-
Rabies is a vaccine-preventable disease with a global goal of zero human deaths by 2030. However, this currently results in an annual loss of millions of disability-adjusted life years, particularly in developing countries[1]. China experienced a peak in human rabies cases, with over 3,300 reported incidents in 2007. However, the subsequent implementation of robust measures, including enhanced animal management and Post-Exposure Prophylaxis (PEP), has led to a more than 90% reduction in rabies cases from 2007 to 2023[2]. The epidemiological trend of human rabies in Beijing, the capital of China, has similarly undergone three stages since 1973. This study aimed to provide a comprehensive description of the observed epidemiological characteristics in Beijing from 1973 to 2023 and to assess the progress made toward elimination targets.
The inclusion of human rabies as a notifiable infectious disease in China dates back to the 1950s when the Chinese Notifiable Disease Reporting System was established in 1955. Nevertheless, owing to the lack of records from 1955 to 1963 and zero human rabies cases reported from 1964 to 1972, this study focused on human rabies cases in Beijing from 1973 to 2023. Medical institutions report all suspected human rabies cases when patients seek medical consultation. Subsequently, the Centers for Disease Control (CDC) conduct epidemiological investigations and collect related information, including demographic information, dates of onset and death, clinical symptoms, and likely rabid animals. Before 2004, cases of communicable diseases were reported via phone or mail without the use of standardized epidemiological questionnaires, resulting in inconsistent and non-uniform data extracted from the annual summary reports. Since January 1, 2004, the establishment of the National Disease Reporting Information System (NDRIS) has mandated the timely reporting of all legally notifiable infectious diseases, including human rabies. This has enabled timely online monitoring of human rabies.
