HTML
-
Three-vessel disease (TVD), characterized by significant stenosis in three main epicardial coronary arteries, is found in 20%-30% of patients with obstructive coronary artery disease (CAD)[1, 2] and 15%-20% of patients with acute myocardial infarction (MI)[3, 4]. It is well established that TVD increases the risk of mortality compared with singlevessel disease[3, 5]. Therefore, risk stratification in patients with TVD is important for improving management and prognosis. The Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) score characterizes the extent and severity of CAD and is tightly related to the outcomes in patients with TVD[6].
As the prominent cation and anion in extracellular fluid, serum sodium, and chloride levels are directly correlated with each other to preserve electroneutrality[7]. Both are commonly assessed as a part of routine biochemical testing in clinical practice. The significance of serum sodium level has been studied in diverse cardiovascular conditions. For example, low serum sodium level at admission was associated with worse prognosis and increased mortality in patients with acute coronary syndrome[8-12] and heart failure (HF)[13, 14]. By contrast, the role of serum chloride in cardiovascular diseases was largely overlooked until recent studies indicated that low serum chloride level was an independent predictor of mortality in patients with HF[7, 15, 16] and acute MI accompanied by systolic dysfunction[17]. However, the application of serum sodium and chloride levels in high-risk CAD patients with advanced coronary atheroma burden remains unclear. Therefore, this study aimed to evaluate the long-term prognostic value of serum chloride and sodium levels in patients with TVD.
-
This prospective cohort study enrolled 8, 943 consecutive patients with TVD at Fuwai Hospital, Chinese Academy of Medical Sciences from April 2004 to February 2011[18]. Patients were eligible for inclusion in the study if they had TVD, defined as angiographically confirmed stenosis of ≥ 50% in all three main epicardial coronary arteries (i.e., left anterior descending, left circumflex and right coronary arteries), with or without involvement of the left main artery, and were willing to receive follow-up. There was no pre-specified exclusion criterion. Patients received medical therapy (MT) alone, percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) according to clinical and anatomical factors, contemporary treatment guidelines[19, 20], and their preferences. After enrollment, the patients were followed up as study protocol defined. Baseline and procedural data for all the participants were collected in a database by independent clinical research coordinators. Outcome data were obtained through telephone interview, follow-up letter, or clinic visit. The last follow-up was completed in 2016, with a response rate of 80.6%. All events were carefully checked and verified by an independent group of clinical physicians. Investigator training, blinded questionnaire survey, and telephone recording were performed to obtain results with high-quality.
The study conformed to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Fuwai Hospital. Written informed consents were obtained from all the participants.
-
Baseline serum chloride and sodium levels were measured by using blood samples which were taken from the patients by direct venipuncture after admission for coronary angiography. The SYNTAX score[6] was calculated by a dedicated research group blinded to the clinical data using an online calculator (http://www.syntaxscore.com). Creatinine clearance was calculated by using the Cockcroft and Gault formula[21].
-
The primary endpoint was all-cause death. Secondary endpoints included cardiac death, major adverse cardiac and cerebrovascular events (MACCE), a composite of all-cause death, myocardial infarction, stroke or unplanned revascularization, and the individual components of the composite endpoint. All deaths were considered as cardiac ones unless an unequivocal non-cardiac cause could be established.
-
Continuous variables are presented as mean ± standard deviation, while categorical variables are presented as numbers of patients and proportions (%). One-way ANOVA was used to compare continuous variables, and χ2 test or Fisher's exact test was used for the comparisons among the categorical variables.
The study population was stratified into tertiles by each of the following two variables: serum chloride levels ≤ 102.0 mmol/L, > 102.0 to ≤ 105.1 mmol/L, and > 105.1 mmol/L; and serum sodium levels ≤ 139.0 mmol/L, > 139.0 to ≤ 141.0 mmol/L, and > 141.0 mmol/L. Spearman correlation coefficient was used to assess the correlation between serum chloride level and serum sodium level. Survival curves were constructed with the Kaplan-Meier method and log-rank tests were used to compare the curves of different groups based on tertiles of serum chloride and sodium levels. Univariable and multivariable Cox proportional hazard models were used to calculate hazard ratio (HR) and 95% confidence interval (CI) to analyze the relationship of serum chloride and sodium levels with long-term outcomes. In multivariable analyses, covariates were selected based on their prognostic relevance, potential confounding effect and clinical significance. A base model was constructed with the following covariates: age, sex, body mass index, medical history and risk factor (hypertension, diabetes mellitus, previous MI, hyperlipidemia, stroke, peripheral artery disease, and chronic kidney disease), presentation [stable angina pectoris (SAP), unstable angina pectoris (UAP), or acute myocardial infarction (AMI)], left ventricular ejection fraction (LVEF), left main coronary artery involvement, creatinine clearance, SYNTAX score (0-22, 23-32, or ≥ 33) and procedure (MT, PCI, or CABG).
