-
Childhood is a crucial period for physical growth, as well as neurodevelopment and psychologic development. Adequate nutrition, as the foundation for growth and development in childhood, can reduce the incidence of infectious diseases for this stage of life and non-communicable diseases (NCDs) in adulthood [1]. Moreover, fostering a healthy diet is associated with lifelong benefits [2]. Childhood malnutrition reduces individual income and societal productivity in adulthood, and thus, constrains overall socioeconomic development [3].
At the National Meeting on Health, which was held on 19 August 2016, President Xi Jinping emphasized that health should be listed as a strategic development priority, with a focus on child health and ensuring the growth and development of children [4]. Child nutrition status is a vital indicator of national socioeconomic development, thus ensuring healthy and nourished children contributes to high-caliber human resources.
The Child Nutrition and Health Survey is an evaluation tool that facilitates implementation of national development goals. Ending child malnutrition is a United Nations sustainable development goal (SDG) [5]. In addition, both the National Programme of Action for Children and the National Plan of Action for Food and Nutrition state goals to improve child nutrition. Indeed, there is an urgent need to collect basic data on child nutritionand health between 2016 and 2020 to meet the aforementioned national goals, to address the current child nutrition and health issues confronting China in a step-by-step manner, and to track the development of national policies on child nutrition.
A Child Nutrition and Health Survey is required to take timely stock of the child nutrition and health data under a fast-developing social context. The fast socioeconomic changes are currently accompanied by the transition for child nutrition and health. In 2013, the under 6 year (U6) stunting rate was as low as 8.1% [6]; however, overweight and obese children are on the rise, affecting 9.6% and 6.4% of children between 6 and 17 years of age in 2010–2012, respectively. As a result of the Nutrition Improvement Program for Rural Compulsory Education Student (implemented in 2011) and Child Nutrition Improvement (Ying Yang Bao) Program in Poor Rural Regions (implemented in 2012), child nutrition and health status have experienced drastic improvements. The profound changes taking place in the social and family structures have also presented new challenges for the child nutrition and health program in the new era [7]. Children who are left behind and grandparent caretakers of only children are prevalent. Children experience the fastest development between 0 and 6 years of age, and dietary intake and psychological behaviors jointly impact the child development [8]; however, nationally representative data on neuropsychological development of children is limited.
A series of child nutrition and health surveys have been conducted since 1949 that have provided basic data on the overall improvement in child nutrition [9]; however, all surveys have been beset by a level of inadequacy, such as a small number of survey indicators, narrow age groups, and under-representation. Therefore, a systematic survey on the basic child nutrition and health data for children < 18 years of age is planned. Nutritional status, growth, dietary intake, physiologic and metabolic indicators, neurodevelopment, and health status of children < 18 years of age will be reported.