Since 2013, human rabies cases have been diagnosed using appropriate clinical specimens such as saliva, cerebrospinal fluid (CSF), and urine, which are collected and transferred to the Beijing CDC for laboratory testing following standardized procedures. Human rabies was classified into clinically diagnosed and laboratory-confirmed cases, according to the Technical Management Regulations of Human Rabies in Beijing. A clinically diagnosed case was defined as a reliable history of contact with a suspected, probable, or confirmed rabid animal plus an acute neurological syndrome (i.e., encephalitis) dominated by forms of hyperactivity (furious rabies) or paralytic syndromes (paralytic rabies) progressing toward coma and death, typically within 7–10 days of the first signs. A laboratory-confirmed case was defined as a clinically diagnosed case confirmed in the laboratory and detected mainly using real-time fluorescent reverse transcriptase-polymerase chain reaction (RT-PCR).
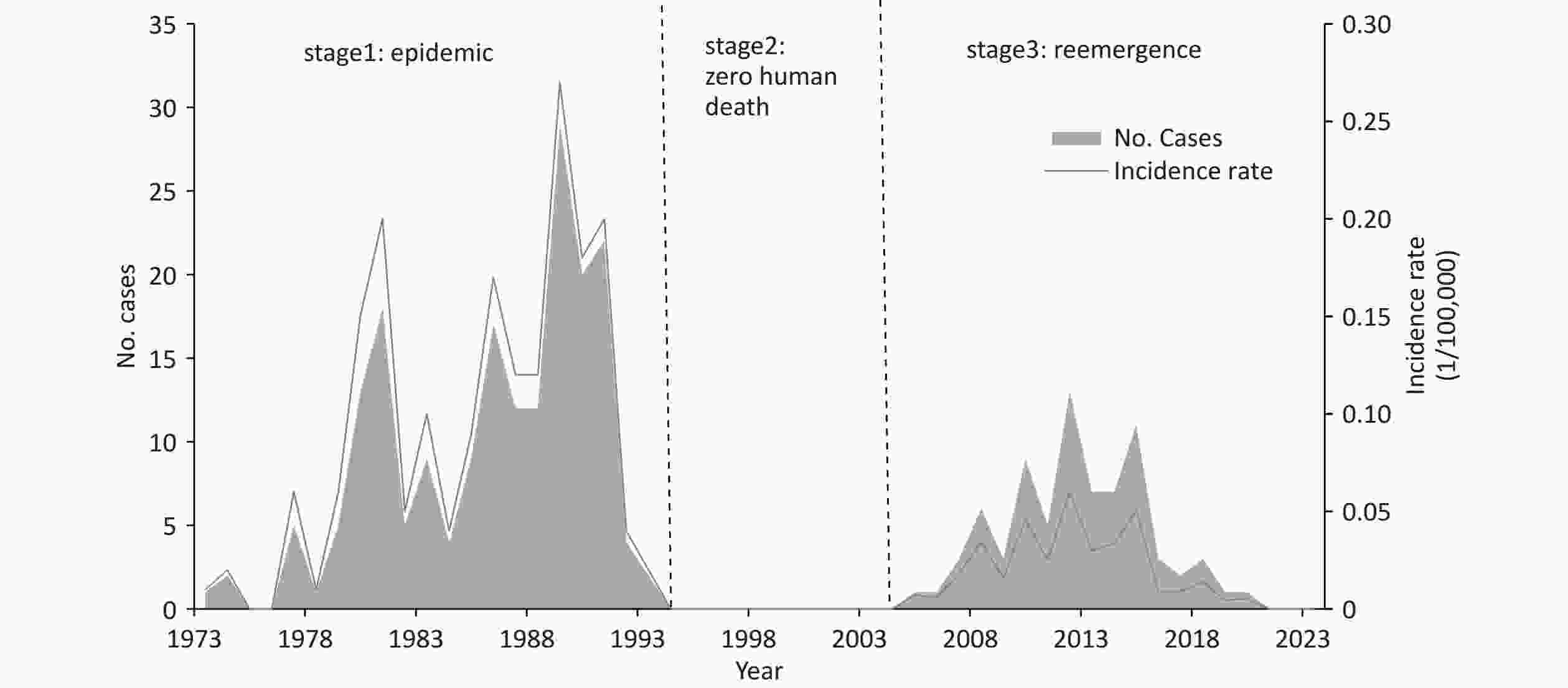
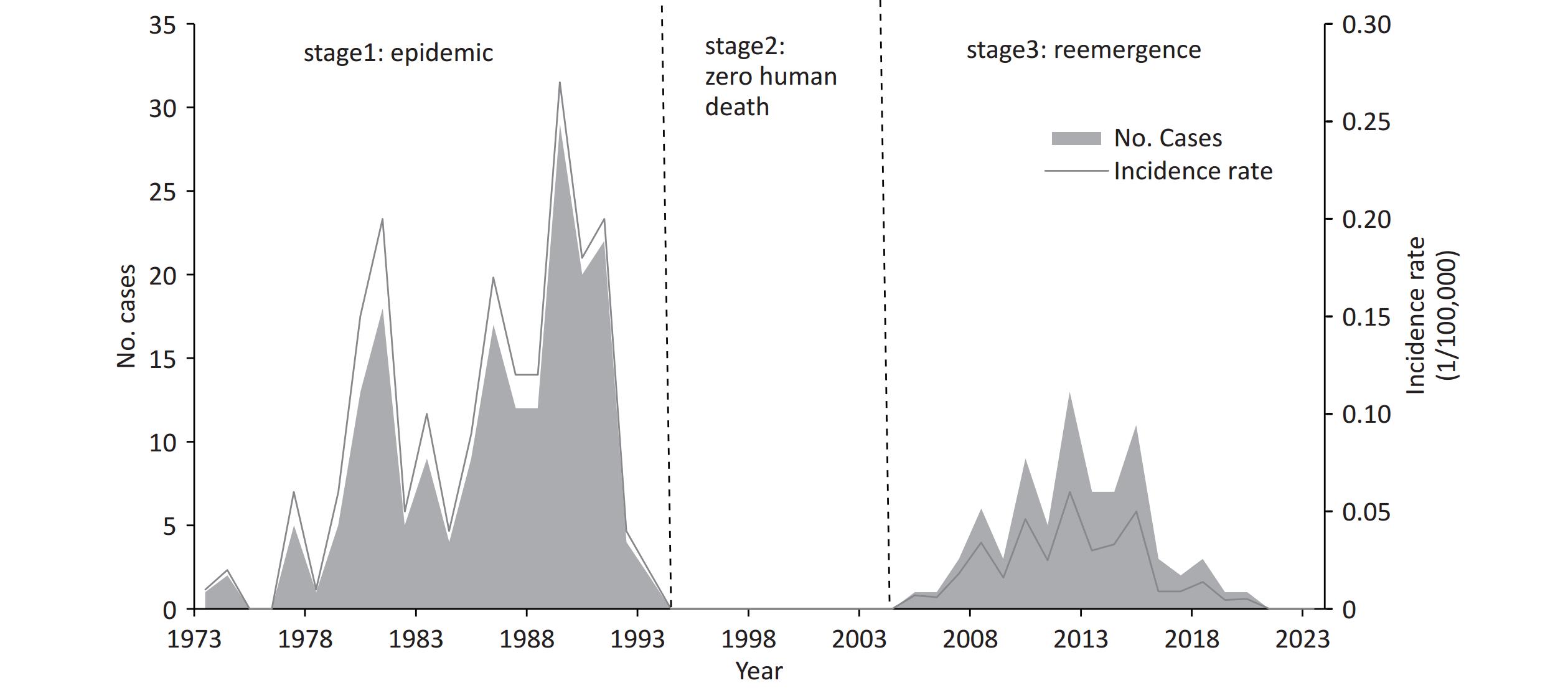
The epidemic trend of human rabies in Beijing can be delineated into three distinct phases, namely, epidemic, zero human death and re-emergence, respectively, from 1973 to 2023 (Figure 1). From 1973 to 1993, 190 human rabies cases were reported, and the annual incidence showed a gradual increase over time, reaching a peak in 1989, with 29 cases and an incidence rate of 0.27 per 100,000 people, which was the epidemic phase. Related individuals may find it difficult to access timely, affordable and adequate PEP[3], and there is a lack of implemented canine management policies in Beijing.
Between 1994 and 2004, Beijing entered the second phase of rabies control efforts, resulting in 11 consecutive years without any reported human deaths. This achievement was attributed to the strict enforcement of the “Regulation on Severely Restricted Dog Ownership” in 1994, which enforced stringent restrictions and comprehensive control measures to effectively manage and regulate dog ownership, along with adequate PEP[4].
