-
Evidence is lacking regarding the combined effects of smoking and obesity on mortality due to coronary heart disease (CHD) in male veterans. This is the first veteran cohort study in Chinese military. Cardiovascular disease (CVD) is a leading cause of death globally, contributing to more than 17 million deaths in 2017, of which mortality from CHD is the most prevalent[1]. The morbidity of CHD in the United States is high, with 300,000 to 400,000 sudden cardiac death cases per year. In China, CHD has been shown to be a main threat to human health[2]. The morbidity of CHD in China was relatively lower than that in Western countries; however, due to the huge population base, was about 23 million CHD cases were reported in China in 2016[3].
Apart from the proven risk factors (age, diabetes mellitus, and insulin resistance), some blood parameters, for example, Apolipoprotein B, apolipoprotein AI, apolipoprotein B/apolipoprotein AI[4], lipoprotein A[5], high fibrinogen acidosis[6], neopterin[7], and adiponectin[8], are also associated with CHD. Other independent risk factors include ankle arm index[9], depression[10], and left ventricular hypertrophy[11]. Among those, smoking is one of the major traditional risk factors for coronary heart disease. Doll and Hill first studied the association between smoking and mortality due to relevant diseases[12]. Their study, which established smoking as an independent risk factor for death, also became a classical cohort epidemiological study because of the high-quality experimental design. Cigarette smoking plays an important role in the onset of acute coronary thrombosis, which causes the majority of sudden cardiac deaths and myocardial infarctions[13]. The mechanism involved includes vascular inflammation, platelet coagulation, vascular dysfunction, and oxidation of low-density lipoprotein cholesterol[14, 15]. Epidemiological, animal, and clinical evidence showed that smoking was not only an independent factor for CHD, but also has combined effect with other factors such as high blood pressure and high cholesterol[16]. In addition, with obesity, there is a higher risk of CHD. Several studies have examined the risk of mortality associated with obesity in nonsmokers[17, 18]. However, only limited data on the magnitude of CHD mortality risk about overweight individuals, who are also former or current smokers, exist.
Currently, evidence of most cohort studies only focused on single factor effect, while evidence on the combined effect of multi-factors is lacking. Additionally, some case control studies with in-hospital patients, are not representative of the general population[19]. Therefore, the present study aimed to clarify the combined effect of smoking and obesity on CHD mortality risk based on a cohort data collected from 1987 to 2016.
-
Ethics approval was obtained from the ethics committee of Xijing Hospital (Xi’an, Shaanxi Province, China). All experiments and study procedures were performed in accordance with the relevant guidelines and regulations, including any relevant details. Informed consent was obtained from each participant. Veterans were recruited from 22 veteran centers in Xi’an (Shaanxi Province, China) from February 1, 1987 to October 30, 2016. The inclusion criteria were male sex, age ≥ 55 years, registered veterans, able to complete the investigations and tests during the study duration, and provision of voluntary informed consent.
-
Each subject was surveyed by trained interviewers (professional clinicians at the veteran centers) for information on age, lifestyle (smoking, drinking, sport activities), and medical history (CHD, hypertension, cerebral stroke, diabetes). The subjects’ physiological parameters, including height, weight, blood pressure, serum cholesterol (enzymatic assay) and triglyceride (acetylacetone assay) were also recorded. Body mass index (BMI), calculated as weight divided height squared (kg/m2), was further categorized into underweight (< 18.5 kg/m2), normal weight (18.5 to 24.0 kg/m2), overweight (24.0 to 28.0 kg/m2), or obesity (fat) (≥ 28.0 kg/m2). Negative affairs in this study included divorce, widowhood, childlessness, social reduction, psychosomatic disorders, and property loss. Past medical history included CHD, hypertension, stroke, and diabetes mellitus.
According to the published 1997 World Health Organization (WHO) criteria, smoking is defined as the consumption of at least one cigarette per day and a smoking history of longer than 1 year. Current smokers were defined as those who were currently smoking while former smokers were defined as those that have discontinued smoking for at least 2 years at the time of the baseline survey. Smoking index (SI) = number of cigarettes per day × duration of smoking. Hypertension was diagnosed as systolic blood pressure of at least 18.7 kPa (140 mmHg) or diastolic blood pressure of at least 12 kPa (90 mmHg) without any anti-hypertension medication. The cause of death was determined from the death certificates or medical records (from a hospital that is at least at municipal level) and was verified by two senior clinicians at Xijing Hospital (Xi’an, Shaanxi Province, China). All deaths were encoded following the WHO International Classification of Diseases (10th version).
