-
Epidemiological studies have demonstrated that cigarette smoking (CS) is an independent risk factor for the development of atherosclerotic cardiovascular disease (ASCVD) and significantly contributes to the morbidity and mortality[1-3]. The effects of CS on cardiovascular system were reported to be doserelated[4], but fortunately, it has also been reported that smoking cessation can diminish the risk and improve the outcomes of ASCVD[5-6]. Importantly, the deleterious impact of CS on the cardiovascular system has been intensively examined, and its potential role has been suggested through multiple interrelated mechanisms, such as inflammation, vasomotor dysfunction, and lipid modifications[7-8]. For example, with regard to lipid metabolism, evidence shows that smokers always have an atherogenic lipid profile, with elevated levels of total cholesterol (TC), low-density lipoprotein (LDL) cholesterol (LDL-C) and triglyceride (TG) and attenuated levels of high-density lipoprotein (HDL) cholesterol (HDL-C)[9-12], suggesting a key role for smoking in lipid metabolism and ASCVD.
Recently, it has been proposed that lipoprotein particles can more accurately capture the atherogenic properties compared with cholesterol concentrations contained in the lipoproteins[13-16]. Previous studies have already indicated a negative impact of smoking on lipoprotein subfraction profiles, especially on HDL subfractions[17-19], even if there was no significant change in the serum levels of cholesterols[19]. The reversal impact of smoking cessation on lipid profile has also been documented in a meta-analysis[20]. However, there is not much information regarding the impact of smoking on lipoprotein subfractions, especially in individuals with smoking cessation. In addition, the mortality and morbidity of coronary artery disease (CAD) have rapidly increased in the young, which is paralleled with the elevated rate of current smoking in Chinese population[21]. This is also a reason due to which we performed the present study focusing on the impact of smoking status on the lipoprotein subfractions.
Apparently, intensive studies on the relationship between smoking and lipoprotein subfractions deepen the current understanding of the link between smoking and the risk of ASCVD[17]. Therefore, in the present study, we consecutively enrolled a relatively large Chinese cohort who were not under a lipid-lowering drug treatment and investigated the impact of current smoking on the distribution of lipid profile and lipoprotein subfractions.
-
The present study fully complied with the Declaration of Helsinki and was approved by the Ethics Committee of FuWai Hospital and Cardiovascular Institute, Beijing, China. All included patients provided prior written consent.
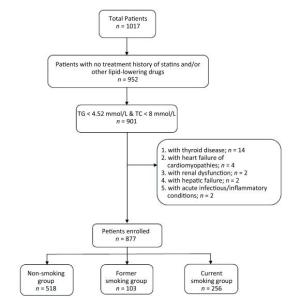
This study recruited consecutive 1017 patients with angina-like chest pain. The exclusion criteria: 1) aged < 18 years; 2) with a treatment history of statins and/or other lipid-lowering drugs prior to entering the study; 3) severe end-stage diseases, such as renal and/or liver dysfunction, heart failure, and malignant carcinoma; 4) systematic inflammatory disease or severe infection; 5) thyroid disorder; and 6) pregnancy. The flow chart of patient recruitment is shown in Figure 1.
Patients with complete data were assessed for medical history, baseline clinical features, and traditional cardiovascular risk factors, and the final 877 eligible patients were subjected to analysis. Smoking status was confirmed using a questionnaire at the lipid clinics and/or during hospitalization[22]. Current smoking was defined as people who smoked at least 100 cigarettes in lifetime and were continuing smoking at the time of interview. Former smoking was defined as those who smoked at least 100 cigarettes in lifetime but had quit smoking at the time of interview. Never smoking was defined as people who never smoked or who have smoked less than 100 cigarettes in lifetime[23]. Type 2 diabetes was diagnosed if the repeated fasting blood glucose (FPG) level was ≥ 7.0 mmol/L and/or non-FPG level was ≥ 11.1 mmol/L or if the subject was currently taking oral hypoglycemic agents or receiving insulin therapy. CAD was diagnosed by elective coronary angiography as least one major epicardial coronary artery (≥ 2 mm) having a diameter of stenosis ≥ 50%. Hypertension was defined as blood pressure measurement of ≥ 140/90 mmHg in multiple determinations under different environments or patients taking antihypertensive drugs although the blood pressure was normal. Patients were divided into nonsmoking (n = 518), former smoking (n = 103), and current smoking (n = 256) groups.