-
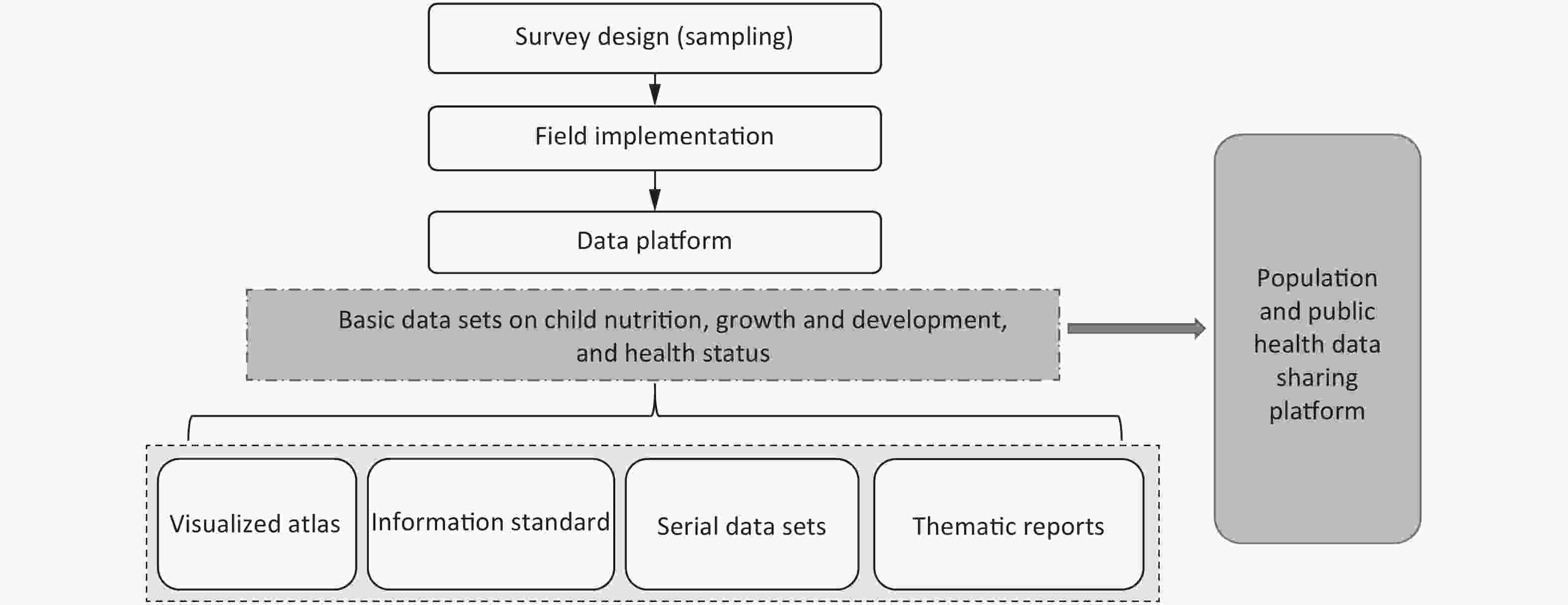
The main objectives of the current study are as follows: obtain basic survey data on child nutrition and health; develop a series of data sets; develop visualized atlases and information standards; share data on the National Population and Health Data Platform; promote the development of basic disciplines related to child nutrition and health; and feed the data into in-depth research and development of policies related to child nutrition and health. The specific aims are as follows:
First, basic data on the nutrition, development, and health status of children 0–17 years of age in different geographic regions, from all socioeconomic backgrounds, age groups, and genders using evidence-based, reliable, and cost-effective approaches will be collected. Such data will include dietary intake, nutrition status, physical growth, body composition, bone mass, physiology and metabolism, physical fitness, lifestyle, and socioeconomic information.
Second, a child nutrition and health survey report will be drafted and an integrated response strategy in this area will be proposed by compiling the historical survey data and taking into consideration the situation on children and the interaction between children and parents.
-
Children 0−17 years of age and their parents or guardians from seven regions (e.g., south, southwest, north, northwest, eastern, central, and northeast) in China were selected. Based on the different health and nutrition profiles of children 0−5 and 6−17 years of age in China, the anemia and obesity rates were used as the sampling indicators to calculate the sample size. Sample size was estimated considering the prevalence of anemia (11.6%) with a precision of 2.6% for children 0−5 years of age, and the prevalence of obesity (6.4%) with a precision of 1.5% for children 6−17 years of age and a 95% confidence interval for each stratum. There were 28 strata (7 regions, 2 urban/rural samples, and 2 genders). Assuming a 10% non-response rate, 38,000 children 0−5 years of age and 66,000 children 6−17 years of age, and their parents or guardians were sampled. Table 1 shows a detailed sample size and source population of the different age groups.
Table 1. Sample size and sources of survey subjects from all age groups
Age group
(years)Months Interval Groups Subjects for
each groupSimple size for
the survey siteTotal
sample sizeSources 0−2 0−5 Every month 6 66 990 27,720 Neighborhood or village 6−11 Every two months 3 12−23 Every three months 4 24−35 Every six months 2 3−5 Every six months 6 66 396 11,088 Kindergarten or village 6−14 Every year 9 196 1,764 49,392 Primary school and junior high school 15−17 Every year 3 196 588 16,464 Senior high school The inclusion criteria were as follows: < 18 years of age; healthy children born locally; lived in the survey site for > 6 months (for children older than 6 months of age); and signed a written informed consent form. Children with acute and chronic diseases, such as acute respiratory tract infection, acute gastroenteritis, and congenital heart defects, were excluded.