-
All information was blindly input into the Foxbase database by two staff separately to check for errors. After cleaning, the data were then converted and analyzed using Statistical Analysis System (SAS 9.3; SAS Institute Inc., NC, USA). Age (years) was categorized into ‘< 60’, ‘60–64’, ‘65–69’, and ‘≥ 70’. The hazard ratio (HR) of each factor and the 95% confidence interval (95% CI) were calculated using a multivariate Cox proportional hazard model and the proportional hazard assumptions were checked using Schoenfeld residuals. To present much stronger association between potential risk factors and CHD deaths, continuous variables were first entered into the multivariate analysis model. After that, important categorical risk factors (age, smoking index, BMI, and systolic blood pressure) were analyzed to further explore correlations. Significant variables with a P value of ≤ 0.05 in univariate analysis were then entered into the multivariate model. However, based on previous evidence, duration of smoking years, alcohol intake, exercise, negative affairs, and total cholesterol were retained in the model regardless of their univariate results. The log-rank statistic was used to compare Kaplan-Meier curves. All statistical analyses were performed using SPSS 23.0 software (Authorization No.6b4543b2xxxxf3c69a68). All P values were two-sided and statistical significance was defined as P < 0.05.
-
During the 24,394.21 person-years of follow-up, 889 deaths, including 192 (21.60%) CHD deaths, were recorded. The adjusted death rate was 3,644 per 100,000 person-years over an observed mean person-years of 19.24. At baseline, the subjects in this cohort study were all older than 50 years, with a mean age of 62.55 ± 5.19 years. In addition, 363 alive and 16 lost-to-follow-up participants were registered.
-
As shown in Table 1, using a Cox proportional hazard model, the results showed that in the univariate analysis, age, BMI, systolic blood pressure, diastolic blood pressure, triglyceride, duration of smoking year, history of hypertension, and diabetes were associated with CHD death. The HR (95% CI) for these factors were 1.122 (1.092–1.152), 1.096 (1.045–1.150), 1.022 (1.015–1.030), 1.020 (1.007–1.033), 1.002 (1.000–1.004), 1.010 (1.001–1.018), 2.664 (1.988–3.570), and 2.736 (1.701–4.403), respectively. After adjusting for age (years), systolic blood pressure, diastolic blood pressure, total cholesterol, triglyceride, alcohol intake, exercise, negative affairs, and past medical history (of CHD, hypertension, cerebral vascular sclerosis, and DM), the HR (95% CI) for BMI and duration of smoking in years were 1.051 (1.000–1.104) and 1.009 (1.000–1.017), respectively.
Table 1. Risk factors for CHD-related deaths at baseline
Variables Univariate analysis Multivariate analysis HR (95% CI) P value aHR (95% CI) P value Age (years) 1.122 (1.092–1.152) < 0.0001 1.108 (1.076–1.142) < 0.0001 Body mass index (kg/m2) 1.096 (1.045–1.150) 0.0002 1.051 (1.000–1.104) 0.0491 Systolic pressure (mmHg) 1.022 (1.015–1.030) < 0.0001 1.012 (1.000–1.024) 0.0472 Diastolic pressure (mmHg) 1.020 (1.007–1.033) 0.0028 0.997 (0.978–1.017) 0.7812 Total cholesterol (mg/dL) 1.002 (0.999–1.005) 0.1925 1.001 (0.997–1.004) 0.7140 Triglyceride (mg/dL) 1.002 (1.000–1.004) 0.0412 1.001 (0.999–1.003) 0.3739 Alcohol intake 1.005 (0.746–1.355) 0.9718 0.902 (0.661–1.231) 0.5157 Exercise 0.756 (0.535–1.068) 0.1125 0.811 (0.570–1.154) 0.2441 Negative affairs 1.312 (0.894–1.926) 0.1655 0.981 (0.661–1.458) 0.9262 Smoking related factors Duration of smoking (years) 1.010 (1.001–1.018) 0.0285 1.009 (1.000–1.017) 0.0574 Duration of quitting smoking (years) 0.998 (0.995–1.001) 0.2024 Cigarettes per day 1.006 (0.991–1.021) 0.4378 Smoking Index 1.000 (1.000–1.001) 0.0862 Family history (Yes/No) Hypertension 1.202 (0.764–1.892) 0.4254 Stroke 1.202 (0.764–1.892) 0.4254 CHD 1.410 (0.904–2.199) 0.1294 Past medical history (Yes/No) CHD 1.857 (1.386–2.488) < 0.0001 1.071 (0.771–1.487) 0.6818 Stroke 1.671 (0.533–5.235) 0.3783 Hypertension 2.664 (1.988–3.570) < 0.0001 1.711 (1.192–2.456) 0.0036 Cerebral vascular sclerosis (CVS) 2.114 (1.481–3.018) < 0.0001 1.314 (0.891–1.937) 0.1677 Hyperlipidemia (HLP) 0.864 (0.356–2.101) 0.7475 Diabetes Mellitus (DM) 2.736 (1.701–4.403) < 0.0001 2.126 (1.301–3.475) 0.0026 Note. Adjusted for age (years), body mass index, systolic pressure, diastolic pressure, total cholesterol, triglyceride, alcohol intake, exercise, negative affairs, duration of smoking years, and past medical history (of coronary heart disease [CHD], hypertension, cerebral vascular sclerosis [CVS], diabetes mellitus [DM]). HR, hazard ratio; CI, confidence interval; aHR, adjusted hazard ratio. Table 2 shows the multivariate results of the categorical variables. Individuals aged ≥ 60 years had a significantly increased risk of mortality compared to those aged ≤ 59 years at baseline (60–64 years, adjusted HR [aHR]: 2.072, 95% CI: 1.393–3.082; 65–69 years, aHR: 3.627, 95% CI: 2.338–5.628; and ≥ 70 years, aHR: 5.787, 95% CI: 3.312–10.111). In addition, risk factors associated with CHD mortality were smoking status with current smokers (aHR: 1.552, 95% CI: 1.074–2.243), and BMI ≥ 28 kg/m2 (aHR: 1.625, 95% CI: 1.024–2.581). The adjusted factors included age, systolic pressure, BMI, total cholesterol, triglyceride, smoking status, alcohol intake, exercise, negative affairs, and past medical history.
