-
Sleep duration plays a crucial role in overall health and well-being and is associated with various aspects of daily functioning and quality of life[1,2]. Recent studies have further explored the implications of sleep duration on health in adolescent and elder adults[3-7]. Conversely, body pain can severely impact an individual's daily functioning and overall life satisfaction[8], whereas self-reported health status serves as a pivotal determinant of subjective well-being and life satisfaction[9]. Understanding the intricate interplay among these factors is essential for developing targeted interventions to improve health outcomes and enhance quality of life.
Previous studies have investigated the independent associations between sleep duration, body pain, self-reported health status, and life satisfaction. A systematic review highlighted the need to understand the mechanisms linking sleep and pain intensity to optimize pain management interventions, identifying putative mediators such as mood, depression, anxiety, stress, and physical activity[10]. Researchers reported that inadequate sleep duration was associated with an increased risk of mortality in a prospective study of men in the United States, highlighting the importance of sufficient sleep for overall health and longevity[11]. Furthermore, scholars have reported a positive correlation between better sleep quality and increased physical activity during the day among patients with chronic pain, underscoring the impact of sleep on pain management and functional outcomes[12]. Another study examined the interrelationships among sleep, pain, and mood disturbances in older adult patients at a pain clinic and provided insights into how sleep disturbances may contribute to both pain and mood disturbances, which in turn can impact life satisfaction. Furthermore, inadequate sleep has consistently been associated with lower life satisfaction, emphasizing the critical role of sufficient sleep in maintaining psychological and emotional well-being[13,14].
Chronic pain has been shown to adversely affect sleep quality and duration, suggesting a bidirectional relationship where pain disrupts sleep and poor sleep exacerbates pain perception[15,16]. The researchers also discussed the potential mediating role of sleep in the relationship between pain and various health outcomes, including life satisfaction[15]. Recent findings further support this connection, as two Mendelian randomization studies have identified that short sleep duration is causally associated with an increased risk of pain[6,7]. Additionally, one study revealed that sleep disturbances were linked to poorer health-related quality of life, both directly and indirectly, through their association with pain intensity[17]. Furthermore, physical, mental and social health status were found being associated with self-rated life satisfaction among older adults in India[18].
Gaps remain in our understanding of the mechanisms by which sleep duration relates to life satisfaction, particularly regarding the mediating effects of body pain and self-reported health status. Given the complex nature of these relationships, robust methodological approaches are crucial for accurately capturing the dynamic interplay among pain, sleep, and life satisfaction. Therefore, the aims of this study were to investigate 1) the associations of sleep duration with body pain, self-reported health status, and life satisfaction and 2) the sequential mediating roles of body pain and self-reported health status on the association between sleep duration and life satisfaction.
-
This study utilized fifth wave data from the China Health and Retirement Longitudinal Survey (CHARLS), which was accessed in 2020. The CHARLS, conducted by the China Center for Economic Research at Peking University, is a nationally representative longitudinal study focusing on middle-aged and older adults across 28 provinces in China. Comprehensive details regarding the CHARLS can be found in the cohort profile[19]. For this study, a total of 19,367 participants completed the fifth wave survey. We excluded individuals with missing data for any variables used in the analysis: individuals with missing data on sleep duration (n = 429), body pain, self-reported health status (n = 1,583), life satisfaction (n = 13), age, sex (n = 199), education (n = 9), marital status, smoking, alcohol consumption, and residence (n = 3). As a result, 17,131 eligible individuals were included in this cross-sectional analysis.
-
Sleep duration was evaluated with a single question: “In the past month, how many hours of sleep did you typically get at night?” Furthermore, nighttime sleep duration was categorized into five groups: < 6 hours, 6–7 hours, 7–8 hours, 8–9 hours, and > 9 hours. The continuous variable of sleep duration serves as the exposure (X) in the chain mediation analysis.
-
The participants responded to the question “Do you often experience distress due to pain?” with the following options: none (1), a little (2), somewhat (3), quite a bit (4), or very (5). We categorized “Body pain” into two binary variables: “quite a bit” or “very” indicated the presence of body pain, whereas “none” (1), “a little” (2), or “somewhat” (3) indicated the absence of body pain. The binary body pain variable was one of the outcomes the in Restricted Cubic Spline (RCS) analysis. We used the 5-point Likert scale data on body pain as the first mediator in the chain mediation analysis.
-
The participants responded to the question “How do you perceive your health condition?” with the following options: very good (1), good (2), fair (3), poor (4), or very poor (5). We categorized “Self-reported health status” into two binary variables: “very good” “good” and “fair” were classified as “good”, whereas “poor” and “very poor” were classified as “poor”. The binary self-reported health status variable was one of the outcomes in the RCS analysis. Additionally, we used the 5-point Likert scale data on self-reported health status as the second mediator in the chain mediation analysis.
-
The dependent variable of our study, life satisfaction, was based on the following question: “How satisfied are you with your life-as-a-whole?” The responses to the question were as follows: completely satisfied (1), very satisfied (2), somewhat satisfied (3), not very satisfied (4), or not at all satisfied (5). We categorized “life satisfaction” into two binary variables: “completely satisfied”, “very satisfied” and “somewhat satisfied” were classified as “satisfied”, whereas “not very satisfied” and “not at all satisfied” were classified as “not satisfied”. The binary life satisfaction variable was included as one of the outcomes in the RCS analysis, and we utilized the 5-point Likert scale data on life satisfaction as the outcome in the chain mediation analysis.
-
In the fifth wave of the CHARLS, sociodemographic data were collected, covering age, sex (male, female), education level [less than lower secondary (1), upper secondary & vocational training (2), tertiary (3)], marital status (married, unmarried), and residential area (rural, urban). Smoking status was categorized as nonsmoker or current or former smoker, whereas alcohol consumption status was classified as nondrinker or current or former drinker.
-
Descriptive statistics were employed to analyse the demographic characteristics and primary variables of interest. Associations between 5 sleep duration groups (exposure) and binary outcomes (body pain, self-reported health status and life satisfaction) were assessed via logistic regression models adjusted for age, sex, education level, marital status, smoking status, alcohol consumption status and residence. RCS analysis was conducted to evaluate the dose‒response relationships between sleep duration and binary outcomes (body pain, self-reported health status and life satisfaction).
-
Body pain: sleep duration group + covariates.
