-
Eczema is a very common inflammatory skin disease characterized by patches of erythematous, itchy, cracked, and scaly skin. According to the 2010 Global Burden of Disease Study, the global prevalence of eczema is 3.33% and the leading cause of skin condition-based disability-adjusted life years is eczema[1]. The large health burden brought about by eczema suggests high direct medical costs and health care utilization[2]. Thus, eczema prevention is of great importance in efforts to eliminate the public health burden of the disease.
Eczema is a complex disease resulting from interactions between multiple genetic and environmental factors[3]. Several studies on the association between air pollution and eczema in adults have been published, but contradictory results are often reported. Fine particular matter (PM2.5, i.e., particulate matter less than 2.5 μm in diameter) constitutes most of the total particulate matter in urban areas[4]. Very few studies have specifically revealed the relation between PM2.5 and eczema, and most available works involve children. However, the prevalence of eczema worldwide has increased rapidly in adults over the last few decades[1]. Because adults with eczema could require substantial out-of-pocket costs from lost workdays and sick days, as well as high health care resource utilization, the effect of PM2.5 on adult eczema must be fully investigated[2].
Air pollution levels in Beijing, especially PM2.5 concentrations in the years 2010-2012, were constantly high[5]. Data during this period in a city-wide reporting system could provide an opportunity to examine the short-term effects of PM2.5 on the risk of adult eczema. All data on daily outpatient visits for eczema between June 1, 2010 and June 31, 2012 (761 days) were obtained from Beijing Medical Claim Data for Employees (BMCDE), a database including anonymized information of all working and retired employees with basic medical insurance in Beijing. The sample size of this database included up to 9 million records, or about half of the Beijing population, at the end of 2012. The BMCDE includes patients' demographic characteristics (age and sex), dates of hospital visits, clinical diagnoses in Chinese and corresponding International Classification of Diseases 10th Revision (ICD-10) codes, dispensed medications, and other reimbursement information. This study only included adults aged 18 years and older. We identified daily cases of eczema by using the ICD-10 code L30.9 for principal diagnosis.
Air pollution data for hourly PM2.5 concentrations were obtained from the monitoring records of the US embassy (http://www.stateair.net/web/historical/1/1.html); pertinent data were collected by an ambient air quality monitoring station established on the rooftop of the embassy building located in Chaoyang District, Beijing. PM2.5 concentrations at this location have been reported to be approximately equal to those in the entire city[6]. Moreover, the distance from residential areas to the monitoring station should be no more than 40 km to enable full exposure. In Beijing, all areas of high population density (> 5, 000 people/km2), 79.2% of all residential areas, 97.8% (44/45) of the tertiary hospitals, and 79.3% (69/87) of the secondary hospitals are located within a 40 km radius of the monitoring station. To further reduce exposure misclassification, we only included urban residents in the study. Information of daily 24-hour average temperature (℃) and relative humidity (%) was collected from the China Meteorological Bureau over the same study period.
In this study, daily outpatient visits for eczema, daily average PM2.5 concentrations, and meteorological conditions were linked by date to enable analysis via a time-series design. A generalized additive Poisson model was applied to examine the short-term associations between PM2.5, as well as weather variables, and eczema after adjusting for day of the week (DOW), calendar time, national holidays in China, and daily average temperature and relative humidity[7].
Log[E(Yt)] = α + β1PM2.5t − i + β2DOW + β3 (Holiday) + ps(Calendar time, df = 10) + ps (Temperature, df = 3) + ps(Relative humidity, df = 3) where E(Yt) is the expected number of outpatient visits for eczema on day t, α is the model intercept, PM2.5t − i is the mean PM2.5 concentration on day t, i is the day lag, β1 is the log-relative risk of eczema associated with an unit increase of PM2.5, β2 and β3 are the regression coefficients of DOW and Holiday, respectively, DOW is the day of the week, Holiday is a binary variable, ps() indicates a penalized spline function, and df represents the degrees of freedom; data of these variable were selected based on previous studies. Moreover, we used a penalty cubic regression spline with a PM2.5 concentration of 3 dfs to explore nonlinear exposure-response correlations because the linear hypothesis between PM2.5 levels and hospital visits may be unreasonable.
