-
In 2015, there were an estimated 422.7 million cases of cardiovascular disease (CVD) and 17.92 million CVD deaths worldwide[1]. CVD remains the major cause of health loss and increasing the disease burden in low- and middle-income regions[2]. In China, CVDs have been the leading cause of death[3] and the total deaths of CVDs reached 3.5 million annually[4]. Rapid environmental changes accompanied with urbanization lead to the increasing prevalence of the major risk factors for CVD[5, 6]. Women's age of CVD occurrence was older than that of men, while the risk of CVDs in women increased rapidly after menopause[7, 8]. Effect of sex differences on CVD was explored during the past decades. Female hormones were hypothesized as an important cardioprotective factor[8-11], which was initially supported by retrospective studies[12-14] and some clinical trials[15, 16].
Hypertension, dyslipidemia, diabetes, obesity, smoking, and physical inactivity are traditional CVD risk factors[17-19]. In addition, female-specific risk factors like pregnancy related disorders, depression and menopause[20] have been given increased attention[8, 21-24]. But there still lacks solid evidence for cost-benefit analysis of these factors and no guidelines of the health practice, especially among Chinese women. It is still challenging to incorporate these emerging risk factors into the current risk assessment tools[25]. Once the issue is clarified, opportunities will afford to take more targeted preventive measures for female CVD.
In the present study, we designed the Jidong Women Health Cohort Study, a large community-based prospective cohort study, to assess the relationship between female-specific characteristics and CVD. The rationale, design, methods and baseline characteristics of Jidong Women Health Cohort Study were described.
-
This study was carried out according to the guideline of the Declaration of Helsinki[26]. Approval was obtained from Ethical Committees of the Staff Hospital of Jidong oil-field of China National Petroleum Corporation. The approval will be renewed every 5 years. Written informed consent was obtained from each of the participants.
-
Jidong Women Health Cohort Study is a community-based prospective cohort study designed to investigate the associations between female-specific characteristics and the risks of non-communicable chronic diseases, especially CVD. Early pathological changes like intima-media thickness (IMT), artery plaques, and arterial stenosis will be included as predictors for potential cardiovascular events[27-29]. Their associations with women's lifestyle exposure, medication, depression, and sleep conditions will also be studied prospectively.
Participants were recruited from Jidong Community, Caofeidian district, Tangshan city, northern China (Figure 1) through cluster sampling. Caofeidian district is located at the south of Tangshan city and near the Bohai sea, with an area of 1, 944 km2 and a population of 268.7 thousand (according to 2012 China census). Tangshan is a large, modern industrial city located in the central section of the circum-Bohai region, where it adjoins two mega cities: Beijing and Tianjin.
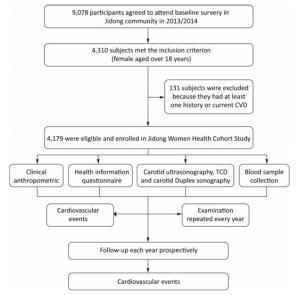
A total of 4, 310 females over 18 years old who agreed to be involved in follow-up investigation were recruited. Among these 4, 310 individuals, 113 subjects were excluded by the following exclusion criteria (1) history of cardiovascular or cerebrovascular condition like stroke, transient ischemic attack, coronary heart disease, heart failure and atrial fibrillation; and (2) any type of cancer. Finally, a total of 4, 179 subjects were included into the Jidong women health cohort study (Figure 2).
All the participants were invited to complete a questionnaire and physical examinations according to the testing program (Table 1). The questionnaire collected information on demographics, lifestyle variables, medical history and female-specific characteristics. Then a long-term follow-up will be conducted annually to collect the information above and data on clinical outcomes.
Table 1. Testing Program in the Jidong Women Health Cohort Study
Test Components Gynecology Gynecologic examination, pap smear, pelvic ultrasound Specimen collection Fasting blood sample Anthropometry Height, weight, ankle-branchial index, waist and hip circumference Participant break Refreshment break with food provided Cardiovascular 12 lead ECG, vascular profiling (blood pressures, pulse wave velocity), transcranial doppler, carotid artery sonography Depression Center Epidemiological Studies Depression (CES-D) scale[30] Sleep conditions Athens Insomnia Scale (AIS)[31] -
We designed the health information questionnaire to collect the participants' pertinent information as below. Demographics included age, ethnic group, marital status, education, and family monthly income per capita. Marital status was categorized as 'unmarried', 'married', or 'divorced or widowed'. Education background was reported as 'illiteracy or primary school', 'junior high school', or 'college or higher'. Family monthly income per capita was classified as '≤ ¥1, 000', '¥1, 001-3, 000', '¥3, 001-5, 000', and ' > ¥5, 000'.
Questionnaire of lifestyle included items on physical activity, alcohol and tobacco use, passive smoking, tea consumption and salt intake. Physical activity was categorized as 'inactive', 'moderately active', or 'very active' using the short form of the International Physical Activity Questionnaire (IPAQ)[32]. Alcohol consumption was measured comparing to one standard drink which is equal to 120 mL of wine or 360 mL of beer or 45 mL of Chinese liquor. Smoking status was regarded as 'never', 'former', or 'current'. Details on daily smoking amount, years of passive smoking and frequencies of tea consumption and salt intake were also collected.