-
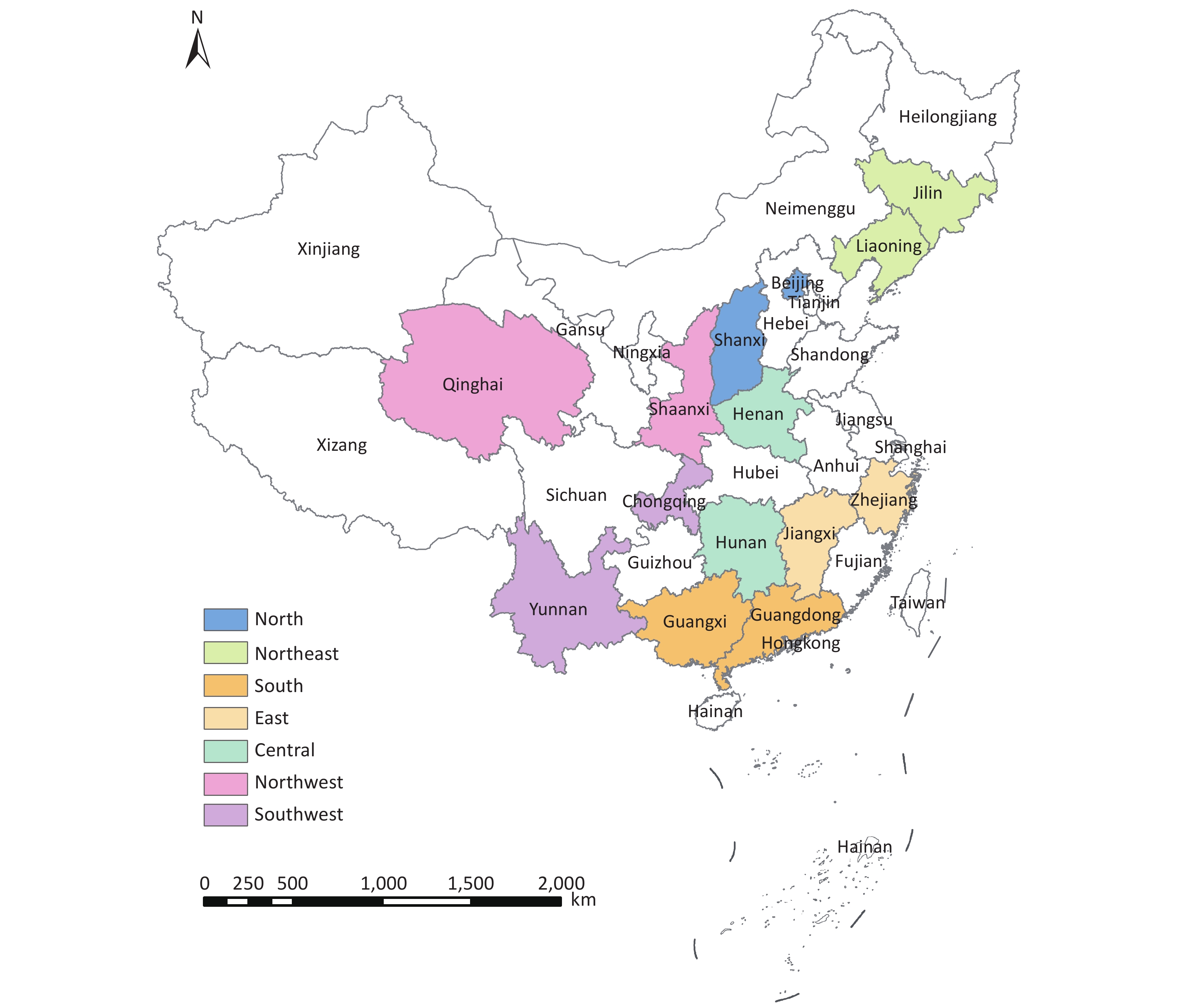
A multi-stage stratified randomized cluster sampling method was used. Two provinces were randomly sampled from each of the seven regions (south, southwest, north, northwest, eastern, central, and northeast China). One urban district and one rural county were randomly sampled from each province, for a total of 28 survey counties/district. The survey counties were not only national representatives, but also represented the urban and rural areas.
First stage: Two provinces were randomly selected from east (7 provinces), north (5 provinces), central (3 provinces), south (3 provinces), southwest (5 provinces), northwest (5 provinces), and northeast China (3 provinces). A total of 14 provinces were selected (Zhejiang, Jiangxi, Shanxi, Beijing, Hunan, Henan, Guangdong, Guangxi, Yunnan, Chongqing, Shaanxi, Qinghai, Jilin, and Liaoning) (Figure 1).
