-
The cardiopulmonary health of children may be affected by acute ozone (O3) exposure during physical activity[1]; however, its effects in high-altitude regions such as the Tibetan Plateau remain uncertain. In high-altitude areas, lower oxygen levels may cause children to experience shortness of breath or require increased respiratory effort during vigorous activities such as running. This could lead to increased pollutant inhalation, potentially elevating the burden on the cardiovascular system and triggering adverse reactions such as increased heart rate and elevated blood pressure. Furthermore, differences in physiological adaptation between Han children who have migrated to Tibet and Tibetan children who are native to the region may contribute to different reactions to environmental exposure[2].
This study aimed to explore the health impacts of O3 exposure during physical activity in children residing in the Tibetan Plateau and to investigate the influence of adaptive responses.
The experiment was conducted in Lahsa, Qinghai-Tibet Plateau, where the O3 concentration is sustained at high levels partly due to strong ultraviolet radiation during summer afternoons, while fine particulate matter (PM2.5) concentration is extremely low. The typical daily maximum 8-h average O3 concentrations is 124 μg/m3, exceeding the air World Health Organization (WHO) guideline of 100 μg/m3. The typical daily mean PM2.5 concentration is 8 μg/m3, well below the WHO guideline of 15 µg/m3. Therefore, we attributed the observed adverse effects of O3 exposure.
Based on the preliminary studies, a total of 60 children were included (28 Han and 32 Tibetan students). Participants were divided into five groups, ensuring equal distribution of boys, girls, Tibetans, and Han Chinese in each group. The experiment were conducted across five afternoons during the week under consistent experimental conditions.
This study aimed to analyze the health effects of O3 exposure through multiple experiments. Upon arrival at the study center, participants rested and underwent baseline health measurements. From 15:00 to 15:30 pm, participants completed a 2-km run at maximal effort. Following the run, they rested and were re-assessed for the same health measurements. Blood pressure and lung function were measured before and after exposure. The study protocol was approved by the institutional ethics review committee, and written informed consent was obtained from all participants and their guardians. Environmental monitoring included measurement of O3, PM1, PM2.5, PM10, carbon monoxide (CO), nitrogen dioxide (NO2), and light intensity using a Personal Exposure Kit (PEK) with a 60-s resolution. Real-time ambient temperature and relative humidity were recorded using a Hobo data logger. All instruments were calibrated before use. Outdoor pollutant levels were measured within 3 m of the exercising area, and indoor pollutant concentrations were also documented as potential confounders because the students spent approximately 12 h indoors. Outdoor pollutant data were aggregated into 30 min intervals, while indoor daily averages were calculated based on 12-h measurements. Trained technicians conducted the lung function and blood pressure measurements at the clinical center. Lung function was measured using a calibrated spirometer according to ATS/ERS recommendations, and included forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), peak expiratory flow (PEF), and mean forced expiratory flow between 25% and 75% of FVC (FEF2575). Three to four maneuvers were performed by each participant. Blood pressure was measured using an Omron HEM-7211 sphygmomanometer which is produced by Omron Corporation in Kyoto, Japan, with three readings averaged for systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP).
A detailed questionnaire was designed for all three parties—households, students, and parents—to better understand and control for potential confounding factors that may influence the results of the study. This information was used to enhance the accuracy and reliability of the findings.
We assessed the differences in lung function and blood pressure from baseline to post-exposure in children following running exercise, identifying the main pollutant as O3. A generalized linear model (GLM) was used to explore the effects of O3 exposure on lung function and blood pressure. In this model, the O3 concentration served as the independent variable, while lung function indices and blood pressure measurements served as dependent variables. We incorporated various potential confounding factors, including age, sex, body mass index (BMI), and ethnicity, as covariates in the GLM. Additional adjustments were made for other covariates such as temperature, humidity, concentrations of other pollutants, indoor O3 concentrations, and questionnaire results. Stratified regression analyses were performed according to ethnicity and sex to explore the effects of O3 on different populations. All statistical analyses were performed using IBM SPSS Statistics V22. Two-tailed P-values < 0.05 were considered statistically significant.
