-
Pneumoconiosis is a group of occupational lung diseases caused by long-term inhalation of different pathogenic industrial dust particles; its main pathological feature is diffuse lung fibrosis[1]. With silicosis being its primary type, pneumoconiosis is the most serious and common occupational disease in China, accounting for 88.3% of all reported occupational diseases[2]. Patients with pneumoconiosis may suffer from serious diseases, such as lung tuberculosis, and require lifelong disease management[3]. The therapeutic principle for pneumoconiosis requires comprehensive health management and aggressive therapy, including oxygen therapy, pulmonary rehabilitation, and symptomatic therapy.
Prior to the Chinese economic reform, pneumoconiosis mainly occurred in state-owned enterprises. Patients either had employment injury insurance or free medical service. Then, a large number of migrant workers began to be employed in industries such as mining, smelting production, and asbestos processing, mostly in small-size enterprises. After several years of exposure to dust, some of these workers developed pneumoconiosis[4]. Because of the low insured rate of industrial injury insurance and the lack of labor contracts and documented occupational history, the migrant workers who developed pneumoconiosis were less likely to be covered by industrial injury insurance and rarely received compensation from the work unit. With the aggravation of the illness, they lost the ability to work and their savings because of the substantial medical costs they had to shoulder. However, reports on the health service utilization of patients with pneumoconiosis are rare.
Recently, health care utilization inequity has become a progressively popular research topic[5]. China has conducted the National Health Services Survey every five years since 1993, with a focus on the utilization of the country’s medical services. The results of follow-up studies have been widely used in the scientific management and decision-making of health administrative departments in China. Previous results have also had an important impact on the allocation of health resources, regulation of the relation between supply and demand of health services, and health administration improvement by policymakers[6]. However, the treatment and rehabilitation of occupational diseases, especially pneumoconiosis, are not included in this survey. To protect the health rights and interests of patients with pneumoconiosis, we initiated a follow-up survey on the treatment and rehabilitation of pneumoconiosis in 2017, focusing on health service utilization among patients with pneumoconiosis. However, owing to funding and time constraints, we could not use random sampling. Instead, we conducted a stratified sampling survey in occupational health hospitals, occupational disease screening clinics where patients were relatively concentrated, and towns with high morbidity of pneumoconiosis. The survey was carried out in hospitals in Guizhou, Hebei, Hubei, Hunan, Jiangsu, Jilin, Shandong, Yunnan, and Zhejiang Provinces. The respondents were recruited from inpatient and outpatient departments, physical screening, and household surveys. The patients with pneumoconiosis were selected based on their previous diagnosis according to the Diagnosis of occupational pneumoconiosis criterion (GBZ70-2015). The exclusion criteria were as follows: 1) those with mental and behavioral disorders; 2) those who could not understand the contents of the questionnaire well for various reasons; 3) those who did not provide informed consent. The inpatient respondents were selected by stratified sampling according to pneumoconiosis stage, disease severity, and occupational injury insurance. Outpatient or physical screening respondents were clinically diagnosed. Household survey respondents were surveyed from villages and towns where pneumoconiosis cases were concentrated. Finally, a total of 1,100 patients were selected, and the effective questionnaire return ratio was 94.3%.
Well-trained investigators used the questionnaire we prepared for investigating all respondents. The questionnaire included sociodemographic characteristics (e.g., age, educational level, monthly income), dust exposure history, disease characteristics (e.g., pneumoconiosis classification, pneumoconiosis stage, dyspnea, sputum expectoration, self-health score), and social security status. Pneumoconiosis in China is diagnosed based on the GBZ70-2015. A patient diagnosed with pneumoconiosis receives a diagnosis certificate, which helps in the verification of an individual’s diagnosis. Based on radiographic results, pneumoconiosis is divided into three phases, which correspond with disease severity. Phase three represents the worst severity, identified when an X-ray chest film shows more than one large shadow. We classified the outpatient institutions as village clinic, town-level health service center, county-level hospital, city-level hospital, or province-level hospital. Regions were classified as western, central, or eastern. Current residence was divided into rural or urban areas. Education level was classified as primary school, middle school, high school and above, others, or illiterate. The survey method was classified as household, outpatient, or hospitalization survey. We defined the health service utilization of patients the behavior of choosing medical institutions in seeking medical help and utilizing medical services, manifested by the proportion of patients visiting medical institutions at all levels. The study was approved by the Ethics Committee of the Institute of Occupational Health and Poisoning Control of Chinese Center for Disease Control and Prevention. Each respondent provided their signed informed consent.
We used Epidata 3.1 to build a database with a double entry method. SPSS 22.0 was used for error detection and statistical analysis. The continuous variables were described by mean and standard deviation values, and the categorical variables were expressed as frequency and percentage values. We conducted a Chi-squared test to evaluate the association between the factors and health service utilization of patients. To analyze the effect of different factors on the health service utilization of patients with pneumoconiosis, we selected as dependent variables the five types of institutions, namely, village clinic, township hospitals/health service center, county-level hospital, city-level hospital, and province-level hospital. The statistically significant factors shown by single-factor analysis were selected as independent variables in the multinomial logistic regression analysis. P < 0.05 was considered as significant.
Among the 1,037 pneumoconiosis patients in this study, 1,029 (99.2%) were men. The average age of the respondents was 55.9 ± 11.2 years. About 70% of the respondents were patients with silicosis, and 21.9% were coal workers, among whom 35.3%, 23.9%, and 31.4% were patients with phases one, two, and three pneumoconiosis, respectively. Moreover, 71.5% of the respondents living in urban areas had occupational injury insurance, 65% had urban employee medical insurance (UEMI), 27.3% had urban and rural residents’ medical insurance (URRMI). Meanwhile, 26.1% of the respondents living in rural areas had occupational injury insurance, 14.7% had UEMI, and 74.9% had URRMI. Other sociodemographic characteristics are presented in Table 1 and Supplementary Table S1 available in www.besjournal.com.
