-
Sleep-wake patterns demonstrate rapid changes during the first year of life, with gradual maturation across childhood [1]. A growing body of evidence suggested that sleep is important in developmental outcomes across the early childhood, including physical health, cognitive development, and emotional and behavioral functioning [1]. Sleep problems have been a major concern for parents of infants and toddlers worldwide. A recent national cross-sectional survey in China revealed that sleep problems was the second most common child-rearing problems (60.72%) for parents of children aged 6–35 months, following feeding problems (63.43%) [2]. Several studies have reported that the most common sleep complaints during the first 3 years of life are frequent night awakenings and difficulty falling asleep in 10%–40% of children [3-7]. Furthermore, these two sleep problems in early childhood tended to persist over time if they were not managed promptly [8, 9].
According to Sadeh et al., daytime sleep is mostly determined by maturation, whereas nocturnal sleep is better predicted by ecological factors [4]. Early childhood was a critical period for the formation of good sleep habits. Evidence suggested that excessive parental involvement or assistance may hinder the development of children’s self-soothing ability and interfere with nighttime sleep consolidation and regulation [4, 10]. The most common methods for parents to intervene and assist sleep during early childhood included sleeping in the same bed, feeding, holding, or rocking to fall asleep [4, 11, 12].
Bed-sharing with parents for young children was a common sleep arrangement. However, previous studies on the prevalence, effect, and reasons for bed-sharing have presented inconsistent results. Cross-cultural differences were also found in bed-sharing sleep arrangements [11, 13]. The rate of bed-sharing ranged from 5.0% in the United Kingdom to 83.2% in Vietnam and 67.59% in China [11]. Various studies have also reported different trends in sleep arrangements with age. Hauck et al. found a decrease in bed-sharing (decreased from 42% to 27%) from 2 weeks to 12 months among a US sample [14]. However, Huang et al. reported that bed-sharing increased from 46% to 60% by 8 months postpartum in Chinese infants [15]. Some researchers demonstrated that bed-sharing could promote breastfeeding, which was beneficial for early childhood health [16, 17]. However, the American Academy of Pediatrics recommend room-sharing without bed-sharing to reduce the risk of sudden infant death syndrome (SIDS) and other sleep-related infant deaths [18]. The results of different studies on the effect of bed-sharing on children’s sleep were also inconsistent. Some studies have indicated that children who sleep in the same bed with their parents had more night awakenings [4, 19, 20]; however, others found no association between bed-sharing and children’s night awakenings [15, 21, 22]. The common reasons for bed-sharing reported abroad were breastfeeding and comforting [23]. However, the reasons why Chinese parents chose bed-sharing have not been well studied.
Self-soothing is an important ability during infant sleep initiation for the development of healthy sleep-wake patterns [24]. A longitudinal Italian cohort study revealed that the proportion of infants who fell asleep alone ranged from 20% to 25% during the first year of life [10]. A US–Canada sample presented an increase in the rate of falling asleep alone (from 18.9% to 52.7% by 1 year and increased to 62.86% by 3 years) from birth to 3 years, and a sharp decrease in other soothing methods such as feeding, nursing, rocking, and holding the infant [4]. Studies have demonstrated that intensive parental involvement and lack of self-soothing skills were associated with night awakenings and difficulty falling asleep [12, 24, 25]. A pilot study indicated that infants who can self-soothe at night by age 12 months were less likely to have a sleep-related problem at 2 years of age [26]. In China, few studies have examined the soothing methods for young children. A longitudinal study conducted in 2012 in Shanghai, China, indicated that the proportions of infants with parental soothing dropped from 96.1% at age 42 days to 78.5% at age 12 months [27]. Therefore, further research is needed to examine the soothing methods during the early childhood period in Chinese population.
To the best of our knowledge, most previous studies have only focused on a single factor of sleep arrangements or soothing methods on the development of infant sleep. In addition, only a few studies have examined the effects of both factors, especially in China, and the reasons for bed-sharing among Chinese populations have not been reported. To address these gaps, this multicenter cross-sectional study was conducted to (1) examine the prevalence of sleep arrangements and soothing methods, (2) determine the reasons for bed-sharing, and (3) explore the associations among sleep arrangements, soothing methods, and sleep problems for children under 3 years in China.
-
This study was a part of the Development and Evaluation of the Chinese Infant and Toddler Sleep Assessment Scale Project, which was conducted from July to November in 2019. This project collected cross-sectional data from six communities and six townships from six provinces in China. The selection of participants was based on a three-stage separate sampling at the provincial, municipal, and community/township levels. At the provincial level, six provinces were selected from the eastern, central, and western regions of China according to geographical location, with two provinces in each region. At the municipal level, one city per study province was chosen. The maternal and children’s hospitals of every city were contacted by the research team to join our study. These hospitals have close contact with the local community health service centers (CHSC) and provide technical guidance for CHSC. At the community/township level, one community and one township with moderate health service capacity and sufficient eligible samples from each city were randomly selected to cover both urban and rural populations. According to the children’s list in CHSC, children aged < 3 years were randomly chosen as sample in each community/township. The sample size of the project was 1,212, calculated based on the number of items in the Chinese Infant and Toddler Sleep Assessment Scale. A total of 104 children in each community/township were randomly chosen.
The inclusion/exclusion criteria of the participants were consistent throughout the project. The inclusion criteria were as follows: (1) permanent urban and rural residents (resided in the location for more than half a year), (2) full term (gestational age ≥ 37 and < 42 weeks), and (3) birth weight ≥ 2,500 g and < 4,000 g. The exclusion criteria were as follows: (1) child had any congenital diseases or experienced any complication at birth or (2) suffered from diseases (e.g., intestinal spasm, gastroesophageal reflux, eczema, cold, and diarrhea) or contagious diseases in the past 2 weeks.
