-
Currently, more than 500, 000 patients with stable coronary artery disease (SCAD) undergo percutaneous coronary intervention (PCI) each year globally[1]. Although most of these patients receive drug therapy after PCI, including dual antiplatelet, statin and antihypertensive therapies, a high proportion of patients experience adverse cardiovascular events. The clinical outcomes utilizing revascularization and aggressive drug evaluation (COURAGE) study[2] showed that after PCI, for patients with SCAD the cumulative event risk (all-cause death and nonfatal myocardial infarction) for 4.6 years was as high as 19%. Therefore, it is crucial to evaluate the risk of patients with SCAD who undergo PCI.
A number of studies have shown that N-terminal pro-brain natriuretic peptide (NT-proBNP) has a good predictive value for the risk stratification and prognosis of patients with acute coronary syndrome[3-9]. A few studies also support the statement that NT-proBNP has prognostic value in SCAD patients[10, 11]. However, most of these studies did not report what kind of treatment was performed: drug therapy alone, PCI or coronary artery bypass grafting (CABG). To the best of our knowledge, only a few studies have evaluated the prognostic value of NT-proBNP in patients undergoing PCI. Ndrepepa G et al.[12] reported that NT-proBNP has predictive value for SCAD after bare metal stent implantation; a small-sample study[13] (345 patients) showed that NT-proBNP was a predictor of major adverse cardiovascular events. However, its predictive value for death was not mentioned.
Whether NT-proBNP can predict the risk of mortality for patients who have undergone drug-eluting stent placement, and are receiving dual antiplatelet therapy, has not yet been investigated in a large-sample clinical study. Therefore, the purpose of the current study was to evaluate the long-term prognostic value of NT-proBNP in Chinese patients with SCAD who have received PCI treatment.
-
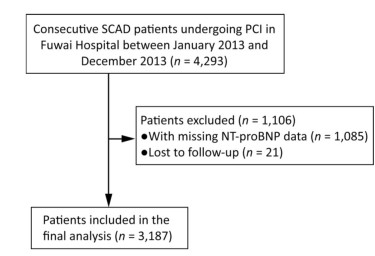
This study is an observational, prospective, single‑center study, which enrolled and collected data from 4, 293 consecutive patients undergoing PCI between January 2013 and December 2013 at Fuwai Hospital, National Center for Cardiovascular Diseases, Beijing, China. The protocol was approved by the local Ethics Committee of the Fuwai hospital's Research Ethics Committee (No. 2013-449) and all patients provided written informed consent. A total of 3, 187 patients were included in the final analysis, after excluding patients for which NT-proBNP data were not obtained (1, 085 patients), or patients who were lost to follow-up (21 patients) (Figure 1).
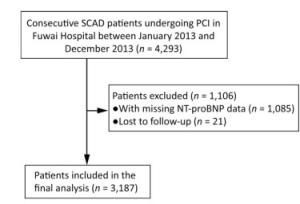
Figure 1. Patient flow chart for the study cohort. SCAD: stable coronary artery disease; PCI: percutaneous coronary intervention; NT-proBNP: N-terminal pro-brain natriuretic peptide.
The indication for PCI included coronary angiography showing a lesion with a coronary stenosis of more than 70% (left main stem greater than 50%) and patients with evidence of ischemia or fractional flow reserve ≤ 0.8; the stent type was left to the treating physician's discretion. If not taking long-term aspirin and P2Y12 inhibitors, selective PCI patients received 300 mg of aspirin and clopidogrel (loading-dose 300 mg) or ticagrelor (loading dose 180 mg), orally, at least 24 h before the procedure. After PCI, patients were prescribed 100 mg of aspirin once daily indefinitely, and either 75 mg of clopidogrel once daily or 90 mg of ticagrelor twice daily for at least 1 year.
-
Blood samples were obtained in the morning after an overnight fast and before coronary angiography and PCI. Blood samples were drawn into tubes containing ethylenediaminetetraacetic acid (EDTA) and sent to the laboratory for NT-proBNP testing as soon as possible. Elisa kits (Biomedica, Austria) were used to measure NT-proBNP plasma levels. The assay range is 0 to 6, 000 pg/mL.
-
The SCAD diagnostic criteria were based on the '2013 ESC guidelines on the management of stable coronary artery disease'[14]. Death was defined as all-cause death and major adverse cardiovascular and cerebrovascular events (MACCE) as a composite of all-cause death, myocardial infarction (MI), revascularization, stent thrombosis (ST) or stroke during follow-up. ST was defined in accordance with the Academic Research Consortium[15], and the analysis included definite, probable and possible ST. Revascularization was defined as unplanned repeated revascularization for ischemic symptoms and events driven by PCI or surgery of any vessel. Spontaneous MI was defined as the presence of clinical symptoms or electrocardiographic changes consistent with myocardial ischemia in the setting of increased levels of cardiac biomarkers above the upper limit of normal, in accordance with the universal definition[16].