-
Fasting venous blood was obtained and collected into ethylenediaminetetraacetic acid (EDTA)-containing tubes and subsequently stored at-80 ℃ for the measurement of lipoprotein subfractions. Concentrations of traditional lipid parameters (TG, TC, LDL-C, and HDL-C) and glucose levels were measured by an automatic biochemistry analyzer (Hitachi 7150, Tokyo, Japan). Using the Lipoprint System (Quantimetrix Corporation, Redondo Beach, CA, USA) and referencing the manual that was described previously[8], electrophoretic technology was performed to analyze the lipoprotein subfractions. The HDL was divided into 10 sorts of subfractions, while the LDL was divided into 7 by this analysis[24]. For HDL, 1-3 subfractions indicate large HDL particles, 4-7 subfractions represent intermediate particles and 8-10 subfractions mean small particles[24]. Meanwhile, LDL subfraction 1 indicates large LDL particles, subfraction 2 represents intermediate particles and subfractions 3-7 mean small particles. Subsequently, the concentration (mg/dL) of each of the lipoprotein subfraction cholesterol and the proportion (%) of the lipoprotein subfractions besides the mean LDL particle size (Å) were determined.
-
SPSS version 19.0 (SPSS Inc., Chicago, IL, USA) was used for analyzing the present data. Continuous variables were presented as mean ± SD and categorical variables as number (percentage). The independent sample t-test or the Mann-Whitney U test was performed to analyze the differences in the clinical characteristics and lipid profiles between the two groups, wherever appropriate. Linear logistic regression analyses were performed for assessing the independent contributors from all lipoprotein subfractions. Statistical significance was defined as a two-tailed P value < 0.05.
-
The characteristics of the enrolled subjects are shown in Table 1. Compared with nonsmoking individuals and former smoking subjects, a significantly higher proportion of current smoking patients had the habit of alcohol consumption (40.2% vs. 21.4% vs. 10.1%, P < 0.001, Table 1). There were also significant differences among the three groups in terms of age, body mass index (BMI), gender, and morbidity of CAD (age: 55 ± 10 vs. 59 ± 10 vs. 56 ± 12 years, P = 0.003; BMI: 26.09 ± 3.48 vs. 26.03 ± 3.31 vs. 25.06 ± 3.56 kg/m2, P = 0.001; rate of male gender: 93.0% vs. 96.1% vs. 41.3%, P < 0.001; morbidity of CAD: 73.0% vs. 83.5% vs. 55.8%, P < 0.001; respectively, Table 1). Moreover, the HDL-C levels of CS patients were substantially low (1.01 ± 0.26 vs. 1.06 ± 0.32 vs. 1.17 ± 0.36 mmol/L, P < 0.001, Table 1), and the difference was significant (adjusted P value = 0.006) even after adjusting for traditional risk factors consisting of gender, age, BMI, alcohol consumption history, family history of CAD, systolic blood pressure, hemoglobin A1C (HbA1C), and CAD. The level of TG was elevated in current smoking patients (1.82 ± 0.81 vs. 1.64 ± 0.68 vs. 1.64 ± 0.79 mmol/L, P = 0.002, Table 1), but the increasing tendency disappeared after adjusting for traditional risk factors (adjusted P = 0.094). The difference in TC levels among the current smoking, former smoking, and nonsmoking groups was not statistically significant even after adjusting for traditional risk factors; in addition, the levels of LDL-C were almost equal among the three groups.
