-
Hemorrhagic fever with renal syndrome (HFRS) is a rodent-borne acute infectious disease caused by hantavirus[1-4]. HFRS is clinically characterized by fever, hemorrhage, and acute kidney damage[3,5,6] and has a rapid onset and progression. If not treated promptly, HFRS can cause serious illness and death. Hantavirus is spread when virus-containing particles from rodent urine, feces, droppings, or saliva are stirred into the air. Infection occurs via inhalation of these aerosolized particles[1]. In China, HFRS is mainly caused by Hantaan virus (HTNV) and Seoul virus (SEOV). HTNV is harbored by the striped field mouse (Apodemus agrarius), and SEOV is harbored by Rattus norvegicus, Mus musculus, and Rattus rattus[7,8]. HFRS has no clinically targeted treatment[5,9,10]. The complex early clinical manifestations of HFRS and the rapidly changing condition result in easy misdiagnosis and missed diagnosis[11-14]. HFRS cases mainly occur in the young and middle-aged rural population[15-17], pose a risk to life and health, place an economic burden on patients’ families[18-20], and considerably impact social and economic development.
Accounting for 70%–90% of the global HFRS cases that are reported annually, China is the region with the most severe HFRS epidemic worldwide[21,22]. Shandong Province is a traditional focal point for HFRS and one of the provinces with the highest HFRS rates in China[15,23-25]. Qingdao City, which is located in the southeast of Shandong Province, is one of the most highly endemic areas for HFRS in Shandong Province[23-27]. HFRS cases have been reported annually since 1974 when the first case was reported in Qingdao[28]. The top 20 districts or counties in Shandong Province by average annual incidence between 2020 and 2022 were classified as Class I districts or counties. Qingdao has five Class I districts or counties[29]: Huangdao, Pingdu, Jiaozhou, Jimo, and Laixi.
The population is generally susceptible to hantavirus. The regional distribution of host animals can change with food and environmental conditions. Factors such as social development and economic activities also considerably affect the ecological characteristics and habitat of rodent populations, thereby affecting the epidemic law of HFRS[28,30-34]. The population that is susceptible to HFRS is heterogeneous in space, socioeconomic status, and geography. Changes in altitude and geographic latitude are known to cause a geographical gradient and spatial heterogeneity in the distribution of HFRS endemic areas[35,36], and the types of HFRS endemic areas in specific regions change in different periods[9,28,37].
HFRS infection has existed in Qingdao City for over 40 years[28,38]. However, the epidemic characteristics of HFRS are still not entirely clear. Therefore, a systematic investigation of the spatio-temporal distribution pattern of HFRS is required to facilitate better prevention and control of HFRS in Qingdao City. This study characterized the epidemiological characteristics and spatio-temporal dynamic of the HFRS epidemic to examine the changing patterns of HFRS in Qingdao over the last 13 years (2010–2022), identify the probable reasons for changes in the epidemic trend of HFRS, and provide valuable scientific support for HFRS monitoring and control.
-
Information on HFRS cases in Qingdao City from 2010 to 2022 was collected from the National Infectious Diseases Surveillance And Reporting System of the Center for Disease Control and Prevention (CDC) of China. The information about individual HFRS cases included age, occupation, disease onset, confirmation date, case category, residential address, and telephone number. Suspected patients with HFRS were diagnosed in accordance with the “Diagnostic Criteria for Epidemic Hemorrhagic Fever Ws278-2008” issued by the Ministry of Health of China in 2008. Data of host surveillance and hantavirus infection were sourced from the Qingdao CDC. Hosts (rodents and shrews) were captured using mousetraps placed outside and inside houses between 2011 and 2015.
-
The population data of each district was sourced from the “Basic Information System of China’s Disease Prevention and Control Information System” and was accessed and downloaded on 9 February 2023. Population data for each street/township was sourced from registered residence population data in 2022 and was collected on 6 April 2023 from the centers for disease control and prevention of 10 districts or counties in Qingdao City. Clinically diagnosed and laboratory-confirmed cases were included in our study.
-
Qingdao City is a tourist port city in Eastern China and is located on the west coast of the Pacific Ocean along the coast of the Yellow Sea, at the southern end of the Shandong Peninsula (35°35′–37°09′ N, 119°30′–121°00′ E). Qingdao governs seven districts and three county-level cities.The land area of the jurisdiction is 11,282 km2, and the sea area is 12,240 km2. The resident population of Qingdao was 10,134,838 in 2022. Qingdao belongs to the northern temperate maritime monsoon climate zone. Qingdao is a hilly city along the seashore, with terrain that is high in the east, low in the west, raised in the north and south, and low in the center. Mountains, hills, plains, and depressions account for approximately 15.5%, 2.1%, 37.7%, and 21.7%, respectively, of the city’s total area.
-
Descriptive epidemiological methods were used to describe the epidemiological characteristics of HFRS cases and death cases in Qingdao City. Excel 2021 software was used to organize data and analyze epidemiological characteristics. Enumerated data were expressed as cases or percentages. A P-value < 0.05 was considered significant.
-
A seasonal-trend decomposition of time series analysis was performed to explore the various characteristics of periodicity and seasonality using R software Version 4.2 (AT&T Bell Laboratories, Auckland, New Zealand). The seasonal index was calculated as the ratio of the average number of cases in the current month to the average monthly number of cases in the 13 twelve-month periods between 2010 and 2022. An index value close to 1.0 indicated no seasonal trend[39].
-
A global spatial autocorrelation analysis and local indicators of spatial association analysis were conducted using Geoda software Version 1.20 (Center for Spatial Data Science, Chicago, USA) to visualize the global and local spatial clustering of HFRS cases in Qingdao City from 2010 to 2022. Global Moran’s I Index (ranging from −1 to 1) was used to analyze global spatial autocorrelation. A Moran’s Index = 0 implies a random spatial distribution. A Moran’s I Index < 0 implies a dispersing spatial distribution, and a Moran’s I Index > 0 implies a clustering spatial distribution. Local Moran’s I was calculated to explore significant hot spots (High–High), cold spots (Low–Low), and outliers (High–Low and Low–High). Maps were made using ArcGIS software Version 10.8 (ESRI Inc., Redlands, CA, USA).
-
A Kulldorff’s spatio-temporal scan statistical analysis was used to identify the spatio-temporal clusters of HFRS cases in Qingdao using SaTScan Software Version 10.1 (Martin Kulldorff, National Cancer Institute, Bethesda, MD, USA). The discrete Poisson probability model using a circular window with a radius was used for scanning. The maximum spatial and temporal size was defined as 20%. A P-value < 0.05 was considered significant. The maps were made in ArcGIS software.
-
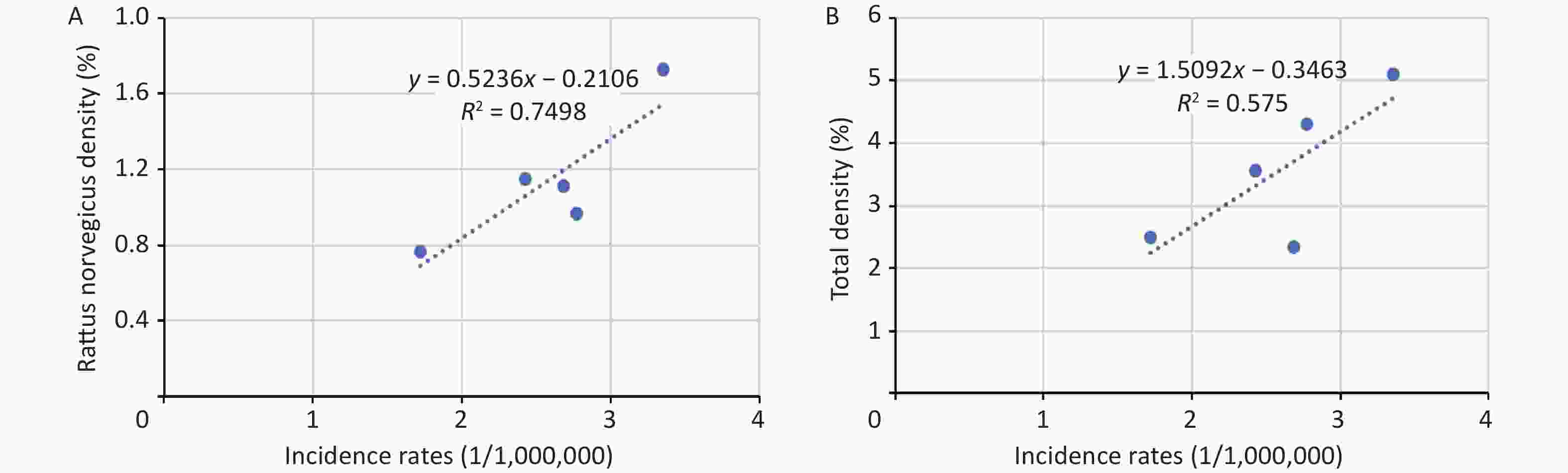
A total of 2,220 HFRS cases were reported in Qingdao City from 2010 to 2022, and the average annual number of cases was 171. The annual incidence fluctuated between 0.75/100,000 and 3.35/100,000, and the average annual incidence was 1.89/100,000. The total number of deaths was 56, with a case fatality rate of 2.52% (Figure 1). From 2010 to 2019, the annual HFRS incidence in Qingdao was higher than that in Shandong Province, and the incidence in Shandong Province was higher than that in China (Figure 2).