The interaction between serum chloride and sodium levels with outcomes was tested by using the multivariable Cox regression hazard model. Subgroup analyses were performed based on the following covariates: age (≥ 65 or < 65 years), sex (male or female), diabetes (yes or no), presentation (SAP, UAP, or AMI), LVEF (≥ 40% vs. < 40%), left main disease (yes or no), SYNTAX score (0-22, 23-32, or ≥ 32), and procedure (MT, PCI, or CABG). Interactions between chloride or sodium levels and these covariates on outcomes were tested to interpret possible subgroup differences.
Comparisons of area under the receiver operating characteristic curves (AUC) were performed to assess differences between predictability of the SYNTAX score with and without serum chloride or sodium levels as an additional variable. Two-sided P-values < 0.05 were considered statistically significant. Statistical analyses were performed with SPSS software version 22.0 (IBM, Armonk, NY, USA).
Study Design and Participants
Definitions
Outcomes and Follow-up
Statistical Analysis
-
A total of 8, 318 (93%) participants with available serum chloride and sodium values were included in the present analysis. The mean levels of serum chloride and sodium were 103.5 ± 3.5 mmol/L and 139.9 ± 3.1 mmol/L, respectively. The correlation between serum chloride level and serum sodium level was modest (r = 0.41, P < 0.001).
Baseline characteristics of the participants grouped by tertiles of serum chloride and sodium levels are presented in Table 1. Patients in the low chloride tertiles group (≤ 102.0 mmol/L) were younger, had higher rates of diabetes and MI, lower LVEF and serum sodium level, higher creatinine clearance, and received MT more frequently. Patients in the low sodium tertiles group (≤ 139.0 mmol/L) showed a higher prevalence of diabetes, chronic kidney disease and MI, with lower LVEF and serum chloride level, and were more likely to receive MT.

Table 1. Baseline Characteristics of the Study Population
-
During the median follow-up of 7.5 years, deaths from any cause were observed in 1, 249 patients (15.0%), including 643 deaths from cardiac causes (7.7%). Most all-cause deaths, cardiac deaths and MACCE occurred in patients in the low tertiles group of serum chloride or sodium level (Table 2).

Table 2. Long-Term Clinical Outcomes of the Study Population
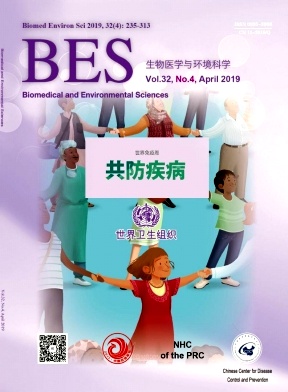
In univariate analyses, patients in the low tertiles group of serum chloride level had a higher risk for all-cause death (HR: 1.25, 95% CI: 1.09-1.43, P = 0.001), cardiac death (HR: 1.52, 95% CI: 1.26-1.84, P < 0.001), and MACCE (HR: 1.13, 95% CI: 1.03-1.24, P = 0.012), but not for MI, stroke or unplanned revascularization, compared with those in the high tertiles group (Table 3 and Supplementary Table S1 available in www.besjournal.com). Comparable findings were also observed in patients in the low tertiles group of serum sodium level (Table 3 and Supplementary Table S1). Kaplan-Meier estimates of all-cause death, cardiac death and MACCE were significantly different across tertiles groups of serum chloride and sodium levels (log-rank P < 0.05 for all) (Figure 1A-F).
Variable Myocardial Infarction Stroke Unplanned Revascularization HR (95% CI) P-value HR (95% CI) P-value HR (95% CI) P-value Chloride ≤ 102.0 mmol/L 0.92 (0.74-1.15) 0.451 1.03 (0.85-1.25) 0.752 1.03 (0.86-1.23) 0.780 Chloride > 102.0 to ≤ 105.1 mmol/L 0.99 (0.80-1.23) 0.944 0.86 (0.70-1.05) 0.127 1.00 (0.84-1.20) 0.977 Chloride > 105.1 mmol/L Reference Reference Reference Sodium ≤ 139.0 mmol/L 0.94 (0.76-1.16) 0.550 1.01 (0.83-1.22) 0.940 0.88 (0.74-1.06) 0.173 Sodium > 139.0 to ≤ 141.0 mmol/L 0.93 (0.74-1.17) 0.520 1.00 (0.81-1.23) 0.994 1.00 (0.83-1.20) 0.989 Sodium > 141.0 mmol/L Reference Reference Reference Note. CI, confidence interval; HR indicates hazard ratio. Table Supplementary Table S1. Univariable Analysis for Other Secondary Endpoints

Table 3. Univariable and Multivariable Analysis for Mortality and MACCE

Figure 1. Kaplan-Meier curves for all-cause death (A, D), cardiac death (B, E) and major adverse cardiac and cerebrovascular events (MACCE; C, F) across tertiles of chloride and sodium. Cl, serum chloride level, mmol/L; Na, serum sodium level, mmol/L.