Our findings revealed that local Tibetan students had higher blood pressure than Han students who migrated to the plateau. Additionally, lung function was better among Tibetans than in Han Chinese individuals. The mean and peak values of O3 were 63.06 ± 18.33 μg/m3 and 84.44 ± 18.00 μg/m3, respectively, and the mean concentrations of PM1, PM2.5, and PM10 were substantially lower: 1.14 ± 0.61 μg/m3, 1.21 ± 0.56 μg/m3 and 1.44 ± 0.53 μg/m3, respectively.
Our study found that children exercising under these pollution-exposed high-altitude conditions had decreased lung function and blood pressure. FVC, FEV1, PEF, and FEF25-75 decreased by 4.99% (95% confidence interval [CI]: −12.20% to 2.22%), 4.70% (95% CI: −11.81% to 2.40%), 2.38% (95% CI: −11.55% to 6.78%), and 6.13% (95% CI: −15.90% to 3.65%) per 1 μg/m3 increase in O3 exposure, respectively, indicating that the adverse effect of O3 on lung function exceeded the benefits from physical activity overall (Figure 1). O3 exposure during physical activities decreased SBP, DBP, and MAP by 0.85% (95% CI: −5.05% to 3.36%), 3.67% (95% CI: −10.40% to 3.06%), and 2.19% (95% CI: −7.02% to 2.64%) per 1 μg/m3 increased in O3 concentration, respectively (Figure 2). These findings are consistent with previous studies. For instance, a strictly controlled laboratory study showed that after 3 h of exercise, FEV1 and FVC were lower in the 70 ppb (P_FEV1 = 0.116 and P_FVC = 0.115) and 120 ppb O3 exposure groups (p_FEV1 = 0.001 and p_FVC = 0.003, respectively) than in those without O3 exposure (0 ppb)[1]. The mean O3 concentration during the 30-min running