-
All patients were evaluated either during clinic visits or by phone at 1, 6, 12, and 24 months of follow-up. Patients were advised to return for coronary angiography if clinically indicated through symptoms or documentation of myocardial ischemia. Patients who reported any ischemic or bleeding events were required to submit related source documents. All adverse events were thoroughly analyzed and adjudicated by two separate cardiologists, and disagreements were resolved through consensus.
-
Continuous variables with normal distribution were expressed as mean ± standard deviation and were compared using Student's t-test, while categorical variables were expressed as number (percentage) and were compared using the Pearson chi-square test or Fisher's exact test. Since NT-proBNP levels were not normally distributed, we log-transformed the values, and NT-proBNP was expressed in median (P25, P75). The predictive value of NT-proBNP was assessed using the area under the receiver operating characteristic curve (AUROC). Survival curves were generated through Kaplan–Meier estimates, and differences in survival were compared using the log-rank test. To evaluate the effect of different levels of NT-pro-BNP on mortality, relative risks and 95 percent confidence intervals were calculated as hazard ratios derived from the Cox proportional-hazards regression model. Model 1 was a univariate model of NT-proBNP; model 2 was a multi-factorial model of age, gender and NT-proBNP; model 3 used stepwise regression to screen for risk factors including body mass index (BMI), hypertension, diabetes, current smoking, previous MI, previous PCI, previous CABG, previous stroke, previous vascular disease, anemia, creatinine clearance (CrCl) < 60 mL/min, left ventricular ejection fraction (LVEF), baseline synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) score, and finally multivariate analysis with NT-proBNP, age and gender. A two-sided P value of less than 0.05 was considered to be statistically significant. All statistical analyses were performed using SAS 9.2 software (SAS Institute, Cary, NC, USA).
-
3, 187 SCAD patients entered in the final analysis after the exclusion of 21 patients who were lost to follow-up and 1, 085 patients with missing NT-proBNP data (Figure 1), with a mean age of 58.09 ± 10.20 year; number of female patients: 705 (22.12%). This patient cohort included 649 cases of asymptomatic myocardial ischemia (20.36%). On discharge, the majority of patients were being treated using clopidogrel (3, 182 patients, 99.84%) and only four patients were taking ticagrelor (0.13%), and 1 patient did not take any P2Y12 receptor antagonist (0.03%). Almost all enrolled patients took aspirin 3, 146 (98.71%). Most enrolled patients were treated using statins (3, 060 patients, 96.02%). Among these, 2, 947 patients had a LVEF > 50% (92.47%). All patients underwent PCI (100%), and 3, 007 patients (94.35%) were successfully implanted with drug-eluting stents; only nine patients (0.28%) were implanted with bare metal stents, and 171 patients (5.37%) were treated through percutaneous transluminal percutaneous coronary angioplasty alone.
After a 2-year follow-up, 36 patients died (1.13%) and 387 patients experienced MACCE (12.14%). Patients who died were older, had a lower BMI and a more significant previous history of MI, a previous history of PCI, a previous history of CABG, a previous history of congestive heart failure, CrCl < 60 mL/min, lower LVEF and underwent more intra-aortic balloon pump (IABP) treatment. Patients with MACCE were older, and were more likely to demonstrate hyperlipidemia, have a previous history of PCI and a higher baseline SYNTAX score, and more of these patients accepted IABP treatment (Table 1).
Table 1. Baseline Clinical Characteristics in SCAD Patients with Versus without Death or MACCE
Characteristing Death
(n = 36)Survival
(n = 3, 151)P
ValueMACCE
(n = 387)No MACCE
(n = 2, 800)P