Medical histories on arterial hypertension, dyslipidemia, diabetes, and cardiovascular or cerebrovascular conditions (atrial fibrillation, heart failure, myocardial infarction, stroke and transient ischemic attack) were collected using questionnaire. Current use of medication and age at initial diagnosis was viewed as major evidence for medical histories taking. Female-specific medical histories included the use of contraceptives and HRT, which was described with initiating time of usage, duration and type of medicine.
Depressive symptoms were evaluated with 20 questions using the Center Epidemiological Studies Depression (CES-D) Scale[30]. The score is the sum of the 20 questions, ranging from 0-60. Participants with a score of 16 points or more were considered depression.
Sleep conditions were assessed by the Athens Insomnia Scale (AIS) with 8 items. Possible range of total score is 0-24. Participants with the score over 6 points were defined as insomnia[31].
-
Female-specific characteristics included menstrual and reproductive history, sexual dysfunction and menopause conditions. Detailed information of menstrual and reproductive history included pregnant frequency, delivery times, age at menarche, regularity of menstrual cycle and gynecologic surgery history. Sexual dysfunction was assessed by self-reported dissatisfaction with sexual life[33]. Participants were asked to fill an item 'How satisfied are you with your current sexual life?' (0 point = satisfied, 1 point = a little unsatisfied, 2 points = unsatisfied, and 3 points = very unsatisfied). The responses were divided into normal sexual function (response 0 point) or sexual dysfunction (response 1, 2, and 3 points).
-
Menopause conditions were assessed in aspects of menopausal age, menopausal processes, menopausal symptoms, use of contraceptives and hormone replacement therapy (HRT). Menopause is defined as the point at which a woman stops having a menstrual period when she has not had a period for 12 consecutive months[34]. Menopause transition begins with menstrual period variability and menopause symptoms occur when estrogen and progesterone levels change. According to the STRAW staging system[35], female population was divided into 3 subgroups: reproductive, the menopausal transition and postmenopausal.
Menopausal symptoms were measured through 11 questions, including hot flushes and sweating, heart symptoms, sleep disorders, depression, irritability, nervousness, behavioral or memory impairment, sexual life, urinary problems, vaginal dryness and arthromuscular symptoms. Scores ranging from 0 to 10 indicated the degree of menopausal symptoms. Participants were asked to report the most influential menopausal symptom from the 11 items above additionally.
Information on use of contraceptives and HRT was collected in medical histories taking.
-
Body weight, body height, waist and hip circumference were measured according to standard anthropometric techniques. Body mass index (BMI) and waist-to-hip ratio (WHR) were calculated. And the BMI was classified as ' < 18.5', '18.5-23.9', '24-27.9', and '≥ 28'. Blood pressure was determined to the nearest 2 mmHg via a mercury column type sphygmomanometer. Three readings of systolic blood pressure (SBP) and diastolic blood pressure (DBP) were taken to calculate the mean value as the final blood pressure value.
Blood samples were collected from the antecubital vein in the morning under fasting conditions using vacuum tubes containing EDTA (ethylene diamine tetraacetic acid) and coagulation-promoting tubes. After on-site processing and centrifugation, serum and plasma samples were collected for plasma glucose, triglyceride (TG), total cholesterol (TC), low-density lipoproteins cholesterol (LDL-C) and high-density lipoproteins cholesterol (HDL-C) testing and biospecimen banking (-80 ℃). Fasting blood glucose was measured by hexokinnase/glucose-6-phosphate dehydrogenase assay. Cholesterol and triglyceride concentrations were determined by enzymatic methods (Mind Bioengineering Co. Ltd, Shanghai, China). Blood samples were also measured using an auto-analyzer (Hitachi 747; Hitachi, Tokyo, Japan) at the central laboratory of the Staff Hospital of Jidong oil-field of China National Petroleum[36].
Arterial hypertension was defined as a SBP > 140 mmHg, or a DBP > 90 mmHg; diabetes was defined as a fasting blood glucose level ≥ 7.0 mmol/L; dyslipidemia was assessed in aspects of serum levels of TG ≥ 1.7 mmol/L, TC ≥ 5.2 mmol/L, LDL-C ≥ 3.4 mmol/L or HDL-C ≤ 1.0 mmol/L[37]. Self-reported disease histories and current use of medication were convenient results for medical diagnoses as well.
-
Bilateral carotid ultrasonography (Philips iU-22 ultrasound system, Philips Medical Systems, Bothell, WA) was used as a noninvasive procedure to provide artery information including carotid IMT and carotid artery plaque. Thus, early stages of arteriosclerosis could be observed. IMT measurements were performed on the far wall of bilateral common arteries and proximal internal carotid arteries. Both sides of common carotid artery (CCA), internal carotid artery (ICA), and subclavian artery were examined for carotid plaques. Detailed information on carotid plaques including numbers, location, length, structure and surface characteristics was recorded.
Internal carotid arterial stenosis (ICAS) and vertebral arterial stenosis were evaluated by a bilateral carotid duplex sonography. Carotid artery stenosis was classified according to the recommendations from Society of Radiologists in Ultrasound Consensus Conference[38]. An ICA peak systolic velocity (PSV) ≥ 125 cm/s, ICA/CCA PSV ratio ≥ 2 or ICA end-diastolic flow velocity (EDV) ≥ 40 cm/s indicates an ICAS (≥ 50%). Brightness mode ultrasonography results were combined as well.