Data were collected using questionnaires completed by the caregivers who mainly took care of the child’s sleep. On-site surveys were conducted by trained doctors from each municipal maternal and children’s hospital, who were responsible for sampling and providing guidance to participants in filling out the questionnaires.
All caregivers gave informed consent for inclusion before they participated in the study. The study was approved by the Ethical Review Committee of the National Center for Women and Children’s Health, Chinese Center for Disease Control and Prevention.
-
Demographics A self-designed demographic questionnaire was used to collect demographic information, such as residential area, caregiver’s identity, caregiver’s age, caregiver’s education level, family’s monthly income, child’s age, and child’s gender.
Sleep Measure The Brief Infant Sleep Questionnaire (BISQ) was used to measure children’s sleep patterns and practices [12]. BISQ is a brief and widely used screening questionnaire to assess sleep quantity and quality in the first 3 years of life. This questionnaire has been validated against actigraphy and sleep logs. The Chinese version of the BISQ has been used in previous studies [11, 22]. The child’s primary caregiver was instructed to complete the BISQ with reference to their child’s sleep characteristics during the past week. In this study, two variables of sleep patterns and two variables of sleep practices in BISQ were analyzed, including the number of night awakenings, latency to falling asleep for the night, sleeping arrangements, and soothing methods.
Reasons for Bed-sharing A self-designed questionnaire was used to record the reasons for bed-sharing. The question was “What is the reason for bed-sharing with your child (single choice)?” The reasons for bed-sharing were categorized into ease of breastfeeding/feeding, convenience for monitoring and taking care of the child or patting/holding after night awakenings, bonding, natural for young child, and others. The caregivers were instructed to mark only one (most appropriate) choice, when they respond to items with a few options.
-
A total of 1,282 caregivers of children aged < 3 years filled out the BISQ and demographic questionnaire. Participants whose demographic information, namely, number of night awakenings, latency to falling asleep for the night, sleeping arrangements, and soothing methods, was missing (N = 87) were excluded. Except for areas and sleep arrangements, no difference was found in the distribution of other demographic information and sleep parameters between the included and excluded participants. Finally, data of 1,195 participants were analyzed in this study.
-
Continuous variables were presented as mean and standard deviation and categorical variables as frequency and percentages. In our study, we defined frequent night awakenings as more than or equal to three times per night and difficulty falling asleep as sleep latency more than 30 minutes according to previous studies [28, 29]. These sleep measures were selected based on background data and the aims of the study. In addition, frequent night awakenings and difficulty falling asleep are among the most common complaints of families and child-care professionals [30]. In this study, frequent night awakenings and difficulty falling asleep across age groups were compared using the Chi-square test. The bivariate association between sleep variables (i.e., frequent night awakenings and difficulty falling asleep) and sleep arrangements, soothing methods, and demographic variables was examined using the Chi-square test. Logistic regression models were established to examine the factors of frequent night awakenings and difficulty falling asleep and to calculate the odds ratio (OR) and 95% confidence intervals (95% CI). Frequent night awakenings and difficulty falling asleep were used as dependent variables, sleep arrangements, soothing methods, and demographic variables as independent variables. According to previous evidence related to sleep problems in early childhood and variables involved in this study, covariates of child’s age and gender, area, caregiver’s age and education level and family’s monthly income [4, 31, 32] were included in the adjusted models. A test with a P-value < 0.05 was considered significant. All analyses were performed with SPSS 18.0.0 (SPSS Inc., Chicago, America).
-
The demographic characteristics of the study participants are presented in Table 1. The number of participants in urban and rural areas was the same. Of the 1,195 caregivers, 84.8% were mothers, 73.1% of them were 26–35 years old, and nearly two-thirds (63.6%) had college or higher education. About half of the children were boys (51.8%).
Table 1. Demographic characteristics of the study participants (N = 1,195)
Characteristic Subgroup N (%) Area Urban 604 (50.5) Rural 591 (49.5) Child’s age (months) 0–5 425 (35.6) 6–11 328 (26.6) 12–23 234 (19.6) 24–35 218 (18.2) Child’s gender Boy 619 (51.8) Girl 576 (48.2) Caregiver’s identity Mother 1,013 (84.8) Father 130 (10.9) Others 52 (4.3) Caregiver’s age (years) 20–25 146 (12.2) 26–30 535 (44.8) 31–35 338 (28.3) ≥ 36 176 (14.7) Caregiver’s education level High school or lower 435 (36.4) College or higher 760 (63.6) Family’s monthly income (RMB) ≤ 5,000 263 (22.0) 5,001–10,000 472 (39.5) > 10,000 460 (38.5) -