To investigate the temporal association between eczema and PM2.5 concentration, we fitted the models with single-day lag (from lag0 to lag3) and multiple-day lags (lag0-2 and lag0-3). We also examined potential effect modifications of eczema risk by age (18-64 years and ≥ 65 years) and sex. The Z-test was used to test the statistical significance of subgroup differences.
We adjusted for daily average temperature, relative humidity, DOW, holiday, and long time-series and expressed results as percent changes and 95% confidence intervals (CIs) in daily eczema outpatient visits associated with 10 mg/m3 increases in PM2.5 concentration. All statistical tests were two-tailed, and a P value < 0.05 was considered significant. All analyses were performed using the R programming language (V.3.2.2, R Development Core Team).
Our city-wide study involving 1, 966, 991 hospital visits from June 1, 2010 to June 30, 2012 (761 days) indicated a strong association between PM2.5 short-term exposure and adult eczema. To the best of our knowledge, this work is the first city-level study to illustrate the effect of PM2.5 on outpatient visits for eczema in an environment with severe air pollution. The basic demographic characteristics of the subjects are shown in Supplementary Table S1 (available in www.besjournal.com). In this study, 40.0% of the patients were males and 66.9% were 18-64 years old. The mean (standard deviation, SD) age of the eczema outpatients was 57.63 (15.54) years.
Table 1 summarizes the data of daily outpatient visits, air pollution, and meteorological conditions collected during the study period. The mean (SD) daily count of eczema-attributed outpatient visits was 2, 585 (1, 503), and the interquartile range for outpatient visits was 2, 279. The overall mean daily PM2.5 concentration during the study period was 101.2 μg/m3 (range, 7.2-492.8 μg/m3). Daily PM2.5 concentrations in 420 of 761 (55.2%) days exceeded Chinese Ambient Air Quality Standards Grade Ⅱ standards for daily mean concentration of PM2.5 (75 μg/m3). Moreover, daily PM2.5 concentrations in 653 (85.8%) days failed to meet WHO Air Quality Standards for daily mean concentration of PM2.5 (25 μg/m3). The means (SD) of daily temperature and relative humidity were 13.9 ℃ (11.5 ℃) and 49.3% (20.7%), respectively.
Table 1. Statistics for Daily Number of Eczema Outpatient Visits, Daily Fine Particulate Matter (PM2.5) Concentrations, and Meteorological Conditions in Beijing, China, from June 1, 2010 to June 30, 2012
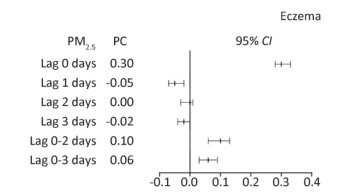
Variables Mean ± SD Minimum Percentile Maximum 25th 50th 75th Outpatient visits 2, 585 ± 1, 503 55 1, 482 2, 174 3, 761 7, 582 Male 1, 033 ± 589 29 590 895 1, 465 2, 909 Female 1, 552 ± 917 26 900 1276 2, 297 4, 673 18-64 (years) 1, 728 ± 986 42 998 1444 2, 497 4, 957 ≥ 65 (years) 857 ± 530 13 430 740 1271 2625 PM2.5 (μg/m3) 101.2 ± 77.6 7.2 42.4 84.6 135.5 492.8 Temperature (℃) 13.9 ± 11.5 -7.8 2.4 15.9 24.5 34.5 Relative humidity (%) 49.3 ± 20.7 9 30 50 66 92 Our study indicated percent changes in hospital outpatient utilization for eczema associated with 10 μg/m3 increases in PM2.5 concentration for different lag structures (Figure 1). We first found that a 10 μg/m3 increase in the PM2.5 of the current day was related to a 0.30% (95% CI, 0.28%-0.33%) percentage change in number of hospital visits. This result contributes to the limited scientific evidence supporting the effects of ambient particulate matter on eczema. Despite the low magnitude of percentage changes in eczema outpatient visits, the increasing number of eczema cases deserves further study. A broad dose-response association between PM2.5 concentration and number of daily eczema outpatient visits was observed (Supplementary Figure S1 available in www.besjournal.com). According to the exposure-response curve, it was approximately linear without threshold concentration. However, why PM2.5 could trigger and exacerbate the dermatological signs of eczema remains unknown. Some researchers believe that short-term PM2.5 exposure may impair the functions of the epidermal barrier, thereby allowing particles to penetrate the skin and induce an inflammatory response; oxidative stress and inflammation may play a dominant role in this mechanism[8].
