-
Irrational drug use and prescription safety are pressing global concerns. The World Health Organization estimated that over half of all prescriptions worldwide contain errors, leading to substantial harm[1,2]. In China, prescription errors occur at a rate of 32%, and improper medication use is reported in over 70% of households[3,4]. Vulnerable populations, including children (16.7%) and older adults (30.4%), are particularly affected[5]. These challenges underscore the urgent need for strategies to improve medication safety. Prescription reviews are vital for addressing irrational medication use; however, a global shortage of pharmacists has challenged their implementation. In China, the pharmacist-to-population ratio is critically low, especially at the grassroots level, with only 1.2 pharmacists per 10,000 people. Moreover, fewer than 30% of primary healthcare institutions (PHIs) meet the required staffing criteria. Advances in artificial intelligence (AI) have transformed healthcare, improving diagnostics and decision-making. AI applications, such as imaging diagnostics and prescription review systems, exhibit the potential to enhance the quality and efficiency of medical services. AI-assisted prescription review systems (AIAPRS) have shown promise for improving prescription safety, with successful implementation in China. For instance, an AIAPRS in Beijing reviewed over 300,000 prescriptions in one year, achieving high accuracy rates and significantly reducing the number of irrational prescriptions. Despite its potential, the cost-effectiveness of AIAPRS in real-world settings, particularly in underdeveloped regions, remains underexplored. This study evaluates the effectiveness and economic benefits of an AIAPRS in a Chinese county.
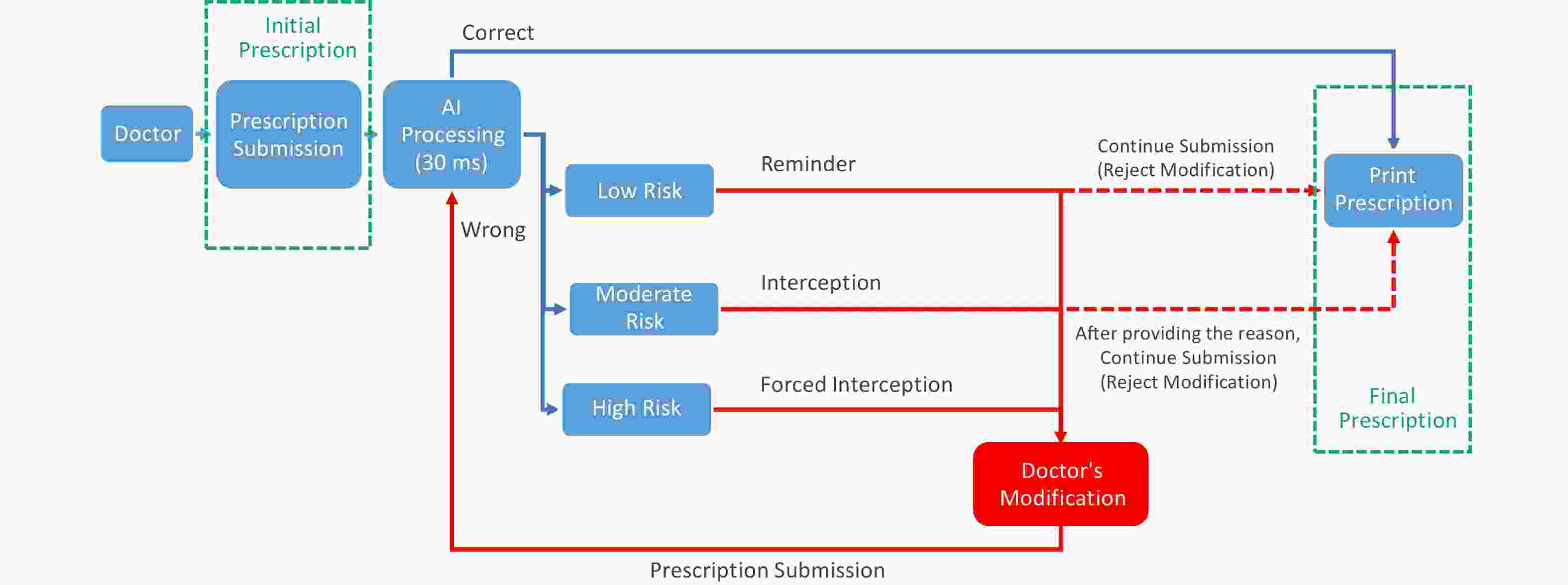
The County in Anhui Province, an underdeveloped region, launched a project in March 2023 to improve medication practices in PHIs. Before AIAPRS implementation, no prescription review system existed. Physicians’ prescriptions are now reviewed by AIAPRS, with errors categorized into “low-risk” “moderate-risk” and “high-risk” levels (Supplementary Figure S1). Data from 318 PHIs (21 township health centers and 297 village clinics) were collected from March to June 2023, covering prescription volume, irrational prescription rates, and expenditures. Key metrics included modification rates and risk-based categorization of prescriptions.