period in this experiment (approximately 30 ppb) was much lower than in the above study, indicating that even low O3 levels (below the WHO guidelines) can degrade lung function. A mechanistic study showed that O3 exposure increased the permeability of epithelial cells, facilitating the entry of inhaled allergens and toxins and triggering the release of inflammatory cytokines (interleukin [IL]-1, IL-6, IL-8, and tumor necrosis factor [TNF]) [3,4]. Other studies also support our results regarding blood pressure. Pun et al.[5] reported that after a 30-min run along a polluted route with an O3 concentration of 73.5 ppb, SBP and DBP decreased by 6.6 mmHg (95% CI: −13.2 to −0.06 mmHg) and 5.8 mmHg (95% CI: −11.0 to −0.70 mmHg), respectively.
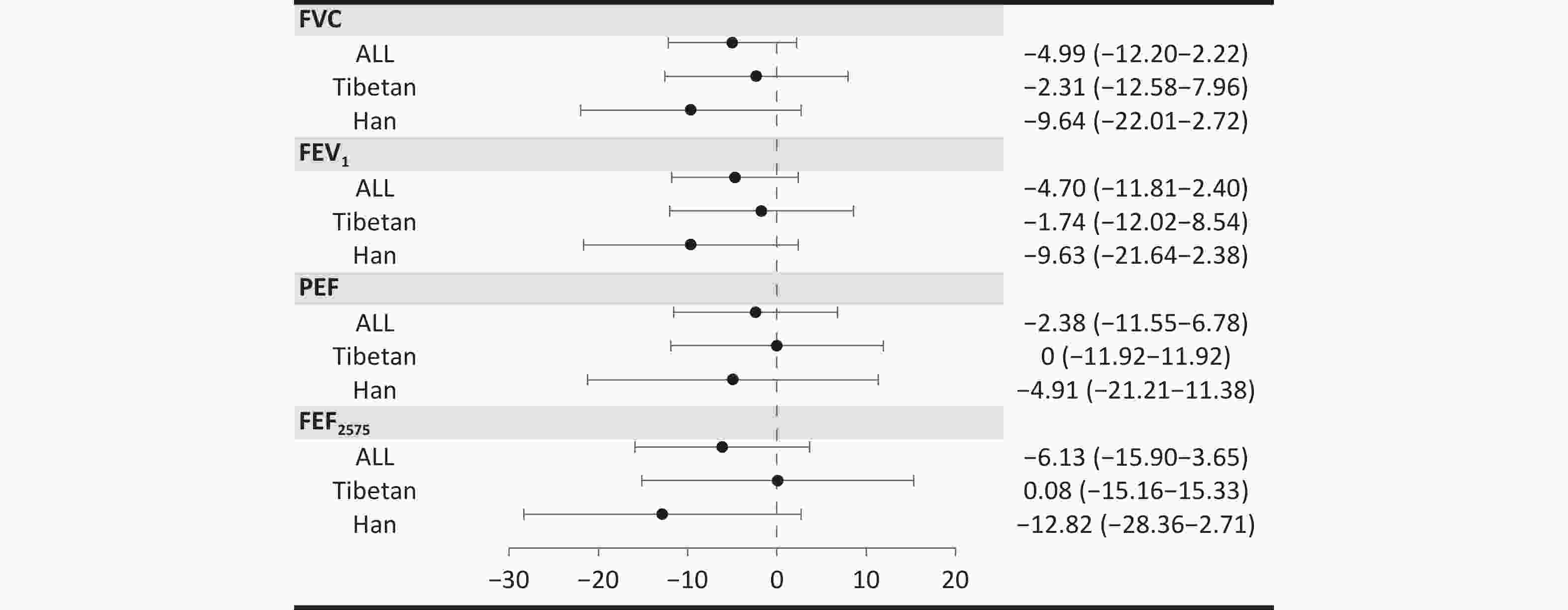
Figure 1. Percent change in lung function change per 1 μg/m3 increase in Ozone (O3) concentration, stratified by Tibetan and Han Chinese groups. The model is adjusted for age, body mass index (BMI), sex, temperature, humidity, indoor O3 concentration, other air pollutants, exercise habits, and household habits. Estimates and 95% confidence intervals (CIs) for percent change in lung function are shown.
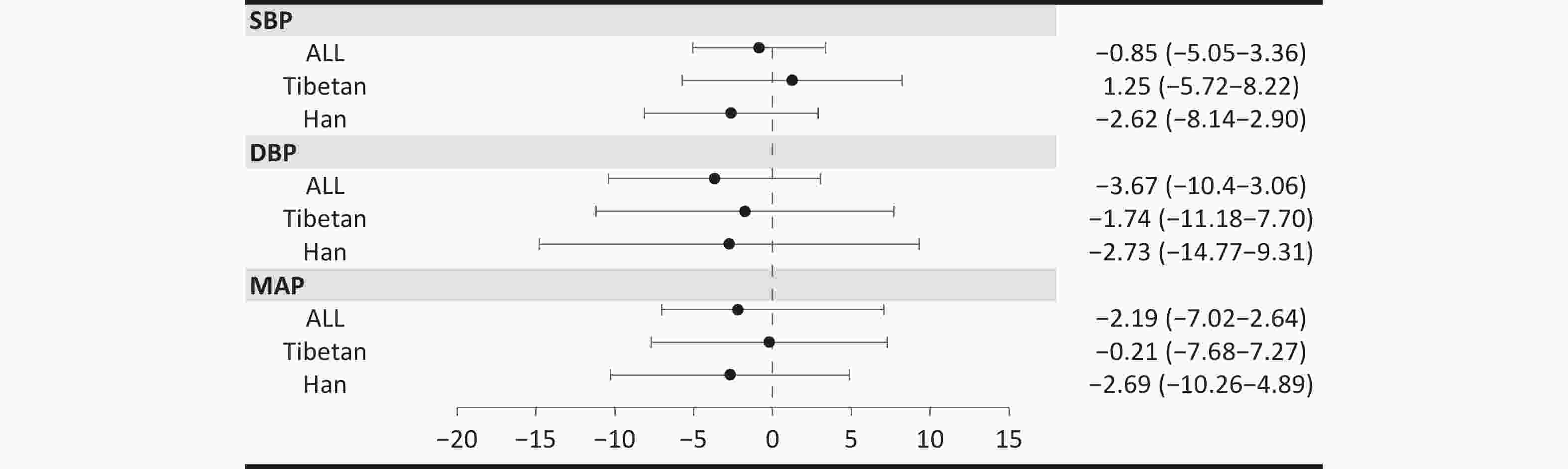
Figure 2. Percent change in blood pressure change per 1 μg/m3 increase in O3 concentration, stratified by Tibetan and Han Chinese groups. The model is adjusted for age, BMI, sex, temperature, humidity, indoor O3 concentration, other air pollutants, exercise habits, and household habits. Estimates and 95% confidence intervals (CIs) for percent change in blood pressure are shown.