ValueAge, y 65.61 ± 11.12 58.00 ± 10.16 < 0.001 59.55 ± 10.62 57.89 ± 10.13 0.003 Female, n (%) 5 (13.89) 700 (22.22) 0.231 75 (19.38) 630 (22.50) 0.166 NT-proBNP (P25, P75, pg/mL) 890.70 (714.70, 1353.25) 547.30 (448.90, 761.90) < 0.001 587.50 (456.80, 815.30) 574.45 (449.20, 761.05) 0.064 BMI, kg/m2 24.68 ± 2.92 26.06 ± 3.18 0.010 25.81 ± 3.36 26.08 ± 3.15 0.122 Hypertension, n (%) 25 (69.44) 2, 060 (65.38) 0.610 261 (67.44) 1, 824 (65.14) 0.373 Diabetes mellitus, n (%) Non Diabetes mellitus 22 (61.11) 2, 132 (67.66) 0.706 245 (63.31) 1, 909 (68.18) 0.137 Non-insulin-treated 9 (25.00) 658 (20.88) 89 (23.00) 578 (20.64) Insulin-treated 5 (13.89) 361 (11.46) 53 (13.70) 313 (11.18) Current smoking, n (%) 23 (63.89) 1, 747 (55.44) 0.311 232 (59.95) 1, 538 (54.93) 0.063 dyslipidemia, n (%) 29 (80.56) 2, 184 (69.31) 0.145 286 (73.90) 1, 927 (68.82) 0.042 Previous MI, n (%) 18 (50.00) 832 (26.40) 0.001 110 (28.42) 740 (26.43) 0.405 Previous PCI, n (%) 16 (44.44) 902 (28.63) 0.037 129 (33.33) 789 (28.18) 0.036 Prevous CABG, n (%) 5 (13.89) 141 (4.47) 0.022 23 (5.94) 123 (4.39) 0.172 Previous stroke, n (%) 5 (13.89) 317 (10.06) 0.631 39 (10.08) 283 (10.11) 0.986 CrCl < 60 mL/min 10 (27.78) 422 (13.50) 0.025 62 (16.10) 370 (13.33) 0.137 LVEF (%) 60.02 ± 9.76 63.66 ± 6.93 0.040 63.03 ± 7.30 63.70 ± 6.93 0.078 CAD extension, n (%) LM extension 1 (2.78) 82 (2.60) 1.000 10 (2.58) 73 (2.61) 0.979 1-vessel disease 29 (80.56) 2, 432 (77.18) 0.631 306 (79.07) 2, 155 (76.96) 0.355 2-vessel disease 6 (16.67) 585 (18.60) 0.767 67 (17.31) 525 (18.75) 0.496 3-vessel disease 0 (0.00) 48 (1.52) 0.954 4 (1.03) 44 (1.57) 0.415 Bridge vascular lesions 0 (0.00) 3 (0.10) 1.000 0 (0.00) 3 (0.11) 1.000 IABP use, n (%) 3 (8.33) 30 (0.95) < 0.001 10 (2.58) 23 (9.82) 0.003 NO. of stents per patient (x ± s) 1.89 ± 1.04 1.84 ± 1.11 0.781 1.85 ± 1.09 1.84 ± 1.11 0.875 Femoral artery puncture, n(%) 4 (11.11) 256 (8.12) 0.730 36 (9.30) 224 (8.00) 0.380 Baseline SYNTAX score (x ± s) 12.25 ± 8.08 12.37 ± 7.91 0.932 13.96 ± 8.40 12.15 ± 7.82 < 0.001 Note.NT-proBNP: N-terminal pro-brain natriuretic peptide; SCAD: stable coronary artery disease; MACCE: major adverse cardiovascular and cerebrovascular events; PCI: percutaneous coronary intervention; BMI: body mass index; MI: myocardial infarction; CABG: coronary artery bypass grafting; CAD: coronary artery disease; CrCl: creatinine clearance; SYNTAX: synergy between percutaneous coronary intervention with taxus and cardiac surgery; IABP: intra-aortic balloon pump. Values are presented as mean ± SD, n (%), or median (P25, P75). -
NT-proBNP levels were significantly higher in the death group compared with the survivor group [890.70 pg/mL (714.70, 1353.25) vs. 547.30 pg/mL (448.90, 761.90), P < 0.001]; but there was no significant difference between the MACCE and the non-MACCE group in terms of NT-proBNP levels [587.50 pg/mL (456.80, 815.30) vs. 574.45 pg/mL (449.20, 761.05), P = 0.064].
-
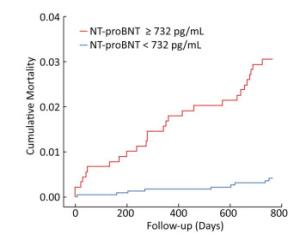
NT-proBNP levels were predictive of all-cause death in the SCAD population (AUROC, 0.768; 95% CI, 0.687-0.849; P < 0.001) (Figure 2). However, NT-proBNP levels did not show a significant predictive value for MACCE (AUROC, 0.529; 95% CI, 0.497-0.561; P = 0.064).

Figure 2. Area under the receiver operating characteristic curve of prognostic value of NT-proBNP in evaluating all-cause death in SCAD population. AUROC, 0.768; 95% CI, 0.687-0.849; P < 0.001. NT-proBNP: N-terminal pro-brain natriuretic peptide; SCAD: stable coronary artery disease; AUROC: area under the receiver operating characteristic curve; CI: confidence interval.
-
When 732 pg/mL was taken as the NT-proBNP cutoff point, the sensitivity was 75.0%, the specificity was 72.3%, the Youden index was the minimum, the sum of specificity and sensitivity was the maximum, and this value was the optimal cutoff point for predicting death.
A Kaplan-Meier survival curve analysis was performed, with a NT-proBNP cutoff point of 732 pg/mL (Figure 3). There were 2, 279 patients with NT-proBNP levels < 732 pg/mL, including nine patients who died during the follow-up period, with an average event-free survival time of 25.27 months. A total of 872 patients with NT-proBNP ≥ 732 pg/mL suffered 27 deaths during the follow-up period, with an average event-free survival time of 24.92 months. A log-rank test was performed, using the NT-proBNP cutoff of 732 pg/mL, and the results suggested that there was a significant difference in survival time between the two groups (P < 0.001).