Second stage: All the districts and counties in every province were tiered into urban and rural categories. For each tier, one district (urban) or one county (rural) was randomly selected as the survey site. District refers to those under the provincial capitals, cities in independent planning status, and prefectures.
Third stage: Four sub-districts (a lower administrative unit under a district) or townships/towns were selected from every urban survey site or each rural survey site. From every district/county, 1−2 senior high schools were selected.
Fourth stage: Four communities or four villages were sampled from each sub-district for urban sites or each township/town for rural sites. One primary school and one junior high school were selected from each sub-district or township/town.
Fifth stage: Children < 3 years of age were randomly cluster-sampled from children roll at the selected neighborhoods or villages. Children 3−5 years of age were randomly cluster-sampled from the kindergartens or villages. Children 6−17 years of age were randomly cluster-sampled from the selected primary, junior, and senior high schools. The sample size of every age group with a gender balance required for each group is depicted in Table 1.
Sixth stage (sampling of advanced survey children): Among the sampled children from each survey site, 48 children (0−23 months of age) were randomly selected (four children for each month except for infants < 1 month of age). Forty children 2−5 years of age were cluster-sampled from the selected subjects at each survey site (5 children for every 6 months). A total of 360 children 6−17 years of age were randomly cluster-sampled from the selected children from primary, junior high, and senior high school (30 for each age group). Gender balance was required for each group.
-
The project was approved by the Medical Ethical Review Committee at the National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention (No. 2019-009). Parents or guardians of the study subjects signed the informed consent form, and for children > 8 years of age, both parents/guardians and the child co-signed the informed consent form.
-
The field survey began in May 2019 and stopped in November 2021. A dietary survey, health examinations, laboratory testing, and questionnaire survey were used to collect diet, nutrition, development, health status, socioeconomic, and demographic status information. The knowledge attitude practice (KAP) survey of children and their parents on nutrition, health, and lifestyle was collected (Figure 2).
-
Food Frequency Questionnaire The food frequency questionnaire was adapted to each age group of children, including an infant and young child feeding questionnaire, 2−5 years old food frequency questionnaire, and 6−17 years old food frequency questionnaire. A validated food frequency questionnaire with 11 groups of foods and 72 food items was administrated to all sampled school children[10].
24-h Dietary Recall and Weighed Food Record For children < 2 years of age, the 1-day (24 h) test weighing method was used to measure the amount of breastmilk intake, which was the children’s body weight difference immediately before and after each breastfeeding. Total breastmilk intake was the sum of breastmilk intake from each breastfeeding over the past 24 h (Seca 335, medical baby scale; Hamburg, Germany). The weighed food record was used to collect all food intakes, except breastmilk (electronic kitchen scale). For children < 2 years of age, the 1-day dietary weighed food record was administrated with all advanced surveys. For children 2−5 years of age, a 3-day dietary weighed food record method was administered to all advanced survey children.
Three-day 24-h dietary recall: Dietary intake data for children 6−17 years of age were collected using a 3-day 24-h dietary recall. Cooking oil, table salt, and spices were weighed at home or school at the same time. All food eaten in the household, kindergarten, or school canteen were recalled during three consecutive days. The sample size for each survey site was subtotaled to 360 children with 30 children every year for the 6−17 years age group.
-
Hemoglobin All children had their fingertip blood collected for hemoglobulin testing using a HemoCue 201+ system (HemoCue AB, Skån, Sweden). Anemia was determined according to the hemoglobin level after adjusting for altitude.
Other Lab Testing Indicators Children who were given the advanced survey had their fasting venous blood and spot urine collected in the morning for nutritional status assessment, including vitamin A, vitamin D, iron, zinc, selenium, and iodine (Tables 2–3).