Activity-based costing was used to estimate AIAPRS implementation costs at 21 township health centers and 297 village clinics. The analysis included resource allocation per prescription review, but excluded installation and facility-related costs. A one-factor sensitivity analysis identified key cost drivers, such as maintenance expenses and application scale. March 2023 was used as the baseline to compare irrational prescription rates, risk levels, and physician modification rates over four months. Monthly changes in prescription volume and expenditure were also analyzed to assess savings from AI intervention. Cost-effectiveness was evaluated by comparing AI intervention costs with savings in prescription expenses and reductions in irrational prescription rates. The input-output ratio was calculated monthly. Data were analyzed using SPSS 26.0, employing chi-squared or Fisher’s exact test for categorical data and Wilcoxon rank-sum test for ordinal data. A P-value < 0.05 was considered significant.
In the same month, the final submission of irrational prescriptions showed a significant decrease (P < 0.001), which is consistent with the effectiveness of the AI-assisted intervention. The most substantial reduction was observed in March 2023 (4.7%), whereas the least was observed in June 2023 (2.4%) (Supplementary Table S1). This trend across months indicates a gradual but consistent improvement in prescription quality. This aligns with the findings of similar studies conducted in hospitals in Israel and China, wherein physician modifications to irrational prescriptions were also significant[6-8]. The relatively lower reduction in June could suggest a stabilization effect over time, where the impact of the intervention becomes less pronounced as prescribing practices improve and doctors adjust to the AI’s feedback.
Additionally, across months, irrational prescriptions continued to show a decreasing trend (P < 0.001). Specifically, the irrational prescription rate decreased from 27.7% in March 2023 to 24.1% in June 2023, confirming the role of the AI intervention in mitigating irrational prescriptions. Following the AI intervention, the overall irrational prescription rate was reduced by 6.0% (Supplementary Table S1). This reduction over just four months, though modest, suggests that the AIAPRS has a meaningful impact on prescription practices, reducing the risks of medication errors and improving the overall safety profile.
A deeper analysis of the risk categories revealed statistically significant differences (P < 0.001), with high-risk prescriptions showing a dramatic decline from 13.6% to 1.5%, and medium-risk prescriptions falling from 22.3% to 16.4%. Interestingly, the proportion of low-risk prescriptions rose from 64.1% to 82.2% (Supplementary Table S1). These changes highlight a noteworthy shift in the nature of irrational prescriptions. The substantial reduction in high-risk prescriptions indicates the ability of AI to address critical safety concerns, particularly in preventing severe medication errors such as inappropriate antibiotic use. This is a positive outcome, suggesting that interactions between AI and experts can help reduce high-risk prescription practices. However, the increase in low-risk prescriptions suggests that physicians may have been more receptive to the AI’s alerts for higher-risk cases but less responsive to low-risk alerts, possibly owing to clinical experience or a belief in their own judgments over AI recommendations.