-
Self-reported health status: sleep duration groups + covariates.
-
Life satisfaction: sleep duration groups + covariates
Spearman correlation analysis was used to assess the associations between sleep duration and the five-point scales for body pain, self-reported health status, and life satisfaction, with Bonferroni correction applied to adjust for multiple comparisons. Chain mediation analysis was performed to examine the sequential mediating roles of body pain (M1) and self-reported health status (M2) in the association between sleep duration (X) and life satisfaction (Y), adjusting for age, sex, education level, marital status, smoking status, alcohol consumption status, and residence. The mediating effect was examined through a bootstrap estimation approach with 5000 repetitions, and the indirect effect was deemed significant if the 95% confidence interval did not encompass 0.
M1: a1 × X + Covariates
M2: a2 × X + d21 × M1 + Covariates
Y: b2 × M2 + b1 × M1 + c1 × X + Covariates
Indirect effect from X to Y via M1: a1 × b1
Indirect effect from X to Y via M2: a2 × b2
Indirect effect from X to Y via M1 and M2: a1 × d21 × b2
Total indirect effects: a1 × b1 + a2 × b2 + a1 × d21 × b2
Total direct effect: c1
Total effect = c1 + a1 × d21 × b2 + a1 × b1 + a2 × b2
Descriptive statistics, logistic regression and Spearman correlation analyses were performed via Stata for Windows software, version 17.1. RCS and chain mediation analysis were performed via R for Windows software, version 4.4.0. The significance threshold was set at P < 0.05.
-
Table 1 summarizes the demographic characteristics and primary variables of interest for the 17,131 participants. This study included 8,020 (46.82%) males and 9,111 (53.18%) females, with a mean age of 63.03 ± 9.51 years. Among the total sample, 14,940 (87.21%) individuals had an education level less than lower secondary, 1,828 (10.67%) had completed upper secondary or vocational training, and 363 (2.12%) had attained tertiary education. With respect to marital status, 14,582 (85.12%) individuals were married, whereas 2,549 (14.88%) currently were not in marriage. There were 6,627 (38.68%) individuals who reported previous smoking habits, 6,256 (36.52%) who reported consuming alcohol, and 1,013 (64.29%) who lived in rural areas.
Table 1. Demographic characteristics of the participants assessed in 2020 (n = 17,131)
Characteristics Mean ± Standard
deviation / n (%)Age, years 63.03 ± 9.51 Sex Male 8,020 (46.82) Female 9,111 (53.18) Education level Less than lower secondary 14,940 (87.21) Upper secondary & vocational training 1,828 (10.67) Tertiary 363 (2.12) Marital status Married 14,582 (85.12) Not in marriage 2,549 (14.88) Smoking Yes 6,627 (38.68) No 1,0504 (61.32) Alcohol consumption Yes 6,256 (36.52) No 1,0875 (63.48) Residence Urban 6,118 (35.71) Rural 11,013 (64.29) Sleep duration, h 6.07 ± 1.85 < 6 6,127 (35.77) 6– 4,297 (25.08) 7– 2,938 (17.15) 8– 2,649 (15.46) ≥ 9 1,120 (6.54) Body pain Yes 3,126 (18.25) No 14,005 (81.75) Self-reported health status Poor 4,233 (24.71) Good 12,898 (75.29) Life satisfaction Not Satisfied 1,373 (8.12) Satisfied 15,260 (89.08) Note. x = Mean, s = Standard Deviation. In terms of the cut-off for sleep duration, 6,127 (35.77%) individuals reported sleeping fewer than 6 hours, 4,297 (25.08%) reported sleeping between 6 and 7 hours, 2,938 (17.15%) reported sleeping 7–8 hours, 2,649 (15.46%) reported sleeping 8–9 hours, and 1,120 (6.54%) reported sleeping ≥ 9 hours. Furthermore, 3,126 (18.25%) individuals reported body pain, 4,233 (24.71%) reported poor health status, and 1,373 (8.12%) reported dissatisfaction with life (Table 1).
-
After adjustment for age, sex, education level, marital status, smoking status, alcohol consumption status and rural living status, compared with individuals who slept 7–8 hours, those who slept fewer than 6 hours [odds ratio (OR) = 2.322, 95% CI: 2.047–2.634, P < 0.001] and those who slept 6–7 hours (OR = 1.202, 95% CI: 1.043–1.385, P = 0.011) had an elevated risk of body pain. Conversely, there was no significant association between sleeping 8–9 hours (OR = 0.943, 95% CI: 0.801–1.111, P = 0.483) or sleeping ≥ 9 hours (OR = 1.119, 95% CI: 0.919–1.363, P = 0.264) and body pain compared with the reference group (Table 2).
Table 2. Associations between sleep duration and body pain, self-reported health status, and life satisfaction
Sleep duration (h) Body pain Self-reported health status Life satisfaction OR 95% CI P OR 95% CI P OR 95% CI P < 6 2.322 2.047−2.634 < 0.001 2.407 2.152−2.693 < 0.001 2.352 2.009−2.752 < 0.001 7– Ref. − − Ref. − − Ref. − − 6– 1.202 1.043−1.385 0.011 1.244 1.099−1.409 0.001 1.283 1.077−1.528 0.005 8– 0.943 0.801−1.111 0.483 1.010 0.877−1.163 0.889 0.976 0.796−1.197 0.816 ≥ 9 1.119 0.919−1.363 0.264 1.321 1.115−1.566 0.001 1.393 1.093−1.776 0.007 Note. CI: confidence Interval; OR: odds ratio; Ref: reference group. All the models were adjusted for age, sex, education level, marital status, smoking status, alcohol consumption status and residence. Furthermore, in terms of the associations with self-reported health status, individuals who slept < 6 hours (OR = 2.407, 95% CI: 2.152–2.693, P < 0.001), those who slept between 6 and fewer than 7 hours (OR = 1.244, 95% CI: 1.099–1.409, P = 0.001), and those who slept ≥ 9 hours (OR = 1.321, 95% CI: 1.115–1.566, P = 0.001) had a heightened risk of poor health status compared with individuals who slept 7–8 hours. Conversely, there was no significant association between sleeping 8–9 hours and poor health status compared with the reference group (OR = 1.010, 95% CI: 0.877–1.163, P = 0.889) (Table 2).