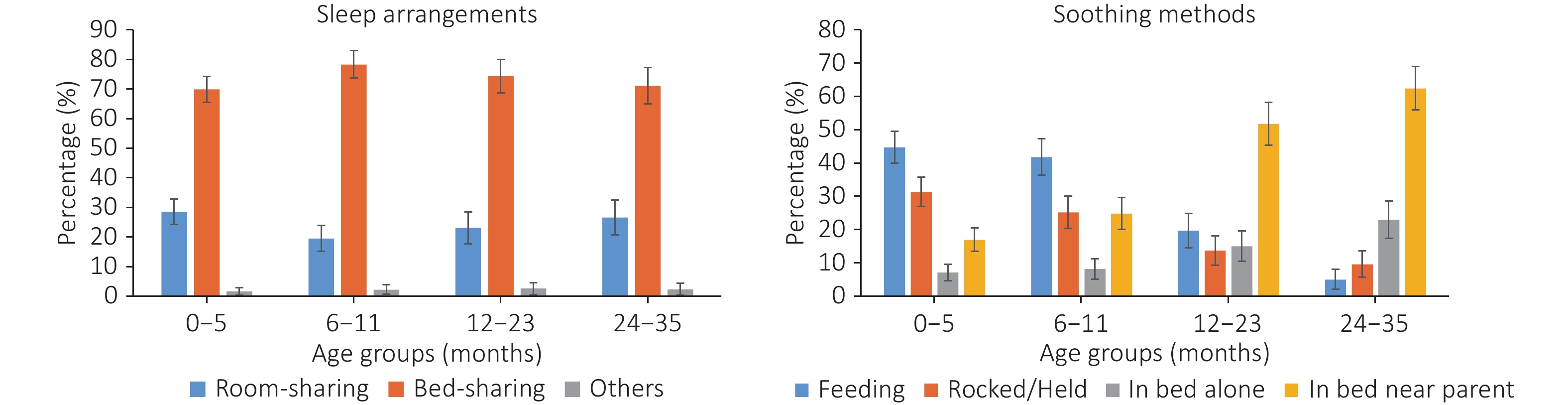
Figure 1 presents the prevalence of sleep arrangements and soothing methods at different ages. The bed-sharing practice was very prevalent at any age, ranging from 69.9% at 0–5 months to 78.3% at 6–11 months. The bed-sharing rate increased gradually before age 1 year and then decreased gradually. However, no significant difference was found among age groups (χ2 = 9.16, P = 0.165). As regards soothing methods, most infants fell asleep while feeding, ranging from 41.8% to 44.7% before age 1 year. As the child grows, the rate of feeding and being rocked/held to fall asleep declined steadily, whereas the rate of falling asleep in bed near parents increased gradually (χ2 = 285.87, P < 0.001). By age 35 months, 62.4% of the children fell asleep in bed near their parents. The rates of falling asleep in bed alone were the lowest before age 1 year, ranging from 7.1% at 0–5 months to 8.2% at 6–11 months, and increased to 22.9% by 35 months.
-
The most common reason for bed-sharing for infants before age 6 months was breastfeeding/feeding (44.9%). After age 6 months, more than half of the caregivers chose bed-sharing because of convenience, ranging from 55.4% at 6–11 months to 70.2% at 24–35 months (Table 2).
Table 2. Distribution of reasons for bed-sharing [n (%)]
Reason 0–5 months 6–11 months 12–23 months 24–35 months Breastfeeding/feeding 119 (44.9) 67 (29.0) 19 (12.4) 2 (1.4) Convenience 103 (38.9) 128 (55.4) 90 (58.8) 99 (70.2) Bonding 7 (2.6) 7 (3.0) 13 (8.5) 14 (9.9) Natural 26 (9.8) 24 (10.4) 23 (15.0) 20 (14.2) Others 10 (3.8) 5 (2.2) 8 (5.2) 6 (4.3) -
The results of the bivariate analyses with regard to factors related to frequent night awakenings and difficulty falling asleep are presented in Table 3. The rate of frequent night awakenings tended to decrease with age, from 38.6% at 0–5 months to 2.3% at 24–35 months (χ2 = 138.86, P < 0.001). Globally, 22.5% of children aged 0–35 months experienced frequent night awakenings, and 13.6% of children across all ages have difficulty falling asleep, and the lowest prevalence was noted in children aged 6–11 months (χ2 = 11.10, P = 0.011). A significant association was noted between soothing methods and frequent night awakenings (P < 0.001) and difficulty falling asleep (P = 0.022). Among children, boys (P = 0.042) were likely to have frequent night awakenings, and families with monthly income ≤ 5,000 RMB (P = 0.030) were more likely to report difficulty falling asleep. No significant differences were found between different sleep arrangements (bed-sharing or not), area, caregiver’s age, and education.
Table 3. Variables associated with frequent night awakenings and difficulty falling asleep by bivariate analyses [n (%)]
Characteristic Subgroup Frequent night awakenings Difficulty falling asleep No Yes P No Yes P Child’s age
(months)0–5 261 (61.4) 164 (38.6) < 0.001 349 (82.1) 76 (17.9) 0.011 6–11 240 (75.6) 78 (24.5) 286 (89.9) 32 (10.1) 12–23 212 (90.6) 22 (9.4) 206 (88.0) 28 (12.0) 24–35 213 (97.7) 5 (2.3) 192 (88.1) 26 (11.9) Area Urban 469 (77.6) 135 (22.4) 0.894 528 (87.4) 76 (12.6) 0.320 Rural 457 (77.3) 134 (22.7) 505 (85.4) 86 (14.6) Child’s gender Boy 465 (75.1) 154 (24.9) 0.042 536 (86.6) 83 (13.4) 0.877 Girl 461 (80.0) 115 (20.0) 497 (86.3) 79 (13.7) Caregiver’s age
(years)20–25 110 (75.3) 36 (24.7) 0.060 127 (87.0) 19 (13.0) 0.132 26–30 405 (75.7) 130 (24.3) 449 (83.9) 86 (16.1) 31–35 261 (77.2) 77 (22.8) 301 (89.1) 37 (10.9) ≥ 36 150 (85.2) 26 (14.8) 156 (88.6) 20 (11.4) Caregiver’s Education level High school or lower 343 (78.9) 92 (21.1) 0.394 372 (85.5) 63 (14.5) 0.479 College or higher 583 (76.7) 177 (23.3) 661 (87.0) 99 (13.0) Family’s monthly income (RMB) ≤ 5,000 200 (76.0) 63 (24.0) 0.473 215 (81.7) 48 (18.3) 0.030 5,001–10,000 361 (76.5) 111 (23.5) 410 (86.9) 62 (13.1) > 10,000 365 (79.3) 95 (20.7) 408 (88.7) 52 (11.3) Bed-sharing No 251 (78.4) 69 (21.6) 0.635 276 (86.2) 44 (13.8) 0.906 Yes 675 (77.1) 200 (22.9) 757 (86.5) 118 (13.5) Soothing methods In bed alone 127 (90.1) 14 (9.9) < 0.001 133 (94.3) 8 (5.7) 0.022 Feeding 218 (57.4) 162 (42.6) 330 (86.8) 50 (13.2) Rocked/held 217 (81.6) 49 (18.4) 224 (84.2) 42 (15.8) In bed near parents 364 (89.2) 445 (10.8) 346 (84.8) 62 (15.2) The results of the logistic regression analyses are presented in Table 4. Children who fell asleep while feeding were more likely to have frequent night awakenings (OR = 3.50, 95% CI 1.87–6.54). The risks of having difficulty falling asleep were almost three times higher in children who fell asleep being rocked/held (OR = 2.72, 95% CI 1.21–6.12) and in bed near parents (OR = 2.89, 95% CI 1.33–6.28). In addition, significant associations were found between sleep variables and child’s age, gender, and family’s monthly income. No association was noted between bed-sharing and sleep variables.