In addition, transcranial Doppler sonography (TCD) was applied to the participants using portable devices (EMC Companion, Nicolet, Madison, WI, USA) to evaluate intracranial arterial stenosis. The intracranial arterial stenosis was diagnosed on the basis of increased flow velocity or disturbed blood flow. Age of the participants should be considered while making a conclusion. Commonly, arterial stenosis was defined by a peak systolic flow velocity of > 120 cm/s for the anterior cerebral artery and siphon internal carotid artery, > 140 cm/s for the middle cerebral artery and > 100 cm/s for the posterior cerebral artery and vertebra-basilar artery. All the examination results were reviewed by two independent specialists.
-
The study participants will be followed up via face-to-face interviews once a year in a routine medical examination up to December 31, 2024, or up to the occurrence of a final event as defined in the study, or occurrence of death. The follow-up is supposed to be performed annually by well-trained research assistants and physical examiners. Questionnaire and physical examinations will be performed with the same standard as the baseline investigation. Data on clinical outcomes will be collected every five years by a standard operational procedure follow-up system which includes hospitalization reports and files from local general practitioners and medical specialists. Besides, data of the registry on all death cause of residents will be obtained for further study.
Primary outcomes are new onset hypertension, dyslipidemia, diabetes, female cancers and major adverse cardiovascular events including ischemic stroke, hemorrhagic stroke, cardiac death, myocardial infarction, ischemic heart disease, heart failure and atrial fibrillation. Meanwhile, IMT, arterial stenosis and arterial plaques are considered while evaluating the primary outcomes. An End Points Committee has been approved by the Project Executive Committee before the start of the study. Disease diagnosis will be finally confirmed by the endpoint adjudication committee after prudent review of all the records.
-
All research assistants, interviewers, and physical examiners are well trained in all items of the questionnaires, or all aspects of measurements (using standardized techniques). Training programs are conducted on-site, and within the laboratories of each of the participating investigators under the supervision of experienced staff, until the required standard of testing and competency has been achieved.
During the survey, regular central monitoring is also undertaken to assess the distribution of certain key variables, the time delay with blood processing and consistency of the data collected. On-site monitoring visits are undertaken every 6-month by staff from Hospital of Jidong oil-field of Chinese National Petroleum. In addition, quality control monitoring regarding the follow-up has also been conducted by staff from a third party (Recovery Medical Technology Development Corporation).
-
Before statistical analysis, all the data will be examined to ensure the accuracy and completeness. Firstly, descriptive statistics are applied to reveal the distribution of baseline characteristics including demographics, lifestyle, female characteristics information and CVD risk factors. Continuous variables are presented as mean ± SD (standard deviation). Categorical variables are presented as counts (percentage). Non-normal distributed variables like serum triglycerides concentration are log transformed. Secondly, parameters differences between groups are evaluated using t-test or analysis of variance (ANOVA) for normally continuous variables and chi-square tests for categorical variables. Longitudinal analysis towards demographics, female characteristics, risk factors, primary outcomes and their relationship will be performed through linear regression, logistic regression, survival analysis and cox proportional hazard models. Hazard ratios (HR) will be presented with their 95% corresponding confidence intervals (CI). The level for statistical significance will be set at α = 0.05 (two tailed).
-
A total of 4, 179 female participants were enrolled in the Jidong Women Health Cohort Study, with 2, 948 of reproductive, 173 of the menopausal transition and 1, 058 of postmenopause. Individuals without the occurrence of hypertension, dyslipidemia or diabetes (n = 1, 535) were identified at baseline ensuring the cohort a sufficient sample size. The baseline characteristics were summarized in Table 2. The mean age of the participants at cohort entry was 42.3 ± 12.8 years. Majority of participants were of Han nationality (97%) and married (91.3%). Most of the participants reported never drinking (98.3%) or smoking (95%), while about 66% of participants reported passive smoking. About 50.1% of participants were very active in physical activity and 53.8% had medium salt intakes.
