-
Chronic sinusitis (CRS), with or without nasal polyps (CRSwNP/CRSsNP), is a common chronic inflammatory disease of the nasal cavity and paranasal sinus mucosa. CRS symptoms mainly include nasal congestion, runny nose, headache, swelling of the face, and olfactory dysfunction or loss, and the disease duration is at least 12 consecutive weeks[1]. According to some multicenter studies, CRS had a mean prevalence of 10.9% (range of 6.9%–27.1%) in 19 Western centers, from 2011 to 2013[2] and 8.0% (range of 4.8%–9.7%) in seven Chinese centers in 2012[3]. CRS is not a life-threatening disease, but CRS patients often suffer from prolonged and repeated attacks of the disease, which significantly reduces their quality of life[4]. Surgical treatment is usually adopted for CRS in cases where drug treatments are ineffective[5].
Functional endoscopic sinus surgery (ESS) is currently the standard nasal surgery for treatment-resistant CRS[6]. ESS is safe, minimally invasive, and can improve the quality of life of patients with severe CRSwNP and CRSsNP; however, some patients (nearly 3/4) have no change in odor perception after operation and about 7%–10% of patients may have deteriorated olfactory function[7-9]. This may be related to the complex pathogenesis of CRS, involving intrinsic (such as infection, allergic inflammation, metabolic diseases, and genetics) and environmental factors (such as air pollution and occupational exposure)[5]. Besides, patients of low socioeconomic status (SES) may have delayed medical diagnosis and limited access to treatment and care[10]; until now only three studies have suggested that low SES may increase symptom severity or reduce the quality of life after ESS[11-13]. However, these studies did not examine the direct or comprehensive effects of socioeconomic factors on prognosis after surgery; moreover, all the data came from high-income countries. As a developing country, China has an imbalanced allocation of medical and health care resources[14]. We aimed to examine the association between SES and prognosis in patients after surgery for CRS, focusing on postoperative inflammatory outcomes and recurrence rates, especially in developing countries or countries with relatively unbalanced health care systems.
-
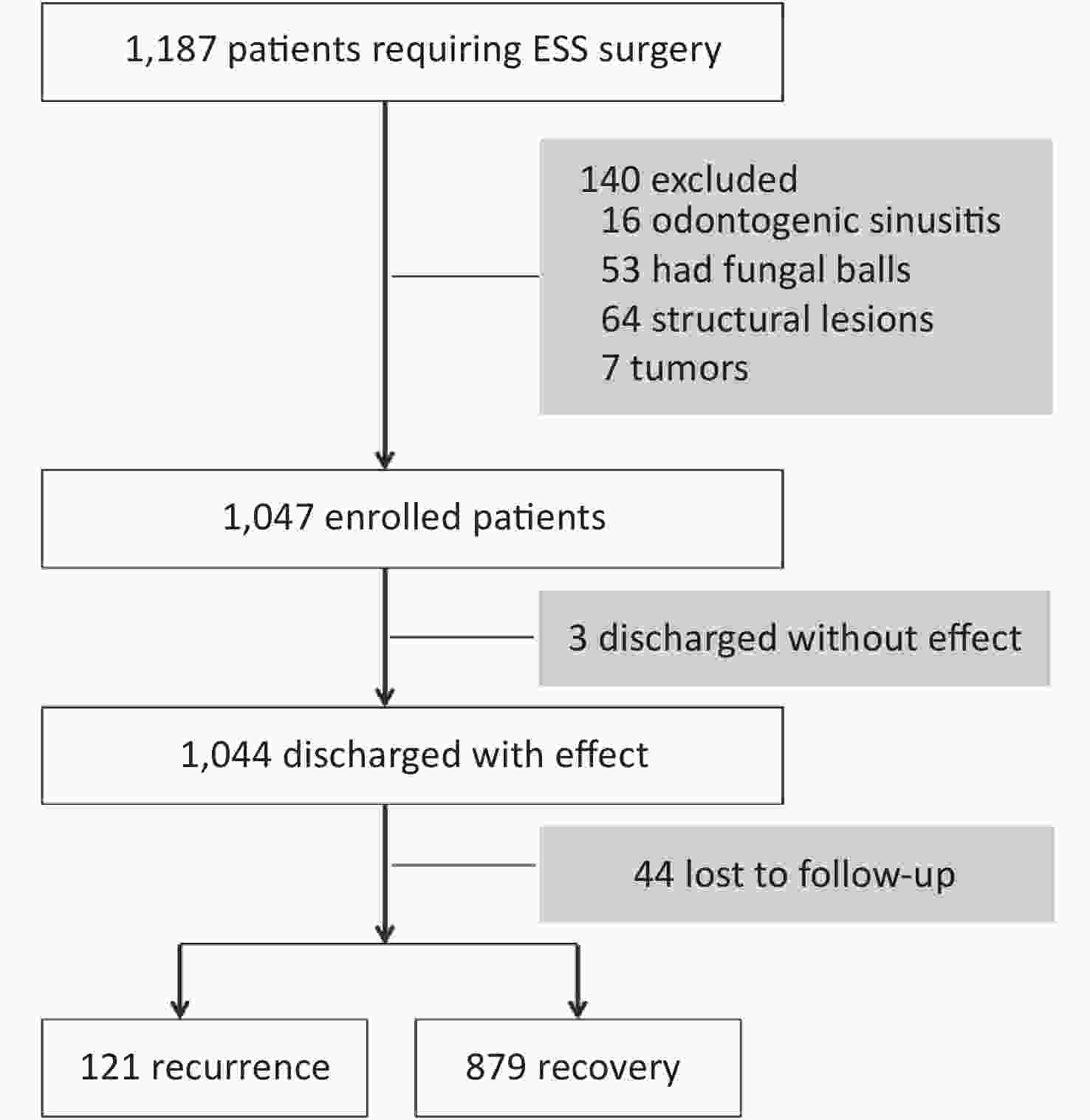
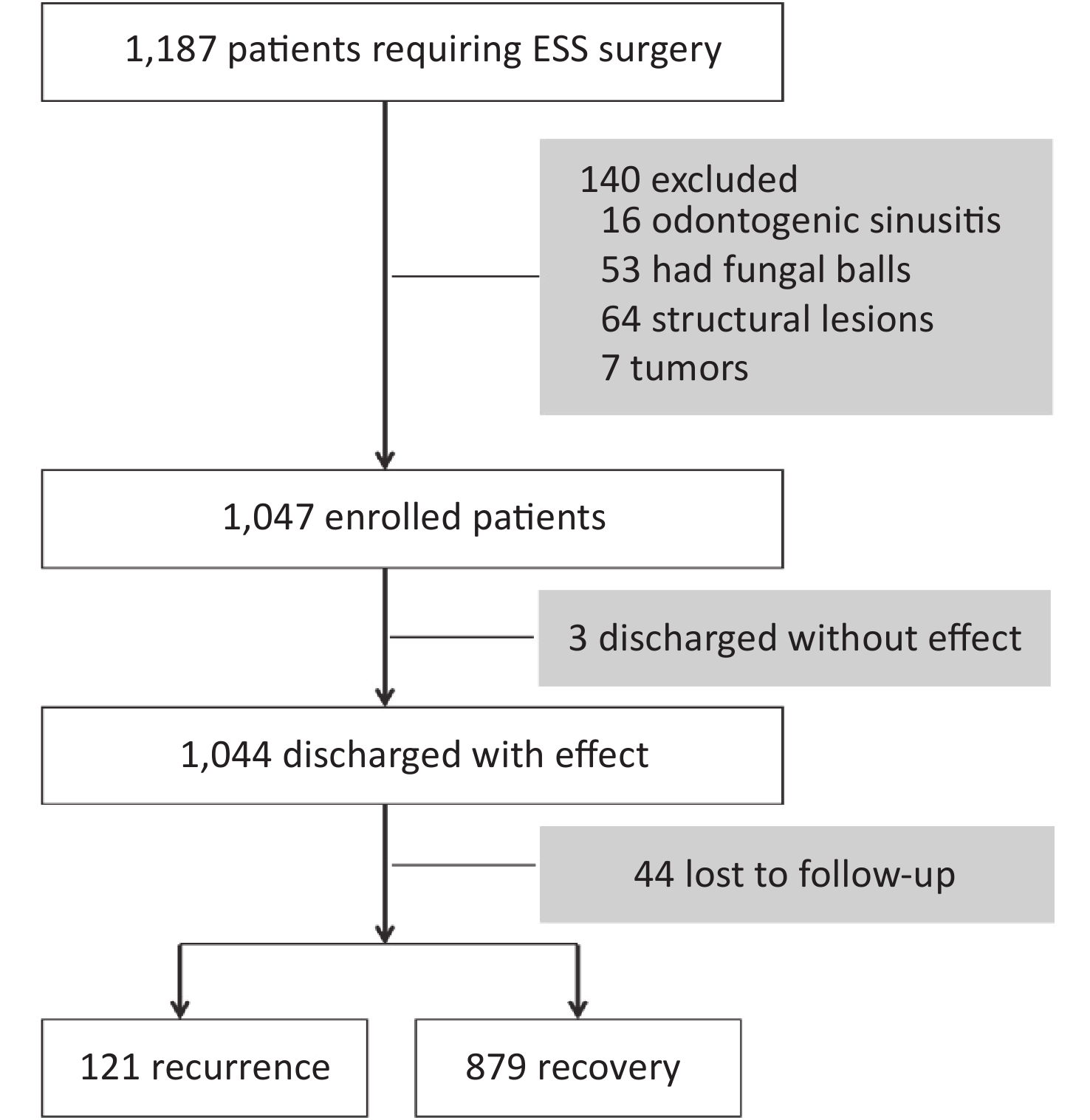
This observational cohort study included a total of 1,047 patients with severe CRS who underwent ESS in the Department of Otolaryngology, First Affiliated Hospital of China Medical University (Shenyang, China) in a 33-month period between February 2019 and October 2021. These patients were aged 18–65 years at the time of operation. The demographic and clinical indicators were also collected. Exclusion criteria were: 1) Patients undergoing ESS for other reasons, including odontogenic sinusitis, fungal balls, structural lesions, benign and malignant tumors; 2) Patients with severe heart disease, hypertension, diabetes, chronic obstructive pulmonary disease, or liver and kidney disease. This study was approved by the medical ethics committee of First Affiliated Hospital of China Medical University. Each included subject signed a written informed consent and could withdraw from the study unconditionally.