-
Model 1: Univariate analysis showed that log NT-proBNP was a predictor of death, and the death risk in patients with NT-proBNP levels ≥ 732 pg/mL was 7.73 times higher than the risk in patients with NT-proBNP levels < 732 pg/mL [hazard ratio (HR): 7.73; 95% CI, 3.64-16.44, P < 0.001].
Model 2: After including age and gender variables to be adjusted, log NT-proBNP was still an independent predictor of death, and the death risk for patients with NT-proBNP levels ≥ 732 pg/mL was 6.28 times for those with NT-proBNP levels < 732 pg/mL (HR: 7.73; 95% CI, 2.92-13.50, P < 0.001).
Model 3: Based on model 2, 14 factors have been filtered through a stepwise regression model, including BMI, hypertension, diabetes, current smoking, hyperlipidemia, previous MI, previous PCI, previous CABG, history of stroke, previous vascular disease, anemia, CrCl < 60 mL/min, LVEF, and baseline SYNTAX score. Only previous PCI was independently associated with mortality. Including previous PCI, log NT-proBNP, age and gender in a multivariate analysis indicated that log NT-proBNP was still an independent predictor of death, whereby patients with NT-proBNP levels ≥ 732 pg/mL demonstrated 6.43 times the risk of death compared with those with NT-proBNP levels < 732 pg/mL (HR: 6.43; 95% CI: 2.99-13.82, P < 0.001) (Table 2).
Table 2. Univariate and Multivariate Cox Model Analysis between NT-proBNP and Survival
Model, pg/mL HR 95% CI P Value Model 1 < 732 1.00 ≥ 732 7.73 3.64-16.44 < 0.001 Model 2 < 732 1.00 ≥ 732 6.28 2.92-13.50 < 0.001 Model 3 < 732 1.00 ≥ 732 6.43 2.99-13.82 < 0.001 Note.Model 1: Univariate Cox Model analyses; Model 2: Adding age, gender variables to be adjusted; Model 3: Model 2+previous PCI (Using stepwise regression, entry probability = 0.05, deletion probability = 0.10, age, gender and LOG NT-proBNP were forcedly introduced; and screening of BMI, hypertension, diabetes, current smoking, hyperlipidemia, previous myocardial infarction, previous PCI, Previous CABG, Previous Stroke, Previous Vascular Disease, Anemia, CrCl < 60 mL/min, LVEF, SQSS, eventually only previous PCI left in mode). NT-proBNP: N-terminal pro-brain natriuretic peptide; CrCl: creatinine clearance; HR: hazard ratio; CI: confidence interval. -
This study included a large sample size, and was a prospective real-world 2-year follow-up study. Our study showed that: 1) among patients with SCAD, even after PCI treatment, there was still a 1.13% mortality rate and a 12.14% MACCE rate (a composite of all-cause death, myocardial infarction, revascularization, stent thrombosis or stroke) at a 2-year follow-up; 2) after adjustment for multiple clinical variables, NT-proBNP was still a strong independent predictor of death, but was not an ideal predictor for MACCE; 3) a NT-proBNP level of 732 pg/mL was the optimal cutoff point for predicting long-term mortality after PCI in patients with SCAD.
For the first time, this large-sample study demonstrated that for SCAD patients, who were mainly treated using drug-eluting stents (94.35%) and optimized drug therapy, baseline NT-proBNP was still predictive of the long-term risk of death. Some previous studies have shown that NT-proBNP has predictive value for patients with SCAD, such as Bibbins-Domingo K et al.[11] who followed 987 patients with SCAD for an average of 3.7 years, and showed that NT-proBNP levels can be used to predict the risk of death; Kragelund C et al.[10] found that for patients with SCAD with angina pectoris symptoms, NT-proBNP levels were significantly higher in patients who died compared with those who survived. However, none of the above studies mentioned whether such patients were treated using revascularization therapy or drug therapy alone. There were very limited reports on whether NT-proBNP had the same predictive value for long-term prognosis among SCAD patients after PCI treatment. In an early study, Ndrepepa G et al.[12] showed that NT-proBNP had a predictive value for death in patients with SCAD who underwent treatment using a bare metal stent. In recent years, drug-eluting stents, and in particular the new generation of drug-eluting stents, have been widely used in coronary heart disease patients, and they significantly reduce the risk of revascularization compared with bare metal stents[17]. However, to the best of our knowledge, there has been no large-scale study investigating the association between NT-proBNP and death after drug-eluting stent treatment. The current study confirmed that NT-proBNP is a strong predictor of 2-year death in SCAD after PCI in the drug-eluting stent era. However, in the current study, NT-proBNP was assessed only upon admission. In future research, it would be interesting to assess if the dynamic measurement of NT-proBNP levels are still good predictor of long-term all-cause death.