Table 1. Baseline Characteristics, Lipid Parameters, and Lipoprotein Subfractions in the Current Smoking and Nonsmoking Patients
Variables Non Smoking (n = 518) Former Smoking (n = 103) Current Smoking (n = 256) P Value Adjusted P Value Clinical Characteristics Male Gender [n (%)] 214 (41.3%) 99 (96.1%) 240 (93.0%) < 0.001 - Age (years) 56 ± 12 59 ± 10 55 ± 10 0.003 - BMI (kg/m2) 25.06 ± 3.56 26.03 ± 3.31 26.09 ± 3.48 0.001 - Drinking [n (%)] 52 (10%) 22 (21.4%) 103 (40.2%) < 0.001 - FH of CAD [n (%)] 81 (15.6%) 18 (17.5%) 46 (18.0%) 0.336 - Dislipidemia [n(%)] 281 (54.2%) 58 (56.3%) 148 (57.8%) 0.803 - Hypertension[n (%)] 279 (53.9%) 63 (61.2%) 155 (60.5%) 0.307 - Diabetes [n (%)] 95 (18.3%) 26 (25.2%) 56 (21.9%) 0.113 - CAD [n (%)] 289 (55.8%) 86 (83.5%) 187 (73%) < 0.001 - ACEI/ARB [n (%)] 97 (18.7%) 23 (22.3%) 42 (16.4%) 0.415 - β-blocker [n (%)] 84 (16.2%) 27 (26.2%) 57 (22.3%) 0.056 - CCB [n (%)] 93 (18.0%) 28 (27.2%) 54 (21.2%) 0.173 - Lipid Profiles TG (mmol/L) 1.64 ± 0.79 1.64 ± 0.68 1.82 ± 0.81 0.002 0.094 TC (mmol/L) 4.83 ± 0.92 4.65 ± 0.95 4.70 ± 0.87 0.046 0.554 HDL-C (mmol/L) 1.17 ± 0.36 1.06 ± 0.32 1.01 ± 0.26 < 0.001 0.006 LDL-C (mmol/L) 3.18 ± 0.87 3.12 ± 0.88 3.19 ± 0.87 0.707 - HDL subfractions Large HDL-C (mg/dL) 15.11 ± 7.84 13.10 ± 5.26 11.34 ± 5.19 < 0.001 0.002 Medium HDL-C (mg/dL) 21.22 ± 5.95 20.39 ± 6.73 19.47 ± 4.59 < 0.001 0.005 Small HDL-C (mg/dL) 7.85 ± 2.66 7.64 ± 3.09 8.40 ± 2.90 0.019 0.032 Large HDL (%) 32.85 ± 8.42 31.37 ± 6.95 28.21 ± 7.29 < 0.001 0.009 Medium HDL (%) 48.81 ± 5.25 49.75 ± 4.37 49.91 ± 4.17 0.063 0.552 Small HDL (%) 18.31 ± 5.67 18.86 ± 5.70 21.85 ± 6.21 < 0.001 0.001 LDL subfractions Large LDL-C (mg/dL) 27.82 ± 9.53 27.60 ± 9.35 26.51 ± 8.17 0.415 - Medium LDL-C (mg/dL) 17.84 ± 8.05 18.80 ± 7.98 20.19 ± 8.13 0.002 0.029 Small LDL-C (mg/dL) 6.24 ± 6.51 6.21 ± 6.55 8.22 ± 8.18 0.042 0.283 Large LDL (%) 14.93 ± 3.99 15.28 ± 3.83 14.69 ± 3.96 0.302 - Medium LDL (%) 9.43 ± 3.49 10.23 ± 3.12 10.87 ± 3.25 < 0.001 0.003 Small LDL (%) 3.27 ± 3.27 3.30 ± 3.36 4.27 ± 3.84 0.013 0.355 Mean LDL particle size (Å) 267.83 ± 4.90 267.60 ± 4.66 266.44 ± 4.89 0.008 0.285 Note. The data shown are the mean ± SD or n (%). Adjusted traditional risk factors include gender, age, BMI, alcohol consumption history, family history of CAD, systolic blood pressure, HbA1C, and CAD. BMI = body mass index; CAD = coronary artery disease; ACEI = angiotensin converting enzyme inhibitors; ARB = angiotensin receptor blockers; CCB = calcium channel blockers; FH = family history; HbA1C = hemoglobin A1C; TG = triglyceride; TC = total cholesterol; HDL-C = high-density lipoprotein cholesterol; LDL-C = low-density lipoprotein cholesterol. -
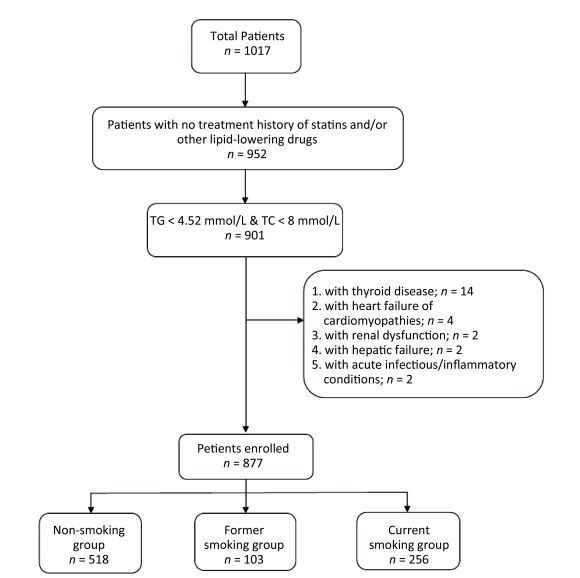
Lipoprotein subfractions were measured in 256 current smoking patients, 103 former smoking patients and 518 nonsmoking individuals. To demonstrate the changes clearly, we elected the typical figure of HDL and LDL subfractions from nonsmoking group, former smoking group, and current smoking group respectively (Figure 2).