-
For each CRS patient, baseline demographic and disease characteristics were collected by experienced attending physician through face-to-face questionnaires and from the inpatient medical record system. Clinical information included CRS classification, preoperative biochemical indicators, nasal endoscopy, and sinus computerized tomography (CT) scan. The diagnostic criteria for CRS were based on the CRS Guidelines for Diagnosis and Treatment[15], and patients with unsatisfactory results from drug treatment for 3 months, consecutively, were subjected to surgical treatment. Demographic information was derived from medical records and questionnaires during hospitalization, including SES (occupation, education, and income), living environment (pets and decoration), work stress, and family stress.
The patients came to our hospital for outpatient follow-up 2 and 4 weeks after discharge, and every 4 weeks thereafter. During the follow-up period, we assessed the postoperative sinus recovery through endoscopic views (Supplementary Figure S1, available in www.besjournal.com), Lund-Kennedy endoscopy score, and postoperative status of care, diet, and rest. Where necessary, CT scan of paranasal sinuses was repeated and compared with preoperative results. CRS patients who did not come to our hospital for outpatient follow-up within the prescribed time limit were considered lost to follow-up if they could not be reached after three phone calls. If recurrence was found, we continued to follow up. The longest follow-up was 72 weeks, and patients lost to follow-up were censored as recovery on the date of the last contact. CRS is a chronic disease, and although inflammation may persist endoscopically, patients may have significant improvement in the quality of life. The recurrence of CRS is not fully-defined and is subjective in the clinical setting; hence, we used the aforementioned indicators to comprehensively assess whether there was recurrence or not.
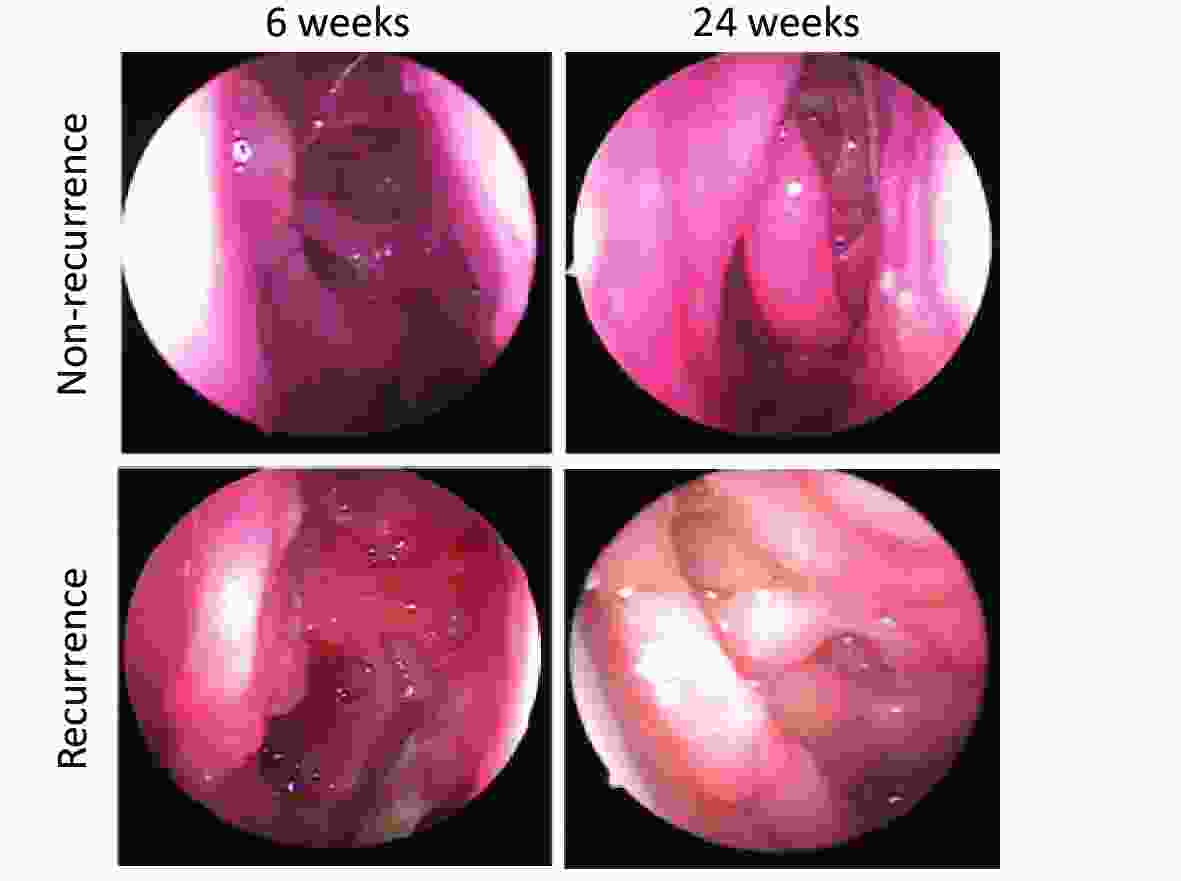
Figure S1. Typical endoscopic views (recurrence and nonrecurrence) of patients who underwent ESS, obtained at 6 weeks and 24 weeks postoperatively.
Based on previous factors[13,16], we established a comprehensive scoring system of SES, which comprises the patient’s occupation, education, and income 1 year before surgery. Annual household income (unit: RMB) was divided into three grades and scored: low (< 5,000/month, 1 point), middle (5,000–8,000/month, 2 points), and high (8,000–/month, 3 points). Occupation was divided into three grades and scored: manual workers, farmers, unemployed people (low, 1 point), businessmen or employees (middle, 2 points), professionals, managers or government employees (high, 3 points). Similarly, education was divided into three grades and scored: lower than high school (low, 1 point), high school graduation or equivalent (middle, 2 points), university graduation or above (high, 3 points). Next, we calculated the total SES scores of CRS patients (3–9 points) and divided patients into approximate terciles of SES status distribution: low (≤ 4 points), middle (5–7 points), and high (≥ 8 points).
