-
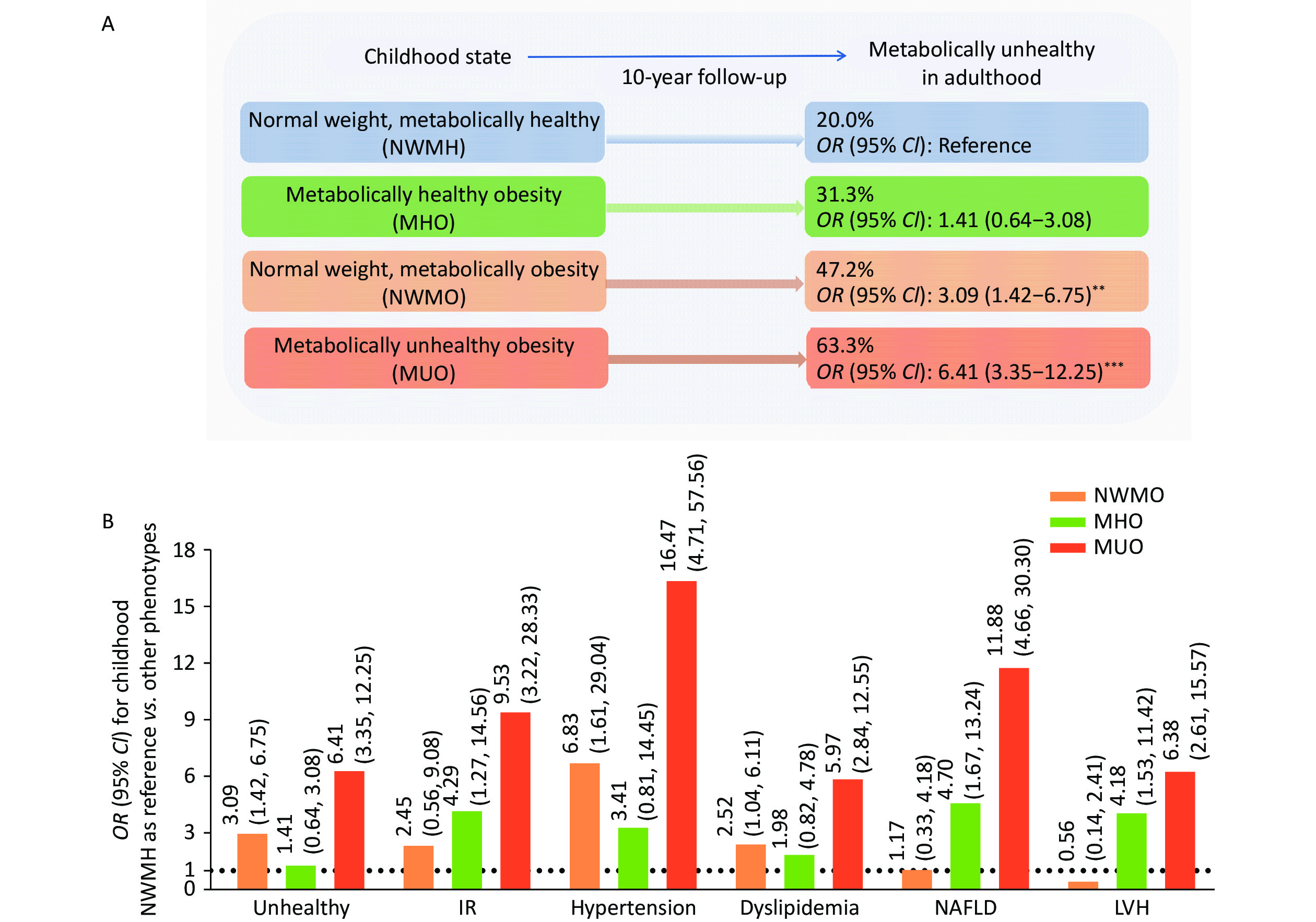
Childhood obesity has become a global epidemic. It has been shown that nearly 55% of children with obesity will remain with obesity during adolescence and about 80% of adolescents with obesity will still suffer from this condition in the adulthood[1]. This increase leads to a myriad of health risks, such as type 2 diabetes (T2D), cardiovascular diseases, and various metabolic disorders[1]. Although the general importance of continuously tracking these children with obesity is undisputed, the metabolic challenges associated with obesity are not only limited to those with excess weight, nor are all obese youths equally affected. The Beijing Children and Adolescents Metabolic Syndrome Study (BCAMS) has previously identified distinct metabolic phenotypes in children, of which nearly one-third are free of cardiometabolic risk factors, such as hyperglycemia, high blood pressure, dyslipidemia, or insulin resistance, namely metabolically healthy obesity (MHO), while others exhibit metabolically unhealthy obesity (MUO). While most children with normal weight are metabolically healthy (NWMH), nearly one-third of children with metabolic abnormalities are of normal weight, that is, normal weight metabolically obese (NWMO)[2-5]. The ten-year follow-up data of the BCAMS showed that the proportion of MHO, NWMO, and MUO children who developed or maintained metabolic abnormalities in adulthood was 31.3%, 47.2%, and 63.3%, respectively (Figure 1A). MHO children have