Table 4. Variables associated with frequent night awakenings and difficulty falling asleep by logistic regression (N = 1,195)
Item Frequent night awakenings Difficulty falling asleep β P OR (95% CI) β P OR (95% CI) Constants −1.19 0.007 −2.09 < 0.001 Child’s age (Ref: 0–5 months) 6–11 −0.67 < 0.001 0.51 (0.37, 0.72) −0.65 0.004 0.52 (0.33, 0.82) 12–23 −1.56 < 0.001 0.21 (0.13, 0.35) −0.50 0.054 0.61 (0.38, 1.01) 24–35 −2.83 < 0.001 0.06 (0.02, 0.15) −0.43 0.122 0.65 (0.38, 1.12) Child’s gender (Ref: boy) −0.35 0.025 0.71 (0.52, 0.96) 0.01 0.953 1.01 (0.72, 1.42) Area (Ref: urban) 0.12 0.476 1.13 (0.81, 1.56) −0.02 0.933 0.98 (0.68, 1.43) Caregiver’s age (Ref: 20–25 years) 26–30 0.18 0.463 1.20 (0.74, 1.93) 0.31 0.268 1.37 (0.79, 2.39) 31–35 0.12 0.655 1.12 (0.68, 1.87) −0.06 0.848 0.94 (0.51, 1.74) ≥ 36 −0.16 0.623 0.86 (0.46, 1.60) −0.07 0.833 0.93 (0.47, 1.85) Caregiver’s education level
(Ref: High school or lower)0.12 0.511 1.13 (0.79, 1.61) −0.04 0.861 0.97 (0.65, 1.43) Family’s monthly income (Ref: ≤ 5,000 RMB) 5,001–10,000 −0.02 0.931 0.98 (0.66, 1.48) −0.37 0.097 0.69 (0.45, 1.07) > 10,000 −0.07 0.774 0.94 (0.60, 1.47) −0.53 0.034 0.59 (0.36, 0.96) Bed-sharing (Ref: no) 0.07 0.712 1.07 (0.75, 1.52) −0.10 0.625 0.91 (0.61, 1.34) Soothing methods
(Ref: alone)Feeding 1.25 < 0.001 3.50 (1.87, 6.54) 0.76 0.066 2.13 (0.95, 4.76) Rocked/held 0.05 0.879 1.05 (0.54, 2.05) 1.00 0.015 2.72 (1.21, 6.12) In bed near parents 0.11 0.755 1.11 (0.57, 2.18) 1.06 0.007 2.89 (1.33, 6.28) -
This study found that bed-sharing practices and excessive parental involvement when falling asleep were prevalent across the early childhood period in the Chinese population. Children who fell asleep with parental involvement were more likely to have frequent night awakenings and difficulty falling asleep. We did not find an association between bed-sharing and sleep patterns in infants and toddlers.
-
Our findings indicated that bed-sharing remained very prevalent at any age during early childhood, ranging from 69.9% to 78.3%. This result is similar to the finding of a previous cross-cultural study of 29,287 children aged 0–36 months in 17 countries. This study reported that the proportion of Chinese young children sleeping in their parents’ bed was as high as 67.6%, which was significantly higher than that of predominantly Caucasian countries (5.00%–15.14%) [11]. The difference in sleep arrangements may stem from different cultural values. Families who value family interdependence were much more likely to share beds than those who emphasize independence [11, 13]. Bed-sharing appears to be a traditional sleep parenting behavior in China. During the period from 2004 to 2005, Huang et al. conducted a national epidemiological survey in 12 cities in China and revealed that 57.7%, 66.1%, and 65.2% of children aged 0–1, 1–2, and 2–3 years slept in the same bed with parents, respectively [33]. Compared with a decade ago, the practice of bed-sharing for Chinese young children in the present study has persisted and increased slightly. However, to reduce the risk of SIDS, room-sharing without bed-sharing is widely recommended for infants, including the Chinese health standard Guideline for sleep hygiene among children aged 0–5 years [34].
In our study, parents of infants younger than 6 months chose bed-sharing mainly because of breastfeeding/feeding, and after 6 months of age, convenience for comfort/monitoring became the main reason. This may be consistent with the gradual decrease in breastfeeding/feeding at night as child age. A previous systematic review summarized the results of 34 studies mainly from the United States, Australia, and New Zealand and found that breastfeeding and comforting were the most common reasons for bed-sharing in infants [23]. Mileva-Seitz et al. systematically reviewed 659 published papers on the topic of parent-child bed-sharing and indicated a positive association between breast feeding and bed-sharing [35]. However, a longitudinal study of 524 infants followed up until 8 months postpartum and a cross-sectional study of 14,883 children aged 0–5 years in China did not find associations between infants’ feeding methods and bed-sharing [15, 33]. Therefore, in view of the high prevalence of bed-sharing among Chinese young children, further research on its influencing factors and underlying reasons is needed.