Table 2. Baseline Characteristics
Characteristics Total (n, %) Reproductive Menopausal Transition Postmenopausal P-value* n 4, 179 (100) 2, 948 (70.5) 173 (4.1) 1, 058 (25.3) Age (years) 42.3 ± 12.8 35.9 ± 8.6 48.3 ± 3.6 59.1 ± 6.1 < 0.001** Ethnic group 0.102 Han 4, 055 (97.0) 2, 851 (96.7) 168 (97.1) 1, 036 (97.9) Else 124 (3.0) 97 (3.3) 5 (2.9) 22 (2.1) Marital status 0.003* Unmarried 247 (5.9) 240 (8.1) 6 (3.5) 7 (0.7) Divorced or Widowed 116 (2.8) 53 (1.8) 167 (96.5) 57 (5.4) Married 3, 816 (91.3) 2, 655 (90.1) 173 (100) 994 (94.0) Education < 0.001** Illiteracy or primary school 194 (4.6) 18 (0.6) 102 (59) 172 (16.3) Junior high school 1, 601 (38.3) 742 (25.2) 67 (38.7) 757 (71.6) College or higher 2, 384 (57.0) 2, 188 (74.2) 173 (100) 129 (12.2) Income < 0.001** ≤ ¥3, 000 1, 733 (41.5) 925 (31.4) 89 (51.4) 743 (70.2) ¥3, 001-5, 000 2, 133 (51.0) 1, 762 (59.8) 16 (9.2) 282 (26.7) > ¥5000 256 (6.1) 215 (7.3) 170 (98.3) 25 (2.4) Smoking 0.157 Never 4, 109 (98.3) 2, 909 (98.7) 166 (96.0) 1, 034 (97.7) Current 65 (1.6) 37 (1.3) 7 (4.0) 21 (2.0) Former 4 (0.1) 1 (0.0) 0 (0.0) 3 (0.3) Passive smoking 2, 758 (66.0) 1, 887 (64.0) 98 (56.6) 773 (73.1) < 0.001** Alcohol consumption 0.021* Never 3, 971 (95.0) 2, 787 (94.5) 162 (93.6) 1, 022 (96.6) Less than one standard drink 106 (2.5) 81 (2.7) 4 (2.3) 21 (2.0) Equal or more than one standard drink 102 (2.4) 80 (2.7) 7 (4.0) 15 (1.4) Tea consumption < 0.001** Never 2, 818 (67.4) 1, 910 (64.8) 104 (60.1) 804 (76.0) Less than once a week 348 (8.3) 288 (9.8) 15 (8.7) 45 (4.3) 1-3 times a week or more 1, 013 (24.2) 750 (25.4) 54 (31.2) 209 (19.8) Salt intake (g) 0.331 < 6 1, 087 (26.0) 765 (25.9) 47 (27.2) 275 (26.0) 6-12 2, 249 (53.8) 1, 550 (52.6) 91 (52.6) 608 (57.5) > 12 842 (20.1) 633 (21.5) 35 (20.2) 174 (16.4) Physical Activity < 0.001** Inactive 1, 481 (35.4) 1, 121 (38.0) 47 (27.2) 313 (29.6) Moderately active 605 (14.5) 512 (17.4) 28 (16.2) 65 (6.1) Very active 2, 093 (50.1) 1, 315 (44.6) 98 (56.6) 680 (64.3) BMI < 0.001** < 18.5 228 (5.5) 215 (7.3) 1 (0.6) 12 (1.1) 18.5-23.9 2, 233 (53.4) 1, 727 (58.6) 93 (53.8) 413 (39.0) 24-27.9 1, 082 (25.9) 622 (21.1) 48 (27.7) 412 (38.9) ≥ 28 453 (10.8) 228 (7.7) 28 (16.2) 197 (18.6) WHR 0.8 ± 0.1 0.8 ± 0.1 0.9 ± 0.1 0.9 ± 0.1 < 0.001** Female-specific characteristics Age at menarche 14.3 ± 1.8 13.9 ± 1.5 14.7 ± 1.7 15.6 ± 1.9 < 0.001** Age of menopause 49.9 ± 4.4 49.9 ± 4.4 Sexual dysfunction 99 (2.4) 43 (1.5) 10 (5.8) 46 (4.3) < 0.001** Take oral contraceptives 31 (1.4) 8 (0.8) 0 (0) 23 (2.2) 0.009 Receive HRT 12 (0.5) 1 (0.1) 0 (0) 11 (1) 0.624 Depression 255 (6.1) 188 (6.4) 14 (8.1) 53 (5.0) 0.150 Insomnia 662 (15.8) 337 (11.4) 47 (27.2) 278 (26.3) < 0.001** Arterial hypertension 429 (10.3) 130 (4.4) 19 (11.0) 280 (26.5) < 0.001** Diabetes 134 (3.2) 30 (1.0) 4 (2.3) 100 (9.5) < 0.001** TG (mmol/L) 1.3 ± 0.98 1.2 ± 0.84 1.4 ± 0.93 1.7 ± 1.19 < 0.001** TC (mmol/L) 4.4 ± 0.91 4.2 ± 0.77 4.7 ± 0.89 5.1 ± 0.95 < 0.001** LDL-C (mmol/L) 2.4 ± 0.63 2.2 ± 0.54 2.6 ± 0.64 2.8 ± 0.63 < 0.001** HDL-C (mmol/L) 1.3 ± 0.27 1.3 ±0.26 1.3 ± 0.30 1.3 ± 0.27 0.005* Note. *P < 0.05, **P < 0.001 indicates statistically significant. BMI, body mass index; WHR, waist-to-hip ratio; HRT, hormone replacement therapy; TG, triglyceride; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol. The mean age at menarche was 14.3 ± 1.8 years. Most of the participants reported having a regular menstrual cycle before 35 years. About 1, 058 participants have been menopausal and the mean age of FMP was 49.9 ± 4.4 years. Besides, 173 participants were in the stage of menopausal transition. Among those over 40 years old, nearly 36% of participants reported varying degrees of menopausal symptoms. Behavioral or memory impairment, hot flushes and sweating, irritability and sleep disorders were the most outstanding affects. 225 participants reported depression, but no significant difference was found between groups. Significant differences were found for WHR, BMI and incidence of sexual dysfunction, insomnia, arterial hypertension, dyslipidemia and diabetes between groups (P < 0.05).
-
CVD continues to be a leading health problem for women with growing and aging populations. China is facing this challenge as well at the stage of economic takeoff accompanied with a transition of the living environment and lifestyle. Recent studies also raised awareness that sex disparity was reflected in aspects of prevention, diagnosis and treatment of CVD. For example, baseline concentrations of some cardiovascular biomarkers were different between men and women[39]. A cohort study in the United Kingdom revealed that high-sensitivity assays on cardiac troponin and a lower diagnosis cut-off point might improve the diagnosis of female myocardial infarction[40]. Some regions have started to make efforts for prevention of female CVD. But researches and potential interventions are still needed. In-depth researches are of great importance for us to take health cohort studies among Chinese women.
Our study revealed differences in the incidence of hypertension, diabetes and dyslipidemia among groups which indicated different cardiovascular risks among these groups stratified by STRAW system at baseline. Further longitudinal study after years of follow-up would give better evidence to reveal the association between menopause and incidence of cardiovascular diseases along with other noncommunicable chronic diseases.
Several women health cohorts were found from website on clinical trials. Characteristics on design and study population of these studies[41-45] are presented in the Table 3. And the similarity and differences between our study and others were also shown. Strengths of our study were discussed as follows. Firstly, we recruited female over 18 years old as the study population. This could help better understanding female physical and psychological changes and cardiovascular risk factor changes as well as their effect on women's health over a wider range of lifetime. Secondly, depression, sleep condition, sexual dysfunction, female menstrual history, reproductive history and menopause condition were comprehensively included as major factors in our study, which is supposed to establish a better risk assessment tool for better disease prevention. Thirdly, arterial pathological changes including carotid IMT, carotid artery plaque and arterial stenosis were observed as predictors for early changes in cardiovascular events. Fourthly, our questionnaire investigations were conducted through face-to-face interview and follow-up investigations will be conducted every year. Lastly, blood samples will be collected every year for detection. Thus, data for female characteristics, risk factors and outcomes can be closely collected and updated which will improve data quality.
Table 3. General Characteristics of Studies on Women's Health
Study Name Sample Size Age Range, years Follow-up Cohort Location Nurses' Health Study[41] 121, 700 30 to 55 1980-2019; every two years The United States Nurses' Health Study Ⅱ 116, 671 24 to 44 1989-?; every two years The United States Healthy Women Study[44] 532 Premenopausal women 1983-2008; every several years The United States Women's Health Initiative Observational Study (WHI-OS)[45] 90, 000 50 to 79 1999-2004; every two years The United States Jidong Women Health Cohort Study 4, 179 over 18 2013-2024; every year Tangshan, China There are still several limitations to this study. Firstly, this is a single-center study in Jidong Oilfield community in northern China, which could not fully represent the whole Chinese female population. Secondly, part of self-reported information like age at menarche, past menstrual cycle and former use of contraceptives or HRT would lead to recall bias. To minimize recall bias, the reliability of self-reported information could be evaluated by the comparison of baseline survey results and follow-up reports.
In conclusion, this report has described the rationale, study design and baseline characteristics of Jidong Women Health Cohort Study. This study is a large cohort study on women's health especially on associations between menopause and cardiovascular risks in China, which is expected to develop preventive measures aiming at reducing risks of CVD for the female population.
doi: 10.3967/bes2019.021
Protocol of Jidong Women Health Cohort Study: Rationale, Design, and Baseline Characteristics
-
Abstract:
Objective The Jidong Women Health Cohort Study is a prospective cohort study on female-specific characteristics and risks of chronic diseases in Chinese women and focuses on the potential association between menopause and risks of cardiovascular disease (CVD). Methods The study includes 4, 179 female participants with an age of older than 18 years from Caofeidian district, Tangshan city, northern China. Baseline information on female-specific characteristics and potential cardiovascular risk factors was collected and all the participants underwent a physical examination with blood samples collected in 2013. To establish a better risk assessment tool of female CVD, updated information from questionnaire investigation, physical examinations and occurrence of outcome events will be collected through a longitudinal follow-up annually up to the year 2024. Results At baseline, Mean age of the participants was 42.3 ±12.8 years. Reproduction occurred in 2, 948 participants (70.5%), menopausal transition in 173 (4.3%), and postmenopause in 1, 058 (25.3%). The incidence of arterial hypertension, dyslipidemia, and diabetes showed significant difference across different groups stratified by Stage of Reproductive Aging Workshop (STRAW) system (P < 0.05). Conclusion The Jidong Women Health Cohort Study will contribute to the scientific evidence on association between female-specific characteristics and cardiovascular risks, and will also be helpful to provide a new path for early detection and prevention of CVD. -