Our study failed to show that NT-proBNP had a predictive value for MACCE (AUROC, 0.529; P = 0.064). In a previous study, Bibbins-Domingo K et al.[11] showed that NT-proBNP levels could be used to predict the risk of cardiovascular events (myocardial infarction, stroke, and heart failure) in patients with SCAD; Mishra RK et al.[18] showed that NT-proBNP was a significant predictor of major adverse cardiovascular events (heart failure, nonfatal myocardial infarction, stroke or transient ischemic attack, cardiovascular death) after an average follow-up of 6.5 ± 3.3 y; however, the results reported by Niccoli et al.[19] differ from the above, whereby N-terminal pro-atrial natriuretic peptide levels significantly affected prognosis after PCI, but not NT-proBNP levels. The difference in the results of these studies may be related to the different definitions of MACCE. The current study showed that NT-proBNP levels demonstrate a statistically significant trend in predicting MACCE. Extending the follow-up time may produce different results, and this deserves further study.
NT-proBNP levels are affected by various factors[20], including age, gender, BMI[21], cardiac dysfunction and renal insufficiency; previous studies have also shown[22] that NT-proBNP is associated with coronary artery stenosis. However, whether NT-proBNP is independent of these factors in affecting the long-term mortality of patients is unknown. The results of the current study indicate that, regardless if univariate analysis, or age and gender-adjusted multivariate analyses, are applied, NT-proBNP levels are still an independent predictor of death. This also holds true if BMI, hypertension, diabetes, current smoking, hyperlipidemia, previous MI, previous PCI, previous CABG, prior stroke, previous vascular disease, anemia, CrCl < 60 mL/min, LVEF, or baseline SYNTAX score are included in the analysis. Therefore, NT-proBNP is a strong independent predictor of death that is independent of the risk factors above.
In the current study, the results showed that 732 pg/mL was the optimal NT-proBNP cutoff point for predicting long-term mortality after PCI in patients with SCAD. The risk of death HR of patients with NT-proBNP levels ≥ 732 pg/mL was 6.43 times of those with NT-proBNP levels < 732 pg/mL. These results will help clinicians to identify patients with SCAD after PCI who are at a high risk of death, and strengthen the monitoring and treatment of these patients to reduce the incidence of death. In clinical practice, individual differences should also be taken into account, such as age, kidney function, heart failure and other clinical conditions to make a comprehensive judgment.
Currently, the exact mechanism underlying the positive correlation between NT-proBNP levels and the death risk in SCAD is still unclear. The current study, and previous studies[7, 12] demonstrated that the correlation between NT-proBNP and death was not linked to LVEF. Therefore, it is not feasible to account for the correlation between the NT-proBNP and the increased risk for death is caused only by the worsening of heart failure. Previous studies have shown that the level of NT-proBNP is not only associated with myocardial ischemia in coronary heart disease, but also in a variety of cardiac pathological conditions. Previous studies have reported that myocardial ischemia could induce an increase in the expression of the natriuretic peptide gene[23, 24], and raise natriuretic peptide levels. In addition, the increase in NT-proBNP levels may reflect subclinical levels of ventricular dysfunction or diastolic dysfunction[11, 25], vascular dysfunction[26], and the activation of the renin-angiotensin- aldosterone system. All these factors could lead to a poor prognosis and an increased risk of death. However, the exact mechanism underlying the link between NT-proBNP and death needs to be studied further.
Whether clinicians should choose treatments to reduce NT-proBNP levels in patients with SCAD who have high levels of NT-proBNP after PCI, thereby potentially reducing the risk of death, is worth further study. Strategies such as adjusting the PCI strategy or drug therapy program based on dynamically monitoring the level of NT-proBNP needs to be explored further.
Some limitations of our analysis should be considered. First, the single center observational nature of the study may limit the generalizability of its findings. Second, we did not measure NT-proBNP dynamically. Therefore, testing NT-proBNP before or after PCI, to achieve a better predictive value, remains to be further evaluated.
In conclusion, in a large real-world population of PCI patients, NT-proBNP is a strong predictive marker of the long-term risk of death in Chinese patients with SCAD in the contemporary drug eluting stent era. NT-proBNP levels of 732 pg/mL represent the optimal cutoff point for predicting long-term mortality in patients with SCAD after PCI.
-
ZXY participated in the study concept and design, analysis and interpretation of the data, and drafting of the manuscript. LJX participated in the study design, analysis and interpretation of the data, and the critical revision of the manuscript. TXF, XJJ, SY, and JL participated in the study concept and design, analysis and interpretation of the data. CJ, SL, GLJ, and GZ participated in the study concept and design, and the critical revision of the manuscript. QSB, YYJ, and GRL participated in the critical revision of the manuscript, and the final approval of the manuscript. YJQ and XB participated in the study concept and design, analysis and interpretation of the data, the critical revision of the manuscript, and the final approval of the manuscript.