-
The follow-up outcome of this study is the all-cause non-recovery (recurrence) rate, that is, the postoperative non-recovery rate of CRS patients influenced by various factors during the follow-up period.
-
Based on the literature[17-20] and clinical experience, we screened for covariates that may affect recovery rates, including patient demographics [sex, body mass index (BMI), and medical insurance] and clinical risk factors [age at operation years, nasal polyposis, smoking, alcohol, dietary patterns, pets, new furniture/redecoration, stressful work-family events, staying up late, fractional exhaled nitric oxide (FeNO), fractional nasal nitric oxide (FnNO), hemoglobin (Hb), and immunoglobulin E (IgE)].
-
We used the Shapiro–Wilk method to test for normality of all continuous variables, and the results are expressed as the median (Interquartile range, IQR) (25th–75th percentile). The Kruskal-Wallis test was used to compare the differences in continuous variables among the three groups (terciles SES status), and Chi-square test or continuity-corrected Chi-square test was used to determine the differences in categorical variables, which are expressed as frequencies (percentages).
The Kaplan-Meier method was used to calculate the recovery rate after ESS and plot the survival curves. The log-rank test was used to compare the postoperative recovery rates across the three SES groups. Through a multivariate Cox proportional hazards regression model, we adjusted other covariates to analyze the effect of SES status (low, middle, and high) on all-cause recovery, estimated adjusted hazard ratio (HR) and its 95 % confidence interval (CI), and the interaction between SES and some potential covariates (with or without nasal polyps, medical insurance, and dietary patterns). These covariates, which may affect postoperative recovery, were screened by using univariate Cox regression models and clinical experience. Because of the differences in demographic and clinical information among CRS patients in different SES groups, we first screened out the covariates and incorporated them into the multivariate Cox regression model together with SES to obtain the effect of SES on recovery after adjusting for covariates. When the categorical variable had more than two categories, it was converted into a dummy variable and then included in the model for analysis. Considering the possibility of loss to follow-up due to recovery, we assumed that all of patients lost to follow-up recovered, and we performed a sensitivity analysis to test the robustness of our main analysis. A P value < 0.05 indicated statistical significance. The data were analyzed by using SPSS software for Windows, version 20.0 (IBM SPSS, Inc., Chicago, IL, USA).
-
Based on the pilot trial, we assumed a 72-week recovery rate of 40% for patients of low SES in the study, assuming α = 0.05 and β = 0.10. The Kaplan-Meier model analysis showed that 237 CRS patients were in low and middle SES groups, and the recovery rates of the two groups were significantly different. Assuming a 10% loss to follow-up rate, this study required at least 790 CRS patients. Finally, 1,047 CRS patients were included in the survival analysis to meet the sample size requirement.
-
From February 1, 2019 to October 31, 2021, 1,047 ESS-treated CRS patients were enrolled in this study (Table 1, Figure 1). The median age of patients at surgery in this cohort was 36 (IQR 27–46) years. Of the patients, 600 (57.3%) patients were male, 764 (73.0%) patients had CRSwNP, 315 (30.1%) patients belonged to low-income status, and 362 (34.6%) patients were farmers, temporary workers, or unemployed, and 172 (16.4%) patients had no medical insurance and paid at their own expense. Compared with patients in the middle SES group, those in the low or high SES groups were older at the time of surgery (P < 0.001) and had higher preoperative FnNO levels (P = 0.039). In addition, the proportion of patients with medical insurance in the high SES group was higher than that in the low and middle SES groups (P < 0.001).
Table 1. Baseline characteristics and clinical features of patients with severe chronic rhinosinusitis (CRS) (n = 1,047) by socioeconomic status tertiles
Characteristics Total (n = 1,047) Low (n = 310) Middle (n = 399) High (n = 338) P-value Age at operation years 34.2 (27.5−46.1) 36.8 (31.8−50.8) 30.6 (24.3−48.9) 36.6 (30.6−44.1) < 0.001 Sex, n (%) 0.626 Males 600 (57.3) 183 (59.0) 230 (57.6) 187 (55.3) Females 447 (42.7) 127 (41.0) 169 (42.4) 151 (44.7) BMI, kg/m2 22.6 (20.6−27.2) 22.8 (20.7−27.3) 22.5 (20.6−27.6) 22.0 (20.4−26.7) 0.594 Educationa, n (%) < High school 92 (8.8) 83 (27.0) 9 (2.2) 0 (0.0) < 0.001 High school 273 (26.2) 178 (58.0) 92 (23.1) 3 (0.9) ≥ College 676 (65.0) 46 (15.0) 298 (74.7) 332 (99.1) Occupation, n (%) < 0.001 Low 362 (34.6) 169 (54.5) 187 (46.9) 6 (1.8) Medium 313 (29.9) 138 (44.5) 89 (22.3) 86 (25.4) High 372 (35.5) 3 (1.0) 123 (30.8) 246 (72.8) Household income/montha, n (%) < 0.001 < ¥5,000 315 (30.2) 124 (40.0) 151 (37.8) 40 (11.9) ¥5,000–8,000 638 (61.1) 186 (60.0) 243 (60.9) 209 (62.4) > ¥8,000 91 (8.7) 0 (0.0) 5 (1.3) 86 (25.7) Nasal polyposis, n (%) 0.607 Without 283 (27.0) 80 (25.8) 105 (26.3) 98 (29.0) With 764 (73.0) 230 (74.2) 294 (73.7) 240 (71.0) Smoking, n (%) 0.538 No 683 (65.2) 203 (65.5) 267 (66.9) 213 (63.0) Yes 364 (34.8) 107 (34.5) 132 (33.1) 125 (37.0) Alcohol, n (%) 0.302 No 697 (66.6) 212 (68.4) 271 (67.9) 214 (63.3) Yes 350 (33.4) 98 (31.6) 128 (32.1) 124 (36.7) Dietary patternsa, n (%) 0.466 Vegetarian-based 134 (13.3) 36 (13.2) 56 (14.0) 42 (12.4) Meat-based 67 (6.6) 24 (8.8) 25 (6.3) 18 (5.3) Mixed 809 (80.1) 213 (78.0) 318 (79.7) 278 (82.2) Furry/feathery Pets, n (%) 0.356 No 892 (85.2) 271 (87.4) 339 (85.0) 282 (83.4) Yes 155 (14.8) 39 (12.6) 60 (15.0) 56 (16.6) New furniture/redecoration, n (%) 0.593 No 902 (86.2) 267 (86.1) 339 (85.0) 296 (87.6) Yes 145 (86.1) 43 (13.9) 60 (15.0) 42 (12.4) Stressful work or family events during the first 1 yearab, n (%) 0.235 No 711 (68.1) 207 (66.8) 284 (71.2) 220 (65.7) Yes 333 (31.9) 103 (33.2) 115 (28.8) 115 (34.3) Often stay up late, n (%) 0.296 No 788 (75.3) 243 (78.4) 293 (73.4) 252 (74.6) Yes 259 (24.7) 67 (21.6) 106 (26.6) 86 (25.4) Before surgery, n (%) FeNO, ppb 24.0 (16.0−34.0) 22.0 (15.0−36.0) 24.0 (18.0−33.0) 26.0 (19.0−33.0) 0.293 FnNO, ppb 201.0 (151.0−322.0) 220.0 (168.0−335.0) 187.0 (145.0−311.0) 213.0 (169.0−323.0) 0.039 Hb, g/L 146.0 (136.0−161.0) 146.5 (140.0−166.0) 142.0 (121.0−162.0) 146.0 (136.0−157.0) 0.711 IgE, IU/mL 44.4 (30.8−66.0) 42.3 (30.3−77.4) 46.0 (31.1−56.0) 47.6 (34.9−60.8) 0.284 Medical insurance, n (%) < 0.001 No 172 (16.4) 83 (26.8) 86 (21.6) 3 (0.9) Yes 875 (83.6) 227 (73.2) 313 (78.4) 335 (99.1) Note. aTotal numbers were not equal to 1,047 for these characteristics due to missing data. bAmong work, separation/divorce, loss of job, serious health problem, or death of a family member or close relative. Values are n (%) or median (IQR). -
Kaplan-Meier analysis (Figure 2, Supplementary Table S1, available in www.besjournal.com) showed that the recovery rates of 1,047 CRS patients at 12 weeks and 24 weeks after operation were 19.1% (95% CI: 18.3%–19.9%) and 44.7% (95% CI: 43.7%–45.7%), respectively.
