-
Diabetes affects approximately 10.5% of adults worldwide, and its chronic complications lead to severely disabling sequelae and premature death, thus placing a heavy healthcare burden on both patients affected and society[1]. China has experienced a dramatic increase in diabetes prevalence from 0.67% in 1980[2] to 12.8% in 2018[3] and has approximately one-quarter of people with diabetes worldwide[1]. It is therefore essential to understand the epidemiologic characteristics of the chronic complications and co-morbidities of diabetes, and the current status of diabetes management to guide planning for appropriate diabetes care and intervention for these complications and co-morbidities at the national level[4-7]. To date, however, no national population-based epidemiologic studies regarding diabetes-related complications and co-morbidities have been reported in China.
The China National Diabetic Chronic Complications Study (China DiaChronic Study) was conducted to investigate the epidemiologic characteristics of multiple chronic complications and co-morbidities of diabetes [retinopathy, nephropathy, peripheral neuropathy, peripheral arterial disease (PAD), and cardiovascular disease (CVD)] and related factors, as well as to assess the attainment rates of metabolic targets and the implementation of standardized diagnosis and treatments in Chinese adults with diagnosed diabetes between March 2018 and January 2020.
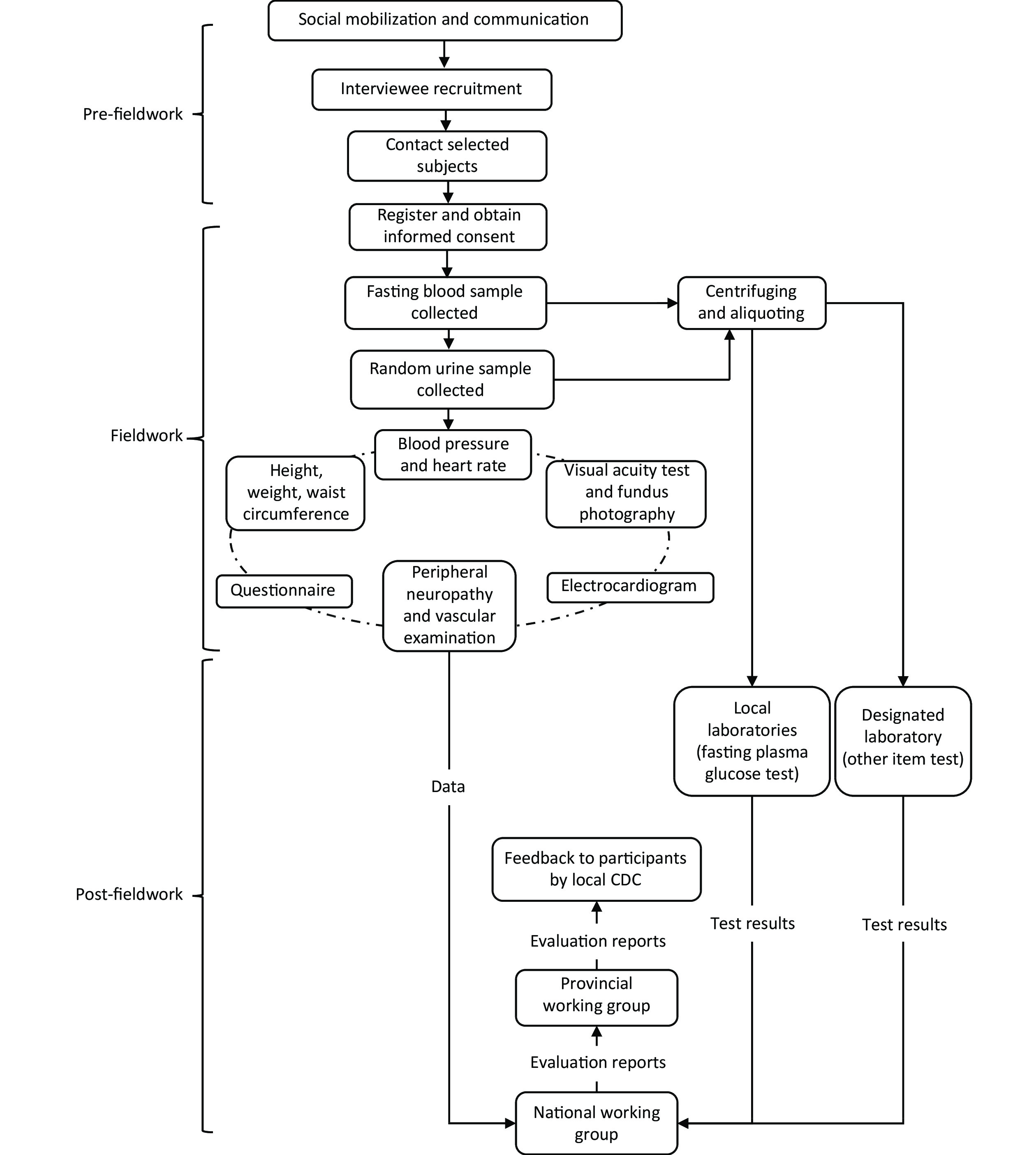
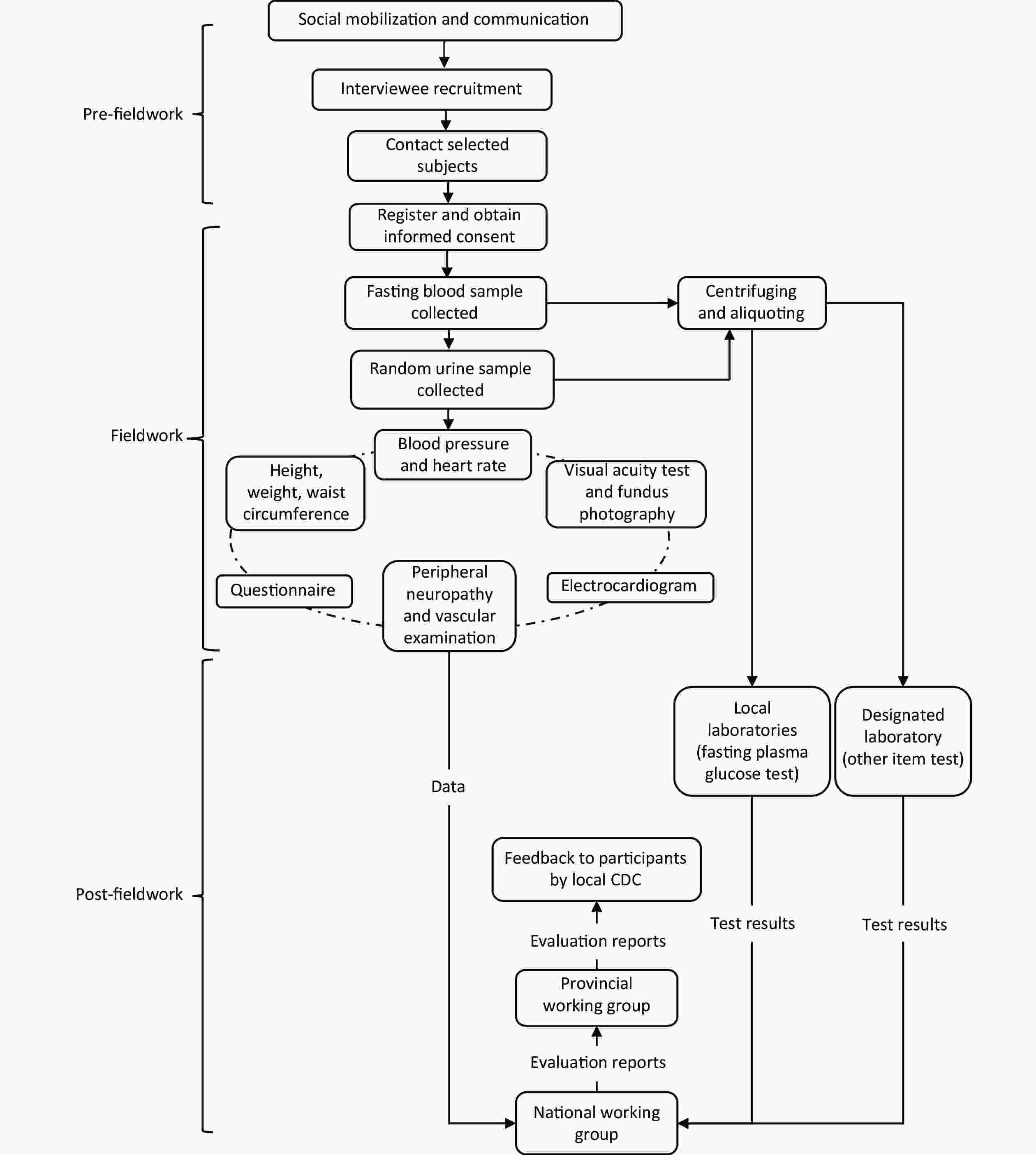
The China DiaChronic Study group consisted of members from the Chinese Diabetes Society (CDS) and the National Center for Chronic Non-communicable Disease Control and Prevention of the Chinese Center for Disease Control and Prevention (China CDC, referred to as CDC hereafter), who formed national, provincial, and local working groups. The national working group developed technical plans, questionnaires, and training materials, designed a system platform for sampling, information collection, and management (Supplementary Figure S1, available in www.besjournal.com), and conducted unified first-tier training for the provincial working group representatives. The provincial working groups conducted second-tier training for the provincial and local working staff. Under the guidance and supervision of the national working group, the provincial working groups organized and carried out the on-site surveys in their provinces in cooperation with the local working groups and uploaded survey data to the system platform. The results of the medical tests and evaluation reports were input into the system platform and were then printed and given out to the participants by the local working groups.