Table 1. Basic characteristics of pneumoconiosis patients in rural and urban areas
Variables Categories Rural areas (n = 700) Urban areas (n = 337) All (n = 1,037) n % n % n % Gender* Male 698 99.7 331 98.2 1,029 99.2 Female 2 0.3 6 1.8 8 0.8 Age** (year) −35 14 2.0 8 2.4 22 2.1 −45 101 14.4 42 12.5 143 13.8 −55 314 44.9 102 30.3 416 40.1 −65 181 25.9 78 23.1 259 25.0 −75 69 9.9 58 17.2 127 12.2 75− 21 3.0 49 14.5 70 6.8 Education** Illiteracy 91 13.0 40 11.9 131 12.6 Primary school 288 41.1 105 31.2 393 37.9 Middle school 210 30.0 133 39.5 343 33.1 High school and above 42 6.0 55 16.3 97 9.4 Others 69 9.9 4 1.2 73 7.0 Registered residence** Eastern 271 38.7 173 51.3 444 42.8 Central 295 42.1 93 27.6 388 37.4 Western 134 19.1 71 21.1 205 19.8 Nature of work units** State-owned 152 21.7 241 71.5 393 37.9 Collective 110 15.7 29 8.6 139 13.4 Private 384 54.9 56 16.6 440 42.4 Others 54 7.7 11 3.3 65 6.3 Note. *P < 0.05, **P < 0.01. Table S1. Status of sickness and medical social security of pneumoconiosis patients
Variables Categories Rural areas (n = 700) Urban areas (n = 337) All (n = 1,037) n % n % n % Pneumoconiosis types* Silicosis 503 71.9 223 66.2 726 70.0 CWP 152 21.7 75 22.3 227 21.9 Others 45 6.4 39 11.6 84 8.1 Pneumoconiosis grades** Phase one 191 27.3 175 51.9 366 35.3 Phase two 175 25.0 73 21.7 248 23.9 Phase three 262 37.4 64 19.0 326 31.4 Others 72 10.3 25 7.4 97 9.4 Occupational injury insurance** Yes 183 26.1 241 71.5 424 40.9 None 517 73.9 96 28.5 613 59.1 Medical insurance** UEMI 103 14.7 219 65.0 322 31.1 URRMI 524 74.9 92 27.3 616 59.4 CMI 39 5.6 14 4.2 53 5.1 None 34 4.9 12 3.6 46 4.4 Current working status** Retired 129 18.4 203 60.2 332 32.0 Unemployed 356 50.9 54 16.0 410 39.5 Long-term workers 77 11.0 11 3.3 88 8.5 Short-term workers 87 12.4 57 16.9 144 13.9 Others 51 7.3 12 3.6 63 6.1 Note. CWP: coal worker pneumoconiosis. UEMI: urban employee medical insurance. URRMI: rural resident’s medical insurance, including urban resident’s medical insurance and new rural cooperative medical insurance. CMI: commercial medical insurance. *P < 0.05, **P < 0.01. Traffic convenience was the main reason for patients choosing a medical service institution. In detail, the most important reason was the institution’s close distance to home (47.3%), followed by high medical level (27.3%), institutions designated by medical insurance or occupational injury insurance (27.2%), and specialist/expert clinics (26.3%). Rural respondents focused on close distance to home, whereas urban respondents paid more attention to the designation of medical or occupational injury insurance, specialist/expert clinics, good doctor’s attitude, good hospital reputation, and short waiting time. Additional details are given in Supplementary Table S2, available in www.besjournal.com.
Table S2. The reasons for medical service choices of respondents
Reasons Rural areas
(n = 700)Urban areas
(n = 337)All areas
(n = 1,037)χ2 P-value n % n % n % Close to home 218 58.1 50 26.0 268 47.3 52.47 ** High medical level 96 25.6 59 30.7 155 27.3 1.682 Designated institutions for medical insurance or industrial injury insurance 65 17.3 89 46.4 154 27.2 54.06 ** Specialist clinic 81 21.6 68 35.4 149 26.3 12.51 ** Good service attitude 42 11.2 44 22.9 86 15.2 13.55 ** Low hospital expenses 60 16.0 26 13.5 86 15.2 0.596 Hospital have good reputation 27 7.2 26 13.5 53 9.3 6.027 * Recommended from pneumoconiosis 11 2.9 7 3.6 18 3.2 0.210 Short waiting time 6 1.6 11 5.7 17 3.0 7.444 ** Note. *P < 0.05, **P < 0.01. A total of 573 outpatients responded to the type of outpatient department, with a response rate of 95%. The outpatient institutions that were selected most frequently by the respondents were county-(37.5%) and city-level hospitals (25.8%). Compared with urban respondents, rural respondents preferred county-level hospitals, township hospitals/health care centers, and village clinics (χ2 = 66.48, P < 0.01; Supplementary Table S3 available in www.besjournal.com). All factors, except for the self-report health status score, had significant influences on health service utilization (Table 2, Supplementary Tables S3–S5 available in www.besjournal.com). The Year Fifth National Health Service Survey in China showed that 72.8% of the patients selected primary medical and health institutions as their first choice, followed by county-level hospitals. However, we found that patients with pneumoconiosis mainly selected county-level hospitals as their first choice, rather than primary medical institutions.
Table S3. Influence of regional and work factors on the outpatient clinics choices of responders
Variables Categories Cases Village clinic Towns and townships/
health service centersCounty/city/
district hospitalPrefecture/
city hospitalsProvincial
hospitaln % n % n % n % n % Habitual residence** Rural area 380 29 7.6 51 13.4 171 45.0 81 21.3 48 12.6 Urban area 193 2 1.0 16 8.3 44 22.8 67 34.7 64 33.2 Registered residence** Eastern 275 22 8.0 19 6.9 90 32.7 99 36.0 45 16.4 Central 225 8 3.6 39 17.3 98 43.6 39 17.3 41 18.2 Western 73 1 1.4 9 12.3 27 37.0 10 13.7 26 35.6 Unit properties** State-owned 221 7 3.2 15 6.8 62 28.1 63 28.5 74 33.5 Collective 90 11 12.2 11 12.2 30 33.3 29 32.2 9 10.0 Private 224 8 3.6 39 17.4 114 50.9 38 17.0 25 11.2 Others 38 5 13.2 2 5.3 9 23.7 18 47.4 4 10.5 Employment status** Retirement 219 14 6.4 14 6.4 54 24.7 80 36.5 57 26.0 Unemployment 228 11 4.8 37 16.2 109 47.8 44 19.3 27 11.8 Short-term workers 32 1 3.1 4 12.5 18 56.3 7 21.9 2 6.3 Long-term workers 59 2 3.4 7 11.9 23 39.0 10 16.9 17 28.8 Others 35 3 8.6 5 14.3 11 31.4 7 20.0 9 25.7 Total 573 31 5.4 67 11.7 215 37.5 148 25.8 112 19.5 Note. *P < 0.05, **P < 0.01. Table 2. Influence of disease characteristic factors on the outpatient clinics choices of responders
Variables Categories Cases Village clinic Towns and townships/
health service leftsCounty/city/
district hospitalPrefecture/
city hospitalsProvincial
hospitaln % n % n % n % n % Pneumoconiosis types** Silicosis 427 25 5.9 47 11.0 171 40.0 116 27.2 68 15.9 CWP 99 4 4.0 19 19.2 33 33.3 20 20.2 23 23.2 Others 47 2 4.3 1 2.1 11 23.4 12 25.5 21 44.7 Pneumoconiosis grades** Phase one 190 5 2.6 11 5.8 56 29.5 54 28.4 64 33.7 Phase two 140 11 7.9 18 12.9 56 40.0 39 27.9 16 11.4 Phase three 202 15 7.4 33 16.3 86 42.6 46 22.8 22 10.9 Others 41 0 0.0 5 12.2 17 41.5 9 22.0 10 24.4 Dyspnea** Yes 396 27 6.8 50 12.6 157 39.6 90 22.7 72 18.2 No 173 4 2.3 17 9.8 56 32.4 57 32.9 39 22.5 Expectoration** Yes 346 23 6.6 34 9.8 112 32.4 100 28.9 77 22.3 No 223 8 3.6 33 14.8 101 45.3 47 21.1 34 15.2 Self-rating health score 30 93 5 5.4 13 14.0 37 39.8 24 25.8 14 15.1 50 177 13 7.3 23 13.0 69 39.0 41 23.2 31 17.5 70 186 8 4.3 20 10.8 70 37.6 50 26.9 38 20.4 90 97 5 5.2 10 10.3 37 38.1 24 24.7 21 21.6 90- 9 0 0.0 0 0.0 1 11.1 3 33.3 5 55.6 Note. *P < 0.05, **P < 0.01. Table S5. Influence of social demographic factors on the outpatient clinics choices of responders
Variables Categories Cases Village clinic Towns and townships/
health service centersCounty/city/
district hospitalPrefecture/
city hospitalsProvincial hospital n % n % n % n % n % Age (years)** −35 12 0 0.0 1 8.3 6 50.0 3 25.0 2 16.7 −45 71 3 4.2 14 19.7 33 46.5 9 12.7 12 16.9 −55 194 7 3.6 23 11.9 85 43.8 37 19.1 42 21.6 −65 185 15 8.1 19 10.3 55 29.7 66 35.7 30 16.2 66− 111 6 5.4 10 9.0 36 32.4 33 29.7 26 23.4 Education level** Illiteracy 70 4 5.7 17 24.3 31 44.3 5 7.1 13 18.6 Primary school 218 16 7.3 26 11.9 91 41.7 55 25.2 30 13.8 Middle school 179 7 3.9 20 11.2 56 31.3 52 29.1 44 24.6 High school and above 56 1 1.8 1 1.8 18 32.1 15 26.8 21 37.5 Others 50 3 6.0 3 6.0 19 38.0 21 42.0 4 8.0 Monthly income (Yuan)** None 217 18 8.3 36 16.6 86 39.6 57 26.3 20 9.2 −1000 88 7 8.0 15 17.0 46 52.3 12 13.6 8 9.1 −2000 59 3 5.1 7 11.9 26 44.1 10 16.9 13 22.0 −3000 83 2 2.4 5 6.0 19 22.9 19 22.9 38 45.8 −4000 57 0 0.0 0 0.0 20 35.1 19 33.3 18 31.6 4000− 59 1 1.7 4 6.8 18 30.5 25 42.4 11 18.6 Smoke** Current 102 3 2.9 9 8.8 37 36.3 28 27.5 25 24.5 Quit 254 15 5.9 30 11.8 111 43.7 69 27.2 29 11.4 Never 217 13 6.0 28 12.9 67 30.9 51 23.5 58 26.7 Note. *P < 0.05, **P < 0.01. According to the stratification results, we observed significant differences in the selection of different outpatient departments (χ2rural = 53.99, P < 0.01; χ2urban = 29.73, P < 0.01; Supplementary Table S6 available in www.besjournal.com). The proportion of respondents choosing village clinics was higher in the eastern region (12.3%). The proportion of respondents living in the eastern, central, and western regions who chose county-level hospitals (43.8%, 49.4%, and 42.9%, respectively) was higher compared with other hospital types. Respondents from the eastern region preferred city-level hospitals (47.8%), whereas their counterparts in the central and western regions preferred province-level hospitals (40.7% and 38.5%, respectively). Rural respondents chose outpatient institutions in the following descending order: county-level hospitals, city-level hospitals, township hospitals/health service centers, province-level hospitals, and village clinics. In the case of urban respondents, the ranking was as follows: city-level hospitals, province-level hospitals, county-level hospitals, and township hospitals/health service centers. The difference in hospital choices between rural and urban residents could be explained by the inequalities in the distribution of medical resources between rural and urban areas[7]. Most province-level hospitals are located in cities, and most county-level hospitals are in rural areas. The transfer of patients from home to hospital tends to be more difficult in rural and remote areas compared with urban areas. Therefore, the disparity in service utilization is a problem for patients in rural areas, causing inconvenience of traffic and medical insurance reimbursement. Further, we found that patients in rural areas of the eastern region were more likely to select village clinics compared with those in the central and western regions. This tendency may be related to the economic status as well as level of diagnosis and treatment among different regions, or to the difference in local medical reimbursement systems[8].
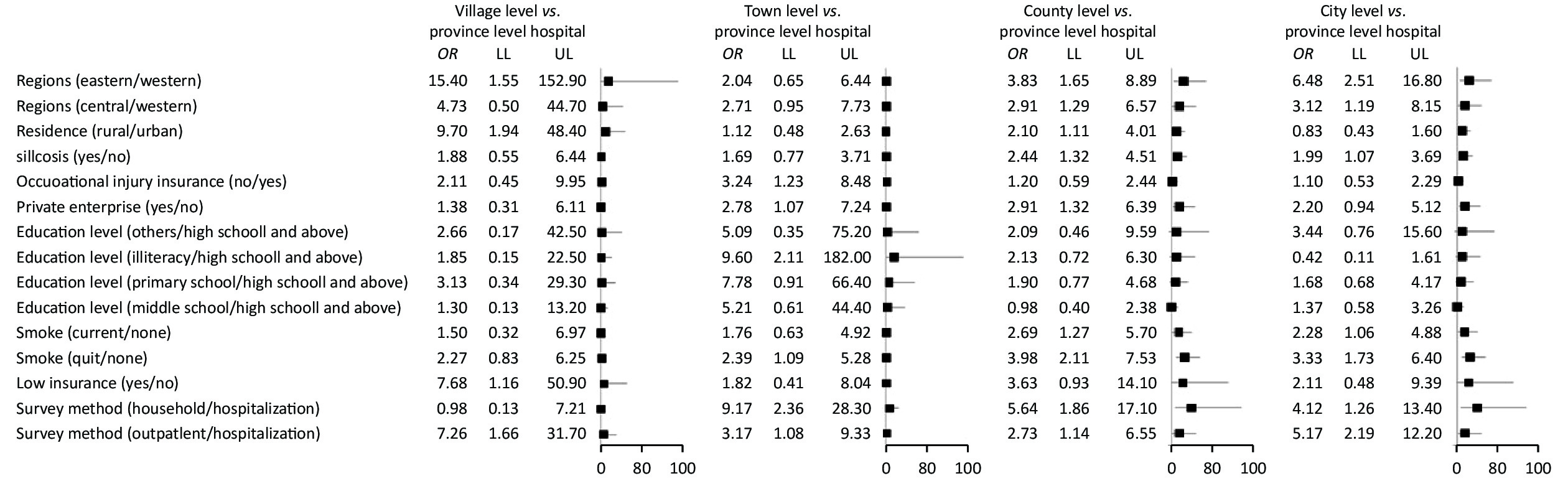
Table S6. Outpatient clinics choices of responders from different regions
Current residence Registered residence Cases Village clinic Towns and townships/
health service centersCounty/city/
district hospitalPrefecture/
city hospitalsProvincial hospital n % n % n % n % n % Rural area Eastern 162 20 12.3 15 9.3 71 43.8 45 27.8 11 6.8 Central 166 8 4.8 30 18.1 82 49.4 29 17.5 17 10.2 Western 52 1 1.9 6 11.5 18 34.6 7 13.5 20 38.5 Subtotal 380 29 7.6 51 13.4 171 45.0 81 21.3 48 12.6 Urban area Eastern 113 2 1.8 4 3.5 19 16.8 54 47.8 34 30.1 Central 59 0 0.0 9 15.3 16 27.1 10 16.9 24 40.7 Western 21 0 0.0 3 14.3 9 42.9 3 14.3 6 28.6 Subtotal 193 2 1.0 16 8.3 44 22.8 67 34.7 64 33.2 Multivariate analysis showed that the factors influencing health service utilization of patients with pneumoconiosis were residence (rural or urban), silicosis diagnosis, occupational injury insurance, employment in private enterprises, education level, social security, and survey methods (Figure 1). The participants who chose the village clinic had the following characteristics: eastern region [odds ratio (OR) = 15.4, 95% confidence interval (CI): 1.55–152.9], rural area residence (OR = 9.70, 95% CI: 1.94–48.4), low insurance (OR = 7.68, 95% CI: 1.16–50.9), and outpatient survey (OR = 7.26, 95% CI: 1.66–31.7). Those who chose township hospitals/health service centers were those who had no occupational injury insurance (OR = 3.24, 95% CI: 1.23–8.48), were illiterate (OR = 19.6, 95% CI: 2.11–182.0), stopped smoking (OR = 2.39, 95% CI: 1.09–5.28), were surveyed at home (OR = 8.17, 95% CI: 2.36–28.3), and were outpatients (OR = 3.17, 95% CI: 1.08–9.33). The participants who chose county-level hospitals were characterized by the following: eastern (OR = 3.83, 95% CI: 1.65–8.89) or central region (OR = 2.91, 95% CI: 129–6.57), rural residence (OR = 2.10, 95% CI: 1.11–4.01), silicosis diagnosis (OR = 2.44, 95% CI: 1.32–4.51), private enterprise employment (OR = 2.91, 95% CI: 1.32–6.39), smoking (OR = 2.69, 95% CI: 1.27–5.70), quit smoking (OR = 3.98, 95% CI: 2.11–7.53), household survey (OR = 5.64, 95% CI: 1.86–17.1), and outpatient survey (OR = 2.73, 95% CI: 1.14–6.55). The characteristics of those who chose the prefectural/municipal hospitals were as follows: eastern region (OR = 6.48, 95% CI: 2.51–16.8), central region (OR = 3.12, 95% CI: 1.19–8.15), silicosis diagnosis (OR = 1.99, 95% CI: 1.07–3.69), smoking (OR = 2.28, 95% CI: 1.06–4.88), quit smoking (OR = 3.33, 95% CI: 1.73–6.40), household survey (OR = 4.12, 95% CI: 1.26–13.4), and outpatient survey (OR = 5.17, 95% CI: 2.19–12.2). Participants from the western region, living in cities and towns, with occupational injury insurance, with no smoking habit, and who were inpatients preferred province-level hospitals.