The log-rank tests showed that after follow-up at 24 weeks, the recovery rate (90.4%, 95% CI: 89.6%–91.2%) of patients of middle SES was higher than those of patients of low SES (13.5%, 95% CI: 12.8%–14.2%) and high SES (31.7%, 95% CI: 30.7%–32.7%) (log-rank P < 0.001). In addition, multivariate Cox regression model analysis showed that SES had no association with nasal polyps (Pinteraction = 0.189), medical insurance mode (Pinteraction = 0.143), and dietary pattern (Pinteraction = 0.438) (Supplementary Table S2, available in www.besjournal.com).
Table S2. Multivariable Cox regression model of an interaction between socioeconomic status (SES) and nasal polyposis, medical insurance, and dietary patterns
Interaction β Wald HR (95% CI) P−Value SES × nasal polyps 0.001 1.722 1.001 (0.999−1.003) 0.189 SES × medical insurance −0.056 2.144 0.946 (0.877−1.019) 0.143 SES × dietary patterns 0.092 0.601 1.097 (0.868−1.385) 0.438 Note. HR, hazard ratio; NA, not applicable. Based on the literature, we selected variables (surgical age, BMI, nasal polyps, smoking, dietary pattern, stress events, FeNO, FnNO, Hb, and medical insurance mode) that might affect prognosis and carried out univariate Cox regression model analysis, followed by multivariate Cox regression model analysis to determine their association with SES. Next, we obtained the influence of SES after adjusting the covariates for recovery rate (Figure 3, Table 2).
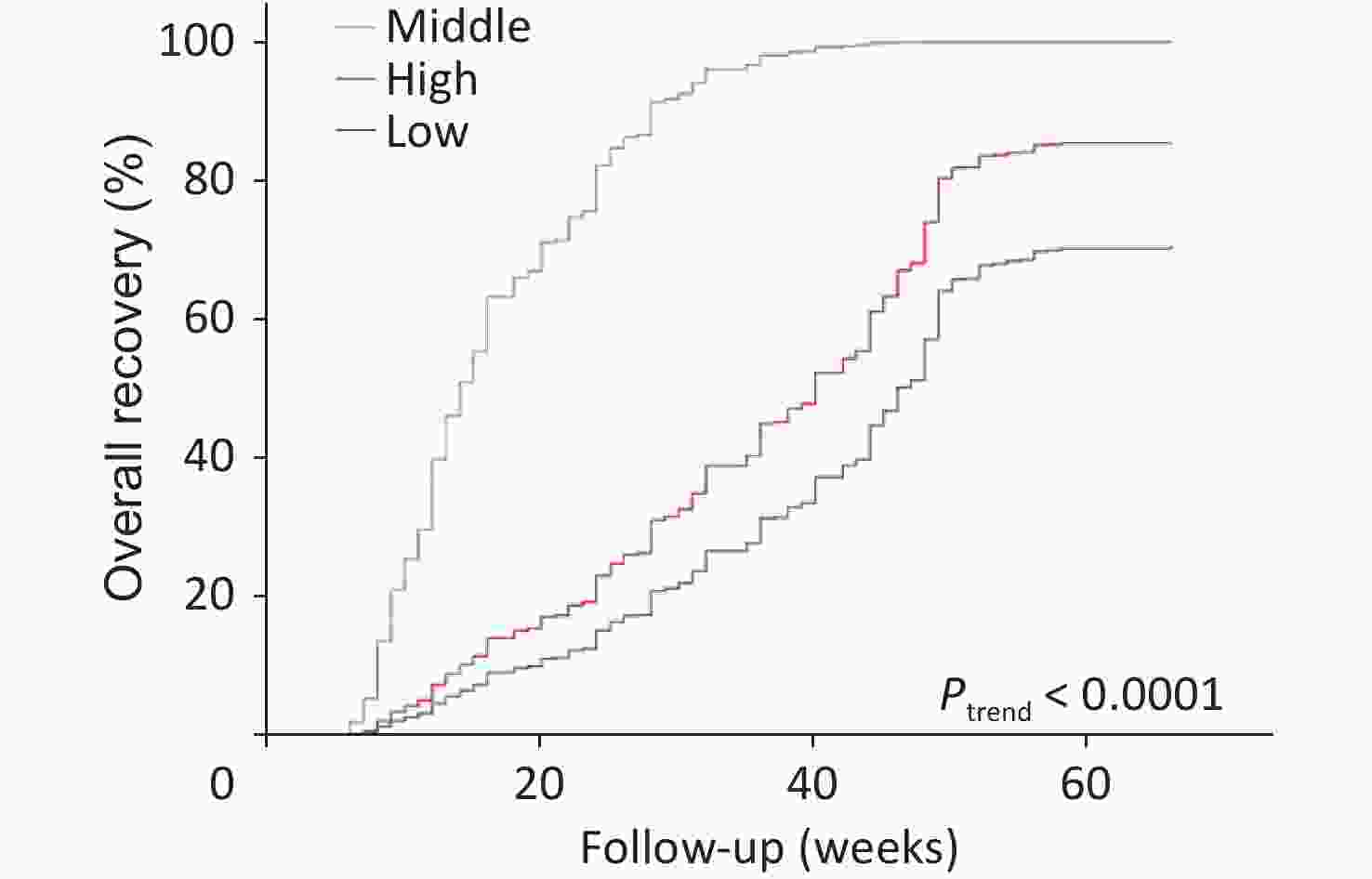
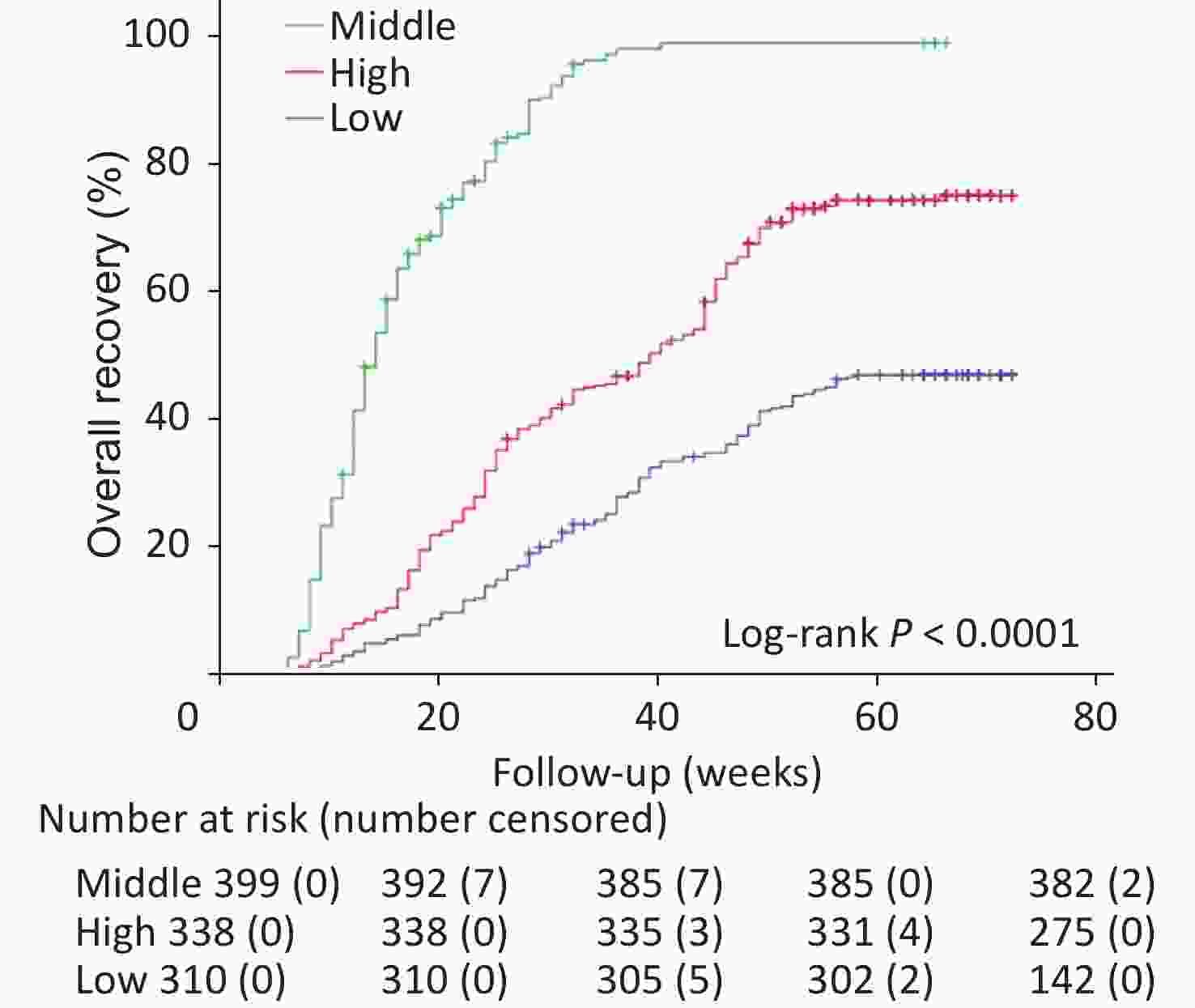
Figure 3. Adjusted survival curves for all-cause recurrence by socioeconomic status. Models were adjusted for age at operation, sex, BMI, nasal polyposis, smoking, dietary patterns, stressful family events during the year that precede the operation, FeNO, FnNO, Hb, and medical insurance. FeNO, fractional exhaled nitric oxide; FnNO, fractional nasal nitric oxide; and Hb, hemoglobin.