Among local Tibetan students, lung function showed marginal changes after physical activity, with FEF2575 increasing slightly by 0.08% (95% CI: −15.16% to 15.33%), possibly due to the beneficial effects of physical activity offsetting the harmful effects of high O3 levels. In contrast, Han Chinese children experienced greater declines in lung function indicators, with FVC, FEV1, PEF, and FEF25−75 decreasing by 9.64% (95% CI: −22.01% to 2.72%), 9.63% (95% CI: −21.64% to 2.38%), 4.91% (95% CI: −21.21% to 11.38%), and 12.82% (95% CI: −28.36% to 2.71%) per 1 μg/m3 increase in O3 exposure, respectively, suggesting that the
Blood pressure showed similar results. O3 exposure showed a positive effect on SBP among Tibetan students but a negative effect among Han students. DBP decreased by 1.74% (95% CI: −11.18% to 7.70%) for Tibetans and 2.73% (95% CI: −14.77% to 9.31%) for Han Chinese per 1 μg/m3 increase in O₃. Physical activity under high-O3 conditions in the highlands also showed unfavorable effects on MAP for both Tibetans and Han Chinese, with greater effects observed in the Han Chinese students.
We also discussed the different outcomes for Tibetan girls, Han Chinese girls, Tibetan boys, and Han Chinese boys and found that for different sexes, there was a more pronounced effect among Han Chinese students compared to Tibetan students. (Table 1)
Table 1. Lung function and blood pressure change (%) per 1 μg/m3 O3 increase and grouped according to sex and Tibetan-Han Chinese
Group β 95% CI Lower Upper FVC Girls Tibetans 4.68 −17.05 26.41 Han Chinese* −22.9 −32.21 −13.58 Boys Tibetans −4.55 −17.08 7.97 Han Chinese 16.34 −1.79 34.47 FEV1 Girls Tibetans 3.81 −17.58 25.20 Han Chinese* −22.05 −32.97 −11.14 Boys Tibetans −3.67 −16.98 9.64 Han Chinese 15.46 −4.48 35.39 PEF Girls Tibetans −0.59 −21.75 20.57 Han Chinese −10.78 −50.07 28.50 Boys Tibetans 2.92 −16.63 22.48 Han Chinese −10.4 −44.90 24.1 FEF2575 Girls Tibetans −5.51 −21.81 10.80 Han Chinese −12.49 −35.79 10.80 Boys Tibetans 2.95 −26.74 32.63 Han Chinese −10.07 −42.34 22.20 SBP Girls Tibetans 1.59 −11.05 14.24 Han Chinese −5.32 −15.45 4.80 Boys Tibetans 2.15 −6.59 10.89 Han Chinese −4.87 −15.99 6.25 DBP Girls Tibetans −3.12 −23.77 17.53 Han Chinese −10.33 −50.08 29.43 Boys Tibetans 0.66 −11.43 12.75 Han Chinese 0.72 −22.01 23.44 MAP Girls Tibetans −0.69 −16.30 14.93 Han Chinese −7.83 −28.07 12.41 Boys Tibetans 1.36 −7.90 10.63 Han Chinese −1.85 −18.88 15.18 Note. The model was adjusted for age, body mass index (BMI), temperature, humidity, indoor O3 concentration, other air pollutants and exercise habits, household habits. Estimates and 95% confidence intervals (CIs) for percent change in blood pressure are shown. Our study showed that exercise in a plateau environment had a greater effect on lung function and blood pressure in Han Chinese children than in Tibetan children. This may be due to differences in adaptation to plateau environments. The cardiorespiratory function of the Tibetan population is usually stronger because of their long-term residence in highland areas. They have larger chest circumference and total lung capacity, higher resting ventilation per minute, higher aerobic capacity, and a sensitive hypoxic ventilatory response[6], resulting in more efficient gas exchange in the low-oxygen environment of the plateau. This adaptation allows Tibetan students to exchange gases more efficiently in the low-oxygen environment of the plateau using a step-by-step load cycling test; they showed higher minute ventilation (P < 0.05), oxygen uptake (P < 0.05), stroke volume (P < 0.05), and cardiac output (P < 0.01) at maximal effort[7]. In contrast, Han Chinese students may be more susceptible to poor cardiorespiratory fitness in the same plateau environment because they have not yet developed such adaptations. Due to their stronger cardiorespiratory function, Tibetans may be able to cope better with the physiological stress brought about by the low-oxygen environment of the plateau, thus keeping their blood pressure stable. In contrast, the Han Chinese students, due to their relatively weaker cardiorespiratory fitness, experience more pronounced blood pressure fluctuations when exercising in a plateau environment. DNA methylation is linked to lifelong high-altitude adaptation. For instance, Quechua populations in Peru exhibit plateau-adapted phenotypes associated with epigenetic modifications. Local genetic variations influence DNA methylation levels, with methylation-related single nucleotide polymorphisms offering a potential avenue for studying genetic adaptations to hypoxia[8]. Similarly, plateau-dwelling Tibetan populations may exhibit such phenotypes. According to the research from the Su Bing laboratory, a series of candidate genes related to Tibetan high-altitude adaptation have been identified, including EPAS1 and EGLN1, and further functional omics analysis has confirmed the involvement of these genes in the adaptation to hypoxic environments[9].