Table 2. Biomedical indicators and sample size for different age groups
Age group (years) Tested content Number per group Total 3−5 Serum ferritin, C-reactive protein, 25-hydroxy vitamin D, retinol, selenium, zinc; whole blood lead; and urinary iodine, sodium, potassium, and creatinine 30 children sampled for their venous blood and urine at each survey site 840 6−17 Serum ferritin, C-reactive protein, 25-hydroxyvitamin D, retinol, selenium, zinc, blood lipids, blood sugar, glycated hemoglobin; whole blood lead; and urine iodine, sodium, potassium, and creatinine 360 children sampled for their venous blood and urine at each survey site 10,080 Table 3. Biomedical indicators and the associated testing method for different age groups
Indicator Testing method Bio-sample Serum ferritin Electrochemiluminescence Serum Serum C-reactive protein Immunoturbidimetric method Serum Serum Vit A HPLC-tandem MS Serum Serum 25 hydroxyvitamin D HPLC-tandem MS Serum Serum zinc ICP-MS Serum Serum selenium ICP-MS Serum Whole blood lead Graphite furnace atomic absorption spectrometry Whole blood Blood lipids Blood total CHO Enzymatic method Serum Triglyceride Enzymatic method Serum HDL-C Immunosuppression Serum LDL-C Selective protection method Serum Blood glucose Enzymatic method Serum Glycated hemoglobulin Immunoturbidimetric HPLC Serum Urine iodine Spectrophotometry Urine Urine sodium Ion selective electrode method Urine Urine potassium Ion selective electrode method Urine Urine creatinine Chemical method Urine Note. HPLC-tandam MS, High performance liquid chromatography tandem mass spectrometry; ICP-MS. Inductively coupled plasma mass spectrometry; CHO, Cholesterol; HDL-C, High-density lipoprotein cholesterol; LDL-C, Low-density lipoprotein cholesterol. -
Weight All children were weighed in the morning after fasting using digital weight scales (GMCS-I electronic scale; Jianmin, Beijing, China). The maximum capacity of the scale was 100 kg and the smallest division was 100 g.
Length/Height The length of all children < 2 years of age was determined with a measuring board (YSC-2, accuracy, 1 mm; Guo Wang Xing Da Scale company, Beijing, China). Height and sitting height for all children 2−17 years of age were determined with a stadiometer (accuracy, 0.1 cm; Jianmin). Body mass index (BMI) was calculated with weight (kg) divided by height squared (m2). Malnutrition and obesity was determined using an age-gender specific BMI cut-off [11].
Circumference Head circumference was measured with insertion circumference tapes for children < 5 years of age (accuracy, 0.1 cm). Arm circumference was measured with insertion circumference tapes (accuracy, 0.1 cm). Waist circumference was measured with waist circumference tapes for children 3−17 years of age (accuracy, 0.1 cm).
Skinfold Thickness Triceps skinfold thickness was measured with a skinfold thickness caliper for all children (accuracy, 1 mm; Jianmin).
-
Bone mineral density (BMD) was measured with dual-energy X-ray absorptiometry (DEXA) for advanced survey children 3−17 years of age.
-
Body fat and lean body mass were measured using the bioelectrical impedance analysis (BIA) method for all children aged 3−17 years of age (InBody 770 body composition analyzer; Seoul, South Korea).
-
British Tanner’s five-stage method was used to measure stages of puberty development for children 8−17 years of age based on self-reported breast and pubic hair development for girls, and penis and pubic hair development for boys [12].
-
Neuropsychological development was assessed by a healthcare physician for children < 6 years of age in the advanced survey group: [WS/T 580−2017 (revised version of the Child Development Scale)], which includes the overall developmental quotient of five developmental domains (gross motor, fine motor, language, adaptability, and social behavior) [13].
Wechsler Intelligence Scale for Children [WISC-IV (Chinese adapted version)] was used to assess intellectual development, including speech comprehension, perceptual reasoning, working memory, processing speed, and full-scale IQ for children 7, 9, 12, and 16 years of age in the advanced survey group by certified professional staff.
-
Physiology and Metabolism An electronic sphygmomanometer was used to measure blood pressure and heart rate for those in the advanced survey group.
Physical Fitness: Myodynamia and Endurance Handgrip strength, standing long jump and 50 m × 8 shuttle run were used to assess muscle strength and endurance for children 6−17 years of age in the advanced survey group.
-
Questionnaires were used to collect data on nutrition and health knowledge, and dietary habits and lifestyle of children and their parents. Knowledge, attitudes, practices, and sources of information on food choices, nutrition and health, and self-evaluation of dietary and health status were included in the nutrition and health knowledge part.