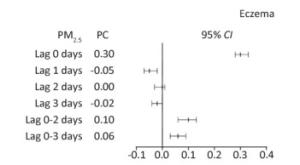
Figure 1. PC and 95% CI in daily outpatient visits for eczema associated with increases of 10 μg/m3 in PM2.5 concentrations at different lag days. CI, confidence interval; PC, percentage change.
Table 2 shows a stratified analysis of the association between PM2.5 exposure and eczema. The number of outpatient eczema visits did not differ between males and females or between warm and cool seasons. However, patients who were ≥ 65 years old showed significantly higher percentage changes in outpatient visits than those who were 18-64 years old on the same day [0.44% (95% CI, 0.40%-0.49%) vs. 0.23% (95% CI, 0.20%-0.26%)]. Older patients may have weaker immune systems than younger ones, and the inflammatory or immune responses triggered by air pollutants in older subjects may differ from those in young adults; thus, elder adults are more vulnerable to high levels of particulate air pollution[9]. In addition, a decline in skin barrier functions associated with aging may increase susceptibility to environmental irritants, pathogens, and allergens, thereby leading to systemic sensitization and, ultimately, a collapse in peripheral immune tolerance[10]. These findings shed light on the importance of certain subgroups reducing their exposure during days with high levels of air pollution.
Table 2. Percentage Changes with 95% CIs in Eczema Outpatient Visits Associated with a 10 μg/m3 Increase in Fine Particulate Matter (PM2.5) Concentration on the Same Day Stratified by Gender, Age, and Season
Variables Percentage Change 95% CI P Gender Male 0.29 0.25, 0.33 < 2 × 10-16 Female 0.31 0.28, 0.34 < 2 × 10-16 Age (year) 18-64 0.23 0.20, 0.26 < 2 × 10-16 ≥ 65 0.44 0.40, 0.49 < 2 × 10-16 Season Warm 0.16 0.12, 0.21 3.50 × 10-11 Cool 0.20 0.16, 0.23 < 2 × 10-16 This work is the study to directly illustrate a clear association between PM2.5 exposure and eczema. This study is based on a large sample of eczema outpatient cases in a heavily polluted city (overall mean daily PM2.5 concentration during the study period, 101.2 mg/m3). The large scale of this study enables demonstration of the complicated relation between environmental factors and disease occurrence.
However, some limitations in our study must be addressed. First, a fixed-site monitoring station was used as a proxy of population exposure to collect daily PM2.5 concentrations. Environmental exposure was an averaged level, not precisely for each patient, which may lead to errors in exposure measurement and underestimation of pollutant effects. Second, the database used only included working and retired employees aged 18 years and older with basic medical insurance. The characteristics of this population may differ from those without a job, those who live in remote regions, those without medical insurance, and children and infants. Potential individual confounders, including socio-economic status, living environment, and medication use, were not taken into account in this work. Since we had no access to monitoring data on other air pollutants, such as SO2, NO2, CO, and O3, the independent effect of PM2.5 could not be explored. Thus, our findings should be interpreted with caution. Further studies examining the independent effect of PM2.5 on eczema are recommended.