Although this study yielded certain findings, it also exhibited several limitations that are crucial for a comprehensive understanding and application of its conclusions. We did not find a significant correlation between air pollution and blood pressure or lung function parameters; however, the consistent trends observed in our results suggest potential physiological relevance and warrant further investigation. The specific mechanisms underlying these trends require further investigation to confirm their universality and reliability. Additionally, the small sample size (n = 60) may limit the generalizability of the findings; however, these preliminary results provide screening and guidance values for subsequent studies. Considering that the study was conducted in a highland area to compare Han Chinese and Tibetan children, this complex environmental and demographic context posed several challenges. However, in this study, we included as many participants as possible. Finally, as an experimental study, this research primarily focused on children with long-term exercise habits who were exposed to relatively high O3 concentrations in the highlands, relying solely on self-controlled experiments to draw epidemiological conclusions. Therefore, the underlying mechanisms and scope of their application must be further explored and validated.
Our study shows that Han Chinese children have a greater decrease in lung function and blood pressure under O3 exposure compared to Tibetan children. These results have important implications for public health strategies and policy development in plateau regions. Schools should develop personalized physical education programs for Tibetan and Han Chinese children. Medical institutions and public health departments should enhance health monitoring and early screening for children living in plateau regions, with early intervention and treatment for those with altitude sickness or cardiopulmonary abnormalities. Families and society should increase awareness of children's health issues in a plateau environment, with parents guiding their children to understand and protect themselves from adverse effects. Society should work together to create healthier and safer living environments for children in plateau regions. Further research on the mechanisms and factors influencing children's health in plateau environments, as well as the health effects of O3 pollution, is needed to provide a scientific basis for more effective health policies and public health interventions.
doi: 10.3967/bes2025.054
Effects of Ozone Exposure on Cardiopulmonary Function and Adaptive Responses in Han and Tibetan Children During Physical Activity at High Altitudes
-
Mengyao Bian: Methodology, Investigation, Data Curation, Formal analysis, Writing - original draft, Visualization; Ling Qi: Methodology, Writing review & editing ; Qian Guo: Methodology ; Yuchen Zhao: Methodology ; Xiaoli Duan: Conceptualization, Methodology, Data Curation, Writing review & editing, Supervision, Project administration, Funding, acquisition.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The Ethics Review Committee of the University of Science and Technology Beijing approved the study (Reference No.: 2021-1-103). All participants have signed the informed consent.
注释:1) Authors’ Contributions: 2) Competing Interests: 3) Ethics: -
Figure 1. Percent change in lung function change per 1 μg/m3 increase in Ozone (O3) concentration, stratified by Tibetan and Han Chinese groups. The model is adjusted for age, body mass index (BMI), sex, temperature, humidity, indoor O3 concentration, other air pollutants, exercise habits, and household habits. Estimates and 95% confidence intervals (CIs) for percent change in lung function are shown.