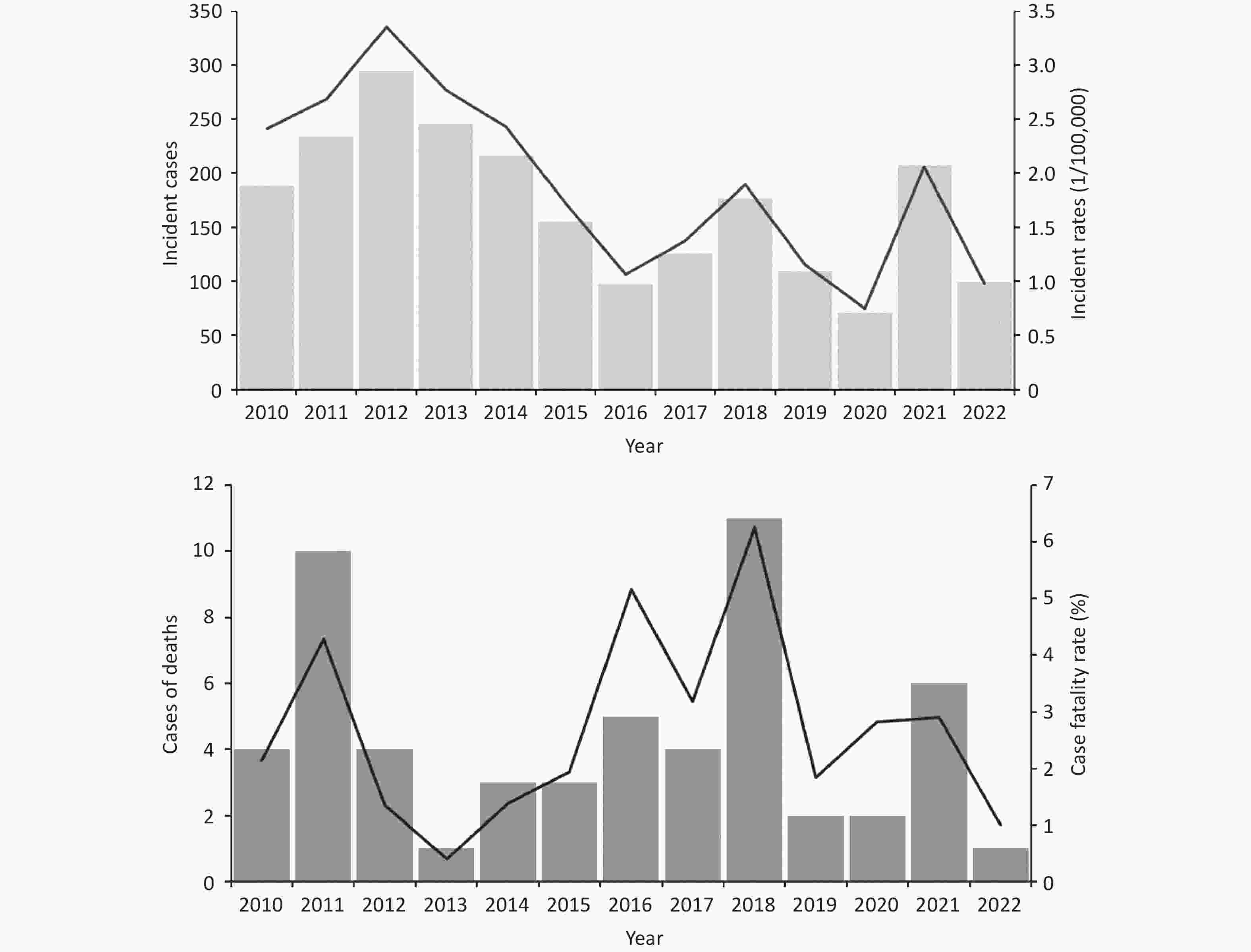
Figure 1. Annual incidence and mortality of hemorrhagic fever with renal syndrome (HFRS) in Qingdao from 2010 to 2022. The figure above indicates the annual number of cases and incidence rate, and the below figure indicates the annual of death and fatality rate.
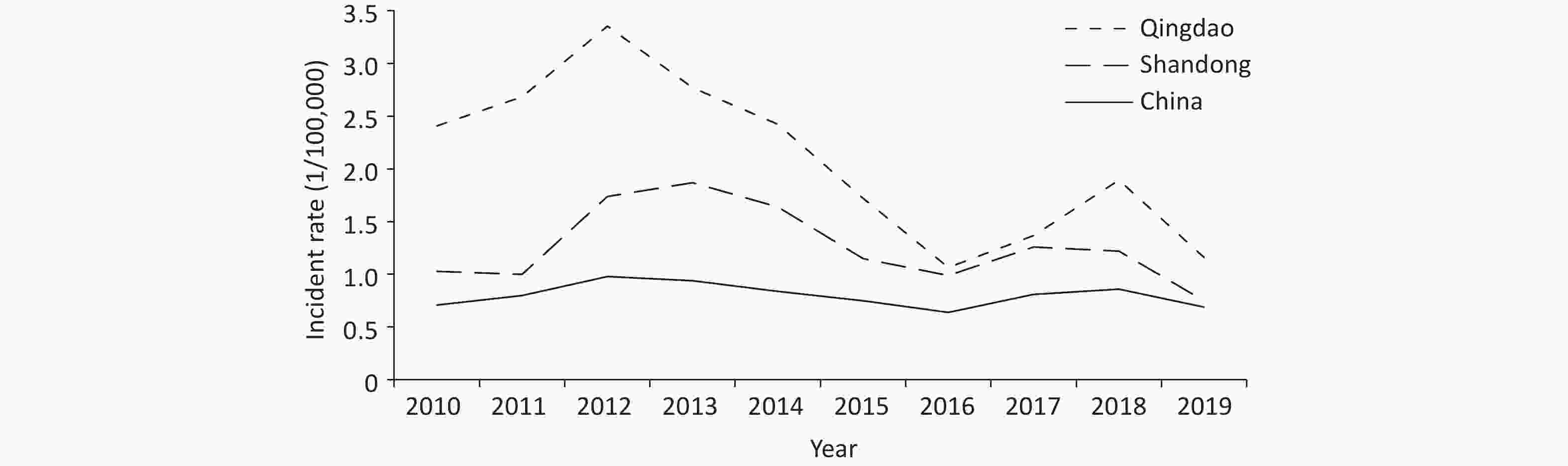
Figure 2. Incidence rate of hemorrhagic fever with renal syndrome (HFRS) in China, Shandong Province and Qingdao City from 2010 to 2019.
A total of 14 patients had been vaccinated against HFRS, including one patient who experienced vaccine breakthrough and 13 patients who received post-infection vaccination.
-
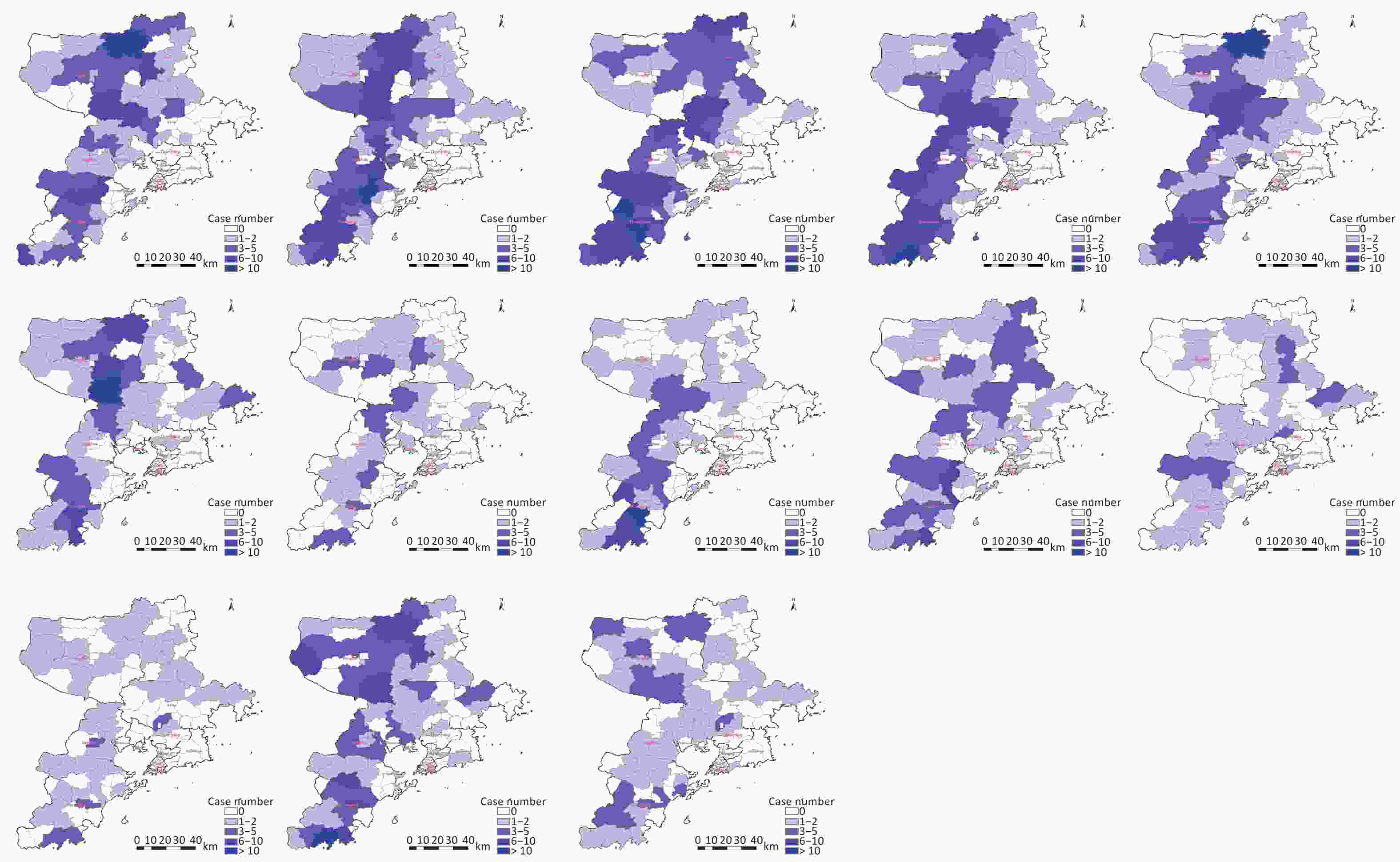
Among the 2,220 HFRS cases, the peak incidence was 295 cases in 2012, and the minimum number of cases was 71 in 2020. The fall-winter peak (from October to January) was observed every year. The spring peak (from March to June) was not obvious, and a peak was not observed in several years (2010, 2018, and 2020; Figures 1 and 3).