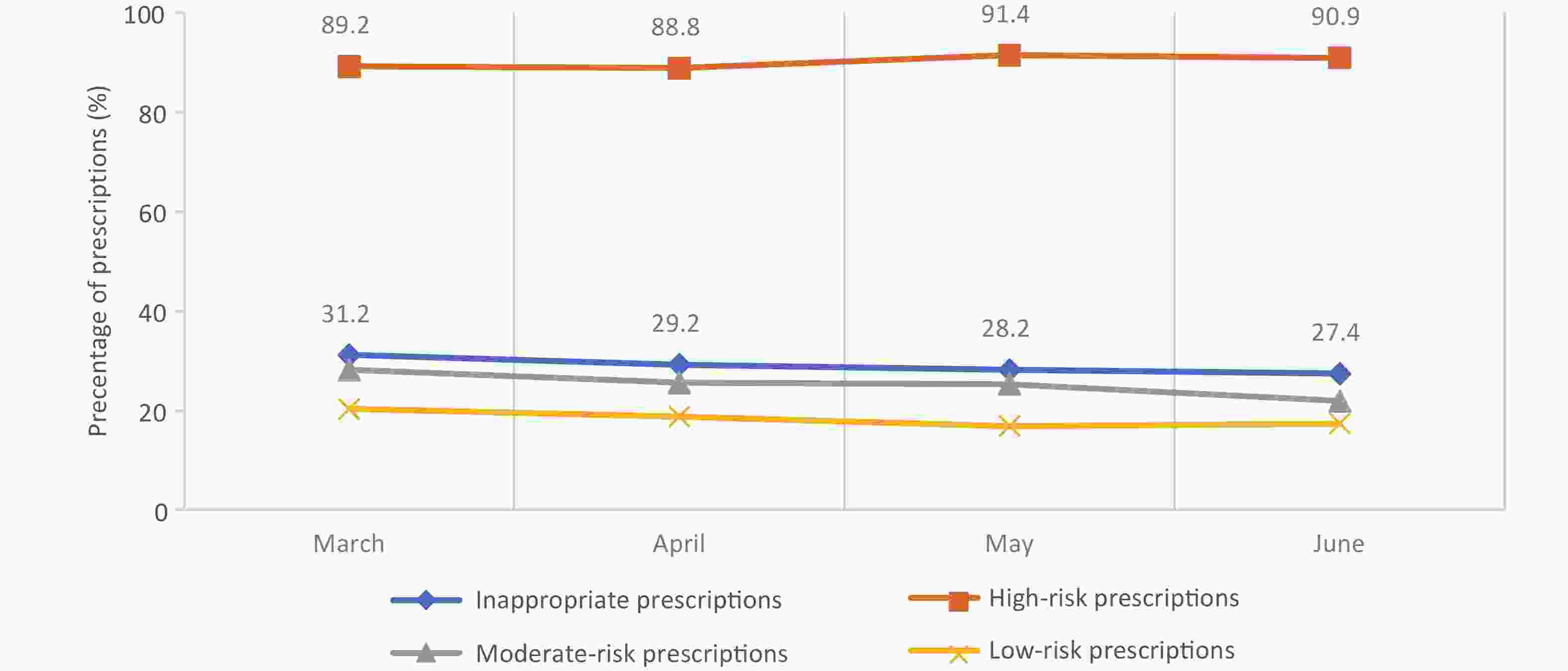
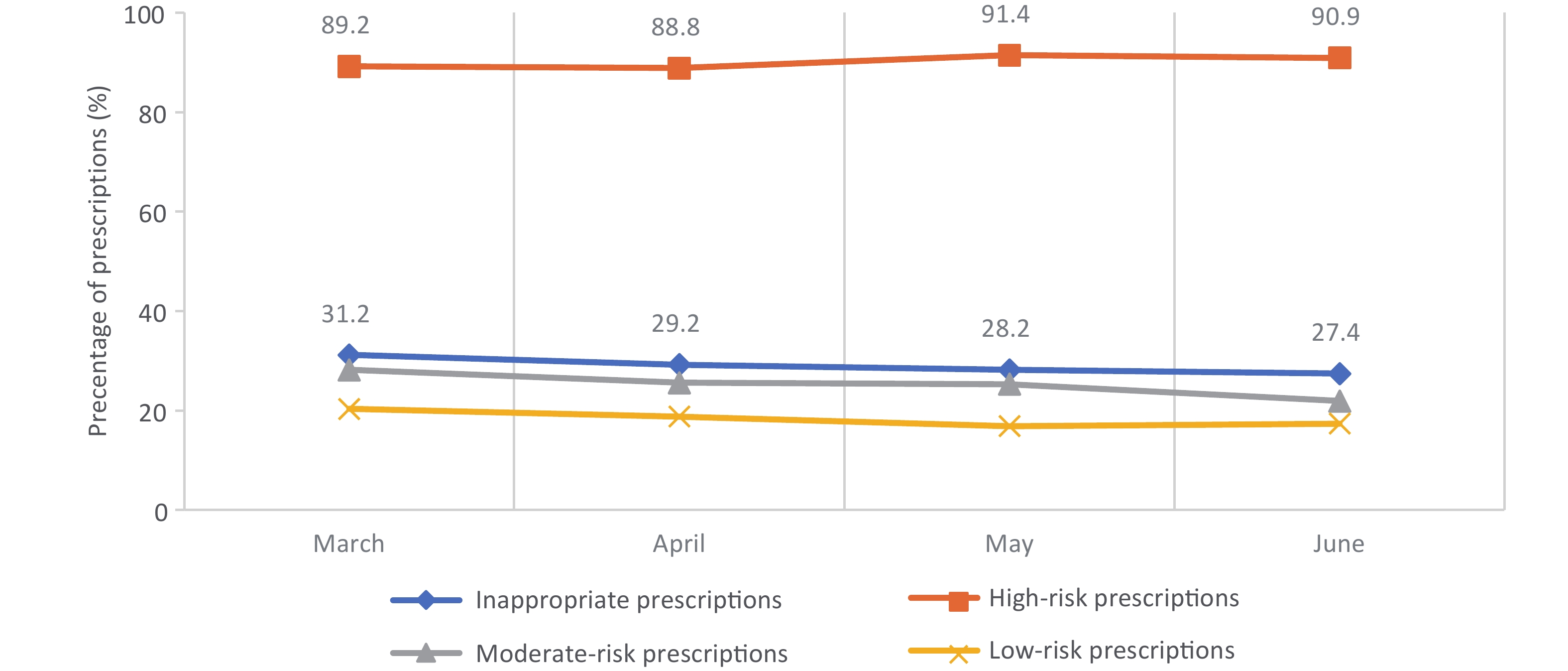
Furthermore, the modification rate of irrational prescriptions by physicians decreased by 3.8% over the four-month period. High-risk prescriptions maintained a modification rate of over 88.5%, indicating that physicians were more likely to act on the AIAPRS’s recommendations for critical errors, whereas medium- and low-risk prescriptions had lower modification rates, under 30% (Figure 1). This result indicates a consistent willingness of physicians to prioritize correcting high-risk issues, but less enthusiasm for adjusting medium- or low-risk prescriptions, possibly owing to perceived lower severity or less familiarity with the AI’s suggestions for these categories[7]. This aligns with findings in prior research indicating that AI interventions are more effective in addressing high-risk issues, but have a limited impact on lower-risk prescriptions[8].
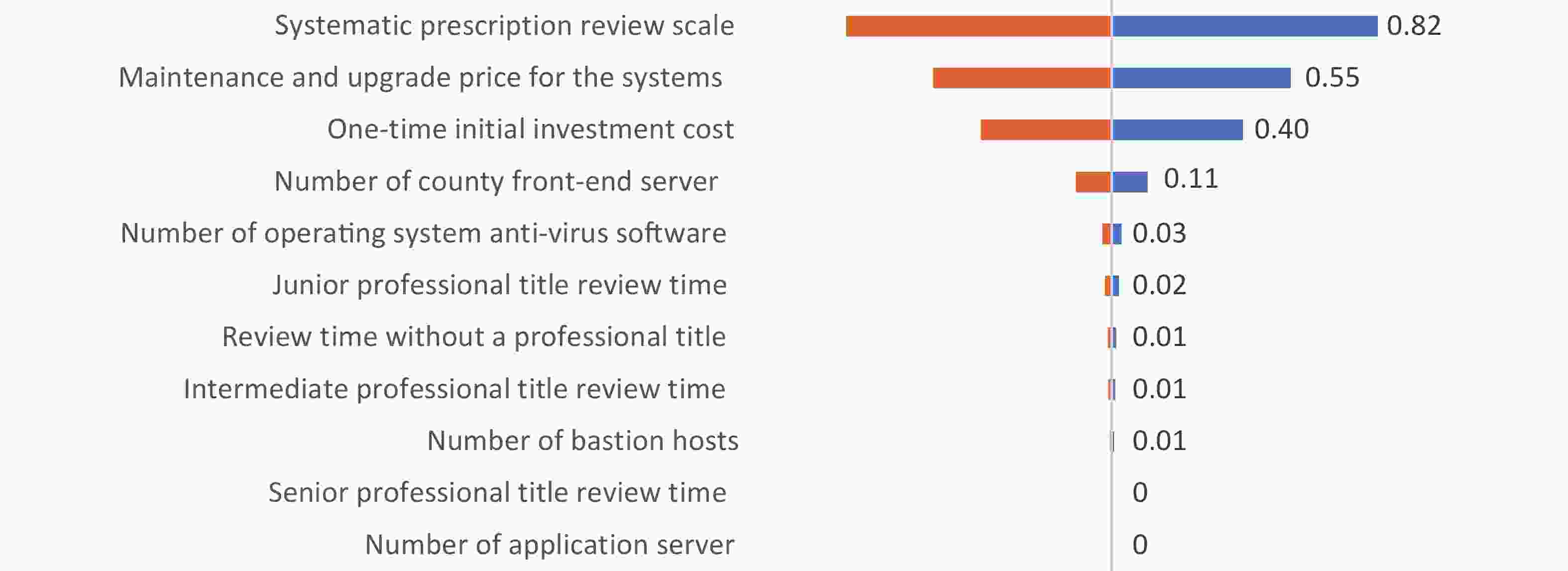
Cost estimation analyses showed that the cost of reviewing one prescription was 2.40 CNY, with fixed costs representing 95.2% of total costs. Maintenance costs were significant, amounting to 1.32 CNY per case, with depreciation costs adding another 0.97 CNY per case (Supplementary Table S2). Despite these costs, a one-factor sensitivity analysis demonstrated that prescription review costs are primarily affected by the scale of application, maintenance, and one-time investment costs, with sensitivity coefficients of 0.82, 0.55, and 0.40, respectively (Figure 2). This suggests that