Figure 2. Percent change in blood pressure change per 1 μg/m3 increase in O3 concentration, stratified by Tibetan and Han Chinese groups. The model is adjusted for age, BMI, sex, temperature, humidity, indoor O3 concentration, other air pollutants, exercise habits, and household habits. Estimates and 95% confidence intervals (CIs) for percent change in blood pressure are shown.
Table 1. Lung function and blood pressure change (%) per 1 μg/m3 O3 increase and grouped according to sex and Tibetan-Han Chinese
Group β 95% CI Lower Upper FVC Girls Tibetans 4.68 −17.05 26.41 Han Chinese* −22.9 −32.21 −13.58 Boys Tibetans −4.55 −17.08 7.97 Han Chinese 16.34 −1.79 34.47 FEV1 Girls Tibetans 3.81 −17.58 25.20 Han Chinese* −22.05 −32.97 −11.14 Boys Tibetans −3.67 −16.98 9.64 Han Chinese 15.46 −4.48 35.39 PEF Girls Tibetans −0.59 −21.75 20.57 Han Chinese −10.78 −50.07 28.50 Boys Tibetans 2.92 −16.63 22.48 Han Chinese −10.4 −44.90 24.1 FEF2575 Girls Tibetans −5.51 −21.81 10.80 Han Chinese −12.49 −35.79 10.80 Boys Tibetans 2.95 −26.74 32.63 Han Chinese −10.07 −42.34 22.20 SBP Girls Tibetans 1.59 −11.05 14.24 Han Chinese −5.32 −15.45 4.80 Boys Tibetans 2.15 −6.59 10.89 Han Chinese −4.87 −15.99 6.25 DBP Girls Tibetans −3.12 −23.77 17.53 Han Chinese −10.33 −50.08 29.43 Boys Tibetans 0.66 −11.43 12.75 Han Chinese 0.72 −22.01 23.44 MAP Girls Tibetans −0.69 −16.30 14.93 Han Chinese −7.83 −28.07 12.41 Boys Tibetans 1.36 −7.90 10.63 Han Chinese −1.85 −18.88 15.18 Note. The model was adjusted for age, body mass index (BMI), temperature, humidity, indoor O3 concentration, other air pollutants and exercise habits, household habits. Estimates and 95% confidence intervals (CIs) for percent change in blood pressure are shown. -
[1] Li T, Yu XM, Li LZ. Analysis of influence and factors of plateau environment on health status of body. Chin Foreign Med Res, 2024; 22, 168−75. (In Chinese) [2] Arjomandi M, Balmes JR, Frampton MW, et al. Respiratory responses to ozone exposure. MOSES (the multicenter ozone study in older subjects). Am J Respir Crit Care Med, 2018; 197, 1319−27. doi: 10.1164/rccm.201708-1613OC [3] Day DB, Xiang JB, Mo JH, et al. Association of ozone exposure with cardiorespiratory pathophysiologic mechanisms in healthy adults. JAMA Intern Med, 2017; 177, 1344−53. doi: 10.1001/jamainternmed.2017.2842 [4] Olivieri D, Scoditti E. Impact of environmental factors on lung defences. Eur Respir Rev, 2005; 14, 51−6. doi: 10.1183/09059180.05.00009502 [5] Pun VC, Ho KF. Blood pressure and pulmonary health effects of ozone and black carbon exposure in young adult runners. Sci Total Environ, 2019; 657, 1−6. doi: 10.1016/j.scitotenv.2018.11.465 [6] Wu TY, Kayser B. High altitude adaptation in Tibetans. High Alt Med Biol, 2006; 7, 193−208. doi: 10.1089/ham.2006.7.193 [7] Chen QH. Characteristice of cardio-puimonary functions during exercise in school children at high altitude. Qinghai High Altitude Medical Science Institute. (In Chinese) [8] Childebayeva A, Goodrich JM, Leon-Velarde F, et al. Genome-wide epigenetic signatures of adaptive developmental plasticity in the Andes. Genome Biol Evol, 2021; 13, evaa239. doi: 10.1093/gbe/evaa239 [9] Zheng WS, He YX, Guo YB, et al. Large-scale genome sequencing redefines the genetic footprints of high-altitude adaptation in Tibetans. Genome Biol, 2023; 24, 73. doi: 10.1186/s13059-023-02912-1 -




 下载:
下载:




 Quick Links
Quick Links