In addition, regarding the associations with life satisfaction, individuals who slept fewer than 6 hours (OR = 2.352, 95% CI: 2.009–2.752, P < 0.001), those who slept between 6 and 7 hours (OR = 1.283, 95% CI = 1.077, 1.528, P = 0.005), and those who slept ≥ 9 hours (OR = 1.393, 95% CI: 1.093–1.776, P = 0.007) had a heightened risk of dissatisfaction with life compared with individuals who slept 7–8 hours. Conversely, there was no significant association between sleeping between 8 and 9 hours and dissatisfaction with life compared with the reference group (OR = 0.976, 95% CI: 0.796–1.197, P = 0.816) (Table 2).
-
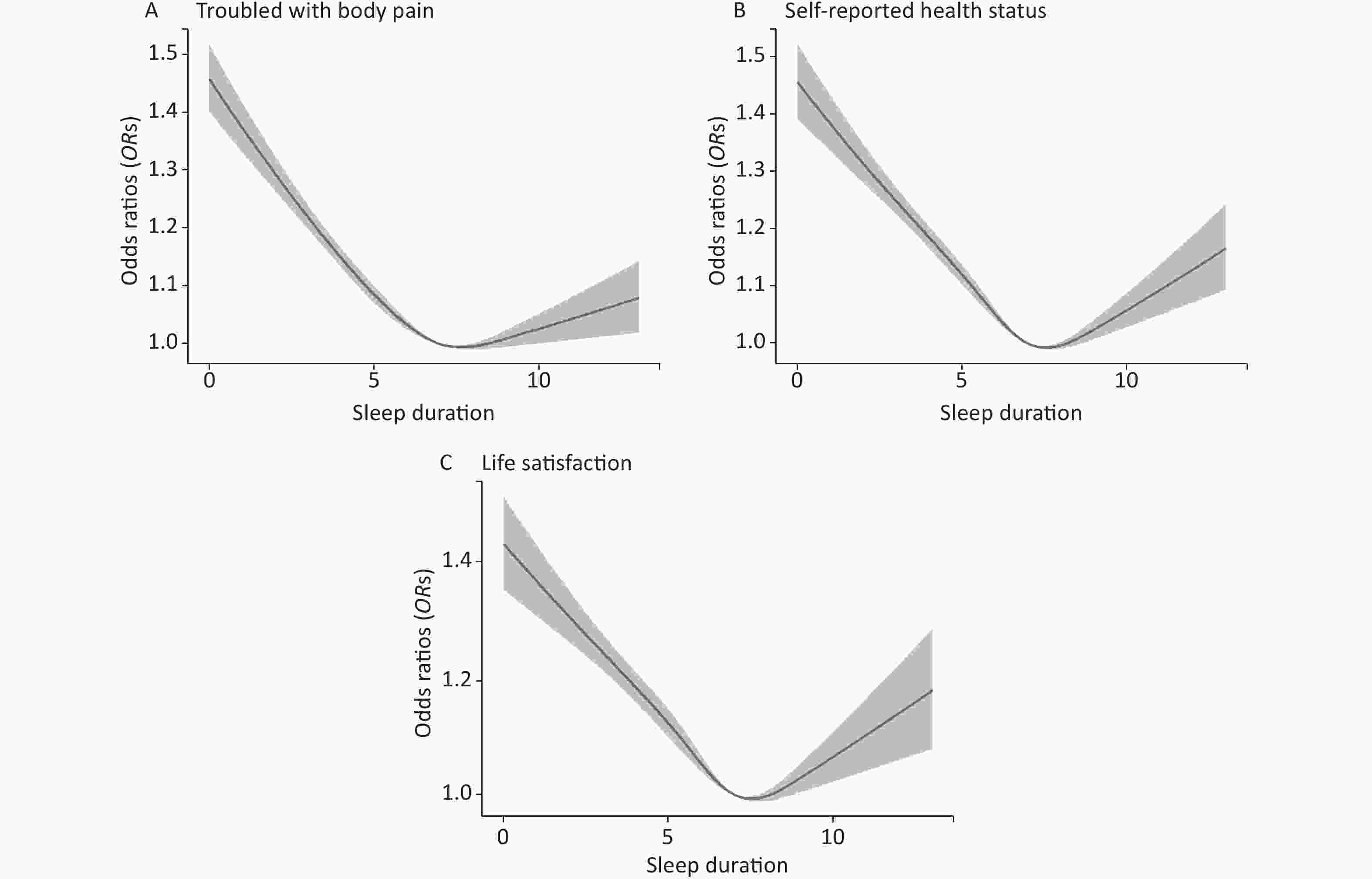
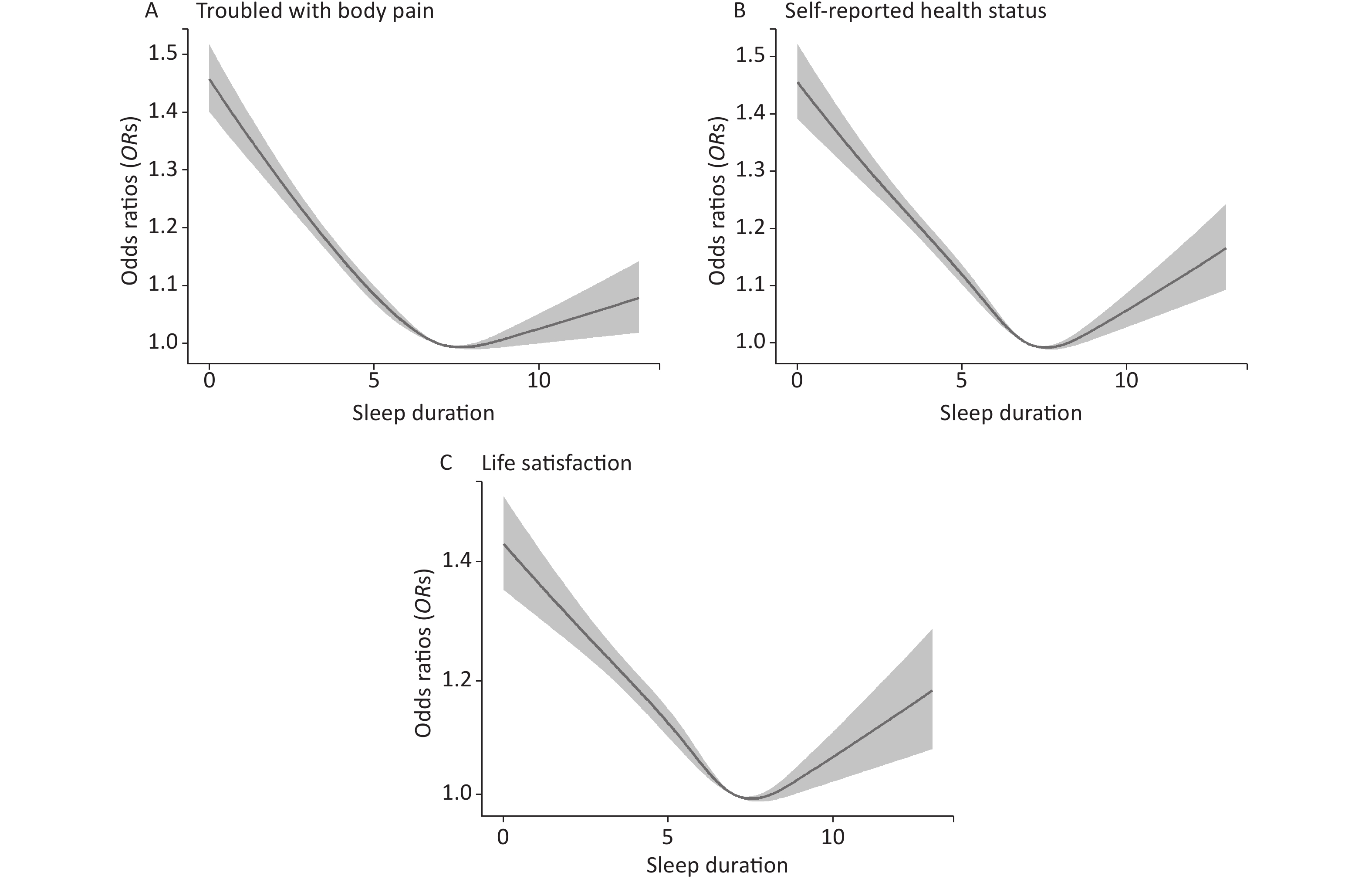
This study investigated the relationships between sleep duration and the risk of body pain, poor health status and dissatisfaction with life via RCS analysis. Figure 1 depicts a U-shaped pattern between sleep duration and the risk of body pain (Figure 1A), poor health status (Figure 1B) and dissatisfaction with life (Figure 1C). Specifically, at shorter sleep durations, there is a gradual decrease in the risk of body pain, poor health status, and dissatisfaction as sleep duration increases. However, once the duration of sleep exceeds 7 hours, the risk of body pain, poor health status, and dissatisfaction paradoxically escalates with further increases in sleep duration. This highlights a pivotal turning point in the trend of adverse outcome risk around a specific sleep duration (i.e., 7 hours), culminating in a U-shaped curve. Further statistical analysis robustly confirmed the statistical significance of this U-shaped relationship (nonlinear test P value: < 0.001).
-
After Bonferroni correction, the Spearman correlation revealed that sleep duration was negatively associated with body pain (r = −0.206, P < 0.001), self-reported health status (r = −0.205, P < 0.001) and life satisfaction (r = −0.117, P < 0.001). In addition, body pain was positively related to self-reported health status (r = 0.444, P < 0.001) and life satisfaction (r = 0.172, P < 0.001). Furthermore, self-reported health status was positively correlated with life satisfaction (r = 0.252, P < 0.001)(Table 3).
Table 3. Spearman correlations between sleep duration, body pain, self-reported status and life satisfaction
Variable 1 2 3 4 Sleep duration 1.000 Body pain −0.206*** 1.000 Self-reported status −0.205*** 0.444*** 1.000 Life satisfaction −0.117*** 0.172*** 0.252*** 1.000 Note. ***P < 0.001. -
A chain mediation analysis was conducted utilizing the “lavaan” package to explore the potential serial mediating roles of body pain and self-reported health status in the relationship between sleep duration and life satisfaction. First, we examined the association between sleep duration and body pain, revealing a negative relationship (β = −0.127, sx = 0.005, P < 0.001). These findings suggest that longer sleep duration is associated with a lower likelihood of body pain. Next, we investigated whether sleep duration and body pain were directly associated with self-reported health status. The results indicated that sleep duration was inversely related to self-reported health status (β = −0.061, sx = 0.004, P < 0.001), meaning that a longer sleep duration was associated with better perceived health. Conversely, body pain was positively