-
Mumps is a prevalent respiratory infectious disease caused by the mumps virus and is characterized by swollen salivary glands, fever, and pain[1]. The most effective preventive measure against this illness is vaccination with a live attenuated mumps-containing vaccine (MuCV). The globally preferred option is the trivalent measles, mumps, and rubella (MMR) vaccine, protecting against the mentioned diseases[2]. Since 2008, China has incorporated MMR vaccination into its national immunization program; the Fujian Province implemented this strategy on April 1, 2008, via introducing a one-dose MMR vaccination policy for children aged 18–24 months. This initiative has significantly decreased the incidence of mumps in Fujian Province[3], with rates stabilizing at approximately 7.8–8.0 cases per 100,000 individuals between 2018 and 2019, which translates to roughly 3,000 cases reported annually.
Despite these efforts, epidemiological data highlights that children and adolescents under 15 years of age remain highly susceptible to mumps[3]. This vulnerability has been underscored by occasional outbreaks, primarily among students. This resurgence has reignited interest in understanding and mitigating mumps outbreaks. In this communication, we present the outcomes of our recent study that delved into the characteristics of the mumps outbreak that occurred in four schools in Fujian Province, China, during 2018–2019. Our investigation highlights the current condition of the school mumps outbreaks and crucial areas for future prevention and control measures.
Ethical clearance was not required as this outbreak investigation was urgent and considered to be a public health response.