The third phase, from 2005 to 2023, saw the re-emergence of human rabies, with 76 reported cases. The highest incidence was observed in 2012, with 13 cases and an incidence rate of 0.01/100,000. This resurgence was primarily attributed to changes in dog ownership regulations, such as the implementation of the “Regulation of Dog Management” in Beijing in 2004. This regulation transitioned from dog restrictions to registration and annual inspections, resulting in an increase in the canine population. However, since 2005, Beijing has established clinics in numerous hospitals and strengthened training and supervision to ensure adequate and convenient PEP; in recent years, nearly 300,000 individuals in Beijing receive rabies vaccine annually. Meanwhile, effective public awareness campaigns promoting responsible dog ownership have been implemented. Sufficient PEP and responsible dog ownership have contributed to maintaining a low incidence of human rabies, and there has been a noticeable decline since 2016, with zero human cases reported in the past three years (2021–2023).
Analyze the geographical distribution; since 1973, human rabies cases have been predominantly concentrated in southeastern Beijing and have spread to the northwest. During the first epidemic phase from 1973 to 1993, geographical distribution data were available for 147 cases. Excluding Mentougou in the western area and Dongcheng and Shijingshan, which are located centrally within the city, most cases (125 cases, 85.03%) were reported in the southern and eastern regions of Beijing. During the re-emergence phase from 2005 to 2023, an initial case of human rabies was reported in Fengtai, a southern district, which subsequently spread outward from this focal point. By 2023, only three districts of Huairou in the northern area, Dongcheng and Xicheng, located centrally within the city, remained with zero reported cases; most incidents (48 cases; 63.16%) occurred in southern and eastern regions, which aligns with the geographical distribution of the first epidemic phase. This spatial distribution partly reflects the endemic movement of dog rabies, which may be associated with the landscape characteristics of the region. The southeastern part of Beijing is primarily characterized by flat plains, whereas the northwestern areas are mainly mountainous.