Table 2. Multivariate analysis for risk factors of mortality from CHD at baseline
Item Number of deaths/
total numberObserved person year/
total observed person yearHR 95% CI P value Age (years) < 60 39/402 744.9/9314.58 Reference 60–64 77/473 1352.8/9248.83 2.072 1.393–3.082 0.0003 65–69 52/250 894.5/4108.92 3.627 2.338–5.628 < 0.0001 ≥ 70 24/143 244.1/1721.87 5.787 3.312–10.111 < 0.0001 Smoking status Never smokers 59/388 1070.5/7982.74 Reference Former smokers 66/461 1165.9/8653.68 0.904 0.622–1.314 0.5966 Current smokers 67/419 1000.0/7757.80 1.552 1.074–2.243 0.0192 BMI (kg/m2) < 18.5 2/39 6.0/590.60 0.648 0.156–2.684 0.5497 18.5–24.0 61/511 1086.7/10056.88 Reference 24.0–28.0 100/587 1643.9/11309.57 1.339 0.966–1.858 0.0798 ≥ 28.0 29/131 499.9/2437.16 1.625 1.024–2.581 0.0395 Systolic pressure (mmHg) < 120 37/300 667.5/6243.15 Reference 120–129 43/381 782.1/7718.01 0.696 0.443–1.094 0.1160 130–139 33/207 520.9/3778.99 1.078 0.661–1.759 0.7636 ≥ 140 79/380 1265.9/6654.06 1.221 0.785–1.899 0.3767 Note. Adjusted for age, systolic blood pressure, body mass index (BMI), total cholesterol, triglyceride, smoking status, alcohol intake, exercise, negative affairs, past medical history (of coronary heart disease [CHD], hypertension, stroke, diabetes mellitus [DM]). HR, hazard ratio; CI, confidence interval. -
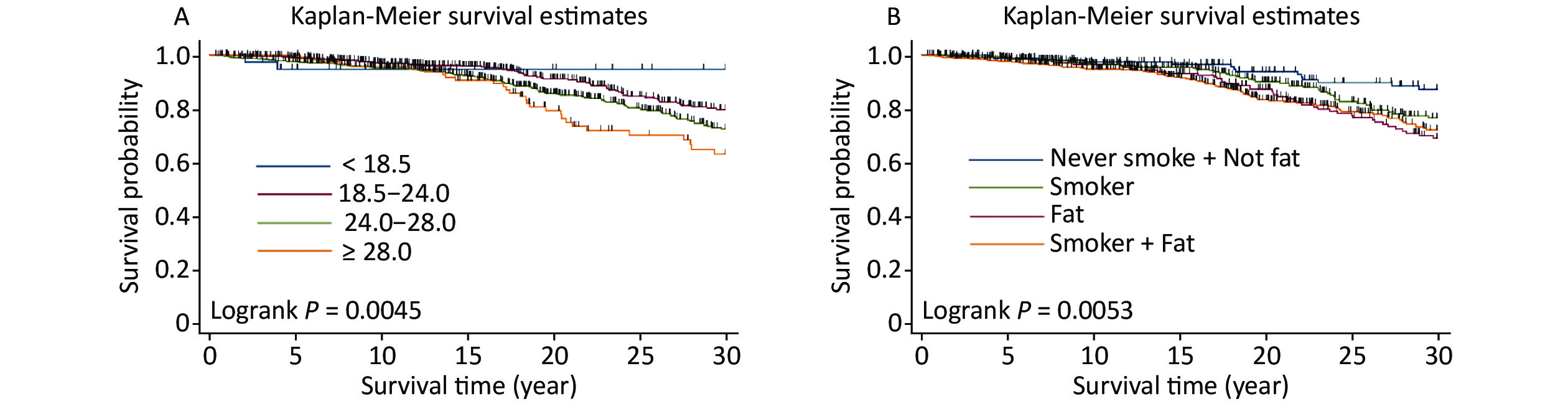
Figure 1A presents the Kaplan-Meier survival curves stratified by baseline BMI. Compared with normal BMI subjects, obese subjects (aHR: 1.603, 95% CI: 1.012–2.538) had significantly increased risk of mortality at baseline, after adjusting for age, systolic blood pressure, total cholesterol, triglyceride, smoking index, alcohol intake history, exercise, negative affairs, and past medical history. Figure 1B shows the cumulative survival for CHD with the combined effect of smoking and obesity. Compared with normal BMI and nonsmoking subjects, the HR and 95% CI of the overweight and obesity nonsmokers was 1.936 (1.053–3.561), while those of smokers with overweight and obesity was 2.828 (1.520–5.262) (Table 3 and Table 4).