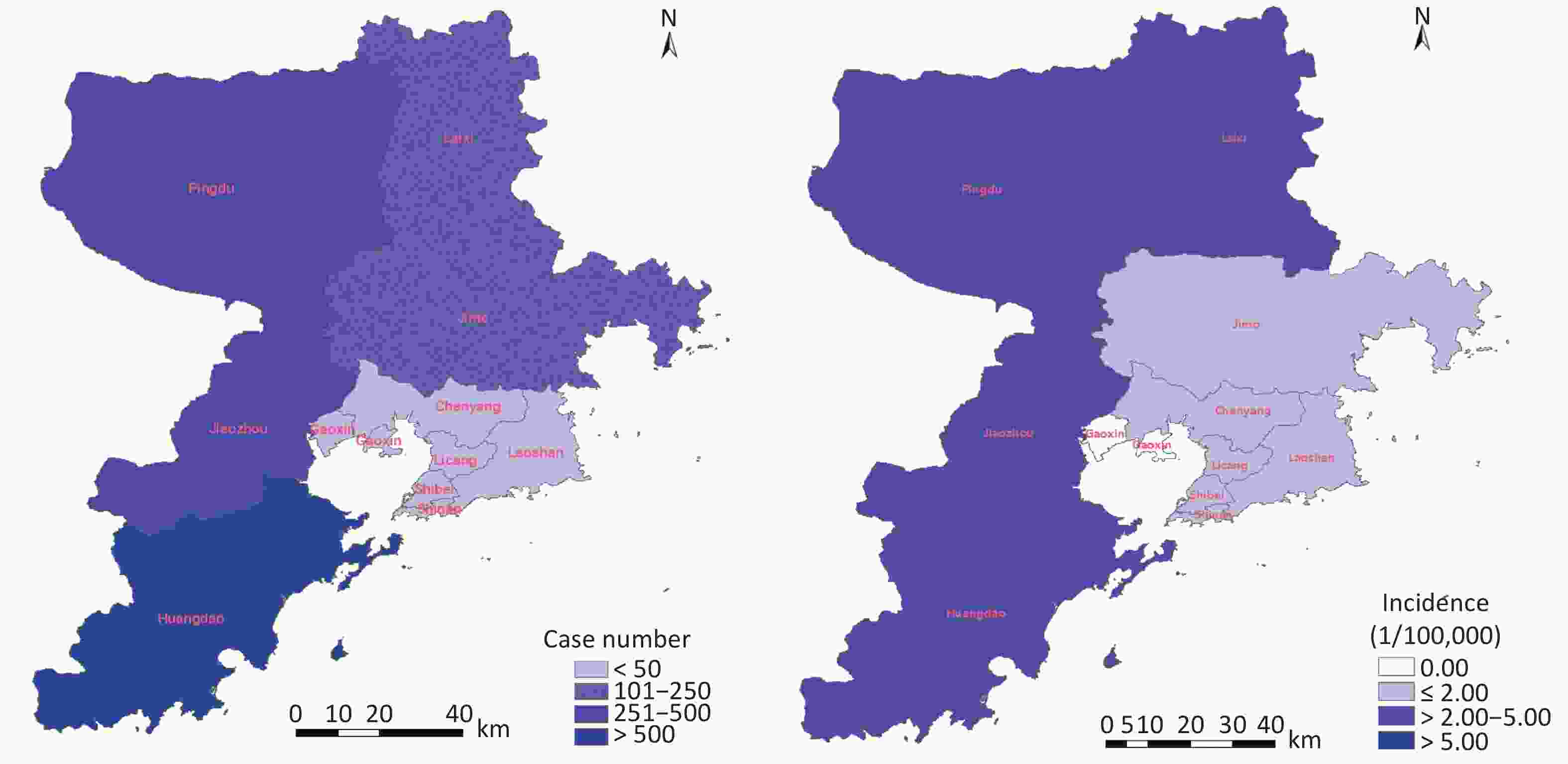
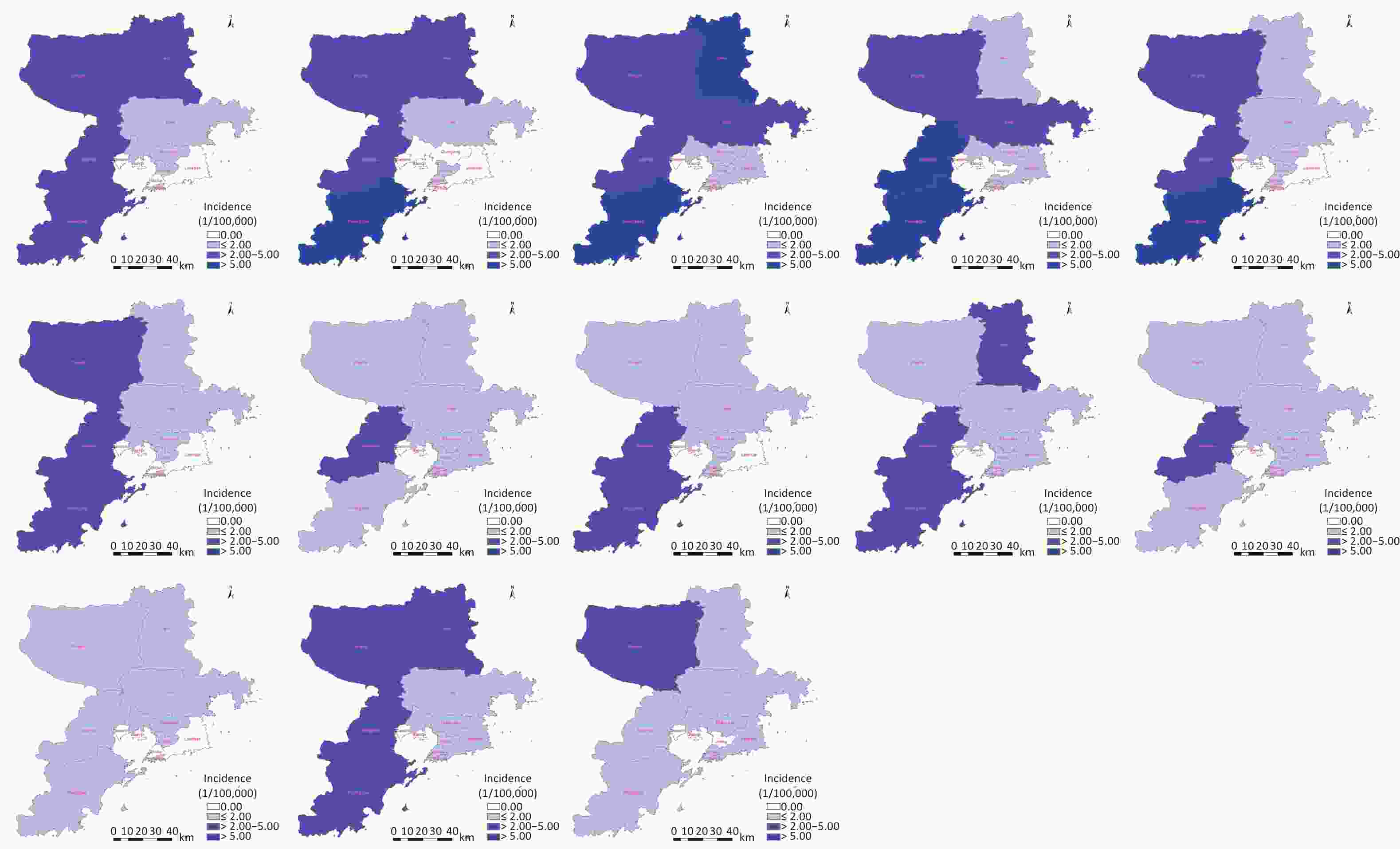
Figure 3. Spatial distribution of cumulative hemorrhagic fever with renal syndrome (HFRS) cases in county/district level of Qingdao City from 2010 to 2022. The figure left indicates the cumulative number of HFRS case; the figure right indicates of the cumulative incidence rates of HFRS cases. Map approval number: GS(2022)1873.
Male cases numbered 1,639 (73.8%), and the male: female ratio ranged from 3.7:1 in 2019 to 2.2:1 in 2013. A total of 75.3% (1,671/2,220) of patients with HFRS were between 16 and 60 years of age (Table 1). Most patients with HFRS were farmers (75.3%, 1,671/2,220), followed by workers (7.4%, 165/2,220) and homemakers/unemployed individuals (4.2%, 94/2,220; Table 2).
Table 1. Characteristics of all 2,220 HFRS cases in Qingdao City, 2010–2022
Year Gender Age Male (%) Female (%) < 16 (%) 16–60 (%) > 60 (%) 2010 142 (75.5) 46 (24.5) 3 (1.6) 149 (79.3) 36 (19.1) 2011 181 (77.4) 53 (22.6) 2 (0.9) 186 (79.5) 46 (19.7) 2012 211 (71.5) 84 (28.5) 4 (1.4) 235 (79.7) 56 (19.0) 2013 169 (68.7) 77 (31.3) 2 (0.8) 197 (80.1) 47 (19.1) 2014 152 (70.0) 65 (30.0) 3 (1.4) 169 (77.9) 45 (20.7) 2015 119 (76.8) 36 (23.2) 4 (2.6) 112 (72.3) 39 (25.2) 2016 73 (75.3) 24 (24.7) 0 (0) 75 (77.3) 22 (22.7) 2017 96 (76.2) 30 (23.8) 3 (2.4) 88 (69.8) 35 (27.8) 2018 135 (76.7) 41 (23.3) 4 (2.3) 129 (73.3) 43 (24.4) 2019 86 (78.9) 23 (21.1) 1 (0.9) 74 (67.9) 34 (31.2) 2020 54 (76.1) 17 (23.9) 0 (0) 53 (74.6) 18 (25.4) 2021 151 (72.9) 56 (27.1) 2 (1.0) 141 (68.1) 64 (30.9) 2022 70 (70.7) 29 (29.3) 1 (1.0) 63 (63.6) 35 (35.4) Total 1639 (73.8) 581 (26.2) 29 (1.3) 1671 (75.3) 520 (23.4) Note. HFRS, hemorrhagic fever with renal syndrome. Table 2. Occupational classification of all 2220 HFRS cases in Qingdao City, 2010–2022
Occupation Number of cases Proportion (%) Farmer 1,672 75.3 Worker 165 7.4 Housework/unemployment 94 4.2 Student 53 2.4 Cadre/staff 52 2.3 Migrant worker 49 2.2 Retired personnel 31 1.4 Self-employed 21 0.9 Business service 18 0.8 Others 65 2.9 Total 2,220 100.0 Note. HFRS, hemorrhagic fever with renal syndrome. Information on clinical symptoms was recorded between 2020 and 2022. Fever was the most common symptom (87.5%, 272/311), followed by fatigue (83.3%, 259/311) and rapid onset (66.9%, 208/311). Sixty-one (19.6%, 61/311) cases had typical “three redness” symptoms of blush, neck redness, and chest redness; 83 (26.7%, 83/311) cases had typical “three pain” symptoms of headache, orbital pain, and low back pain; and 36 cases (11.6%, 36/311) had both “three red” and “three pain” symptoms (Tables 3 and 4).