the broader implementation of the AIAPRS will lead to significant cost reductions, as unit costs decrease with scale. This observation is consistent with the economic principles of scale, wherein expanding the system’s use lowers the per-prescription cost, making it more cost-effective over time.
Regarding drug costs, the AIAPRS contributed to a monthly reduction in drug expenses, with an average decrease of 7.4, 3.4, 4.4, and 2.6 CNY for each month from March to June 2023. The average drug cost per prescription decreased from 34.8 CNY to 32.2 CNY over the study period, resulting in a net reduction of 5.2 CNY per prescription (Table 1). These findings are consistent with those of previous studies showing that AI can significantly reduce medication costs through better prescription practices and reducing unnecessary or inappropriate medications[9,10]. Moreover, the intervention led to total savings of 125,929.4 CNY over the four months, further demonstrating its cost-effectiveness.
Table 1. Cost-effectiveness analysis
Month Cost of Prescription Review
(CNY)Drug Savings by Prescription
(CNY)Total Saving
(CNY)#Change Rate of Irrational
Prescriptions (%)*March 204,829.2 514,804.1 309,974.9 4.7 April 163,375.7 198,813.8 35,438.1 3.3 May 181,985.2 279,699.9 97,714.7 3.6 June 160,862.5 221,452.6 60,590.1 2.4 Average 177,763.2 303,692.6 125,929.4 3.5 Note. #total saving = savings by prescription – Cost of Prescription Review; *Change in the proportion of irrational prescriptions before and after AI intervention in the same month. Our analysis highlights that the AIAPRS not only reduces irrational prescriptions, but also has a significant financial impact, making it a cost-effective solution for improving prescription quality at the grassroots level. The cost savings from drug expenses outweighed the technology’s operational costs, with a net savings of 2.1 CNY per prescription. These savings were largely driven by the AI’s role in optimizing medication choices and reducing unnecessary prescriptions, confirming its economic viability. Although savings decreased over time as the proportion of rational prescriptions increased, this trend did not undermine the cost-effectiveness of the AIAPRS. The opportunity costs remained stable, and the overall benefits to medication safety and prescription quality continued to outweigh the technological costs identified as the primary factors influencing the economic viability of the technology, including implementation scale and initial investment costs. The principle of economies of scale suggests that large-scale implementation reduces unit costs. This is critical for cost efficiency, and ensuring an appropriate estimation of the service volume is essential for maximizing the benefits of the technology. Additionally, upfront investments and ongoing maintenance costs, which, together, account for a significant portion of total expenses, must be carefully managed. Exploring cost-effective business models and alternative funding sources, such as integrating pharmacy service fees, could further reduce financial barriers and promote wider adoption of the AIAPRS.