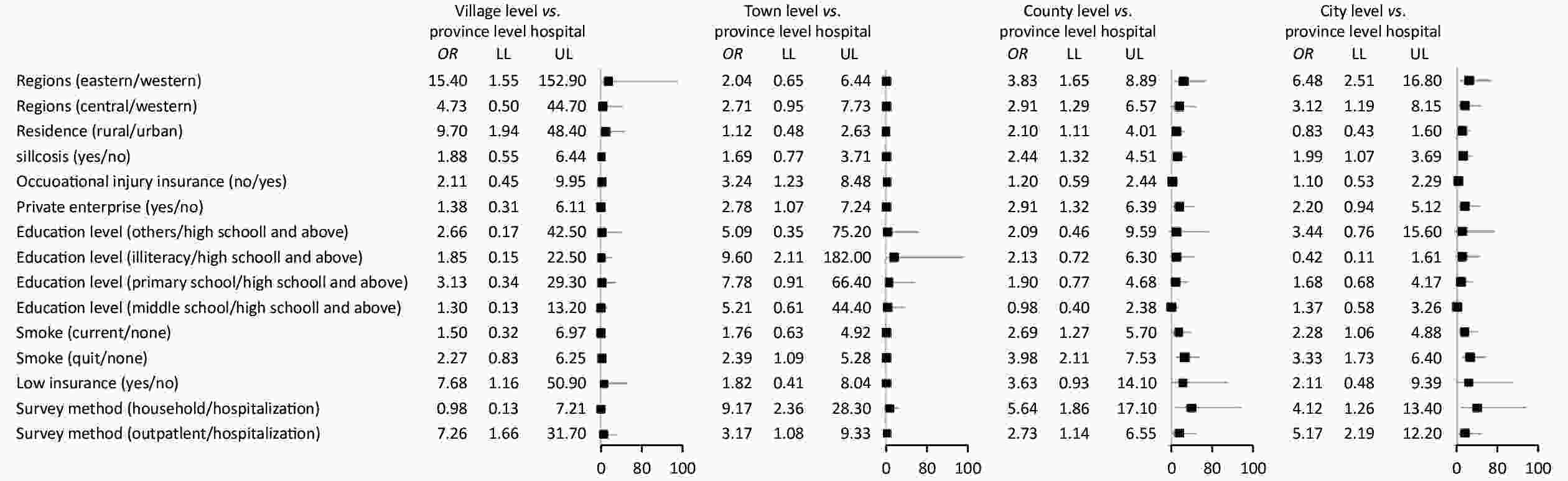
Figure 1. Multiple logistic regression of medical institution selection for pneumoconiosis patients. OR: odds ratio; LL: lower bound of 95% confidence level of OR; UL: upper bound of 95% confidence level of OR
These results coincided with those in previous studies[9]. First, registered residence and habitual residence were closely related to the income of patients with pneumoconiosis, as described above. Those who lived in the eastern region and rural areas preferred rural clinics, because of traffic convenience. Therefore, regional location was an important factor in determining health service utilization. Second, private enterprises in China, compared with state-owned enterprises, provide a lower level of insurance. As such, patients employed in state-owned enterprises would prefer city- and province-level hospitals. Conversely, patients employed in private enterprises would need to spend much of their own money to see a doctor, which would motivate them to choose county-level hospitals. Third, we found that patients with silicosis were more likely to choose county- and city-level hospitals compared with patients with other types of pneumoconiosis. Our findings may be closely related to the characteristics of pneumoconiosis and the distribution of institutions for occupational diseases. In China, most of the hospitals with qualifications for providing occupational disease diagnoses are county- and higher-level institutions, and most of the pneumoconiosis cases are silicosis. Silicosis progresses faster than other types of pneumoconiosis, and as such, patients with silicosis would choose a higher-level hospital for better treatment[10]. Fourth, basic living insurance has some impact on the selection of health service institutions, which might be related to the reimbursement policy in China. Our results also revealed that patients with pneumoconiosis who had a smoking habit tended to choose county- and city-level hospitals. However, reverse causation may also be at play. Smoking cessation may be higher in larger hospitals because they have better programs to help patients; thus, the size may not necessarily be a factor in the choice of hospital for this group of patients with pneumoconiosis.
Our study has a number of strengths and limitations. We were the first to describe the health service utilization of patients with pneumoconiosis based on a national survey in China. Inequity in health service utilization was found to be attributable to region, area of residence, economic status, education, disease severity, and insurance type. However, our study may have some bias owing to the variety in the methods of respondents’ recruitment, as well as to inconsistent quality control for household, outpatient, inpatient, and health examination surveys. Centralized and standardized training are needed in future research. Nonetheless, our results provide a good reference for further investigation on the inequity in health service utilization in China.
Inequity in health service utilization is a major health policy challenge in many low- and middle-income countries, such as China. Our findings were reasonable owing to the difference in health service utilization of patients with pneumoconiosis with different characteristics, such as region, area of residence, economic status, and type of insurance. Therefore, the government should increase financial investment in primary hospitals and the coverage of insurance and primary health care in future, to improve the diagnostic and therapeutic technology of primary hospitals and reduce the pressure on high-level hospitals.
The authors have no conflict of interest to declare.
