-
The epidemiologic characteristics of 631 infant pertussis cases < 12 months, which accounted for 57.42% of the total cases, were analyzed by descriptive epidemiology in Tianjin, between 2010 and 2015. The incidence of infants was 104.66/100, 000, which was 118 times higher than in other age groups (P < 0.001). The primary type of pertussis simultaneously presented in households was adult-to-infant (70.51%). The parents were identified as the source of infection in 80.18% of cases for infants. The positive rate of placental antibody transfer was 31.06% and 3.13% for 3-month-old infants. Infants presented the highest age-specific pertussis incidence. The most important reason was parents were the important sources of infection, and secondly the lower level of antibodies in neonates and the rapid waning of maternal antibody titer.
Pertussis is still a highly contagious and potentially fatal disease, although it can be prevented by vaccination[1]. In 2014, the World Health Organization (WHO) estimated there were 50 million cases of pertussis with 300, 000 fatalities worldwide, of which 95% of cases occurred in developing countries[2]. China, as a developing country, faces the challenge of reinforcing and sustaining the control of pertussis. Although the pertussis vaccination coverage among target populations has always been above 95%, the incidence was 23.52/100, 000 among communities in Tianjin, China[3]. In addition to being at increased risk for developing pertussis, infants < 12 months of age also bear the greatest disease burden[4]. Most whooping cough deaths occur in this age group, which is consistent with observations in other countries. The highest incidence was observed in infants in the USA, and a case-fatality ratio of 6.8/1, 000 infant from 2001 through 2010[5]. In Mexico, it was concluded that the most affected age group was children < 1 year of age, which accounted for 70.4% of all reported cases[6].
In China, the epidemiological characteristics and risk factors of infant pertussis cases have not been previously reported in the literature. With the aim of determining the epidemiological characteristics and risk factors of infants, we carried out this study in Tianjin between 2010 and 2015. This study was designed to determine the source of B. pertussis transmission to young infants in households, and to assess placental antibody transfer to the child at birth and their persistence up to 3 months of age. Based on our research findings, we propose an improved immunization strategy to prevent and control pertussis in China.
This study was carried out in two populations: infant cases < 12 months of age and their household contact on one hand, a cohort of neonates followed prospectively until the age of 3 months (prior to the first dose of pertussis vaccine) on the other hand. Index cases were eligible if the infants were diagnosed with laboratory confirmed pertussis [including polymerase chain reaction (PCR) and serology]. Household contacts of the infant cases were defined as persons living in the same residence as the index infant cases during the month prior to diagnosis. Anti-pertussis antibodies were determined at birth and at 3 months of age at the Tianjin Hangu Hospital between January 2013 and July 2013. A random sample of 120 subjects was calculated using the formula for the cross-sectional study with the following parameters[7]: Zα = 1.64 (significance level: 0.05), P1= 0.70 (the first population parameter), Q = 0.30, δ = 0.08, n = 120. Considering a 10% loss, the final sample was 132.
Familial aggregation was defined as two or more laboratory confirmed pertussis cases, within the family of a laboratory-confirmed index infant case during the month. A secondary case was defined as a laboratory confirmed pertussis case identified between 4-21 days after diagnosis of the index case. The parents or guardians of participants were recruited with informed consent and interviewed in person using a standard questionnaire to obtain demographic, clinical and vaccination data. The informed consent was obtained from the legal guardian of the cases, newborn's umbilical cord, and the child at 3 months of age, as authorized by the Tianjin Centers for Disease Control and Prevention Ethics Committee.
One nasopharyngeal (NP) swab was collected for PCR detection of B. pertussis from case. The PCR positive results would be considered B. pertussis positive, when both insertion sequence IS481 (137 bp) and the PT gene (191 bp) tested positive at the same time. Two milliliter of venous blood was collected from case for IgG antibodies against pertussis toxin (anti-PT IgG) detection. Two blood samples were drawn to assess placental antibody transfer. Sample number 1 was obtained at delivery section from the cord serum and the sample number 2 was obtained from the child at 3 months, respectively. Anti-PT IgG levels were determined using enzyme-linked immunosorbent assays (ELISA) PT IgG kits (quantitative) (Institut Virion-Serion GmbH, Germany) according to the manufacturer's instructions. Based on the standards provided with the kits, anti-PT IgG levels ≥ 80 IU/mL (no vaccination) were considered as recently infected. Anti-Pertussis IgG levels were determined using ELISA B. pertussis IgG kits (quantitative) (Institut Virion-Serion GmbH, Germany), and regarded as positive if the level was ≥ 30 IU/mL. All laboratory testing was conducted at the Tianjin Centers for Disease Control and Prevention.
Data were analyzed using the Statistical Package for the Social Sciences 19.0 (SPSS 19.0) and Microsoft Excel 2003. Statistical comparisons were performed using Pearson's χ2 tests or Fisher's exact test as appropriate. Significance was determined at α = 0.05.
A total of 1, 099 pertussis cases were reported from 2010 through 2015 in Tianjin (mean annual incidence rate 1.31/100, 000). In age-stratified analysis, there were 631 infant cases, which accounted for 57.42% (631/1, 099) of the total cases. Out of the 631 cases, 544 (86.22%) were positive for PCR, 27 (4.27%) were positive for anti-PT IgG, and 60 (9.51%) were both positive. The incidence in infants was 104.66/100, 000, which was 118 times higher than other age groups (P < 0.001). The number of cases in infants increased abruptly from 36 in 2010 to 226 in 2015, and the incidence in this age group increased from 36.10/100, 000 to 217.02/100, 000. One reason for this sudden increase was the strengthens of surveillance system from 2010. Thus, the results suggested that infants presented the highest age-specific mean incidence of pertussis compared to other age groups in Tianjin. Similar to our findings, studies from Israel and Australia, reported that infants under one year presented, respectively, a five-fold and three-fold greater pertussis notification rate than all other age groups[1, 7]. In our early research of the pertussis disease burden, the average cost of treatment for patients under 1 year of age was 7, 250, which was significantly higher than other age groups ( 2, 130) (P < 0.001)[8]. Therefore, protecting infants from pertussis infection is a high priority.
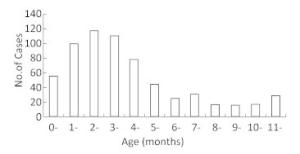
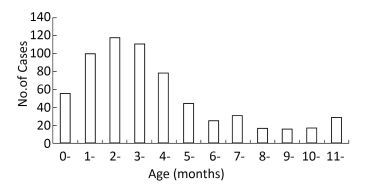
Among the 631 cases, there was no difference in gender distribution with 311 males and 320 females. In terms of age distribution, the youngest and the oldest cases were aged 7 days and 348 days, respectively. The majority of the infected cases fell in the 0-2 and 3-4 months age groups, which accounted for 42.95% (271/631) and 29.64% (187/631), respectively (Figure 1). Expectedly, infants who were too young to begin or have completed their primary vaccination series accounted for 72.58% (458/631) of cases. According to our findings, 173 infant cases were aged 5-11 months, among whom 7 patients had never been vaccinated. In the latter age-group, 36.99% (64/173) contracted the disease before the entire vaccination schedule was completed. Most strikingly, 58.96% (102/173) infants had been fully vaccinated. This result suggested that the efficacy of the DTaP vaccine in China is sub-optimal.
A total of 132 samples of neonatal cord blood were tested for pertussis antibodies, among which there were 56 females and 76 males. The positive rate was only 31.06% (41/132), in which females and males accounted for 32.14% and 30.26%, respectively. There were no significant differences between the two groups (P > 0.05). The results indicated that the positive rate of pertussis antibody at 3 months of age was 3.13% (4/128), which was significantly lower than the neonatal level (P < 0.001). The degradation rate was up to 89.92% after 3 months. There were 4 lost subjects (3.03%).
Incidence in infants < 5 months of age was the highest (72.58%). Possible explanations for this observation are that they are not the right group for vaccination or that they have not completed their primary vaccination. Because, the diphtheria-tetanus-acellular pertussis (DTaP) vaccine is administered in the 4th, 5th, and 6th months after birth in China, the protection for infants against pertussis may only come from maternal antibodies transferred through the placenta. However, the positive rate was just only 31.06% in neonates, and this decayed very rapidly. The result was only 4.3% in Mexico[9]. So, the lower level of antibody in neonates and its rapid decline were the main reasons for infant pertussis in children < 5 months of age. The findings indicated that routine vaccination may not be sufficient to protect children from pertussis infection in China.
Through the epidemiology investigation and laboratory detection, 139 familial pertussis aggregations, and 269 secondary cases were identified. A mean of 3.5 (range = 1-7) contacts were enrolled per index infant case. The results showed that the rate of familial pertussis aggregation around infant was 73.16% (139/190). There were seven grades of infection rate in households, and the average rate was 80.79% (60%-100%). Noticeably, 36.69% (51/139) of families had an infection rate of 100% (Table 1).
Table 1. The Attack Rate of Pertussis of Familial Aggregation
Grade* No. of Aggregations No. of Cases Tested Infection Rate No. of Cases Rate (%) 1 51 160 160 100.00 2 6 30 27 90.00 3 3 15 12 80.00 4 57 201 145 72.14 5 5 22 15 68.18 6 14 62 40 64.52 7 3 15 9 60.00 Total 139 505 408 80.79 Note. *The grade of infection rate in households from high to low. Four types of household pertussis transmission were observed. The primary type was adult-to-infant (70.51%, 98/139). Infant-to-adult and infant-to-adolescent each accounted for 10.07% (14/139). Adolescent-to-infant accounted for 9.53% (13/139). Therefore, the main mode of pertussis transmission was adult-to-infant.Among the 111 infants for whom an initial case was identified, mothers accounted for 63.06%, followed by fathers (17.12%), siblings (11.71%) and grandparents (8.11%) (Table 2). Among the 13 siblings identified as initial cases, 8 were sisters and 5 brothers. When calculating the proportion of source cases among all index cases, parents were identified as the source case for 80.18% of infants. The median (M) of infection time was 14 days, and the inter quartile range (IQR) was 8-18 days.This study revealed that the child-to-child transmission typical of the pre-vaccination era has been replaced by a primarily adult-to-infant transmission.
Table 2. The Results of Infection Source of Infant Pertussis Cases in Household
Initial Case Type No. of Aggregations M (d) IQR (d) Percentage (%) Mother 70 14 7-18 63.06 Father 19 13 9-17 17.12 Grandparents 9 15 7-19 8.11 Sister/brother 13 11 8-15 11.71 Total 111 14 8-18 100.00 In summary, this study provided two solid risk factors for this observation. One reason was the lower level of antibodies in neonates and the rapid waning of maternal antibodies. The second reason was parents were the important sources of infection. So, the China National Immunization Program with DTaP vaccine is unable to protect infants from the pertussis infection. The Global Pertussis Initiative (GPI) recommends 'cocoon' vaccination for all close contacts with infants[10]. Considering the current epidemiological features of pertussis in China, we suggest using the cocooning strategy, which involves vaccinating parents, caregivers, and other close contacts, to indirectly protect infants by preventing disease and transmission by those in close proximity.
We wish to express our gratitude to SHANG Xu Hong, YU Xue Feng, DONG Li Jing, LIU Peng, and ZHANG Ying for their assistance with experiments.
doi: 10.3967/bes2017.073
Epidemiological Characteristics and Risk Factors of the Pertussis in Infants < 12 Months of Age in Tianjin, China
-
注释:
-
Table 1. The Attack Rate of Pertussis of Familial Aggregation
Grade* No. of Aggregations No. of Cases Tested Infection Rate No. of Cases Rate (%) 1 51 160 160 100.00 2 6 30 27 90.00 3 3 15 12 80.00 4 57 201 145 72.14 5 5 22 15 68.18 6 14 62 40 64.52 7 3 15 9 60.00 Total 139 505 408 80.79 Note. *The grade of infection rate in households from high to low. Table 2. The Results of Infection Source of Infant Pertussis Cases in Household
Initial Case Type No. of Aggregations M (d) IQR (d) Percentage (%) Mother 70 14 7-18 63.06 Father 19 13 9-17 17.12 Grandparents 9 15 7-19 8.11 Sister/brother 13 11 8-15 11.71 Total 111 14 8-18 100.00 -
[1] Chen Stein Zamir, Dana Bardugo Dahan, Hanna Shoob. Pertussis in infants under one year old:Risk markers and vaccinationstatus-A case-control study. Vaccine, 2015; 33, 2073-8. doi: 10.1016/j.vaccine.2015.02.050 [2] World Health Organization. WHO-recommended surveillance standard of pertussis. 2014. Retrieved from http://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/passive/pertussis_standards/en/ [3] Huang HT, Zhu T, Gao C, et al. Epidemiological features of pertussis resurgence based on community populations with high vaccination coverage in China. Epidemiol Infect, 2015; 143, 1950-6. doi: 10.1017/S095026881400260X [4] Kevin Forsyth, Stanley Plotkin, Tina Tan, et al. Strategies to decrease pertussis transmission to infants. Pediatrics, 2015; 135, e1475-82. doi: 10.1542/peds.2014-3925 [5] Terranella A, Asay GR, Messonnier ML, et al. Pregnancy dose Tdap and postpartum cocooning to prevent infant pertussis:a decision analysis. Pediatrics, 2013; 131, e1748-56. doi: 10.1542/peds.2012-3144 [6] Suárez-Idueta L, Herbas-Rocha I, Gómez-Altamirano CM. Tosferina, un problema vigente de salud pública en México. Planteamiento de la necesidad para introducir una nueva vacuna. Bol Med Hosp Infant Mex, 2012; 69, 314-20. https://www.researchgate.net/publication/262462613_Tos_ferina_un_problema_vigente_de_salud_publica_en_Mexico_Planteamiento_de_la_necesidad_para_introducir_una_nueva_vacuna [7] Foxwell AR, McIntyre P, Quinn H, et al. Severe pertussis ininfants:estimated impact of first vaccine dose at 6 versus 8 weeks in Australia. Pediatr Infect Dis, J 2011; 30, 161-3. doi: 10.1097/INF.0b013e3181f43906 [8] Huang HT, Zhang Y, Li YC, et al. The investigation of pertussis disease burden under the different monitoring modes in Tianjin. Disease Surveillance, 2014; 29, 597-600. (In Chinese) http://www.researchgate.net/profile/Nicholas_Wood3/publication/23163354_Pertussis_review_of_epidemiology_diagnosis_management_and_prevention._Paediatr_Respir_Rev_9201-212/links/02e7e5284325564624000000.pdf [9] Villarreal-Pérez JZ, Ramírez-Aranda JM, Rodríguez-Rodríguez J, et al. Absence of antibodies against Bordetella pertussis in pregnant women and newborns in the state of Nuevo Leon. J Perinat Med, 2014; 42, 649-54. [10] Forsyth KD, Campins-Marti M, Caro J, et al. New pertussis vaccination strategies beyond infancy:recommendations by the global pertussis initiative. Clinical Infectious Diseases, 2004; 39, 1802-9. doi: 10.1086/426020 -




 下载:
下载:



 Quick Links
Quick Links