-
The authors have no conflicts of interest to declare.
doi: 10.3967/bes2018.117
Prognostic Value of NT-proBNP in Stable Coronary Artery Disease in Chinese Patients after Percutaneous Coronary Intervention in the Drug-eluting Stent Era
-
Abstract:
Objective The predictive value of N-terminal pro-brain natriuretic peptide (NT-proBNP) in patients with stable coronary artery disease (SCAD) in the drug-eluting stent era is not yet clear. We aimed to evaluate the prognostic value of NT-proBNP in SCAD patients after percutaneous coronary intervention (PCI). Methods We examined 4, 293 consecutive SCAD patients who underwent PCI between January 2013 and December 2013 in Fuwai Hospital, China. The primary endpoint was all-cause death. NT-proBNP levels were measured before PCI using Elisa kits (Biomedica, Austria). The indication for PCI was based on the degree of coronary stenosis and evidence of ischemia. Results Among 3, 187 SCAD patients with NT-proBNP data, after a 2-year follow-up, NT-proBNP levels were predictive for all-cause death in the SCAD population[area under the receiver operating characteristic curve, 0.768; 95% confidence interval (CI), 0.687-0.849; P < 0.001]. At the optimum cutoff point of 732 pg/mL, the sensitivity and specificity of death was 75.0% and 72.3%, respectively. In a multivariable Cox regression model, the death hazard ratio was 6.43 (95% CI, 2.99-13.82; P < 0.001) for patients with NT-proBNP levels ≥ 732 pg/mL, compared with < 732 pg/mL. Conclusion NT-proBNP is a strong predictor of 2-year death with SCAD after PCI in the drug-eluting stent era. -
Key words:
- NT-proBNP /
- Stable coronary disease /
- Death /
- Prognosis /
- Percutaneous coronary intervention
-
Figure 2. Area under the receiver operating characteristic curve of prognostic value of NT-proBNP in evaluating all-cause death in SCAD population. AUROC, 0.768; 95% CI, 0.687-0.849; P < 0.001. NT-proBNP: N-terminal pro-brain natriuretic peptide; SCAD: stable coronary artery disease; AUROC: area under the receiver operating characteristic curve; CI: confidence interval.
Table 1. Baseline Clinical Characteristics in SCAD Patients with Versus without Death or MACCE
Characteristing Death
(n = 36)Survival
(n = 3, 151)P
ValueMACCE
(n = 387)No MACCE
(n = 2, 800)P
ValueAge, y 65.61 ± 11.12 58.00 ± 10.16 < 0.001 59.55 ± 10.62 57.89 ± 10.13 0.003 Female, n (%) 5 (13.89) 700 (22.22) 0.231 75 (19.38) 630 (22.50) 0.166 NT-proBNP (P25, P75, pg/mL) 890.70 (714.70, 1353.25) 547.30 (448.90, 761.90) < 0.001 587.50 (456.80, 815.30) 574.45 (449.20, 761.05) 0.064 BMI, kg/m2 24.68 ± 2.92 26.06 ± 3.18 0.010 25.81 ± 3.36 26.08 ± 3.15 0.122 Hypertension, n (%) 25 (69.44) 2, 060 (65.38) 0.610 261 (67.44) 1, 824 (65.14) 0.373 Diabetes mellitus, n (%) Non Diabetes mellitus 22 (61.11) 2, 132 (67.66) 0.706 245 (63.31) 1, 909 (68.18) 0.137 Non-insulin-treated 9 (25.00) 658 (20.88) 89 (23.00) 578 (20.64) Insulin-treated 5 (13.89) 361 (11.46) 53 (13.70) 313 (11.18) Current smoking, n (%) 23 (63.89) 1, 747 (55.44) 0.311 232 (59.95) 1, 538 (54.93) 0.063 dyslipidemia, n (%) 29 (80.56) 2, 184 (69.31) 0.145 286 (73.90) 1, 927 (68.82) 0.042 Previous MI, n (%) 18 (50.00) 832 (26.40) 0.001 110 (28.42) 740 (26.43) 0.405 Previous PCI, n (%) 16 (44.44) 902 (28.63) 0.037 129 (33.33) 789 (28.18) 0.036 Prevous CABG, n (%) 5 (13.89) 141 (4.47) 0.022 23 (5.94) 123 (4.39) 0.172 Previous stroke, n (%) 5 (13.89) 317 (10.06) 0.631 39 (10.08) 283 (10.11) 0.986 CrCl < 60 mL/min 10 (27.78) 422 (13.50) 0.025 62 (16.10) 370 (13.33) 0.137 LVEF (%) 60.02 ± 9.76 63.66 ± 6.93 0.040 63.03 ± 7.30 63.70 ± 6.93 0.078 CAD extension, n (%) LM extension 1 (2.78) 82 (2.60) 1.000 10 (2.58) 73 (2.61) 0.979 1-vessel disease 29 (80.56) 2, 432 (77.18) 0.631 306 (79.07) 2, 155 (76.96) 0.355 2-vessel disease 6 (16.67) 585 (18.60) 0.767 67 (17.31) 525 (18.75) 0.496 3-vessel disease 0 (0.00) 48 (1.52) 0.954 4 (1.03) 44 (1.57) 0.415 Bridge vascular lesions 0 (0.00) 