤ 3 1, 379 (36.6) 786 (41.1) 593 (31.9) 4-6 740 (19.6) 360 (18.8) 380 (20.5) 7-12 539 (14.3) 258 (13.5) 281 (15.1) ≥ 13 1, 114 (29.5) 510 (26.6) 604 (32.5) Missing (never in lifetime) 2, 224 - - Consultation during latest HIV VCT 0.005 Yes 2, 123 (56.3) 1, 101 (57.5) 1, 022 (55.0) No 1, 037 (27.5) 483 (25.2) 554 (29.8) Can't remember 612 (16.2) 330 (17.2) 282 (15.2) Missing (never in lifetime) 2, 224 - - Site of the latest HIV VCT < 0.001 CDC 1, 343 (35.6) 696 (36.4) 647 (34.8) Hospital 1, 328 (35.2) 559 (29.2) 769 (41.4) Blood donation station 111 (2.9) 70 (3.7) 41 (2.2) NGO 792 (21.0) 423 (22.1) 369 (19.9) Others 198 (5.2) 166 (8.7) 32 (1.7) Missing (never in lifetime) 2, 224 - - HIV Self-testing Knowledge and Attitudes Sources of information on HIV self-testinge Mobile Apps 3, 670 (61.2) 1, 269 (53.3) 2, 401 (66.5) Posters 1, 552 (25.9) 617 (25.9) 935 (25.9) Consultation with medical professionals 1, 090 (18.2) 555 (23.3) 535 (14.8) Friends 1, 556 (26.0) 787 (33.0) 769 (21.3) Websites 2, 668 (44.5) 1, 026 (43.1) 1, 642 (45.4) Other 79 (1.3) 43 (1.8) 36 (1.0) Willingness to use an HIV self-test kit in the future < 0.001 Willing 5, 535 (92.3) 2, 310 (96.9) 3, 225(89.3) Unwilling 461 (7.7) 73 (3.1) 388 (10.7) Best feature of HIV self-testing < 0.001 Easy to purchase 151 (2.5) 79 (3.3) 72 (2.0) Simple operation 967 (16.1) 449 (18.8) 518 (14.3) Protection of privacy 3, 307 (55.2) 1, 203 (50.5) 2, 104 (58.2) Convenient 1, 538 (25.7) 643 (27.0) 895 (24.8) Other 33 (0.6) 9 (0.4) 24 (0.7) Disadvantages of HIV self-testinge Difficult to obtain 2, 143 (35.7) 772 (32.4) 1, 371 (37.9) Lack of consultation 1, 765 (29.4) 584 (24.5) 1, 181 (32.7) Difficult operation 1, 004 (16.7) 365 (15.3) 639 (17.7) Difficult results interpretation 1, 507 (25.1) 491 (20.6) 1, 016 (28.1) High price 1, 385 (23.1) 631 (26.5) 754 (20.9) Quality concerns 3, 438 (57.3) 1, 269 (53.3) 2, 169 (60.0) Other 187 (3.1) 76 (3.2) 111 (3.1) Note.CNY: Chinese Yuan; CDC: Centers for Disease Control; NGO: non-government organization; STI: sexually-transmitted infection; VCT: voluntary counseling and HIV testing. aThe category 'High School' includes also vocational or technical school. bThe category 'Cohabitating' includes those who live with their spouse, roommate, or other. cThese sexual behavior characteristics were limited to the prior 3 months. dSeeking healthcare for STI symptoms was limited to the last year. eFor these two variables, more than one response was allowed in the survey. No statistical comparison was performed for these variables. 'Self-testers' indicates those who had used HIV self-testing and 'non-self-testers' those who had never used HIV self-testing. Table 2. Determinants of HIV self-testing as assessed by univariate and multivariate regression