A sample size of approximately 49,800 was estimated according to the following formula[8]:
$$ n=\frac{\text{}{1.96}^{2}p\left(\text{1-}p\right)\left(\text{Deff}\right)N}{{\left(p*\sigma \right)}^{2}} $$ A prevalence of peripheral arterial disease of 10.7% was drawn from the Shanghai diabetic complications study[9], and prevalence of peripheral arterial disease was estimated to be 8.56% (or 10.7 x 0.8) at the China national level, which was expected to be the lowest among the rates of various diabetes-related complications. Then, the prevalence (p) of 8.56% was used to estimate the sample size for this survey. The two-sided significant level was 0.05, the design effect was 2 (Deff), the desired level of relative precision was 0.1 (σ), and the number of stratification (N) was 6 (sex and geographical regions). Then, based on an assumed 90% response rate, a nationally representative sample size was estimated to be 55,333 individuals.
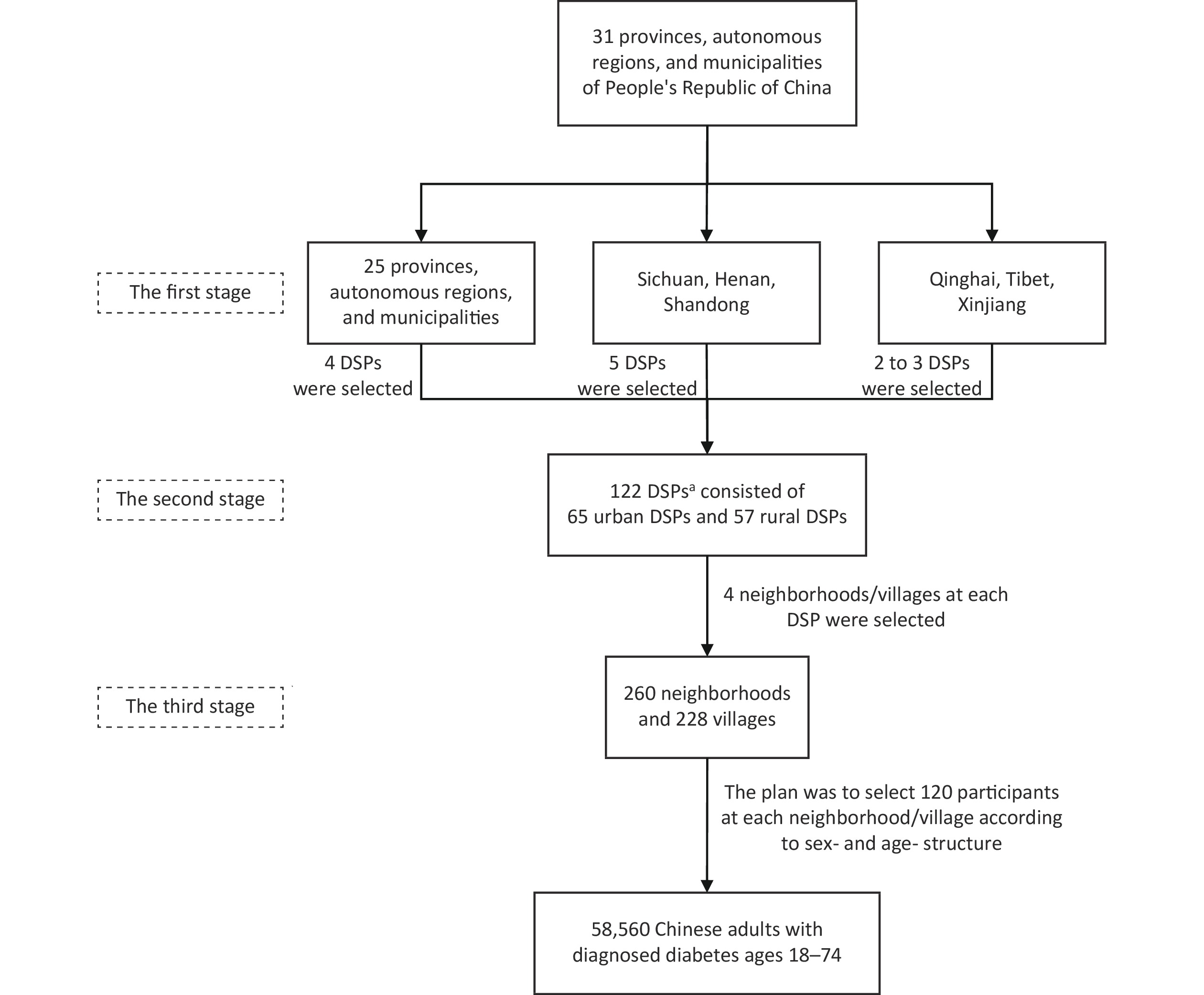
The multistage sampling scheme (stratification, clustering, and random) was used to sample study participants based on the disease surveillance points (DSPs) started in 2013 from the China Chronic Disease and Risk Factors Surveillance (CCDRFS)[10-11]. The CCDRFS was designed to reflect the epidemiologic characteristics of chronic diseases and related factors at both the national and provincial levels and covered all 31 provinces, autonomous regions, and municipalities of mainland China. One DSP from the CCDRFS usually represented a rural county or an urban district. Every county/district in mainland China has a diabetes management registration system for its local patients.
In the first stage, generally, four DSPs were selected from each province after considering urbanization levels. Three municipalities (Beijing, Tianjin, and Shanghai) have been fully urbanized; one rural DSP was added in three provinces (Sichuan, Henan, and Shandong) with larger population sizes, and the number of DSPs was reduced in one province (Qinghai) and two autonomous regions (Tibet and Xinjiang) with smaller population sizes. Then, a total of 122 DSPs (65 urban and 57 rural DSPs) from the 2013 CCDRFS were invited to participate. Of the DSPs invited, 15 refused to participate and were replaced with other CDC sites (not included in the 2013 CCDRFS) in the same province with similar urbanization levels (referred to as study sites hereafter), as shown in Supplementary Figure S2, available in www.besjournal.com. Approximately 1.68 million patients with diagnosed diabetes have been registered in the diabetes management registration system in these 122 study sites.