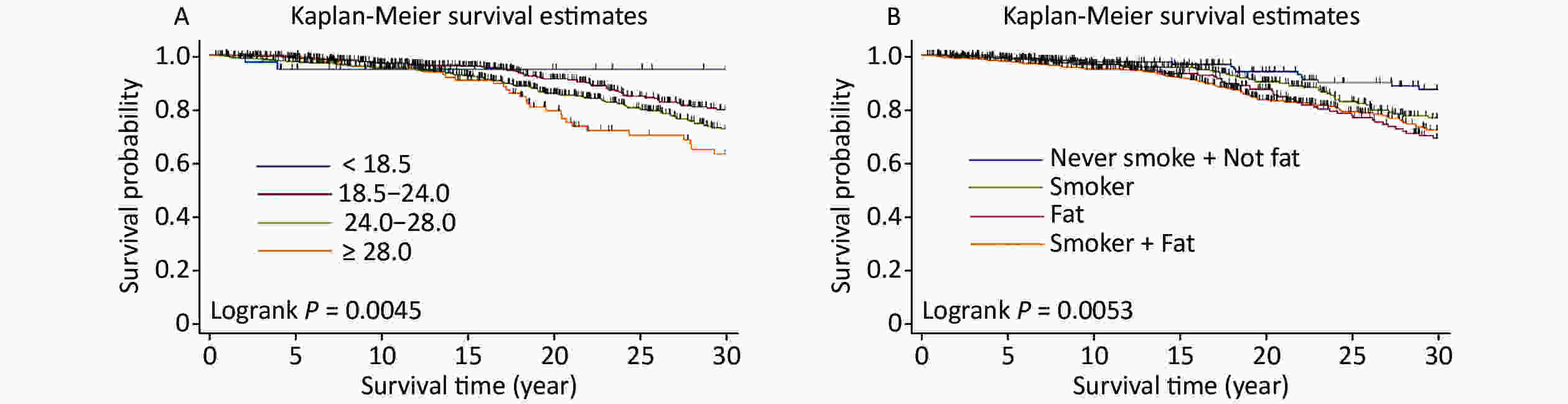
Figure 1. Comparison of the cumulative survival rates of the different body mass index (BMI) categories, for different smoker, fat, or the combined smoker and fat groups. (A) Comparison of the cumulative survival rates of the different BMI groups; (B) Comparison of the cumulative survival rates of the different smoker, fat, or the combined smoker and fat groups.
-
This cohort study is the first reported veteran cohort study in Chinese military. There is lack of evidence regarding the combined effects of smoking and obesity on CHD mortality in male veterans. There is now an urgent need to identify approach by which male veterans can give up smoking and for weight control management by the military health care personnel, especially because of deaths from CHD.
In this prospective cohort study conducted in male veterans in China, we observed that obese subjects with heavy smoking history had significantly increased risk of CHD death. This risk was found to be 183% higher among them than among the nonsmoking and normal weight subjects.
In accordance with the well-established evidence on the relationship between obesity and CHD mortality, our findings confirm that CHD mortality was higher in veterans with higher BMI. Notably, when BMI was entered into the multivariate analysis model as a categorical variable, it was found to be an independent predictor of CHD mortality. With the increasing living standards, more and more people are becoming obese[20, 21], and most studies have reported the association between obesity and CHD[22–25]. The American Heart Association and the National Institutes of Health have identified obesity as the strongest risk factor for CHD. A meta-analysis[26] showed that compared with those of normal weight, the relative risks (RRs) of overweight men and women were 1.097 (95% CI, 1.001–1.201) and 1.159 (95% CI, 1.088–1.235), while the RRs of obese men and women were 1.624 (95% CI, 1.459–1.806) and 1.508 (95% CI, 1.362–1.67), respectively. According to the UK biobank[23], Mendelian randomization analyses support a causal association between higher BMI and mortality from CHD (HR: 1.12; 95% CI: 1.00–1.25). Importantly, veterans differ from other populations of patients in several other respects. One of the most prominent differences is the need to meet the selection criteria at the time of enlistment. Subjects who had certain preexisting health problems would have been excluded during the recruitment. In addition, volunteering individuals who qualify for military service may be more likely to be physical fit or have other health attributes than those not volunteering for military service. Therefore, at baseline, in our study, the subjects seemed to be much healthier than the general population to some extent, which implies the need for caution when interpreting our findings.