Children’s Physical Activity: Daily physical activity, exercise, travel, static state, reading, video watching, and sleep information was collected with a pre-tested children physical activity questionnaire for all children 6−17 years of age [14]. A wearable device was used to record the physical activity of children 3−17 years of age in the advanced survey group.
Dietary habits were collected, including food preferences, eating and drinking habits, places and time of eating, meal frequencies, fast food, snacks, drinks, and nutrient supplements. Awareness of the health examination results and risky behaviors, such as tobacco and alcohol use, were also included.
Parents’ Knowledge and Dietary Habits: Based on the characteristics of children at different ages, data regarding parent knowledge, attitudes, behaviors, and sources of information about nutrition, health, and parenting were collected. The self-evaluation of dietary habits was also surveyed.
-
We built an integrated data management platform with computers and tablets. We established a computer-aided survey system with tablets as a data collector and achieved partial visualization of survey results. This platform included a collection and storage data function, monitoring operations, control quality, and carrying out management to ensure standardization, high efficiency, and high quality of information collection.
-
The results of this project will be shared in a multi-level access restricted approach through the Public Health Scientific Data Centre under the National Population and Health Science Data Sharing Platform. The shared content includes project documents, such as project plans, survey questionnaires, and dataset standards, datasets of 28 survey sites and seven regional visualization atlases, published papers, and special reports. This project will regularly submit scientific data collected to the project management agency.
-
To visually present the nutrition and health status of Chinese children, we applied corresponding statistical analysis methods, established the analysis process, and built an analysis model on the basic geographic data and data on child nutrition and health. The data system automatically generates statistical analysis results and realizes visual presentation in the form of line graphs, histograms, and spatial geographic maps so that the visual atlas of all the data can be produced.
-
A project quality control team consisted of dedicated personnel from the leading project agency. Overall quality control plan was established. Quality control specialists were appointed for each sub-project to conduct field quality control in accordance with the overall plan, identified critical control points in project implementation, and created a standard operating procedure (hereinafter referred to as the SOP), which was reviewed and filed by the project quality control team. Each provincial project site was equipped with one or two quality supervisors who were responsible for supervising investigators under the SOP requirements and carried out spot checks on the quality of findings.
-
Quality control covered the entire process, including field investigation, data entry, sample collection, storage and transportation, pretreatment, laboratory testing, and atlas development.
General Requirements National or provincial level training was given to all team members. Training materials were videotaped and made available for all team members. All project staff underwent relevant training and passed qualification tests before undertaking any project work.
All instruments used in field measurements were unified with the same brand and model and were verified or calibrated by a qualified institution following the requirements for measurement and calibration. All instruments met the requirements of field measurement before being used.
All reagents and consumables used in the project followed the specifications formulated by the project team and purchased and accepted by the team. Replacing the approved reagents and consumables were not allowed in any sub-project. Special replacement needs to be reviewed and filed by the quality control team.
Third-party laboratories undertaking the project outsourced analysis had CMA/CNAS certification with approved experience that recognizes its capacity to undertake outsourced tests. They passed the central quality control test organized by the project.
All data were copied and saved to two hard disks and kept by two different people to prevent any damage and loss.
Questionnaires were filled out on the spot. No question was allowed to be left blank or filled in afterward.
Establishment of Standard Operating Procedures (SOPs) SOPs for field investigation, sample collection, storage, transportation and disposal, project inspection, and data entry were established.
-
A national quality control team checked the capacity of field investigators, questionnaire quality, samples, lab test results, internal quality control, data entry, implementation of the quality control plan, and quality records, and conducted ad hoc inspections to supervise and evaluate the entire quality control process regularly and irregularly. The team took corrective and preventive measures for issues not meeting the requirements and explored the quality control approaches, models, roles, and effects for large projects involving testing of a huge sample size and population, while ensuring the quality of the project.
-
The investigation team consists of child nutrition and health experts from the following areas, such as nutrition, epidemiology, child healthcare, mental health, information standard, and mathematical statistics. The field investigations were conducted by the Center for Disease Control (CDC) system and Maternal and Child Healthcare (MCH) system.
-
By 8 November 2021, the questionnaire survey was completed, the physical examination was near-completion, and > 94% of dietary intake data based on weighed food record or dietary recall method was completed for all three age groups of children (Table 4). Greater than 95% (73,237/76,944) of children 3−17 years of age completed the body composition examination and 96% (3,359/3,500) of child psychological development was tested using the Wechsler Intelligence Scale.