Figure S2. Geographical distribution of the 122 study sites in the 31 provinces, autonomous regions, and municipalities of mainland China
In the second stage, four neighborhoods in urban areas or four villages in rural areas were selected from each study site, and a total of 488 neighborhoods/villages were obtained.
In the third stage, the national sample size of 55,333 was equally divided by 488 neighborhoods/villages, then 113 study participants were sampled at each neighborhood/village. Subsequently, an age structure of 16% of the younger individuals (18–44 years), 44% of the middle-aged individuals (45–59 years), and 40% of the elderly individuals (60–74 years) according to the CCDRFS 2013 diabetes data[12], and an equal ratio of male to female participants were adopted. Finally, we set the sample size at 120 individuals for each neighborhood/village, then increased the national sample size to 58,560 individuals. The multistage stratified sampling procedure is depicted in Figure 1.
Figure 1. Flowchart of the multistage sampling scheme of the China National Diabetic Chronic Complications Study. aOf the 122 DSPs, 15 were replaced with other CDC sites (not included in the 2013 CCDRFS) in the same province with similar urbanization levels. CCDRFS, China Chronic Disease and Risk Factors Surveillance; CDC, Center for Disease Control and Prevention; DSPs, disease surveillance points.
The China DiaChronic Study was approved by the Ethical Review Committee (Approval No: 2018-010) and was registered in the Chinese Clinical Trial registry (ChiCTR1800014432). Written informed consent was obtained from each participant prior to data collection.
People with diagnosed diabetes aged 18−74 years, and who had resided in the study sites for at least 6 months of the last year before the survey were eligible for participating in this survey. Pregnant women or people with severe health conditions or illnesses that prevented them from participating, including the bedridden or the intellectually disabled, were excluded.
All data collection was performed at a local hospital or community health service center by the CDS and CDC medical staff. All investigators completed a training program and were qualified to use specific tools and methods before participating in on-site surveys. The flowchart of fieldwork is shown in Supplementary Figure S3, available in www.besjournal.com. Data collection consisted of the following four examination components: questionnaire surveys, physical examinations, laboratory testing, and special examinations [electrocardiogram (ECG), diabetic retinopathy, peripheral neuropathy, and peripheral vascular]. A summary of the four examination components is presented in Supplementary Tables S1–S4, available in www.besjournal.com.
Part Item Content 1 Demographic and socioeconomic information Patient ID, Sex, Date of birth, Race, Education, Occupation, Residence, Income and expenses, Marriage status, and Medical insurance 2 Smoking status Current cigarette consumption (frequency, duration), Cigarette cessation, and Passive smoking 3 Alcohol, tea, and coffee consumption Current alcohol consumption (frequency, degree, duration), Alcohol cessation, Tea consumption (frequency, species), and Coffee consumption (frequency) 4 Diet Fourteen kinds of food: grains (rice, noodles, steamed bread, etc.), whole grains (corn, buckwheat, millet, etc.), potatoes (russet potato, yam, yuca root, sweet potato, etc.), soybean products, fresh vegetables, fresh fruits, dairy foods, red meat (pork, beef, lamb, etc.), poultry (chicken, duck, etc.), seafood, eggs, nuts, sugar-sweetened beverages, and fresh juices 5 Physical activity and sleep Work, agriculture, and housework; Transit; Recreational activities and exercise; Total/leisure-time sedentary behavior; and Sleep behavior 6 Family history Family history of hypertension, diabetes, obesity, coronary heart disease, stroke, tumor, and dyslipidemia 7 Medical history Medical history of diabetes, hypertension, coronary heart disease, stroke, dyslipidemia, urinary system diseases, chronic hepatitis, hepatocirrhosis, and malignancy (date of diagnosis and/or treatment of the disease) 8 Medication Current medication for diabetes, hypertension, coronary heart disease, stroke, dyslipidemia, and other diseases (names of medicines taken) 9 Weight and its control Frequency of weight measuring and weight change in a year 10 Menstrual and obstetrical historya Age at first menstruation, Menopausal status, Age at menopause, History of gestational hypertension, gestational diabetes, and ovarian surgery Note. aOnly applicable for female participants. Table S1. Summary of the questionnaire
Item Description Equipment used Electrocardiogram A standard resting 12-lead electrocardiogram was performed and additional leads were completed if necessary Six-channel automatic electrocardiography (Mode FX-8222T) Visual acuity test It was measured at a distance of five meters with each eye tested separately Log-MAR visual acuity chart Diabetic retinopathy Two 45-degree color fundus photographs were taken for each eye; one was centered on the optic disc and the other on the macula Digital non-mydriatic retinal camera (Canon CR-2 or TRC-NW400) Peripheral neuropathy An inspection of the feet and evaluation of ankle reflexes, pinprick, and vibration, pressure, and temperature sensations were carried out Diabetic foot sensory examination kit, including 10 g monofilament, Tip-Therm, 128-Hz tuning fork, and a reflex hammer with sensory needle Peripheral arterial disease Peripheral vascular lesions were assessed by palpation of the dorsalis pedis, posterior tibial, and popliteal arteries, and by the Edinburgh intermittent claudication questionnaire / Table S4. Summary of special examinations
Face-to-face personal interviews were conducted through a digital questionnaire using a portable Android device. The questionnaire consisted of the following items: 1) demographic and socioeconomic information; 2) lifestyle factors, including smoking, alcohol intake, tea and coffee consumption, diet, physical activity, and sleep; 3) family history of disease; 4) medical history; 5) weight measurement and control; and 6) menstrual and obstetric history (Supplementary Table S1). A global physical activity questionnaire was adopted for physical activities[13]. A metabolic equivalent (MET) was calculated according to the total of moderate- and vigorous-intensity physical activity (the moderate MET value was 4.0 and the vigorous MET value was 8.0) for work, in-transit activity, and leisure time throughout a week[13]. If the participant had difficulties in answering the above questions, the family members who were most familiar with him/her would respond. In the survey of diet and physical activity, images for estimating dietary portion size and a classification table for physical activity were provided as a reference for the participants (Supplementary Table S5, available in www.besjournal.com).
Work, agriculture, and housework Recreational activities and exercise Sedentary behavior Moderate-intensity physical activitya High-intensity physical activityb Moderate-intensity physical activitya High-intensity physical activityb Sitting, leaning, or lying outside of sleep time Examples: Cleaning (such as vacuuming, mopping the floor, polishing the floor, wiping the table, sweeping the floor, ironing, etc.), Washing (brushing carpet, hand laundry, etc.), Gardening work (such as watering, soiling, fertilizing, etc.), Manual milking, Hand-weaving, Woodworking (carve, sawing softwood, etc.), Using tools such as mills and shovels to mix cement, sand, etc., Carrying/moving moderate loads (< 20 kg), Lifting water, Stocking livestock, etc. Examples: Forestry work (cutting and moving timber), Sawing hardwood, Cultivating land, Sowing, Harvesting crops (wheat, rice, sugar cane, etc.), Gardening work (excavation, heavy loads, etc.), Artificial grinding (using tweezers or stone grinders, etc.), Construction work (moving building materials, building walls, etc.), Carrying/moving heavy loads (> 20 kg), Fitness coaching (such as spinning, aerobics, yoga, etc.), Courier work (on foot or by bike), Pulling, picking up rickshaws, pushing wheelbarrows, operating jackhammers, etc. Examples: Bicycling, Jogging, Dancing, Riding, Tai Chi, Yoga, Pilates, Yangge, Dance, etc. Examples: Long-distance running, Playing football, Playing soccer, Playing tennis, Spinning/cycling, Lifting dumbbells, barbells, Ballet, Swimming, etc. Examples:Working, Studying, Reading, Watching TV, Using a computer, Riding a motor vehicle, Resting, etc. Note. aPhysical activity requires a moderate amount of effort and noticeably accelerates the heart rate. bPhysical activity requires a large amount of effort and causes rapid breathing and a substantial increase in heart rate. Table S5. Physical activity classification
The physical examinations included blood pressure, heart rate, and anthropometric measurements (height, weight, and waist circumference), and were performed in a fasting state in the morning according to a standard protocol[14]. Blood pressure was measured in the left arm three times consecutively with a 1-min interval between the measurements with the participant in a seated position after 5 minutes of rest using an automated device. Waist circumference was measured in the horizontal plane midway between the lower edge of the costal arch and the upper edge of the iliac crest (Supplementary Table S2).