Table 3. The main clinical symptoms among HFRS cases in Qingdao City in 2020–2022
Symptom 2020 2021 2022 2020–2022 Number of cases Proportion (%) Number of cases Proportion (%) Number of cases Proportion (%) Number of cases Proportion (%) Rapid onset 40 76.9 105 63.3 63 67.7 208 66.9 Fatigue 41 78.8 145 87.3 73 78.5 259 83.3 Fever 49 94.2 139 83.7 84 90.3 272 87.5 Headache 31 59.6 106 63.9 51 54.8 188 60.5 Low back pain 25 48.1 87 52.4 29 31.2 141 45.3 Orbital pain 24 46.2 62 37.3 17 18.3 103 33.1 Blush 29 55.8 66 39.8 28 30.1 123 39.5 Neck redness 20 38.5 46 27.7 20 21.5 86 27.7 Chest redness 17 32.7 36 21.7 14 15.1 67 21.5 Joint pains 11 21.2 42 25.3 21 22.6 74 23.8 Whole body pains 9 17.3 63 38.0 20 21.5 92 29.6 Abdominal pain 12 23.1 45 27.1 30 32.3 87 28.0 Diarrhea 11 21.2 54 32.5 36 38.7 101 32.5 Constipation 9 17.3 2 1.2 4 4.3 15 4.8 Nausea 15 28.8 74 44.6 41 44.1 130 41.8 Vomiting 12 23.1 67 40.4 39 41.9 118 37.9 Conjunctival congestion 18 34.6 29 17.5 16 17.2 63 20.3 Puffy eyelids 12 23.1 27 16.3 16 17.2 55 17.7 Jaundice 5 9.6 4 2.4 6 6.5 15 4.8 Skin bleeding spots in the armpits, upper arms, chest, or other areas 14 26.9 25 15.1 10 10.8 49 15.8 Bleeding spots in the oral and nasal mucosa 6 11.5 12 7.2 1 1.1 19 6.1 Little or no urination 18 34.6 57 34.3 35 37.6 110 35.4 Hypotension 6 11.5 27 16.3 26 28.0 59 19.0 Shock 4 7.7 9 5.4 5 5.4 18 5.8 Normal leukocyte count 10 19.2 21 12.7 12 12.9 43 13.8 Increased leukocyte count 22 42.3 60 36.1 34 36.6 116 37.3 Decreased leukocyte count 4 7.7 3 1.8 5 5.4 12 3.9 Thrombocytopenia 22 42.3 71 42.8 43 46.2 136 43.7 Urinary protein 15 28.8 14 8.4 17 18.3 46 14.8 Urinary membrane/tubular urine/hematuria 2 3.8 5 3.0 3 3.2 10 3.2 Note. HFRS, hemorrhagic fever with renal syndrome. Table 4. The main typical clinical symptoms among HFRS cases in Qingdao City in 2020–2022
Typical symptoms 2020 2021 2022 2020–2022 Number of cases Proportion (%) Number of cases Proportion (%) Number of cases Proportion (%) Number of cases Proportion (%) Three red 17 32.7 32 19.3 12 12.9 61 19.6 Three pain 19 36.5 51 30.7 13 14.0 83 26.7 Three red and three pain 11 21.2 21 12.7 4 4.3 36 11.6 Note. HFRS, hemorrhagic fever with renal syndrome. Among the 56 cases of deaths, none of whom had been vaccinated, 41 were men (73.2%) and 15 were women (26.8%). The minimum, maximum, and median ages were 14, 85, and 53 years, respectively. Farmers, accounted for 75.0% of deaths. The shortest and longest courses of disease were 2 days and 44 days, respectively, and the maximum distribution was 7 and 8 days, which together accounted for 32.1% of all the deaths.
All the 10 districts or counties in the city had HFRS cases. The cumulative number of cases in the top three districts or counties was 757 in Huangdao District, 427 in Pingdu City, and 340 in Jiaozhou City, with cumulative incidences of 3.86/100,000, 2.41/100,000, and 2.92/100,000, respectively (Figure 3). All the 2,220 cases were distributed in 83.3% (120/144) of the streets/townships of Qingdao City, whereas the remaining 16.7% (24/144) streets/townships did not have cases. The top five streets/townships with the highest cumulative number of cases were Jiudian Town (Pingdu City, 78), Poli Town (Huangdao District, 74), Zhangjialou Town (Huangdao District, 72), Liuwang Town, (Huangdao District, 62), and Nancun Town (Pingdu City, 62; Figures 4 and 5).
-
The seasonal trend was explored with a season-trend decomposition analysis using R software (Figure 6). A rhythmic vibration was observed in the raw data from 2010 to 2022. Seasonality and trend components from the raw data were isolated, and part of the random noise or reminder component was also eliminated. The HFRS epidemic showed two-peak seasonality each year, with a primary fall-winter peak and a minor spring peak. In addition, the HFRS epidemic showed a downward trend and periodic variation of decreasing amplitude and magnitude.
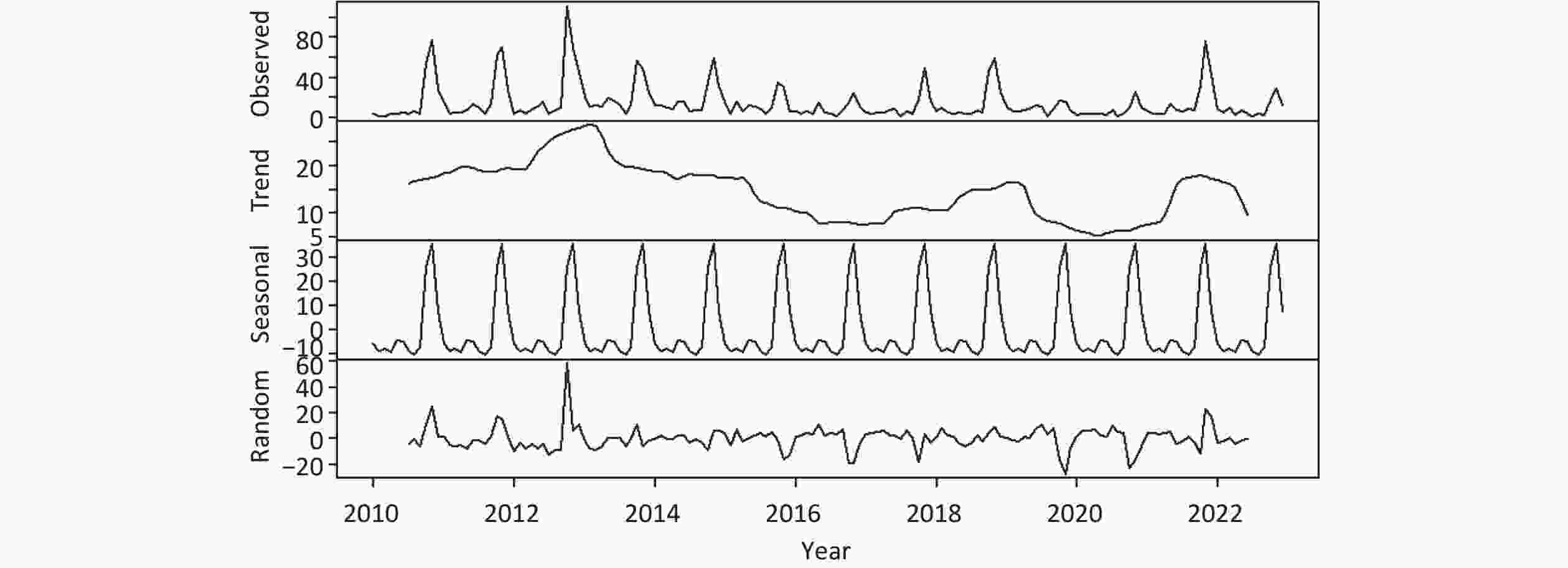
Figure 6. Seasonal decomposition of hemorrhagic fever with renal syndrome (HFRS) cases in Qingdao City, China from 2010 to 2022.
By summarizing the number of HFRS cases each year, we drew season index distribution and radar charts to more clearly visualize the monthly changes in the number of HFRS cases. The months with the largest seasonal indices were November and October, followed by December (Figure 7); these months represented the peak HFRS period. The period between January and September had a smaller seasonal index and showed a trough in HFRS cases.
-
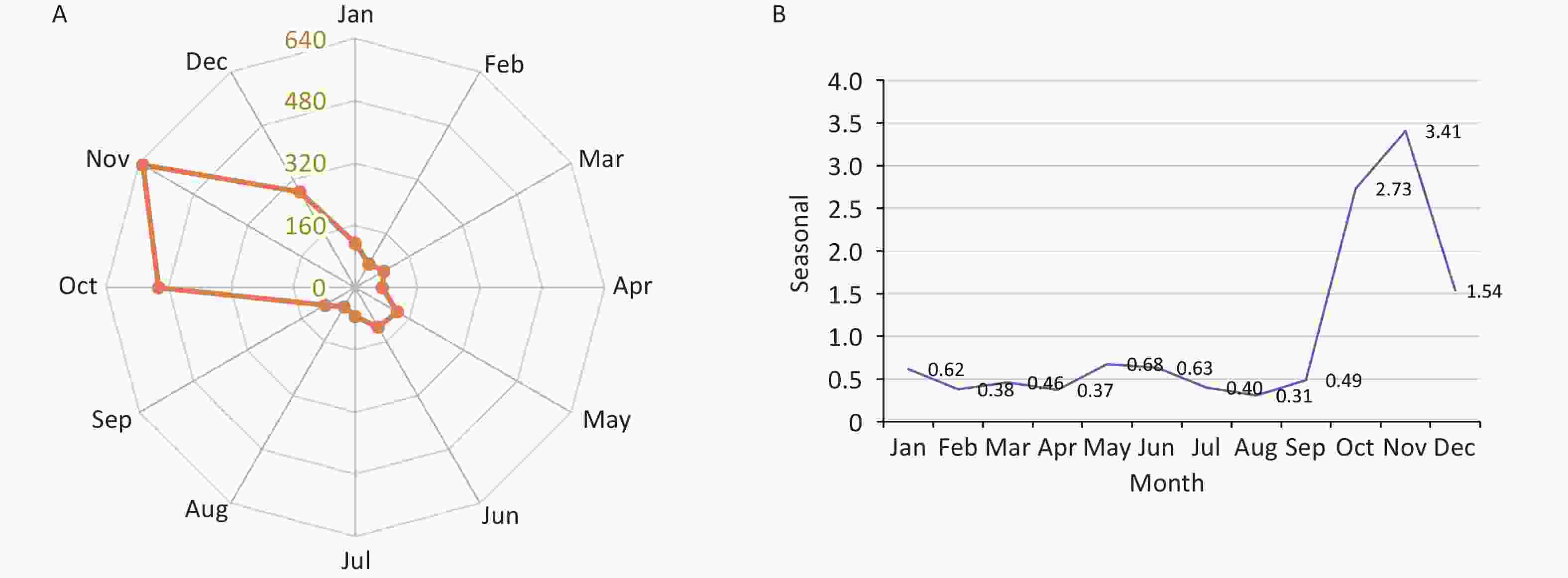
A global spatial autocorrelation analysis was performed based on street/township-level HFRS cases in Qingdao City. The annual global Moran’s I indexes, which ranged from 0.15 to 0.66, all passed the significance level test (P < 0.05), indicating that the spatial distribution of the HFRS epidemic was not random from 2010 to 2022 and showing t-shaped spatial autocorrelation characteristics at street/township-level scale. Moran’s I indexes showed an upward trend from 2010 to 2013, then an overall downward trend from 2014 onward. The distribution of the HFRS epidemic was significantly heterogeneous in Qingdao City from 2010 to 2022. (Table 5)
Table 5. Global spatial autocorrelation analysis of reported HFRS cases in Qingdao City, 2010–2022
Year Moran’s I Z-value P-value 2010 0.43 5.80 0.001 2011 0.42 5.27 0.001 2012 0.66 8.18 0.001 2013 0.66 8.18 0.001 2014 0.30 4.38 0.001 2015 0.23 3.35 0.009 2016 0.18 2.35 0.017 2017 0.32 4.58 0.002 2018 0.42 5.49 0.001 2019 0.35 4.60 0.001 2020 0.15 2.18 0.02 2021 0.27 3.82 0.002 2022 0.16 2.42 0.013 Note. HFRS, hemorrhagic fever with renal syndrome. A local indicators of spatial association analysis was performed to detect local (street/township-level) spatial clusters of the HFRS epidemic. From 2010 to 2022, the range of HFRS hot spots (High–High cluster area) in Qingdao City showed dynamic changes that were mostly distributed in Huangdao, Pingdu, and Jiaozhou (Figure 8).