Table 2. Univariable and multivariable Cox regression model of factors associated with all-cause recurrence
Characteristics All-cause non-recovery Crude HR (95% CI) P-value Adjusted HR* (95% CI) P-value Socioeconomic status Low 10.42 (8.55−12.66) < 0.001 7.69 (6.17−9.71) < 0.001 High 6.54 (5.49−7.81) < 0.001 6.19 (4.78−7.93) < 0.001 Middle 1 (ref) 1 (ref) Age at operation, years 1.01 (1.00−1.02) 0.013 1.01 (0.99−1.02) 0.128 Sex Males 0.86 (0.72−1.01) 0.27 0.93 (0.79−1.08) 0.313 Females 1 (ref) 1 (ref) BMI, kg/m2 1.02 (1.00−1.03) 0.19 NA Nasal polyposis Without 0.75 (0.65−0.87) < 0.001 0.83 (0.69−1.00) 0.039 With 1 (ref) 1 (ref) Smoking NA No 0.87 (0.76−0.99) 0.039 Yes 1 (ref) Alcohol NA No 1.03 (0.89−1.19) 0.648 Yes 1 (ref) Dietary patterns* Vegetarian-based 2.11 (1.69−2.64) < 0.001 1.45 (0.87−2.42) 0.149 Meat-based 1.66 (1.23−2.22) 0.001 0.88 (0.50−1.52) 0.631 Mixed 1 (ref) 1 (ref) Furry/feathery Pets NA No 0.94 (0.78−1.13) 0.511 Yes 1 (ref) New furniture/redecoration NA No 0.89 (0.73−1.08) 0.231 Yes 1 (ref) Stressful work or family events
during the first 1 yearNo 0.80 (0.66−0.99) 0.032 1.02 (0.80−1.30) 0.871 Yes 1 (ref) 1 (ref) Often stay up late No 1.00 (0.85−1.17) 0.989 NA Yes 1 (ref) Before surgery FeNO, ppb 1.00 (1.00−1.01) < 0.001 1.00 (0.98−1.02) 0.954 FnNO, ppb 0.99 (0.99−1.00) 0.001 0.99 (0.99−1.01) 0.196 Hb, g/L 1.00 (1.00−1.01) 0.025 0.99 (0.98−1.01) 0.122 IgE, IU/mL 1.00 (0.99−1.01) 0.538 1.00 (1.00−1.01) 0.032 Medical insurance No 1.26 (1.19−1.33) < 0.001 1.23 (1.07−1.42) 0.003 Yes 1 (ref) 1 (ref) Note. CRS, chronic sinusitis; FeNO, fractional exhaled nitric oxide; FnNO, fractional nasal nitric oxide; HR, hazard ratio; NA, not applicable. *Adjusted for age at operation, sex, BMI, nasal polyposis, smoking, dietary patterns, stressful work or family events during the first 1 year, FeNO, FnNO, Hb, and medical insurance. SES was an independent predictor of postoperative all-cause non-recovery in CRS patients after adjusting for other covariates. During the whole follow-up period of 72 weeks, the risk of non-recovery of patients of low and high SES was significantly higher than that of patients of middle SES.
Patients of low SES had the highest risk of non-recovery, with an HR of 7.69 (95% CI: 6.17–9.71, Ptrend < 0.001), followed by patients of high SES, with HR of 6.19 (95 % CI: 4.78–7.93, Ptrend < 0.001) (Figure 3, Table 2).
-
In sensitivity analysis, we assumed that all the 44 patients lost to follow-up had reached the end point of recovery. Therefore, we performed univariate and multivariate Cox regression analyses, which yielded similar outcomes: HRs for recurrence were 8.77 (95% CI: 7.09–10.87) for the low SES group and 7.19 (95% CI: 5.95–8.70) for the high SES group, compared with the middle SES group (Ptrend < 0.001) (Supplementary Table S3, available in www.besjournal.com).
Table S3. Univariable and multivariable Cox regression model of factors associated with all-cause recurrence (All chronic sinusitis patients lost to follow-up are regarded as recovery)
Characteristics All-cause non-recovery Adjusted HR* (95% CI) P-value Socioeconomic status Low 8.77 (7.09−10.87) < 0.001 High 7.19 (5.95−8.70) < 0.001 Middle 1 (ref) Age at operation, years 0.99 (0.98−1.00) 0.111 Sex Males 0.97 (0.83−1.13) 0.722 Females 1 (ref) Nasal polyposis Without 0.88 (0.74−1.05) 0.026 With 1 (ref) Dietary patterns Vegetarian-based 1.52 (0.98−2.51) 0.747 Meat-based 0.64 (0.54−1.54) 0.058 Mixed 1 (ref) Stressful work or family events during the first 1 year No 0.99 (0.80−1.23) 0.919 Yes 1 (ref) Before surgery FeNO, ppb 1.00 (1.00−1.00) 0.527 FnNO, ppb 1.00 (1.00−1.00) 0.224 Hb, g/L 1.00 (1.00−1.01) 0.113 IgE, IU/mL 1.00 (1.00−1.00) 0.538 Medical insurance No 1.23 (1.06−1.56) 0.023 Yes 1 (ref) Note. CRS, chronic sinusitis; FeNO, fractional exhaled nitric oxide; FnNO, fractional nasal nitric oxide; HR, hazard ratio; NA, not applicable. *Adjusted for age at operation, sex, BMI, nasal polyposis, smoking, dietary patterns, stressful work or family events during the first 1 year, FeNO, FnNO, Hb, and medical insurance. -
This study demonstrated that CRS patients of low and high SES had a greater risk of postoperative all-cause non-recovery (recurrence) after ESS surgery than patients of middle SES. This trend persisted after adjustment for demographic and clinical characteristics. The risk of non-recovery in CRS patients of low SES was nearly eight folds higher than that of patients of middle SES, and the most significant feature was that the risk of non-recovery in patients of high SES was six folds higher than that of patients of middle SES, which contradicted the previous reports of better clinical prognosis in patients of high SES after surgery[11,13,16]. This possibly reflects the challenges associated with SES.
