-
Since the 1950s, several reports of locally acquired rabies in Xinjiang Province, China, have been published. The Yili Friendship Hospital received a suspected human rabies case on April 30, 2016. The patient presented with fever and back pain, and he reported having been bitten by a fox on March 6 in Nilka County. The patient had not been previously vaccinated against rabies. During hospitalization, the patient demonstrated rabies symptoms, including fear of water and wind, irritability, excitement, and paroxysmal pharyngeal muscle spasms, among others. The patient died on May 7, 2016, and his blood RT-PCR test results came out positive on July 11, 2016.
The patient was a Kazakh herdsman, aged 29 years, and married. While out grazing sheep near Bubulake (43°42'16" W, 83°18'7" E; altitude, 1, 700 m) at around 15:00-16:00 on March 6, 2016, he saw a fox attacking a lamb. He shouted at the fox in an attempt to frighten it away, but he was attacked by the animal instead. The patient struck the fox on the head with a stone to kill it, but his hands (muscle of the hypothenar on the right hand and thumbnail on the left hand) were bitten during the attack. The wounds he sustained were not very deep, and the patient experienced minimal bleeding. At around 16:00-17:00 of the same day, the herdsman returned to his home to clean the wound with soap and disinfect it with alcohol. He and his brother-in-law then skinned the fox and buried the body. About a week later, the herdsman's wounds appeared to heal, but he experienced numbness and itching. The patient was not vaccinated against rabies and did not receive an injection of any specific anti-rabies immunoglobulin. On April 25, the patient began to experience back pain, which increased in severity from April 26 onward. On April 28, he visited the village clinic because of abdominal pain and fever. During his hospitalization, he developed a fear of water, sound sensitivity, and irritability. On April 29, he was transferred to the Kunas County Hospital, where he vomited blood and his temperature was recorded as 38.5 ℃. On April 30, the patient was transferred to a state hospital because of difficulty breathing, and he received a tracheotomy the next day. The patient died at 19:00 on May 7, 2016. On the same day, we found two fox heads that could be used for virus detection, one from the fox that had bitten the patient and another from a natural death nearby.
The two fox heads were sent to the laboratory for testing. One of the heads was recovered as a skull; this sample was considered to belong to a fox that had died of natural causes. The head of the fox presumed to have bitten the patient was crushed at the top of the skull and filled with maggots. After cleansing and treating the sample, no brain tissues were obtained, likely because these had been consumed by the maggots. As such, we were unable to obtain samples from the fox heads for testing. We were also unable to obtain any of the patient's brain tissue, cerebrospinal fluid, and neck skin because of the family's religious beliefs. Thirteen samples obtained from the patient, including saliva and arterial blood, were tested by RT-PCR; the details of this process are described below. All tests were done by the Institute of Viral Diseases of the China Center for Disease Control and Prevention.
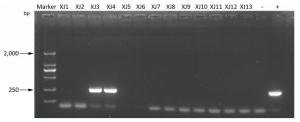
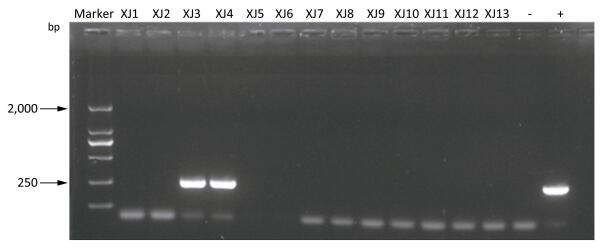
We used Trizol LS to extract total RNA from the specimen and obtained cDNA by RT-PCR. The complete sequence of the N gene was amplified with two pairs of primers: (Table 1) N127 and N8m primers were used for the first half segment with the locations of the primer sequences with respect to the full genome sequence of Pasteur virus (PV) strain (M13215); N577 and N829 primers for the latter half. During nested PCR amplification, the final amplification product was 256 bp long (Figure 1). After completion of the reaction, agarose gel electrophoresis was performed on the secondary PCR products. Two blood samples acquired from the patient before dying tested positive for specific nucleic acids found in the rabies virus; thus, the patient was confirmed as a rabies case by laboratory diagnosis. Because of the effects of long-distance transportation and suboptimal cold storage, the virus was heavily decayed and fragments of the N gene could not be obtained. As such, we were unable to build an evolutionary tree to understand the source of the virus.
Table 1. Primers of the PCR Reaction
Primers Sequence (5'-3') Location N127 ATGTAACACCTCTACAATGG 55-74 N8 m CAGTCTCYTCNGCCATCT 1, 570-1, 587 N577 AAGATGTGYGCYAAYTGGAG 644-663 N829 GCCCTGGTTCGAACATTCT 881-899 Note. The location of primers was based on the Pasteur virus strain M13215. To determine other cases of rabies in the area, we searched the records of four local hospitals (i.e., Nilka County Hospital, Kunas County Hospital, Xinhua Hospital, and Yili Friendship Hospital) from 2005 to the present. We focused on diagnoses of rabies and 15 other encephalitis-like diseases according to the hospital ICD-10 code and then filtered death cases within 10 days. We found a total of 642 encephalitis-like cases, 12 of which died. We were unable to gain access to the medical records of 2 of these 12 cases because they involved lawsuits; the remaining 9 cases were confirmed cases of other diseases without animal exposure and the last case was suspected of rabies. The suspected rabies case showed an obvious history of dog exposure without typical rabies manifestations and pathogen testing.
Rabies is a viral disease that causes acute inflammation of the brain in humans and other mammals; it is 100% fatal[1]. Rabies can occur at any time of the year in China but occurs most often in the summer and autumn (29.48% and 32.88%, respectively, of all cases recorded)[2]. Most rabies victims (61.60%) in the area are farmers. Students (18.37%) and children living in marginal areas (9.1%) are also at high risk of rabies infection[2]. These infection rates are reasonable because farmers and students tend to be widely exposed to dogs and wild animals. Contracting rabies during dog rabies epizootics is highly likely.
In China, three major dog-maintained rabies epidemics have been reported within the period 1950-2006[3]; however, disease rates have declined substantially over the years. In China, 95% of all rabies cases in humans are linked to dog bites[4-5]. Of the human deaths from rabies reported, 99% were caused by dog bites[6-7]. Wild animals, such as stoats, bats, raccoons, wolves, deer, and others, may be affected by rabies in the northeastern and northwestern regions of China, and such infection has been confirmed by multiple laboratory-based testing namely viral isolation, antibody screening, antigen detection, and nucleic acid detection[8]. Incidental rabies epizootics in sheep associated with foxes have been reported in Inner Mongolia with no human casualties thus far[3].
The Xinjiang Uyghur Autonomous Region, the largest province of China, is located at the northwestern portion of the country. Xinjiang, in fact, is relatively far from provinces with a high incidence of rabies, such as Guangxi, Hunan, and Guizhou. Nine other provinces are located between Xinjiang and provinces with a high incidence of rabies and limited or no incidence of rabies has been recorded in these nine provinces. In Xinjiang, a rabies incident caused by a wild wolf attack was reported in 1996. At the time, however, no laboratory test for pathogenic microorganisms was available[3]. Rabies has been controlled in developed countries, as a result, wild animal as fox, blood feeding bat, skunk and raccoon have become the important infection source[9]. According to the National Infectious Diseases Surveillance and Reporting System, no records of local human rabies infection have been reported in Xinjiang since the 1950s, likely because of the low human population density and low dog count in the area; long winters also decrease the locals' involvement with dogs. Good treatment of dogs with rabies and good management are other important reasons contributing to this fact. However, carnivores, such as foxes, raccoon dogs, and wolves, infected with rabies could infect humans or livestock.
Besides wolves, red foxes may be found in the farming areas of Xinjiang. These foxes live in forests, grass fields, semi-deserts, hills, and holes in trees and the ground; they hunt for food in the evening and return to their homes after daybreak. Food for these animals includes mice, wild rabbits, and wild fruits. Red foxes are very careful; they do not usually hunt for food in the day time, they keep their distance from areas inhabited by humans, and generally avoid involvement with dogs bred by humans. According to brother in law of patient, the sheep that attacked by the fox on 3rd of March had no sheep skin left. The attack wasn't look like big carnivores' such as wolf's, so they assumed that it was fox. Why then would a timid and careful animal, such as a fox, be involved with humans? Recent changes in policy have remarkably improved the vegetation and animal ecosystems. An increasing number of herbivorous animals, such as prairie rats, large ground squirrels, and wild rabbits, has been observed, and these animals serve as food sources for foxes, coyotes, and raccoon dogs. In turn, the number of these wild animals has also increased. Because of human activity, especially the building of industrial companies, farming activities have moved deeper within the hills, causing increasing involvement between farmers, livestock, and wild animals. We found a coking plant (43°42'16" W, 83°18'7" E; altitude, 1, 600 m) about 5 km from the field in which our patient was bitten. Human industrial activities has caused the shift of farming activities to the deep hills, causing overlaps between areas where wild animals live and farming occurs.
Kazakhs in Xinjiang often keep dogs. During our investigation, we noticed a large number of stray dogs in the areas of Kalatuobie, in Nilka, and Bubulake. These animals may carry with them the rabies virus, which they obtained from fights with wild animals, such as foxes. Unfortunately, these dogs may also spread the rabies virus among humans through contact. In our investigation, the patient's wound was not deep; a simple treatment was applied, but no vaccination was performed. Our inquiry of the patient's family and other famers living around the area revealed that they had no basic knowledge of wild animals causing rabies or vaccination against rabies. No curative treatment is available for rabies after the onset of symptoms, and the disease is always lethal. As early biological diagnosis of infection (i.e., prior to the onset of symptoms) is not possible in humans, preventing the disease is crucial, as is administration of prophylaxis post-exposure; this measure is relatively effective, except in rare cases. According to World Health Organization recommendations, the patient's type of contact could be considered grade Ⅲ; thus, he should have been vaccinated and injected with specific anti-rabies immunoglobulins. Unfortunately, the local health department does not provide RIG.