-
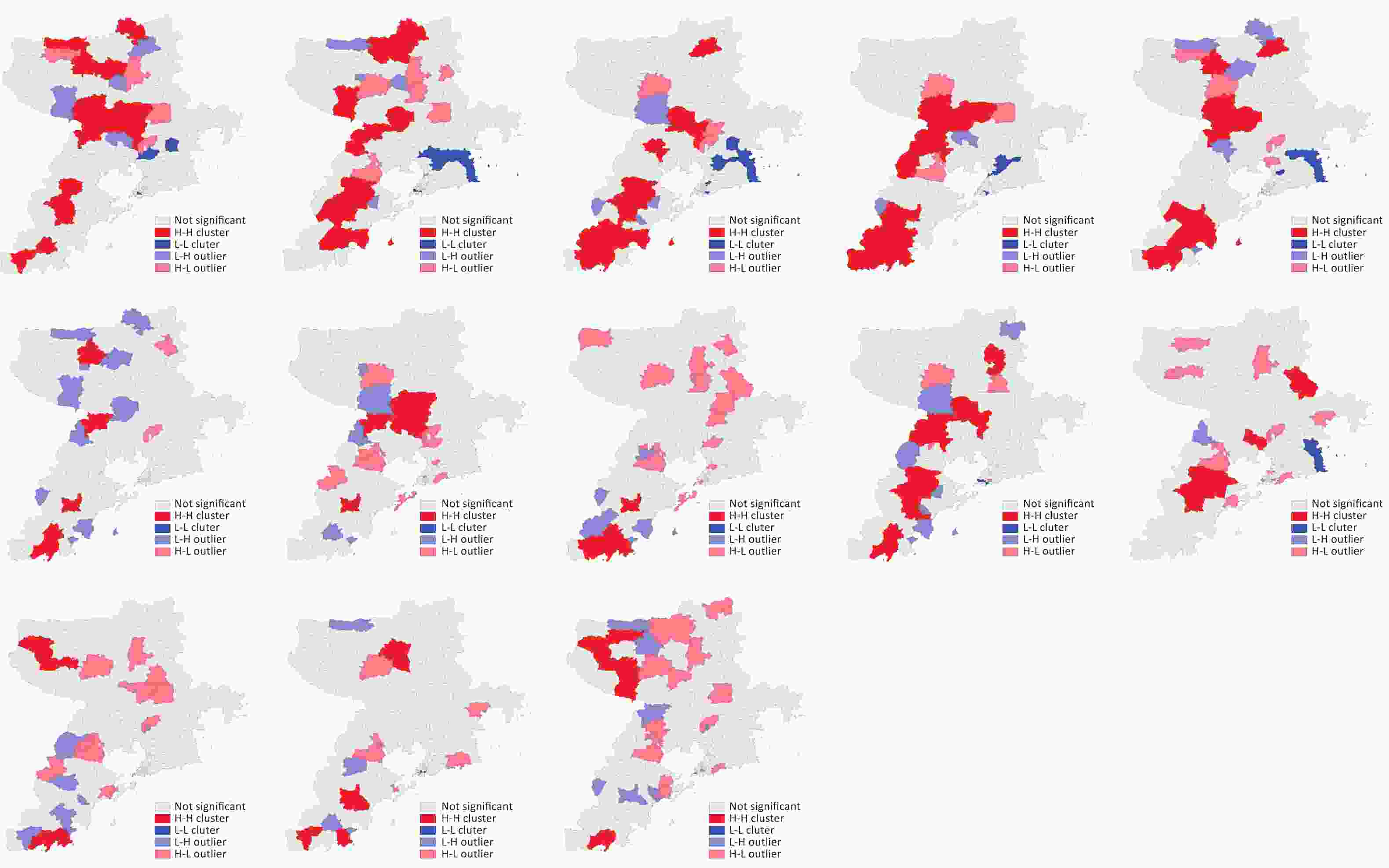
The incidence of HFRS was aggregated through space and time using Kulldorff’s spatio-temporal scan statistics. All the three significant clusters detected were located in the southern parts of Huangdao. The first cluster (RR = 3.14, log likelihood ratio [LLR] = 27.49) was in a 41.58 km radius from October to November 2012 and included 13 streets/townships; the expected case number was 20.1, and the observed case number was 61. The second cluster (RR = 4.55, LLR = 6.09) was in a 14.73 km radius from October to November 2017 and included four of the 13 streets/townships in the first and second clusters; the expected case number was 6.09, and the observed case number was 27. The third cluster (RR = 2.86, LLR = 11.61) was in a 49.16 km radius from October to November 2021 and included the same 13 streets/townships as the first cluster; the expected case number was 11.61, and the observed case number was 32. The spatio-temporal scanning results from 2010 to 2022 showed that the three cluster areas in Qingdao City were located in the south of Huangdao District during the fall-winter peak (Figure 9 and Table 6).

Figure 9. Spatio-temporal clusters of hemorrhagic fever with renal syndrome (HFRS) cases in Qigndao city at the street/township level, 2010–2022. The spatio-temporal scanning from 2010 to 2022 was conducted in three time periods. The left figure shows the results from 2010 to 2015, the middle figure shows the results from 2014 to 2019, and the right figure shows the results from 2018 to 2022. Most likely cluster: P-value < 0.05. Map approval number: GS(2022)1873.
Table 6. Spatio-temporal clusters analysis of reported HFRS cases in Qingdao City, 2010–2022
Radius (km) Occurrence time (year/month) Observed number of cases Expected number of cases LLR RR P value Number of streets/townships 41.58 2012/10-2012/11 61 20.10 27.49 3.14 < 0.001 13 14.73 2017/10-2017/11 27 6.09 19.58 4.55 < 0.001 4 49.16 2021/10-2021/11 32 11.61 12.41 2.86 < 0.001 13 Note. LLR, log likelihood ratio; RR, relative risk. -
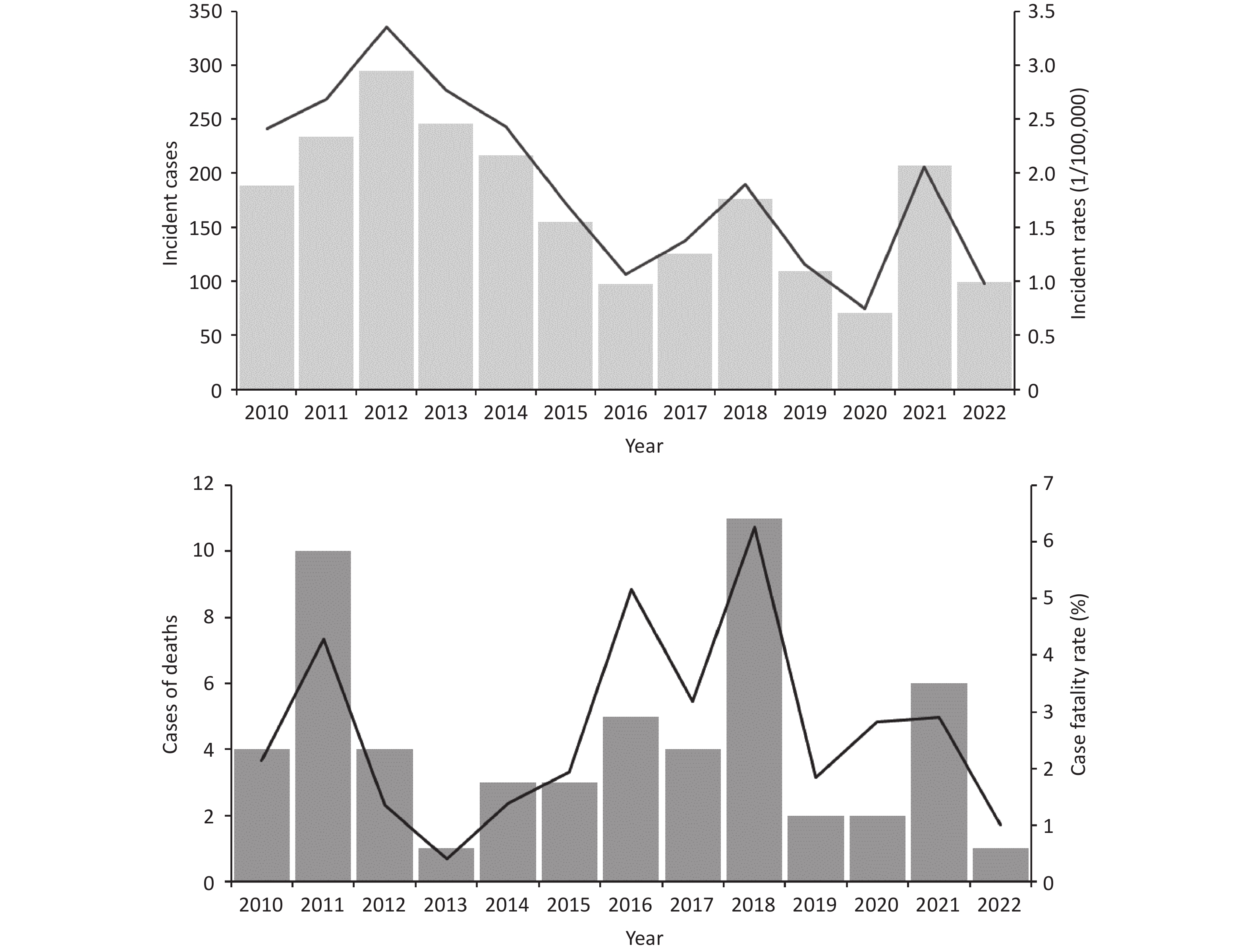
A total of 4,081 rodents and shrews were captured using 111,154 valid snap-traps that were set between 2011 and 2015. The average capture rate of hosts was 3.56%, and the average hantavirus infection rate of hosts was 8.82% from 2011 to 2015 (Table 1). The R-squared values of the linear fit to the trend lines for the incidence of HFRS versus Rattus norvegicus density and total host density were 0.75 and 0.58, respectively (Figure 10).