There is currently no standard method for measuring SES, as previous studies were mainly based on census area/community-based SES measurement. The premise of this method is that the national socio-economic data is promptly completed and updated[11-13,16], which makes it unsuitable for SES assessment in China primarily because such data are not available[14]. Moreover, the CRS patients enrolled in this study come from different regions of Northeast China, which introduces great regional and cultural differences. In addition, we included monthly family income as part of the SES measurement indices because the hospital treated CRS patients from all over Northeast China. However, the economic development in these different regions is extremely unbalanced, and even in the same occupation, the income gap is large.
Among CRS patients of low SES, 27% had no medical insurance, and among those of high SES, only 0.9% had no medical insurance. The patients of low SES had relatively low access to medical resources, including routine physical examination[21-24]. In addition, the cost of ESS operation is about ¥20,000 and medical insurance can reimburse ¥10,000, leaving ¥10,000, which most patients can afford. However, considering the backward economy in Liaoning, it is still a big burden for most patients of low SES[22], and therefore, these patients delay their operation. From this trend, it is expected that patients of high SES would pay more attention to their own health because they have physical examination at least once a year (unit welfare) and do not have to worry about the operation cost[22]. However, our data showed that patients of high SES also delayed their operation, which was similar to the trend observed with low SES patients. This suggests that people of high SES faced greater mental pressure from responsibility than those of middle SES in the current Chinese society. Our study also found that patients of high SES had the highest proportion of major stressful events at work or family, as well as increased smoking and drinking, during a period of 1 year before surgery, which explains the mental stress associated with this group[23,25]. Although the difference was not statistically significant from that observed with low and middle SES, patients of high SES experienced the highest mental stress in contemporary China. Chronic psychological stress may be one of the factors that increase CRS severity and lead to uncontrolled disease in CRS patients[26]. FnNO is used as a noninvasive long-term biomarker to monitor sinus disease severity and to determine the prognosis of CRS patients[27]. This also corresponded to the slower postoperative recovery observed in CRS patients of low and high SES.
This study had several limitations. First, all the CRS patients in this cohort were from a single center and the results might not reflect the situation of other nasal endoscopy centers in China. However, single-center surgeons with similar surgical expertise and standardized medical practices do not need to readjust for variables. Second, we did not analyze the impact of each indicator of SES on all-cause non-recovery. Because a single index can only reflect one dimension of SES, and even if it is analyzed one by one, it will only reflect the impact of different dimensions on prognosis. The SES indicators are more comprehensive, scientific, and more suitable for China’s national conditions. Third, our data came from Liaoning Province in Northeast China, which is an economically backward area (population: 8.32 million, area: 12,948 km2). SES in Liaoning is lower than the national average as a whole, and hence, it cannot represent the impact of SES status in other parts of China on CRS after ESS operation. Fourth, this study did not show the interactions between SES, pollutant exposure, and CRS prognosis. However, it has been previously reported that lower SES predicted higher exposure to air pollution and disease severity in patients with CRS[12]. Fifth, European Position Paper on Rhinosinusitis and Nasal Polyps 2020 criteria does not include the traditional classification methods for CRSwNP/CRSsNP, but it classifies CRS into primary and secondary, local and diffuse, as well as eosinophilic and non-eosinophilic CRS. Based on the difference in surgical effect and recurrence rate, CRSwNP can be simply divided into eosinophilic or non-eosinophilic CRSwNP. Eosinophilic CRSwNP easily recurs and is not easily treated[28]; however, our study did not classify CRS into eosinophilic and non-eosinophilic CRS.
In conclusion, CRS patients of low and high SES had greater risk of postoperative recurrence rate than those of middle SES, even after adjusting for nasal polyps, dietary patterns, stressful events, medical insurance methods, and demographic and clinical characteristics in a multivariate Cox proportional risk regression model. SES represents the socioeconomic status of patients and is generally considered a difficult factor to change. Our results showed two-handed intervention policies for CRS patients of different SES status. On the one hand, we urge the government to introduce policies that can reduce the burden of medical expenses on patients and provide more high-quality health care services. On the other hand, the attention of the society should be called to the long-term mental stress experienced by CRS patients of high SES. These strategies may improve the surgical prognosis of CRS patients.
-
The study was conducted in accordance with the Declaration of Helsinki and approved by medical ethics committee of First Affiliated Hospital of China Medical University. (Approval number: SCXK_LN CMU 2019-1302).
-
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
-
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
-
Table S1. Kaplan-Meier analysis of the recovery rate (%) (95 % confidence interval) and Log-rank tests after 24 weeks follow-up
Time (week) Total (n = 1,047) Low (n = 310) Middle (n = 399) High (n = 338) 12 19.1 (18.3−19.9) 3.2 (2.1−4.9) 30.9 (29.2−31.8) 4.7 (3.1−5.9) 24 44.7 (43.7−45.7) 13.5 (12.8−14.2) 90.4 (89.6−91.2) 31.7 (30.7−32.7)
doi: 10.3967/bes2023.135
Socioeconomic Status Impacts the Prognosis of Chronic Rhinosinusitis Treated by Endoscopic Sinus Surgery: An Observational Cohort Study in Northeast China
-
Abstract:
Objective To explore the association between socioeconomic status (SES) and postoperative outcomes in patients with chronic sinusitis (CRS) after functional endoscopic sinus surgery (ESS). Methods We conducted an observational cohort study of 1,047 patients with CRS undergoing ESS. Discharged patients were followed up to 72 weeks for all-cause recurrence events. Baseline SES was established based on occupation, education level, and family income of the patients 1 year before the operation. Kaplan–Meier method was used to calculate the recovery rate after ESS, and Cox proportional hazards regression analysis was used to evaluate the relationship between SES and prognosis. Results Patients of middle SES had lower unadjusted all-cause recurrence than those of low or high SES; 24-week overall recovery rate was 90.4% [95 % confidence interval (CI): 89.6%–91.2%] in patients of middle SES, 13.5% (95 % CI: 12.8%–14.2%) in patients of low SES, and 31.7% (95 % CI: 30.7%–32.7%) in patients of high SES (both log-rank P < 0.001). After adjustment for covariates, hazard ratios (HRs) were 7.69 (95 % CI: 6.17–9.71, Ptrend < 0.001) for all-cause recurrence for low SES versus middle SES, and 6.19 (95 % CI: 4.78–7.93, Ptrend < 0.001) for middle SES versus high SES. Conclusion Low SES and high SES were more associated with the worse prognosis of CRS patients after ESS than middle SES. -
Key words:
- Chronic rhinosinusitis /
- Endoscopic sinus surgery /
- Socioeconomic status
The authors declare no conflict of interest.
注释:1) AUTHORS’ CONTRIBUTIONS: 2) CONFLICTS OF INTEREST: -
Figure 3. Adjusted survival curves for all-cause recurrence by socioeconomic status. Models were adjusted for age at operation, sex, BMI, nasal polyposis, smoking, dietary patterns, stressful family events during the year that precede the operation, FeNO, FnNO, Hb, and medical insurance. FeNO, fractional exhaled nitric oxide; FnNO, fractional nasal nitric oxide; and Hb, hemoglobin.