associated with self-reported health status (β = 0.319, sx = 0.006, P < 0.001), indicating that individuals reporting more body pain tended to perceive their health as poorer. Finally, we delved into the interplay among sleep duration, body pain, self-reported health status, and life satisfaction. Sleep duration was negatively associated with life satisfaction (β = −0.028, sx = 0.003, P < 0.001), whereas body pain (β = 0.046, sx = 0.005, P < 0.001) and self-reported health status (β = 0.175, sx = 0.006, P < 0.001) were positively associated with life satisfaction (Figure 2 and Supplementary Table S1, available in www.besjournal.com). We utilized the bootstrap method with 5000 iterations to examine the mediating effects. A significant mediating effect was indicated by a 95% confidence interval that did not encompass 0. The total indirect effect of sleep duration (β = −0.024, sx = 0.001, 95% CI: −0.026 to −0.021, P < 0.001) on life satisfaction in the elderly population was decomposed into three pathways:
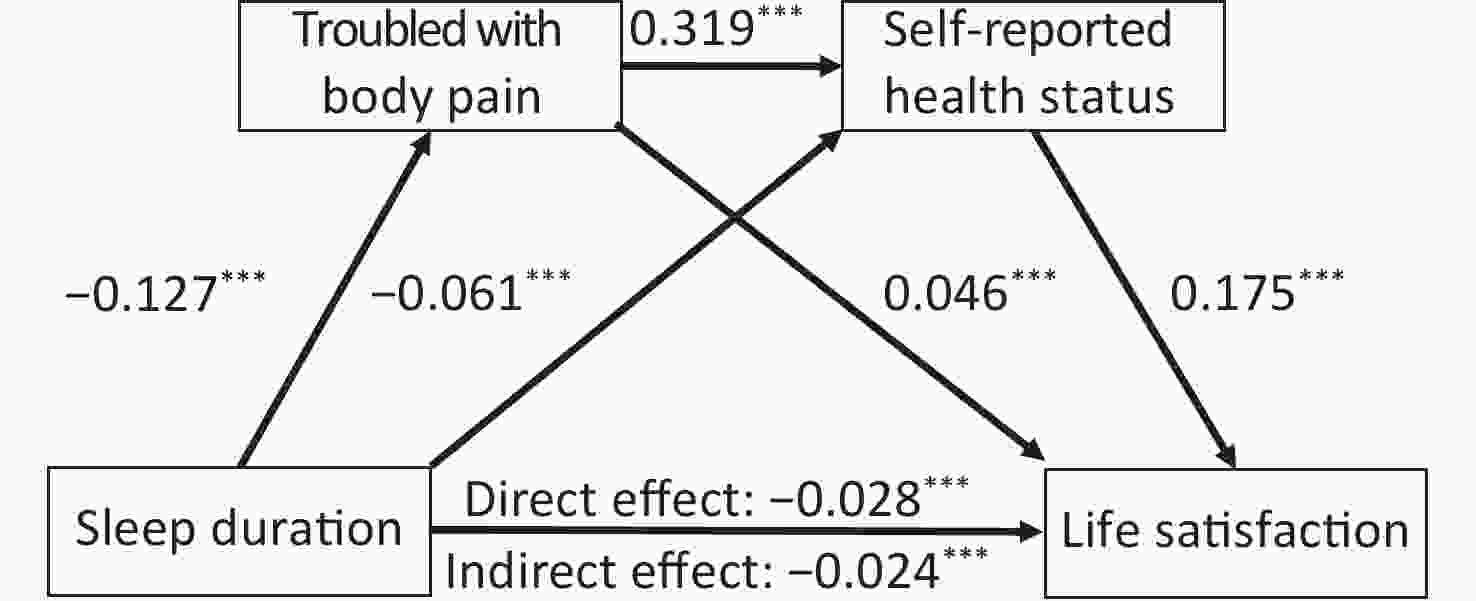
Figure 2. Chain mediation analysis. The models investigate the effect of sleep duration (independent variable) on life satisfaction. The sequential mediators in this analysis included body pain and self-reported health status. The mediation model was adjusted for age, sex, education level, marital status, smoking status, alcohol consumption status, and residence. ***P < 0.001.
Sleep duration → body pain → life satisfaction (β = −0.006, sx = 0.001, 95% CI: −0.007 to −0.004, P < 0.001).
Sleep duration → self-reported health status → life satisfaction (β = −0.011, sx = 0.001, 95% CI: −0.012 to −0.009, P < 0.001).
Sleep duration → body pain → self-reported health status → life satisfaction (β = −0.007, sx = 0.000, 95% CI: −0.008 to −0.006, P < 0.001) (Supplementary Table S2, available in www.besjournal.com).
Table S2. Results of the chain mediating effect based on Bootstrapping Test (n = 5,000). Estimates = non-standardized coefficients.
Estimates SE T P 95% CI LCI UCI Sleep duration → Troubled with body pain → Life satisfaction −0.006 0.001 −8.437 < 0.001 −0.007 −0.004 Sleep duration → Self-reported health status → Life satisfaction −0.011 0.001 −13.771 < 0.001 −0.012 −0.009 Sleep duration → Troubled with body pain → Self-reported health status →
Life satisfaction−0.007 0.000 −17.410 < 0.001 −0.008 −0.006 Total mediation effects −0.024 0.001 −21.406 < 0.001 −0.026 −0.021 Direct effect of sleep duration on life satisfaction −0.028 0.003 −8.626 < 0.001 −0.034 −0.022 Total effects of sleep duration on life satisfaction −0.052 0.003 −15.764 < 0.001 −0.058 −0.045 Proportion mediated by mediators 46.15% Note. CI: confidence interval; LCI: lower confidence interval; SE: standard error; UCL: upper confidence interval. The model adjusted for age, gender, education level, marital status, smoke, drink, and living residence. The effect of sleep duration on life satisfaction in the elderly population was partially serially mediated by body pain and self-reported health status, with a mediated proportion of 46.15% (Supplementary Table S2).
-
This study demonstrated U-shaped relationships between sleep duration and body pain, self-reported health status, and subjective life satisfaction in a national sample of Chinese elderly individuals. Furthermore, the chain mediation model revealed that body pain and self-reported health status were significantly associated with life satisfaction, whereas sleep duration had a negative and significant effect on life satisfaction in the elderly population. Hence, to increase life satisfaction among elderly individuals, it is imperative to monitor and address factors such as sleep duration, body pain, and self-reported health status and implement suitable interventions to improve these aspects.
In the present study, both short sleep duration (< 6 hours or 6–7 hours) and long sleep duration (≥ 9 hours) were linked to lower life satisfaction, indicating a U-shaped curve between sleep duration and life satisfaction. This finding is consistent with previous research. For example, a cross-sectional study conducted among Norwegian adolescents revealed a positive statistical association between sleep duration on school days and psychological well-being[20]. Similarly, another study reported a positive association between sleep duration and life satisfaction in a homogeneous sample of healthy governmental employees[21]. Specifically, this phenomenon in the elderly population warrants attention. Research indicates that older adults may face greater challenges to life satisfaction when experiencing both short and long sleep durations. This may be due to their heightened sensitivity to health and quality of life issues. Additionally, older adults might struggle more with adjusting and optimizing sleep duration due to physiological changes and social factors[22]. Future studies could further explore the specific impact of sleep duration on life satisfaction in older adults, considering individual differences and special needs, to better develop intervention strategies and improve their quality of life.
On the one hand, short sleep duration was associated with an increased risk of body pain, whereas long sleep duration was not significantly related to body pain. Among individuals with temporomandibular disorders, a significantly greater number of patients in the short sleep group reported pain than did those in the long sleep group[23]. Moreover, a noteworthy cohort study revealed that a comprehensive sleep score, incorporating variables such as sleep duration, chronotype, insomnia, snoring, and daytime sleepiness, was linked to the persistence or recurrence of chronic musculoskeletal pain lasting more than three months[24]. Additionally, a prior investigation revealed no significant correlation between longer sleep duration and subsequent pain[25]. However, individuals reporting short sleep durations were 2.4 times more likely to utilize nonprescription pain medication than those who did not[26]. On the other hand, both short and long sleep durations were related to poor subjective health status, which indicated a U-shaped relationship between sleep duration and self-rated health status. Previous research revealed that a short sleep duration of < 6 hours was linked to poorer self-rated health and a greater frequency of days with poor physical health over the previous 30 days than an optimal sleep duration of 7–9 hours[27]. Consistent with another study, the findings revealed an anticipated inverted U-shaped (i.e., quadratic) relationship between the previous night’s sleep duration and self-rated health[28].