Figure 2. The distribution of lipoprotein subfractions in typical patients from the nonsmoking group (A: HDL subfractions; B: LDL subfractions), former smoking group (C: HDL subfractions; D: LDL subfractions), and current smoking group (E: HDL subfractions; F: LDL subfractions)
As shown in Table 1 and Figure 3, compared with the nonsmoking and former smoking groups, in the unadjusted analysis, the current smoking group presented a significant reduction in large HDL-C subfraction concentration and percentage and in medium HDL-C concentration (15.11 ± 7.84 vs. 13.10 ± 5.26 vs. 11.34 ± 5.19 mg/dL, P < 0.001, after adjusted P = 0.002; 32.85% ± 8.42% vs. 31.37% ± 6.95% vs. 28.21% ± 7.29%, P < 0.001, after adjusted P = 0.009; 21.22 ± 5.95 vs. 20.39 ± 6.73 vs. 19.47 ± 4.59 mg/dl, P < 0.001, after adjusted P = 0.005; respectively); nevertheless, the small HDL subfraction concentration and percentage were distinctly higher (7.85 ± 2.66 vs. 7.64 ± 3.09 vs. 8.40 ± 2.90 mg/dL, P = 0.019, after adjusted P = 0.032; 18.31% ± 5.67% vs. 18.86% ± 5.70% vs. 21.85% ± 6.21%, P < 0.001, after adjusted P = 0.001, respectively). Table 1 also indicates that compared with nonsmoking individuals and former smoking subjects, the medium LDL-C concentration and percentage were significantly higher in the current smoking patients (17.84 ± 8.05 vs. 18.80 ± 7.98 vs. 20.19 ± 8.13 mg/dL, P = 0.002, after adjusted P = 0.029; 9.43% ± 3.49% vs. 10.23% ± 3.12% vs. 10.87% ± 3.25%, P < 0.001, after adjusted P = 0.003; respectively). Moreover, the results demonstrate that the mean LDL particle size of current smoking patients showed a decreasing tendency (267.83 ± 4.90 vs. 267.60 ± 4.66 vs. 266.44 ± 4.89 Å, P = 0.008) while the small LDL-C concentration and small LDL percentage showed increasing tendencies (6.24 ± 6.51 vs. 6.21 ± 6.55 vs. 8.22 ± 8.18 mg/dL, P = 0.042; 3.27% ± 3.27% vs. 3.30% ± 3.36% vs. 4.27% ± 3.84%, P = 0.013; respectively), but these tendencies disappeared after adjusting for traditional risk factors. However, no significant difference was observed among the other lipoprotein subfractions in the three groups.
-
The changes in the lipoprotein subfractions, the influencing factors, and interventions are of novel interest in lipid-related research field. The present relatively large cross-sectional study demonstrated a significant increase in medium LDL subfraction percentage, medium LDL-C and small HDL-C concentrations, and small HDL subfraction percentage but a notable decrease in large HDL-C concentration, medium HDL-C concentration, and HDL subfraction percentage among CS individuals, which were closer to the atherogenic subfraction pattern compared with the nonsmoking and former smoking individuals. More interestingly, the analysis also suggested that smoking cessation could attenuate the above mentioned worse pattern of lipoprotein subfractions but not completely reverse these changes (not shown in table). Thus, our data highlight an important pathophysiological role of smoking in the changes of lipoprotein particles, which may be valuable for future prevention and intervention of ASCVD.
Previous studies have suggested that lipoprotein subfractions composed of lipoprotein particles were heterogeneous; in other words, and groups of subfractions had different size, density, and functions[25-26]. Thus, the lipoprotein related risks might be explained more clearly by the lipoprotein subfractions. The features and functions of lipoprotein subfractions were found to be changed in the status of ASCVD, diabetes, hypertension, or inflammation[22, 27-29]. In a recent study on 413 Chinese Han subjects with CAD, the authors found that small HDL and LDL subfractions were positively associated with the presence of CAD[24].
Although the relationship between smoking and ASCVD has been well documented, the mechanisms by which smoking increases ASCVD risk seems to be multifactorial and incompletely understood. Based on the previous studies and clinical trials[7-8], the potential links between smoking and the increased risk of ASCVD cover the pathways, including inflammation, systemic hemostatic and coagulatory dysfunctions, oxidative stress, and dyslipidemia (in particular, lipoprotein and lipoprotein subfractions). Indeed, a previous study strongly suggested that CS was associated with reductions in HDL-C and mild increase in TG[9]. In the present study, coincident with the previous study, the data indicated that CS patients showed a significant decrease in HDL-C levels and an elevated tendency of TG levels compared to those in nonsmoking individuals. In addition to the changes in HDL-C and TG levels, CS patients had frequently higher plasma levels of TC and LDL-C[10-11], although our study failed to test this change due to unknown reasons, but the result was similar to a study on male subjects with chronic smoking[19].