Bed-sharing has also been found to be associated with frequent night awakenings and difficulty falling asleep in some previous studies [19, 20, 36]. For example, a longitudinal study of 18 infants followed up between 3 and 15 months, which used a portable time-lapse video recording system, revealed that co-sleeping infants had a mean of 5.8 awakenings per night while solitary sleeping infants had a mean of 3.2 awakenings per night [19]. However, our study did not find a relationship between bed-sharing and frequent night awakenings and difficulty falling asleep after adjustment for soothing methods and demographic variables. As mentioned in the Introduction, other studies have not found a relationship between bed-sharing and infant sleep [15,21,22]. A longitudinal study of 139 infants reported that compared with families whose infants were solitary sleepers by 6 months, persistent co-sleeping was associated with sleep disruption in mothers but not in infants [21]. A longitudinal study of 524 infants and a cross-sectional study of 1,102 children (2–30 months) both did not find an association between bedroom sharing and frequent nighttime awakenings for infants and toddlers in China [15, 22]. In addition, a previous study revealed that some parents felt that bed-sharing could facilitate better sleep for infants [23]. These inconsistencies likely stemmed from the differences in the study population, sleep measures, sleep parameter definitions, and covariates included in the analysis.
-
Parental involvement in falling asleep in early childhood was very common in our study, as > 90% of infants and 75% of toddlers fell asleep with parental involvement. This incidence was close to the results of another domestic longitudinal cohort study of 262 infants, which indicated that 78.5%–96.1% of infants fell asleep with parental involvement [27]. Compared with data reported abroad, more young children in China could not fall asleep in bed alone. A longitudinal cohort study of 704 Italian infants revealed that the rates of infants who fell asleep alone were fixed at 20%–25% during the first year of life [10]. A study with 5,006 US–Canada infants and toddlers presented that the rate of falling asleep in crib alone increased from 18.9% to 52.7% by 1 year and increased to 62.86% by 3 years [4]. Therefore, the development of Chinese young children’s self-soothing ability appeared to be relatively slow. Therefore, it will be necessary to understand the underlying reasons for soothing to fall asleep, which will be helpful to develop targeted sleep education strategies.
Self-soothing refers to the ability to regulate states of arousal [24]. The capacity to “self-soothe” begins in the first 12 weeks of life [37]. The Asia Pacific Paediatric Sleep Alliance recommends that a good time to start teaching babies to fall asleep on their own is between 3 and 6 months of age [38]. A prospective study with 33 children reported that infants aged 12 months with the ability of self-soothe at night were less likely to have a sleep-related problem at age 2 years [26]. Inappropriate soothing methods of falling asleep tend to persist and cause trouble to children’s sleep and parental stress. The results of behavioral intervention studies have also confirmed that after reducing parental involvement, children’s difficulty falling asleep and night awakenings have been improved [39, 40].
Consistent with the findings of previous studies, we found that children who fell asleep in bed alone had less frequent night awakenings and difficulty falling asleep [12, 24, 25, 41]. A large Internet survey consisted of 1028 infants and young children (0–3 years of age) found that parents of infants who fell asleep in their cribs alone reported fewer night wakings, shorter periods of wakefulness during the night and shorter settling times [12]. A large prospective multidisciplinary nationally birth cohort study of 11,783 infants in France indicated that feeding to fall asleep was associated with frequent sleep-onset difficulties compared with never having sleep-onset difficulties [41]. Therefore, parents should help their infant to develop self-soothing skills and gradually reduce parental involvement.
-
This study was conducted in a large nationwide sample of infants and toddlers and was performed to explore the association of both sleep arrangements and soothing methods on early childhood sleep problems. To our knowledge, this was the first study to report the reasons for bed-sharing and soothing methods among Chinese populations. These findings might help health workers better understand early childhood sleep practice and develop appropriate interventions. Despite the important findings, this study has some limitations. First, sleep measures in this study were derived from caregivers’ self-reports, and a subjective report bias existed. Second, some factors that might confound the relationship between sleep arrangements, soothing methods, and sleep problems were not measured in this study, such as breastfeeding. Third, not all cities were selected in this study, and some participants were excluded, which may introduce some selection biases; thus, the conclusions may not be generalized to other populations. Finally, this was a cross-sectional study, so causality cannot be inferred. Future longitudinal studies are needed to investigate the effects of sleep arrangements and soothing methods on the sleep development during early childhood.
-
Our findings indicate that bed-sharing and parents’ involvement when falling asleep were very common during early childhood. Children who fell asleep with parental involvement were more likely to have frequent night awakenings and difficulty falling asleep. The most common reasons for bed-sharing were breastfeeding/feeding and convenience. Anticipatory guidance for sleep arrangements and soothing methods in young children is essential.