a lower cardiovascular risk in adulthood than MUO children, although it is still relatively higher than that in children with NWMH. In contrast, NWMO children may have a higher cardiovascular metabolic risk than MHO children (Figure 1B). Mechanistically, the BCAMS study found that an imbalanced adipokine profile could serve as a novel biomarker for early identification and precise phenotyping of different metabolic types of obesity[4]. The BCAMS study also provided the first evidence of gene-diet (soft drink consumption) and gene-environment (with walking to school) interactions predisposing to MHO[3,6]. These results underscore the necessity for tailored interventions targeting each metabolic subtype of childhood and adolescent obesity.
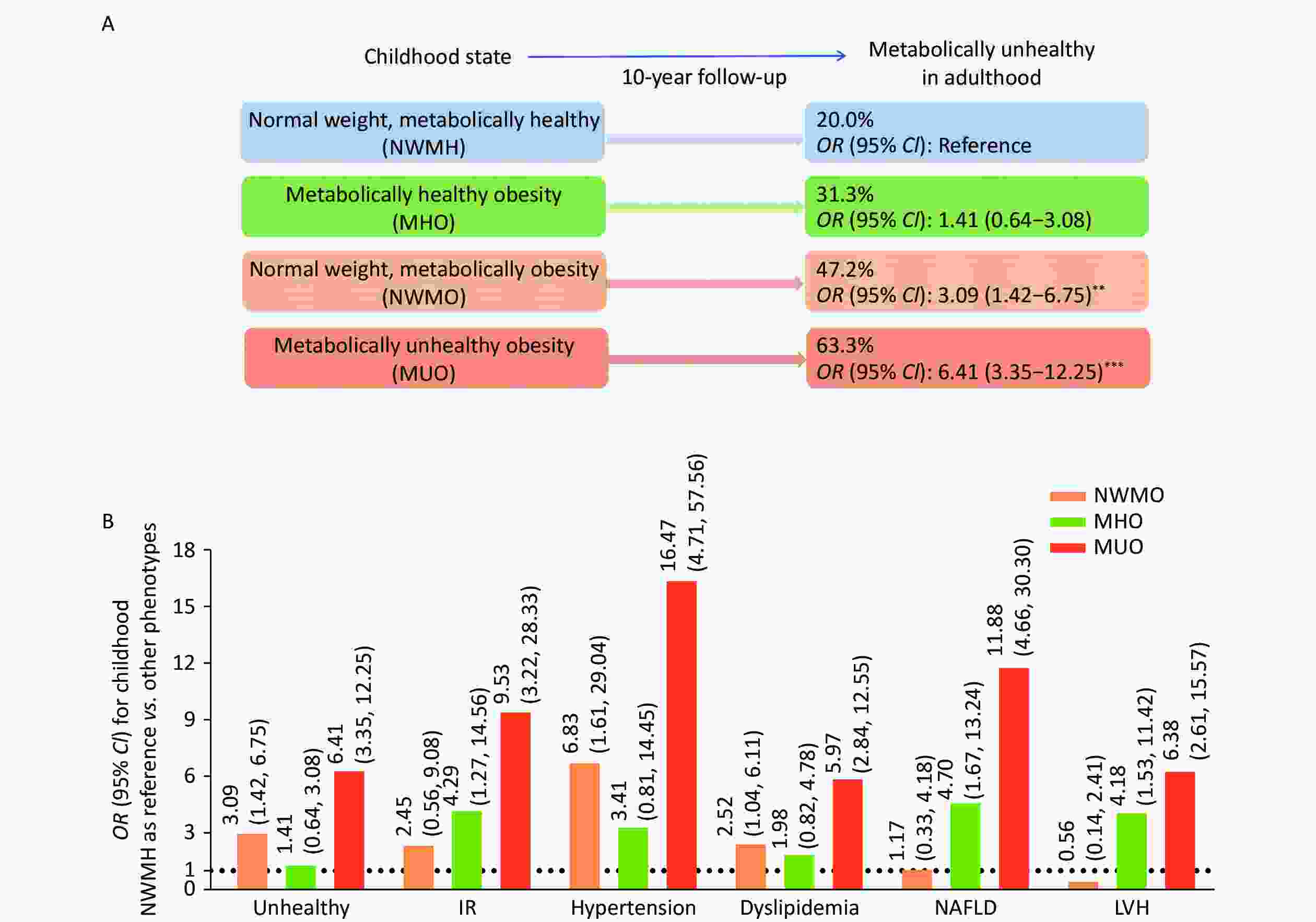
Figure 1. Cardiovascular risk at follow-up. Unhealthy: Defined by the presence of classical metabolic syndrome components according to the harmonized definition. IR: Defined by homeostasis model assessment of insulin resistance (HOMA-IR) > 3.0. Hypertension was defined as participants with SBP/DBP ≥ 95th percentile for age and sex (< 18 years old) and ≥ 140/90 mmHg for subjects over 18 years. Dyslipidemia: Defined as the presence of any of the following lipid abnormalities: total cholesterol (TC) ≥ 200 mg/dL (≥ 5.18 mmol/L); triglycerides (TG): ≥ 150 mg/dL (≥ 1.7 mmol/L); low-density lipoprotein cholesterol (LDL-C): ≥ 130 mg/dL (≥ 3.37 mmol/L); high-density lipoprotein cholesterol (HDL-C): < 40 mg/dL (< 1.04 mmol/L). NAFLD: diagnosed by ultrasonography. LVH: Defined by left ventricular mass index above the sex-specific 90th percentile. IR, Insulin Resistant; NAFLD, nonalcoholic fatty liver disease; LVH, left ventricular hypertrophy; MHO, Metabolically Healthy Obesity; MUO, Metabolically Unhealthy Obesity; NWMO, Normal Weight Metabolically Obesity; NWMH, Normal Weight Metabolically Healthy. **: P < 0.01, ***: P < 0.001.
Existing research has highlighted the heterogeneity between childhood and adolescent obesity. A study involving 1,180 children and adolescents, the Young Finns Study, found that individuals in the NWMO group had a higher rate of BMI increase in adulthood than those in the NWMH group[7]. An analysis by the International Consortium for Vascular Structure Evaluation in Children, based on 3,497 children and adolescents aged 6–17 years from five countries, indicated that carotid intima-media thickness was higher in children with MHO and NWMO than in those with NWMH[8]. Another cohort of more than 2,000 adolescents found that MUO is associated with an increased risk of T2D and metabolic syndrome (MetS) in early adulthood for both genders, while both NWMO and MHO phenotypes are associated with an increased risk of adult MetS in males[9]. These findings support our BCAMS conclusions and highlight the importance of classifying childhood and adolescent obesity. These differences require a deeper understanding of unique intervention strategies to manage and treat obesity in children and adolescents.