Table 4. Survey contents completed rate of CNHSC by November 8, 2021
Study contents Children
(under 2 years)Children
(2−5 years)Children
(6−17 years)Questionnaire 100.4% (24,111/24,024)* 102.3% (15,127/14,784) 100.6% (66,277/65,856) Physical examination 99.5% (23,907/24,024) 104.0% (15,368/14,784) 98.7% (64,999/65,856) Dietary intake 97.4% (1,309/1,344) 94.4% (1,057/1,120) 95.0% (9,574/10,080) Note. *Number of children completed/sample size for all values. This study was a large scale and comprehensive child nutrition and health survey with > 100,000 children in 7 regions across China, that covered dietary intake, dietary pattern, physical growth, body composition, bone mass, puberty development, psychological development, micronutrient status, physiology, metabolism, and physical fitness. The results from CNHSC could be used to identify the current nutrition and health issues and to assess the impact of child nutrition improvement in China. Furthermore, the CNHSC data will be shared via national scientific data sharing platform and researchers across broad areas could make use of the data to investigate potential risk factors and improvement methods for child nutrition and health for future studies.
-
WZ, ZY, QZ, YZ, TX, XT, BC, and YW designed the study. WZ, ZY, QZ, TX, RL, YW, XY, HF, YZ, XP, SW, JX, and XS implemented the study. WZ, ZY, and QZ drafted the manuscript. All authors reviewed the final content of the manuscript.
-
We are grateful for the hard work of the field staff and study subjects for their participation. We greatly appreciate Dr. LI Shu Juan for survey map making and Ms. HU Zhuo Lun for English editing.
doi: 10.3967/bes2021.122
National Nutrition and Health Systematic Survey for Children 0–17 Years of Age in China
-
Abstract: The main purpose of the National Nutrition and Health Systematic Survey for children 0−17 years of age in China (CNHSC) was to collect basic data on the nutrition, development, and health status for children in different regions across China using evidence-based, reliable, and cost-effective approaches. Children and their parents or guardians from seven regions (south, southwest, north, northwest, eastern, central, and northeast China) in China were recruited. A multi-stage stratified randomized sampling method was used. Two provinces were randomly sampled from each of the seven regions, from which one urban district and one rural country were also randomly sampled, resulting in a total of 28 survey counties/districts. Dietary surveys, health examinations, laboratory testing, and questionnaires were used to collect dietary intake, nutritional status, child development, and health status information. Nutrition, health, and lifestyle assessment of children and their parents was determined using the Knowledge Attitude Practice (KAP) survey. Greater than 100,000 children (38,000 children < 6 years of age and 66,000 children 6−17 years of age) completed the survey. The survey provided comprehensive data on child nutrition and health status for future studies and will serve as the basis for an integrated nutrition and health improvement strategies proposal for children in China.
-
Key words:
- Children 0−17 years of age /
- Nutritional status /
- Health status /
- Study protocol
注释: -
Table 1. Sample size and sources of survey subjects from all age groups
Age group
(years)Months Interval Groups Subjects for
each groupSimple size for
the survey siteTotal
sample sizeSources 0−2 0−5 Every month 6 66 990 27,720 Neighborhood or village 6−11 Every two months 3 12−23 Every three months 4 24−35 Every six months 2 3−5 Every six months 6 66 396 11,088 Kindergarten or village 6−14 Every year 9 196 1,764 49,392 Primary school and junior high school 15−17 Every year 3 196 588 16,464 Senior high school Table 2. Biomedical indicators and sample size for different age groups
Age group (years) Tested content Number per group Total 3−5 Serum ferritin, C-reactive protein, 25-hydroxy vitamin D, retinol, selenium, zinc; whole blood lead; and urinary iodine, sodium, potassium, and creatinine 30 children sampled for their venous blood and urine at each survey site 840 6−17 Serum ferritin, C-reactive protein, 25-hydroxyvitamin D, retinol, selenium, zinc, blood lipids, blood sugar, glycated hemoglobin; whole blood lead; and urine iodine, sodium, potassium, and creatinine 360 children sampled for their venous blood and urine at each survey site 10,080 Table 3. Biomedical indicators and the associated testing method for different age groups
