-
Currently, there is a lack of conclusive evidence regarding nutritional interventions for treating depression in rescuers, both domestically and internationally. Interventions for depression mainly follow the principles of “regulating qi, relieving depression, and empathy”[1]. As over-the-counter (OTC) preparations or nutritional supplements, some studies have explored the effectiveness of herbal remedies such as saffron, turmeric, rose root, lavender, and so on in alleviating depression[2]. Intervention methods have evolved from single use to the combination of two or more herbal plants to achieve optimal results. Feng et al.[3] found that traditional Chinese medicine formulas such as BanxiaHoupu Tang, ChaihuShugan San, GanmaiDazao Tang, ShuganJieyu capsules, Kaixin San, Wuling Capsules, Xiaoyao San, and Yueju could alleviate depressive symptoms. Liu et al.[4] found that ginseng, epimedium, peony, Rhodiola, and saffron can alleviate depressive symptoms, and there are also various herbal formulas that can be used as a means of relieving depressive symptoms. Considering the side effects of western medicine, herbal formulas are gradually becoming popular for their good tolerance, fewer side effects, and low cost.
However, there is a lack of evidence regarding the efficacy of nutritional interventions in treating depression among rescuers in China. The lifetime prevalence of adult depression in China is 6.8%[5]; therefore, how to intervene early to treat depression is an urgent problem that needs to be solved. At the beginning of the 21st century, the incidence of depression in the general population was from 25.20% to 51.00%[6-7]. Compared with the general population, rescuers face a dangerous, complex, and harsh working environment, high training intensity, and a higher risk of depression. If timely screening and effective intervention are not carried out, their daily training, task execution, and combat capability are affected. Given the limitations of the various intervention methods, it is necessary to find safer and more effective intervention methods to improve the combat effectiveness of rescuers. This study conducted a randomized controlled trial to provide a nutritional intervention for treating rescuers who were evaluated positive for depression. It also aimed to explore the intervention effects of herbal plant formulations on depression status and provide conclusive evidence regarding the efficacy of nutritional interventions for treating depression in rescuers.
-
A total of 4,460 valid questionnaires were collected from one military unit between June to August, 2022. The inclusion criteria were as follows: (1) aged 18–60; (2) intelligible with no language barriers and capable of independently reading and understanding questionnaires; (3) recently involved in military training or disaster relief; (4) evaluated to have depression based on their Self-Rating Depression Scale score; and (5) provided informed consent. The exclusion criteria were as follows: (1) those with mental illnesses or severe physical diseases and (2) those currently receiving other psychological treatments. This study was approved by the Ethics Committee of the PLA General Hospital (approval number S201910801) and registered for clinical trials under the number ChiCTR1900023441. All study participants signed an informed consent form. The participants were recruited from a large group of individuals who tested positive for depression on the self-rating depression scale, and were voluntarily enrolled in the study after signing an informed consent form. A completely randomized method was used to generate random numbers for grouping. Both the participants and data analysis were blinded to the grouping. The control group in this study received health education, and the participants were unaware of the experimental design and groupings, making it a single-blind design. Sample size calculation: According to the sample size estimationFormula: $ n=\dfrac{\left[Z_\alpha \sqrt{2\bar{p}(1-\bar{p} )}+Z_\beta \sqrt{p_1(1-p_1)+p_2(1-p_2)} \right]^2}{(p_1-p_2)^2} $, $ p_1$ is the effectiveness of the experimental group and $ p_2$ is the self-healing rate of the control group, $ \bar{p}=\dfrac{(p_1+p_2)}{2} $. A literature review estimated that the self-healingrate of p2 was 26%. According to traditional Chinese medicine texts such as the Compendium of Materia Medica, the estimated effective rate of p1 is 81%. A sample size of 24 cases, with 12 cases in each group, satisfied the experimental requirements.