Smoking was observed to be an independent risk factor for CHD mortality in our study, and it seemed that higher mortality appears to be confined to the current smoker subgroup. This finding is in agreement with those of previous prospective studies[27–29]. In 2017, smoking was the leading risk factor for the burden of disease in China[30], and it is considered an important modifiable factor that can be prevented, to decrease mortality. Additionally, with increasing rates of smoking, passive smoking is becoming an increasingly severe social problem in China. However, our study had no information on passive smoking. The effect of passive smoking on CHD mortality needs further studies.
Although there are more studies on the independent effects of risk factors, there is less evidence on the multiple effects of multiple risk factors. Smoking and obesity are independent risk factors for CHD. This study investigated the combined effect of smoking and obesity on CHD mortality. In this study, the association of the combined effect of BMI and smoking on CHD mortality was found. In terms of the present study results, there is another issue worth mentioning. The estimated HR of the combined effects was higher than that of either BMI or smoking. Evaluation of the combined effects of BMI and smoking are of particular importance because it provides insights on the potential mechanism of the individual change in risk in relation to the values of conventional risk factors and convey the clinical importance. The potential reasons for these may be that the combination of the two risk factors, resulted in significantly high point estimates (HR) with wide CIs. However, the interaction effect on the extent of effect of these risk factors, for example, the effect of the severity of smoking and the change in BMI trend, deserved to be further explored. As traditional risk factors for CHD, BMI and smoking were simple to assess, and might improve the identification of high-risk CHD patients for a more intensive secondary prevention treatment.
Several limitations in our study should be considered. First, the subjects in our study were all males (all of whom had prior military service and heavy exercise experience); therefore, the results should be considered population-specific. Therefore, our results may not apply to more general populations. Second, although BMI is the most commonly used factor to identify obesity status, it is not the optimal index. Other indexes (waist to hip ratio and lean body weight) are suggested to be superior. Furthermore, our analysis only included the baseline BMI measurements. We did not examine the influence of changes in body habitus during the follow-up. We also only had the baseline data on cardiorespiratory fitness, and other exposure variables. Therefore, we do not know if changes in any of these variables occurred during the follow-up or how they might have influenced the results. Third, the present study did not investigate possible inequality in the uptake of treatments for CHD, which might have affected the direction of the associations of potential risk factors with CHD mortality. Finally, smoking status was self-reported; this approach to measurement was sometimes questioned under the assumption that smokers tend to underestimate the amount smoked or even deny smoking.
-
Our results suggest that obese veterans who smoke might be an important target population for coronary heart disease mortality control. Thus, we conclude that more attention should be paid to the prevention of the combined risk factors in the management of CHD. Efficient interventions on smoking and obesity could have significant result on CHD death; further study is needed to provide stronger evidence.
-
None.
-
The authors wish to thank the doctors in Xijing Hospital and the staff at the 22 veteran centers for their help in data collection and ensuring that the surveys were successful.
Table 3. Effect of BMI of CHD related death at baseline
BMI (kg/m2) < 18.5 18.5–24.0 24.0–28.0 ≥ 28.0 < 18.5 1 1.670 (0.399–6.989) 2.094 (0.503–8.724) 2.677 (0.614–11.671) 18.5–24.0 1 1.254 (0.905–1.737) 1.603 (1.012–2.538) 24.0–28.0 1 1.278 (0.835–1.956) ≥ 28.0 1 Note. Adjusted for age, systolic pressure, total cholesterol, triglyceride, smoking index, alcohol intake, exercise, negative affairs, past medical history (of coronary heart disease [CHD], hypertension, stroke, diabetes mellitus [DM]). BMI, body mass index. Table 4. Combined effect of smoking and obesity of CHD related death at baseline (HR and 95% CI)
Smoking and fat Never smoker
+ not fatNever smoker
+ fatFormer smoker
+ not fatFormer smoker
+ fatCurrent smoker
+ not fatCurrent smoker
+ fatNever smoker + not fat 1 1.936
(1.053–3.561)1.451
(0.736–2.861)1.435
(0.769–2.678)1.853
(0.959–3.579)2.828
(1.520–5.262)Never smoker + fat 1 0.750
(0.445–1.263)0.741
(0.479–1.148)0.957
(0.582–1.575)1.461
(0.936–2.279)Former smoker + not fat 1 0.989
(0.591–1.655)1.277
(0.723–2.254)1.949
(1.150–3.302)Former smoker + fat 1 1.291
(0.780–2.138)1.971
(1.262–3.078)Current smoker + not fat 1 1.527
(0.923–2.524)Current smoker + fat 1 Note. Adjusted for age, systolic pressure, total cholesterol, triglyceride, alcohol intake, exercise, negative affairs, past medical history (of coronary heart disease [CHD], hypertension, stroke, diabetes mellitus [DM]), fat refers to body mass index (BMI) > 28.0.