When both chloride and sodium were simultaneously integrated into the base model, low sodium level (≤ 139.0 mmol/L) remained significantly associated with an increased risk for all-cause death (HR: 1.16, 95% CI: 1.01-1.34, P = 0.041) and cardiac death (HR: 1.26, 95% CI: 1.03-1.55, P = 0.027), while serum chloride level was no longer significantly associated with the outcomes (Table 3). There was no interaction of serum chloride and sodium levels with all-cause or cardiac death (P = 0.705 and 0.618, respectively).
-
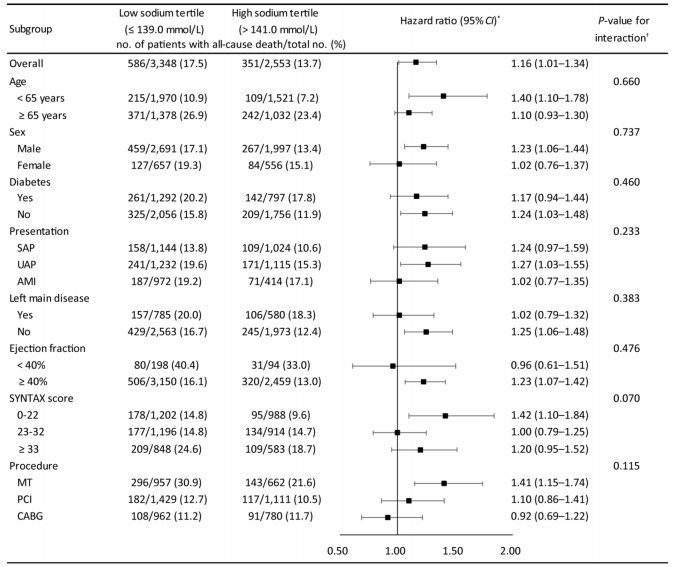
The relationship of serum sodium level with all-cause death was relatively consistent across the subgroups of age, sex, diabetes, presentation, left main disease, LVEF, SYNTAX score or procedure (Figure 2). There was no significant interaction of tertiles of sodium and these covariates (interaction P-value > 0.05 for all subgroups).
Figure 2. Associations of tertiles of serum sodium with risk of all-cause death across subgroups. AMI, acute myocardial infarction; CABG, coronary artery bypass grafting; MT, medical therapy; PCI, percutaneous coronary intervention; SAP, stable angina pectoris; UAP, unstable angina pectoris. *Multivariable Cox regression was used to determine mortality risk of patients in low sodium tertile (≤ 139.0 mmol/L) compared with patients in high sodium tertile (> 141.0 mmol/L). †The interaction between sodium tertiles and each covariate was tested using multivariable Cox regression hazard model.
-
Since serum sodium level was more strongly associated with outcomes compared with serum chloride, tertiles of serum sodium level were combined with SYNTAX score for prediction of mortality to evaluate its incremental information. There was a modest but significant improvement for AUC values between the two prediction sets [SYNTAX score: 0.570 (0.552-0.588) vs. SYNTAX score with serum sodium level 0.586 (0.568-0.603), P = 0.011].
Study Population
Clinical Outcomes
Subgroup Analysis
Prognostic Value Assessment
-
In a large prospective cohort of patients with three-vessel coronary artery disease, we found that both serum chloride level and serum sodium level were prognostically similar in univariate analysis. However, when incorporated into the base model, only low sodium level remained to be associated with increased risks for all-cause and cardiac death. Although serum chloride level and serum sodium level were modestly correlated, there was no significant interaction for mortality prediction. Subgroup analysis revealed that the relationship of serum sodium level with all-cause death was relatively consistent across the subgroups. There was no significant interaction of serum sodium level with those covariates, suggesting that there was no true subgroup difference. Taken together, these findings indicate that low serum sodium level, rather than serum chloride level, is an independent predictor of mortality in patients with TVD.