Moreover, few studies have focused on the impacts of current smoking on lipoprotein subfractions. Beauchamp A et al. studied 612 participants using nuclear magnetic resonance spectroscope techniques and found that the mean total LDL particle concentration was higher, while the total HDL and large HDL particle concentrations were lower in female smokers than in nonsmokers. They concluded that female smokers have a more atherogenic lipoprotein profile than that of nonsmokers, but they did not observe any significant difference among males[19]. Another small sample size study (n = 46) from Japan on the effects of smoking on HDL-C subfractions in young women showed significantly lower HDL2-C levels[30], which was similar to the observation reported by Moffatt RJ et al[31]. In our large sample size study, on untreated patients, the data suggested that CS patients had attenuated medium-and elevated small-HDL particles besides the lower levels of large HDL and higher levels of medium LDL subfractions. This change in the lipoprotein subfractions in our study may be more important for triggering ASCVD because the large HDL subfractions have been supposed to be antiatherosclerotic agents, whereas the small subfractions were supposed to be atherogenic agents[32]. Based on these findings including ours, the data strongly indicated that CS was an overt trigger for the perturbation of lipoprotein subfractions, which might increase the atherogenic potential.
Several studies have demonstrated that smoking cessation could reverse the lipid changes, in particular, the changes in HDL-C levels[17-20]. However, only two studies had examined the effects of smoking cessation on the distribution of lipoprotein subfractions. A prospective study carried out by Beauchamp A et al. indicated that former smokers had larger HDL and lower medium LDL particle concentrations than those of current smokers in female subjects[19]. Gepner AD et al.[17] found that smoking cessation could improve large HDL particles especially in women. Apparently, these studies suggested reverse effects of smoking on these lipoprotein subclasses. Similarly, the present study, using the Lipoprint System, showed remarkable reversing effects on the distribution of lipoprotein subfractions after smoking cessation. Though a non significant increase in the level of HDL-C in smoking cessation subjects was found, an increase in large HDL particles and a decrease in small particles were detected, suggesting a potential attenuation in ASCVD risk. More importantly, the present data clearly showed that the reversions of HDL subfractions by smoking cessation were partial. Furthermore, the data showed that the small LDL subfractions were lower and the mean size of LDL particles were larger in former smoking patients than those in current smoking subjects but were similar to those in nonsmokers.
In this cross-sectional study on untreated patients with angina-like chest pain, we illustrated the changes in the lipoprotein subfractions in different smoking status. Compared with nonsmokers and former smokers, current smoking patients manifested a more atherogenic lipoprotein subfraction profile that was primarily reflected by the decrease in large HDL particles and the increase in small particles. The negative effects of smoking on lipoprotein subfractions could be reversed to some degree by smoking cessation. Hence, our data provided additional information concerning the relationship between CS and ASCVD and strongly suggested a benefit on lipoprotein subfractions through smoking cessation.
-
The present study certainly exhibit several limitations. First, since this was a cross-sectional study on the Chinese Han cohort who were not under a lipid-lowering therapy from a single center, a long-term follow-up should be carried out. Second, smoking was self-reported, and other behaviors such as sedentary and unhealthy dietary habits were not considered in this study, which might cause a bias. In additional, there are different measurements of lipoprotein subfractions; thus, other methods might produce different results. Moreover, the subjects enrolled in the present study included only a small proportion of women, and thus the sexual differences cannot be delineated in our data. Furthermore, we did not analyze the dose-dependent effect of smoking and time course of smoking cessation, which is also another limitation of our study. Finally, selecting the subjects with angina-like chest pain in this study might increase the potential confounding factor, thereby influencing results.