doi: 10.3967/bes2021.012
Combined Effect of Smoking and Obesity on Coronary Heart Disease Mortality in Male Veterans: A 30-year Cohort Study
-
Abstract:
Objective Evidence is lacking regarding the combined effects of smoking and obesity on mortality from coronary heart disease in male veterans. This study aimed to explore the combined effect of smoking and obesity on coronary heart disease mortality in male veterans in China. Methods A cohort of 1,268 male veterans from 22 veteran centers in Xi’an (Shaanxi Province, China) were followed up once every 2 years from February 1, 1987 to October 30, 2016. The endpoint was death from any cause. The hazard ratio (HR) of each risk factor and the 95% confidence interval (CI) were calculated using a multivariate Cox proportional hazard model. Results The total follow-up was 24394.21 person-years; each subject was followed up for a mean duration of 19.24 years. By the end of the study, of the 1,268 veterans, 889 had died, 363 were alive, and 16 were lost to follow-up. Cox regression analysis results revealed that current smoking (HR: 1.552, 95% CI: 1.074–2.243), obesity (HR: 1.625, 95% CI: 1.024–2.581), and the combined effect of the two factors (HR: 2.828, 95% CI: 1.520–5.262) were associated with coronary heart disease mortality. Conclusion Our results suggest that obese veterans who smoke might be an important target population for coronary heart disease mortality control. -
Key words:
- Smoking /
- Obesity /
- Coronary heart disease /
- Combined effect /
- Cohort study
注释: -
Figure 1. Comparison of the cumulative survival rates of the different body mass index (BMI) categories, for different smoker, fat, or the combined smoker and fat groups. (A) Comparison of the cumulative survival rates of the different BMI groups; (B) Comparison of the cumulative survival rates of the different smoker, fat, or the combined smoker and fat groups.
Table 1. Risk factors for CHD-related deaths at baseline
Variables Univariate analysis Multivariate analysis HR (95% CI) P value aHR (95% CI) P value Age (years) 1.122 (1.092–1.152) < 0.0001 1.108 (1.076–1.142) < 0.0001 Body mass index (kg/m2) 1.096 (1.045–1.150) 0.0002 1.051 (1.000–1.104) 0.0491 Systolic pressure (mmHg) 1.022 (1.015–1.030) < 0.0001 1.012 (1.000–1.024) 0.0472 Diastolic pressure (mmHg) 1.020 (1.007–1.033) 0.0028 0.997 (0.978–1.017) 0.7812 Total cholesterol (mg/dL) 1.002 (0.999–1.005) 0.1925 1.001 (0.997–1.004) 0.7140 Triglyceride (mg/dL) 1.002 (1.000–1.004) 0.0412 1.001 (0.999–1.003) 0.3739 Alcohol intake 1.005 (0.746–1.355) 0.9718 0.902 (0.661–1.231) 0.5157 Exercise 0.756 (0.535–1.068) 0.1125 0.811 (0.570–1.154) 0.2441 Negative affairs 1.312 (0.894–1.926) 0.1655 0.981 (0.661–1.458) 0.9262 Smoking related factors Duration of smoking (years) 1.010 (1.001–1.018) 0.0285 1.009 (1.000–1.017) 0.0574 Duration of quitting smoking (years) 0.998 (0.995–1.001) 0.2024 Cigarettes per day 1.006 (0.991–1.021) 0.4378 Smoking Index 1.000 (1.000–1.001) 0.0862 Family history (Yes/No) Hypertension 1.202 (0.764–1.892) 0.4254 Stroke 1.202 (0.764–1.892) 0.4254 CHD 1.410 (0.904–2.199) 0.1294 Past medical history (Yes/No) CHD 1.857 (1.386–2.488) < 0.0001 1.071 (0.771–1.487) 0.6818 Stroke 1.671 (0.533–5.235) 0.3783 Hypertension 2.664 (1.988–3.570) < 0.0001 1.711 (1.192–2.456) 0.0036 Cerebral vascular sclerosis (CVS) 2.114 (1.481–3.018) < 0.0001 1.314 (0.891–1.937) 0.1677 Hyperlipidemia (HLP) 0.864 (0.356–2.101) 0.7475 Diabetes Mellitus (DM) 2.736 (1.701–4.403) < 0.0001 2.126 (1.301–3.475) 0.0026 Note. Adjusted for age (years), body mass index, systolic pressure, diastolic pressure, total cholesterol, triglyceride, alcohol intake, exercise, negative affairs, duration of smoking years, and past medical history (of coronary heart disease [CHD], hypertension, cerebral vascular sclerosis [CVS], diabetes mellitus [DM]). HR, hazard ratio; CI, confidence interval; aHR, adjusted hazard ratio. Table 2. Multivariate analysis for risk factors of mortality from CHD at baseline
Item Number of deaths/
total numberObserved person year/