-
An overall decreasing trend in the incidence of HFRS in China has been observed in recent years[15,16,40,41]. However, HFRS has persisted under the current preventive measures that include rodent control and high-risk populations vaccination. The HFRS incidence rate in Qingdao is higher than that in Shandong Province and China (Figure 3). However, because the epidemic’s characteristics and the dynamic spatio-temporal distribution of HFRS in Qingdao City have not been systematically explored, this study analyzed these elements using case surveillance data from 2010 to 2022 at the street/township level in Qingdao.
The study revealed that the distribution of HFRS over the past 13 years in Qingdao City was regional, periodic and seasonal-consistent with the characteristics of the previous distribution of HFRS in Qingdao[28,38]. The top three districts or counties in the cumulative number of cases were Huangdao District, Pingdu City, and Jiaozhou City. Similarly, the results of the spatial autocorrelation analysis suggested spatial heterogeneity in the distribution of HFRS in Qingdao, with “high-high” clusters mostly dynamically distributed in Huangdao, Pingdu, and Jiaozhou. HFRS had a periodic epidemic peak approximately every 10 years. Results of this study showed that Qingdao had epidemic peaks in 2012 and 2021, which was roughly in line with a 10-year periodic distribution. The spatio-temporal scanning clusters were distributed in the south of Huangdao District at the time of the fall-winter peak, which conformed to the periodic distribution characteristics of HFRS. The Huangdao District consists of low-lying hills with forests and farmlands—a typical niche for the presence of hantavirus animal hosts. Consistent with the findings of previous studies, our results showed that each year, the incidence of HFRS in Qingdao City had a major epidemic season (October to January) and a minor seasonal peak (March to June) that corresponded to the fall-winter peak and spring peak HFRS, respectively. These bi-peaks may be associated with the living habits of local mice. There is a trend of linear correlation between the incidence rate and the density of host (Figure 10 and Table 7). However, we have lacked systematic and refined host surveillance data until now to totally confirm these assumptions. Therefore, continuous and uninterrupted research is needed in host surveillance and causative agent detection in Qingdao City to guide targeted HFRS prevention and control strategies.
Table 7. Data of annual human HFRS incidence and host surveillance in Qingdao City, 2011–2015
Year HFRS incidence Capture rate of hosts (%) Hantavirus-positive rate (%) Apodemus agrarius Rattus norvegicus Mus musculus Rattus rattus Sorex araneus Cricetulus triton Cricetulus arabensis Total Apodemus agrarius Rattus norvegicus Mus musculus Rattus rattus Sorex Araneus Cricetulus triton Cricetulus arabensis Total 2011 2.68 0.05 1.11 0.74 0.42 0 0 0.02 2.34 0 0.54 0 0 0 0.54 2012 3.35 0.88 1.73 1.36 0.02 0.35 0.62 0.15 5.11 6.5 3.1 3.26 0 0 0 0 12.86 2013 2.77 0.84 0.97 1.19 0 0.61 0.69 0.01 4.31 3.3 5.4 2.31 0 0 0 11.01 2014 2.42 0.49 1.15 1.22 0.16 0.21 0.31 0.02 3.56 5.06 2.17 2.56 0 0 0 0 9.79 2015 1.72 0.45 0.77 0.98 0 0.06 0.1 0.14 2.5 2.78 6.5 0.64 0 0 0 9.92 Average 2.59 0.54 1.15 1.1 0.12 0.25 0.34 0.07 3.56 3.52 3.54 1.75 8.82 HFRS is a natural infectious disease, and its main transmission occurs when people come into contact with mice and their excreta during work and life. Climate change, environmental alteration, and rapid urbanization and economic activities largely influence the HFRS incidence[42-44]. Physical labor in the fields, agricultural operations, and underdeveloped socioeconomic conditions are associated with the disease. The main susceptible population remains male farmers between 16 and 60 years of age. The higher risk of infection in male farmers compared with other groups may be attributable to their increased opportunity for contact with rodents. Given that most (75.3%) patients are farmers, strengthening the monitoring of the rodent situation and promoting education about HFRS prevention and control in rural areas are necessary. In addition, increasing residents' awareness of HFRS, actively conducting rodent prevention and control activities, and taking protective measures when engaging in high-risk behaviors can reduce disease occurrence.
The incidence (11.6%) of co-occurrence of typical “three red” and “three pain” between 2020 and 2022 was low. In contrast, consistent with the findings of previous studies[13,14,45,46], the proportion of gastrointestinal symptoms was relatively high (nausea 41.8%, vomiting 40.4%, and diarrhea 32.5%). HFRS is easily misdiagnosed because of the complex and diverse clinical symptoms in the early disease stages. Therefore, during the peak period of epidemic HFRS, clinicians should consider the possibility of HFRS if a suspicious or clear history of rodent contact exists and initial symptoms are mainly high fever with or without digestive symptoms.
Vaccination is the most effective measure for preventing epidemic HFRS[1,10]. Since 2008, China has included HFRS immunization in the expanded immunization plan, targeting high-risk townships in high-risk provinces and providing routine immunization to people aged 16–60 years. The population aged 60 years and above accounted for 23.4% of patients between 2010 and 2022, illustrating a shift in the high-prevalence age group of HFRS to above 60 years[16,22,43,44]. Broadening the age range of the vaccinated group is recommended. Among the 14 patients who were vaccinated against HFRS, 13 were vaccinated after infection, indicating that residents in areas with a high incidence of HFRS have insufficient awareness of the importance of HFRS vaccination. Therefore, strengthening HFRS vaccine knowledge is also necessary.
In the endeavor to prevent and control HFRS, several pivotal measures also should be undertaken. Firstly, there is an urgent need to bolster education and awareness regarding HFRS, especially during periods of peak incidence. This endeavor necessitates the elevation of public knowledge and comprehension of the disease, with a specific emphasis on high-risk regions, such as the southern area of Huangdao, where the frequency and intensity of promotional activities ought to be augmented. Secondly, rodent control measures must be vigorously implemented and seamlessly integrated with patriotic hygiene campaigns to forge a cohesive strategy for disease prevention. Regular rodent monitoring is also imperative to maintain vigilance and swiftly respond to any indications of rodent activity. Moreover, citizens must actively participate in daily preventative measures, emphasizing the significance of household hygiene and efficacious rodent control practices. It is of utmost importance to steer clear of potential sources of infection, such as contact with rodent urine or feces, and to adopt appropriate safety precautions when engaging in activities in rodent-dense areas.
Some limitations should be considered when interpreting our findings. First, because HFRS cases were identified by a passive surveillance system and we did not differentiate HTNV from SEOV infections, some bias may have been introduced. Second, given the gradual decrease in the area of cultivated land, the main occupation of many farmers is no longer agriculture; some farmers may also engage in other types of work. Thus, error may have been introduced during classification by occupation.
-
This study comprehensively analyzed the epidemic and spatio-temporal patterns of HFRS in Qingdao City from 2010 to 2022. The distribution of HFRS exhibited periodic, seasonal, and regional trends, peaking in 2012 and 2021. Typically, there were two seasonal peaks-a major fall-winter peak and a minor spring peak. Cases were mostly reported in Huangdao, Pingdu, and Jiaozhou. Spatial clustering was observed annually, with “high-high” clusters dynamically occurring in these regions. The spatio-temporal clusters were concentrated in southern Huangdao during the fall-winter peak, aligning with the disease’s 10-year cycle. Men and farmers were disproportionately affected. Vaccination awareness was low in high-risk areas, while the occurrence of “three red” and “three pain” symptoms was rare; gastrointestinal symptoms were more common. We suggest raising awareness of HFRS vaccination, expanding the vaccinated population, intensifying rural prevention education, and implementing rodent control measures in high-risk areas.
-
HFRS is classified as a Category B infectious disease in China, and confirmed cases must be reported to the Chinese Center for Disease Control and Prevention (China CDC) through the China National Notifiable Disease Surveillance System within 24 hours. Data collection is part of routine public health surveillance and is exempt from institutional review board evaluation. Ethical approval for this study was not required.
-
Ying Li, Renze Lu and Liyan Dong were joint corresponding authors who contributed equally to this work. Jing Jia, Huilai Ma, Fachun Jiang and Lijie Zhang conceived the study design and analytical plan. Liyan Dong, Litao Sun, Zongyi Zhang and Yating Zhao acquired the data. Qing Duan provided technical support in data analysis. Ying Li, Renze Lu and Liyan Dong performed statistical analysis and drafted the paper. Jing Jia, Huilai Ma was responsible for the revision of the draft. All authors critically revised the manuscript for important content and gave final approval for the version to be published.
doi: 10.3967/bes2024.092
Epidemic Characteristics and Spatio-Temporal Patterns of HFRS in Qingdao City, China, 2010–2022
-
Abstract:
Objective This study investigated the epidemic characteristics and spatio-temporal dynamics of hemorrhagic fever with renal syndrome (HFRS) in Qingdao City, China. Methods Information was collected on HFRS cases in Qingdao City from 2010 to 2022. Descriptive epidemiologic, seasonal decomposition, spatial autocorrelation, and spatio-temporal cluster analyses were performed. Results A total of 2,220 patients with HFRS were reported over the study period, with an average annual incidence of 1.89/100,000 and a case fatality rate of 2.52%. The male:female ratio was 2.8:1. 75.3% of patients were aged between 16 and 60 years old, 75.3% of patients were farmers, and 11.6% had both “three red” and “three pain” symptoms. The HFRS epidemic showed two-peak seasonality: the primary fall-winter peak and the minor spring peak. The HFRS epidemic presented highly spatially heterogeneous, street/township-level hot spots that were mostly distributed in Huangdao, Pingdu, and Jiaozhou. The spatio-temporal cluster analysis revealed three cluster areas in Qingdao City that were located in the south of Huangdao District during the fall-winter peak. Conclusion The distribution of HFRS in Qingdao exhibited periodic, seasonal, and regional characteristics, with high spatial clustering heterogeneity. The typical symptoms of “three red” and “three pain” in patients with HFRS were not obvious. -
Key words:
- Hemorrhagic fever with renal syndrome /
- Epidemic characteristics /
- Spatio-temporal distribution
注释: -
Figure 1. Annual incidence and mortality of hemorrhagic fever with renal syndrome (HFRS) in Qingdao from 2010 to 2022. The figure above indicates the annual number of cases and incidence rate, and the below figure indicates the annual of death and fatality rate.