On January 23, 2018, the county-level Center for Disease Control and Prevention (CDC) in Zhangzhou City received a report regarding multiple suspected cases of mumps among grade 7 students in School A. These suspected cases in children primarily aged 12–13 years with a gender distribution of 7 males and 12 females, were investigated based on case definitions and classifications adapted from the Diagnostic Criteria for Mumps (WS 207-2007). Cases were defined as those occurring between December 1 and February 29, with an epidemiological link to a confirmed case at the local school. A confirmed case required laboratory confirmation of the mumps virus, including virus isolation, nucleic acid detection, or specific IgM antibody response, with or without clinical criteria such as self-reported or doctor-diagnosed salivary gland swelling (often parotitis) with or without fever. Probable cases were defined as an individual having the clinical and epidemiological criteria.
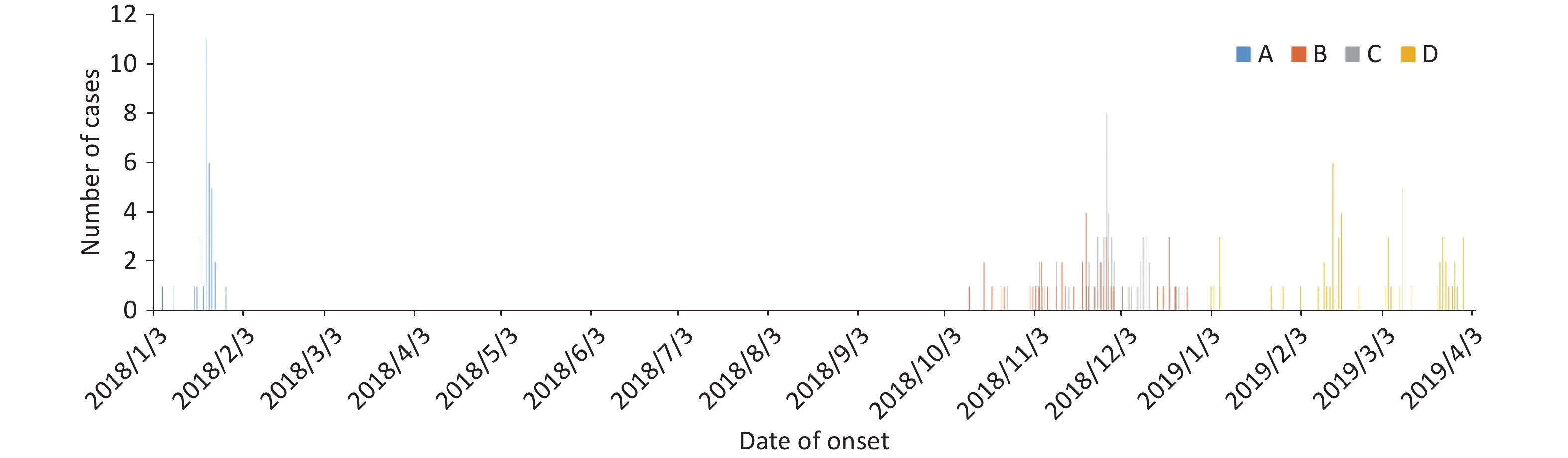
As mumps is a notifiable disease in China, all diagnosed cases must be reported individually through the National Notifiable Diseases Reporting System (NNDRS) of the China CDC. On receiving the report, the local CDC promptly dispatched a team of three professionals and two decontaminators to School A for case verification, on-site investigation, and disposal. The investigation revealed that the first case of a 12-year-old girl in Class 4, grade 7, presented with non-purulent swelling, pain, and fever in one parotid gland on January 3. The second case was reported three days later. The outbreak peaked on January 21 with 11 reported cases and ended after 25 days on January 28, 2018 (Figure 1). Most cases occurred in classes 3, 4, and 5 of grade 7, which were all located on the same floor, and affected 584 students. CDC personnel collected 17 throat swabs from suspected cases across various classes, resulting in 34 confirmed cases. Five cases were laboratory-confirmed, whereas the rest were clinically diagnosed.
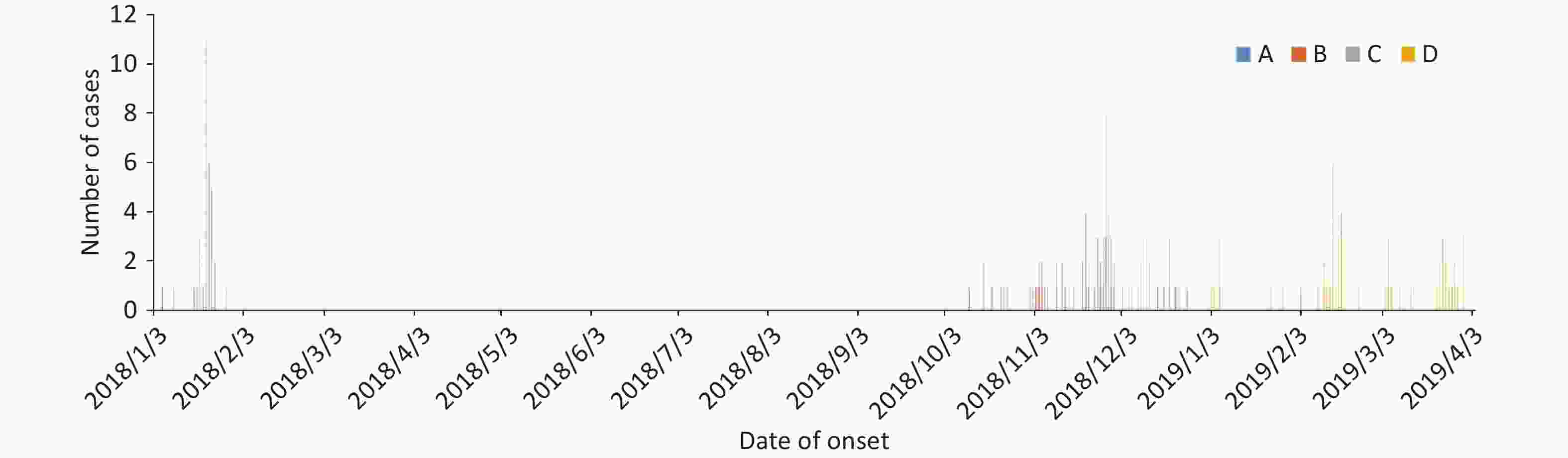
Figure 1. Epidemic distribution of mumps confirmed cases, by date of onset of symptoms, Fujian, 2018−2019 (n = 190).