doi: 10.3967/bes2017.033
Impact of Smoking Status on Lipoprotein Subfractions: Data from an Untreated Chinese Cohort
-
Abstract:
Objective Cigarette smoking is one of the established risk factors of atherosclerotic cardiovascular disease, however, its impact on lipids is not completely understood, especially in the Chinese population. Therefore, this study evaluated the impact of smoking status (non, former, and current smoking) on the distribution of lipoprotein subfractions in untreated patients with angina-like chest pain. Methods A total of 877 patients were consecutively enrolled and divided into nonsmoking (n = 518), former smoking (n = 103), and current smoking (n = 256) groups. Both low-and high-density lipoprotein cholesterol (LDL-C and HDL-C) subfractions were measured using the Quantimetrix Lipoprint System. The distributions of lipoprotein subfractions were evaluated among the groups. Results Compared with nonsmoking subjects, the current smoking group had significantly lower large/medium HDL-C (both P < 0.001) concentration and large HDL subfraction percentage but higher small HDL-C and medium LDL-C concentrations as well as medium LDL subfraction percentage. Importantly, former smoking subjects showed elevated levels of large HDL-C concentration, large HDL particle percentage, and mean LDL particle size and attenuation in small HDL/LDL percentages and small LDL-C concentration, but these levels did not reach the optimal status compared with those of the non-smoking group (data not shown). Conclusion Smoking has an adverse impact on the lipoprotein subfractions, presented as lower large HDL particles besides higher small HDL and medium LDL particles, whereas smoking cessation could reverse these change to a certain degree. -
Key words:
- Smoking /
- Smoking cessation /
- Lipoprotein subfractions /
- Chinese
注释:1) Conflict of interest: -
Table 1. Baseline Characteristics, Lipid Parameters, and Lipoprotein Subfractions in the Current Smoking and Nonsmoking Patients
Variables Non Smoking (n = 518) Former Smoking (n = 103) Current Smoking (n = 256) P Value Adjusted P Value Clinical Characteristics Male Gender [n (%)] 214 (41.3%) 99 (96.1%) 240 (93.0%) < 0.001 - Age (years) 56 ± 12 59 ± 10 55 ± 10 0.003 - BMI (kg/m2) 25.06 ± 3.56 26.03 ± 3.31 26.09 ± 3.48 0.001 - Drinking [n (%)] 52 (10%) 22 (21.4%) 103 (40.2%) < 0.001 - FH of CAD [n (%)] 81 (15.6%) 18 (17.5%) 46 (18.0%) 0.336 - Dislipidemia [n(%)] 281 (54.2%) 58 (56.3%) 148 (57.8%) 0.803 - Hypertension[n (%)] 279 (53.9%) 63 (61.2%) 155 (60.5%) 0.307 - Diabetes [n (%)] 95 (18.3%) 26 (25.2%) 56 (21.9%) 0.113 - CAD [n (%)] 289 (55.8%) 86 (83.5%) 187 (73%) < 0.001 - ACEI/ARB [n (%)] 97 (18.7%) 23 (22.3%) 42 (16.4%) 0.415 - β-blocker [n (%)] 84 (16.2%) 27 (26.2%) 57 (22.3%) 0.056 - CCB [n (%)] 93 (18.0%) 28 (27.2%) 54 (21.2%) 0.173 - Lipid Profiles TG (mmol/L) 1.64 ± 0.79 1.64 ± 0.68 1.82 ± 0.81 0.002 0.094 TC (mmol/L) 4.83 ± 0.92 4.65 ± 0.95 4.70 ± 0.87 0.046 0.554 HDL-C (mmol/L) 1.17 ± 0.36 1.06 ± 0.32 1.01 ± 0.26 < 0.001 0.006 LDL-C (mmol/L) 3.18 ± 0.87 3.12 ± 0.88 3.19 ± 0.87 0.707 - HDL subfractions Large HDL-C (mg/dL) 15.11 ± 7.84 13.10 ± 5.26 11.34 ± 5.19 < 0.001 0.002 Medium HDL-C (mg/dL) 21.22 ± 5.95 20.39 ± 6.73 19.47 ± 4.59 < 0.001 0.005 Small HDL-C (mg/dL) 7.85 ± 2.66 7.64 ± 3.09 8.40 ± 2.90 0.019 0.032 Large HDL (%) 32.85 ± 8.42 31.37 ± 6.95 28.21 ± 7.29 < 0.001 0.009 Medium HDL (%) 48.81 ± 5.25 49.75 ± 4.37 49.91 ± 4.17 0.063 0.552 Small HDL (%) 18.31 ± 5.67 18.86 ± 5.70 21.85 ± 6.21 < 0.001 0.001 LDL subfractions Large LDL-C (mg/dL) 27.82 ± 9.53 27.60 ± 9.35 26.51 ± 8.17 0.415 - Medium LDL-C (mg/dL) 17.84 ± 8.05 18.80 ± 7.98 20.19 ± 8.13 0.002 0.029 Small LDL-C (mg/dL) 6.24 ± 6.51 6.21 ± 6.55 8.22 ± 8.18 0.042 0.283 Large LDL (%) 14.93 ± 3.99 15.28 ± 3.83 14.69 ± 3.96 0.302 - Medium LDL (%) 9.43 ± 3.49 10.23 ± 3.12 10.87 ± 3.25 < 0.001 0.003 Small LDL (%) 3.27 ± 3.27 3.30 ± 3.36 4.27 ± 3.84 0.013 0.355 Mean LDL particle size (Å) 267.83 ± 4.90 267.60 ± 4.66 266.44 ± 4.89 0.008 0.285 Note. The data shown are the mean ± SD or n (%). Adjusted traditional risk factors include gender, age, BMI, alcohol consumption history, family history of CAD, systolic blood pressure, HbA1C, and CAD. BMI = body mass index; CAD = coronary artery disease; ACEI = angiotensin converting enzyme inhibitors; ARB = angiotensin receptor blockers; CCB = calcium channel blockers; FH = family history; HbA1C = hemoglobin A1C; TG = triglyceride; TC = total cholesterol; HDL-C = high-density lipoprotein cholesterol; LDL-C = low-density lipoprotein cholesterol. -
[1] Lioyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics-2010 update: a report from the American Heart Association. Circulation, 2010; 121, e46-e215. doi: 10.1161/CIRCULATIONAHA.109.192667 [2] Doll R, Peto R, Boreham J, et al. Mortality in the relation to smoking: 50 years' observations on the male British doctors. BMJ, 2004; 328, 1519. doi: 10.1136/bmj.38142.554479.AE [3] Freund KM, Belanger AJ, D'Agostino RB, et al. The health risks of smoking. The Framingham Study: 34 years of follow-up. Ann Epidemiol, 1993; 3, 417-24. doi: 10.1016/1047-2797(93)90070-K [4] Celermajer DS, Sorensen KE, Georgakopoulos D, et al. Cigarette smoking is associated with dose-related and potentially reversible impairment of endothelium-dependent dilation in healthy young adults. Circulation, 1993; 88, 2149-55. doi: 10.1161/01.CIR.88.5.2149 [5] Rosenberg L, Kaufman DW, Helmrich SP, et al. The risk of myocardial infarction after quitting smoking in men under 55 years of age. N Engl J Med, 1985; 13, 1511-4. https://www.ncbi.nlm.nih.gov/pubmed/4069159 [6] Rosenberg L, Palmer JR, Shapiro S. Decline in the risk of myocardial infarction among women who stop smoking. N Engl J Med, 1990; 322, 213-7. doi: 10.1056/NEJM199001253220401 [7] Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol, 2004; 43, 1731-7. doi: 10.1016/j.jacc.2003.12.047 [8] Benowitz NL. Cigarette smoking and cardiovascular disease: pathophysiology and implication for treatment. Prog Cardiovasc Dis, 2003; 46, 91-111. doi: 10.1016/S0033-0620(03)00087-2 [9] Craig WY, Palomaki GE, Haddow JE. Cigarette smoking and serum lipid and lipoprotein concentrations: an analysis of published data. BMJ, 1989; 298, 784-8. doi: 10.1136/bmj.298.6676.784 [10] Mjos OD. Lipid effects and smoking. Am Heart J, 1988; 115, 272-5. doi: 10.1016/0002-8703(88)90649-7 [11] Criqui MH, Wallace RB, Heiss G, et al. Cigarette smoking and plasma high-density lipoprotein cholesterol: The Lipid Research Clinics Program Prevalence Study. Circulation, 1980; 62, IV70-6. https://uncch.pure.elsevier.com/en/publications/cigarette-smoking-and-plasma-high-density-lipoprotein-cholesterol [12] Athyros VG, Katsiki N, Doumas M, et al. Effect of tobacco smoking and smoking cessation on plasma lipoproteins and associated major cardiovascular risk factors: a narrative review. Curr Med Res Opin, 2013; 29, 1263-74. doi: 10.1185/03007995.2013.827566 [13] Xu RX, Li S, Li XL, et al. High-density lipoprotein subfractions in relation with the severity of coronary artery disease: a Gensini score assessment. J Clin Lipidol, 2015; 9, 26-34. doi: 10.1016/j.jacl.2014.11.003 [14] Martin SS, Khokhar AA, May HT, et al. HDL cholesterol subclasses, myocardial infarction, and mortality in secondary prevention: the Lipoprotein Investigators Collaborative. Eur Heart J, 2015; 36, 22-30. doi: 10.1093/eurheartj/ehu264 [15] Mikhailidis DP, Elisaf M, Rizzo M, et al. "European