HFRS, hemorrhagic fever with renal syndrome.
Figure 3. Spatial distribution of cumulative hemorrhagic fever with renal syndrome (HFRS) cases in county/district level of Qingdao City from 2010 to 2022. The figure left indicates the cumulative number of HFRS case; the figure right indicates of the cumulative incidence rates of HFRS cases. Map approval number: GS(2022)1873.
Figure 9. Spatio-temporal clusters of hemorrhagic fever with renal syndrome (HFRS) cases in Qigndao city at the street/township level, 2010–2022. The spatio-temporal scanning from 2010 to 2022 was conducted in three time periods. The left figure shows the results from 2010 to 2015, the middle figure shows the results from 2014 to 2019, and the right figure shows the results from 2018 to 2022. Most likely cluster: P-value < 0.05. Map approval number: GS(2022)1873.
Table 1. Characteristics of all 2,220 HFRS cases in Qingdao City, 2010–2022
Year Gender Age Male (%) Female (%) < 16 (%) 16–60 (%) > 60 (%) 2010 142 (75.5) 46 (24.5) 3 (1.6) 149 (79.3) 36 (19.1) 2011 181 (77.4) 53 (22.6) 2 (0.9) 186 (79.5) 46 (19.7) 2012 211 (71.5) 84 (28.5) 4 (1.4) 235 (79.7) 56 (19.0) 2013 169 (68.7) 77 (31.3) 2 (0.8) 197 (80.1) 47 (19.1) 2014 152 (70.0) 65 (30.0) 3 (1.4) 169 (77.9) 45 (20.7) 2015 119 (76.8) 36 (23.2) 4 (2.6) 112 (72.3) 39 (25.2) 2016 73 (75.3) 24 (24.7) 0 (0) 75 (77.3) 22 (22.7) 2017 96 (76.2) 30 (23.8) 3 (2.4) 88 (69.8) 35 (27.8) 2018 135 (76.7) 41 (23.3) 4 (2.3) 129 (73.3) 43 (24.4) 2019 86 (78.9) 23 (21.1) 1 (0.9) 74 (67.9) 34 (31.2) 2020 54 (76.1) 17 (23.9) 0 (0) 53 (74.6) 18 (25.4) 2021 151 (72.9) 56 (27.1) 2 (1.0) 141 (68.1) 64 (30.9) 2022 70 (70.7) 29 (29.3) 1 (1.0) 63 (63.6) 35 (35.4) Total 1639 (73.8) 581 (26.2) 29 (1.3) 1671 (75.3) 520 (23.4) Note. HFRS, hemorrhagic fever with renal syndrome. Table 2. Occupational classification of all 2220 HFRS cases in Qingdao City, 2010–2022
Occupation Number of cases Proportion (%) Farmer 1,672 75.3 Worker 165 7.4 Housework/unemployment 94 4.2 Student 53 2.4 Cadre/staff 52 2.3 Migrant worker 49 2.2 Retired personnel 31 1.4 Self-employed 21 0.9 Business service 18 0.8 Others 65 2.9 Total 2,220 100.0 Note. HFRS, hemorrhagic fever with renal syndrome. Table 3. The main clinical symptoms among HFRS cases in Qingdao City in 2020–2022
Symptom 2020 2021 2022 2020–2022 Number of cases Proportion (%) Number of cases Proportion (%) Number of cases Proportion (%) Number of cases Proportion (%) Rapid onset 40 76.9 105 63.3 63 67.7 208 66.9 Fatigue 41 78.8 145 87.3 73 78.5 259 83.3 Fever 49 94.2 139 83.7 84 90.3 272 87.5 Headache 31 59.6 106 63.9 51 54.8 188 60.5 Low back pain 25 48.1 87 52.4 29 31.2 141 45.3 Orbital pain 24 46.2 62 37.3 17 18.3 103 33.1 Blush 29 55.8 66 39.8 28 30.1 123 39.5 Neck redness 20 38.5 46 27.7 20 21.5 86 27.7 Chest redness 17 32.7 36 21.7 14 15.1 67 21.5 Joint pains 11 21.2 42 25.3 21 22.6 74 23.8 Whole body pains 9 17.3 63 38.0 20 21.5 92 29.6 Abdominal pain 12 23.1 45 27.1 30 32.3 87 28.0 Diarrhea 11 21.2 54 32.5 36 38.7 101 32.5 Constipation 9 17.3 2 1.2 4 4.3 15 4.8 Nausea 15 28.8 74 44.6 41 44.1 130 41.8 Vomiting 12 23.1 67 40.4 39 41.9 118 37.9 Conjunctival congestion 18 34.6 29 17.5 16 17.2 63 20.3 Puffy eyelids 12 23.1 27 16.3 16 17.2 55 17.7 Jaundice 5 9.6 4 2.4 6 6.5 15 4.8 Skin bleeding spots in the armpits, upper arms, chest, or other areas 14 26.9 25 15.1 10 10.8 49 15.8 Bleeding spots in the oral and nasal mucosa 6 11.5 12 7.2 1 1.1 19 6.1 Little or no urination 18 34.6 57 34.3 35 37.6 110 35.4 Hypotension 6 11.5 27 16.3 26 28.0 59 19.0 Shock 4 7.7 9 5.4 5 5.4 18 5.8 Normal leukocyte count 10 19.2 21 12.7 12 12.9 43 13.8 Increased leukocyte count 22 42.3 60 36.1 34 36.6 116 37.3 Decreased leukocyte count 4 7.7 3 1.8 5 5.4 12 3.9 Thrombocytopenia 22 42.3 71 42.8 43 46.2 136 43.7 Urinary protein 15 28.8 14 8.4 17 18.3 46 14.8 Urinary membrane/tubular urine/hematuria 2 3.8 5 3.0 3 3.2 10 3.2 Note. HFRS, hemorrhagic fever with renal syndrome. Table 4. The main typical clinical symptoms among HFRS cases in Qingdao City in 2020–2022
Typical symptoms 2020 2021 2022 2020–2022 Number of cases Proportion (%) Number of cases Proportion (%) Number of cases Proportion (%) Number of cases Proportion (%) Three red 17 32.7 32 19.3 12 12.9 61 19.6 Three pain 19 36.5 51 30.7 13 14.0 83 26.7 Three red and three pain 11 21.2 21 12.7 4 4.3 36 11.6 Note. HFRS, hemorrhagic fever with renal syndrome. Table 5. Global spatial autocorrelation analysis of reported HFRS cases in Qingdao City, 2010–2022
Year Moran’s I Z-value P-value 2010 0.43 5.80 0.001 2011 0.42 5.27 0.001 2012 0.66 8.18 0.001 2013 0.66 8.18 0.001 2014 0.30 4.38 0.001 2015 0.23 3.35 0.009 2016 0.18 2.35 0.017 2017 0.32 4.58 0.002 2018 0.42 5.49 0.001 2019 0.35 4.60 0.001 2020 0.15 2.18 0.02 2021 0.27 3.82 0.002 2022 0.16 2.42 0.013 Note. HFRS, hemorrhagic fever with renal syndrome. Table 6. Spatio-temporal clusters analysis of reported HFRS cases in Qingdao City, 2010–2022
Radius (km) Occurrence time (year/month) Observed number of cases Expected number of cases LLR RR P value Number of streets/townships 41.58 2012/10-2012/11 61 20.10 27.49 3.14 < 0.001 13 14.73 2017/10-2017/11 27 6.09 19.58 4.55 < 0.001 4 49.16 2021/10-2021/11 32 11.61 12.41 2.86 < 0.001 13 Note. LLR, log likelihood ratio; RR, relative risk. Table 7. Data of annual human HFRS incidence and host surveillance in Qingdao City, 2011–2015
Year HFRS incidence Capture rate of hosts (%) Hantavirus-positive rate (%) Apodemus agrarius Rattus norvegicus Mus musculus Rattus rattus Sorex araneus Cricetulus triton Cricetulus arabensis Total Apodemus agrarius Rattus norvegicus Mus musculus Rattus rattus Sorex Araneus Cricetulus triton Cricetulus arabensis Total 2011 2.68 0.05 1.11 0.74 0.42 0 0 0.02 2.34 0 0.54 0 0 0 0.54 2012 3.35 0.88 1.73 1.36 0.02 0.35 0.62 0.15 5.11 6.5 3.1 3.26 0 0 0 0 12.86 2013 2.77 0.84 0.97 1.19 0 0.61 0.69 0.01 4.31 3.3 5.4 2.31 0 0 0 11.01 2014 2.42 0.49 1.15 1.22 0.16 0.21 0.31 0.02 3.56 5.06 2.17 2.56 0 0 0 0 9.79 2015 1.72 0.45 0.77 0.98 0 0.06 0.1 0.14 2.5 2.78 6.5 0.64 0 0 0 9.92 Average 2.59 0.54 1.15 1.1 0.12 0.25 0.34 0.07 3.56 3.52 3.54 1.75 8.82 -
[1] Avšič-Županc T, Saksida A, Korva M. Hantavirus infections. Clin Microbiol Infect, 2019; 21S, e6−16. [2] Centers for Disease Control and Prevention. Hantaviruses. https://www.cdc.gov/hantavirus/technical/hanta/virology.html. [2012-08-29] [3] Noh JY, Jung J, Song JW. Hemorrhagic fever with renal syndrome. Infect Chemother, 2019; 51, 405−13. doi: 10.3947/ic.2019.51.4.405 [4] Vaheri A, Strandin T, Hepojoki J, et al. Uncovering the mysteries of hantavirus infections. Nat Rev Microbiol, 2013; 11, 539−50. doi: 10.1038/nrmicro3066 [5] Vial PA, Ferrés M, Vial C, et al. Hantavirus in humans: a review of clinical aspects and management. Lancet Infect Dis, 2023; 23, e371−82. doi: 10.1016/S1473-3099(23)00128-7 [6] Jiang H, Du H, Wang LM, et al. Hemorrhagic fever with renal syndrome: pathogenesis and clinical picture. Front Cell Infect Microbiol, 2016; 6, 1. [7] Xiao H, Gao LD, Li XJ, et al. Environmental variability and the transmission of haemorrhagic fever with renal syndrome in Changsha, People's Republic of China. Epidemiol Infect, 2013; 141, 1867−75. doi: 10.1017/S0950268812002555 [8] Tian HY, Hu SX, Cazelles B, et al. Urbanization prolongs hantavirus epidemics in cities. Proc Natl Acad Sci USA, 2018; 115, 4707−12. doi: 10.1073/pnas.1712767115 [9] Zou LX, Chen MJ, Sun L. Haemorrhagic fever with renal syndrome: literature review and distribution analysis in China. Int J Infect Dis, 2016; 43, 95−100. doi: 10.1016/j.ijid.2016.01.003 [10] Sehgal A, Mehta S, Sahay K, et al. Hemorrhagic fever with renal syndrome in asia: history, pathogenesis, diagnosis, treatment, and prevention. Viruses, 2023; 15, 561. doi: 10.3390/v15020561 [11] Gao JL, Yu J, Wang ZY, et al. Epidemiological and clinical characteristics of hemorrhagic fever with renal syndrome. J Dalian Med Univ, 2019; 41, 521−4. (In Chinese) [12] Xiang S. Clinical characteristics and influertial factors of severe hemorrhagic fever with renal syndrome in 247 cases. Fujian Medical University. 