Similarly, on November 15, 2018, the CDC staff in another city were notified of three clinically diagnosed mumps cases in School B through the NNDRS. An on-site investigation was conducted, examining epidemiological cases from October 1 to December 31. After investigating 48 ill students and excluding three suspected cases, 45 clinically diagnosed cases were confirmed, supported by disease certificates from medical institutions. Concurrently, School C, located six miles away, reported an outbreak starting on October 20; a male high school sophomore was experiencing enlarged parotid gland and fever, for which he was hospitalized because of orchitis complications. The local community health service center actively searched proximal health centers and confirmed 55 cases using epidemiological data. The cases were primarily clinically diagnosed in 12 affected classes. As shown in Figure 1, confirmed cases in both schools occurred on October 11 and ended on December 22 (School C) and December 25 (School B), respectively, with no further suspected cases detected thereafter.
On February 10, 2019, during a case review from the NNDRS, the local CDC staff discovered an outbreak at School D after the school reported students with parotid gland enlargement symptoms. The staff immediately conducted an investigation and actively searched for school-related cases since January 2019, until suspected cases were found after March 30 (Figure 1). In addition to five other suspected cases, 56 cases were confirmed in total.
Upon receiving the notification, the local CDC swiftly implemented outbreak-control measures in the affected schools. These measures included isolating students with suspected mumps infections, conducting vaccination status investigations among affected students, mandating vaccination for those without prior vaccination history[4], and excluding cases from attending school for a minimum of five days following symptom onset. Because of these comprehensive control measures, no additional cases or clusters of mumps were reported within the district.
Table 1 summarizes the details of the 190 confirmed mumps cases across four schools; 180 cases were clinically confirmed and 10 cases were confirmed using polymerase chain reaction to detect the mumps virus nucleic acid. No serum samples were collected for IgM detection. The demographics show that 58.9% (n = 112) cases were those of males between 11–18 years old. An acute onset of parotitis, either self-diagnosed or confirmed by a doctor, was reported in 84.7% (n = 161) cases, whereas only 46.8% had a history of fever or pain. A single case of orchitis complication was identified, which was lower than expected, based on other studies[5], potentially because of the delayed onset of complications and lack of routine follow-up data collection for NNDRS-reported cases.
Table 1. Characteristics of confirmed mumps cases in four schools in Fujian Province from 2018 to 2019 (n =190)