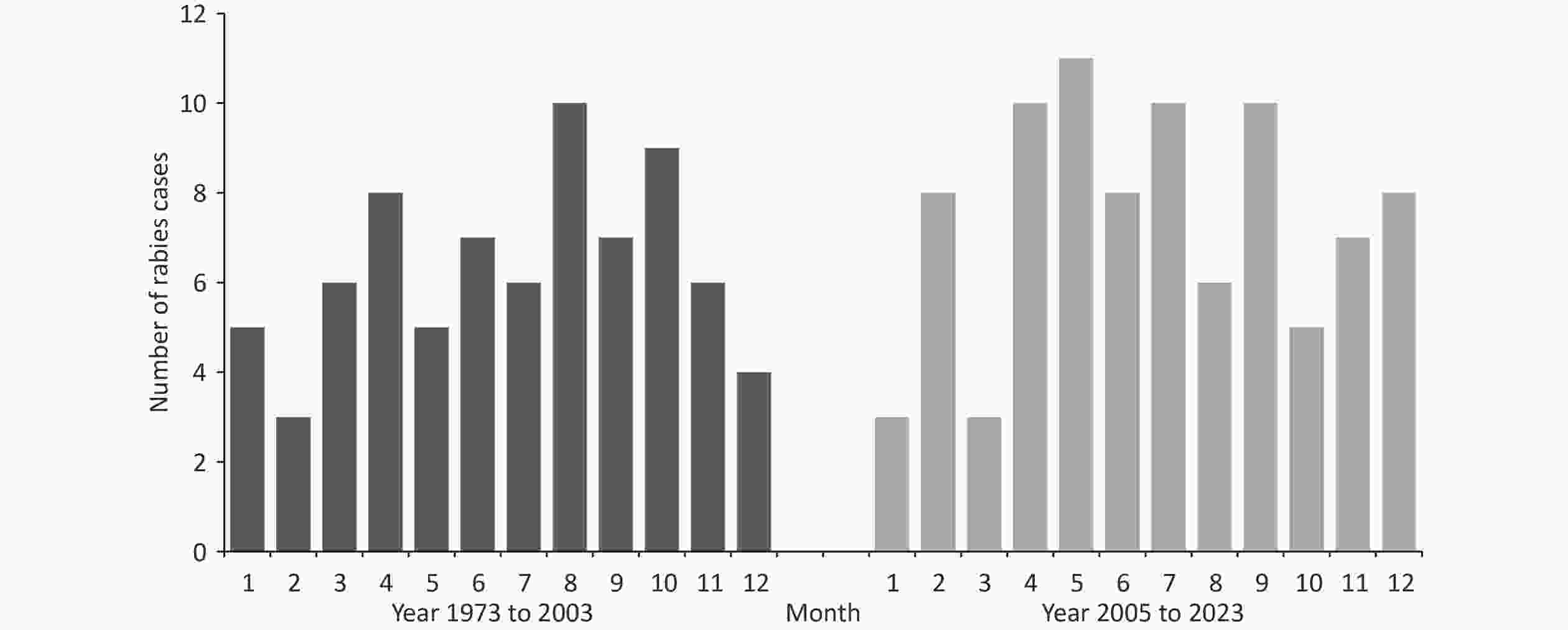
In contrast to the nationwide pattern with a peak in August[3], there was no clear seasonal pattern observed in Beijing during the initial phase of the epidemic and its third re-emergence (P = 0.50) (Figure 2). In the first phase, 89 cases were analyzed for seasonal distribution. The highest morbidity rate was observed in August, accounting for 11.24% (10 cases), whereas February had the lowest rate at 3.37% (3 cases). During the re-emergence phase, May exhibited the highest morbidity rate of 14.47% (11 cases), while January and March had the lowest rates of 3.95% (3 cases).
Population distribution analysis revealed that the male-to-female ratio of the 89 recorded cases from 1973 to 1993 was 2.42:1, whereas, for the 76 cases from 1993 to 2023, it was at 4.43:1. There was no significant difference between the two phases. Notably, the age distribution underwent significant changes, with two distinct peaks observed before 1993 in the total 127 cases with age records: individuals ≤ 14 years age group (46 cases, 36.22%) and adults in the age group of 30–39 (21 cases, 16.54%). However, there was only one single peak after 2005, namely the age group of 50–59 (29 cases, 38.16%); ages ≤ 14 years accounted for only two cases (2.63%). The proportion of students and preschool children declined from an initial stage value of 40.60% (41 cases ) before 1993 to a third-stage value of only 5.28% (2 cases, P < 0.01) from 2005 to 2023. This may be related to the increased rate of vaccination after dog bites among children, which has increased[5], indicating an increased awareness and knowledge of rabies among the general public. However, since 1973, farmers have always represented the largest proportion, accounting for 48.51% (49 cases) before 1993 and 44.74% (34 cases) after 2005. This may be attributed to a lack of awareness and limited accessibility to PEP owing to economic constraints or geographical distance for farmers[6]. Therefore, targeted efforts should be made to raise awareness and improve the accessibility of PEP in this specific population.