total observed person yearHR 95% CI P value Age (years) < 60 39/402 744.9/9314.58 Reference 60–64 77/473 1352.8/9248.83 2.072 1.393–3.082 0.0003 65–69 52/250 894.5/4108.92 3.627 2.338–5.628 < 0.0001 ≥ 70 24/143 244.1/1721.87 5.787 3.312–10.111 < 0.0001 Smoking status Never smokers 59/388 1070.5/7982.74 Reference Former smokers 66/461 1165.9/8653.68 0.904 0.622–1.314 0.5966 Current smokers 67/419 1000.0/7757.80 1.552 1.074–2.243 0.0192 BMI (kg/m2) < 18.5 2/39 6.0/590.60 0.648 0.156–2.684 0.5497 18.5–24.0 61/511 1086.7/10056.88 Reference 24.0–28.0 100/587 1643.9/11309.57 1.339 0.966–1.858 0.0798 ≥ 28.0 29/131 499.9/2437.16 1.625 1.024–2.581 0.0395 Systolic pressure (mmHg) < 120 37/300 667.5/6243.15 Reference 120–129 43/381 782.1/7718.01 0.696 0.443–1.094 0.1160 130–139 33/207 520.9/3778.99 1.078 0.661–1.759 0.7636 ≥ 140 79/380 1265.9/6654.06 1.221 0.785–1.899 0.3767 Note. Adjusted for age, systolic blood pressure, body mass index (BMI), total cholesterol, triglyceride, smoking status, alcohol intake, exercise, negative affairs, past medical history (of coronary heart disease [CHD], hypertension, stroke, diabetes mellitus [DM]). HR, hazard ratio; CI, confidence interval. Table 3. Effect of BMI of CHD related death at baseline
BMI (kg/m2) < 18.5 18.5–24.0 24.0–28.0 ≥ 28.0 < 18.5 1 1.670 (0.399–6.989) 2.094 (0.503–8.724) 2.677 (0.614–11.671) 18.5–24.0 1 1.254 (0.905–1.737) 1.603 (1.012–2.538) 24.0–28.0 1 1.278 (0.835–1.956) ≥ 28.0 1 Note. Adjusted for age, systolic pressure, total cholesterol, triglyceride, smoking index, alcohol intake, exercise, negative affairs, past medical history (of coronary heart disease [CHD], hypertension, stroke, diabetes mellitus [DM]). BMI, body mass index. Table 4. Combined effect of smoking and obesity of CHD related death at baseline (HR and 95% CI)
Smoking and fat Never smoker
+ not fatNever smoker
+ fatFormer smoker
+ not fatFormer smoker
+ fatCurrent smoker
+ not fatCurrent smoker
+ fatNever smoker + not fat 1 1.936
(1.053–3.561)1.451
(0.736–2.861)1.435
(0.769–2.678)1.853
(0.959–3.579)2.828
(1.520–5.262)Never smoker + fat 1 0.750
(0.445–1.263)0.741
(0.479–1.148)0.957
(0.582–1.575)1.461
(0.936–2.279)Former smoker + not fat 1 0.989
(0.591–1.655)1.277
(0.723–2.254)1.949
(1.150–3.302)Former smoker + fat 1 1.291
(0.780–2.138)1.971
(1.262–3.078)Current smoker + not fat 1 1.527
(0.923–2.524)Current smoker + fat 1 Note. Adjusted for age, systolic pressure, total cholesterol, triglyceride, alcohol intake, exercise, negative affairs, past medical history (of coronary heart disease [CHD], hypertension, stroke, diabetes mellitus [DM]), fat refers to body mass index (BMI) > 28.0. -
[1] GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, 2018; 392, 1736−88. doi: 10.1016/S0140-6736(18)32203-7 [2] He L, Tang X, Song Y, et al. Prevalence of cardiovascular disease and risk factors in a rural district of Beijing, China: a population-based survey of 58, 308 residents. BMC Public Health, 2012; 12, 34. doi: 10.1186/1471-2458-12-34 [3] Liu SW, Li YC, Zeng XY, et al. Burden of cardiovascular diseases in China, 1990-2016: findings from the 2016 global burden of disease study. JAMA Cardiol, 2019; 4, 342−52. doi: 10.1001/jamacardio.2019.0295 [4] Pischon T, Girman CJ, Sacks FM, et al. Non-high-density lipoprotein cholesterol and apolipoprotein B in the prediction of coronary heart disease in men. Circulation, 2005; 112, 3375−83. doi: 10.1161/CIRCULATIONAHA.104.532499 [5] Hartmann M, von Birgelen C, Mintz GS, et al. Relation between lipoprotein(a) and fibrinogen and serial intravascular ultrasound plaque progression in left main coronary arteries. J Am Coll Cardiol, 2006; 48, 446−52. doi: 10.1016/j.jacc.2006.03.047 [6] Koenig W. Fibrin(ogen) in cardiovascular disease: an update. Thromb Haemost, 2003; 89, 601−9. doi: 10.1055/s-0037-1613566 [7] Avanzas P, Arroyo-Espliguero R, Quiles J, et al. Elevated serum neopterin predicts future adverse cardiac events in patients with chronic stable angina pectoris. Eur Heart J, 2005; 26, 457−63. doi: 10.1093/eurheartj/ehi111 [8] Nakamura Y, Shimada K, Fukuda D, et al. Implications of plasma concentrations of adiponectin in patients with coronary artery disease. Heart, 2004; 90, 528−33. doi: 10.1136/hrt.2003.011114 [9] Lee