Informed on domestic research findings[2-5] and global epidemic trends, along with international criteria[6,10], we propose a new classification system for childhood and adolescent obesity, the BCAMS classification, encompassing four distinct categories (Table 1).
Table 1. The definition of the BCAMS classification
BCAMS classification Definition MHO Meet all of the following criteria: SBP and DBP < 90th percentile, TG < 150 mg/dL (1.70 mmol/L), HDL-c > 40 mg/dL (1.03 mmol/L), and FBG < 100 mg/dL (5.6 mmol/L) in children of corresponding age and sex. MUO At least one metabolic abnormality: (1) elevated blood pressure (SBP and/or DBP ≥ 90th percentile for age and sex; (2) elevated TG levels [TG ≥ 150 mg/dL (1.70 mmol/L)]; (3) reduced serum HDL-C [defined as ≤ 40 mg/dL (1.03 mmol/L)]; or (4) elevated FBG [defined as ≥ 100 mg/dL (5.6 mmol/L)]. NWMO Any classic pediatric metabolic syndrome component in normal-weight children: (1) elevated blood pressure (SBP and/or DBP ≥ 90th percentile for age and sex; (2) elevated TG levels [TG ≥ 150 mg/dL (1.70 mmol/L)]; (3) reduced serum HDL-C [defined as ≤ 40 mg/dL (1.03 mmol/L)]; or (4) elevated FBG [defined as ≥ 100 mg/dL (5.6 mmol/L)]. NWMH Normal weight and free of any classific metabolic syndrome features. Note. MHO, Metabolically Healthy Obesity; MUO, Metabolically Unhealthy Obesity; NWMO, Normal Weight Metabolically Obesity; NWMH, Normal Weight Metabolically Healthy. The Introduction of the BCAMS classification is crucial for accurately recognizing and distinguishing between different subtypes of childhood and adolescent obesity, enabling effective monitoring and targeted intervention strategies. Future research should focus on developing and implementing personalized interventions that hold promise for improving long-term health outcomes in children and addressing the epidemic of childhood and adolescent obesity more effectively.
doi: 10.3967/bes2025.006
A New Classification System for Childhood and Adolescent Obesity: Definition of the BCAMS Classification
-
The authors declare no conflicts of interest.
注释:1) Competing Interests: -
Figure 1. Cardiovascular risk at follow-up. Unhealthy: Defined by the presence of classical metabolic syndrome components according to the harmonized definition. IR: Defined by homeostasis model assessment of insulin resistance (HOMA-IR) > 3.0. Hypertension was defined as participants with SBP/DBP ≥ 95th percentile for age and sex (< 18 years old) and ≥ 140/90 mmHg for subjects over 18 years. Dyslipidemia: Defined as the presence of any of the following lipid abnormalities: total cholesterol (TC) ≥ 200 mg/dL (≥ 5.18 mmol/L); triglycerides (TG): ≥ 150 mg/dL (≥ 1.7 mmol/L); low-density lipoprotein cholesterol (LDL-C): ≥ 130 mg/dL (≥ 3.37 mmol/L); high-density lipoprotein cholesterol (HDL-C): < 40 mg/dL (< 1.04 mmol/L). NAFLD: diagnosed by ultrasonography. LVH: Defined by left ventricular mass index above the sex-specific 90th percentile. IR, Insulin Resistant; NAFLD, nonalcoholic fatty liver disease; LVH, left ventricular hypertrophy; MHO, Metabolically Healthy Obesity; MUO, Metabolically Unhealthy Obesity; NWMO, Normal Weight Metabolically Obesity; NWMH, Normal Weight Metabolically Healthy. **: P < 0.01, ***: P < 0.001.
Table 1. The definition of the BCAMS classification
BCAMS classification Definition MHO Meet all of the following criteria: SBP and DBP < 90th percentile, TG < 150 mg/dL (1.70 mmol/L), HDL-c > 40 mg/dL (1.03 mmol/L), and FBG < 100 mg/dL (5.6 mmol/L) in children of corresponding age and sex. MUO At least one metabolic abnormality: (1) elevated blood pressure (SBP and/or DBP ≥ 90th percentile for age and sex; (2) elevated TG levels [TG ≥ 150 mg/dL (1.70 mmol/L)]; (3) reduced serum HDL-C [defined as ≤ 40 mg/dL (1.03 mmol/L)]; or (4) elevated FBG [defined as ≥ 100 mg/dL (5.6 mmol/L)]. NWMO Any classic pediatric metabolic syndrome component in normal-weight children: (1) elevated blood pressure (SBP and/or DBP ≥ 90th percentile for age and sex; (2) elevated TG levels [TG ≥ 150 mg/dL (1.70 mmol/L)]; (3) reduced serum HDL-C [defined as ≤ 40 mg/dL (1.03 mmol/L)]; or (4) elevated FBG [defined as ≥ 100 mg/dL (5.6 mmol/L)]. NWMH Normal weight and free of any classific metabolic syndrome features. Note. MHO, Metabolically Healthy Obesity; MUO, Metabolically Unhealthy Obesity; NWMO, Normal Weight Metabolically Obesity; NWMH, Normal Weight Metabolically Healthy. -
[1] Olsen NJ, Østergaard JN, Bjerregaard LG, et al. A literature review of evidence for primary prevention of overweight and obesity in healthy weight children and adolescents: a report produced by a working group of the Danish Council on Health and Disease Prevention. Obes Rev, 2024; 25, e13641. doi: 10.1111/obr.13641 [2] Li M, Yin J, Xu L, Gao S, et al. A large cohort study of children Li M, Yin J, Xu L, Gao S, Li C. A large cohort study of Chinese children suggests adipokine profile as new biomarkers to define metabolically healthy obesity (Abstract). Diabetes, 2014; 63, A316. doi: 10.1038/jhh.2014.124 [3] Li LJ, Yin JH, Cheng H, et al. Identification of genetic and environmental factors predicting metabolically healthy obesity in children: data from the BCAMS study. J Clin Endocrinol Metab, 2016; 101, 1816−25. doi: 10.1210/jc.2015-3760 [4] Fu JL, Li Y, Esangbedo IC, et al. Circulating osteonectin and adipokine profiles in relation to metabolically healthy obesity in Chinese children: findings from BCAMS. J Am Heart Assoc, 2018; 7, e009169. doi: 10.1161/JAHA.118.009169 [5] Li G, Li Y, Han LW, et al. Interaction between early environment and genetic predisposition instigates the metabolically obese, normal weight phenotype in children: findings from the BCAMS study. Eur J Endocrinol, 2020; 182, 393−403. doi: 10.1530/EJE-19-0755 [6] Phillips CM. Metabolically healthy obesity across the life course: epidemiology, determinants, and implications. Ann N Y Acad Sci, 2017; 1391, 85−100. doi: 10.1111/nyas.13230 [7] Viitasalo A, Pahkala K, Lehtimäki T, et al. Changes in BMI and physical activity from youth to adulthood distinguish normal-weight, metabolically obese adults from those who remain healthy. Front Endocrinol (Lausanne), 2022; 13, 923327. doi: 10.3389/fendo.2022.923327 [8] Zhao M, López-Bermejo A, Caserta CA, et al. Metabolically healthy obesity and high carotid intima-media thickness in children and adolescents: international childhood vascular structure evaluation consortium. Diabetes Care, 2019; 42, 119−25. doi: 10.2337/dc18-1536 [9] Yaghoubpour K, Tasdighi E, Abdi H, et al. Association of obesity phenotypes in adolescents and incidence of early adulthood type 2 diabetes mellitus: Tehran lipid and glucose study. Pediatr Diabetes, 2021; 22, 937−45. doi: 10.1111/pedi.13243 [10] Damanhoury S, Newton AS, Rashid M, et al. Defining metabolically healthy obesity in children: a scoping review. Obes Rev, 2018; 19, 1476−91. doi: 10.1111/obr.12721 -




 下载:
下载:



 Quick Links
Quick Links