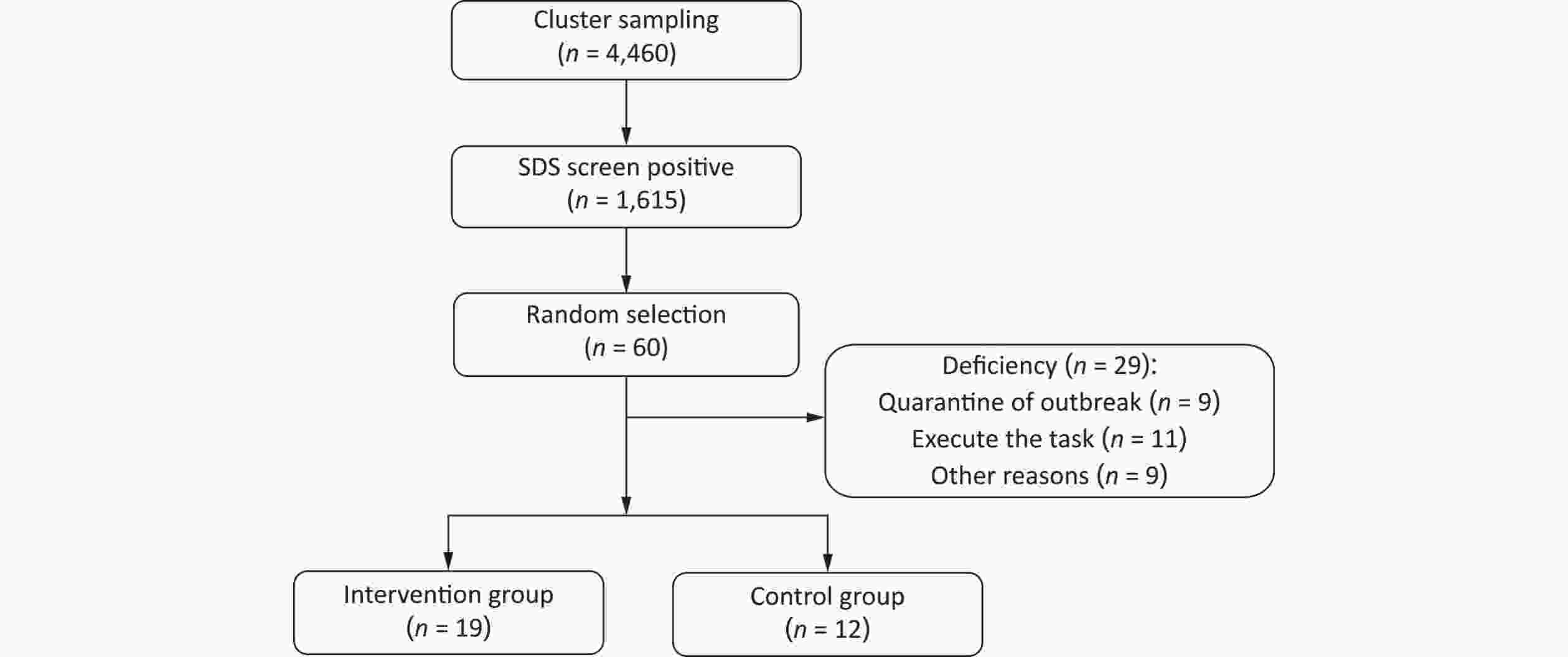
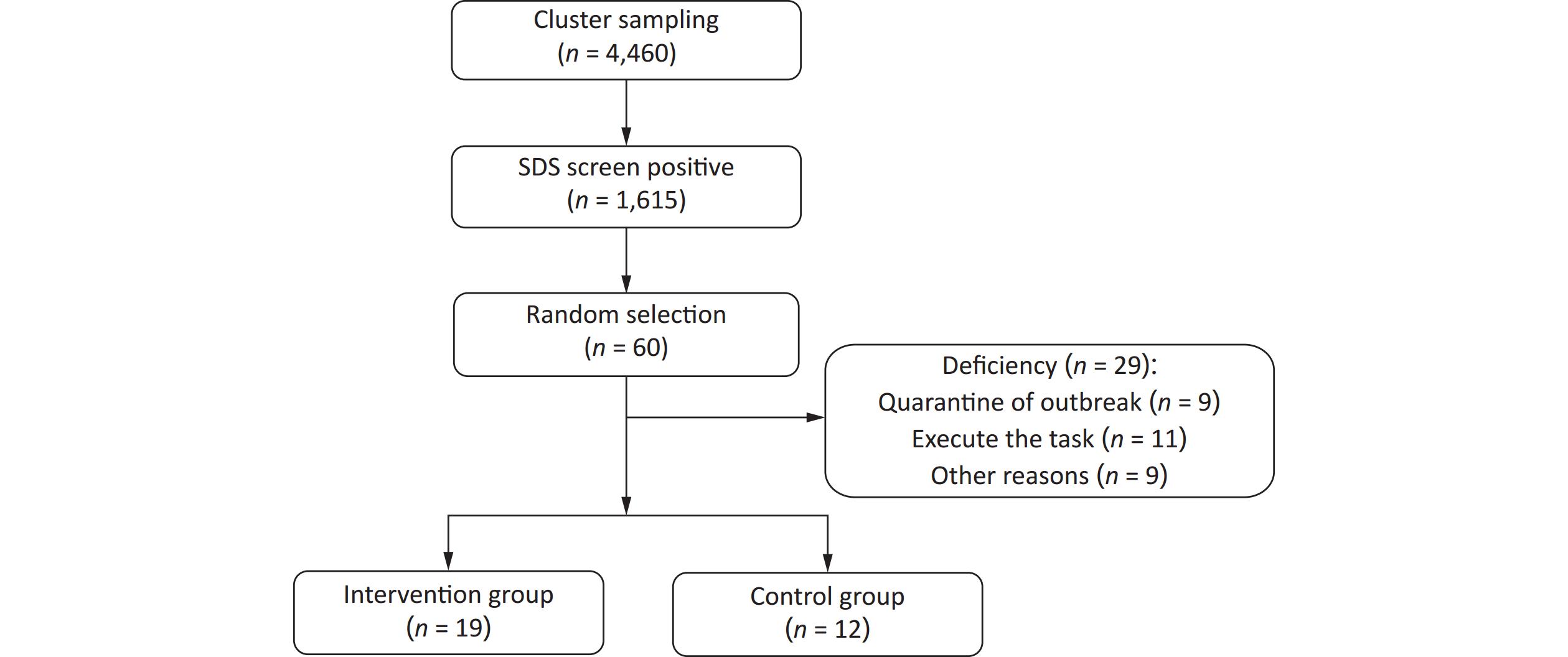
In this study, the SDS was used to screen rescuers, and initially, 1,615 positive cases were identified. Sixty individuals were then recruited from this group and randomly divided into two groups of 30 each. After excluding 9 cases who had to self- isolate owing to the pandemic, 11 who went on missions, and 9 for other reasons such as resignation, a total of 31 subjects were finally included in the study: 19 in the intervention group and 12 in the control group (Figure 1).
-
We took “rescuer” to signify an individual who participates in various special tasks such as earthquake relief, flood relief, anti-terrorism and maintaining peace and stability, search and rescue, and military exercises and trainings.
-
The SDS consists of 20 items rated on a 4-point scale. Fifteen items are scored positively from 1 to 4, with “1” indicating “rarely or never experiencing the symptom,” “2” indicating “sometimes experiencing the symptom,” “3” indicating “often experiencing the symptom,” and “4” indicating “experiencing the symptom most or all of the time.” The five items are scored in reverse, ranging from 4 to 1. The total raw score is the sum of all item scores; the standard score = total raw score × 1.25, rounded to the nearest whole number. The cutoff for the SDS standard score is 53 points, with scores less than 53 indicating no depression, 53–62 indicating mild depression, 63–72 indicating moderate depression, and > 73 indicating severe depression.
-
Education level: 1 = college degree or higher; 2 = high school or lower. Marital status: 1 = unmarried; 2 = married. Time: 0 = before intervention; 1 = after the first intervention; 2 = after the intervention ended. Groups: 1, intervention group; 2, control group.
-
The intervention group underwent nutritional intervention that included a compound paste therapy and health education. The main ingredients of the compound paste were double-petaled red rose, Seville orange flower, red yeast rice, peach kernel, cordyceps militaris, Angelica, sea buckthorn, hawthorn, licorice, and oligoisomaltose. The dosage was 10 g administered orally twice daily for a duration of six weeks.