In conclusion, the AIAPRS significantly improves prescription quality, reduces medication costs, and enhances medication safety, particularly by addressing high-risk prescriptions. Although the effectiveness of the technology decreases slightly over time as prescribing practices improve, it remains a cost-effective and valuable tool, particularly for grassroots healthcare settings in underdeveloped areas.
This study evaluated the implementation of an AIAPRS in PHIs in an underdeveloped region of China, addressing the paucity of economic evidence on its potential to mitigate pharmacist shortages and enhance medication safety. Our findings revealed that the AIAPRS reduces irrational prescriptions and achieves cost-effectiveness, with medication savings offsetting technological expenses. However, the study had the following limitations: the observation period was brief, reliance on the system by physicians may increase latent risks in the absence of pharmacist oversight, and interviews with physicians and patients were not conducted, limiting insights into user experiences and medication-related concerns.
-
Table S1. Prescription review status from March to June 2023
Characteristics March April May June Between
different monthsn (%) χ2/Ζ P n (%) χ2/Ζ P n (%) χ2/Ζ P n (%) χ2/Ζ P χ2/Ζ P Prescription Review Status Total Initial Prescriptions 66,991 55,027 60,620 55,875 Final Prescriptions 66,390 54,618 60,115 53,262 Irrational Prescriptions 382.013 ** 174.431 ** 221.930 ** 84.823 ** Initial Irrational Prescriptions 18,527 (27.7) 13,120 (23.8) 15,336 (25.3) 13,441 (24.1) 303.951 ** Final Irrational Prescriptions 15,270 (23.0) 11,212 (20.5) 13,023 (21.7) 11,564 (21.7) 108.882 ** Risk Level# 832.985 **a 586.431 **a 741.078 **a 481.105 ** a Initial 226.934 **a High Risk 2,519 (13.6) 1,824 (13.9) 2,030 (13.2) 1,714 (12.8) Moderate Risk 4,132 (22.3) 1,936 (14.8) 2,918 (19.0) 2,024 (15.1) Low Risk 11,876 (64.1) 9,360 (71.3) 10,388 (67.7) 9,703 (72.2) Final 214.6 **a High Risk 307
(2.0)214
(1.9)178
(1.4)168
(1.5)Moderate Risk 3,312 (21.7) 1,716
(15.3)2,425 (18.6) 1,896 (16.4) Low Risk 11,651 (76.3) 9,282 (82.8) 10,420 (80.0) 9,500 (82.2) Cost situation Total Initial Prescription Amount (CNY) 2,333,626.2 1,669,220.0 1,987,196.5 1,796,740.6 Final Prescription Amount (CNY) 1,818,822.1 1,470,406.2 1,707,496.6 1,575,288.1 Saving Cost Savings on Medication (CNY) 514,804.1 198,813.8 279,699.9 221,452.6 Average Medication Cost Saved per Initial Prescription (CNY / CASE) 34.8 30.3 32.8 32.2 Average Medication Cost Saved per Final Prescription (CNY / CASE) 27.4 26.9 28.4 29.6 Average Cost Savings per Prescription (CNY / CASE) 7.4 3.4 4.4 2.6 Note. **P < 0.001. aWilcoxon rank-sum test. #Risk Level: Low Risk: inappropriate drug selection, incorrect solvent selection judgment, lack of solvent judgment, incorrect solvent dosage judgment, inappropriate dosing frequency, and excessive treatment duration. Moderate Risk: Harmful drug interactions, repeated medication less than twice; off-label use: antibiotics for non-infectious diagnoses or complications of infectious diseases. High Risk: Absolute contraindications, repeated medication more than twice, off-label use: antibiotics for non-infectious diseases, antibiotics for nonbacterial infectious diagnoses. Table S2. Cost components of prescription review
Cost CNY / CASE % Total 2.40 - Fixed Cost 2.29 95.2 Equipment Depreciation 0.97 40.2 Intelligent Prescription Review System 0.880 36.6 Front-end Server 0.036 1.5 Application Server 0.003 0.1 Bastion Host 0.015 0.6 Operating System Anti-virus Software 0.010 0.4 Third-Party Interface Fee 0.022 0.9 Equipment Maintenance 1.32 54.9 Maintenance and Upgrade 1.32 54.9 Variable Cost 0.116 4.8 Labor Costs 0.116 4.8 Associate Chief Physician / Chief Physician 0.007 0.3 Attending Physician 0.026 1.1 Physician 0.052 2.2 Medical Assistant 0.031 1.3 Note. Rounded to the nearest decimal place.