doi: 10.3967/bes2019.080
Association between Fine Particulate Air Pollution and Outpatient Visits for Eczema in Beijing, China: A Time-series Analysis
-
-
Table 1. Statistics for Daily Number of Eczema Outpatient Visits, Daily Fine Particulate Matter (PM2.5) Concentrations, and Meteorological Conditions in Beijing, China, from June 1, 2010 to June 30, 2012
Variables Mean ± SD Minimum Percentile Maximum 25th 50th 75th Outpatient visits 2, 585 ± 1, 503 55 1, 482 2, 174 3, 761 7, 582 Male 1, 033 ± 589 29 590 895 1, 465 2, 909 Female 1, 552 ± 917 26 900 1276 2, 297 4, 673 18-64 (years) 1, 728 ± 986 42 998 1444 2, 497 4, 957 ≥ 65 (years) 857 ± 530 13 430 740 1271 2625 PM2.5 (μg/m3) 101.2 ± 77.6 7.2 42.4 84.6 135.5 492.8 Temperature (℃) 13.9 ± 11.5 -7.8 2.4 15.9 24.5 34.5 Relative humidity (%) 49.3 ± 20.7 9 30 50 66 92 Table 2. Percentage Changes with 95% CIs in Eczema Outpatient Visits Associated with a 10 μg/m3 Increase in Fine Particulate Matter (PM2.5) Concentration on the Same Day Stratified by Gender, Age, and Season
Variables Percentage Change 95% CI P Gender Male 0.29 0.25, 0.33 < 2 × 10-16 Female 0.31 0.28, 0.34 < 2 × 10-16 Age (year) 18-64 0.23 0.20, 0.26 < 2 × 10-16 ≥ 65 0.44 0.40, 0.49 < 2 × 10-16 Season Warm 0.16 0.12, 0.21 3.50 × 10-11 Cool 0.20 0.16, 0.23 < 2 × 10-16 -
[1] Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010:an analysis of the prevalence and impact of skin conditions. J Invest Dermatol, 2014; 134, 1527-34. doi: 10.1038/jid.2013.446 [2] Silverberg JI. Health care utilization, patient costs, and access to care in US adults with eczema:A population-based study. JAMA Dermatol, 2015; 151, 743-52. doi: 10.1001/jamadermatol.2014.5432 [3] Plotz SG, Wiesender M, Todorova A, et al. What is new in atopic dermatitis/eczema? Expert Opin Emerg Drugs, 2014; 19, 441-58. doi: 10.1517/14728214.2014.953927 [4] Fontes T, Li P, Barros N, et al. Trends of PM2.5 concentrations in China:A long term approach. J Environ Manage, 2017; 196, 719-32. doi: 10.1016/j.jenvman.2017.03.074 [5] Downes MJ, Bettington EK, Gunton JE, et al. Triple therapy in type 2 diabetes:A systematic review and network meta-analysis. Peer J, 2015; 3, e1461. doi: 10.7717/peerj.1461 [6] Wang JF, MG Hu, CD Xu, et al. Estimation of citywide air pollution in Beijing. PLoS One, 2013; 8, e53400. doi: 10.1371/journal.pone.0053400 [7] He S, S Mazumdar, VC Arena. A comparative study of the use of GAM and GLM in air pollution research. Environmetrics, 2006; 17, 81-93. doi: 10.1002/env.751 [8] Puri P, SK Nandar, S Kathuria, et al. Effects of air pollution on the skin:A review. Indian J Dermatol Venereol Leprol, 2017; 83, 415-23. doi: 10.4103/0378-6323.199579 [9] Weinberg A, J Canniff, N Rouphael, et al. Varicella-Zoster Virus-Specific Cellular Immune Responses to the Live Attenuated Zoster Vaccine in Young and Older Adults. J Immunol, 2017; 199, 604-12. doi: 10.4049/jimmunol.1700290 [10] Tanei R, Y Hasegawa. Atopic dermatitis in older adults:A viewpoint from geriatric dermatology. Geriatr Gerontol Int, 2016; 16 Suppl 1, 75-86. http://www.ncbi.nlm.nih.gov/pubmed/27018286 -




 下载:
下载:



 Quick Links
Quick Links