There was a significant difference in the exposure sites after 2005 compared to those before 1993 (P < 0.01). In total, 107 cases with reliable records of exposure sites were identified before 1993; hand exposure accounted for 43.93% (47 cases), head and face accounted for 21.50% (23 cases), upper limb as well as lower limb including feet, and multiple positions each accounted for 10.28% (11 cases), and other exposure sites accounted for 3.74% (4 cases). After 2005, out of 56 human rabies cases for which exposure details were collected, 55 cases were animal-mediated. Most exposure sites were located on the hands (60.00%, 33 cases), followed by the lower limbs and feet (23.63%, 13 cases), head and face (9.09%, 5 cases), and upper limbs (7.27%, 4 cases), none of which reported multiple exposures (Table 1).
Table 1. Differences of human rabies characteristics between 1973 to 1989 and 2005 to 2023 in Beijing
Characteristics Number of cases (%) Statistics value P value 1973–1989 2005–2023 Sex 2.60 0.11 Male 63 (70.79) 62 (81.58) Female 26 (29.21) 14 (18.42) Age group, years 66.57 < 0.01 ≤ 14 46 (36.22) 2 (2.63) 15– 24 (18.90) 2 (2.63) 30– 21 (16.54) 10 (13.16) 40– 15 (11.81) 18 (23.68) 50– 8 (6.30) 29 (38.16) ≥ 60 13 (10.24) 15 (19.74) Occupation 57.03 < 0.01 Preschool 23 (22.78) 1 (1.32) Student 18 (17.82) 1 (1.32) Workers 7 (6.93) 16 (21.05) Official 4 (3.96) 7 (9.21) Farmer 49 (48.51) 34 (44.74) Retired and others 0 (0) 17 (22.37) Exposure sites 17.57 < 0.01 Hand 47 (43.93) 33 (60.00) Head and face 23 (21.50) 5 (9.09) Upper limb 11 (10.28) 4 (7.27) Lower limb, feet 11 (10.28) 13 (23.64) Multiple and Others 15 (14.02) 0 (0) Of the 118 cases with a reliable history of exposure before 1993, dog-mediated rabies constituted the majority (96.61%, 114 cases), whereas cat-mediated rabies represented only a small proportion (3.39%, 4 cases). After 2005, all 55 animal-mediated human rabies cases were attributed to dog bites; 63.63% (35 cases) were bitten by wild dogs, and the remaining 36.36% (20 cases) were bitten by domestic dogs. A substantial proportion (85.00%) of the domestic dogs either lacked vaccination or had an unknown vaccination status. This reminds us that the management and vaccination of dogs need to be strengthened in Beijing. Dog-mediated rabies can be significantly reduced or even eliminated through sustained mass dog vaccination programs, based on the experiences of nations that have successfully eliminated dog-mediated human rabies[1].
Additionally, a unique route of rabies exposure was reported in Beijing in August 2017; human rabies was transmitted through kidney transplantation. Before this case, in March 2017, one liver transplantation rabies case from the same donor had been documented in Shanxi province, China. Both recipients were admitted to the same medical facility and underwent transplantation on the same day in Beijing in October 2016. Although transmission of the rabies virus through transplantation exposure is rare, recent years have witnessed a significant increase in both donations and clinical transplants, highlighting the need for enhanced donor assessment[7].
Currently, a significant challenge encountered in Beijing is the absence of an effective dog monitoring system, resulting in inadequate data on the canine population and vaccination coverage. Regional elimination is an essential component of national rabies programs[8]. Beijing is on the way to the phase of zero human deaths; zero human cases may benefit from sufficient, adequate, and timely PEP[9], while elimination shows interruption of rabies virus transmission and no canine cases. In recent years, sporadic cases of canine rabies have been reported in Beijing, indicating the ongoing circulation of the rabies virus within animal populations and the potential for a resurgence of human rabies cases. The absence of a comprehensive monitoring system and insufficient vaccination coverage for canines adds to the uncertainty and difficulty of rabies control. It is essential to accelerate efforts through the implementation of canine vaccination initiatives[10] and the establishment of a monitoring system for canines.
This study had several limitations. Before 1993, all rabies cases were clinically diagnosed rather than laboratory-confirmed; however, the presence of notable signs, typical symptoms, rapid disease progression, and a history of exposure may facilitate clinical diagnosis, and since 2005, all clinically diagnosed cases with qualified specimen collection (29 cases) have been confirmed by laboratory tests, indicating high clinical diagnostic accuracy in Beijing. Additionally, there is a lack of complete data on geographical distribution, sex, etc., from 1973 to 1993, which may introduce selection bias; the missing data in this study were derived from various years, introducing a random element that may potentially result in minor bias.