Table 1. Baseline characteristics and clinical features of patients with severe chronic rhinosinusitis (CRS) (n = 1,047) by socioeconomic status tertiles
Characteristics Total (n = 1,047) Low (n = 310) Middle (n = 399) High (n = 338) P-value Age at operation years 34.2 (27.5−46.1) 36.8 (31.8−50.8) 30.6 (24.3−48.9) 36.6 (30.6−44.1) < 0.001 Sex, n (%) 0.626 Males 600 (57.3) 183 (59.0) 230 (57.6) 187 (55.3) Females 447 (42.7) 127 (41.0) 169 (42.4) 151 (44.7) BMI, kg/m2 22.6 (20.6−27.2) 22.8 (20.7−27.3) 22.5 (20.6−27.6) 22.0 (20.4−26.7) 0.594 Educationa, n (%) < High school 92 (8.8) 83 (27.0) 9 (2.2) 0 (0.0) < 0.001 High school 273 (26.2) 178 (58.0) 92 (23.1) 3 (0.9) ≥ College 676 (65.0) 46 (15.0) 298 (74.7) 332 (99.1) Occupation, n (%) < 0.001 Low 362 (34.6) 169 (54.5) 187 (46.9) 6 (1.8) Medium 313 (29.9) 138 (44.5) 89 (22.3) 86 (25.4) High 372 (35.5) 3 (1.0) 123 (30.8) 246 (72.8) Household income/montha, n (%) < 0.001 < ¥5,000 315 (30.2) 124 (40.0) 151 (37.8) 40 (11.9) ¥5,000–8,000 638 (61.1) 186 (60.0) 243 (60.9) 209 (62.4) > ¥8,000 91 (8.7) 0 (0.0) 5 (1.3) 86 (25.7) Nasal polyposis, n (%) 0.607 Without 283 (27.0) 80 (25.8) 105 (26.3) 98 (29.0) With 764 (73.0) 230 (74.2) 294 (73.7) 240 (71.0) Smoking, n (%) 0.538 No 683 (65.2) 203 (65.5) 267 (66.9) 213 (63.0) Yes 364 (34.8) 107 (34.5) 132 (33.1) 125 (37.0) Alcohol, n (%) 0.302 No 697 (66.6) 212 (68.4) 271 (67.9) 214 (63.3) Yes 350 (33.4) 98 (31.6) 128 (32.1) 124 (36.7) Dietary patternsa, n (%) 0.466 Vegetarian-based 134 (13.3) 36 (13.2) 56 (14.0) 42 (12.4) Meat-based 67 (6.6) 24 (8.8) 25 (6.3) 18 (5.3) Mixed 809 (80.1) 213 (78.0) 318 (79.7) 278 (82.2) Furry/feathery Pets, n (%) 0.356 No 892 (85.2) 271 (87.4) 339 (85.0) 282 (83.4) Yes 155 (14.8) 39 (12.6) 60 (15.0) 56 (16.6) New furniture/redecoration, n (%) 0.593 No 902 (86.2) 267 (86.1) 339 (85.0) 296 (87.6) Yes 145 (86.1) 43 (13.9) 60 (15.0) 42 (12.4) Stressful work or family events during the first 1 yearab, n (%) 0.235 No 711 (68.1) 207 (66.8) 284 (71.2) 220 (65.7) Yes 333 (31.9) 103 (33.2) 115 (28.8) 115 (34.3) Often stay up late, n (%) 0.296 No 788 (75.3) 243 (78.4) 293 (73.4) 252 (74.6) Yes 259 (24.7) 67 (21.6) 106 (26.6) 86 (25.4) Before surgery, n (%) FeNO, ppb 24.0 (16.0−34.0) 22.0 (15.0−36.0) 24.0 (18.0−33.0) 26.0 (19.0−33.0) 0.293 FnNO, ppb 201.0 (151.0−322.0) 220.0 (168.0−335.0) 187.0 (145.0−311.0) 213.0 (169.0−323.0) 0.039 Hb, g/L 146.0 (136.0−161.0) 146.5 (140.0−166.0) 142.0 (121.0−162.0) 146.0 (136.0−157.0) 0.711 IgE, IU/mL 44.4 (30.8−66.0) 42.3 (30.3−77.4) 46.0 (31.1−56.0) 47.6 (34.9−60.8) 0.284 Medical insurance, n (%) < 0.001 No 172 (16.4) 83 (26.8) 86 (21.6) 3 (0.9) Yes 875 (83.6) 227 (73.2) 313 (78.4) 335 (99.1) Note. aTotal numbers were not equal to 1,047 for these characteristics due to missing data. bAmong work, separation/divorce, loss of job, serious health problem, or death of a family member or close relative. Values are n (%) or median (IQR). S2. Multivariable Cox regression model of an interaction between socioeconomic status (SES) and nasal polyposis, medical insurance, and dietary patterns
Interaction β Wald HR (95% CI) P−Value SES × nasal polyps 0.001 1.722 1.001 (0.999−1.003) 0.189 SES × medical insurance −0.056 2.144 0.946 (0.877−1.019) 0.143 SES × dietary patterns 0.092 0.601 1.097 (0.868−1.385) 0.438 Note. HR, hazard ratio; NA, not applicable. Table 2. Univariable and multivariable Cox regression model of factors associated with all-cause recurrence
Characteristics All-cause non-recovery Crude HR (95% CI) P-value Adjusted HR* (95% CI) P-value Socioeconomic status Low 10.42 (8.55−12.66) < 0.001 7.69 (6.17−9.71) < 0.001 High 6.54 (5.49−7.81) < 0.001 6.19 (4.78−7.93) < 0.001 Middle 1 (ref) 1 (ref) Age at operation, years 1.01 (1.00−1.02) 0.013 1.01 (0.99−1.02) 0.128 Sex Males 0.86 (0.72−1.01) 0.27 0.93 (0.79−1.08) 0.313 Females 1 (ref) 1 (ref) BMI, kg/m2 1.02 (1.00−1.03) 0.19 NA Nasal polyposis Without 0.75 (0.65−0.87) < 0.001 0.83 (0.69−1.00) 0.039 With 1 (ref) 1 (ref) Smoking NA No 0.87 (0.76−0.99) 0.039 Yes 1 (ref) Alcohol NA No 1.03 (0.89−1.19) 0.648 Yes 1 (ref) Dietary patterns* Vegetarian-based 2.11 (1.69−2.64) < 0.001 1.45 (0.87−2.42) 0.149 Meat-based 1.66 (1.23−2.22) 0.001 0.88 (0.50−1.52) 0.631 Mixed 1 (ref) 1 (ref) Furry/feathery Pets NA No 0.94 (0.78−1.13) 0.511 Yes 1 (ref) New furniture/redecoration NA No 0.89 (0.73−1.08) 0.231 Yes 1 (ref) Stressful work or family events
during the first 1 yearNo 0.80 (0.66−0.99) 0.032 1.02 (0.80−1.30) 0.871 Yes 1 (ref) 1 (ref) Often stay up late No 1.00 (0.85−1.17) 0.989 NA Yes 1 (ref) Before surgery FeNO, ppb 1.00 (1.00−1.01) < 0.001 1.00 (0.98−1.02) 0.954 FnNO, ppb 0.99 (0.99−1.00) 0.001 0.99 (0.99−1.01) 0.196 Hb, g/L 1.00 (1.00−1.01) 0.025 0.99 (0.98−1.01) 0.122 IgE, IU/mL 1.00 (0.99−1.01) 0.538 1.00 (1.00−1.01) 0.032 Medical insurance No 1.26 (1.19−1.33) < 0.001 1.23 (1.07−1.42) 0.003 Yes 1 (ref) 1 (ref) Note. CRS, chronic sinusitis; FeNO, fractional exhaled nitric oxide; FnNO, fractional nasal nitric oxide; HR, hazard ratio; NA, not applicable. *Adjusted for age at operation, sex, BMI, nasal polyposis, smoking, dietary patterns, stressful work or family events during the first 1 year, FeNO, FnNO, Hb, and medical insurance. S3. Univariable and multivariable Cox regression model of factors associated with all-cause recurrence (All chronic sinusitis patients lost to follow-up are regarded as recovery)
Characteristics All-cause non-recovery Adjusted HR* (95% CI) P-value Socioeconomic status Low 8.77 (7.09−10.87) < 0.001 High 7.19 (5.95−8.70) < 0.001 Middle 1 (ref) Age at operation, years 0.99 (0.98−1.00) 0.111 Sex Males 0.97 (0.83−1.13) 0.722 Females 1 (ref) Nasal polyposis Without 0.88 (0.74−1.05) 0.026 With 1 (ref) Dietary patterns Vegetarian-based 1.52 (0.98−2.51) 0.747 Meat-based 0.64 (0.54−1.54) 0.058 Mixed 1 (ref) Stressful work or family events during the first 1 year No 0.99 (0.80−1.23) 0.919 Yes 1 (ref) Before surgery FeNO, ppb 1.00 (1.00−1.00) 0.527 FnNO, ppb 1.00 (1.00−1.00) 0.224 Hb, g/L 1.00 (1.00−1.01) 0.113 IgE, IU/mL 1.00 (1.00−1.00) 0.538 Medical insurance No 1.23 (1.06−1.56) 0.023 Yes 1 (ref) Note. CRS, chronic sinusitis; FeNO, fractional exhaled nitric oxide; FnNO, fractional nasal nitric oxide; HR, hazard ratio; NA, not applicable. *Adjusted for age at operation, sex, BMI, nasal polyposis, smoking, dietary patterns, stressful work or family events during the first 1 year, FeNO, FnNO, Hb, and medical insurance. S1. Kaplan-Meier analysis of the recovery rate (%) (95 % confidence interval) and Log-rank tests after 24 weeks follow-up