-
Health education was provided by a psychological counselor in the control group.
-
The intervention was conducted using a group-therapy approach, with the primary researcher acting as the main intervener. A member of the research team served as the recruiter and introduced the study theme to potential participants. Interested individuals could acquire the intervener's contact information by scanning the WeChat QR code. The participants were randomly assigned to either the intervention or control group using a randomized number table. Baseline measurements were conducted using the Wenjuan Xing (Questionnaire Star) platform. The intervention group received the compound paste therapy nutritional intervention, with a frequency of twice daily for six consecutive weeks. Upon completion of the intervention, data collection for both groups was completed using the Wenjuan Xing platform.
-
Data analysis was performed using SPSS 23.0. For data following a normal distribution, descriptive statistics were presented as mean ± standard deviation (x̄ ± s), and independent samples t-tests were used for analysis. Non-normally distributed data were described as medians and interquartile ranges and analyzed using the rank sum test. Categorical data were expressed in frequency and percentage, and analyzed by the Chi-square (χ2) test. A generalized linear mixed model was used for statistical analysis. All analyses were two-tailed, and a P < 0.05 was considered statistically significant.
-
Qualified psychological counselors who had undergone unified training conducted the research. Cluster sampling was used during the questionnaire data collection phase. All surveyors were required to pass a unified training and examination before commencing their duties. They used a standardized instruction to assist the participants in filling out the questionnaires. The participants independently completed the questionnaires on the Wen Juan Xing (Questionnaire Star) platform and submitted them on the spot. The surveyors conducted a preliminary check of the questionnaires to immediately correct any omissions or errors and ensure the completeness and accuracy of the data.
After collection, the questionnaires were double-entered by different data entry personnel to ensure quality of data entry. A 10% sample was selected for repeated measurements, achieving a consistency rate > 99%.
-
There were no statistically significant differences between the intervention and control groups in terms of age, gender, educational level, marital status, and monthly family income (P > 0.05) at baseline. Additionally, there was no significant difference in the SDS scores between the intervention and control groups before the intervention (P > 0.05) (Table 1).
Table 1. Baseline characteristics of study subjects
Variable Grouping N Intervention group (n, %) Control group (n, %) t/z/χ2 P Age (years) 22 (21, 26) 22 (21, 25.25) −0.247 0.805 Gender − 0.142 Male 29 19 10 Female 2 0 2 Educational level 1.106 0.293 Collage and above 17 9 8 High school or below 14 10 4 Marital status 0.000 1.000 Single 26 16 10 Married 5 3 2 Monthly family income (Yuan) − 0.660 2,999 and below 10 6 4 3,000–7,999 13 7 6 8,000 and above 8 6 2 SDS 63 (63, 63) 63 (60, 65.25) −0.316 0.752 Note. There were no statistically significant differences between the intervention and control groups in terms of age, gender, educational level, marital status, and monthly family income (P > 0.05) at baseline. Additionally, there was no significant difference in the SDS scores between the intervention and control groups before the intervention (P > 0.05). SDS, Self-Rating Depression Scale. -
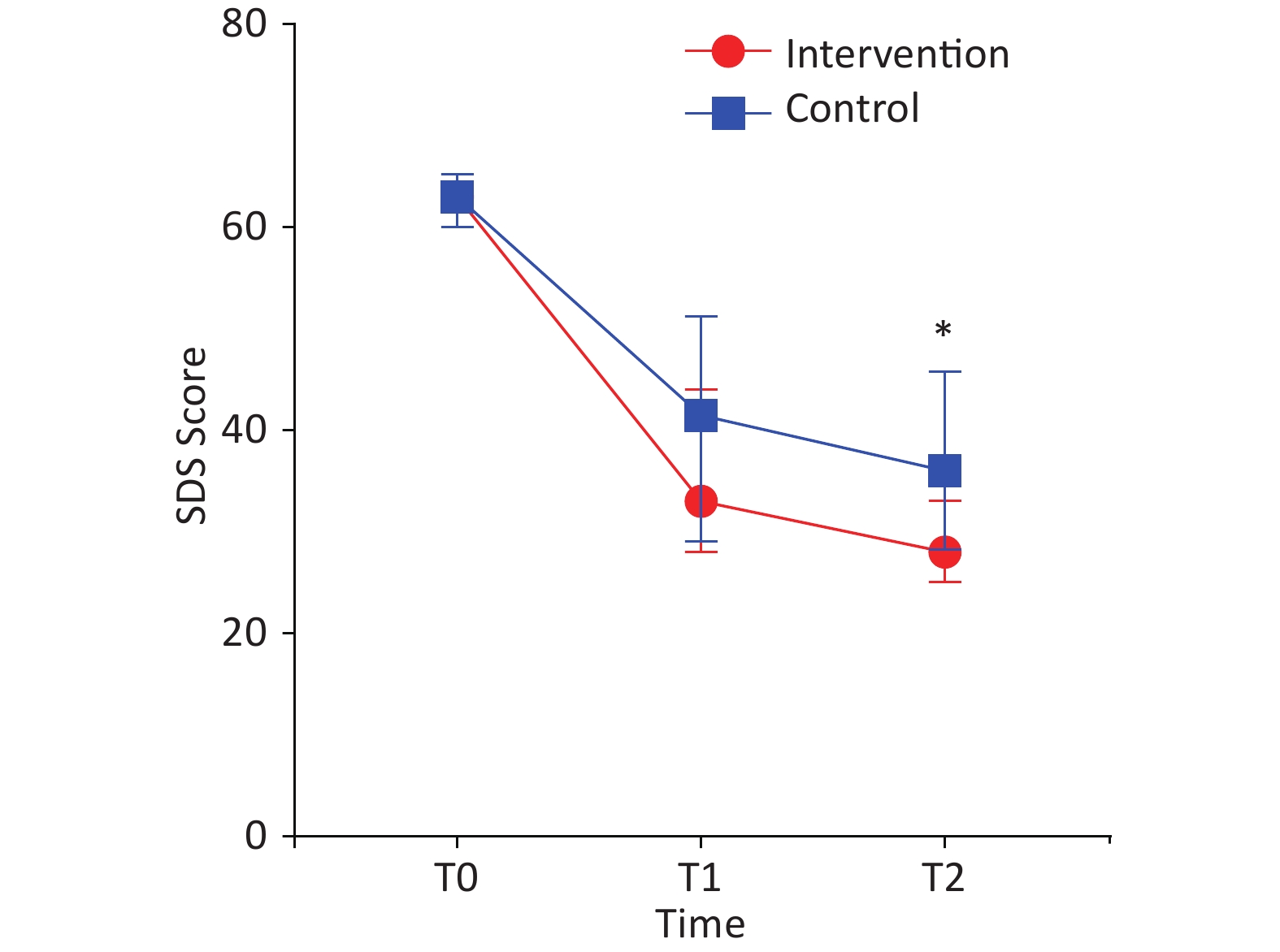
A generalized linear mixed model was used that included age, marital status, time, group, and time × group interactions compared with the SDS scores of the groups before intervention, the SDS scores of the intervention and control groups decreased significantly after the first intervention and after the conclusion of the intervention (P < 0.05). After the first intervention, the SDS scores of the intervention group were higher than those of the control group, and there was no significant difference (β = 4.129, P > 0.05); however, there was significant difference (β = 8.383, P < 0.05).
Within-group comparisons revealed that both the intervention and control groups had significantly lower SDS scores after the intervention than before the intervention (P < 0.05), indicating the effectiveness of the intervention in reducing depressive symptoms (Table 2 and Figure 2).
Table 2. Results of the generalized linear mixed model for SDS scores post-Intervention in both groups
Group N SDS scores, median (IQR) Per-intervention Post-1st intervention Post-intervention Treatment group 19 63 (63, 63) 33 (28, 44) 28 (25, 33) Control group 12 63 (60, 65) 41.5 (29, 51) 36 (28, 46) β −1.665 4.129 8.383 P 0.201 0.302 0.024 Note. The model includes age, gender, marital status, level of education, average monthly income per household member, time, group, and the interaction between time and group. SDS, Self-Rating Depression Scale; IQR, interquartile range. -
During the intervention process, no adverse reactions were reported in either the nutritional intervention group or the control group.
-
As socioeconomic development accelerates, various types of accidents have emerged, and rescuers are increasingly burdened with the task of reacting to sudden disasters. Constantly in a state of duty and combat readiness, rescuers experience intense mental strain. This has led to a range of adverse psychological reactions such as anxiety and depression, making mental health issues increasingly prominent among rescuers. For instance, during the Wenchuan earthquake rescue operation, the incidence rate of depression was 38% among personnel engaged in relief work. Rescuers’ psychological issues are worthy of significant attention, as neglecting them can severely impact the safety, stability, and combat effectiveness of rescuers.
Currently, although there are multiple approaches for treating depression, each has its own limitations. Literature indicates that the existing monoamine antidepressants have shortcomings such as slow onset, numerous adverse reactions, and the need for long-term medication. Additionally, new rapid-acting antidepressants may pose risks of drug addiction and neurotoxicity[8]. Acupuncture and acupoint stimulation primarily focus on treating primary depressive disorders, yet lack robust evidence regarding their effectiveness[9]. Other therapies such as psychological interventions often have slow efficacy and poor compliance. Consequently, alternative treatment methods for depression are urgently needed. Compared with other therapies, nutritional interventions offer advantages such as safety, convenience, and patient acceptance. It also reduces the adverse effects associated with pharmacological treatments. Therefore, nutritional intervention can be considered as a supplementary approach to antidepressant therapy. However, few clinical trials have investigated nutritional interventions for depression till date.
Depression is caused by long-term worry, fatigue, anger, panic, and other extreme emotions, resulting in qi and blood loss, zang-fu dysfunction, and disease, often mixed with excess and deficiency syndromes. Excess syndromes are mainly liver depression, fire excess, qi stagnation, blood stasis, and food stagnation, while deficiency syndromes are mainly qi and blood deficiency. Treatment is mostly used to tonify the heart, regulate the spirit, soothe the liver, strengthen the spleen, regulate qi, and eliminate phlegm[10]. This study employed a compound edible paste, with red rose, Seville orange flower, and sea buckthorn as the main components, for depression intervention, drawing from traditional Chinese medical texts such as Chinese Medicine Chi, ShenNong’s herbal classic, and the Compendium of Materia Medica. According to these texts, double-petaled red rose regulates qi and relieves depression and despair; Seville orange flower soothes the liver, regulates qi, and lowers lipids; red yeast rice invigorates blood circulation, relieves stasis, and strengthens the spleen; peach kernel breaks blood stasis, moistens dryness, and lubricates the intestines; Cordyceps nourishes the lungs and kidneys, lowers blood pressure, and calms the spirit; Angelica dispels wind, dries dampness, moistens the intestines, and facilitates bowel movements; sea buckthorn activates blood circulation, relieves stasis, transforms phlegm, and expands the chest; hawthorn promotes qi circulation, relieves food stagnation, and dissolves stasis; and licorice moderates urgency, detoxifies, and harmonizes the other herbs; all these herbs show great promise for future applications.
Literature also supports these findings: Liang et al.’s[11] research isolated and detected a high proportion of flavonoids from roses, which are highly similar in structure to antidepressant compounds. Yan et al.[12] discovered that roses possess pharmacological actions such as antioxidation, anti-tumor, anti-inflammation, anti-atherosclerosis, immunoregulation, liver protection, cardiovascular protection, and health functions like lowering blood sugar, lipids, regulating insulin, and improving skin against aging. Zhang et al.[13] conducted studies on the mechanisms of Schisandra and rose in repairing intestinal barriers and improving inflammation levels in depressed mice, confirming that their antidepressant effects are potentially linked to repairing intestinal mucosal barriers, reducing the release of intestinal inflammatory mediators, and increasing the levels of 5-HT and BDNF in the hippocampus. Costa et al.[14] found that Seville orange flower essential oil had antidepressant effects on mice. Yang et al.[15] used the “Five-Flower Soup” (rose, Seville orange flower, Albizia flower, Campsis flower, and chrysanthemum) for its liver-soothing and depression-relieving effects to treat various diseases. Li et al.[16-17] discovered that cordycepin has rapid and significant antidepressant effects on mice, and it exerts its effects faster than current clinical antidepressants, with stable and sustained effects without side effects. Sun et al.[18] found that Cordyceps polysaccharides can lower the levels of acetylcholine and glutamate salts and increase the level of 5-hydroxytryptamine in the brain, thereby producing sedative and hypnotic effects in mice. The flavonoid-rich part of sea buckthorn (SBF) stimulates neuronal cell differentiation and simulates the function of neurotrophic proteins in cultured neurons. In a mild stress-induced mouse model, ingestion of SBF reversed depressive behaviors in mice[19]. With the development and promotion of traditional Chinese medicine, an increasing amount of research has shown that traditional Chinese medicine compounds or traditional Chinese medicine extracts can affect gastrointestinal nerve function by regulating the intestinal flora and improving nervous system diseases. For example, the Xingpi Jieyu formula can maintain normal tryptophan metabolism and exert an antidepressant effect[20]. In recent years, research on the antidepressant effects, structure-activity relationships, and related mechanisms of flavonoids has increased dramatically. Many studies have reported that the total flavonoids extracted from Gancao (Gly-cyrrhizae Radix et Rhizoma), Suanzaoren (Ziziphispino-sae Semen), Xuancao (Hemerocallis Fulva), Yuxingcao (Houttuyniae Herba), and other functional foods, medicines, and homologous food products have significant antidepressant activity[21].
This study demonstrates that after six weeks of consuming a compound edible paste, the median SDS score among rescuers decreased from 63 to 35. This suggests that nutritional intervention might be effective in the early stages of depression among those who initially screen positive. This finding aligns with Zhang’s research[22], in which the intervention group of patients with depression treated with modified Xiao Yao pills for 12 weeks saw their SDS scores drop from 72 to 51. Similarly, Liu’s[23] study on patients with coronary heart disease accompanied by depression treated with the ShuGanJie Yu Decoction showed a reduction in SDS scores from 45.82 to 27.17. These results not only align with the effectiveness of these two traditional Chinese medicine treatments but also indicate a greater decrease in SDS scores after treatment with the paste, suggesting its potential in treating depression. This study provides robust clinical evidence and technical support for the use of nutritional formulas to alleviate depression.
This study has extensive and far-reaching military value, social benefits, clinical application value, and scientific research value. For the military, this study could provide powerful tools for maintaining the mental health of rescuers in complex and stressful environments such as comprehensive drills and practical confrontations. The study can also help reduce depression scale scores in rescuers, ensure smooth daily training and task execution, and enhance the cohesion and combat effectiveness of the troops. Regarding social benefits, early detection of depression and interventions to treat it can reduce the burden on families and society and rebuild confidence and positive attitudes in rescruers. Regarding clinical application, the nutritional intervention was easy to perform and could provide patients with safer treatment plans with better compliance. Regarding scientific research, it could provide researchers with new ideas and broaden their directions for depression treatment. In the past two years, our group has carried out research to provide evidence support[24-26].
Regarding contributions, first, this study selected rescuers with SDS-positive initial screening for early intervention, which can help identify and intervene in the depression status of rescuers earlier. Second, it takes the lead in applying nutritional formulas to intervene in the depression status of rescuers and explore their intervention effect for the first time.
The study has some limitations. First, no long-term follow-up was conducted to verify the long-term effects of the intervention measures. Second, this study is a single-center study, and our research will further validate it using subsequent multicenter data. In the future, our research team will conduct more research on various intervention methods to provide more evidence regarding the efficacy of early nutritional interventions to treat depression in rescuers.
-
Our study shows that a nutritional intervention effectively reduced the depression scores of rescuers, and that early nutritional intervention is recommended for rescuers who initially screen positive for depression.
-
All respondents gave informed consent (Clinical research registration no. ChiCTR19000023441; hospital ethics no.S2019-108-01).
doi: 10.3967/bes2024.096
Efficacy of a Nutritional Cream Intervention to Treat Depression in Rescuers: A Randomized Controlled Trial
-
Abstract:
Objective To explore the effectiveness of a nutritional intervention in rescuers who screened positive for depression. Methods A randomized controlled trial design was employed. From June to August, 2022, 4,460 rescuers were screened using the Self-Rating Depression Scale (SDS), and 1,615 positive cases were identified. Thirty-one volunteers were recruited and randomly divided into a nutritional intervention group and a control group. The intervention group received health education and nutritional intervention (a compound paste therapy primarily composed of red roses and Seville orange flowers), while the control group received psychological education. SDS scores were assessed before and after the intervention. Results There was a statistically significant decline in SDS scores in the nutritional intervention group after the intervention (P < 0.05). Furthermore, the SDS scores of the intervention group were significantly lower than those of the control group, both before and after the intervention (P < 0.05). No severe adverse reactions were observed during safety evaluation. Conclusion The nutritional intervention effectively reduced the depression scores in rescuers. Early nutritional intervention is recommended for rescuers who initially screen positive for depression. -
Key words:
- Nutritional intervention /
- Rescuers /
- Depression /
- Randomized controlled trial
The authors declare that they have no conflict of interest.
&These authors contributed equally to this work.
注释:1) AUTHOR CONTRIBUTIONS: 2) CONFLICT OF INTEREST: -
Table 1. Baseline characteristics of study subjects
Variable Grouping N Intervention group (n, %) Control group (n, %) t/z/χ2 P Age (years) 22 (21, 26) 22 (21, 25.25) −0.247 0.805 Gender − 0.142 Male 29 19 10 Female 2 0 2 Educational level 1.106 0.293 Collage and above 17 9 8 High school or below 14 10 4 Marital status 0.000 1.000 Single 26 16 10 Married 5 3 2 Monthly family income (Yuan) − 0.660 2,999 and below 10 6 4 3,000–7,999 13 7 6 8,000 and above 8 6 2 SDS 63 (63, 63) 63 (60, 65.25) −0.316 0.752 Note. There were no statistically significant differences between the intervention and control groups in terms of age, gender, educational level, marital status, and monthly family income (P > 0.05) at baseline. Additionally, there was no significant difference in the SDS scores between the intervention and control groups before the intervention (P > 0.05). SDS, Self-Rating Depression Scale. Table 2. Results of the generalized linear mixed model for SDS scores post-Intervention in both groups
Group N SDS scores, median (IQR) Per-intervention Post-1st intervention Post-intervention Treatment group 19 63 (63, 63) 33 (28, 44) 28 (25, 33) Control group 12 63 (60, 65) 41.5 (29, 51) 36 (28, 46) β −1.665 4.129 8.383 P 0.201 0.302 0.024 Note. The model includes age, gender, marital status, level of education, average monthly income per household member, time, group, and the interaction between time and group. SDS, Self-Rating Depression Scale; IQR, interquartile range. -
[1] Zhao YQ, Teng J, Yang HJ. Analysis on medication regularity of modern traditional Chinese medicines in treating melancholia based on data mining technology. China J Chin Mater Med, 2015; 40, 2042−6. (In Chinese [2] Dobrek L, Głowacka K. Depression and its phytopharmacotherapy-a narrative review. Int J Mol Sci, 2023; 24, 4772. doi: 10.3390/ijms24054772 [3] Feng DD, Tang T, Lin XP, et al. Nine traditional Chinese herbal formulas for the treatment of depression: an ethnopharmacology, phytochemistry, and pharmacology review. Neuropsychiatr Dis Treat, 2016; 12, 2387−402. doi: 10.2147/NDT.S114560 [4] Liu L, Liu CH, Wang YC, et al. Herbal medicine for anxiety, depression and insomnia. Curr Neuropharmacol, 2015; 13, 481−93. doi: 10.2174/1570159X1304150831122734 [5] Li YS, Chen XY, Zhu DR. Progress of multi-parameter artificial intelligence in evaluating depression. Armed Police Med, 2023; 34, 730−4. [6] Feng ZZ. Military psychology. Military Medical Science Press. 2009, 130-42. (In Chinese [7] Li J, Li BR, Li Q, et al. Advances in research of depression in different groups of Chinese servicemen. Chin J Med Libr Inf Sci, 2010; 19, 14−6. (In Chinese [8] "Guidelines for Clinical Application of Proprietary Chinese Medicines in Treating Dominant Diseases" Standardization Project Group. Guidelines for clinical application of Chinese patent medicine in the treatment of rheumatoid arthritis (2022). Chin J Integr Tradit West Med, 2023; 43, 261−73. (In Chinese [9] Yang NN, Lin LL, Li YJ, et al. Potential mechanisms and clinical effectiveness of acupuncture in depression. Curr Neuropharmacol, 2022; 20, 738−50. doi: 10.2174/1570159X19666210609162809 [10] Qi XQ, Qi XM, Liu TM, et al. Exploration into pathogenesis of depression based on the grease theory in inner canon of yellow emperor. Jilin J Chin Med, 2023; 43, 389−92. (In Chinese [11] Liang MM, Shao XX, Chen C, et al. The basis and mechanism of Rosae Rugosae Flos antidepressants based on network pharmacology. Shandong Sci, 2022; 35, 38−48. (In Chinese [12] Yan BF, Liu J, Zhang JZ, et al. Prediction of potential pharmacological and health benefits of Rosaerugosaeflos based on network pharmacology. Chin J Bioprocess Eng, 2022; 20, 65−73. [13] Zhang T, Ren Y, Li L, et al. Study on the function mechanism of Schisandra chinensis and rose based on repairing intestinal barrier and improving inflammation level in mice with depression. J Shaanxi Univ Sci Technol, 2023; 41, 62−70. (In Chinese [14] Costa CARA, Cury TC, Cassettari BO, et al. Citrus aurantium L. essential oil exhibits anxiolytic-like activity mediated by 5-HT1A-receptors and reduces cholesterol after repeated oral treatment. BMC Complement Altern Med, 2013; 13, 42. doi: 10.1186/1472-6882-13-42 [15] Yang ZR, Dou YL, Feng WJ. Feng Wu Jin's experience in applying Jie Yu Wu Hua decoction and examples of cases. World Latest Med Inf, 2023; 23, 241−4. [16] Li B. Cordycepin produces a rapid and robust antidepressant effect via enhancing prefrontal AMPA receptor signaling pathway. Yunnan University. 2016. (In Chinese [17] Li B, Luo SL, Hou YY, et al. Cordycepin produces an antidepressant effect via activating synaptic plasticity. Mod Tradit Chin Med Mater Med World Sci Technol, 2017; 19, 1141−50. (In Chinese [18] Sun JB, An LP, Zhang ZX, et al. Extraction methods and sedative-hypnotic effects of polysaccharide and total flavonoids of Cordyceps militaris. Biotechnol Biotechnol Equip, 2018; 32, 498−505. doi: 10.1080/13102818.2017.1336942 [19] Xia CX, Gao AX, Zhu Y, et al. Flavonoids from Seabuckthorn (Hippophae rhamnoides L.) restore CUMS-induced depressive disorder and regulate the gut microbiota in mice. Food Funct, 2023; 14, 7426−38. doi: 10.1039/D3FO01332D [20] Qi WH, Jiang C, Gao YG. Research progress on pathogenesis of depression and prevention and treatment of traditional Chinese medicine. Chin J Gerontol, 2023; 43, 3302−7. (In Chinese [21] Ye T, Xu MT, Fang JP, et al. Antidepressant-like active ingredients and their related mechanisms of functional foods or medicine and food homologous products. Digital Chin Med, 2023; 6, 9−27. (In Chinese doi: 10.1016/j.dcmed.2023.02.001 [22] Zhang ZS. Discussion on the clinical treatment of depression by traditional Chinese medicine. Healthful Friend, 2021; 72. [23] Liu Y. Effect of ShuGanJie Yu decoction on depression score and anxiety score in treating coronary heart disease complicated with depression. China Health Care Nutr, 2021; 31, 244. (In Chinese [24] Sai XY, Gao F, Zhang WY, et al. Combined effect of smoking and obesity on coronary heart disease mortality in male veterans: a 30-year cohort study. Biomed Environ Sci, 2021; 34, 184−91. [25] Li CY, Song YJ, Zhao L, et al. Insomnia burden among informal caregivers of hospitalized lung cancer patients and its influencing factors. Biomed Environ Sci, 2023; 36, 715−24. [26] Sai XY, Xing X, Luan HY, et al. Incorporating hybrid networks into urban transportation infrastructures for improved COVID-19 transmission forecasting. Mod Phys Lett B, 2023; 37, 2350118. -




 下载:
下载:



 Quick Links
Quick Links