doi: 10.3967/bes2025.025
A Health Economic Evaluation of an Artificial Intelligence-assisted Prescription Review System in a Real-world Setting in China
-
Study design: Junrui Pei, Wenqi Fu, Yue Xiao; Experimentation and data analysis: Di Wu, Yingpeng Qiu, Liwei Shi; Manuscript writing: Di Wu; Study coordination and manuscript advice: Kejun Liu, Xueqing Tian, Ping Ren, Mao You. All authors participated in the critical revision and approval of the final manuscript.
The authors declare that no potential conflicts of interest exist.
No ethical approval is required as no individual data were used in this research.
&These authors contributed equally to this work.
注释:1) Authors’ Contributions: 2) Competing Interests: 3) Ethics: -
Table 1. Cost-effectiveness analysis
Month Cost of Prescription Review
(CNY)Drug Savings by Prescription
(CNY)Total Saving
(CNY)#Change Rate of Irrational
Prescriptions (%)*March 204,829.2 514,804.1 309,974.9 4.7 April 163,375.7 198,813.8 35,438.1 3.3 May 181,985.2 279,699.9 97,714.7 3.6 June 160,862.5 221,452.6 60,590.1 2.4 Average 177,763.2 303,692.6 125,929.4 3.5 Note. #total saving = savings by prescription – Cost of Prescription Review; *Change in the proportion of irrational prescriptions before and after AI intervention in the same month. S1. Prescription review status from March to June 2023
Characteristics March April May June Between
different monthsn (%) χ2/Ζ P n (%) χ2/Ζ P n (%) χ2/Ζ P n (%) χ2/Ζ P χ2/Ζ P Prescription Review Status Total Initial Prescriptions 66,991 55,027 60,620 55,875 Final Prescriptions 66,390 54,618 60,115 53,262 Irrational Prescriptions 382.013 ** 174.431 ** 221.930 ** 84.823 ** Initial Irrational Prescriptions 18,527 (27.7) 13,120 (23.8) 15,336 (25.3) 13,441 (24.1) 303.951 ** Final Irrational Prescriptions 15,270 (23.0) 11,212 (20.5) 13,023 (21.7) 11,564 (21.7) 108.882 ** Risk Level# 832.985 **a 586.431 **a 741.078 **a 481.105 ** a Initial 226.934 **a High Risk 2,519 (13.6) 1,824 (13.9) 2,030 (13.2) 1,714 (12.8) Moderate Risk 4,132 (22.3) 1,936 (14.8) 2,918 (19.0) 2,024 (15.1) Low Risk 11,876 (64.1) 9,360 (71.3) 10,388 (67.7) 9,703 (72.2) Final 214.6 **a High Risk 307
(2.0)214
(1.9)178
(1.4)168
(1.5)Moderate Risk 3,312 (21.7) 1,716
(15.3)2,425 (18.6) 1,896 (16.4) Low Risk 11,651 (76.3) 9,282 (82.8) 10,420 (80.0) 9,500 (82.2) Cost situation Total Initial Prescription Amount (CNY) 2,333,626.2 1,669,220.0 1,987,196.5 1,796,740.6 Final Prescription Amount (CNY) 1,818,822.1 1,470,406.2 1,707,496.6 1,575,288.1 Saving Cost Savings on Medication (CNY) 514,804.1 198,813.8 279,699.9 221,452.6 Average Medication Cost Saved per Initial Prescription (CNY / CASE) 34.8 30.3 32.8 32.2 Average Medication Cost Saved per Final Prescription (CNY / CASE) 27.4 26.9 28.4 29.6 Average Cost Savings per Prescription (CNY / CASE) 7.4 3.4 4.4 2.6 Note. **P < 0.001. aWilcoxon rank-sum test. #Risk Level: Low Risk: inappropriate drug selection, incorrect solvent selection judgment, lack of solvent judgment, incorrect solvent dosage judgment, inappropriate dosing frequency, and excessive treatment duration. Moderate Risk: Harmful drug interactions, repeated medication less than twice; off-label use: antibiotics for non-infectious diagnoses or complications of infectious diseases. High Risk: Absolute contraindications, repeated medication more than twice, off-label use: antibiotics for non-infectious diseases, antibiotics for nonbacterial infectious diagnoses. S2. Cost components of prescription review