TVD is common in patients with obstructive CAD[1, 2], with an almost 2-fold risk of mortality compared with single-vessel CAD[5]. SYNTAX Score is widely used to assess risk of adverse cardiac events in patients with TVD, but it showed only a modest predictability in previous studies as well as in our study[22, 23]. In this regard, SYNTAX score Ⅱ, in which clinical factors were included, has been developed to provide improved prognostic information[24]. But it showed only a moderate discrimination ability for long-term mortality prediction in patients with multivessel disease[25, 26]. Additional prognosis-associated clinical markers may add important information to SYNTAX score.
Previous studies reported that low serum sodium level was associated with mortality in patients with acute coronary syndromes[8-12], and was an independent predictor of adverse outcomes in diverse cardiovascular diseases[8, 13]. In the present study, we extended this finding to the setting of TVD. In addition, sodium level provided modest but significant prognostic information on top of SYNTAX score for prediction of mortality. This is of great importance because risk stratification can add in treatment decision and improve prognosis of patients.
A recent epidemiologic study suggested that mild hyponatremia even within the normal range of serum sodium level was associated with an increased risk for cardiovascular death[27]. Indeed, a more conservative definition of hyponatremia (< 139.0 mmol/L) has been suggested[28]. In support, we found that patients in the low tertiles group of serum sodium level (≤ 139.0 mmol/L) had significantly increased risk of mortality compared with those in the high tertiles group. Thus, low serum sodium level, even within the normal range, increases risk for mortality and requires prompt correction in patients with TVD.
A J or U curve was reported with respect to the association of serum sodium level with mortality[14, 27]. For example, hypernatremia was also associated with an increased risk for mortality compared with normal sodium level[29]. However, we found that patients in the high tertiles group of serum sodium level (> 141.0 mmol/L) had the lowest risk for mortality, with no evidence of a J or U curve. This might be related to the low numbers of patients (276; 12.6%) with serum sodium level > 145.0 mmol/L (hypernatremia), and only one patient with serum sodium level > 155 mmol/L (severe hypernatremia) in this high tertiles group.
The levels of serum sodium and chloride are tightly related with each other. High level of serum sodium is typically accompanied by high level of serum chloride, and vice versa. However, consistent with previous studies[16, 17], we found only a modest correlation of serum chloride level with serum sodium level (r < 0.5), suggesting that serum chloride and sodium levels might provide distinct predictive information. Assessment of serum chloride level was largely ignored until recent studies suggesting a stronger prognostic value than serum sodium level in HF patients and in MI patients complicated by systolic dysfunction[7, 15-17]. Thus, we evaluated the relationship of both serum chloride and sodium levels with long-term outcomes in patients with TVD. The prognostic value of serum chloride level diminished when serum sodium level was added into the multivariable model for all-cause death, suggesting that serum sodium level has a stronger association with long-term outcomes in patients with TVD compared with serum chloride level. Both low chloride level and low sodium level were associated with complex neurohormonal activation, including activation of the renin-angiotensin system[30, 31], which was associated with increased mortality in both HF patients and CAD patients[32-34]. Moreover, low serum chloride level was strongly associated with diuretic resistance[31, 35], a marker of poor decongestion and related to an increased risk for mortality in HF[36]. In the setting of TVD, however, diuretics were not used as often as that in HF[37]. This might partly explain why serum chloride level provided less prognostic information in TVD than that in HF.
The present study has several limitations. First, this was a registry-based observational study, with potential for selection bias that cannot be balanced with multivariable analysis. Second, all the patients in the study were recruited from a single specialized center for cardiovascular disease. Therefore, our findings might be population specific, especially the cut-off values among serum chloride and/or sodium level tertiles might differ in various populations. Third, medication information on diuretics, which could influence serum chloride and sodium levels, was not recorded in the database. Fourth, despite the strong association of low serum sodium level with mortality, the definite pathophysiology underlying this association still needs to be fully elucidated and further functional studies are required.
-
In patients with TVD, serum sodium level had a stronger association with long-term outcomes compared with serum chloride level, which was different from the setting of heart failure. Low serum sodium level (≤ 139.0 mmol/L) was an independent risk factor for mortality. Serum sodium level could provide modest improvement in discrimination for mortality prediction after adding it to SYNTAX score.
-
We thank all staff members for data collection, data entry, and monitoring as part of this study.
the Beijing Municipal Natural Science Foundation grant number 7181008
the CAMS Innovation Fund for Medical Sciences 2016-I2M-1-002
the CAMS Innovation Fund for Medical Sciences CAMS-I2M
the National Natural Science Foundation of China 81870286






 Quick Links
Quick Links
 DownLoad:
DownLoad: