-
Birth defects are a global public health concern, with approximately one in every 33 babies born with a defect[1]. In China, the number of birth defect cases is projected to increase to 900, 000 each year with an incidence rate of 5.6%[2]. Further, more than 19% of infant deaths in China are caused by congenital anomalies[2]. Since 2003, there has been a rapid decline in premarital check rates, leading to a 3.0% to 5.6% increase in birth defects, such as neural tube defects (NTDs), congenital heart disease, cleft lips, mental retardation, and epilepsy[3-5]. This trend is attributed to China's shift in policy from 'mandatory premarital checks' to 'voluntary premarital checks, ' as of October 1, 2003[3-4]. As a result, the premarital check rate in Tianjin, China was only 4.6% in 2013[3]. Multiple studies have suggested that folic acid and folate intake play an important role in the prevention of congenital abnormalities, such as NTDs, congenital heart disease, cleft lips and palates, limb defects, and anorectal malformations, as well as in pregnancy outcomes, including placental abruption, placental weight, and gestational age[6-10]. Folate has been shown to affect mother and infant health through involvement in DNA synthesis, methylation reactions, and cell division[6-7, 11].
Adequate levels of folate are difficult to obtain through diet alone, and pregnant women are required to take a dose of folate that is five-to ten-times higher than that of women who are not pregnant[8]. Thus, pregnant women are more at risk of having folate deficiency. Currently, over 50 countries worldwide have implemented mandatory FA fortification and FA supplementation policies to ensure women maintain adequate levels of dietary folate during their pregnancy[9, 12]. In the United States, the Food and Drug Administration has enforced the fortification of cereal products, such as flour, rice, and bread, with FA since 1998, while in Canada, flour has been fortified with FA since 1997-1998[9, 12]. After these measures were implemented, the rate of NTDs in the United States and Canada considerably decreased by 26% and 46%, respectively[9]. While the benefits of FA supplementation before and during pregnancy are well-documented in literature, China currently has no policies regarding the mandatory FA fortification or supplementation.
However, the Chinese Government places a high priority on the prevention of congenital anomalies by promoting FA supplementation. Since 1998, the National Health and Family Planning Commission (NHFPC) of the People's Republic of China has recommended that pregnant women take a FA supplement[13]. In 2000, China launched a nationwide project to prevent NTDs, with the primary mechanism of preventing being FA supplementation among reproductive women[13]. Since 2009, the project of 'folic acid supplementation to prevent neural tube defects' has been included in basic public health services, and free FA supplements have been provided to reproductive Chinese women living in rural areas[13-14]. Currently, the NHFPC recommends that Chinese women who are planning a pregnancy should take 400 μg/d of FA from three months preconception until the end of the first trimester of pregnancy[14]. The incidence of NTDs in Northern China is three-to five-times higher than in the United States[9, 15]. This high rate may be attributed to the fact that the neural tube closes at day 28 of gestation, at which point many women are not aware of their pregnancy. In addition, reproductive women in China tend to have relatively poor folate nutrition and low plasma folate concentration levels[15-16]. Only approximately 40% of Chinese women take FA supplements before pregnancy[13]. Hence, adequate folate status during early pregnancy is difficult to maintain, resulting in higher incidences of NTDs. In previous studies, we have analyzed the association between the duration of FA intake and neurobehavioral development in rodent offspring, showing that prolonged maternal FA use throughout the pregnancy could improve neurobehavioral develo-pment[11]. Therefore, the investigation of the time of FA supplementary initiation and intake duration among pregnant Chinese women is important.
Previous Chinese studies have reported that 15.0%-77.3% of women of childbearing age take FA supplement during the periconceptional period, and approximately 40% of these women take FA before pregnancy[7, 13, 15]. However, data on the time of commencement, intake duration, and dosage of FA supplementation are limited in China. This study aimed to describe the current status of FA supplementation and determinants of its use among pregnant Chinese women. By examining periconceptional FA usage, the time of supplement initiation and termination, preconceptional and post-conceptional intake duration, the frequency of use, and FA dosage, this study intended to provide useful information that would have meaningful implications for women, their families, health care professionals and the government, such as the standardization of FA supplementation require-ments for women of reproductive age in China.
-
This cross-sectional study used a survey to collect data from pregnant women residing in Tianjin, China. Women who visited two maternal and child healthcare centers for their first postnatal check-up at 6-12 weeks postpartum between July 2015 and July 2016 were recruited for this study. Surveys were administered that had questions pertaining to FA supplementation use, socio-demographic and lifestyle characteristics, and obstetric history. If surveys were returned with no information on FA supplementation use or three skipped questions regarding socio-demographics, lifestyle factors, and obstetric history, the respective participant was excluded from the analysis. In total, 84 women were excluded, resulting in a final sample size of 1, 921 women.
-
All eligible participants were required to complete two questionnaires: one general health questionnaire (GHQ), which was used to collect information of demographic characteristics, lifestyles and obstetric history, and one dietary supplement questionnaire (DSQ), which was used to collect information of FA supplementation. All data were collected via a face-to-face interview by trained investigators, who were able to help respondents recall the information and evaluate the accuracy of their information. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Ethics Committee of Tianjin Medical University (number 2015005). Written informed consent was obtained from all participants.
-
The GHQ measured general the socio-demographic characteristics, lifestyle information, and obstetric history of the consenting participants and their spouses. Participants' age at pregnancy was classified into four categories: < 25 years, 25-29 years, 30-34 years and ≥ 35 years. Subjects were divided into three education levels: low level (i.e., high school degree or lower), intermediate level (i.e., college or university degree), and high level (i.e., master's degree or higher). Employment status was classified into two categories (unemployment and employment), family monthly income into three categories [ < 5, 000 China Yuan (CNY), 5, 000-9, 999 CNY, and ≥ 10, 000 CNY], parity into two categories (primipara: 0 previous children, multipara: ≥ 1 previous children), and history of abortion into two categories (yes and no). Body mass index (BMI) was calculated by the formula of weight (in kilograms) divided by height (in meters) squared. Pre-pregnancy BMI was categorized using the cut-points recommended by the Working Group on Obesity in China: underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2≤ BMI < 24 kg/m2), overweight (24 kg/m2≤ BMI < 28 kg/m2) and obese (BMI ≥ 28.0 kg/m2)[17]. Tobacco use was divided into non-users and smokers (active and/or passive) during pregnancy. Alcohol consumption was divided into non-users and alcohol consumers during pregnancy.
-
A self-reported DSQ was used to collect information on FA supplement intake before and during pregnancy, including the supplement brand name, the time of supplement initiation and termination, intake duration (before and during pregnancy), frequency, and dosage. Participants who took FA supplements alone and/or FA-containing multivitamins during preconception (one year before pregnancy) and/or post-conception were defined as FA supplement users. Those who never took FA supplements and FA-containing multivitamins during preconception and pregnancy were defined as non-users. The NHFPC of the People's Republic of China recommends reproductive women regularly take 400 μg/d of FA for three months prior to pregnancy until the end of the first trimester of pregnancy[14]. According to this recommendation, subjects were categorized into three levels of FA intake duration: 1) non-users, 2) users not meeting the recommendation, and 3) users meeting the recommendation. The tolerable upper limit (TUL) of FA is 1, 000 μg/d for pregnant women in China[18].
-
Analyses were performed using SPSS version 17.0 software (SPSS Inc, Chicago, IL, USA). Subjects' and their spouses' social-demographic characteristics, lifestyle information, and obstetric history were reported as percentages of categorical values. The chi-squared test was conducted to determine whether or not there were differences in periconceptional FA usage stratified by pre-defined groups. Those variables showing statistically significant association with FA supplementation from univariate analysis were included in the multivariate analysis. A multivariate logistic regression model was used to explore the potential associations between periconceptional FA supplementation and selected baseline characteristics of participants, showcased by odds ratios (OR) and a 95% confidence interval (CI). P-values < 0.05 were considered statistically significant.
-
A total of 1, 921 pregnant women were recruited in the study. Table 1 shows the participants' baseline characteristics, including the participants' socio-demographic characteristics, health-related behaviors, and obstetric history. The mean (standard deviation, SD; range) age of the participants was 30.9 years old (SD = 4.3, age range: 18-44 years old), and 54.6% of the study participants were older than 30 years old. Approximately 80% of the participants and their spouses had post-secondary education. The majority of the participants (74.6%) were working during their pregnancy, and 72.7% of the subjects' household incomes were less than 10, 000 CNY per month. The mean pre-pregnancy BMI was 21.7 kg/m2 (SD = 3.2, pre-pregnancy BMI range: 14.6-32.0 kg/m2). About 16% of the participants were identified as underweight before pregnancy, while 22.5% of the subjects were identified as overweight/obese. A large proportion of the women (67.2%) were primip-arous, and 26.3% of the subjects had a history of abortion. The proportion of women who had (passive and/or active) cigarette and alcohol consumption during pregnancy was low (15.0% and 4.6%, respectively).
Table 1. Characteristics of Study Participants (n = 1, 921)
Characteristics n % Age (y) < 25 142 7.4 25- 729 38.0 30- 696 36.2 ≥ 35 354 18.4 Education level Low 347 18.1 Intermediate 1, 373 71.5 High 201 10.4 Spouses' education level Low 396 20.6 Intermediate 1, 289 67.1 High 236 12.3 Employment Unemployment 487 25.4 Employment 1, 434 74.6 Family monthly income (CNY) < 5, 000 528 27.5 5, 000- 869 45.2 ≥ 10, 000 524 27.3 Pre-pregnancy BMI Underweight 309 16.1 Normal weight 1, 180 61.4 Overweight 338 17.6 Obese 94 4.9 Parity Primipara 1, 290 67.2 Multipara 631 32.8 History of abortion Yes 506 26.3 No 1, 415 73.7 Smoking (passive and/or active) during pregnancy Smokers 289 15.0 Nonusers 1, 632 85.0 Alcohol consumption during pregnancy Alcohol consumers 89 4.6 Nonusers 1, 832 95.4 -
From July 2015 to July 2016, 93.1% of the study participants took a FA supplement before and/or during pregnancy, 87.9% took a FA supplement during pregnancy, and 5.2% took FA supplement only in the preconceptional period (Table 2). Among the 1, 788 participants who took FA, 1, 664 (93.1%) took FA regularly, 715 (37.2%) took FA supplements before pregnancy, and 708 (39.6%) took FA during pregnancy for a duration of six months or greater. Of the women who took periconceptional FA supplements of a wide dose range (200-5, 000 μg/d), 99.2% of them took a FA dose of 400-1, 000 μg/d, while 57.4% took a FA dose of 400 μg/d. Only 14.4% of the participants adhered to the NHFPC of the People's Republic of China's recommendation for FA intake.
Table 2. Folic Acid Supplementation Status of the Study Participants
Folic Acid Supplement Use n % Periconceptional folic acid supplementation (n = 1, 921) Yes 1, 788 93.1 No 133 6.9 Regularly intake of folic acid supplementation (n = 1, 788) Regularly intake 1, 664 93.1 Irregularly intake 124 6.9 Dosage of folic acid supplementation (n = 1, 788) < 400 μg/d 5 0.3 400 μg/d 1, 027 57.4 401-600 μg/d 136 7.6 601-800 μg/d 579 32.4 801-1, 000 μg/d 33 1.8 > 1, 000 μg/d 8 0.5 Time of folic acid supplement initiation (n = 1, 788) < 1 month preconception 190 10.6 1-3 months preconception 126 7.1 ≥ 3 months preconception 399 22.3 < 1 month postconception 13 0.7 1-3 months postconception 996 55.7 ≥ 3 months postconception 64 3.6 Intake duration of folic acid supplementation (n = 1, 788) Preconception only 100 5.6 < 3 months during postconception only 202 11.3 3-6 months during postconception only 438 24.5 ≥ 6 months during postconception only 434 24.3 Preconception and < 3 months during postconception 65 3.6 Preconception and 3-6 months during postconception 275 15.4 Preconception and ≥ 6 months during postconception 274 15.3 Folic acid supplementation based on NHFPC's recommendation* (n = 1, 921) Nonusers 133 6.9 Users not meeting NHFPC's recommendation* 1, 512 78.7 Users meeting NHFPC's recommendation* 276 14.4 Note. *The recommendation is that 400 μg of folic acid should be taken daily from three months preconception until three months of pregnancy, according to the National Health and Family Planning Commission of the People's Republic of China. -
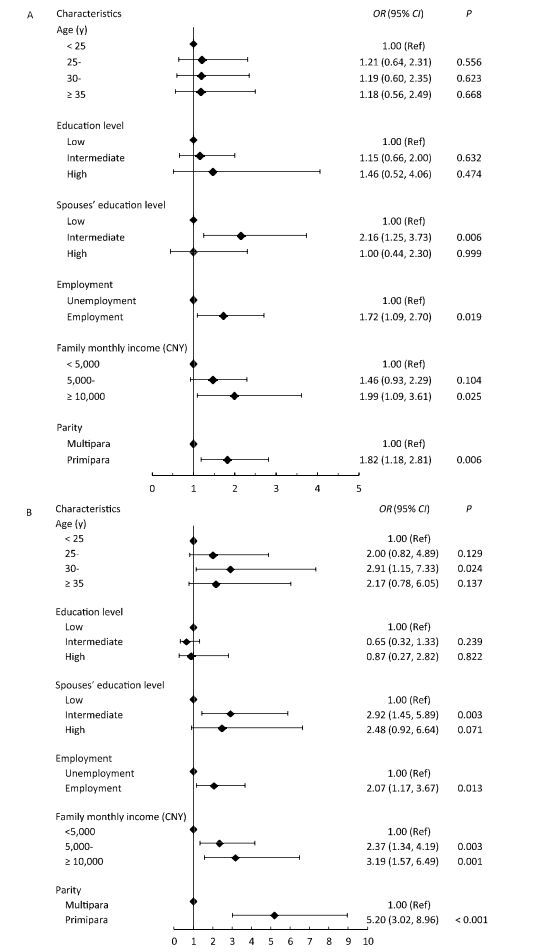
Significant statistical differences were found in the periconceptional use of FA supplementation between groups of different ages, education levels, spouse education levels, employment statuses, family monthly income, and parity (Table 3). Women who reported using a FA supplement from three months preconception and during pregnancy for a duration of three months or longer were more likely to be between 30 and 34 years old, primiparity, employed, married to a spouse with a better education level, and earn a higher family monthly income (Figure 1). Results from the unconditional logistic regression analysis revealed that primiparity was the most important determinant in the taking of FA at a dose that adhered to the NHFPC's recommendation, followed by a family monthly income greater than 10, 000 CNY, a spouse with an intermediate education level, an age between 30-and 34 years old, and employment, with an OR of 5.20 (95% CI: 3.02, 8.96), 3.19 (95% CI: 1.57, 6.49), 2.92 (95% CI: 1.45, 5.89), 2.91 (95% CI: 1.15, 7.33), and 2.07 (95% CI: 1.17, 3.67), respectively (P < 0.05).
Table 3. Participants' Characteristics Related to Folic Acid Supplementation Status based on the NHFPC's Recommendation among Pregnant Women (n = 1, 921)
Characteristic Nonusers Users not Meeting the
RecommendationaUsers Meeting the
RecommendationaPb n % n % n % Age (y) 0.001 < 25 17 12.0 114 80.3 11 7.7 25- 42 5.8 581 79.7 106 14.5 30- 43 6.2 530 76.1 123 17.7 ≥ 35 31 8.8 287 81.1 36 10.2 Education level < 0.001 Low 54 15.6 256 73.8 37 10.7 Intermediate 71 5.2 1, 107 80.6 195 14.2 High 8 4.0 149 74.1 44 21.9 Spouses' education level < 0.001 Low 63 15.9 297 75.0 36 9.1 Intermediate 55 4.3 1, 049 81.4 185 14.4 High 15 6.4 166 70.3 55 23.3 Employment < 0.001 Unemployment 68 14.0 374 76.8 45 9.2 Employment 65 4.5 1, 138 79.4 231 16.1 Family monthly income (CNY) < 0.001 < 5, 000 67 12.7 416 78.8 45 8.5 5, 000- 45 5.2 682 78.5 142 16.3 ≥ 10, 000 21 4.0 414 79.0 89 17.0 Pre-pregnancy BMI 0.444 Underweight 23 7.4 245 79.3 41 13.3 Normal weight 74 6.3 932 79.0 174 14.7 Overweight 31 9.2 256 75.7 51 15.1 Obese 5 5.3 79 84.0 10 10.6 Parity 0.000 Primipara 65 5.0 998 77.4 227 17.6 Multipara 68 10.8 514 81.5 49 7.8 History of abortion 0.979 Yes 36 7.1 397 78.5 73 14.4 No 97 6.9 1, 115 78.8 203 14.3 Smoking (passive and/or active) during pregnancy 0.813 Smokers 22 7.6 228 78.9 39 13.5 Nonusers 111 6.8 1, 284 78.7 237 14.5 Alcohol consumption during pregnancy 0.577 Alcohol consumers 5 5.6 74 83.1 10 11.2 Nonusers 128 7.0 1, 438 78.5 266 14.5 Note. aThe recommendation is that 400 μg of folic acid should be taken daily from three months preconception until three months of pregnancy, according to the National Health and Family Planning Commission of the People's Republic of China. bAnalysis of chi-squared test. 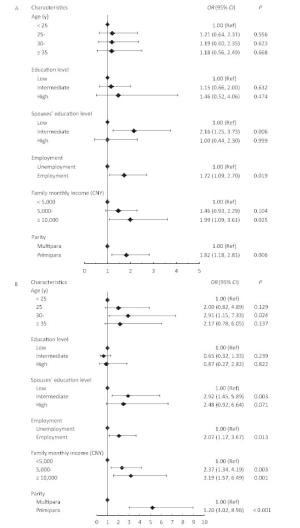
Figure 1. Forest plots of the association between participants' characteristics and folic acid supplementation in (A) folic acid users not meeting the recommendation (n= 1, 512) and (B) folic acid users meeting the recommendation (n = 276). OR, odds ratios; 95% CI, 95% confidence interval. Analysis of multivariable logistic regression model. The recommendation is that 400 μg of folic acid should be taken daily from three months preconception until three months of pregnancy, according to the National Health and Family Planning Commission of the People's Republic of China.
-
Previous studies in different countries have investigated the periconceptional use of FA. For example, a 2012 cross-sectional study in Nigeria reported that 29.2% of the participating women took FA during pregnancy, while only 2.5% took preconceptional FA[10]. In a study conducted between 2005 and 2008 in the United States, 66% of the participants took FA during pregnancy, while 51% of them took FA before pregnancy[19]. A Norwegian study conducted between 2000 and 2003 found that 71.6% of participants used FA supplements before or during pregnancy, while only 10% regularly took FA from one month before pregnancy throughout the first trimester[20]. In a 2009 Australian study, 79% of the recruited women reported taking FA supplementation during pregnancy, while only 29% took FA before conception[21]. In a 2012 Italian study, 84% of the female participants took FA during pre-pregnancy and/or pregnancy, while only 23.5% took FA before pregnancy[22]. In an Irish study conducted between 2014 and 2016, 97% of the enrolled women took FA during the periconceptional period, and 44% took FA before pregnancy[23]. Further, several studies have shown that the rate of FA supplement use in British, Danish, and European women is 12%, 34%, and 43.9%, respectively[24-26]. In Georgia, a reported 25% of pregnant women use preconception FA[27], while in Korea, an estimated 26.4% of low-income pregnant women use preconception FA[28]. Three previous studies have described FA supplementation use among Chinese women: Ren et al.[15] (2006) reported that 15% of northern Chinese women took a FA supplement during early pregnancy, with women of a lower education, agrarian occupation, rural homestead, and multiparity being less likely to take FA; Chen et al.[13] (2012) indicated that the rate of FA intake was 76.5% among rural Chinese women (rate of preconceptional FA use: 39.3%), but only differences among age groups were analyzed (protective factor: ages between 26 and 30 years old); and Liu et al.[7] investigated FA supplementation use among Lanzhou women (rate of FA use: 77.3%, rate of preconceptional FA use: 32.7%) between 2010 and 2012, but the study did not analyze the influencing factors. Compared with these three studies of Chinese women, the present study investigated more factors pertaining to FA supplementation use, such as periconceptional FA usage, the time of supplement initiation and termination, pre-conceptional and post-conceptional intake duration, the frequency of use, and dosage. Further, the present study and included more variables in the analysis of influencing factors, such as general socio-demographic characteristics, lifestyle information, and obstetric history. According to results, the rate of periconceptional FA intake among the study participants was 93.1%, which was lower than the rate found in Ireland[23], but higher than the rates reported in other previous studies[7, 10, 13, 15, 19-22, 24-25, 29]. In addition, 37.2% of the women began to take FA before conception, which was lower than the rates reported in rural Chinese areas[13], the United States[19], and Ireland[23]. These finding are in accordance with data from a Netherlands study which reported that 37% of women stated FA intake before pregnancy[30].
A study conducted by the World Health Organization (WHO) analyzed the FA supplementation recommendations of 36 countries worldwide. This study reported that 69.4% of the countries upheld the WHO recommendation of 400 μg/d of FA from preconception (four to twelve weeks) until post-conception (eight to twelve weeks), and the dose range of adopted recommendations was 400-600 μg/d[9]. Besides, TUL of FA is 1, 000 μg/d for pregnant women in China[18]. The findings of the current study indicated that 99.2% of the participants who took FA, took a dose between 400-1, 000 μg/d during the periconceptional period. Further, 57.4% of the FA users took a FA dose of 400 μg/d, while 7.6% took a FA dose of 401-600 μg/d. Conversely, a study of American women reported that approximately 80% of the women who used FA, took a dose up to 1, 000 μg/d[19], while a study of Irish women reported that approximately 91.3% of the women who used FA, took 400 μg/d[23]. The present study showed that only 0.3% of FA users took a FA dose less than 400 μg/d, while only 0.5% of them took a daily FA dose exceeding the TUL ( > 1, 000 μg/d). The data from an American study demonstrated that 23.4% of FA users took a daily supplement of FA of more than 1, 000 μg before pregnancy, and 17.1% had a FA intake of more than 1, 000 μg/d during pregnancy[19]. An Irish study showed that 6.3% of FA users reported a FA intake of more than 1, 000 μg/d during the periconceptional period[23].
Recently, conflicting views have emerged regarding the use of FA supplementation after the first trimester of pregnancy. Several studies have found that continued FA supplementation in the second and third trimesters of pregnancy increases the risk of large-for-gestational-age birth[8] and childhood asthma[29]. However, multiple studies have provided evidence that prolonged maternal FA supplementation use throughout the pregnancy can cause an increase in maternal and cord blood folate status, thus reducing the risk of a preterm birth[6-7]. In addition, we have shown through previous studies that maternal FA use throughout pregnancy improves the neurobehavioral development of offspring in rats[11]. Therefore, the investigation of the date supplement intake began and intake duration of FA supplementation is critical to the evaluation of health benefits and implementation of health services for pregnant women. With the NHFPC's recommendation, the majority of Chinese women take FA during the first trimester, but many of these women do not continue to take the supplement during the second and third trimesters[13]. The current study showed that 37.2% of the participating women started to take FA before their pregnancy, while 54.9% started taking FA during the first trimester. Similarly, Nilsen et al. reported that 23.5% of the participants took FA during the periconceptional period, while 52.5% of the participants started FA intake during the first trimester[22]. In contrast, the results of an Ireland study showed that 43.8% of the participants took FA during the periconceptional period, but only 19.6% started taking FA during the first trimester[23]. Further, 73.9% of the participants took FA for three months or longer during pregnancy, with 36.9% taking FA for six months or longer during pregnancy. Compared to the present study, Liu et al. reported that 30.3% of the participants took FA for longer than three months during the periconceptional period in Lanzhou, China[7].
Currently, the NHFPC of the People's Republic of China recommends reproductive women take a FA supplement of 400 μg/d from preconception at 12 weeks until pregnancy at 12 weeks[2, 14]. However, based on the findings of the present study, only a small portion of women (14.4%) adhere to this recommendation. There are several potential reasons for this low proportion of adherence. First, some women (6.9%) irregularly took FA supplements, meaning they did not continue FA supplementation daily. This finding concurred with the data of a study conducted between 2010 and 2012 among rural Chinese women of reproductive age, which indicated that the 5.4% of these women irregularly used FA supplements[13]. Second, 59.3% of FA users reported starting a later FA supplementation (after day 28 of gestation), which corresponds to a critical time period of birth defect prevention, especially NTDs. In China, the time of FA supplement initiation is varied, ranging from before pregnancy, to the first, second, or third trimester. Early exposure to FA in periconceptional period has been shown to be important in the protection against birth defects; however, most women are not aware of their pregnancy during the first month[6, 9-10, 12]. For example, several studies have shown that women who take FA during preconception and/or throughout the first trimester of pregnancy have a significantly reduced incidence of NTDs[6, 9-10]. However, more than 50% of these women started FA supplementation after day 28 of pregnancy. These findings are in accordance with data from two previous Chinese studies which reported that 30%-40% of women take FA supplements during the preconceptional period[7, 13]. Further, in this study, most of the women did not take FA from three months of the preconception period until three months post-conception. Of the FA users, 5.6% of them took preconceptional FA only, while 60.1% of them took post-conceptional FA only. Only 34.3% of them took FA before and during pregnancy, including some women who used FA for less than three months before pregnancy and/or some women who used FA for less than three months during pregnancy. Hence, the rate of FA supplementation use was far below the NHFPC's requirement. Knowledge of the benefits of FA supplementation should be strengthened to improve the rate of birth defects and pregnancy outcomes.
Similar to the findings of other studies, the participants' baseline characteristics, such as their socio-demographics, lifestyle habits, and obstetric history, played important roles in the periconceptional use of FA[10, 15, 19-26, 30]. In the present study, the women who were the most likely to take FA from three months before amenorrhea to three months post-conception were those who were between 30 and 34 years old[10, 15, 20-23, 30], employed[10, 26], and had a high family income[10, 20-21, 25]. Concordant results have been reported among women in Nigeria[10], Norway[20], Australia[21], Italy[22], Ireland[23], Denmark[25], and the Netherlands[30]. In Tianjin, there are two health services projects that offer free FA supplements to women who are between three months preconception and three months of pregnancy. For reproductive women living in rural areas, there is a national project that provide free FA supplements in support of 'folic acid supplementation to prevent neural tube defects'[14]. For reproductive women living in urban areas, there is a local project that provides free FA supplements in support of 'women and children health promotion program in Tianjin'[31]. However, many eligible women are not aware of these public health policies and/or are not aware of the benefits of FA supplementation. In the current study, only 10 women reported using free FA supplements, which may be attributed to inadequacy education on the use of FA. Individuals with higher income tend to be more informed about periconceptional FA supplementation and often participate in preconception counselling from a physician, who would provide information on FA supplementation[32]. Thus, since having a higher family income is associated with a greater awareness of FA use, women with higher family incomes are more likely to take FA supplements from three months preconception until three months during pregnancy.
In addition, the current study showed that having a spouse with an intermediate level of education was a significant independent factor of FA use; however, a Norwegian study found that having a spouse with a high education level was associated with FA use during pregnancy[20]. In other studies, significant associations between the participants' education levels and FA use have been found[10, 15, 20-22, 25, 28, 30]; however, in the present study, these variables were not significant independent factors. Consistent with three previous studies[20, 22, 30], pre-pregnancy BMI was not identified as an influencing factor of FA use followed the NHFPC'S requirement. In contrast, Mckeating et al.[26] identified non-obesity as a determinant of FA use. The present study showed that a history of abortion was not an influencing factor of FA use, which was different from the results obtained in studies conducted in Italy[22], Denmark[25], and the Netherlands[30]. While previous studies have shown an association between non-smokers and FA use[20-21, 25, 30], this study did not find a relationship between the two variables. Further, in contrast to the findings of a Danish[25] and a Netherland survey[30], alcohol consumption during pregnancy was not an influencing factor of periconceptional FA use or longer intake duration in this study.
The main strength of this study was the comprehensive assessment of periconceptional FA use, including the time of FA supplement initiation and intake duration. In addition, this study involved a large number of participants and evaluated multiple influencing factors, including different socio-economic groups. The data were up-to-date, thus providing valuable information for the development of national basic public health services and programs regarding FA supplementation. However, the present study did have several limitations. First, recall bias was possible. To obtain comprehensive information of periconceptional FA supplementation use, this study used a survey to collect information of FA supplementation between 6 and 12 weeks after giving birth. To minimize the effects of recall bias, in-person interviews were implemented by professional and well-trained investigators who were able to help respondents remember information and evaluate the accuracy of the information. Second, since this was a cross-sectional study, causation cannot be concluded. This study analyzed baseline data and future work is needed to elucidate correlations between FA supplementation use and maternal and infant health. The final limitation of this study is that paternal FA supplementation was not assessed. Thus, additional research is needed to investigate the role and status of paternal FA use.
-
In this study, most of the participants took FA supplements during pregnancy, but the majority of the participants did not take FA in a standardized way that adhered to the NHFPC's recommendation. The prevalence of periconceptional FA intake was much lower than the NHFPC's requirements. The time of FA supplement initiation and intake duration may be influenced by age, spouse education level, employment status, family monthly income, and number of births. This study investigated FA supplementation status among pregnant Chinese women and provided valuable information that can be used to implement national basic public health services and projects to improve the rate of birth defects and pregnancy outcomes.
-
The authors are grateful to all the women who participated in this study.
-
No conflict of interest to declare.
-
YAN Jing and ZHENG Yu Zhi participated in planning and designing of the study, data collection, data analysis and drafting manuscript. HUANG Guo Wei contributed to the conception, study design and manuscript draft. CAO Lu Jia, LIU Yu Yan, and LI Wen performed the data collection, results interpretation and subsequently manuscript revising. All of the authors have read and approved the final manuscript.
doi: 10.3967/bes2017.099
Periconceptional Folic Acid Supplementation in Chinese Women:A Cross-sectional Study
-
-
Key words:
- Folic acid /
- Supplementation /
- Periconception /
- Cross-sectional study
-
Figure 1. Forest plots of the association between participants' characteristics and folic acid supplementation in (A) folic acid users not meeting the recommendation (n= 1, 512) and (B) folic acid users meeting the recommendation (n = 276). OR, odds ratios; 95% CI, 95% confidence interval. Analysis of multivariable logistic regression model. The recommendation is that 400 μg of folic acid should be taken daily from three months preconception until three months of pregnancy, according to the National Health and Family Planning Commission of the People's Republic of China.
Table 1. Characteristics of Study Participants (n = 1, 921)
Characteristics n % Age (y) < 25 142 7.4 25- 729 38.0 30- 696 36.2 ≥ 35 354 18.4 Education level Low 347 18.1 Intermediate 1, 373 71.5 High 201 10.4 Spouses' education level Low 396 20.6 Intermediate 1, 289 67.1 High 236 12.3 Employment Unemployment 487 25.4 Employment 1, 434 74.6 Family monthly income (CNY) < 5, 000 528 27.5 5, 000- 869 45.2 ≥ 10, 000 524 27.3 Pre-pregnancy BMI Underweight 309 16.1 Normal weight 1, 180 61.4 Overweight 338 17.6 Obese 94 4.9 Parity Primipara 1, 290 67.2 Multipara 631 32.8 History of abortion Yes 506 26.3 No 1, 415 73.7 Smoking (passive and/or active) during pregnancy Smokers 289 15.0 Nonusers 1, 632 85.0 Alcohol consumption during pregnancy Alcohol consumers 89 4.6 Nonusers 1, 832 95.4 Table 2. Folic Acid Supplementation Status of the Study Participants
Folic Acid Supplement Use n % Periconceptional folic acid supplementation (n = 1, 921) Yes 1, 788 93.1 No 133 6.9 Regularly intake of folic acid supplementation (n = 1, 788) Regularly intake 1, 664 93.1 Irregularly intake 124 6.9 Dosage of folic acid supplementation (n = 1, 788) < 400 μg/d 5 0.3 400 μg/d 1, 027 57.4 401-600 μg/d 136 7.6 601-800 μg/d 579 32.4 801-1, 000 μg/d 33 1.8 > 1, 000 μg/d 8 0.5 Time of folic acid supplement initiation (n = 1, 788) < 1 month preconception 190 10.6 1-3 months preconception 126 7.1 ≥ 3 months preconception 399 22.3 < 1 month postconception 13 0.7 1-3 months postconception 996 55.7 ≥ 3 months postconception 64 3.6 Intake duration of folic acid supplementation (n = 1, 788) Preconception only 100 5.6 < 3 months during postconception only 202 11.3 3-6 months during postconception only 438 24.5 ≥ 6 months during postconception only 434 24.3 Preconception and < 3 months during postconception 65 3.6 Preconception and 3-6 months during postconception 275 15.4 Preconception and ≥ 6 months during postconception 274 15.3 Folic acid supplementation based on NHFPC's recommendation* (n = 1, 921) Nonusers 133 6.9 Users not meeting NHFPC's recommendation* 1, 512 78.7 Users meeting NHFPC's recommendation* 276 14.4 Note. *The recommendation is that 400 μg of folic acid should be taken daily from three months preconception until three months of pregnancy, according to the National Health and Family Planning Commission of the People's Republic of China. Table 3. Participants' Characteristics Related to Folic Acid Supplementation Status based on the NHFPC's Recommendation among Pregnant Women (n = 1, 921)
Characteristic Nonusers Users not Meeting the
RecommendationaUsers Meeting the
RecommendationaPb n % n % n % Age (y) 0.001 < 25 17 12.0 114 80.3 11 7.7 25- 42 5.8 581 79.7 106 14.5 30- 43 6.2 530 76.1 123 17.7 ≥ 35 31 8.8 287 81.1 36 10.2 Education level < 0.001 Low 54 15.6 256 73.8 37 10.7 Intermediate 71 5.2 1, 107 80.6 195 14.2 High 8 4.0 149 74.1 44 21.9 Spouses' education level < 0.001 Low 63 15.9 297 75.0 36 9.1 Intermediate 55 4.3 1, 049 81.4 185 14.4 High 15 6.4 166 70.3 55 23.3 Employment < 0.001 Unemployment 68 14.0 374 76.8 45 9.2 Employment 65 4.5 1, 138 79.4 231 16.1 Family monthly income (CNY) < 0.001 < 5, 000 67 12.7 416 78.8 45 8.5 5, 000- 45 5.2 682 78.5 142 16.3 ≥ 10, 000 21 4.0 414 79.0 89 17.0 Pre-pregnancy BMI 0.444 Underweight 23 7.4 245 79.3 41 13.3 Normal weight 74 6.3 932 79.0 174 14.7 Overweight 31 9.2 256 75.7 51 15.1 Obese 5 5.3 79 84.0 10 10.6 Parity 0.000 Primipara 65 5.0 998 77.4 227 17.6 Multipara 68 10.8 514 81.5 49 7.8 History of abortion 0.979 Yes 36 7.1 397 78.5 73 14.4 No 97 6.9 1, 115 78.8 203 14.3 Smoking (passive and/or active) during pregnancy 0.813 Smokers 22 7.6 228 78.9 39 13.5 Nonusers 111 6.8 1, 284 78.7 237 14.5 Alcohol consumption during pregnancy 0.577 Alcohol consumers 5 5.6 74 83.1 10 11.2 Nonusers 128 7.0 1, 438 78.5 266 14.5 Note. aThe recommendation is that 400 μg of folic acid should be taken daily from three months preconception until three months of pregnancy, according to the National Health and Family Planning Commission of the People's Republic of China. bAnalysis of chi-squared test. -
[1] Centers for Disease Control and Prevention. Birth defects. https://www.cdc.gov/features/birth-defects-day/index.html. [2017-05-21] [2] National Health and Family Planning Commission of the People's Republic of China. Report of birth defects prevention in China, 2012. http://www.moh.gov.cn/wsb/pxwfb/201209/55840.shtml. [2017-05-17] (In Chinese) [3] Zhao Y, Luo S, Li H, et al. Secular trends of premarital medical examination in China during 1996 and 2013. Journal of Peking University (Health science), 2015; 47, 437-42. (In Chinese) [4] Cai R, Richardus JH, Looman CW, et al. Trends in high-risk sexual behaviors among general population groups in China:a systematic review. PLOS One, 2013; 8, e79320. doi: 10.1371/journal.pone.0079320 [5] Li Y, Zhang Y, Fang S, et al. Analysis of inequality in maternal and child health outcomes and mortality from 2000 to 2013 in China. Int J Equity Health, 2017; 16, 66-76. doi: 10.1186/s12939-017-0558-2 [6] McNulty B, McNulty H, Marshall B, et al. Impact of continuing folic acid after the first trimester of pregnancy:findings of a randomized trial of Folic Acid Supplementation in the Second and Third Trimesters. Am J Clin Nutr, 2013; 98, 92-9. doi: 10.3945/ajcn.112.057489 [7] Liu X, Lv L, Zhang H, et al. Folic acid supplementation, dietary folate intake and risk of preterm birth in China. Eur J Nutr, 2016; 55, 1411-22. doi: 10.1007/s00394-015-0959-1 [8] Wang S, Ge X, Zhu B, et al. Maternal Continuing Folic Acid Supplementation after the First Trimester of Pregnancy Increased the Risk of Large-for-Gestational-Age Birth:A Population-Based Birth Cohort Study. Nutrients, 2016; 8, 493-503. doi: 10.3390/nu8080493 [9] Gomes S, Lopes C, Pinto E. Folate and folic acid in the periconceptional period:recommendations from official health organizations in thirty-six countries worldwide and WHO. Public Health Nutr, 2016; 19, 176-89. doi: 10.1017/S1368980015000555 [10] Lawal TA, Adeleye AO. Determinants of folic acid intake during preconception and in early pregnancy by mothers in Ibadan, Nigeria. Pan Afr Med J, 2014; 19, 113-8. doi: 10.12968/bjom.2017.25.6.358 [11] Wang X, Li W, Li S, et al. Maternal Folic Acid Supplementation During Pregnancy Improves Neurobehavioral Development in Rat Offspring. Mol Neurobiol, 2017; DOI: 10.1007/s12035-017-0534-2. [12] Chitayat D, Matsui D, Amitai Y, et al. Folic acid supplementation for pregnant women and those planning pregnancy:2015 update. J Clin Pharmacol, 2016; 56, 170-5. doi: 10.1002/jcph.v56.2 [13] Chen J, Zhang S, Wang Q, et al. Investigation on folic acid supplementation status among Chinese women in the first trimester of pregnancy. Natl Med J China, 2016; 96, 1215-9. (In Chinese) [14] National Health and Family Planning Commission of the People's Republic of China. The project management plan of folic acid supplement to prevent neural tube defects, 2010. http://www.nhfpc.gov.cn/fys/s3581/201006/942109bebb4340b2922898f565489a6f.shtml. [2017-05-20] (In Chinese) [15] Ren A, Zhang L, Li Z, et al. Awareness and use of folic acid, and blood folate concentrations among pregnant women in northern China——an area with a high prevalence of neural tube defects. Reprod Toxicol, 2006; 22, 431-6. doi: 10.1016/j.reprotox.2006.02.003 [16] Zhao Y, Hao L, Zhang L, et al. Plasma folate status and dietary folate intake among Chinese women of childbearing age. Matern Child Nutr, 2009; 5, 104-16. doi: 10.1111/mcn.2009.5.issue-2 [17] Chen C, Lu FC, Working Group on Obesity in China, Department of Disease Control, Ministry of Health. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci, 2004; 17, 1-35. https://www.nhlbi.nih.gov/health/health-topics/topics/obe/ [18] Chinese Nutrition Society. Chinese Dietary Reference Intakes 2013. Beijing:Science Press, 2014. [19] Hoyo C, Murtha AP, Schildkraut JM, et al. Folic acid supplementation before and during pregnancy in the Newborn Epigenetics STudy (NEST). BMC Public Health, 2011; 11, 46-53. doi: 10.1186/1471-2458-11-46 [20] Nilsen RM, Vollset SE, Gjessing HK, et al. Patterns and predictors of folic acid supplement use among pregnant women:the Nowegian Mother and Child Cohort Study. Am J Clin Nutr, 2006; 84, 1134-41.
[21] Forster DA, Wills G, Denning A, et al. The use of folic acid and other vitamins before and during pregnancy in a group of women in Melbourne, Australia. Midwifery, 2009; 25, 134-46. doi: 10.1016/j.midw.2007.01.019 [22] Nilsen RM, Leoncini E, Gastaldi P, et al. Prevalence and determinants of preconception folic acid use:an Italian multicenter survey. Ital J Pediatr, 2016; 42, 65-74. doi: 10.1186/s13052-016-0278-z [23] Cawley S, Mullaney L, Kennedy R, et al. Duration of periconceptional folic acid supplementation in women booking for antenatal care. Public Health Nurtition, 2017; 20, 371-9. [24] Peake JN, Copp AJ, Shawe J. Knowledge and periconceptional use of folic acid for the prevention of neural tube defects in ethnic communities in the United Kingdom:systematic review and meta-analysis. Birth Defects Res A Clin Mol Teratol, 2013; 97, 444-51. doi: 10.1002/bdra.23154 [25] Cueto HT, Riis AH, Hatch EE, et al. Predictors of preconceptional folic acid or multivitamin supplement use:a cross-sectional study of Danish pregnancy planners. Clin Epidemiol, 2012; 4, 259-65. https://www.dovepress.com/article_metric.php?article_id=11191 [26] McKeating A, Farren M, Cawley S, et al. Maternal folic acid supplementation trends 2009-2013. Acta Obstet Gynecol Scand, 2015; 94, 727-33. doi: 10.1111/aogs.2015.94.issue-7 [27] Mukhtar A, Kramer MR, Oakley GP Jr, et al. Race and ethnicity and preconception folic acid supplement use among pregnant women in Georgia, PRAMS 2009 to 2011. Birth Defects Res, 2017; 109, 38-48. doi: 10.1002/(ISSN)2472-1727 [28] Kim J, Yon M, Kim C, et al. Preconceptional use of folic acid and knowledge about folic acid among low-income pregnant women in Korea. Nutrition Research and Practice, 2017; 11, 240-6. doi: 10.4162/nrp.2017.11.3.240 [29] Whitrow MJ, Moore VM, Rumbold AR, et al. Effect of supplemental folic acid in pregnancy on childhood asthma:a prospective birth cohort study. Am J Epidemiol, 2009; 170, 1486-93. doi: 10.1093/aje/kwp315 [30] Timmermans S, Jaddoe VW, Mackenbach JP, et al. Determinants of folic acid use in early pregnancy in a multi-ethnic urban population in The Netherlans:the Generation R study. Prev Med, 2008; 47, 427-32. doi: 10.1016/j.ypmed.2008.06.014 [31] Health and Family Planning Commission of Tianjin. Women and children health promotion program in Tianjin. 2015; http://www.tjdpf.org.cn/yw/system/2015/08/27/011500281.shtml. [2017-09-14] (In Chinese) [32] Temel S, Erdem Ö, Voorham TA, et al. Knowledge on preconceptiona lfolic acid supplementation and intention to seek for preconceptioncare among men and women in an urbancity:a population-based cross-sectional study. BMC Pregnancy Childbirth, 2015; 15, 340-50. doi: 10.1186/s12884-015-0774-y -




 下载:
下载:



 Quick Links
Quick Links