Finally, our study revealed that sleep duration can indirectly predict life satisfaction through the chain mediation of body pain and self-reported health status. Our findings align with those of previous studies, indicating that sleep duration significantly negatively predicts an individual’s chronic pain[15,29,30]. For a deeper exploration, sleep duration has been shown to involve various neurobiological mechanisms, encompassing the opioid, monoaminergic, orexinergic, immune, melatonergic, and endocannabinoid systems. Additionally, it influences the hypothalamus-pituitary-adrenal axis, as well as the adenosine and nitric oxide signalling pathways. These mechanisms collectively modulate endogenous pain responses, inflammation, affective states, mood, and other physiological conditions. Moreover, different endogenous substances, such as dopamine, orexin, melatonin, and vitamin D, play roles in augmenting pain sensitivity[31-33]. However, pain is a crucial risk factor for self-rated health, especially among elderly individuals, and can trigger a range of self-reported health issues[34]. Pain is an important public health concern and has documented negative associations with various health outcomes and detrimental effects on quality of life, ultimately contributing to poor self-rated health[35,36]. A previous study confirmed that individuals with body pain in the general population are more inclined to have poor self-rated health[37]. Therefore, chronic pain is significantly associated with poor self-rated health. A shorter duration of sleep exacerbates bodily pain, consequently heightening the likelihood of reporting poorer health status and ultimately diminishing life satisfaction. In summary, the findings of this study not only enhance our comprehension of the inherent mechanisms linking sleep duration to life satisfaction by exploring the chained mediation involving body pain and self-reported health status but also advance and extend research on the factors impacting life satisfaction.
Expanding on the limitations of this study, it is crucial to acknowledge that the reliance on questionnaires for data collection opens the door to potential biases in responses, necessitating careful consideration during interpretation. Next, we only considered sleep quantity without accounting for sleep quality, which has also been linked to adverse outcomes in previous research[38,39]. This omission may affect the comprehensiveness of our findings and limit our understanding of the full impact of sleep on health. Additionally, in the present study, we did not control for unobserved family background confounders. This oversight may result in an overestimation of the effects of sleep, as we did not account for family-level heterogeneity[40]. Furthermore, in this study, we focused on elderly Chinese adults, which may limit the applicability of the findings to other populations due to cultural and demographic factors. Future research should address these limitations to enhance generalizability. Finally, given the correlational and predictive design of this study, it is challenging to establish definitive causal relationships. Enhancing the validity of the findings could be achieved through longitudinal studies, which are useful for capturing temporal changes and offering deeper insights into the dynamics of the relationships observed. It is crucial that such studies include meticulous control of various factors to minimize the influence of confounding variables and enhance the reliability of the outcomes.
-
Table S1. Results of the chain mediating analysis. Estimates = non-standardized coefficient
Estimates SE T P PATH: Sleep duration → Troubled with body pain → Self-reported health status → Life satisfaction Dependent variable: Troubled with body pain Sleep duration −0.127 0.005 −24.490 < 0.001 Dependent variable: Self-reported health status Sleep duration −0.061 0.004 −15.919 < 0.001 Troubled with body pain 0.319 0.006 57.289 < 0.001 Dependent variable: Life satisfaction Sleep duration −0.028 0.003 −8.626 < 0.001 Troubled with body pain 0.046 0.005 8.988 < 0.001 Self-reported health status 0.175 0.006 27.448 < 0.001 Note. The model adjusted for age, gender, education level, marital status, smoke, drink, and living residence.
doi: 10.3967/bes2024.185
The Sequential Mediating Roles of Body Pain and Self-Reported Health Status in the Relationship between Sleep Duration and Life Satisfaction
-
Abstract:
Objective This study examines the sequential mediating roles of body pain and self-reported health in the association between sleep duration and self-reported life satisfaction among elderly Chinese adults. Methods Data from the fifth wave of the China Health and Retirement Longitudinal Survey (CHARLS) were used to analyse the relationships between sleep duration and body pain, self-reported health, and life satisfaction through logistic regression and Restricted Cubic Spline (RCS) analyses. The sequential mediation effects of body pain and self-reported health status were examined via chain mediation analysis. Results Logistic regression analysis showed that sleeping fewer than 6 hours or 6–7 hours was linked to higher risks of body pain, poor health, and dissatisfaction with life compared to sleeping 7–8 hours (all P < 0.05). Additionally, those sleeping more than 9 hours also had increased risks of poor health and dissatisfaction with life compared to those sleeping 7–8 hours (all P < 0.05). Chain mediation analysis showed that body pain and self-reported health status sequentially mediated 46.15% of the association between sleep duration and life satisfaction. Conclusion Body pain and self-reported health may shape the relationship between sleep duration and life satisfaction in elderly Chinese adults. -
Key words:
- Sleep /
- Life satisfaction /
- Health status /
- Pain
Approval for the CHARLS study was obtained from the Institutional Review Board at Peking University (IRB00001052-11015).
&These authors contributed equally to this work.
注释:1) Competing Interests: 2) Ethics: -
Figure 2. Chain mediation analysis. The models investigate the effect of sleep duration (independent variable) on life satisfaction. The sequential mediators in this analysis included body pain and self-reported health status. The mediation model was adjusted for age, sex, education level, marital status, smoking status, alcohol consumption status, and residence. ***P < 0.001.