AJ, Price JF, Russell MJ, et al. Improved prediction of fatal myocardial infarction using the ankle brachial index in addition to conventional risk factors: the Edinburgh Artery Study. Circulation, 2004; 110, 3075−80. doi: 10.1161/01.CIR.0000143102.38256.DE [10] Ford DE, Mead LA, Chang PP, et al. Depression is a risk factor for coronary artery disease in men: the precursors study. Arch Intern Med, 1998; 158, 1422−6. doi: 10.1001/archinte.158.13.1422 [11] Mehta SK, Rame JE, Khera A, et al. Left ventricular hypertrophy, subclinical atherosclerosis, and inflammation. Hypertension, 2007; 49, 1385−91. doi: 10.1161/HYPERTENSIONAHA.107.087890 [12] Doll R, Peto R, Wheatley K, et al. Mortality in relation to smoking: 40 years' observations on male British doctors. BMJ: Br Med J, 1994; 309, 901−11. doi: 10.1136/bmj.309.6959.901 [13] Barua RS, Ambrose JA. Mechanisms of coronary thrombosis in cigarette smoke exposure. Arterioscler Thromb Vasc Biol, 2013; 33, 1460−7. doi: 10.1161/ATVBAHA.112.300154 [14] Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol, 2004; 43, 1731−7. doi: 10.1016/j.jacc.2003.12.047 [15] Siasos G, Tsigkou V, Kokkou E, et al. Smoking and atherosclerosis: mechanisms of disease and new therapeutic approaches. Curr Med Chem, 2014; 21, 3936−48. doi: 10.2174/092986732134141015161539 [16] Nakamura K, Nakagawa H, Sakurai M, et al. Influence of smoking combined with another risk factor on the risk of mortality from coronary heart disease and stroke: pooled analysis of 10 Japanese cohort studies. Cerebrovasc Dis, 2012; 33, 480−91. doi: 10.1159/000336764 [17] Meyer HE, Søgaard AJ, Tverdal A, et al. Body mass index and mortality: the influence of physical activity and smoking. Med Sci Sports Exerc, 2002; 34, 1065−70. doi: 10.1097/00005768-200207000-00002 [18] Sempos CT, Durazo-Arvizu R, Mcgee DL, et al. The influence of cigarette smoking on the association between body weight and mortality. the Framingham heart study revisited. Ann Epidemiol, 1998; 8, 289−300. [19] Cheng J, Zhao D, Zeng ZC, et al. The impact of demographic and risk factor changes on coronary heart disease deaths in Beijing, 1999-2010. BMC Public Health, 2009; 9, 30. doi: 10.1186/1471-2458-9-30 [20] Mi YJ, Zhang B, Wang HJ, et al. Prevalence and secular trends in obesity among Chinese adults, 1991-2011. Am J Prev Med, 2015; 49, 661−9. doi: 10.1016/j.amepre.2015.05.005 [21] NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet, 2016; 387, 1377−96. doi: 10.1016/S0140-6736(16)30054-X [22] Chen Y, Copeland WK, Vedanthan R, et al. Association between body mass index and cardiovascular disease mortality in East Asians and south Asians: pooled analysis of prospective data from the Asia Cohort Consortium. BMJ, 2013; 347, f5446. doi: 10.1136/bmj.f5446 [23] Wade KH, Carslake D, Sattar N, et al. BMI and mortality in UK Biobank: revised estimates using Mendelian randomization. Obesity, 2018; 26, 1796−806. doi: 10.1002/oby.22313 [24] Manson JE, Colditz GA, Stampfer MJ, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med, 1990; 322, 882−9. doi: 10.1056/NEJM199003293221303 [25] Logue J, Murray HM, Welsh P, et al. Obesity is associated with fatal coronary heart disease independently of traditional risk factors and deprivation. Heart, 2011; 97, 564−8. doi: 10.1136/hrt.2010.211201 [26] McGee DL. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol, 2005; 15, 87−97. doi: 10.1016/j.annepidem.2004.05.012 [27] Chang CM, Corey CG, Rostron BL, et al. Systematic review of cigar smoking and all cause and smoking related mortality. BMC Public Health, 2015; 15, 390. doi: 10.1186/s12889-015-1617-5 [28] Sai XY, He Y, Men K, et al. All-cause mortality and risk factors in a cohort of retired military male veterans, Xi’an, China: an 18-year follow up study. BMC Public Health, 2007; 7, 290. doi: 10.1186/1471-2458-7-290 [29] Gupta PC, Mehta HC. Cohort study of all-cause mortality among tobacco users in Mumbai, India. Bull World Health Organ, 2000; 78, 877−83. [30] Zhou MG, Wang HD, Zeng XY, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, 2019; 394, 1145−58. doi: 10.1016/S0140-6736(19)30427-1 -




 下载:
下载:



 Quick Links
Quick Links