Characteristics A (n = 34) B (n = 45) C (n = 55) D (n = 56) Total (n = 190) Clinically diagnosed cases, n (%) 29 (85.3) 44 (97.8) 53 (96.4) 54 (96.4) 180 (94.7) Agea (years), x ± s 12.4 ± 0.5 12.6 ± 0.7 13.7 ± 2.2 16.6 ± 0.7 14 ± 2.1 Male, n (%) 13 (38.2) 29 (64.4) 34 (61.8)% 36 (64.3) 112 (58.9) Unilateral or bilateral parotid gland swelling, n (%) 28 (82.3) 34 (75.6) 48 (87.3) 51 (91.1) 161 (84.7) Fever or pain, n (%) 16 (47.1) 25 (55.6) 25 (45.5) 23 (41.1) 89 (46.8) Other symptoms (Orchitis), n (%) − − 1 (1.8) − 1 (1.8) The number of throat swabs was collected, n (%) 17 (50.0) 2 (4.4) 3 (5.5) 4 (7.1) 26 (13.7) The number of SH gene sequences, n (%) 5 (14.7) 1 (2.2) 2 (3.6) 2 (3.6) 10 (5.3) MuCV vaccination ≥ One dose, n (%) 9 (26.4) 21 (45.7) 14 (25.5) 16 (28.6) 60 (31.6) Unknown, n (%) 20 (58.9) 20 (44.4) 34 (61.8) 25 (44.6) 99 (52.1) Not vaccinated, n (%) 5 (14.7) 4 (8.9) 7 (12.7) 15 (26.8) 31 (16.3) Age (years) at the time of last MuCV dose, x ± sb 1.7 ± 2.4 2.2 ± 1.7 2.9 ± 1.7 3.4 ± 2.4 2.3 ± 1.9 Time (years) between last MuCV dose and onset of symptoms, x ± sb 10.7 ± 2.3 9.8 ± 3.0 8.6 ± 2.0 11.2 ± 3.4 9.9 ± 2.7 Note. aAt the time of the study; bStatistics presented: mean. Between 2013 and 2015, China showed an increase in mumps virus genotypes F (99.0%) and G (1.0%); genotype F maintained its prevalent position for over two decades[6]. The current mumps vaccine is produced via utilizing the S79 strain, a further attenuated derivative of the Jeryl Lynn strain, which is of genotype A[7]. Analyzing the 26 throat swab samples collected from four schools revealed ten successful sequences of the mumps virus SH gene, all belonging to genotype F, implying that the outbreaks were predominantly caused by genotype F strains. However, sequencing of the remaining 16 specimens was unsuccessful because of low viral loads. Sequence comparison revealed a significant dissimilarity between genotype F strains detected in Fujian and the vaccine genotype A strains, with sequence similarity ranging only from 82.9%–84.2%.
Vaccination status data revealed that 31.6% (n = 60) cases had received at least one dose of MuCV, all of which were derived from the Jeryl Lynn strain, which protected against genotype A[7]. However, for 52.1% (n = 99) cases, vaccination status could not be confirmed, and 31 cases were unvaccinated. The average age at vaccination was 2.3 ± 1.9 years, with a mean interval of 9.9 ± 2.7 years between the last MuCV dose and symptom onset (Table 1).
We hypothesize that the low vaccination rates, waning immunity, and potential mismatch between circulating and vaccine mumps virus strains contribute to the occurrence of these outbreaks. Prior to 2008, the MuCV in Fujian Province was voluntarily paid for, which resulted in an unsatisfactory vaccination rate. An evaluation by the Fujian Vaccine and Immunization Information Management System revealed that the first-dose coverage rate for children born before 2005 was below 30%, which increased to 78% for those born in 2007 and surpassed 90% post-2008. Of the cases investigated in the four schools, 79.5% (n = 151) were born before 2005 (Figure 2). However, a MuCV vaccination rate as low as 31.6% among these individuals would be insufficient to confer effective immune protection, highlighting the need for more robust vaccination strategies to safeguard these vulnerable children[3].
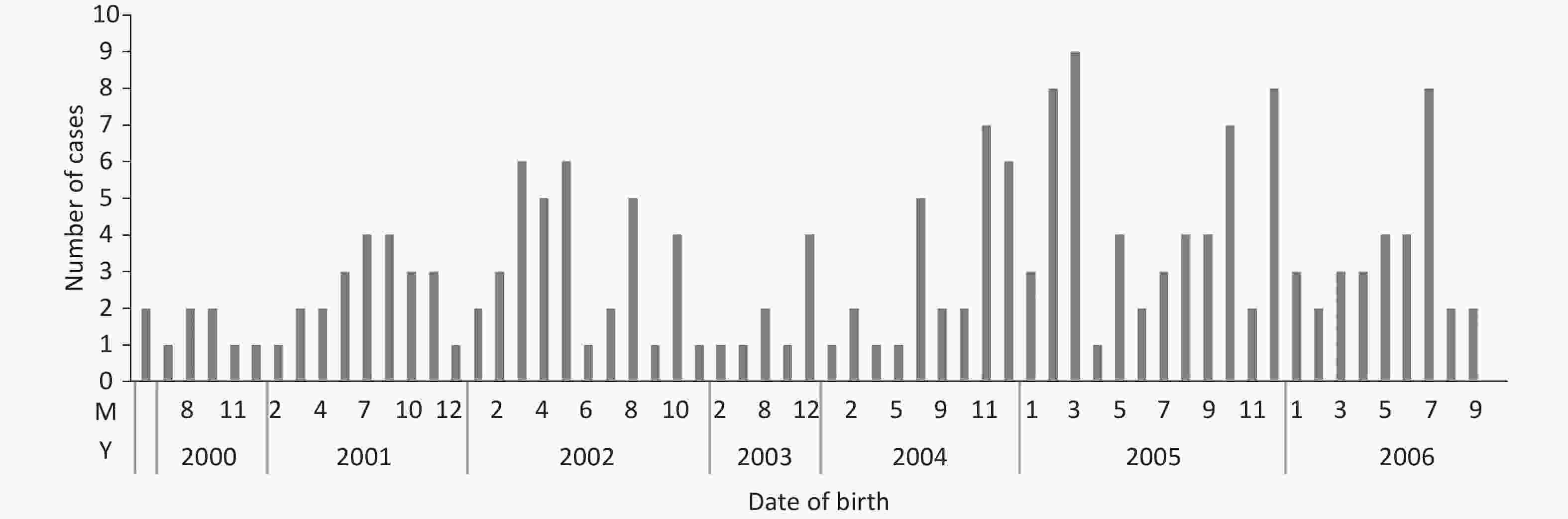
Figure 2. Date of birth of confirmed mumps cases in four schools in Fujian Province from 2018 to 2019 (n = 190).
Research conducted by Qin Wei et al. has demonstrated that the effectiveness of a single dose of the MuCV wanes over time, decreasing from 82% within five years post-vaccination to 41% after a decade, hence elevating the risk of mumps outbreaks[8]. In our study, the mean interval between the last vaccination and disease onset was 9.9 ± 2.7 years, with only eight cases (4.2%) having received vaccination within the preceding five years, indicating the gradual erosion of protection provided by a single dose over time. While serum samples were not procured for direct antibody titer measurement, our prior surveillance data on the entire population in Fujian Province revealed a mumps antibody prevalence of only 75.4% among 10–15 years old in 2018[3], which is the primary age bracket affected by school outbreaks. Consequently, revising China’s current single-dose mumps immunization strategy is imperative. China incorporated an additional MMR vaccine dose into its routine immunization schedule, administered at 8 and 18 months of age; however, as of June 1, 2020, further research is essential to gauge its impact on the scale and longevity of outbreaks among schoolchildren and adolescents. In the interim, we steadfastly advocate for booster vaccinations for all unvaccinated individuals and those previously vaccinated as children to safeguard these high-risk groups during outbreaks.
Our investigation further shows that outbreaks of mumps F among children and young adults vaccinated with the Jeryl Lynn strain (genotype A) over the past few decades are not infrequent, even in regions boasting high vaccine coverage[6,7]. These outbreaks are often characterized by mild to moderate clinical symptoms, which may not always prompt individuals to seek healthcare services. Consequently, the magnitude of an outbreak is heavily influenced by herd immunity and the specific environment in which cases arise, particularly in densely populated settings[8,9]. Therefore, we propose that future mumps surveillance efforts should transcend focusing solely on overt clinical manifestations and instead be directed towards to cases presenting with milder to moderate symptoms.
No potential conflicts of interest were disclosed.
doi: 10.3967/bes2024.143
-
Dong Li conceived and designed the study. Zhifei Chen, Ruihong Wu, Xiuhui Yang, Yong Zhou, Weiyi Pan experimental operation and data analysis. Dong Li, Zhifei Chen wrote the paper. All authors read and approved the manuscript.
注释:1) Author Contrubition: -
Table 1. Characteristics of confirmed mumps cases in four schools in Fujian Province from 2018 to 2019 (n =190)
Characteristics A (n = 34) B (n = 45) C (n = 55) D (n = 56) Total (n = 190) Clinically diagnosed cases, n (%) 29 (85.3) 44 (97.8) 53 (96.4) 54 (96.4) 180 (94.7) Agea (years), x ± s 12.4 ± 0.5 12.6 ± 0.7 13.7 ± 2.2 16.6 ± 0.7 14 ± 2.1 Male, n (%) 13 (38.2) 29 (64.4) 34 (61.8)% 36 (64.3) 112 (58.9) Unilateral or bilateral parotid gland swelling, n (%) 28 (82.3) 34 (75.6) 48 (87.3) 51 (91.1) 161 (84.7) Fever or pain, n (%) 16 (47.1) 25 (55.6) 25 (45.5) 23 (41.1) 89 (46.8) Other symptoms (Orchitis), n (%) − − 1 (1.8) − 1 (1.8) The number of throat swabs was collected, n (%) 17 (50.0) 2 (4.4) 3 (5.5) 4 (7.1) 26 (13.7) The number of SH gene sequences, n (%) 5 (14.7) 1 (2.2) 2 (3.6) 2 (3.6) 10 (5.3) MuCV vaccination ≥ One dose, n (%) 9 (26.4) 21 (45.7) 14 (25.5) 16 (28.6) 60 (31.6) Unknown, n (%) 20 (58.9) 20 (44.4) 34 (61.8) 25 (44.6) 99 (52.1) Not vaccinated, n (%) 5 (14.7) 4 (8.9) 7 (12.7) 15 (26.8) 31 (16.3) Age (years) at the time of last MuCV dose, x ± sb 1.7 ± 2.4 2.2 ± 1.7 2.9 ± 1.7 3.4 ± 2.4 2.3 ± 1.9 Time (years) between last MuCV dose and onset of symptoms, x ± sb 10.7 ± 2.3 9.8 ± 3.0 8.6 ± 2.0 11.2 ± 3.4 9.9 ± 2.7 Note. aAt the time of the study; bStatistics presented: mean. -
[1] Anders H, Steven R, Kathrin M. Mumps. The Lancet, 2008; 371, 932−944. [2] Sun X, Tang FY, Hu Y, et al. High risk of mumps infection in children who received one dose of mumps-containing vaccine: waning immunity to mumps in children aged 2-5 years from kindergartens in Jiangsu Province, China. Hum Vaccin Immunother, 2020; 16, 1738−42. doi: 10.1080/21645515.2019.1708162 [3] Li D, Zhang HR, You N, et al. Mumps serological surveillance following 10 years of a one-dose mumps-containing-vaccine policy in Fujian Province, China. Hum Vaccin Immunother, 2022; 18, 2096375. doi: 10.1080/21645515.2022.2096375 [4] Clemmons NS, Redd SB, Gastañaduy PA, et al. Characteristics of large mumps outbreaks in the United States, July 2010–December 2015. Clin Infect Dis, 2019; 68, 1684−90. doi: 10.1093/cid/ciy779 [5] Veneti L, Borgen K, Borge KS, et al. Large outbreak of mumps virus genotype G among vaccinated students in Norway, 2015 to 2016. Euro Surveill, 2018; 23, 1700642. [6] Cui AL, Zhu Z, Hu Y, et al. Mumps epidemiology and mumps virus genotypes circulating in mainland China during 2013-2015. PLoS One, 2017; 12, e0169561. doi: 10.1371/journal.pone.0169561 [7] Cui AL, Zhu Z, Mao NY, et al. Assessment of one-dose mumps-containing vaccine effectiveness on wild-type genotype F mumps viruses circulating in mainland China. Vaccine, 2018; 36, 5725−31. doi: 10.1016/j.vaccine.2018.08.028 [8] Duque M P, San-Bento A, Léon L, et al. Mumps outbreak among fully vaccinated school-age children and young adults, Portugal 2019/2020. Epidemiol Infect, 2021; 149, e205. doi: 10.1017/S0950268821002028 [9] Melgar M, Yockey B, Marlow MA. Impact of vaccine effectiveness and coverage on preventing large mumps outbreaks on college campuses: implications for vaccination strategy. Epidemics, 2022; 40, 100594. doi: 10.1016/j.epidem.2022.100594 -




 下载:
下载:



 Quick Links
Quick Links