Time (week) Total (n = 1,047) Low (n = 310) Middle (n = 399) High (n = 338) 12 19.1 (18.3−19.9) 3.2 (2.1−4.9) 30.9 (29.2−31.8) 4.7 (3.1−5.9) 24 44.7 (43.7−45.7) 13.5 (12.8−14.2) 90.4 (89.6−91.2) 31.7 (30.7−32.7) -
[1] Sahlstrand-Johnson P, Ohlsson B, von Buchwald C, et al. A multi-centre study on quality of life and absenteeism in patients with CRS referred for endoscopic surgery. Rhinology, 2011; 49, 420−8. doi: 10.4193/Rhino11.101 [2] Orlandi RR, Kingdom TT, Smith TL, et al. International consensus statement on allergy and rhinology: rhinosinusitis 2021. Int Forum Allergy Rhinol, 2021; 11, 213−739. doi: 10.1002/alr.22741 [3] Shi JB, Fu QL, Zhang H, et al. Epidemiology of chronic rhinosinusitis: results from a cross-sectional survey in seven Chinese cities. Allergy, 2015; 70, 533−9. doi: 10.1111/all.12577 [4] Croy I, Nordin S, Hummel T. Olfactory disorders and quality of life–an updated review. Chem Senses, 2014; 39, 185−94. doi: 10.1093/chemse/bjt072 [5] Ahmed OG, Rowan NR. Olfactory dysfunction and chronic rhinosinusitis. Immunol Allergy Clin North Am, 2020; 40, 223−32. doi: 10.1016/j.iac.2019.12.013 [6] Wright ED, Agrawal S. Impact of perioperative systemic steroids on surgical outcomes in patients with chronic rhinosinusitis with polyposis: evaluation with the novel perioperative sinus endoscopy (POSE) scoring system. Laryngoscope, 2007; 117, 1−28. [7] Al-Qudah M. Refractory chronic rhinosinusitis: a new rhinological disease. Glob J Oto, 2017; 4, 555637. [8] Jiang RS, Lu FJ, Liang KL, et al. Olfactory function in patients with chronic rhinosinusitis before and after functional endoscopic sinus surgery. Am J Rhinol, 2008; 22, 445−8. doi: 10.2500/ajr.2008.22.3195 [9] Soler ZM, Mace J, Smith TL. Symptom-based presentation of chronic rhinosinusitis and symptom-specific outcomes after endoscopic sinus surgery. Am J Rhinol, 2008; 22, 297−301. doi: 10.2500/ajr.2008.22.3172 [10] Duerson W, Lafer M, Ahmed O, et al. Health care disparities in patients undergoing endoscopic sinus surgery for chronic rhinosinusitis: differences in disease presentation and access to care. Ann Otol Rhinol Laryngol, 2019; 128, 608−13. doi: 10.1177/0003489419834947 [11] Shen SA, Jafari A, Qualliotine JR, et al. Socioeconomic and demographic determinants of postoperative outcome after endoscopic sinus surgery. Laryngoscope, 2020; 130, 297−302. doi: 10.1002/lary.28036 [12] Velasquez N, Gardiner L, Cheng TZ, et al. Relationship between socioeconomic status, exposure to airborne pollutants, and chronic rhinosinusitis disease severity. Int Forum Allergy Rhinol, 2022; 12, 172−80. doi: 10.1002/alr.22884 [13] Beswick DM, Mace JC, Rudmik L, et al. Socioeconomic factors impact quality of life outcomes and olfactory measures in chronic rhinosinusitis. Int Forum Allergy Rhinol, 2019; 9, 231−9. [14] Xiang L, Su ZH, Liu YW, et al. Effect of family socioeconomic status on the prognosis of complex congenital heart disease in children: an observational cohort study from China. Lancet Child Adolesc Health, 2018; 2, 430−9. doi: 10.1016/S2352-4642(18)30100-7 [15] Subspecialty Group of Rhinology, Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery, Subspecialty Group of Rhinology, Society of Otorhinolaryngology Head and Neck Surgery, Chinese Medical Association. Chinese guidelines for diagnosis and treatment of chronic rhinosinusitis (2018). Chin J Otorhinolaryngol Head Neck Surg, 2019; 54, 81−100. (In Chinese [16] Beswick DM, Mace JC, Soler ZM, et al. Socioeconomic status impacts postoperative productivity loss and health utility changes in refractory chronic rhinosinusitis. Int Forum Allergy Rhinol, 2019; 9, 1000−9. doi: 10.1002/alr.22374 [17] Odat H, Al-Qudah M. Food elimination in the management of refractory chronic rhinosinusitis: a pilot study. Ear Nose Throat J, 2021; 100, NP424−8. doi: 10.1177/0145561320924150 [18] Alkholaiwi FM, Almutairi RR, Alrajhi DM, et al. Occupational and environmental exposures, the association with chronic sinusitis. Saudi Med J, 2022; 43, 125−31. doi: 10.15537/smj.2022.43.2.20210849 [19] Lind H, Joergensen G, Lange B, et al. Efficacy of ESS in chronic rhinosinusitis with and without nasal polyposis: a Danish cohort study. Eur Arch Otorhinolaryngol, 2016; 273, 911−9. doi: 10.1007/s00405-015-3667-9 [20] Kambara R, Minami T, Akazawa H, et al. Lower airway inflammation in eosinophilic chronic rhinosinusitis as determined by exhaled nitric oxide. Int Arch Allergy Immunol, 2017; 173, 225−32. doi: 10.1159/000479387 [21] Ma CJ, Zhang YM, Li Y, et al. Healthcare, insurance, and medical expenditure of the floating population in Beijing, China. Front Public Health, 2020; 8, 375. doi: 10.3389/fpubh.2020.00375 [22] Wang Q, Zhang DL, Hou ZY. Insurance coverage and socioeconomic differences in patient choice between private and public health care providers in China. Soc Sci Med, 2016; 170, 124−32. doi: 10.1016/j.socscimed.2016.10.016 [23] Yang TZ, Rockett IRH, Lv QH, et al. Stress status and related characteristics among urban residents: a six-province capital cities study in China. PLoS One, 2012; 7, e30521. doi: 10.1371/journal.pone.0030521 [24] Xu RH, Wang LL, Zhou LM, et al. Urban-rural differences in financial toxicity and its effect on cancer survivors’ health-related quality of life and emotional status: a latent class analysis. Support Care Cancer, 2022; 30, 4219−29. doi: 10.1007/s00520-021-06762-0 [25] Hao W, Su ZH, Liu BL, et al. Drinking and drinking patterns and health status in the general population of five areas of China. Alcohol Alcohol, 2004; 39, 43−52. doi: 10.1093/alcalc/agh018 [26] Tomljenovic D, Pinter D, Kalogjera L. Perceived stress and severity of chronic rhinosinusitis in allergic and nonallergic patients. Allergy Asthma Proc, 2014; 35, 398−403. doi: 10.2500/aap.2014.35.3774 [27] Lee DJ, Yip J, Lee JM. Nasal nitric oxide as a long-term monitoring and prognostic biomarker of mucosal health in chronic rhinosinusitis. Int Forum Allergy Rhinol, 2020; 10, 971−7. doi: 10.1002/alr.22581 [28] Hellings PW, Fokkens WJ, Orlandi R, et al. The EUFOREA pocket guide for chronic rhinosinusitis. Rhinology, 2023; 61, 85−9. -
 22431+Supplementary Materials.pdf
22431+Supplementary Materials.pdf

-




 下载:
下载:





 Quick Links
Quick Links