Table S4. Influence of medical security and survey methods on distribution of outpatient clinics
Variables Categories Cases Village clinic Towns and townships/
health service centersCounty/city/
district hospitalPrefecture/
city hospitalsProvincial hospital n % n % n % n % n % Employment injury insurance** Have 225 4 1.8 11 4.9 68 30.2 67 29.8 75 33.3 None 298 24 8.1 47 15.8 132 44.3 72 24.2 23 7.7 Unclear 50 3 6.0 9 18.0 15 30.0 9 18.0 14 28.0 Medical insurance** UEMI 189 3 1.6 7 3.7 52 27.5 63 33.3 64 33.9 URRMI 338 25 7.4 54 16.0 148 43.8 76 22.5 35 10.4 CMI 24 2 8.3 0 0.0 7 29.2 5 20.8 10 41.7 None 22 1 4.5 6 27.3 8 36.4 4 18.2 3 13.6 Reimbursement ratio** None 282 21 7.4 40 14.2 121 42.9 61 21.6 39 13.8 Partly 82 3 3.7 11 13.4 34 41.5 25 30.5 9 11.0 All 131 2 1.5 9 6.9 27 20.6 51 38.9 42 32.1 Low insurance** Have 79 4 5.1 15 19.0 47 59.5 10 12.7 3 3.8 None 485 26 5.4 52 10.7 165 34.0 136 28.0 106 21.9 Social financial aid** Have 75 2 2.7 18 24.0 39 52.0 13 17.3 3 4.0 None 498 29 5.8 49 9.8 176 35.3 135 27.1 109 21.9 Survey methods** Household 123 2 1.6 23 18.7 68 55.3 25 20.3 5 4.1 Outpatient 139 20 14.4 15 10.8 40 28.8 53 38.1 11 7.9 Hospitalization 311 9 2.9 29 9.3 107 34.4 70 22.5 96 30.9 Note. UEMI: urban employee medical insurance. URRMI: rural residents medical insurance, including urban residents medical insurance and new rural cooperative medical insurance. CMI: commercial medical insurance. *P < 0.05; **P < 0.01.
doi: 10.3967/bes2021.011
Analysis of Health Service Utilization and its Influencing Factors among Patients with Pneumoconiosis in China
-
Abstract: Pneumoconiosis, an interstitial lung disease that occurs from breathing in certain kinds of damaging dust particles, is a major occupational disease in China. Patients diagnosed with occupational pneumoconiosis can avail of free medical treatment, whereas patients without a diagnosis of occupational diseases cannot not claim free medical treatment in most provinces from the government before 2019. This study aimed to analyze the priority of medical facility selection and its influencing factors among patients with pneumoconiosis. A total of 1,037 patients with pneumoconiosis from nine provinces in China were investigated. The health service institutions most frequently selected by the patients were county-level hospitals (37.5%). The main reason for the choice was these hospitals’ close distance to the patients’ homes (47.3%). The factors for the choice of health care institutions were living in the eastern region (OR = 2.91), living in rural areas (OR = 2.10), silicosis diagnosis (OR = 2.44), employment in private enterprises (OR = 2.91), smoking (OR = 2.69), and quit smoking (OR = 3.98). The diagnosis, treatment, and rehabilitation therapy of pneumoconiosis should be enhanced in primary medical institutions.
-
Key words:
- Pneumoconiosis /
- Health service /
- Utilization
注释: -
Table 1. Basic characteristics of pneumoconiosis patients in rural and urban areas
Variables Categories Rural areas (n = 700) Urban areas (n = 337) All (n = 1,037) n % n % n % Gender* Male 698 99.7 331 98.2 1,029 99.2 Female 2 0.3 6 1.8 8 0.8 Age** (year) −35 14 2.0 8 2.4 22 2.1 −45 101 14.4 42 12.5 143 13.8 −55 314 44.9 102 30.3 416 40.1 −65 181 25.9 78 23.1 259 25.0 −75 69 9.9 58 17.2 127 12.2 75− 21 3.0 49 14.5 70 6.8 Education** Illiteracy 91 13.0 40 11.9 131 12.6 Primary school 288 41.1 105 31.2 393 37.9 Middle school 210 30.0 133 39.5 343 33.1 High school and above 42 6.0 55 16.3 97 9.4 Others 69 9.9 4 1.2 73 7.0 Registered residence** Eastern 271 38.7 173 51.3 444 42.8 Central 295 42.1 93 27.6 388 37.4 Western 134 19.1 71 21.1 205 19.8 Nature of work units** State-owned 152 21.7 241 71.5 393 37.9 Collective 110 15.7 29 8.6 139 13.4 Private 384 54.9 56 16.6 440 42.4 Others 54 7.7 11 3.3 65 6.3 Note. *P < 0.05, **P < 0.01. S1. Status of sickness and medical social security of pneumoconiosis patients
Variables Categories Rural areas (n = 700) Urban areas (n = 337) All (n = 1,037) n % n % n % Pneumoconiosis types* Silicosis 503 71.9 223 66.2 726 70.0 CWP 152 21.7 75 22.3 227 21.9 Others 45 6.4 39 11.6 84 8.1 Pneumoconiosis grades** Phase one 191 27.3 175 51.9 366 35.3 Phase two 175 25.0 73 21.7 248 23.9 Phase three 262 37.4 64 19.0 326 31.4 Others 72 10.3 25 7.4 97 9.4 Occupational injury insurance** Yes 183 26.1 241 71.5 424 40.9 None 517 73.9 96 28.5 613 59.1 Medical insurance** UEMI 103 14.7 219 65.0 322 31.1 URRMI 524 74.9 92 27.3 616 59.4 CMI 39 5.6 14 4.2 53 5.1 None 34 4.9 12 3.6 46 4.4 Current working status** Retired 129 18.4 203 60.2 332 32.0 Unemployed 356 50.9 54 16.0 410 39.5 Long-term workers 77 11.0 11 3.3 88 8.5 Short-term workers 87 12.4 57 16.9 144 13.9 Others 51 7.3 12 3.6 63 6.1 Note. CWP: coal worker pneumoconiosis. UEMI: urban employee medical insurance. URRMI: rural resident’s medical insurance, including urban resident’s medical insurance and new rural cooperative medical insurance. CMI: commercial medical insurance. *P < 0.05, **P < 0.01. S2. The reasons for medical service choices of respondents
Reasons Rural areas
(n = 700)Urban areas
(n = 337)All areas
(n = 1,037)χ2 P-value n % n % n % Close to home 218 58.1 50 26.0 268 47.3 52.47 ** High medical level 96 25.6 59 30.7 155 27.3 1.682 Designated institutions for medical insurance or industrial injury insurance 65 17.3 89 46.4 154 27.2 54.06 ** Specialist clinic 81 21.6 68 35.4 149 26.3 12.51 ** Good service attitude 42 11.2 44 22.9 86 15.2 13.55 ** Low hospital expenses 60 16.0 26 13.5 86 15.2 0.596 Hospital have good reputation 27 7.2 26 13.5 53 9.3 6.027 * Recommended from pneumoconiosis 11 2.9 7 3.6 18 3.2 0.210 Short waiting time 6 1.6 11 5.7 17 3.0 7.444 ** Note. *P < 0.05, **P < 0.01. S3. Influence of regional and work factors on the outpatient clinics choices of responders
Variables Categories Cases Village clinic Towns and townships/
health service centersCounty/city/
district hospitalPrefecture/
city hospitalsProvincial
hospitaln % n % n % n % n % Habitual residence** Rural area 380 29 7.6 51 13.4 171 45.0 81 21.3 48 12.6 Urban area 193 2 1.0 16 8.3 44 22.8 67 34.7 64 33.2 Registered residence** Eastern 275 22 8.0 19 6.9 90 32.7 99 36.0 45 16.4 Central 225 8 3.6 39 17.3 98 43.6 39 17.3 41 18.2 Western 73 1 1.4 9 12.3 27 37.0 10 13.7 26 35.6 Unit properties** State-owned 221 7 3.2 15 6.8 62 28.1 63 28.5 74 33.5 Collective 90 11 12.2 11 12.2 30 33.3 29 32.2 9 10.0 Private 224 8 3.6 39 17.4 114 50.9 38 17.0 25 11.2 Others 38 5 13.2 2 5.3 9 23.7 18 47.4 4 10.5 Employment status** Retirement 219 14 6.4 14 6.4 54 24.7 80 36.5 57 26.0 Unemployment 228 11 4.8 37 16.2 109 47.8 44 19.3 27 11.8 Short-term workers 32 1 3.1 4 12.5 18 56.3 7 21.9 2 6.3 Long-term workers 59 2 3.4 7 11.9 23 39.0 10 16.9 17 28.8 Others 35 3 8.6 5 14.3 11 31.4 7 20.0 9 25.7 Total 573 31 5.4 67 11.7 215 37.5 148 25.8 112 19.5 Note. *P < 0.05, **P < 0.01. Table 2. Influence of disease characteristic factors on the outpatient clinics choices of responders
Variables Categories Cases Village clinic Towns and townships/
health service leftsCounty/city/
district hospitalPrefecture/
city hospitalsProvincial
hospitaln % n % n % n % n % Pneumoconiosis types** Silicosis 427 25 5.9 47 11.0 171 40.0 116 27.2 68 15.9 CWP 99 4 4.0 19 19.2 33 33.3 20 20.2 23 23.2 Others 47 2 4.3 1 2.1 11 23.4 12 25.5 21 44.7 Pneumoconiosis grades** Phase one 190 5 2.6 11 5.8 56 29.5 54 28.4 64 33.7 Phase two 140 11 7.9 18 12.9 56 40.0 39 27.9 16 11.4 Phase three 202 15 7.4 33 16.3 86 42.6 46 22.8 22 10.9 Others 41 0 0.0 5 12.2 17 41.5 9 22.0 10 24.4 Dyspnea** Yes 396 27 6.8 50 12.6 157 39.6 90 22.7 72 18.2 No 173 4 2.3 17 9.8 56 32.4 57 32.9 39 22.5 Expectoration** Yes 346 23 6.6 34 9.8 112 32.4 100 28.9 77 22.3 No 223 8 3.6 33 14.8 101 45.3 47 21.1 34 15.2 Self-rating health score 30 93 5 5.4 13 14.0 37 39.8 24 25.8 14 15.1 50 177 13 7.3 23 13.0 69 39.0 41 23.2 31 17.5 70 186 8 4.3 20 10.8 70 37.6 50 26.9 38 20.4 90 97 5 5.2 10 10.3 37 38.1 24 24.7 21 21.6 90- 9 0 0.0 0 0.0 1 11.1 3 33.3 5 55.6 Note. *P < 0.05, **P < 0.01. S5. Influence of social demographic factors on the outpatient clinics choices of responders
Variables Categories Cases Village clinic Towns and townships/
health service centersCounty/city/
district hospitalPrefecture/
city hospitalsProvincial hospital n % n % n % n % n % Age (years)** −35 12 0 0.0 1 8.3 6 50.0 3 25.0 2 16.7 −45 71 3 4.2 14 19.7 33 46.5 9 12.7 12 16.9 −55 194 7 3.6 23 11.9 85 43.8 37 19.1 42 21.6 −65 185 15 8.1 19 10.3 55 29.7 66 35.7 30 16.2 66− 111 6 5.4 10 9.0 36 32.4 33 29.7 26 23.4 Education level** Illiteracy 70 4 5.7 17 24.3 31 44.3 5 7.1 13 18.6 Primary school 218 16 7.3 26 11.9 91 41.7 55 25.2 30 13.8 Middle school 179 7 3.9 20 11.2 56 31.3 52 29.1 44 24.6 High school and above 56 1 1.8 1 1.8 18 32.1 15 26.8 21 37.5 Others 50 3 6.0 3 6.0 19 38.0 21 42.0 4 8.0 Monthly income (Yuan)** None 217 18 8.3 36 16.6 86 39.6 57 26.3 20 9.2 −1000 88 7 8.0 15 17.0 46 52.3 12 13.6 8 9.1 −2000 59 3 5.1 7 11.9 26 44.1 10 16.9 13 22.0 −3000 83 2 2.4 5 6.0 19 22.9 19 22.9 38 45.8 −4000 57 0 0.0 0 0.0 20 35.1 19 33.3 18 31.6 4000− 59 1 1.7 4 6.8 18 30.5 25 42.4 11 18.6 Smoke** Current 102 3 2.9 9 8.8 37 36.3 28 27.5 25 24.5 Quit 254 15 5.9 30 11.8 111 43.7 69 27.2 29 11.4 Never 217 13 6.0 28 12.9 67 30.9 51 23.5 58 26.7 Note. *P < 0.05, **P < 0.01. S6. Outpatient clinics choices of responders from different regions