Key words:
- Cardiovascular disease /
- Menopause /
- Women /
- Protocol /
- Chinese population-based
-
Table 1. Testing Program in the Jidong Women Health Cohort Study
Test Components Gynecology Gynecologic examination, pap smear, pelvic ultrasound Specimen collection Fasting blood sample Anthropometry Height, weight, ankle-branchial index, waist and hip circumference Participant break Refreshment break with food provided Cardiovascular 12 lead ECG, vascular profiling (blood pressures, pulse wave velocity), transcranial doppler, carotid artery sonography Depression Center Epidemiological Studies Depression (CES-D) scale[30] Sleep conditions Athens Insomnia Scale (AIS)[31] Table 2. Baseline Characteristics
Characteristics Total (n, %) Reproductive Menopausal Transition Postmenopausal P-value* n 4, 179 (100) 2, 948 (70.5) 173 (4.1) 1, 058 (25.3) Age (years) 42.3 ± 12.8 35.9 ± 8.6 48.3 ± 3.6 59.1 ± 6.1 < 0.001** Ethnic group 0.102 Han 4, 055 (97.0) 2, 851 (96.7) 168 (97.1) 1, 036 (97.9) Else 124 (3.0) 97 (3.3) 5 (2.9) 22 (2.1) Marital status 0.003* Unmarried 247 (5.9) 240 (8.1) 6 (3.5) 7 (0.7) Divorced or Widowed 116 (2.8) 53 (1.8) 167 (96.5) 57 (5.4) Married 3, 816 (91.3) 2, 655 (90.1) 173 (100) 994 (94.0) Education < 0.001** Illiteracy or primary school 194 (4.6) 18 (0.6) 102 (59) 172 (16.3) Junior high school 1, 601 (38.3) 742 (25.2) 67 (38.7) 757 (71.6) College or higher 2, 384 (57.0) 2, 188 (74.2) 173 (100) 129 (12.2) Income < 0.001** ≤ ¥3, 000 1, 733 (41.5) 925 (31.4) 89 (51.4) 743 (70.2) ¥3, 001-5, 000 2, 133 (51.0) 1, 762 (59.8) 16 (9.2) 282 (26.7) > ¥5000 256 (6.1) 215 (7.3) 170 (98.3) 25 (2.4) Smoking 0.157 Never 4, 109 (98.3) 2, 909 (98.7) 166 (96.0) 1, 034 (97.7) Current 65 (1.6) 37 (1.3) 7 (4.0) 21 (2.0) Former 4 (0.1) 1 (0.0) 0 (0.0) 3 (0.3) Passive smoking 2, 758 (66.0) 1, 887 (64.0) 98 (56.6) 773 (73.1) < 0.001** Alcohol consumption 0.021* Never 3, 971 (95.0) 2, 787 (94.5) 162 (93.6) 1, 022 (96.6) Less than one standard drink 106 (2.5) 81 (2.7) 4 (2.3) 21 (2.0) Equal or more than one standard drink 102 (2.4) 80 (2.7) 7 (4.0) 15 (1.4) Tea consumption < 0.001** Never 2, 818 (67.4) 1, 910 (64.8) 104 (60.1) 804 (76.0) Less than once a week 348 (8.3) 288 (9.8) 15 (8.7) 45 (4.3) 1-3 times a week or more 1, 013 (24.2) 750 (25.4) 54 (31.2) 209 (19.8) Salt intake (g) 0.331 < 6 1, 087 (26.0) 765 (25.9) 47 (27.2) 275 (26.0) 6-12 2, 249 (53.8) 1, 550 (52.6) 91 (52.6) 608 (57.5) > 12 842 (20.1) 633 (21.5) 35 (20.2) 174 (16.4) Physical Activity < 0.001** Inactive 1, 481 (35.4) 1, 121 (38.0) 47 (27.2) 313 (29.6) Moderately active 605 (14.5) 512 (17.4) 28 (16.2) 65 (6.1) Very active 2, 093 (50.1) 1, 315 (44.6) 98 (56.6) 680 (64.3) BMI < 0.001** < 18.5 228 (5.5) 215 (7.3) 1 (0.6) 12 (1.1) 18.5-23.9 2, 233 (53.4) 1, 727 (58.6) 93 (53.8) 413 (39.0) 24-27.9 1, 082 (25.9) 622 (21.1) 48 (27.7) 412 (38.9) ≥ 28 453 (10.8) 228 (7.7) 28 (16.2) 197 (18.6) WHR 0.8 ± 0.1 0.8 ± 0.1 0.9 ± 0.1 0.9 ± 0.1 < 0.001** Female-specific characteristics Age at menarche 14.3 ± 1.8 13.9 ± 1.5 14.7 ± 1.7 15.6 ± 1.9 < 0.001** Age of menopause 49.9 ± 4.4 49.9 ± 4.4 Sexual dysfunction 99 (2.4) 43 (1.5) 10 (5.8) 46 (4.3) < 0.001** Take oral contraceptives 31 (1.4) 8 (0.8) 0 (0) 23 (2.2) 0.009 Receive HRT 12 (0.5) 1 (0.1) 0 (0) 11 (1) 0.624 Depression 255 (6.1) 188 (6.4) 14 (8.1) 53 (5.0) 0.150 Insomnia 662 (15.8) 337 (11.4) 47 (27.2) 278 (26.3) < 0.001** Arterial hypertension 429 (10.3) 130 (4.4) 19 (11.0) 280 (26.5) < 0.001** Diabetes 134 (3.2) 30 (1.0) 4 (2.3) 100 (9.5) < 0.001** TG (mmol/L) 1.3 ± 0.98 1.2 ± 0.84 1.4 ± 0.93 1.7 ± 1.19 < 0.001** TC (mmol/L) 4.4 ± 0.91 4.2 ± 0.77 4.7 ± 0.89 5.1 ± 0.95 < 0.001** LDL-C (mmol/L) 2.4 ± 0.63 2.2 ± 0.54 2.6 ± 0.64 2.8 ± 0.63 < 0.001** HDL-C (mmol/L) 1.3 ± 0.27 1.3 ±0.26 1.3 ± 0.30 1.3 ± 0.27 0.005* Note. *P < 0.05, **P < 0.001 indicates statistically significant. BMI, body mass index; WHR, waist-to-hip ratio; HRT, hormone replacement therapy; TG, triglyceride; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol. Table 3. General Characteristics of Studies on Women's Health