-
This was a multicenter study. Data were collected by child health care workers in Maternal and Children Health hospitals of Fangshan, Suzhou, Wuhan, Taiyuan, Baoji, and Guiyang city. We also thank all the families that participated in the study.
doi: 10.3967/bes2022.031
Understanding the Choice of Sleep Arrangements and Soothing Methods and Their Associations with Sleep Problems among Children Under 3 Years Old: A Chinese Population-Based Study
-
Abstract:
Objective This study aimed to examine the sleep arrangements and soothing methods and to assess their associations with sleep problems among children aged < 3 years in China. Methods A cross-sectional survey was conducted in 2019 from six provinces in China. A total of 1,195 caregivers of children aged 0–35 months were included in the study. Data on sleep arrangements, soothing methods, and sleep problems (i.e., frequent night awakenings and difficulty falling asleep) were assessed using the Brief Infant Sleep Questionnaire. The reasons for bed-sharing in sleep arrangements were recorded using a self-designed questionnaire. Results The bed-sharing practice was very prevalent at any age, which ranged from 69.9% to 78.3%. Most infants fell asleep while feeding or being rocked/held before age 12 months. By age 35 months, 62.4% of the children fell asleep in bed near parents. The most common reasons for bed-sharing were breastfeeding/feeding and convenience. Parental involvement when falling asleep was significantly related with frequent night awakenings and difficulty falling asleep. No association was found between bed-sharing and sleep. Conclusion Bed-sharing and parental involvement were very common among Chinese children aged < 3 years. Children who fall asleep with parental involvement were more likely to have sleep problems. -
Key words:
- Sleep arrangements /
- Soothing methods /
- Sleep /
- Children
-
Table 1. Demographic characteristics of the study participants (N = 1,195)
Characteristic Subgroup N (%) Area Urban 604 (50.5) Rural 591 (49.5) Child’s age (months) 0–5 425 (35.6) 6–11 328 (26.6) 12–23 234 (19.6) 24–35 218 (18.2) Child’s gender Boy 619 (51.8) Girl 576 (48.2) Caregiver’s identity Mother 1,013 (84.8) Father 130 (10.9) Others 52 (4.3) Caregiver’s age (years) 20–25 146 (12.2) 26–30 535 (44.8) 31–35 338 (28.3) ≥ 36 176 (14.7) Caregiver’s education level High school or lower 435 (36.4) College or higher 760 (63.6) Family’s monthly income (RMB) ≤ 5,000 263 (22.0) 5,001–10,000 472 (39.5) > 10,000 460 (38.5) Table 2. Distribution of reasons for bed-sharing [n (%)]
Reason 0–5 months 6–11 months 12–23 months 24–35 months Breastfeeding/feeding 119 (44.9) 67 (29.0) 19 (12.4) 2 (1.4) Convenience 103 (38.9) 128 (55.4) 90 (58.8) 99 (70.2) Bonding 7 (2.6) 7 (3.0) 13 (8.5) 14 (9.9) Natural 26 (9.8) 24 (10.4) 23 (15.0) 20 (14.2) Others 10 (3.8) 5 (2.2) 8 (5.2) 6 (4.3) Table 3. Variables associated with frequent night awakenings and difficulty falling asleep by bivariate analyses [n (%)]
Characteristic Subgroup Frequent night awakenings Difficulty falling asleep No Yes P No Yes P Child’s age
(months)0–5 261 (61.4) 164 (38.6) < 0.001 349 (82.1) 76 (17.9) 0.011 6–11 240 (75.6) 78 (24.5) 286 (89.9) 32 (10.1) 12–23 212 (90.6) 22 (9.4) 206 (88.0) 28 (12.0) 24–35 213 (97.7) 5 (2.3) 192 (88.1) 26 (11.9) Area Urban 469 (77.6) 135 (22.4) 0.894 528 (87.4) 76 (12.6) 0.320 Rural 457 (77.3) 134 (22.7) 505 (85.4) 86 (14.6) Child’s gender Boy 465 (75.1) 154 (24.9) 0.042 536 (86.6) 83 (13.4) 0.877 Girl 461 (80.0) 115 (20.0) 497 (86.3) 79 (13.7) Caregiver’s age
(years)20–25 110 (75.3) 36 (24.7) 0.060 127 (87.0) 19 (13.0) 0.132 26–30 405 (75.7) 130 (24.3) 449 (83.9) 86 (16.1) 31–35 261 (77.2) 77 (22.8) 301 (89.1) 37 (10.9) ≥ 36 150 (85.2) 26 (14.8) 156 (88.6) 20 (11.4) Caregiver’s Education level High school or lower 343 (78.9) 92 (21.1) 0.394 372 (85.5) 63 (14.5) 0.479 College or higher 583 (76.7) 177 (23.3) 661 (87.0) 99 (13.0) Family’s monthly income (RMB) ≤ 5,000 200 (76.0) 63 (24.0) 0.473 215 (81.7) 48 (18.3) 0.030 5,001–10,000 361 (76.5) 111 (23.5) 410 (86.9) 62 (13.1) > 10,000 365 (79.3) 95 (20.7) 408 (88.7) 52 (11.3) Bed-sharing No 251 (78.4) 69 (21.6) 0.635 276 (86.2) 44 (13.8) 0.906 Yes 675 (77.1) 200 (22.9) 757 (86.5) 118 (13.5) Soothing methods In bed alone 127 (90.1) 14 (9.9) < 0.001 133 (94.3) 8 (5.7) 0.022 Feeding 218 (57.4) 162 (42.6) 330 (86.8) 50 (13.2) Rocked/held 217 (81.6) 49 (18.4) 224 (84.2) 42 (15.8) In bed near parents 364 (89.2) 445 (10.8) 346 (84.8) 62 (15.2) Table 4. Variables associated with frequent night awakenings and difficulty falling asleep by logistic regression (N = 1,195)