panel on low density lipoprotein (LDL) subclasses": a statement on the pathophysiology, atherogenicity and clinical significance of LDL subclasses: executive summary. Curr Vasc Pharmacol, 2011; 9, 531-2. doi: 10.2174/157016111796642698 [16] Mikhailidis DP, Elisaf M, Rizzo M, et al. "European panel on low density lipoprotein (LDL) subclasses": a statement on the pathophysiology, atherogenicity and clinical significance of LDL subclasses. Curr Vasc Pharmacol, 2011; 9, 533-71. doi: 10.2174/157016111796642661 [17] Gepner AD, Piper ME, Johnson HM, et al. Effects of smoking and smoking cessation on lipids and lipoproteins: Outcomes from a randomized clinical trial. Am Heart J, 2011; 161, 145-51. doi: 10.1016/j.ahj.2010.09.023 [18] Gossett LK, Johnson HM, Piper ME, et al. Smoking intensity and lipoprotein abnormalities in active smokers. J Clin Lipidol, 2009; 3, 372-8. doi: 10.1016/j.jacl.2009.10.008 [19] Beauchamp A, Tonkin A, Peeters A, et al. Associations among smoking status, lifestyle and lipoprotein subclasses. J Clin Lipidol, 2010; 4, 522-30. doi: 10.1016/j.jacl.2010.09.003 [20] Maeda K, Noguchi Y, Fukui T. The effects of cessation from cigarette smoking on the lipid and lipoprotein profiles: A meta-analysis. Prev Med, 2003; 37, 283-90. doi: 10.1016/S0091-7435(03)00110-5 [21] Vedanthan R, Seligman B, Fuster V, et al. Global perspective on acute coronary syndrome: a burden on the young and poor. Circ Res, 2014; 114, 1959-75. doi: 10.1161/CIRCRESAHA.114.302782 [22] Cotes JE, Chinn DJ. MRC questionnaire (MRCQ) on respiratory symptoms. Occup Med (Lond), 2007; 57, 388. doi: 10.1093/occmed/kqm051 [23] National health interview survey: adult tobacco use information. Centers for Disease Control and Prevention. https://www.cdc.govchshis/tobacco/tobacco_glossary.htm [24] Xu RX, Zhang Y, Ye P, et al. Analysis of lipoprotein subfractions in Chinese Han patients with stable coronary artery disease. Heart Lung Circ, 2015; 24, 1203-10. doi: 10.1016/j.hlc.2015.05.002 [25] Superko HR, Pendyala L, Williams PT, et al. High-density lipoprotein subclasses and their relationship to cardiovascular disease. Lipidol, 2012; 6, 496-523. doi: 10.1016/j.jacl.2012.03.001 [26] Vandermeersch A, Ameye S, Puype D, et al. Estimation of the low-density lipoprotein (LDL) subclass phenotype using a direct, automated assay of small dense LDL-cholesterol without sample pretreatment. Clin Chim Acta, 2010; 411, 1361-6. doi: 10.1016/j.cca.2010.05.038 [27] Mackey RH, Mora S, Bertoni AG, et al. Lipoprotein particles and incident type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis. Diabetes Care, 2015; 38, 628-36. [28] Zhang Y, Li S, Xu RX, et al. Distribution of high-density lipoprotein subfractions and hypertensive status: A cross-sectional study. Medicine, 2015; 94, e1912. doi: 10.1097/MD.0000000000001912 [29] Corsetti JP, Gansevoort RT, Sparks CE, et al. Inflammation reduces HDL protection against primary cardiac risk. Invest, 2010; 40, 483-9. http://www.ncbi.nlm.nih.gov/pubmed/20412290 [30] Imamura H, Teshima K, Miyamoto N, et al. Cigarette smoking, high-density lipoprotein cholesterol subfractions, and lecithin: Cholesterol acyltransferase in young women. Metabolism, 2002; 51, 1313-6. doi: 10.1053/meta.2002.34040 [31] Moffatt RJ, Chelland SA, Pecott DL, et al. Acute exposure to environmental tobacco smoke reduces HDL-C and HDL2-C. Prev Med, 2004; 38, 637-41.32.Kontush A. HDL particle number and size as predictors of cardiovascular disease. Front Pharmacol, 2015; 6, 218. doi: 10.1016/j.ypmed.2003.12.002 [32] Kontush A. HDL particle number and size as predictors of cardiovascular disease. Front Pharmacol, 2015; 6, 218. doi: 10.3389/fphar.2015.00218/pdf -




 下载:
下载:




 Quick Links
Quick Links