Study Name Sample Size Age Range, years Follow-up Cohort Location Nurses' Health Study[41] 121, 700 30 to 55 1980-2019; every two years The United States Nurses' Health Study Ⅱ 116, 671 24 to 44 1989-?; every two years The United States Healthy Women Study[44] 532 Premenopausal women 1983-2008; every several years The United States Women's Health Initiative Observational Study (WHI-OS)[45] 90, 000 50 to 79 1999-2004; every two years The United States Jidong Women Health Cohort Study 4, 179 over 18 2013-2024; every year Tangshan, China -
[1] Roth GA, Johnson C, Abajobir A, et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol, 2017; 70, 1-25. doi: 10.1016/j.jacc.2017.04.052 [2] Roth GA, Huffman MD, Moran AE, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation, 2015; 132, 1667-78. doi: 10.1161/CIRCULATIONAHA.114.008720 [3] Zhao D, Liu J. The burden of cardiovascular disease and its impact on life expectancy in China. Eur Heart J, 2014; 35, 2625-6. http://europepmc.org/abstract/med/25512993 [4] Gao F, Sun RJ, Ji Y, et al. Cardiovascular research is thriving in China. Br J Pharmacol, 2015; 172, 5430-4. doi: 10.1111/bph.12826 [5] Chan F, Adamo S, Coxson P, et al. Projected impact of urbanization on cardiovascular disease in China. Int J Public Health, 2012; 57, 849-54. doi: 10.1007/s00038-012-0400-y [6] Yang G, Kong L, Zhao W, et al. Emergence of chronic non-communicable diseases in China. Lancet, 2008; 372, 1697-705. doi: 10.1016/S0140-6736(08)61366-5 [7] Giralt D, Domingues-Montanari S, Mendioroz M, et al. The gender gap in stroke:a meta-analysis. Acta Neurol Scand, 2012; 125, 83-90. doi: 10.1111/ane.2012.125.issue-2 [8] Sharma S, Wood MJ. The Global Burden of Cardiovascular Disease in Women. Curr Treat Options Cardiovasc Med, 2018; 20, 81. doi: 10.1007/s11936-018-0676-1 [9] Daly C, Clemens F, Lopez Sendon JL, et al. Gender differences in the management and clinical outcome of stable angina. Circulation, 2006; 113, 490-8. doi: 10.1161/CIRCULATIONAHA.105.561647 [10] Vaccarino V, Parsons L, Peterson ED, et al. Sex differences in mortality after acute myocardial infarction:changes from 1994 to 2006. Arch Intern Med, 2009; 169, 1767-74. [11] O'Neil A, Scovelle AJ, Milner AJ, et al. Gender/Sex as a Social Determinant of Cardiovascular Risk. Circulation, 2018; 137, 854-64. doi: 10.1161/CIRCULATIONAHA.117.028595 [12] Stampfer MJ, Colditz GA, Willett WC, et al. Postmenopausal estrogen therapy and cardiovascular disease. Ten-year follow-up from the nurses' health study. N Engl J Med, 1991; 325, 756-62. doi: 10.1056/NEJM199109123251102 [13] Grodstein F, Stampfer MJ, Colditz GA, et al. Postmenopausal hormone therapy and mortality. N Engl J Med, 1997; 336, 1769-75. doi: 10.1056/NEJM199706193362501 [14] Grodstein F, Manson JE, Colditz GA, et al. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med, 2000; 133, 933-41. doi: 10.7326/0003-4819-133-12-200012190-00008 [15] Hsia J, Langer RD, Manson JE, et al. Conjugated equine estrogens and coronary heart disease:the Women's Health Initiative. Arch Intern Med, 2006; 166, 357-65. doi: 10.1001/archinte.166.3.357 [16] Salpeter SR, Walsh JM, Greyber E, et al. Brief report:Coronary heart disease events associated with hormone therapy in younger and older women. A meta-analysis. J Gen Intern Med, 2006; 21, 363-6. doi: 10.1111/j.1525-1497.2006.00389.x [17] Manson JE, Colditz GA, Stampfer MJ, et al. A prospective study of maturity-onset diabetes mellitus and risk of coronary heart disease and stroke in women. Arch Intern Med, 1991; 151, 1141-7. doi: 10.1001/archinte.1991.00400060077013 [18] Wilson PW, D'Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk:the Framingham experience. Arch Intern Med, 2002; 162, 1867-72. doi: 10.1001/archinte.162.16.1867 [19] Sattelmair J, Pertman J, Ding EL, et al. Dose response between physical activity and risk of coronary heart disease:a meta-analysis. Circulation, 2011; 124, 789-95. doi: 10.1161/CIRCULATIONAHA.110.010710 [20] Matthews KA, Meilahn E, Kuller LH, et al. Menopause and risk factors for coronary heart disease. N Engl J Med, 1989; 321, 641-6. doi: 10.1056/NEJM198909073211004 [21] Wenger NK. Juggling Multiple Guidelines:A Woman's Heart in the Balance. Journal of Women's Health (15409996), 2016; 25, 213-21. doi: 10.1089/jwh.2015.5467 [22] Kessous R, Shoham-Vardi I, Pariente G, et al. An association between preterm delivery and long-term maternal cardiovascular morbidity. Am J Obstet Gynecol, 2013; 209, 368. e1-8. doi: 10.1016/j.ajog.2013.05.041 [23] Vrachnis N, Augoulea A, Iliodromiti Z, et al. Previous