Item Frequent night awakenings Difficulty falling asleep β P OR (95% CI) β P OR (95% CI) Constants −1.19 0.007 −2.09 < 0.001 Child’s age (Ref: 0–5 months) 6–11 −0.67 < 0.001 0.51 (0.37, 0.72) −0.65 0.004 0.52 (0.33, 0.82) 12–23 −1.56 < 0.001 0.21 (0.13, 0.35) −0.50 0.054 0.61 (0.38, 1.01) 24–35 −2.83 < 0.001 0.06 (0.02, 0.15) −0.43 0.122 0.65 (0.38, 1.12) Child’s gender (Ref: boy) −0.35 0.025 0.71 (0.52, 0.96) 0.01 0.953 1.01 (0.72, 1.42) Area (Ref: urban) 0.12 0.476 1.13 (0.81, 1.56) −0.02 0.933 0.98 (0.68, 1.43) Caregiver’s age (Ref: 20–25 years) 26–30 0.18 0.463 1.20 (0.74, 1.93) 0.31 0.268 1.37 (0.79, 2.39) 31–35 0.12 0.655 1.12 (0.68, 1.87) −0.06 0.848 0.94 (0.51, 1.74) ≥ 36 −0.16 0.623 0.86 (0.46, 1.60) −0.07 0.833 0.93 (0.47, 1.85) Caregiver’s education level
(Ref: High school or lower)0.12 0.511 1.13 (0.79, 1.61) −0.04 0.861 0.97 (0.65, 1.43) Family’s monthly income (Ref: ≤ 5,000 RMB) 5,001–10,000 −0.02 0.931 0.98 (0.66, 1.48) −0.37 0.097 0.69 (0.45, 1.07) > 10,000 −0.07 0.774 0.94 (0.60, 1.47) −0.53 0.034 0.59 (0.36, 0.96) Bed-sharing (Ref: no) 0.07 0.712 1.07 (0.75, 1.52) −0.10 0.625 0.91 (0.61, 1.34) Soothing methods
(Ref: alone)Feeding 1.25 < 0.001 3.50 (1.87, 6.54) 0.76 0.066 2.13 (0.95, 4.76) Rocked/held 0.05 0.879 1.05 (0.54, 2.05) 1.00 0.015 2.72 (1.21, 6.12) In bed near parents 0.11 0.755 1.11 (0.57, 2.18) 1.06 0.007 2.89 (1.33, 6.28) -
[1] McLaughlin Crabtree V, Williams NA. Normal sleep in children and adolescents. Child Adolesc Psychiatr Clin N Am, 2009; 18, 799−811. doi: 10.1016/j.chc.2009.04.013 [2] Zhang Y, Sanders M, Feng WW, et al. Using epidemiological data to identify needs for child-rearing support among Chinese parents: a cross-sectional survey of parents of children aged 6 to 35 months in 15 Chinese cities. BMC Public Health, 2019; 19, 1470. doi: 10.1186/s12889-019-7635-y [3] Williamson AA, Mindell JA, Hiscock H, et al. Child sleep behaviors and sleep problems from infancy to school-age. Sleep Med, 2019; 63, 5−8. doi: 10.1016/j.sleep.2019.05.003 [4] Sadeh A, Mindell JA, Luedtke K, et al. Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res, 2009; 18, 60−73. doi: 10.1111/j.1365-2869.2008.00699.x [5] Jiang F, Shen XM, Yan CG, et al. Epidemiological study of sleep characteristics in Chinese children 1–23 months of age. Pediatr Int, 2007; 49, 811−6. doi: 10.1111/j.1442-200X.2007.02449.x [6] Huang X N, Jiang J X, Ma Y Y, et al. Study on sleep habit and sleep disorder among children aged 0–5 years. Chin J Child Health Care, 2006; 14, 585−7. (In Chinese [7] Netsi E, Santos IS, Stein A, et al. A different rhythm of life: sleep patterns in the first 4 years of life and associated sociodemographic characteristics in a large Brazilian birth cohort. Sleep Med, 2017; 37, 77−87. doi: 10.1016/j.sleep.2017.06.001 [8] Byars KC, Yolton K, Rausch J, et al. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics, 2012; 129, e276−84. doi: 10.1542/peds.2011-0372 [9] Al Mamun A, O'Callaghan F, Scott J, et al. Continuity and discontinuity of trouble sleeping behaviors from early childhood to young adulthood in a large Australian community-based-birth cohort study. Sleep Med, 2012; 13, 1301−6. doi: 10.1016/j.sleep.2012.07.003 [10] Bruni O, Baumgartner E, Sette S, et al. Longitudinal study of sleep behavior in normal infants during the first year of life. J Clin Sleep Med, 2014; 10, 1119−27. doi: 10.5664/jcsm.4114 [11] Mindell JA, Sadeh A, Wiegand B, et al. Cross-cultural differences in infant and toddler sleep. Sleep Med, 2010; 11, 274−80. doi: 10.1016/j.sleep.2009.04.012 [12] Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics, 2004; 113, e570−7. doi: 10.1542/peds.113.6.e570 [13] Zreik G, Asraf K, Tikotzky L, et al. Sleep ecology and sleep patterns among infants and toddlers: a cross-cultural comparison between the Arab and Jewish societies in Israel. Sleep Med, 2020; 75, 117−27. doi: 10.1016/j.sleep.2020.07.017 [14] Hauck FR, Signore C, Fein SB, et al. Infant sleeping arrangements and practices during the first year of life. Pediatrics, 2008; 122 Suppl 2, S113-20. [15] Huang XN, Wang HS, Chang JJ, et al. Feeding methods, sleep arrangement, and infant sleep patterns: a Chinese population-based study. World J Pediatr, 2016; 12, 66−75. doi: 10.1007/s12519-015-0012-8 [16] Blair PS, Heron J, Fleming PJ. Relationship between bed sharing and breastfeeding: longitudinal, population-based analysis. Pediatrics, 2010; 126, e1119−26. doi: 10.1542/peds.2010-1277 [17] The Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol #6: guideline on co-sleeping and breastfeeding. Revision, March 2008. Breastfeed Med, 2008; 3, 38−43. [18] Task Force on Sudden Infant Death Syndrome, Moon