Items Unadjusted OR(CI) P-value Adjusted OR(CI) P-value Age (years) 18-24 1.00 1.00 25-29 1.27 (1.11-1.45) < 0.001 0.94 (0.78-1.13) 0.495 ≥ 30 1.08 (0.95-1.23) 0.233 0.69 (0.57-0.83) < 0.001 Employment status Unemployed or part-time 1.00 - Student 0.84 (0.64-1.11) 0.221 - - Full-time 1.07 (0.84-1.36) 0.609 - - Monthly income (CNY) ≤ 1, 500 1.00 1.00 1, 501-5, 000 1.25 (1.02-1.5) 0.029 1.18 (0.89-1.55) 0.245 5, 001-10, 000 1.34 (1.10-1.64) 0.004 1.13 (0.85-1.50) 0.403 > 10, 000 1.69 (1.37-2.08 < 0.001 1.49 (1.10-2.02) 0.010 Marital status Married 1.00 - Unmarried 1.24 (1.07-1.44) 0.004 - - Cohabitation status Alone 1.00 - Cohabitating 0.79 (0.71-0.89) < 0.001 - - Sexual orientation Homosexual 1.00 1.00 Bisexual 0.83 (0.74-0.94) 0.002 0.85 (0.73-0.99) 0.034 Unknown/unsure 0.18 (0.07-0.52) 0.002 0.36 (0.11-1.21) 0.098 Role in sexual intercourse Anal receptive 1.00 1.00 Anal insertive 1.22 (1.05-1.42) 0.011 1.37 (1.12-1.68) 0.002 Both 1.18 (1.03-1.34) 0.014 1.34 (1.13-1.59) 0.001 Number of male sex partners 0 1.00 - 1 1.29 (1.13-1.47) < 0.001 1.00 ≥ 2 1.94 (1.70-2.21) < 0.001 1.24 (1.09-1.43) 0.002 Condom use with latest male sex partner Yes 1.00 - No 0.77 (0.67-0.90) 0.001 - - Condom use with male sex partner Always 1.00 - Ever 1.03 (0.90-1.18) 0.678 - - Never 0.66 (0.53-0.83) < 0.001 - - Number of commercial male sex partner 0 1.00 1.00 1 1.13 (0.88-1.44) 0.339 1.18 (0.88-1.59) 0.258 ≥ 2 2.05 (1.48-2.83) < 0.001 1.94 (1.34-2.82) 0.001 Sought healthcare for STI symptoms No 1.00 - Yes 1.28 (1.07-1.53) 0.006 - - Drug use ever in lifetime No 1.00 1.00 Yes 1.93 (1.73-2.15) < 0.001 1.42 (1.23-1.62) < 0.001 HIV VCT attendance Ever in lifetime 3.85 (3.42-4.35) < 0.001 3.62 (3.11-4.22) < 0.001 Never in lifetime 1.00 1.00 Willingness to use an HIV self-test kit in the future Willing 1.00 1.00 Unwilling 0.26 (0.20-0.34) < 0.001 0.20 (0.15-0.28) < 0.001 -
[1] UNAIDS. Prevention Gap Report. Geneva: UNAIDS; 2016. [2] UNAIDS. 90-90-90 An ambitious treatment target to help end the AIDS epidemic. Geneva: UNAIDS; 2014. [3] International Association of Providers of AIDS Care. Global HIV 90-90-90 Watch. Washington DC: International Association of Providers of AIDS Care; 2016. [4] NCAIDS, NCSTD. 2015 National Annual Reports on HIV/AIDS/STD/hepatitis Prevention and Treatment. Beijing: China CDC/NCAIDS; 2015. [5] Wu Z, Sullivan SG, Wang Y, et al. Evolution of China's response to HIV/AIDS. Lancet (London, England), 2007; 369, 679-90. doi: 10.1016/S0140-6736(07)60315-8 [6] National Health and Family Planning Commission of the People's Republic of China. 2015 China AIDS response progress report. May, 2015 ed. Beijing: UNAIDS; 2015. [7] Tang S, Tang W, Meyers K, et al. HIV epidemiology and responses among men who have sex with men and transgender individuals in China: a scoping review. BMC Infect Dis, 2016; 16, 588. doi: 10.1186/s12879-016-1904-5 [8] Zou H, Hu N, Xin Q, et al. HIV testing among men who have sex with men in China: a systematic review and meta-analysis. AIDS and behavior, 2012; 16, 1717-28. doi: 10.1007/s10461-012-0225-y [9] Liu Y, Sun X, Qian HZ, et al. Qualitative Assessment of Barriers and Facilitators of Access to HIV Testing Among Men Who Have Sex with Men in China. AIDS patient care and STDs, 2015; 29, 481-9. doi: 10.1089/apc.2015.0083 [10] Wei C, Yan H, Yang C, et al. Accessing HIV testing and treatment among men who have sex with men in China: a qualitative study. AIDS care, 2014; 26, 372-8. doi: 10.1080/09540121.2013.824538 [11] Tao J, Li MY, Qian HZ, et al. Home-based HIV testing for men who have sex with men in China: a novel community-based partnership to complement government programs. PLoS One, 2014; 9, e102812. doi: 10.1371/journal.pone.0102812 [12] UNITAID. Technology landscape HIV rapid diagnostic tests for self-testing. 2nd ed. Geneva: UNITAID; 2016. [13] Estem KS, Catania J, Klausner JD. HIV Self-Testing: a Review of Current Implementation and Fidelity. Curr HIV/AIDS Rep, 2016; 13, 107-15. doi: 10.1007/s11904-016-0307-y [14] WHO, UNAIDS, Brocher Foundation, LSTM. Report on the first international symposium on self-testing for HIV: The legal, ethical, gender, human rights and public health implications of self-testing scale-up. Meeting report -Geneva, Switzerland. 8-9 April 2013. Geneva: WHO; 2013. [15] Xun H, Kang D, Huang T, et al. Factors associated with willingness to accept oral fluid HIV rapid testing among most-at-risk populations in China. PLoS One, 2013; 8, e80594. doi: 10.1371/journal.pone.0080594 [16] Xu Y, Zhang Z, Li D, et al. Willingness to use the oral fluid HIV rapid test among men who have sex with men in Beijing, China. PLoS One, 2013; 8, e64652. doi: 10.1371/journal.pone.0064652 [17] Han L, Wei C, Muessig KE, et al. HIV test uptake among MSM in China: Implications for enhanced HIV test promotion campaigns among key populations. Glob Public Health, 2016; 1-14. http://www.popline.org/node/657968 [18] Han L, Bien CH, Wei C, et al. HIV self-testing among online MSM in China: implications for expanding HIV testing among key populations. J Acquir Immune Defic Syndr, 2014; 67, 216-21. doi: 10.1097/QAI.0000000000000278 [19] Yan H, Yang H, Raymond HF, et al. Experiences and correlates of HIV self-testing among men who have sex with men in Jiangsu province, China. AIDS and Behavior, 2015, 19, 485-91. doi: 10.1007/s10461-014-0968-8 [20] Wong HT, Tam HY, Chan DP, et al. Usage and acceptability of HIV self-testing in men who have sex with men in Hong Kong. AIDS and Behavior, 2015; 19, 505-15. doi: 10.1007/s10461-014-0881-1 [21] Zhong F, Tang W, Cheng W, et al. Acceptability and feasibility of a social entrepreneurship testing model to promote HIV self-testing and linkage to care among men who have sex with men. HIV Med, 2017; 18, 376-82. doi: 10.1111/hiv.2017.18.issue-5 [22] Figueroa C, Johnson C, Verster A, et al. Attitudes and Acceptability on HIV Self-testing Among Key Populations: A Literature Review. AIDS and Behavior, 2015; 19, 1949-65. doi: 10.1007/s10461-015-1097-8 [23] Krause J, Subklew-Sehume F, Kenyon C, et al. Acceptability of HIV self-testing: a systematic literature review. BMC Public Health, 2013; 13, 735. doi: 10.1186/1471-2458-13-735 -




 下载:
下载:



 Quick Links
Quick Links