gestational diabetes mellitus and markers of cardiovascular risk. Int J Endocrinol, 2012; 2012, 458610. http://d.old.wanfangdata.com.cn/OAPaper/oai_pubmedcentral.nih.gov_3317164 [24] Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease:epidemiology, biology, and treatment. Arch Gen Psychiatry, 1998; 55, 580-92. doi: 10.1001/archpsyc.55.7.580 [25] Garcia M, Mulvagh SL, Merz CN, et al. Cardiovascular Disease in Women:Clinical Perspectives. Circ Res, 2016; 118, 1273-93. doi: 10.1161/CIRCRESAHA.116.307547 [26] Declaration of Helsinki. Ethical principles for medical research involving human subjects. J Indian Med Assoc, 2009; 107, 403-5. http://d.old.wanfangdata.com.cn/OAPaper/oai_doaj-articles_a3ed8c7027cfbfe5fd9072adbd450d0c [27] Polak JF, Pencina MJ, Meisner A, et al. Associations of carotid artery intima-media thickness (IMT) with risk factors and prevalent cardiovascular disease:comparison of mean common carotid artery IMT with maximum internal carotid artery IMT. J Ultrasound Med, 2010; 29, 1759-68. doi: 10.7863/jum.2010.29.12.1759 [28] Naqvi TZ, Lee MS. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging, 2014; 7, 1025-38. doi: 10.1016/j.jcmg.2013.11.014 [29] Lorenz MW, Markus HS, Bots ML, et al. Prediction of clinical cardiovascular events with carotid intima-media thickness:a systematic review and meta-analysis. Circulation, 2007; 115, 459-67. doi: 10.1161/CIRCULATIONAHA.106.628875 [30] Radloff LS. The CES-D Scale:A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas, 1977; 1, 385-401. doi: 10.1177/014662167700100306 [31] Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale:validation of an instrument based on ICD-10 criteria. J Psychosom Res, 2000; 48, 555-60. doi: 10.1016/S0022-3999(00)00095-7 [32] Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire:12-country reliability and validity. Med Sci Sports Exerc, 2003; 35, 1381-95. doi: 10.1249/01.MSS.0000078924.61453.FB [33] McCabe MP, Sharlip ID, Atalla E, et al. Definitions of Sexual Dysfunctions in Women and Men:A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. J Sex Med, 2016; 13, 135-43. doi: 10.1016/j.jsxm.2015.12.019 [34] Nelson HD. Menopause. Lancet, 2008; 371, 760-70. doi: 10.1016/S0140-6736(08)60346-3 [35] Harlow SD, Gass M, Hall JE, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10:addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab, 2012; 97, 1159-68. doi: 10.1210/jc.2011-3362 [36] Wang Y, Ge S, Yan Y, et al. China suboptimal health cohort study:rationale, design and baseline characteristics. J Transl Med, 2016; 14, 291. doi: 10.1186/s12967-016-1046-y [37] Chu J, Gao R, Zhao S, et al. Guidelines for the prevention and treatment of dyslipidemia in Chinese adults (2016 Revision). Chinese Circulation J, 2016; 31, 937-53. (In Chinese) [38] Grant EG, Benson CB, Moneta GL, et al. Carotid artery stenosis:gray-scale and Doppler US diagnosis——Society of Radiologists in Ultrasound Consensus Conference. Radiology, 2003; 229, 340-6. doi: 10.1148/radiol.2292030516 [39] Daniels LB, Maisel AS. Cardiovascular biomarkers and sex:the case for women. Nat Rev Cardiol, 2015; 12, 588-96. doi: 10.1038/nrcardio.2015.105 [40] Shah AS, Griffiths M, Lee KK, et al. High sensitivity cardiac troponin and the under-diagnosis of myocardial infarction in women:prospective cohort study. BMJ, 2015; 350, g7873. http://pubmedcentralcanada.ca/pmcc/articles/PMC4301191/ [41] Belanger CF, Hennekens CH, Rosner B, et al. The nurses' health study. Am J Nurs, 1978; 78, 1039-40. http://d.old.wanfangdata.com.cn/OAPaper/oai_doaj-articles_90ce0bdde3ba0c9cad67f79fc899f50a [42] Colditz GA, Willett WC, Stampfer MJ, et al. Menopause and the risk of coronary heart disease in women. N Engl J Med, 1987; 316, 1105-10. doi: 10.1056/NEJM198704303161801 [43] LaMonte MJ, Hovey KM, Millen AE, et al. Accuracy of self-reported periodontal disease in the Women's Health Initiative Observational Study. J Periodontol, 2014; 85, 1006-18. doi: 10.1902/jop.2013.130488 [44] Kuller LH, Matthews KA, Sutton-Tyrrell K, et al. Coronary and aortic calcification among women 8 years after menopause and their premenopausal risk factors:the healthy women study. Arterioscler Thromb Vasc Biol, 1999; 19, 2189-98. doi: 10.1161/01.ATV.19.9.2189 [45] Trabert B, Brinton LA, Anderson GL, et al. Circulating Estrogens and Postmenopausal Ovarian Cancer Risk in the Women's Health Initiative Observational Study. Cancer Epidemiol Biomarkers Prev, 2016; 25, 648-56. doi: 10.1158/1055-9965.EPI-15-1272-T -





 下载:
下载:




 Quick Links
Quick Links