RY, Darnall RA, et al. SIDS and other sleep-related infant deaths: updated 2016 Recommendations for a safe infant sleeping environment. Pediatrics, 2016; 138, e20162938. doi: 10.1542/peds.2016-2938 [19] Mao A, Burnham MM, Goodlin-Jones BL, et al. A comparison of the sleep-wake patterns of cosleeping and solitary-sleeping infants. Child Psychiatry Hum Dev, 2004; 35, 95−105. doi: 10.1007/s10578-004-1879-0 [20] Ramos KD, Youngclarke D, Anderson JE. Parental perceptions of sleep problems among co-sleeping and solitary sleeping children. Inf Child Dev, 2007; 16, 417−31. doi: 10.1002/icd.526 [21] Teti DM, Shimizu M, Crosby B, et al. Sleep arrangements, parent-infant sleep during the first year, and family functioning. Dev Psychol, 2016; 52, 1169−81. doi: 10.1037/dev0000148 [22] Sun WQ, Li SX, Jiang YR, et al. A community-based study of sleep and cognitive development in infants and toddlers. J Clin Sleep Med, 2018; 14, 977−84. doi: 10.5664/jcsm.7164 [23] Ward TCS. Reasons for mother-infant bed-sharing: a systematic narrative synthesis of the literature and implications for future research. Matern Child Health J, 2015; 19, 675−90. doi: 10.1007/s10995-014-1557-1 [24] Burnham MM, Goodlin-Jones BL, Gaylor EE, et al. Nighttime sleep-wake patterns and self-soothing from birth to one year of age: a longitudinal intervention study. J Child Psychol Psychiatry, 2002; 43, 713−25. doi: 10.1111/1469-7610.00076 [25] Anuntaseree W, Mo-Suwan L, Vasiknanonte P, et al. Night waking in Thai infants at 3 months of age: association between parental practices and infant sleep. Sleep Med, 2008; 9, 564−71. doi: 10.1016/j.sleep.2007.07.009 [26] Gaylor EE, Goodlin-Jones BL, Anders TF. Classification of young children's sleep problems: a pilot study. J Am Acad Child Adolesc Psychiatry, 2001; 40, 61−7. doi: 10.1097/00004583-200101000-00017 [27] Dong SM, Lin QM, Zhu LX, et al. Sleep patterns and sleep-related factors in normal infants: a prospective cohort study. Chin Ment Health J, 2016; 30, 721−7. (In Chinese [28] Wang L, Jansen W, Boere-Boonekamp MM, et al. Sleep and body mass index in infancy and early childhood (6-36 mo): a longitudinal study. Pediatr Obes, 2019; 14, e12506. doi: 10.1111/ijpo.12506 [29] Sha TT, Yan Y, Gao X, et al. Association between sleep and body weight: a panel data model based on a retrospective longitudinal cohort of Chinese infants. Int J Environ Res Public Health, 2017; 14, 458. doi: 10.3390/ijerph14050458 [30] Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev, 2010; 14, 89−96. doi: 10.1016/j.smrv.2009.05.003 [31] Nevarez MD, Rifas-Shiman SL, Kleinman KP, et al. Associations of early life risk factors with infant sleep duration. Acad Pediatr, 2010; 10, 187−93. doi: 10.1016/j.acap.2010.01.007 [32] Costanian C, Abdullah P, Sawh N, et al. Factors associated with shorter night-time sleep in toddlers: the survey of young Canadians. Can J Public Health, 2017; 108, e571−7. doi: 10.17269/CJPH.108.6236 [33] Wang HS, Huang XN, Jiang JX, et al. Sleep location in Chinese children aged 0–5 years old. Chin J Child Health Care, 2008; 16, 420−2. (In Chinese [34] National Health and Family Planning Commission of the People's Republic of China. Guideline for sleep hygiene among children aged 0–5 years. 2018. http://www.nhc.gov.cn/wjw/pqt/201710/e63c5fc4c3d74daf9f5234150c4f400a.shtml. [2021-08-11]. (In Chinese) [35] Mileva-Seitz VR, Bakermans-Kranenburg MJ, Battaini C, et al. Parent-child bed-sharing: the good, the bad, and the burden of evidence. Sleep Med Rev, 2017; 32, 4−27. [36] DeLeon CW, Karraker KH. Intrinsic and extrinsic factors associated with night waking in 9-month-old infants. Infant Behav Dev, 2007; 30, 596−605. doi: 10.1016/j.infbeh.2007.03.009 [37] Owens JA, Mindell JA. Pediatric insomnia. Pediatr Clin North Am, 2011; 58, 555−69. doi: 10.1016/j.pcl.2011.03.011 [38] Asia Pacific Paediatric Sleep Alliance. Recommendations for better baby sleep from a global sleep survey. http://www.appsasleep.org/node/17/download/dd78d1b5e5b2374f064a504049e8284a. [2006-06-02]. [39] Gradisar M, Jackson K, Spurrier NJ, et al. Behavioral interventions for infant sleep problems: a randomized controlled trial. Pediatrics, 2016; 137, e20151486. doi: 10.1542/peds.2015-1486 [40] Hiscock H, Wake M. Randomised controlled trial of behavioural infant sleep intervention to improve infant sleep and maternal mood. BMJ, 2002; 324, 1062−5. doi: 10.1136/bmj.324.7345.1062 [41] Messayke S, Franco P, Forhan A, et al. Sleep habits and sleep characteristics at age one year in the ELFE birth cohort study. Sleep Med, 2020; 67, 200−6. doi: 10.1016/j.sleep.2019.11.1255 -





 下载:
下载:



 Quick Links
Quick Links