Indicator Testing method Bio-sample Serum ferritin Electrochemiluminescence Serum Serum C-reactive protein Immunoturbidimetric method Serum Serum Vit A HPLC-tandem MS Serum Serum 25 hydroxyvitamin D HPLC-tandem MS Serum Serum zinc ICP-MS Serum Serum selenium ICP-MS Serum Whole blood lead Graphite furnace atomic absorption spectrometry Whole blood Blood lipids Blood total CHO Enzymatic method Serum Triglyceride Enzymatic method Serum HDL-C Immunosuppression Serum LDL-C Selective protection method Serum Blood glucose Enzymatic method Serum Glycated hemoglobulin Immunoturbidimetric HPLC Serum Urine iodine Spectrophotometry Urine Urine sodium Ion selective electrode method Urine Urine potassium Ion selective electrode method Urine Urine creatinine Chemical method Urine Note. HPLC-tandam MS, High performance liquid chromatography tandem mass spectrometry; ICP-MS. Inductively coupled plasma mass spectrometry; CHO, Cholesterol; HDL-C, High-density lipoprotein cholesterol; LDL-C, Low-density lipoprotein cholesterol. Table 4. Survey contents completed rate of CNHSC by November 8, 2021
Study contents Children
(under 2 years)Children
(2−5 years)Children
(6−17 years)Questionnaire 100.4% (24,111/24,024)* 102.3% (15,127/14,784) 100.6% (66,277/65,856) Physical examination 99.5% (23,907/24,024) 104.0% (15,368/14,784) 98.7% (64,999/65,856) Dietary intake 97.4% (1,309/1,344) 94.4% (1,057/1,120) 95.0% (9,574/10,080) Note. *Number of children completed/sample size for all values. -
[1] Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet, 2013; 382, 427−51. doi: 10.1016/S0140-6736(13)60937-X [2] Wells JC, Sawaya AL, Wibaek R, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet, 2020; 395, 75−88. doi: 10.1016/S0140-6736(19)32472-9 [3] Hawkes C, Ruel MT, Salm L, et al. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet, 2020; 395, 142−55. doi: 10.1016/S0140-6736(19)32506-1 [4] The State Council the People's Republic of China. Leaders call for full protection of people’s health. http://english.www.gov.cn/news/top_news/2016/08/21/content_281475421847599.htm. [2016-08-20]. [5] United Nations. Sustainable development goals. https://sdgs.un.org/goals/goal2. [2021-11-16]. [6] Yu DM, Zhao LY, Yang ZY, et al. Comparison of undernutrition prevalence of children under 5 years in China between 2002 and 2013. Biomed Environ Sci, 2016; 29, 165−76. [7] Baker P, Santos T, Neves PA, et al. First-food systems transformations and the ultra-processing of infant and young child diets: the determinants, dynamics and consequences of the global rise in commercial milk formula consumption. Matern Child Nutr, 2021; 17, e13097. [8] Prado EL, Larson LM, Cox K, et al. Do effects of early life interventions on linear growth correspond to effects on neurobehavioural development? A systematic review and meta-analysis. Lancet Global Health, 2019; 7, e1398−413. doi: 10.1016/S2214-109X(19)30361-4 [9] Yang ZY, Zhang HM, Wang Y, et al. Strategies and measures of nutrition improvement for children under 5 years in China. J Food Sci Technol, 2020; 38, 8−13. (In Chinese [10] Liu D, Ju LH, Yang ZY, et al. Food frequency questionnaire for Chinese children aged 12-17 years: validity and reliability. Biomed Environ Sci, 2019; 32, 486−95. [11] National Health and Family Planning Commission of the People's Republic of China. Screening standard for malnutrition of school-age children and adolescents (WS/ T 456-2014). Beijing: Standards Press of China, 2014. (In Chinese) [12] Tanner JM. Growth at adolescence. 2nd ed. Blackwell Scientific Publications. 1962. [13] National Health Standard of China. Development scale for children aged 0-6 years 2017. [14] Yang X, Jago R, Zhai Y, et al. Validity and reliability of Chinese physical activity questionnaire for children aged 10-17 years. Biomed Environ Sci, 2019; 32, 647−58. -





 下载:
下载:



 Quick Links
Quick Links