3 (0.10) 1.000 0 (0.00) 3 (0.11) 1.000 IABP use, n (%) 3 (8.33) 30 (0.95) < 0.001 10 (2.58) 23 (9.82) 0.003 NO. of stents per patient (x ± s) 1.89 ± 1.04 1.84 ± 1.11 0.781 1.85 ± 1.09 1.84 ± 1.11 0.875 Femoral artery puncture, n(%) 4 (11.11) 256 (8.12) 0.730 36 (9.30) 224 (8.00) 0.380 Baseline SYNTAX score (x ± s) 12.25 ± 8.08 12.37 ± 7.91 0.932 13.96 ± 8.40 12.15 ± 7.82 < 0.001 Note.NT-proBNP: N-terminal pro-brain natriuretic peptide; SCAD: stable coronary artery disease; MACCE: major adverse cardiovascular and cerebrovascular events; PCI: percutaneous coronary intervention; BMI: body mass index; MI: myocardial infarction; CABG: coronary artery bypass grafting; CAD: coronary artery disease; CrCl: creatinine clearance; SYNTAX: synergy between percutaneous coronary intervention with taxus and cardiac surgery; IABP: intra-aortic balloon pump. Values are presented as mean ± SD, n (%), or median (P25, P75). Table 2. Univariate and Multivariate Cox Model Analysis between NT-proBNP and Survival
Model, pg/mL HR 95% CI P Value Model 1 < 732 1.00 ≥ 732 7.73 3.64-16.44 < 0.001 Model 2 < 732 1.00 ≥ 732 6.28 2.92-13.50 < 0.001 Model 3 < 732 1.00 ≥ 732 6.43 2.99-13.82 < 0.001 Note.Model 1: Univariate Cox Model analyses; Model 2: Adding age, gender variables to be adjusted; Model 3: Model 2+previous PCI (Using stepwise regression, entry probability = 0.05, deletion probability = 0.10, age, gender and LOG NT-proBNP were forcedly introduced; and screening of BMI, hypertension, diabetes, current smoking, hyperlipidemia, previous myocardial infarction, previous PCI, Previous CABG, Previous Stroke, Previous Vascular Disease, Anemia, CrCl < 60 mL/min, LVEF, SQSS, eventually only previous PCI left in mode). NT-proBNP: N-terminal pro-brain natriuretic peptide; CrCl: creatinine clearance; HR: hazard ratio; CI: confidence interval. -
[1] Al-Lamee R, Thompson D, Dehbi HM, et al. Percutaneous coronary intervention in stable angina (ORBITA):a double-blind, randomised controlled trial. Lancet, 2017; 391, 31-40. http://www.ncbi.nlm.nih.gov/pubmed/29103656 [2] Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med, 2007; 356, 1503-16. doi: 10.1056/NEJMoa070829 [3] Scirica BM, Sabatine MS, Jarolim P, et al. Assessment of multiple cardiac biomarkers in non-ST-segment elevation acute coronary syndromes:observations from the MERLIN-TIMI 36 trial. Eur Heart J, 2011; 32, 697-705. doi: 10.1093/eurheartj/ehq468 [4] Heeschen C, Hamm CW, Mitrovic V, et al. N-terminal pro-B-type natriuretic peptide levels for dynamic risk stratification of patients with acute coronary syndromes. Circulation, 2004; 110, 3206-12. doi: 10.1161/01.CIR.0000147611.92021.2B [5] Windhausen F, Hirsch A, Sanders GT, et al. N-terminal pro-brain natriuretic peptide for additional risk stratification in patients with non-ST-elevation acute coronary syndrome and an elevated troponin T:an Invasive versus Conservative Treatment in Unstable coronary Syndromes (ICTUS) substudy. Am Heart J, 2007; 153, 485-92. doi: 10.1016/j.ahj.2006.12.012 [6] James SK, Lindahl B, Siegbahn A, et al. N-terminal pro-brain natriuretic peptide and other risk markers for the separate prediction of mortality and subsequent myocardial infarction in patients with unstable coronary artery disease:a Global Utilization of Strategies To Open occluded arteries (GUSTO)-Ⅳ substudy. Circulation, 2003; 108, 275-81. doi: 10.1161/01.CIR.0000079170.10579.DC [7] de Lemos JA, Morrow DA, Bentley JH, et al. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med, 2001; 345, 1014-21. doi: 10.1056/NEJMoa011053 [8] Kurtul A, Yarlioglues M, Murat SN, et al. N-Terminal Pro-Brain Natriuretic Peptide Level is Associated With Severity and Complexity of Coronary Atherosclerosis in Patients With Acute Coronary Syndrome. Clin Appl Thromb Hemost, 2016; 22, 69-76. doi: 10.1177/1076029614541954 [9] Kurtul A, Duran M, Yarlioglues M, et al. Association between N-terminal pro-brain natriuretic peptide levels and contrast-induced nephropathy in patients undergoing percutaneous coronary intervention for acute coronary syndrome. Clin Cardiol, 2014; 37, 485-92. doi: 10.1002/clc.2014.37.issue-8 [10] Kragelund C, Gronning B, Kober L, et al. N-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med, 2005; 352, 666-75. doi: 10.1056/NEJMoa042330 [11] Bibbins-Domingo K, Gupta R, Na B, et al. N-terminal fragment of the prohormone brain-type natriuretic peptide (NT-proBNP), cardiovascular events, and mortality in patients with stable coronary heart disease. JAMA, 2007; 297, 169-76. doi: 10.1001/jama.297.2.169 [12] Ndrepepa G, Braun S, Niemoller K, et al. Prognostic value of N-terminal pro-brain natriuretic peptide in patients with chronic stable angina. Circulation, 2005; 112, 2102-7. doi: 10.1161/CIRCULATIONAHA.105.550715 [13] Dai DF, Hwang JJ, Lin JL, et al. Joint effects of N-terminal pro-B-type-natriuretic peptide and C-reactive protein vs. angiographic severity in predicting major adverse cardiovascular events and clinical restenosis after coronary angioplasty in patients with stable coronary artery disease. Circ J, 2008; 72, 1316-23. doi: 10.1253/circj.72.1316 [14] Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease:the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J, 2013; 34, 2949-3003. doi: 10.1093/eurheartj/eht296 [15] Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials:a case for standardized definitions. Circulation, 2007; 115, 2344-51. doi: 10.1161/CIRCULATIONAHA.106.685313 [16] Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol, 2012; 60, 1581-98. doi: 10.1016/j.jacc.2012.08.001 [17] Bonaa KH, Mannsverk J, Wiseth R, et al. Drug-Eluting or Bare-Metal Stents for Coronary Artery Disease. N Engl J Med, 2016; 375, 1242-52. doi: 10.1056/NEJMoa1607991 [18] Mishra RK, Beatty AL, Jaganath R, et al. B-type natriuretic peptides for the prediction of cardiovascular events in patients with stable coronary heart disease:the Heart and Soul Study. J Am Heart Assoc, 2014; 3, e000907. http://europepmc.org/abstract/MED/25053234 [19] Niccoli G, Conte M, Marchitti S, et al. NT-proANP and NT-proBNP circulating levels as predictors of cardiovascular outcome following coronary stent implantation. Cardiovasc Revasc Med, 2016; 17, 162-8. doi: 10.1016/j.carrev.2016.02.012 [20] van Kimmenade RR, Pinto YM, Januzzi JL Jr. Importance and interpretation of intermediate (gray zone) amino-terminal pro-B-type natriuretic peptide concentrations. Am J Cardiol, 2008; 101, 39-42. doi: 10.1016/j.amjcard.2007.11.018 [21] Das SR, Drazner MH, Dries DL, et al. Impact of body mass and body composition on circulating levels of natriuretic peptides:results from the Dallas Heart Study. Circulation, 2005; 112, 2163-8. doi: 10.1161/CIRCULATIONAHA.105.555573 [22] Wu N, Ma F, Guo Y, et al. Association of N-terminal pro-brain natriuretic peptide with the severity of coronary artery disease in patients with normal left ventricular ejection fraction. Chin Med J, 2014; 127, 627-32. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhcmj201404007 [23] Hama N, Itoh H, Shirakami G, et al. Rapid Ventricular Induction of Brain Natriuretic Peptide Gene Expression in Experimental Acute Myocardial Infarction. Circulation, 1995; 92, 1558-64. doi: 10.1161/01.CIR.92.6.1558 [24] Goetze JP, Christoffersen C, Perko M, et al. Increased cardiac BNP expression associated with myocardial ischemia. FASEB J, 2003; 17, 1105-7. doi: 10.1096/fj.02-0796fje [25] Bibbins-Domingo K, Ansari M, Schiller NB, et al. B-type natriuretic peptide and ischemia in patients with stable coronary disease:data from the Heart and Soul study. Circulation, 2003; 108, 2987-92. doi: 10.1161/01.CIR.0000103681.04726.9C [26] D'Souza SP, Davis M, Baxter GF. Autocrine and paracrine actions of natriuretic peptides in the heart. Pharmacol Ther, 2004; 101, 113-29. doi: 10.1016/j.pharmthera.2003.11.001 -




 下载:
下载:



 Quick Links
Quick Links