We thank all the Epidemiological investigators in Beijing. Thanks to Dr Cheng Gong and Ming Luo for their assistance with the experiments.
doi: 10.3967/bes2024.169
Elimination Progress of Human Rabies in Beijing, 1973–2023: A Descriptive Epidemiological Study
-
Tao Zhou: Conceptualization, methodology, investigation, formal analysis, writing-original draft. Xiaomei Li: Investigation, formal analysis, data curation. Cheng Gong and Ming Luo: Experiments. Dan Zhao, Jingbin Pan and Ziang Li: Investigation, data curation. Quanyi Wang and Luodan Suo: Conceptualization, supervision, reviewing, editing. Li Lu: Conceptualization, supervision, critical revision of the manuscript.
注释:1) Author’s Contribution: -
Table 1. Differences of human rabies characteristics between 1973 to 1989 and 2005 to 2023 in Beijing
Characteristics Number of cases (%) Statistics value P value 1973–1989 2005–2023 Sex 2.60 0.11 Male 63 (70.79) 62 (81.58) Female 26 (29.21) 14 (18.42) Age group, years 66.57 < 0.01 ≤ 14 46 (36.22) 2 (2.63) 15– 24 (18.90) 2 (2.63) 30– 21 (16.54) 10 (13.16) 40– 15 (11.81) 18 (23.68) 50– 8 (6.30) 29 (38.16) ≥ 60 13 (10.24) 15 (19.74) Occupation 57.03 < 0.01 Preschool 23 (22.78) 1 (1.32) Student 18 (17.82) 1 (1.32) Workers 7 (6.93) 16 (21.05) Official 4 (3.96) 7 (9.21) Farmer 49 (48.51) 34 (44.74) Retired and others 0 (0) 17 (22.37) Exposure sites 17.57 < 0.01 Hand 47 (43.93) 33 (60.00) Head and face 23 (21.50) 5 (9.09) Upper limb 11 (10.28) 4 (7.27) Lower limb, feet 11 (10.28) 13 (23.64) Multiple and Others 15 (14.02) 0 (0) -
[1] World Health Organization. Rabies vaccines: WHO position paper, April 2018-recommendations. Vaccine, 2018; 36, 5500−3. doi: 10.1016/j.vaccine.2018.06.061 [2] Tao XY, Liu SQ, Zhu WY, et al. Rabies surveillance and control in China over the last twenty years. Biosaf Health, 2021; 3, 142−7. doi: 10.1016/j.bsheal.2020.11.004 [3] Zhou H, Vong S, Liu K, et al. Human rabies in China, 1960-2014: a descriptive epidemiological study. PLoS Negl Trop Dis, 2016; 10, e0004874. [4] Lin FT. The protective effect of the large-scale use of phkc rabies vaccine in humans in China. Bull World Health Organ, 1990; 68, 449−54. [5] Song M, Tang Q, Rayner S, et al. Human rabies surveillance and control in China, 2005-2012. BMC Infect Dis, 2014; 14, 212. doi: 10.1186/1471-2334-14-212 [6] Wu XF, Hu RL, Zhang YZ, et al. Reemerging rabies and lack of systemic surveillance in People’s Republic of China. Emerg Infect Dis, 2009; 15, 1159−64. doi: 10.3201/eid1508.081426 [7] Lu XX, Zhu WY, Wu GZ. Rabies virus transmission via solid organs or tissue allotransplantation. Infect Dis Poverty, 2018; 7, 82. doi: 10.1186/s40249-018-0467-7 [8] Gibson AD, Yale G, Corfmat J, et al. Elimination of human rabies in goa, India through an integrated one health approach. Nat Commun, 2022; 13, 2788. doi: 10.1038/s41467-022-30371-y [9] Burnett MW. Rabies: 2015 update. J Spec Oper Med, 2015; 15, 105−7. [10] Yue YJ, Chen QL, Mu D, et al. A descriptive analysis of human rabies in mainland china, 2005-2020. Int J Environ Res Public Health, 2022; 20, 380. -




 下载:
下载:



 Quick Links
Quick Links