Cost CNY / CASE % Total 2.40 - Fixed Cost 2.29 95.2 Equipment Depreciation 0.97 40.2 Intelligent Prescription Review System 0.880 36.6 Front-end Server 0.036 1.5 Application Server 0.003 0.1 Bastion Host 0.015 0.6 Operating System Anti-virus Software 0.010 0.4 Third-Party Interface Fee 0.022 0.9 Equipment Maintenance 1.32 54.9 Maintenance and Upgrade 1.32 54.9 Variable Cost 0.116 4.8 Labor Costs 0.116 4.8 Associate Chief Physician / Chief Physician 0.007 0.3 Attending Physician 0.026 1.1 Physician 0.052 2.2 Medical Assistant 0.031 1.3 Note. Rounded to the nearest decimal place. -
[1] Holloway KA. Combating inappropriate use of medicines. Expert Rev Clin Pharmacol, 2011; 4, 335−48. doi: 10.1586/ecp.11.14 [2] Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet, 2017; 390, 156−68. doi: 10.1016/S0140-6736(16)32585-5 [3] Machowska A, Stålsby Lundborg C. Drivers of irrational use of antibiotics in Europe. Int J Environ Res Public Health, 2019; 16, 27. [4] Chao JQ, Gu JY, Zhang H, et al. The impact of the national essential medicines policy on rational drug use in primary care institutions in Jiangsu Province of China. Iran J Public Health, 2018; 47, 24−32. [5] World Health Organization. WHO launches global effort to halve medication-related errors in 5 years. https://www.who.int/news/item/29-03-2017-who-launches-global-effort-to-halve-medication-related-errors-in-5-years. [2024-05-15] [6] Liu JB, Zhang YM, Chen NN, et al. Remote pharmacy service in primary care: the implementation of a cloud-based pre-prescription review system. J Am Pharm Assoc (2003), 2021; 61, e176−82. doi: 10.1016/j.japh.2020.12.008 [7] Bu FJ, Sun H, Li L, et al. Artificial intelligence-based internet hospital pharmacy services in China: perspective based on a case study. Front Pharmacol, 2022; 13, 1027808. doi: 10.3389/fphar.2022.1027808 [8] Segal G, Segev A, Brom A, et al. Reducing drug prescription errors and adverse drug events by application of a probabilistic, machine-learning based clinical decision support system in an inpatient setting. J Am Med Inform Assoc, 2019; 26, 1560−5. doi: 10.1093/jamia/ocz135 [9] Fan XC, Chen DX, Bao SW, et al. Prospective prescription review system correlated with more rational PPI medication use, better clinical outcomes and reduced PPI costs: experience from a retrospective cohort study. BMC Health Serv Res, 2023; 23, 1014. doi: 10.1186/s12913-023-09931-5 [10] Chalasani SH, Syed J, Ramesh M, et al. Artificial intelligence in the field of pharmacy practice: a literature review. Explor Res Clin Soc Pharm, 2023; 12, 100346. -
 24263+Supplementary Materials.pdf
24263+Supplementary Materials.pdf

-




 下载:
下载:





 Quick Links
Quick Links