2020. (In Chinese) [13] Jiang RM, Chen ZH, Xu H, et al. Analysis of 244 misdiagnosed cases of Hantavirus hemorrhagic fever with renal syndrome in Beijing. Chin J Intern Med, 2006; 45, 590−1. (In Chinese) [14] Ji YS, Zhang YB, Wu C, et al. Analysis of 291 cases of misdiagnosis of hemorrhagic fever in renal syndrome. Chin J Misdiagn, 2007; 7, 4458. (In Chinese) [15] Deng XF, Du SS, Huang XX, et al. Epidemiological characteristics of hemorrhagic fever of renal syndrome in China, 2004−2021. Dis Surveill, 2023; 38, 70−4. (In Chinese) [16] Liu T, Tong YQ, Liu M, et al. Analysis of the trend of hemorrhagic fever with renal syndrome in China from 2004 to 2017. Chin J Zoonoses, 2022; 38, 515−22,547. (In Chinese) [17] Klein SL, Marks MA, Li W, et al. Sex differences in the incidence and case fatality rates from hemorrhagic fever with renal syndrome in China, 2004-2008. Clin Infect Dis, 2011; 52, 1414−21. doi: 10.1093/cid/cir232 [18] Yang QS. Study on spatio-temporal distribution and economic burden of hemorrhagic fever with renal syndrome in Yichun City from 2010 to 2017. Nanchang University. 2019. (In Chinese) [19] Zhang L, Wang T. An analysis of epidemiological and clinical data of hemorrhagic fever with renal syndrome in Zibo City, Shandong Province in 2015. Chin J Endemiol, 2016; 35, 922−5. (In Chinese) [20] Zhang RJ, Wang YL, Zheng HB. Early clinical characteristics and evaluation indexes of 180 cases of hemorrhagic fever with renal syndrome. Shanxi Med J, 2021; 50, 65−7. (In Chinese) [21] Yan L, Fang LQ, Huang HG, et al. Landscape elements and hantaan virus–related hemorrhagic fever with renal syndrome, People’s Republic of China. Emerg Infect Dis, 2007; 13, 1301−6. doi: 10.3201/eid1309.061481 [22] Chen JJ, Guo TC, Song SX, et al. Epidemiological characteristics and the development of spatiotemporal analysis models on hemorrhagic fever with renal syndrome in China. Chin J Epidemiol, 2020; 41, 1735−40. (In Chinese) [23] Duan Q, Xing YF, Kou ZQ, et al. Spatio-temporal aggregation of hemorrhagic fever with renal syndrome in Shandong Province from 2017 to 2020. Chin J Endemiol, 2022; 41, 715−21. (In Chinese) [24] Zheng ZL, Wang PZ, Xu QQ, et al. Analysis on epidemiological and temporal-spatial distribution characteristics of hemorrhagic fever with renal syndrome in Shandong province, 2010-2016. Chin J Epidemiol, 2018; 39, 58−62. (In Chinese) [25] Fang LQ, Wang XJ, Liang S, et al. Spatiotemporal trends and climatic factors of hemorrhagic fever with renal syndrome epidemic in Shandong Province, China. PLoS Negl Trop Dis, 2010; 4, e789. doi: 10.1371/journal.pntd.0000789 [26] She KL, Li CY, Qi C, et al. Epidemiological characteristics and regional risk prediction of hemorrhagic fever with renal syndrome in Shandong Province, China. Int J Environ Res Public Health, 2021; 18, 8495. doi: 10.3390/ijerph18168495 [27] Liu YX, Wang ZQ, Guo J, et al. Spatio-temporal evolution on geographic boundaries of HFRS endemic areas in Shandong Province, China. Biomed Environ Sci, 2013; 26, 972−8. [28] Jiang FC, Wang L, Wang S, et al. Meteorological factors affect the epidemiology of hemorrhagic fever with renal syndrome via altering the breeding and hantavirus-carrying states of rodents and mites: a 9 years' longitudinal study. Emerg Microbes Infect, 2017; 6, e104. [29] Shandong Center for Disease Control and Prevention. Notice on Holding 2023 Field Training Course on Hantavirus hemorrhagic fever with renal syndrome Prevention and Control Technology in Shandong Province. 2023. (In Chinese) [30] Jiang FC, Dong LY, Zhang ZT, et al. Evolution characteristics of hemorrhagic fever with renal syndrome in Huangdao and Jiaonan of Qingdao City, Shandong Province from 1979 to 2014. Chin J Endemoil, 2017; 36, 819−23. (In Chinese) [31] Wang XC, Shen WQ, Qin YF, et al. A case-control study on the risk factors for hemorrhagic fever with renal syndrome. BMC Infect Dis, 2020; 20, 103. doi: 10.1186/s12879-020-4830-5 [32] Li SJ, Zhu LL, Zhang LD, et al. Urbanization-related environmental factors and hemorrhagic fever with renal syndrome: a review based on studies taken in China. Int J Environ Res Public Health, 2023; 20, 3328. doi: 10.3390/ijerph20043328 [33] Jiang FC, Dong LY, Hao B, et al. The influence of agricultural mechanization progress on epidemiological characteristics of hemorrhagic fever with renal syndrome in Qingdao areas. Chin J Endemiol, 2018; 37, 997−1001. (In Chinese) [34] Jiang FC, Dong LY, Hao B, et al. The influence of urbanization development and topographic on the epidemiological characteristics of hemorrhagic fever with renal syndrome in Qingdao areas. Proceedings of the Eighth Technical Forum on Research and Application of Infectious Disease Prevention and Control Technologies. 2017: 139-47. (In Chinese) [35] Zhu LL, Li YP, Lu L, et al. Spatial heterogeneity and influencing factors of HFRS epidemics in rural and urban areas: a study in Guanzhong plain of shaanxi Province, China. Biomed Environ Sci, 2022; 35, 1012−24. [36] He JY, Christakos G, Wu JP, et al. Spatiotemporal variation of the association between climate dynamics and HFRS outbreaks in Eastern China during 2005-2016 and its geographic determinants. PLoS Negl Trop Dis, 2018; 12, e0006554. doi: 10.1371/journal.pntd.0006554 [37] Ge L, Zhao YL, Zhou K, et al. Spatio-temporal pattern and influencing factors of hemorrhagic fever with renal syndrome (HFRS) in Hubei Province (China) between 2005 and 2014. PLoS One, 2016; 11, e0167836. doi: 10.1371/journal.pone.0167836 [38] Bo T, Jiang FC. Epidemiological characteristics of hemorrhagic fever with renal syndrome in Qingdao from 1979 to 2003. J Med Pest Control, 2007; 23, 594−5. (In Chinese) [39] Wu ZC, Fu GF, Wen Q, et al. Spatiotemporally comparative analysis of HIV, pulmonary tuberculosis, HIV-pulmonary tuberculosis coinfection in Jiangsu Province, China. Infect Drug Resist, 2023; 16, 4039−52. doi: 10.2147/IDR.S412870 [40] Xiao YH, Li YY, Li YH, et al. Estimating the long-term epidemiological trends and seasonality of hemorrhagic fever with renal syndrome in China. Infect Drug Resist, 2021; 14, 3849−62. doi: 10.2147/IDR.S325787 [41] Wang YB, Xu CJ, Wu WD, et al. Time series analysis of temporal trends in hemorrhagic fever with renal syndrome morbidity rate in China from 2005 to 2019. Sci Rep, 2020; 10, 9609. doi: 10.1038/s41598-020-66758-4 [42] Shen L, Sun MH, Wei X, et al. Spatiotemporal association of rapid urbanization and water-body distribution on hemorrhagic fever with renal syndrome: a case study in the city of Xi'an, China. PLoS Negl Trop Dis, 2022; 16, e0010094. doi: 10.1371/journal.pntd.0010094 [43] Liang WF, Gu X, Li X, et al. Mapping the epidemic changes and risks of hemorrhagic fever with renal syndrome in Shaanxi Province, China, 2005-2016. Sci Rep, 2018; 8, 749. doi: 10.1038/s41598-017-18819-4 [44] Li X, Liu K, Gu X, et al. Epidemiological characteristics and environmental risk factors of hemorrhagic fever with renal syndrome in Wei River basin, China, 2005-2015. Chin J Epidemiol, 2018; 39, 1159−64. (In Chinese) [45] Lee GY, Kim WK, No JS, et al. Clinical and immunological predictors of hemorrhagic fever with renal syndrome outcome during the early phase. Viruses, 2022; 14, 595. doi: 10.3390/v14030595 [46] Du H, Wang PZ, Li J, et al. Clinical characteristics and outcomes in critical patients with hemorrhagic fever with renal syndrome. BMC Infect Dis, 2014; 14, 191. doi: 10.1186/1471-2334-14-191 -




 下载:
下载:



 Quick Links
Quick Links