Current residence Registered residence Cases Village clinic Towns and townships/
health service centersCounty/city/
district hospitalPrefecture/
city hospitalsProvincial hospital n % n % n % n % n % Rural area Eastern 162 20 12.3 15 9.3 71 43.8 45 27.8 11 6.8 Central 166 8 4.8 30 18.1 82 49.4 29 17.5 17 10.2 Western 52 1 1.9 6 11.5 18 34.6 7 13.5 20 38.5 Subtotal 380 29 7.6 51 13.4 171 45.0 81 21.3 48 12.6 Urban area Eastern 113 2 1.8 4 3.5 19 16.8 54 47.8 34 30.1 Central 59 0 0.0 9 15.3 16 27.1 10 16.9 24 40.7 Western 21 0 0.0 3 14.3 9 42.9 3 14.3 6 28.6 Subtotal 193 2 1.0 16 8.3 44 22.8 67 34.7 64 33.2 S4. Influence of medical security and survey methods on distribution of outpatient clinics
Variables Categories Cases Village clinic Towns and townships/
health service centersCounty/city/
district hospitalPrefecture/
city hospitalsProvincial hospital n % n % n % n % n % Employment injury insurance** Have 225 4 1.8 11 4.9 68 30.2 67 29.8 75 33.3 None 298 24 8.1 47 15.8 132 44.3 72 24.2 23 7.7 Unclear 50 3 6.0 9 18.0 15 30.0 9 18.0 14 28.0 Medical insurance** UEMI 189 3 1.6 7 3.7 52 27.5 63 33.3 64 33.9 URRMI 338 25 7.4 54 16.0 148 43.8 76 22.5 35 10.4 CMI 24 2 8.3 0 0.0 7 29.2 5 20.8 10 41.7 None 22 1 4.5 6 27.3 8 36.4 4 18.2 3 13.6 Reimbursement ratio** None 282 21 7.4 40 14.2 121 42.9 61 21.6 39 13.8 Partly 82 3 3.7 11 13.4 34 41.5 25 30.5 9 11.0 All 131 2 1.5 9 6.9 27 20.6 51 38.9 42 32.1 Low insurance** Have 79 4 5.1 15 19.0 47 59.5 10 12.7 3 3.8 None 485 26 5.4 52 10.7 165 34.0 136 28.0 106 21.9 Social financial aid** Have 75 2 2.7 18 24.0 39 52.0 13 17.3 3 4.0 None 498 29 5.8 49 9.8 176 35.3 135 27.1 109 21.9 Survey methods** Household 123 2 1.6 23 18.7 68 55.3 25 20.3 5 4.1 Outpatient 139 20 14.4 15 10.8 40 28.8 53 38.1 11 7.9 Hospitalization 311 9 2.9 29 9.3 107 34.4 70 22.5 96 30.9 Note. UEMI: urban employee medical insurance. URRMI: rural residents medical insurance, including urban residents medical insurance and new rural cooperative medical insurance. CMI: commercial medical insurance. *P < 0.05; **P < 0.01. -
[1] Bian LQ, Mao L, Bi Y, et al. Loss of regulatory characteristics in CD4+ CD25+/hi T cells induced by impaired transforming growth factor beta secretion in pneumoconiosis. APMIS, 2017; 125, 1108−16. doi: 10.1111/apm.12748 [2] Xia Y, Liu JF, Shi TT, et al. Prevalence of pneumoconiosis in Hubei, China from 2008 to 2013. Int J Environ Res Public Health, 2014; 11, 8612−21. doi: 10.3390/ijerph110908612 [3] Skowronski M, Halicka A, Barinow-Wojewódzki A. Pulmonary tuberculosis in a male with silicosis. Adv Respir Med, 2018; 86, 121−2. doi: 10.5603/ARM.2018.0019 [4] Doney BC, Blackley D, Hale JM, et al. Respirable coal mine dust at surface mines, United States, 1982-2017. Am J Ind Med, 2020; 63, 232−9. doi: 10.1002/ajim.23074 [5] Abouie A, Majdzadeh R, Khabiri R, et al. Socioeconomic inequities in health services' utilization following the Health Transformation Plan initiative in Iran. Health Policy Plann, 2018; 33, 1065−72. doi: 10.1093/heapol/czy096 [6] Zhou ZL, Su YF, Gao JM, et al. Assessing equity of healthcare utilization in rural China: results from nationally representative surveys from 1993 to 2008. Int J Equity Health, 2013; 12, 34. doi: 10.1186/1475-9276-12-34 [7] Song XL, Zou GY, Chen W, et al. Health service utilisation of rural-to-urban migrants in Guangzhou, China: does employment status matter? Trop Med Int Health, 2017; 22, 82−91. doi: 10.1111/tmi.12801 [8] Qian YY, Gao JM, Zhou ZL, et al. An equity analysis of health examination service utilization by women from underdeveloped areas in western China. PLoS One, 2017; 12, e0186837. doi: 10.1371/journal.pone.0186837 [9] Wang Y, Wang LH, Gu XX. The analysis of the influence factors on selecting hospital in occupational disease patient. China Health Ind, 2015; 135-6, 42. (In Chinese) [10] He LG, Wu PF, Peng YH, et al. Modified Glasgow prognostic score, and neutrophil/lymphocyte and platelet/lymphocyte ratios in different stages of silicosis. Biomed Environ Sci, 2019; 32, 376−9. -




 下载:
下载:



 Quick Links
Quick Links