Item No. of measurements Equipment used Precision Height (cm) 1 TGZ height gauge 0.1 Weight (kg) 1 TANITA HD-390 body weight scale 0.1 Waist circumference (cm) 2 1.5 Meter soft retractable measuring tape 0.1 Blood pressure (mmHg) 3 Omron blood pressure monitora 1 Heart rate (beats/min) 3 Omron blood pressure monitora 1 Note. aModels included HBP-1300, HEM-7207, HEM-7071, HEM-770A, HEM-7118, HEM-7133, HEM-7130, and HEM-8102A. Table S2. Summary of physical examinations
After a 10-hour overnight fast, a 15-mL blood sample and a random urine sample were collected from each participant. The fasting plasma glucose level was measured within 48 hours by local laboratories that had completed a standardization and certification program. The day after the survey, the blood and urine specimens were shipped to the Guangzhou KingMed Diagnostics Group Co., Ltd. (Guangzhou, China) in a refrigerator with a temperature range of 2−8 ℃ to test for glycated hemoglobin (HbA1c), lipid, liver function (alanine transaminase, glutamyl transferase, aspartate transaminase, albumin, and total protein), kidney function (creatinine, urea, and uric acid), urinary albumin, and urinary creatinine concentrations (Supplementary Table S3).
Item Method Equipment used Precision Blood FPG (mmol/L)a Glucose oxidase or hexokinase method Equipment available in local laboratoriesa 0.01 HbA1c (%)b High-performance liquid chromatography BioRad D10 Hemoglobin Analyzer 0.1 Lipid (mmol/L)b,c Enzymatic method Roche cobas c701/702 0.01 Creatinine (μmol/L)b Enzymatic method Roche cobas c701/702 1 Urine Urinary albumin (mg/L) Immunoturbidimetry Roche cobas c701/702 0.1 Urinary creatine (μmol/L) Enzymatic method Roche cobas c701/702 1 Note. aFPG was measured by local laboratories with a unified quality control plan, as follows. Before carrying out fasting blood glucose testing, each laboratory was required to verify the testing system using uniformly-issued serum chemistry controls: 1) repeatability precision verification [the staff aliquoted 20 copies of the low-, medium-, and high-concentration quality control products, performed repeated tests (a total of 60 measurement data), and the verification pass standard was that the coefficients of variation (CV) of each concentration were < 2.5%]; and 2) intermediate precision verification [the staff took one quality control product with low, medium, and high concentrations, tested once every hour, repeated four times a day for five days (20 data for each concentration; a total of 60 data), and the verification standards included that for each concentration, the means and the CVs of the daily test results were within the ranges declared by the manufacturer]. During the test period, each laboratory was required to perform real-time quality control using quality control products. On each experimental day, the staff needed to test quality controls in three levels (before, during, and after testing). If the test results met the following conditions, they were considered to be under quality control: 1) the test results of a specific concentration level cannot exceed the target value ± 3 standard deviations (SDs) within one day or exceed the target value ± 2 SDs for two consecutive days; and 2) the test results of two specific concentration levels cannot exceed the target value by ± 2 SDs at the same time within one day. After the test, we summarized the quality control results of each laboratory. The data showed that the CVs were all < 3.3% (0.05%–3.18%) and the cumulative target values [hexokinase method (level 1, 3.06–3.62; level 2, 6.08–7.02; level 3, 18.40–21.02); glucose oxidase method (level 1, 3.11–3.39; level 2, 6.16–6.75; level 3, 18.60–20.55)] were within the range declared by the manufacturer [hexokinase method (level 1, 2.89–3.68; level 2, 5.94–7.13; level 3, 18.20–22.20); glucose oxidase method (level 1, 2.66–3.91; level 2, 5.54–7.58; level 3, 17.40–23.80)]. bHbA1c, lipids, and creatinine, as well as urinary albumin and creatinine, were centrally measured and HbA1c was measured with a national glycohemoglobin standardization program-certified method. cLipid test included triglycerides, total cholesterol, high-density lipoprotein-cholesterol, and low-density lipoprotein-cholesterol. FPG, fasting plasma glucose; HbA1c, hemoglobin A1c. Table S3. Summary of laboratory tests
An ECG and screening for diabetic retinopathy, peripheral neuropathy, and peripheral arterial disease were performed using uniform medical equipment. A six-channel automatic analysis electrocardiograph (FX-8222T; Fukuda Denshi Co., Ltd., Tokyo, Japan) was used to perform a standard resting 12-lead electrocardiography, adding additional leads if necessary. These electrocardiograms were reviewed and interpreted by medical professionals who were blinded to the conditions of the participants. In addition, electrocardiograms were characterized as ECG coronary probable (ST-segment elevation and pathologic Q waves), ECG coronary possible (detected ST-segment depression and T-wave changes), ECG coronary unlikely (all other remaining abnormal ECG records), and a normal ECG according to the European Society of Cardiology/American Heart Association recommendations. The ophthalmic examinations included a visual acuity test and fundus photography. Logarithm of the minimal angle of resolution (log-MAR) charts were used at a distance of five meters with each eye tested separately. Two 45-degree color fundus photographs were taken for each eye; one was centered on the optic disc and another on the macula, using a digital non-mydriatic retinal camera (Canon CR-2; Canon Inc., Tokyo, Japan or TRC-NW400; Topcon Corporation, Tokyo, Japan). The severity of diabetic retinopathy was graded into the following five levels according to the 2002 International Clinical Diabetic Retinopathy Disease Severity Scales[15]: no apparent retinopathy; mild, moderate, and severe non-proliferative retinopathy; and proliferative retinopathy. Every photograph was reviewed and rated by two ophthalmologists, and if the diagnosis or the grading of diabetic retinopathy was inconsistent, the photograph was reviewed by another senior ophthalmologist. All ophthalmologists were blinded to the participants' conditions and the results graded by other ophthalmologists. An inspection of the feet and evaluation of ankle reflexes, and pinprick, pressure, temperature, and vibration sensations were carried out for neuropathy testing using a reflex hammer with a sensory needle, 10-g monofilament, and Tip-Therm (Beijing Laxons Technology Co., Ltd., Beijing, China), and 128-Hz tuning fork (Berchtold GmbH & CO.KG, Esslingen, Germany), respectively. Peripheral neuropathy was scored according to the 1994 Michigan Neuropathy Screening Instrument[16]. Peripheral vascular lesions were assessed by palpation of the dorsalis pedis, posterior tibial, and popliteal arteries. Intermittent claudication was assessed using the Edinburgh intermittent claudication questionnaire (Supplementary Table S4).
Data are presented as the mean (standard deviation) for continuous variables and number (percentage) for categorical variables. The difference in means and proportions between two groups was tested using a t-test and χ2 test, respectively. All analyses were conducted using SAS (version 9.4; SAS Institute, Cary, NC, USA). The map was created using R (version 4.0.4; R Foundation for Statistical Computing, Vienna, Austria). All tests were two-sided and a P < 0.05 was considered statistically significant.