The related departments for epidemic prevention should provide education for rabies prevention. Hunting of foxes and wolves is not recommended because of the costs associated with this endeavor and the risk of upsetting the balance of the ecosystem. Medical institutions should pay increased attention to encephalitis patients, especially those from farming areas known for rabies incidents, to enable immediate diagnosis of the disease. Centers for disease control and prevention at county-level should implement vaccination campaigns and ensure the vaccine supply due to lack type Ⅱ vaccines (There are two types of vaccines in China, type Ⅰ is the free vaccine that provided by the government, type Ⅱ is paid). A joint defense system should be established with neighboring countries. Joint monitoring, testing, and vaccination activities between China and Kazakhstan, China and Mongolia, and China and Russia, for example, should be promoted to build an immune isolation belt and prevent rabies infection through foxes and wolves[10].
Special thanks to TAO Xiao Yan for assistance with experiments, TALIPU Jiangatai and YIMAMU Tuohetiyaer from Yili state CDC for their field coordination; Dr. Ronald Moolenaar from the United States Centers for Disease Control and Prevention for assistance in writing article.
doi: 10.3967/bes2017.110
An Investigation of the First Case of Human Rabies Caused by a Fox in China in May 2016
-
Abstract: This study assesses the causes and prevention measures of rabies through epidemiological investigation and analysis. A field epidemiological survey was conducted to investigate a case of rabies by fox bite. The onset of symptoms began 50 days after the bite. The patient did not receive standard treatment, rabies vaccination, or rabies immunoglobulin injection. The fox was killed on the spot. Saliva and pre-death blood samples were collected at different periods, and only blood RT-PCR tests yielded positive results. Wild fox bite is a major risk factor of rabies infection in Xinjiang Province, China.
-
Table 1. Primers of the PCR Reaction
Primers Sequence (5'-3') Location N127 ATGTAACACCTCTACAATGG 55-74 N8 m CAGTCTCYTCNGCCATCT 1, 570-1, 587 N577 AAGATGTGYGCYAAYTGGAG 644-663 N829 GCCCTGGTTCGAACATTCT 881-899 Note. The location of primers was based on the Pasteur virus strain M13215. -
[1] Carrieri ML, Peixoto ZM, Paciencia ML, et al. Laboratory diagnosis of equine rabies and its implications for human postexposure prophylaxis. J Virol Methods, 2006; 138, 1-9. doi: 10.1016/j.jviromet.2006.07.005 [2] Song M, Tang Q, Feng ZJ, et al. Analysis of the epidemiological characteristics of rabies prevalent in China from 1996 to 2006. Chinese Journal of Zoonoses, 2008; 24, 584-6. (In Chinese) http://en.cnki.com.cn/Article_en/CJFDTOTAL-ZRSZ200806026.htm [3] Wang LH, Tang Q, Liang GD, et al. Rabies and rabies virus in wildlife in mainland China, 1990-2013. Int J Infect Dis, 2014; 25, 122-9. doi: 10.1016/j.ijid.2014.04.016 [4] Hu R, Tang Q, Tang J, et al. Rabies in China:an update. Vector Borne Zoonotic Dis, 2009; 9, 1-12. doi: 10.1089/vbz.2008.0046 [5] Tang XC, Luo M, Zhang SY, et al. Pivotal role of dogs in rabies transmission, China. Emerging infectious diseases, 2005; 11, 1970-2. doi: 10.3201/eid1112.050271 [6] Song M, Tang Q, Wang DM, et al. Epidemiological investigations of human rabies in China. BMC Infect Dis, 2009; 9, 210. doi: 10.1186/1471-2334-9-210 [7] WHO Expert Consultation on rabies. World Health Organ Tech Rep Ser, 2005; 931, 1-88, back cover. [8] Tao XY, Li Hao, Jiao WT, et al. Grouping and evolution characteristics of rabies virus in China. Disease Surveillance, 2013; 5, 340-3. [9] BOGEL K, MOEGLE H, STECK F, et al. Assessment of fox control in areas of wildlife rabies. Bulletin of the World Health Organization, 1981; 59, 269-79. https://www.pubmedcentral.nih.gov/pmc/articles/PMC2396044/ [10] Chen JZ, Gu WX, Zhong Q, et al. Identification and sequence analysis of the rabies virus N gene from sheep in Xinjiang Uygur Autonomous Region, China. Chinese Journal of Zoonoses, 2014; 30, 494-8. (In Chinese) http://en.cnki.com.cn/Article_en/CJFDTotal-ZRSZ201405013.htm -




 下载:
下载:



 Quick Links
Quick Links