Table 1. Demographic characteristics of the participants assessed in 2020 (n = 17,131)
Characteristics Mean ± Standard
deviation / n (%)Age, years 63.03 ± 9.51 Sex Male 8,020 (46.82) Female 9,111 (53.18) Education level Less than lower secondary 14,940 (87.21) Upper secondary & vocational training 1,828 (10.67) Tertiary 363 (2.12) Marital status Married 14,582 (85.12) Not in marriage 2,549 (14.88) Smoking Yes 6,627 (38.68) No 1,0504 (61.32) Alcohol consumption Yes 6,256 (36.52) No 1,0875 (63.48) Residence Urban 6,118 (35.71) Rural 11,013 (64.29) Sleep duration, h 6.07 ± 1.85 < 6 6,127 (35.77) 6– 4,297 (25.08) 7– 2,938 (17.15) 8– 2,649 (15.46) ≥ 9 1,120 (6.54) Body pain Yes 3,126 (18.25) No 14,005 (81.75) Self-reported health status Poor 4,233 (24.71) Good 12,898 (75.29) Life satisfaction Not Satisfied 1,373 (8.12) Satisfied 15,260 (89.08) Note. x = Mean, s = Standard Deviation. Table 2. Associations between sleep duration and body pain, self-reported health status, and life satisfaction
Sleep duration (h) Body pain Self-reported health status Life satisfaction OR 95% CI P OR 95% CI P OR 95% CI P < 6 2.322 2.047−2.634 < 0.001 2.407 2.152−2.693 < 0.001 2.352 2.009−2.752 < 0.001 7– Ref. − − Ref. − − Ref. − − 6– 1.202 1.043−1.385 0.011 1.244 1.099−1.409 0.001 1.283 1.077−1.528 0.005 8– 0.943 0.801−1.111 0.483 1.010 0.877−1.163 0.889 0.976 0.796−1.197 0.816 ≥ 9 1.119 0.919−1.363 0.264 1.321 1.115−1.566 0.001 1.393 1.093−1.776 0.007 Note. CI: confidence Interval; OR: odds ratio; Ref: reference group. All the models were adjusted for age, sex, education level, marital status, smoking status, alcohol consumption status and residence. Table 3. Spearman correlations between sleep duration, body pain, self-reported status and life satisfaction
Variable 1 2 3 4 Sleep duration 1.000 Body pain −0.206*** 1.000 Self-reported status −0.205*** 0.444*** 1.000 Life satisfaction −0.117*** 0.172*** 0.252*** 1.000 Note. ***P < 0.001. S2. Results of the chain mediating effect based on Bootstrapping Test (n = 5,000). Estimates = non-standardized coefficients.
Estimates SE T P 95% CI LCI UCI Sleep duration → Troubled with body pain → Life satisfaction −0.006 0.001 −8.437 < 0.001 −0.007 −0.004 Sleep duration → Self-reported health status → Life satisfaction −0.011 0.001 −13.771 < 0.001 −0.012 −0.009 Sleep duration → Troubled with body pain → Self-reported health status →
Life satisfaction−0.007 0.000 −17.410 < 0.001 −0.008 −0.006 Total mediation effects −0.024 0.001 −21.406 < 0.001 −0.026 −0.021 Direct effect of sleep duration on life satisfaction −0.028 0.003 −8.626 < 0.001 −0.034 −0.022 Total effects of sleep duration on life satisfaction −0.052 0.003 −15.764 < 0.001 −0.058 −0.045 Proportion mediated by mediators 46.15% Note. CI: confidence interval; LCI: lower confidence interval; SE: standard error; UCL: upper confidence interval. The model adjusted for age, gender, education level, marital status, smoke, drink, and living residence. S1. Results of the chain mediating analysis. Estimates = non-standardized coefficient
Estimates SE T P PATH: Sleep duration → Troubled with body pain → Self-reported health status → Life satisfaction Dependent variable: Troubled with body pain Sleep duration −0.127 0.005 −24.490 < 0.001 Dependent variable: Self-reported health status Sleep duration −0.061 0.004 −15.919 < 0.001 Troubled with body pain 0.319 0.006 57.289 < 0.001 Dependent variable: Life satisfaction Sleep duration −0.028 0.003 −8.626 < 0.001 Troubled with body pain 0.046 0.005 8.988 < 0.001 Self-reported health status 0.175 0.006 27.448 < 0.001 Note. The model adjusted for age, gender, education level, marital status, smoke, drink, and living residence. -
[1] Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 2015; 1, 40−3. doi: 10.1016/j.sleh.2014.12.010 [2] Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep, 2017; 9, 151−61. doi: 10.2147/NSS.S134864 [3] Park GR, Kim J. Short sleep duration and adolescent health: does weekend catch-up sleep work and for whom? Public Health, 2023; 214, 91-5. [4] Park GR, Kim J. The gendered health consequences of persistent exposure to short sleep duration during adolescence. J Adolescence, 2023; 95, 1311−20. doi: 10.1002/jad.12203 [5] Essien SK, Feng CX, Sun WJ, et al. Sleep duration and sleep disturbances in association with falls among the middle-aged and older adults in China: a population-based nationwide study. BMC Geriatr, 2018; 18, 196. doi: 10.1186/s12877-018-0889-x [6] Williams JC, Hum RM, Alam U, et al. Insomnia and short sleep duration, but not chronotype, is associated with chronic widespread pain: Mendelian randomization study. Rheumatol Int, 2024. [7] Xu C, Ren XS, Lin P, et al. Exploring the causal effects of sleep characteristics on TMD-related pain: a two-sample Mendelian randomization study. Clin Oral Invest, 2024; 28, 384. doi: 10.1007/s00784-024-05776-2 [8] Fayaz A, Croft P, Langford RM, et al. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open, 2016; 6, e010364. doi: 10.1136/bmjopen-2015-010364 [9] Stubbs B, Vancampfort D, Veronese N, et al. Depression and pain: primary data and meta-analysis among 237 952 people across 47 low- and middle-income countries. Psychol Med, 2017; 47, 2906−17. doi: 10.1017/S0033291717001477 [10] Whibley D, AlKandari N, Kristensen K, et al. Sleep and pain: a systematic review of studies of mediation. Clin J Pain, 2019; 35, 544−58. doi: 10.1097/AJP.0000000000000697 [11] Li YP, Zhang XH, Winkelman JW, et al. Association between insomnia symptoms and mortality: a prospective study of US men. Circulation, 2014; 129, 737−46. doi: 10.1161/CIRCULATIONAHA.113.004500 [12] Tang NKY, Sanborn AN. Better quality sleep promotes daytime physical activity in patients with chronic pain? A multilevel analysis of the within-person relationship. PLoS One, 2014; 9, e92158. doi: 10.1371/journal.pone.0092158 [13] Vanderlind WM, Beevers CG, Sherman SM, et al. Sleep and sadness: exploring the relation among sleep, cognitive control, and depressive symptoms in young adults. Sleep Med, 2014; 15, 144−9. doi: 10.1016/j.sleep.2013.10.006 [14] Sella E, Miola L, Toffalini E, et al. The relationship between sleep quality and quality of life in aging: a systematic review and meta-analysis. Health Psychol Rev, 2023; 17, 169−91. doi: 10.1080/17437199.2021.1974309 [15] Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain, 2013; 14, 1539−52. doi: 10.1016/j.jpain.2013.08.007 [16] Selvanathan J, Pham C, Nagappa M, et al. Cognitive behavioral therapy for insomnia in patients with chronic pain - a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev, 2021; 60, 101460. doi: 10.1016/j.smrv.2021.101460 [17] Smith A, Andruski B, Deng G, et al. The association between sleep disturbance and health outcomes in chronic whiplash-associated disorders: a series of mediation analyses. Clin J Pain, 2022; 38, 612−9. doi: 10.1097/AJP.0000000000001066 [18] Bramhankar M, Kundu S, Pandey M, et al. An assessment of self-rated life satisfaction and its correlates with physical, mental and social health status among older adults in India. Sci Rep, 2023; 13, 9117. doi: 10.1038/s41598-023-36041-3 [19] Zhao Y, Hu Y, Smith JP, et al. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol, 2014; 43, 61−8. doi: 10.1093/ije/dys203 [20] Grasaas E, Rohde G, Haraldstad K, et al. Sleep duration in schooldays is associated with health-related quality of life in norwegian adolescents: a cross-sectional study. BMC Pediatr, 2023; 23, 473. doi: 10.1186/s12887-023-04306-5 [21] Kósa K, Vincze S, Veres-Balajti I, et al. The pendulum swings both ways: evidence for U-shaped association between sleep duration and mental health outcomes. Int J Environ Res Public Health, 2023; 20, 5650. doi: 10.3390/ijerph20095650 [22] Melikyan ZA, Kawas CH, Paganini-Hill A, et al. Neuropathologic changes at age 90+ related to sleep duration 19 to 40 years earlier: the 90+ study. Alzheimers Dement, 2024; 20, 3495−503. doi: 10.1002/alz.13798 [23] Kim Y, Son C, Park YK, et al. Sleep duration and inflammatory mediator levels associated with long-term prognosis in temporomandibular disorders. J Oral Rehabil, 2023; 50, 830−9. doi: 10.1111/joor.13494 [24] Hodges S, Guler S, Sacca V, et al. Associations among acute and chronic musculoskeletal pain, sleep duration, and C-reactive protein (CRP): a cross-sectional study of the UK biobank dataset. Sleep Med, 2023; 101, 393−400. doi: 10.1016/j.sleep.2022.11.013 [25] Lücke AJ, Wrzus C, Gerstorf D, et al. Bidirectional links of daily sleep quality and duration with pain and self-rated health in older adults' daily lives. J Gerontol: Series A, 2023; 78, 1887−96. doi: 10.1093/gerona/glac192 [26] Hernandez E, Griggs S. Substance use, sleep duration, and health among adults in Ohio. Prev Chronic Dis, 2023; 20, E117. [27] Huynh N, Kendzor DE, Ra CK, et al. The association of sleep with physical and mental health among people experiencing homelessness. Sleep Health, 2024; 10, 48−53. doi: 10.1016/j.sleh.2023.10.004 [28] Andreasson A, Axelsson J, Bosch JA, et al. Poor sleep quality is associated with worse self-rated health in long sleep duration but not short sleep duration. Sleep Med, 2021; 88, 262−6. doi: 10.1016/j.sleep.2021.10.028 [29] Lautenbacher S, Kundermann B, Krieg JC. Sleep deprivation and pain perception. Sleep Med Rev, 2006; 10, 357−69. doi: 10.1016/j.smrv.2005.08.001 [30] Edwards RR, Almeida DM, Klick B, et al. Duration of sleep contributes to next-day pain report in the general population. Pain, 2008; 137, 202−7. doi: 10.1016/j.pain.2008.01.025 [31] Haack M, Simpson N, Sethna N, et al. Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications. Neuropsychopharmacology, 2020; 45, 205−16. doi: 10.1038/s41386-019-0439-z [32] Herrero Babiloni A, De Koninck BP, Beetz G, et al. Sleep and pain: recent insights, mechanisms, and future directions in the investigation of this relationship. J Neural Transm, 2020; 127, 647−60. doi: 10.1007/s00702-019-02067-z [33] Alexandre C, Latremoliere A, Ferreira A, et al. Decreased alertness due to sleep loss increases pain sensitivity in mice. Nat Med, 2017; 23, 768−74. doi: 10.1038/nm.4329 [34] Chireh B, D'Arcy C. Pain and self-rated health among middle-aged and older Canadians: an analysis of the Canadian community health survey-healthy aging. BMC Public Health, 2018; 18, 1006. doi: 10.1186/s12889-018-5912-9 [35] Johnston KJA, Huckins LM. Chronic pain and psychiatric conditions. Complex Psychiatry, 2023; 9, 24−43. doi: 10.1159/000527041 [36] Foley HE, Knight JC, Ploughman M, et al. Association of chronic pain with comorbidities and health care utilization: a retrospective cohort study using health administrative data. Pain, 2021; 162, 2737−49. doi: 10.1097/j.pain.0000000000002264 [37] Mäntyselkä PT, Turunen JHO, Ahonen RS, et al. Chronic pain and poor self-rated health. JAMA, 2003; 290, 2435−42. doi: 10.1001/jama.290.18.2435 [38] Kim J, Park GR, Sutin AR. Adolescent sleep quality and quantity and educational attainment: a test of multiple mechanisms using sibling difference models. J Child Psychol Psychiatry, 2022; 63, 1644−57. doi: 10.1111/jcpp.13686 [39] Stafford A, Oduola S, Reeve S. Sleep and socio-occupational functioning in adults with serious mental illness: a systematic review. Psychiatry Res, 2024; 339, 116111. doi: 10.1016/j.psychres.2024.116111 [40] Park GR, Kim J. Adolescent sleep duration and cardiometabolic risk in adulthood: Evidence from sibling comparison designs with biomarker data. Health Psychol, 2022; 41, 683−92. doi: 10.1037/hea0001158 -




 下载:
下载:



 Quick Links
Quick Links