The response rate for each item in the China DiaChronic Study for the 58,560 participants is shown in Table 1. The overall response rate was 91.2% (males, 90.4%; females, 92.0%; young participants, 74.7%; middle-aged participants, 93.9%; and elderly participants, 95.1%). Some participants were excluded from the response rate calculation for a given complication because the participants were ineligible for the examination (e.g., a participant with a two-leg amputation was not eligible for a peripheral nerve examination). Then, under the condition of a complete interview, the individual response rates for anthropometric measurements, blood pressure measurements, blood sample testing, and urine sample testing were 91.2%, 91.1%, 91.1%, and 90.6%, respectively. The individual response rates for of ECG examination, visual acuity test, and diabetic retinopathy, peripheral neuropathy, and peripheral arterial disease screening were 90.3%, 90.6%, 90.1%, 90.5%, and 90.5%, respectively.
Population Questionnaire Anthropometric indices Blood pressure Blood test Urine test Electrocardiogram Visual acuity test Diabetic retinopathy Peripheral neuropathy Peripheral arterial disease N Response rate (%) N Response rate (%) N Response rate (%) N Response rate (%) N Response rate (%) N Response rate (%) N Response rate (%) N Response rate (%) N Response rate (%) N Response rate (%) Total 53,401 91.2 53,378 91.2 53,359 91.1 53,367 91.1 53,064 90.6 52,872 90.3 52,875 90.6 52,134 90.1 53,002 90.5 52,967 90.5 Sex Men 26,471 90.4 26,459 90.4 26,447 90.3 26,453 90.3 26,361 90.0 26,182 89.4 26,226 89.8 25,884 89.4 26,255 89.7 26,236 89.6 Women 26,930 92.0 26,919 91.9 26,912 91.9 26,914 91.9 26,703 91.2 26,690 91.2 26,649 91.4 26,250 90.9 26,747 91.4 26,731 91.3 Age group, years 18–44 7,289 74.7 7,288 74.7 7,284 74.6 7,279 74.6 7,193 73.7 7,201 73.8 7,185 73.9 7,134 73.5 7,215 74.0 7,209 73.9 45–59 23,834 93.9 23,822 93.9 23,815 93.8 23,823 93.9 23,730 93.5 23,588 93.0 23,631 93.4 23,390 93.0 23,662 93.3 23,645 93.2 60–74 22,278 95.1 22,268 95.1 22,260 95.0 22,265 95.1 22,141 94.5 22,083 94.3 22,059 94.5 21,610 94.0 22,125 94.5 22,113 94.4 Setting Urban 28,457 91.2 28,449 91.2 28,437 91.1 28,435 91.1 28,279 90.6 28,115 90.1 28,216 90.7 27,744 90.0 28,259 90.6 28,240 90.5 Rural 24,944 91.2 24,929 91.1 24,922 91.1 24,932 91.1 24,785 90.6 24,757 90.5 24,659 90.5 24,390 90.2 24,743 90.5 24,727 90.4 Geographical region Eastern 19,865 92.0 19,858 91.9 19,856 91.9 19,854 91.9 19,748 91.4 19,657 91.0 19,695 91.4 19,437 91.2 19,711 91.3 19,699 91.2 Central 14,539 91.8 14,536 91.8 14,527 91.7 14,526 91.7 14,442 91.2 14,389 90.8 14,364 90.9 14,208 90.8 14,453 91.3 14,435 91.2 Western 18,997 89.9 18,984 89.9 18,976 89.8 18,987 89.9 18,874 89.4 18,826 89.1 18,816 89.5 18,489 88.6 18,838 89.2 18,833 89.2 Note. For the visual acuity test, and diabetic retinopathy, peripheral neuropathy, and peripheral arterial disease screening, 197, 714, 15, and 13 participants were excluded, respectively, from the response rate calculation because the participants were ineligible for these examinations (e.g., a subject with a two-leg amputation was not eligible for a peripheral nerve examination). In addition, the definition of completion of all above examinations was under the condition of a complete interview (date of diabetes diagnosis and approximately 80% of the questions in our questionnaire were completed). Table 1. Response rates in the China National Diabetic Chronic Complications study
A total of 53,401 patients, with a mean age of 57.1 years, had complete interviews. Among them, 49.6% were males, 13.7% were young (18−44 years), 44.6% were middle-aged (45−59 years), 41.7% were elderly, 46.7% lived in rural areas, 37.2% resided in eastern regions, 27.2% in central regions, 35.6% in western regions, and 25.3% had high school or greater education levels. Males had a lower mean age and higher education level compared to females. The mean duration of diabetes was 7.0 years and the mean BMI was 25.7 kg/m2 (Table 2).
Characteristic Total Sex P value Male Female N (%) 53,401 (100.0) 26,471 (49.6) 26,930 (50.4) 0.047 Age, years 57.1 (10.1) 57.0 (10.1) 57.3 (10.0) 0.009 Age group (years), n (%) 0.125 18–44 7,289 (13.7) 3,694 (14.0) 3,595 (13.4) 45–59 23,834 (44.6) 11,774 (44.5) 12,060 (44.8) 60–74 22,278 (41.7) 11,003 (41.6) 11,275 (41.9) Setting, n (%) 0.166 Urban 28,457 (53.3) 14,186 (53.6) 14,271 (53.0) Rural 24,944 (46.7) 12,285 (46.4) 12,659 (47.0) Geographical region, n (%) 0.127 Eastern 19,865 (37.2) 9,806 (37.0) 10,059 (37.4) Central 14,539 (27.2) 7,139 (27.0) 7,400 (27.5) Western 18,997 (35.6) 9,526 (36.0) 9,471 (35.2) Educational levels, n (%) < 0.001 Middle school and below 39,910 (74.7) 18,111 (68.4) 21,799 (81.0) High school and above 13,491 (25.3) 8,360 (31.6) 5,131 (19.1) Diabetes duration, years 7.0 (5.9) 7.1 (6.0) 7.0 (5.9) 0.137 Body mass index, kg/m2 25.7 (3.6) 25.7 (3.5) 25.7 (3.8) 0.825 Note. Data were presented as the mean (standard deviation) for continuous variables and number (percentage) for categorical variables. Table 2. Characteristics of study participants with a complete interview
Based on the existing evidence, which was derived mostly from developed countries, patients with diabetes had a 20%−50% prevalence of various microvascular complications, as follows: diabetic retinopathy, the leading cause of blindness, affects approximately one-third of adults with diabetes[17-19]; diabetic nephropathy, the most common cause of end-stage renal disease[20-21], occurs in 20%−40% of patients with diabetes[22-24]; and diabetic peripheral neuropathy [DPN] may be present in approximately 50% of patients with diabetes[25]. Compared to those without diabetes, patients with diabetes have a 1.5-fold higher risk of developing CVD during their lifetime, which accounts for two-thirds of their deaths[26-27]. The reported prevalence of PAD varies greatly, and together with DPN, is related to an increased risk of lower extremity amputation[28]. Large-scale population-based studies regarding diabetes-related complications are currently focused on Europe, North America, and other high-income countries[29], while there is limited data available for the low- and middle-income countries with the largest increases in diabetes prevalence, such as China.
The China DiaChronic Study is the first database to be used for determining the epidemiologic characteristics of multiple chronic complications and co-morbidities of diabetes (retinopathy, nephropathy, peripheral neuropathy, PAD, and CVD), assess the attainment rates of metabolic targets, and implement standardized diagnosis and treatments in Chinese adults with diagnosed diabetes at the national level. The main implication of this study was to provide the scientific basis for the government to formulate prevention and control measures for chronic complications and co-morbidities of diabetes in China.
This study had several apparent strengths. First, this study was the first large-scale survey of multiple chronic complications and co-morbidities of diabetes based on primary health care management populations, while previous data on these complications and co-morbidities were mainly drawn from hospitals or regional areas, or only focused on a single disease[19,30-32]. Second, the sample was nationally representative through multistage stratified random sampling over 31 provinces, autonomous regions, and municipalities in China. Third, a unified protocol, the unified medical equipment, and the unified testing laboratory (except for fasting blood glucose levels in a local laboratory with unified quality control) were used for all study sites, ensuring the consistency and reliability of the data. Fourth, stringent quality control was implemented across the entire survey process. Before the investigation, all investigators and research staff underwent a training session. During the investigation, provincial supervisors selected at least 5% of the participants to be re-examined to confirm whether the investigators followed the standardized procedures for physical examination, peripheral neuropathy screening, and PAD screening. After the investigation, all collected data were uploaded to the information management platform, reviewed, and checked. Fifth, two fundus photographs were taken for each eye (one was centered on the optic disc and another on the macula), which reduced the likelihood of a missed diagnosis of diabetic retinopathy.
The study had several limitations. First, as a cross-sectional survey, causal relationships were not drawn. Second, lower response rates were found in younger participants in some study sites. However, the total sample size of the young participants was sufficient for a national analysis. Finally, some behavior-related questionnaires required the participant to recall situations in the past year (mainly the dietary survey), and there may be some recall biases.
Acknowledgments We thank all the investigators and participants for their contributions to this study.
We are grateful for the support from the Bethune Charitable Foundation, Novo Nordisk (China) Pharmaceuticals Co., Ltd., Lilly China, Merck Serono Co., Ltd., Bayer Healthcare Co., Ltd., Shenyang Sansheng Pharmaceutical Co., Ltd., and Shanghai Renhui Bio-pharmaceutical Co., Ltd.
Conflicts of
Interest The authors declare that they have no conflicts of interest. Author Contributions JIA Wei Ping, HOU Xu Hong, WANG Li Min, and HUANG Zheng Jing designed the study protocol. JIA Wei Ping, HOU Xu Hong, WANG Li Min, and ZHANG Mei developed the questionnaire. JIA Wei Ping, HOU Xu Hong, WANG Li Min, CHEN Si Yu, and WU Jing drafted the manuscript. All authors made substantial contributions to the study conception and design. All authors have read and approved the final manuscript.
Members of the China National Diabetic Chronic Complications Study Group are listed in Supplementary Table S6, available in www.besjournal.com.
Name Affiliation Xiaohui Guo Department of Endocrinology, Peking University First Hospital, Beijing, China Kai Wu Department of Endocrinology, Peking University First Hospital, Beijing, China Liming Chen Tianjin Metabolic Diseases Hospital & Tianjin Institute of Endocrinology, Tianjin Medical University, Tianjin, China Demin Liu Tianjin Metabolic Diseases Hospital & Tianjin Institute of Endocrinology, Tianjin Medical University, Tianjin, China Guangyao Song Department of Endocrinology, Hebei General Hospital, Shijiazhuang, Hebei, China Linyi Shu Department of Endocrinology, Hebei General Hospital, Shijiazhuang, Hebei, China Jing Yang Department of Endocrinology, The First Hospital of Shanxi Medical University, Taiyuan, Shanxi, China Yan Wang Department of Endocrinology, The First Hospital of Shanxi Medical University, Taiyuan, Shanxi, China Dongmei Li Department of Endocrinology, Inner Mongolia People's Hospital, Hohhot, Inner Mongolia, China Qiansha Guo Department of Endocrinology, Inner Mongolia People's Hospital, Hohhot, Inner Mongolia, China Ling Li Department of Endocrinology, Shengjing Hospital, China Medical University, Shenyang, Liaoning, China Na Wu Department of Endocrinology, Shengjing Hospital, China Medical University, Shenyang, Liaoning, China Yadong Sun Department of Endocrinology, Jilin Province People's Hospital, Changchun, Jilin, China Huifang Cheng Department of Endocrinology, Jilin Province People's Hospital, Changchun, Jilin, China Hongyu Kuang Department of Endocrinology, The First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, China Huijuan Zhang Department of Endocrinology, The First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, China Weiping Jia Department of Endocrinology and Metabolism, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai Diabetes Institute, Shanghai Key Laboratory of Diabetes Mellitus, Shanghai Clinical Center for Diabetes, Shanghai Key Clinical Center for Metabolic Disease, Shanghai, China Xuhong Hou Department of Endocrinology and Metabolism, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai Diabetes Institute, Shanghai Key Laboratory of Diabetes Mellitus, Shanghai Clinical Center for Diabetes, Shanghai Key Clinical Center for Metabolic Disease, Shanghai, China Dalong Zhu Department of Endocrinology, Drum Tower Hospital Affiliated to Nanjing University Medical School, Nanjing, Jiangsu, China Jian Zhu Department of Endocrinology, Drum Tower Hospital Affiliated to Nanjing University Medical School, Nanjing, Jiangsu, China Hong Li Department of Endocrinology, Sir Run Run Shaw Hospital Affiliated to School of Medicine, Zhejiang University, Hangzhou, Zhejiang, China Fenping Zheng Department of Endocrinology, Sir Run Run Shaw Hospital Affiliated to School of Medicine, Zhejiang University, Hangzhou, Zhejiang, China Qiu Zhang Department of Endocrinology, First Affiliated Hospital of Anhui Medical University, Hefei, Anhui, China Honglin Hu Department of Endocrinology, First Affiliated Hospital of Anhui Medical University, Hefei, Anhui, China Gang Chen Department of Endocrinology, Fujian Provincial Hospital, Fuzhou, Fujian, China Xingquan Yang Department of Endocrinology, Fujian Provincial Hospital, Fuzhou, Fujian, China Xiaoyang Lai Department of Endocrinology, The Second Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, China Jianping Liu Department of Endocrinology, The Second Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, China Li Chen Department of Endocrinology, Qilu Hospital of Shandong University, Jinan, Shandong, China Ming Dong Department of Endocrinology, Qilu Hospital of Shandong University, Jinan, Shandong, China Zhigang Zhao Department of Endocrinology, Yihe Hospital of Zhengzhou, Zhengzhou, Henan, China Jian Liu Department of Endocrinology, Yihe Hospital of Zhengzhou, Zhengzhou, Henan, China Guangda Xiang Department of Endocrinology, General Hospital of Central Theater Command, Wuhan, Hubei, China Junxia Zhang Department of Endocrinology, General Hospital of Central Theater Command, Wuhan, Hubei, China Zhiguang Zhou Institute of Metabolism and Endocrinology, Key Laboratory of Diabetes Immunology, Ministry of Education, National Clinical Research Center for Metabolic Diseases, The Second Xiangya Hospital and the Diabetes Center, Central South University, Changsha, Hunan, China Jian Peng Institute of Metabolism and Endocrinology, Key Laboratory of Diabetes Immunology, Ministry of Education, National Clinical Research Center for Metabolic Diseases, The Second Xiangya Hospital and the Diabetes Center, Central South University, Changsha, Hunan, China Jianping Weng Department of Endocrinology and Metabolic Disease, The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, Guangdong, China Longyi Zeng Department of Endocrinology and Metabolic Disease, The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, Guangdong, China Yuzhen Liang Department of Endocrinology, The Second Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China Guoqiao Li Department of Endocrinology, The Second Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China Kaining Chen Department of Endocrinology, Hainan General Hospital, Haikou, Hainan, China Leweihua Lin Department of Endocrinology, Hainan General Hospital, Haikou, Hainan, China Qifu Li Department of Endocrinology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China Qingfeng Cheng Department of Endocrinology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China Xingwu Ran Department of Endocrinology and Metabolism, West China Hospital, Sichuan University, Chengdu, Sichuan, China Dawei Chen Department of Endocrinology and Metabolism, West China Hospital, Sichuan University, Chengdu, Sichuan, China Hong Li Department of Endocrinology, First Affiliated Hospital of Kunming Medical University, Kunming, Yunnan, China Xin Nian Department of Endocrinology, First Affiliated Hospital of Kunming Medical University, Kunming, Yunnan, China Lihui Yang Department of Endocrinology, People's Hospital of Tibet Autonomous Region, Lhasa, Tibet, China Shuyou Meng Department of Endocrinology, People's Hospital of Tibet Autonomous Region, Lhasa, Tibet, China Jing Xu Department of Endocrinology, The Second Affiliated Hospital of Xi'an Jiaotong University, Xi'an, Shaanxi, China Junhong Long Department of Endocrinology, The Second Affiliated Hospital of Xi'an Jiaotong University, Xi'an, Shaanxi, China Jing Liu Department of Endocrinology, Gansu Provincial Hospital, Lanzhou, Gansu, China Qi Zhang Department of Endocrinology, Gansu Provincial Hospital, Lanzhou, Gansu, China Qingxiang Dai Geriatrics Department, Qinghai university Affiliated Hospital, Xining, Qinghai, China Xiaomin Xie Department of Endocrinology, The First People's Hospital of Yinchuan, Yinchuan, Ningxia, China Guirong Bai Department of Endocrinology, The First People's Hospital of Yinchuan, Yinchuan, Ningxia, China Jun Li Department of Endocrinology, The First Affiliated Hospital, School of medicine, Shihezi University, Shihezi, Xinjiang, China Tao Li Department of Endocrinology, The First Affiliated Hospital, School of medicine, Shihezi University, Shihezi, Xinjiang, China Zhong Dong Beijing Provincial Center for Disease Control and Prevention, Beijing, China Tao Zhang Beijing Provincial Center for Disease Control and Prevention, Beijing, China Sijia Liu Beijing Provincial Center for Disease Control and Prevention, Beijing, China Yong Yang Beijing Provincial Center for Disease Control and Prevention, Beijing, China Kun Geng Beijing Provincial Center for Disease Control and Prevention, Beijing, China Wenlong Zheng Tianjin Provincial Center for Disease Control and Prevention, Tianjin, China Zhihong Li Tianjin Provincial Center for Disease Control and Prevention, Tianjin, China Hui Wang Tianjin Provincial Center for Disease Control and Prevention, Tianjin, China Zuojun Wu Tianjin Provincial Center for Disease Control and Prevention, Tianjin, China Miao Wang Tianjin Provincial Center for Disease Control and Prevention, Tianjin, China Jixin Sun Hebei Provincial Center for Disease Control and Prevention, Hebei, China Jianwei Zhou Hebei Provincial Center for Disease Control and Prevention, Hebei, China Jun An Hebei Provincial Center for Disease Control and Prevention, Hebei, China Huaqing Shen Hebei Provincial Center for Disease Control and Prevention, Hebei, China Yanfang Li Hebei Provincial Center for Disease Control and Prevention, Hebei, China Zeping Ren Shanxi Provincial Center for Disease Control and Prevention, Shanxi, China Xiuli Xue Shanxi Provincial Center for Disease Control and Prevention, Shanxi, China Shaohui Jia Shanxi Provincial Center for Disease Control and Prevention, Shanxi, China Yongping Zheng Shanxi Provincial Center for Disease Control and Prevention, Shanxi, China Jiaoxia Li Shanxi Provincial Center for Disease Control and Prevention, Shanxi, China Yonggang Qian Inner Mongolia Provincial Center for Disease Control and Prevention, Inner Mongolia, China Ping Ma Inner Mongolia Provincial Center for Disease Control and Prevention, Inner Mongolia, China Yan Su Inner Mongolia Provincial Center for Disease Control and Prevention, Inner Mongolia, China Liang Cao Inner Mongolia Provincial Center for Disease Control and Prevention, Inner Mongolia, China Xuyi Yang Inner Mongolia Provincial Center for Disease Control and Prevention, Inner Mongolia, China Guowei Pan Liaoning Provincial Center for Disease Control and Prevention, Liaoning, China Guangzhi Pan Liaoning Provincial Center for Disease Control and Prevention, Liaoning, China Ling Jin Liaoning Provincial Center for Disease Control and Prevention, Liaoning, China Quanfu Yu Liaoning Provincial Center for Disease Control and Prevention, Liaoning, China Yunfei Liu Liaoning Provincial Center for Disease Control and Prevention, Liaoning, China Yingli Zhu Jilin Provincial Center for Disease Control and Prevention, Jilin, China Zhifang Cheng Jilin Provincial Center for Disease Control and Prevention, Jilin, China Jun Yang Jilin Provincial Center for Disease Control and Prevention, Jilin, China Chundi Jia Jilin Provincial Center for Disease Control and Prevention, Jilin, China Qing Wang Jilin Provincial Center for Disease Control and Prevention, Jilin, China Shichun Yan Heilongjiang Provincial Center for Disease Control and Prevention, Heilongjiang, China Jingyang Huang Heilongjiang Provincial Center for Disease Control and Prevention, Heilongjiang, China Yumei Chi Heilongjiang Provincial Center for Disease Control and Prevention, Heilongjiang, China Li Zhang Heilongjiang Provincial Center for Disease Control and Prevention, Heilongjiang, China Ruifa Pang Heilongjiang Provincial Center for Disease Control and Prevention, Heilongjiang, China Yan Shi Shanghai Provincial Center for Disease Control and Prevention, Shanghai, China Yan Lu Shanghai Provincial Center for Disease Control and Prevention, Shanghai, China Yiling Wu Shanghai Provincial Center for Disease Control and Prevention, Shanghai, China Jie Yu Shanghai Provincial Center for Disease Control and Prevention, Shanghai, China Chunxiang Wu Shanghai Provincial Center for Disease Control and Prevention, Shanghai, China Jinyi Zhou Jiangsu Provincial Center for Disease Control and Prevention, Jiangsu, China Yunxia Wu Jiangsu Provincial Center for Disease Control and Prevention, Jiangsu, China Ning Zhang Jiangsu Provincial Center for Disease Control and Prevention, Jiangsu, China Jing Sun Jiangsu Provincial Center for Disease Control and Prevention, Jiangsu, China Xiumei Tian Jiangsu Provincial Center for Disease Control and Prevention, Jiangsu, China Jieming Zhong Zhejiang Provincial Center for Disease Control and Prevention, Zhejiang, China Jingying Chen Zhejiang Provincial Center for Disease Control and Prevention, Zhejiang, China Kaixu Xie Zhejiang Provincial Center for Disease Control and Prevention, Zhejiang, China Lingjuan Fu Zhejiang Provincial Center for Disease Control and Prevention, Zhejiang, China Xiaohua Wang Zhejiang Provincial Center for Disease Control and Prevention, Zhejiang, China Yeji Chen Anhui Provincial Center for Disease Control and Prevention, Anhui, China Ling Zeng Anhui Provincial Center for Disease Control and Prevention, Anhui, China Zhenqian Cao Anhui Provincial Center for Disease Control and Prevention, Anhui, China Maomin Yang Anhui Provincial Center for Disease Control and Prevention, Anhui, China Biao Hu Anhui Provincial Center for Disease Control and Prevention, Anhui, China Wenling Zhong Fujian Provincial Center for Disease Control and Prevention, Fujian, China Qingyan Liu Fujian Provincial Center for Disease Control and Prevention, Fujian, China Zhiding Huang Fujian Provincial Center for Disease Control and Prevention, Fujian, China Qingbin Lai Fujian Provincial Center for Disease Control and Prevention, Fujian, China Yuyu Zhang Fujian Provincial Center for Disease Control and Prevention, Fujian, China Liping Zhu Jiangxi Provincial Center for Disease Control and Prevention, Jiangxi, China Yujing Zhao Jiangxi Provincial Center for Disease Control and Prevention, Jiangxi, China Wuming Tao Jiangxi Provincial Center for Disease Control and Prevention, Jiangxi, China Yonghai Tu Jiangxi Provincial Center for Disease Control and Prevention, Jiangxi, China Lin Zhou Jiangxi Provincial Center for Disease Control and Prevention, Jiangxi, China Xiaolei Guo Shandong Provincial Center for Disease Control and Prevention, Shandong, China Benzheng Chai Shandong Provincial Center for Disease Control and Prevention, Shandong, China Liping Ding Shandong Provincial Center for Disease Control and Prevention, Shandong, China Yuewei Zou Shandong Provincial Center for Disease Control and Prevention, Shandong, China Dongzhi Li Shandong Provincial Center for Disease Control and Prevention, Shandong, China Li Hua Shandong Provincial Center for Disease Control and Prevention, Shandong, China Shixian Feng Henan Provincial Center for Disease Control and Prevention, Henan, China Jianli Guo Henan Provincial Center for Disease Control and Prevention, Henan, China Wanguang Liu Henan Provincial Center for Disease Control and Prevention, Henan, China Qingxiang Li Henan Provincial Center for Disease Control and Prevention, Henan, China Yunzhi Zheng Henan Provincial Center for Disease Control and Prevention, Henan, China Minli Xu Henan Provincial Center for Disease Control and Prevention, Henan, China Lan Zhang Hubei Provincial Center for Disease Control and Prevention, Hubei, China Chunbo Li Hubei Provincial Center for Disease Control and Prevention, Hubei, China Yingchao Wan Hubei Provincial Center for Disease Control and Prevention, Hubei, China Chi Hu Hubei Provincial Center for Disease Control and Prevention, Hubei, China Shengping Xu Hubei Provincial Center for Disease Control and Prevention, Hubei, China Biyun Chen Hunan Provincial Center for Disease Control and Prevention, Hunan, China Huilin Liu Hunan Provincial Center for Disease Control and Prevention, Hunan, China Xiaojia Bian Hunan Provincial Center for Disease Control and Prevention, Hunan, China Wenwei Chen Hunan Provincial Center for Disease Control and Prevention, Hunan, China Honghua Li Hunan Provincial Center for Disease Control and Prevention, Hunan, China Yanjun Xu Guangdong Provincial Center for Disease Control and Prevention, Guangdong, China Fan Weng Guangdong Provincial Center for Disease Control and Prevention, Guangdong, China Hong Wu Guangdong Provincial Center for Disease Control and Prevention, Guangdong, China Weijin Zhang Guangdong Provincial Center for Disease Control and Prevention, Guangdong, China Liankai Zhu Guangdong Provincial Center for Disease Control and Prevention, Guangdong, China Jun Meng Guangxi Provincial Center for Disease Control and Prevention, Guangxi, China Jin Yang Guangxi Provincial Center for Disease Control and Prevention, Guangxi, China Yongsong Zeng Guangxi Provincial Center for Disease Control and Prevention, Guangxi, China Gaoke Zhai Guangxi Provincial Center for Disease Control and Prevention, Guangxi, China Lingfeng Qin Guangxi Provincial Center for Disease Control and Prevention, Guangxi, China Yi Lu Guangxi Provincial Center for Disease Control and Prevention, Guangxi, China Zhenwang Fu Hainan Provincial Center for Disease Control and Prevention, Hainan, China Shukuan Wu Hainan Provincial Center for Disease Control and Prevention, Hainan, China Caigang Li Hainan Provincial Center for Disease Control and Prevention, Hainan, China Na Wang Hainan Provincial Center for Disease Control and Prevention, Hainan, China Lianfen Chen Hainan Provincial Center for Disease Control and Prevention, Hainan, China Xianbin Ding Chongqing Provincial Center for Disease Control and Prevention, Chongqing, China Qi Zhou Chongqing Provincial Center for Disease Control and Prevention, Chongqing, China Yiling Xie Chongqing Provincial Center for Disease Control and Prevention, Chongqing, China Rui Chen Chongqing Provincial Center for Disease Control and Prevention, Chongqing, China Dongsheng Yang Chongqing Provincial Center for Disease Control and Prevention, Chongqing, China Ying Deng Sichuan Provincial Center for Disease Control and Prevention, Sichuan, China Youping Hu Sichuan Provincial Center for Disease Control and Prevention, Sichuan, China Bo Huang Sichuan Provincial Center for Disease Control and Prevention, Sichuan, China Ping Wang Sichuan Provincial Center for Disease Control and Prevention, Sichuan, China Peng Cai Sichuan Provincial Center for Disease Control and Prevention, Sichuan, China Changyan Peng Sichuan Provincial Center for Disease Control and Prevention, Sichuan, China Xiaofang Chen Sichuan Provincial Center for Disease Control and Prevention, Sichuan, China Ling Li Guizhou Provincial Center for Disease Control and Prevention, Guizhou, China Liang Xiao Guizhou Provincial Center for Disease Control and Prevention, Guizhou, China Chenglin Wang Guizhou Provincial Center for Disease Control and Prevention, Guizhou, China Chaogang Tan Guizhou Provincial Center for Disease Control and Prevention, Guizhou, China Daobin Chen Guizhou Provincial Center for Disease Control and Prevention, Guizhou, China Min Chen Guizhou Provincial Center for Disease Control and Prevention, Guizhou, China Mingfang Qin Yunnan Provincial Center for Disease Control and Prevention, Yunnan, China Zhaomin Lei Yunnan Provincial Center for Disease Control and Prevention, Yunnan, China Jianzhi Qiu Yunnan Provincial Center for Disease Control and Prevention, Yunnan, China Wei Yu Yunnan Provincial Center for Disease Control and Prevention, Yunnan, China Yunfei Li Yunnan Provincial Center for Disease Control and Prevention, Yunnan, China Guoxia Bai Tibet Provincial Center for Disease Control and Prevention, Tibet, China Ying Wang Tibet Provincial Center for Disease Control and Prevention, Tibet, China Lin Qiu Shaanxi Provincial Center for Disease Control and Prevention, Shaanxi, China Ning Wang Shaanxi Provincial Center for Disease Control and Prevention, Shaanxi, China Xudong Zhao Shaanxi Provincial Center for Disease Control and Prevention, Shaanxi, China Ani Yan Shaanxi Provincial Center for Disease Control and Prevention, Shaanxi, China Jianfei Liu Shaanxi Provincial Center for Disease Control and Prevention, Shaanxi, China Tingcai Wang Gansu Provincial Center for Disease Control and Prevention, Gansu, China Kaihua Hao Gansu Provincial Center for Disease Control and Prevention, Gansu, China Zaihong Zhang Gansu Provincial Center for Disease Control and Prevention, Gansu, China Zhanqi Xian Gansu Provincial Center for Disease Control and Prevention, Gansu, China Tenghuan Ma Gansu Provincial Center for Disease Control and Prevention, Gansu, China Zhihua Xu Qinghai Provincial Center for Disease Control and Prevention, Qinghai, China Yi Yang Ningxia Provincial Center for Disease Control and Prevention, Ningxia, China Hongli Wang Ningxia Provincial Center for Disease Control and Prevention, Ningxia, China Rong Li Ningxia Provincial Center for Disease Control and Prevention, Ningxia, China Zhonggang Zhao Ningxia Provincial Center for Disease Control and Prevention, Ningxia, China Caixia Fan Ningxia Provincial Center for Disease Control and Prevention, Ningxia, China Purhati Xinjiang Provincial Center for Disease Control and Prevention, Xinjiang, China Hongjun Xu Xinjiang Provincial Center for Disease Control and Prevention, Xinjiang, China Liping Gao Xinjiang Provincial Center for Disease Control and Prevention, Xinjiang, China Table S6. China National Diabetic Chronic Complications Study Group
HTML
 21502Supplementary Materials.pdf
21502Supplementary Materials.pdf
|

|








 Quick Links
Quick Links
 DownLoad:
DownLoad: