-
With the coronavirus disease 2019 (COVID-19) pandemic ongoing worldwide, there has been the emergence of new variants [1-3]. A previous study demonstrated that most COVID-19 patients have favorable outcomes [4]. However, after recovery from COVID-19, long-term consequences (i.e., smell and taste disorder, hair loss, fatigue, dyspepsia, anxiety, and depression) have been reported, which could affect the quality of life of patients, the healthcare system, and the economy, and have become an increasing concern globally [5-6]. Moreover, we know very little about the long-term follow-up of COVID-19 individuals with comorbidities, such as pulmonary tuberculosis (PTB), after recovery.
Tuberculosis (TB) is a serious public health problem and social issue worldwide. As COVID-19 and TB are top ongoing health crises globally, coinfection is not rare worldwide. According to a meta-analysis that included 114 studies from 38 countries, the prevalence of comorbid TB among COVID-19 patients was 1.6%, and different studies varied greatly across (0.4%–9.0%) [7]. Some researchers have observed that TB could increase the risk of severe COVID-19 and death. Studies have shown that COVID-19 could reactivate or worsen TB [8-10]. The main manifestation of TB is PTB, which is a respiratory infectious disease caused by Mycobacterium TB. A meta-analysis showed that active PTB was 1.07% among COVID-19 [11]. Although these studies have been conducted to present epidemiological features, clinical characteristics, and treatment outcomes of COVID-19 with PTB coinfection, we know very little about follow-up, including long-term sequela and recurrence after discharge in recovered COVID-19 with PTB survivors, which is urgently needed to understand the long-term follow-up after discharge among the coinfections in this field. Therefore, we conducted a prospective, multicenter study to explore clinical outcomes, including sequela and recurrence of COVID-19 with TB survivors after discharge. The findings may provide a reference for developing prevention and treatment policies for COVID-19 with TB.
-
A prospective, multicenter follow-up study was conducted from 13 hospitals in four provinces of China (Sichuan, Hebei, Shanxi, and Heilongjiang) from January 22, 2020, to May 6, 2022. As of August 26, 2022, all COVID-19 with PTB subjects were laboratory confirmed. The inclusion criteria for COVID-19 with PTB patients were as follows: 1) laboratory-confirmed COVID-19 cases and 2) a history of PTB. Patients who declined to participate were excluded.
-
COVID-19 The Diagnosis and Treatment Protocol for COVID-19 in China was used to determine COVID-19 severity: 1) for mild cases, the clinical symptoms were minimal, and there was no sign of pneumonia CT image; 2) for moderate cases, the patients only had a fever and respiratory symptoms with radiological findings of pneumonia on the CT image; 3) severe cases were defined as having any of the following respiratory distress, needing invasive ventilation, pulse oxygen saturation ≤ 93%, or arterial partial pressure of oxygen/oxygen concentration ≤ 300 mmHg.
Asymptomatic infections refer to the positive detection of nucleic acids of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in patient samples by reverse transcriptase-polymerase chain reaction (RT-PCR) but with no typical clinical symptoms or signs [12].
PTB PTB is defined as TB lesions in the lung tissue, trachea, bronchi, and pleura, according to the Diagnosis for Pulmonary Tuberculosis [13]. In this study, PTB was divided into active and non-active PTB.
Treatment outcomes were categorized according to the China Tuberculosis Program Implementation Guide [14]. Cure was defined as patients who completed treatment and at least had their final two sputum smear cultures proved negative. Treatment completed was defined as patients who completed their therapy without evidence of treatment failure but with no record of sputum smear results in the last month of treatment. Treatment failure was defined as positive sputum smear culture results at the fifth month of treatment or at the time the treatment had already been completed. Died was defined as a patient who died from any cause during the treatment. Lost to follow-up was defined as a patient whose treatment was interrupted for more than two consecutive months without clinicians’ permission.
-
In this study, follow-up consultations were conducted by trained medical staff with a uniformly designed questionnaire in every hospital. Methods of follow-up included face-to-face interviews and telephone calls. If participants could not come to the hospital for an interview due to COVID-19, follow-up consultations were conducted via telephone instead of face-to-face interviews. Every participant was asked to complete a questionnaire including results of PCR retests, recurrence of PTB, and self-reported symptoms (i.e., smell and taste disorder, anxiety or depression, sleep difficulties, and hair loss) at 3, 12, and 24 months after discharge. If the trained staff could not reach the participants at the time of the appointment, the interview will be rescheduled.
In this study, recurrence of COVID-19 referred to survivors who tested re-positive for SARS-CoV-2 by real-time reverse transcription PCR assays in the upper respiratory tract (nasal and pharyngeal) specimens collected after discharge.
Recurrence of PTB referred to a patient previously having clear TB history who has been declared cured after completing a treatment course and is now diagnosed with both sputum smear and culture positive and/or active lesions on chest image.
-
Categorical variables were expressed as percentages (%), and continuous variables were presented as median (interquartile range) and standard deviation. All data analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA). The detailed course after discharge was drawn using the Python Matplotlib package 3.8.3 (Python Software Foundation, Delaware, USA).
-
This study was approved by the Institutional Review Board of the Institute of Basic Research in Clinical Medicine, China Academy of Chinese Medical Sciences (No. P20009/PJ09).
-
Thirty-five patients with COVID-19 were discharged from 13 hospitals from January 22, 2020 to May 6, 2022. Three cases were excluded. Among them, one case declined to attend the follow-up, one case could not be reached during the follow-up, and one case died 2 months after discharge due to cardiovascular, renal failure, electrolyte disturbance, and so forth. The patient was an 81-year-old man with a 60-year history of PTB, 20 years of hypertension, and 50 years of smoking. The patient was a critical COVID-19 case on admission.
In this study, 32 cases were enrolled in the analysis. The median (P25, P75) age was 51.5 (44.5, 62.5) years, and 23 (71.9%) were men. Apart from PTB, more than half [19 (59.4%)] had at least one comorbidity, mainly including hypertension [4 (12.5%)], fatty liver [3 (9.4%)], diabetes [2 (6.3%)], and coronary heart disease [2 (6.3%)]. The most common symptoms were fever [14 (43.8%)], cough [13 (40.6%)], followed by fatigue [8 (25.0%)], sore throat [4 (12.5%)], and asthma [4 (12.5%)]. Additionally, 22 (68.8%) survivors showed abnormal changes in their lung lesions on admission. Demographics and clinical characteristics are shown in Table 1.
Table 1. Characteristics of 32 COVID-19 with PTB patients
Characteristics Total
(n = 32)Non-severe
(n = 22)Severe
(n = 3)Asymptomatic
(n = 7)Age, years [M (P25, P75)] 51.5 (44.5, 62.5) 50.5 (43.2, 59.5) 72 (47.0, 72.0) 52.0 (39.0, 57.0) Gender, n (%) Male 23 (71.9) 15 (68.2) 3 (100.0) 5 (71.4) Female 9 (28.1) 7 (31.8) 0 (0) 2 (28.6) History of close contact with
confirmed COVID-19, n (%)20 (62.5) 15 (68.2) 2 (66.7) 3 (42.9) Comorbidities, n (%) Any 19 (59.4) 12 (54.5) 2 (66.7) 5 (71.4) Hypertension 4 (12.5) 1 (4.5) 2 (66.7) 1 (14.3) Diabetes 2 (6.3) 0 (0) 1 (33.3) 1 (14.3) Coronary heart disease 2 (6.3) 2 (9.0) 0 (0) 0 (0) Fatty liver 3 (9.4) 3 (13.6) 0 (0) 0 (0) Other 12 (37.5) 7 (31.8) 2 (66.7) 3 (42.9) Classification of PTB Active 1 (3.1) 1 (4.5) 0 (0) 0 (0) Non-active 31 (96.9) 21 (95.5) 3 (100.0) 7 (100.0) Symptoms in hospital, n (%) Fever 14 (43.8) 12 (54.5) 2 (66.7) 0 (0) Cough 13 (40.6) 10 (45.5) 3 (75.0) 0 (0) Expectoration 3 (9.4) 1 (4.5) 2 (66.7) 0 (0) Fatigue 8 (25.0) 5 (22.7) 3 (75.0) 0 (0) Anorexia 2 (6.3) 1 (4.5) 1 (33.3) 0 (0) Sore throat 4 (12.5) 4 (18.2) 0 (0) 0 (0) Nasal congestion 2 (6.3) 1 (4.5) 0 (0) 0 (0) Rhinorrhea 1 (3.1) 0 (0) 1 (33.3) 0 (0) Asthma 4 (12.5) 2 (9.0) 2 (66.7) 0 (0) Diarrhea 3 (9.4) 2 (9.0) 1 (33.3) 0 (0) CT findings, n (%) No abnormal lesions 10 (31.3) 3 (13.6) 0 (0) 7 (100.0) Unilateral lung injury 8 (25.0) 8 (36.4) 0 (0) 0 (0) Bilateral lung injury 14 (43.87) 11 (50.0) 3 (100.0) 0 (0) Treatment, n (%) Antiviral 24 (75.0) 17 (77.3) 3 (100.0) 4 (57.1) Antibiotic 11 (34.4) 8 (36.4) 3 (100.0) 0 (0) Glucocorticoids 3 (9.4) 1 (4.5) 2 (66.7) 0 (0) TCM 26 (81.3) 18 (81.8) 2 (66.7) 6 (85.7) Symptomatic treatment 19 (59.4) 13 (59.1) 2 (66.7) 4 (57.1) Outcomes, days [M (P25, P75)] Length of first viral shedding 10.0 (7.3, 13.0) 9.5 (6.7, 13.7) 15.0 (13.0, 15.0) 8.0 (2.0, 11.0) Length of hospital stay 14.5 (10.0, 21.0) 12.0 (9.7, 21.5) 20.0 (18.0, 20.0) 14.0 (11.0, 15.0) -
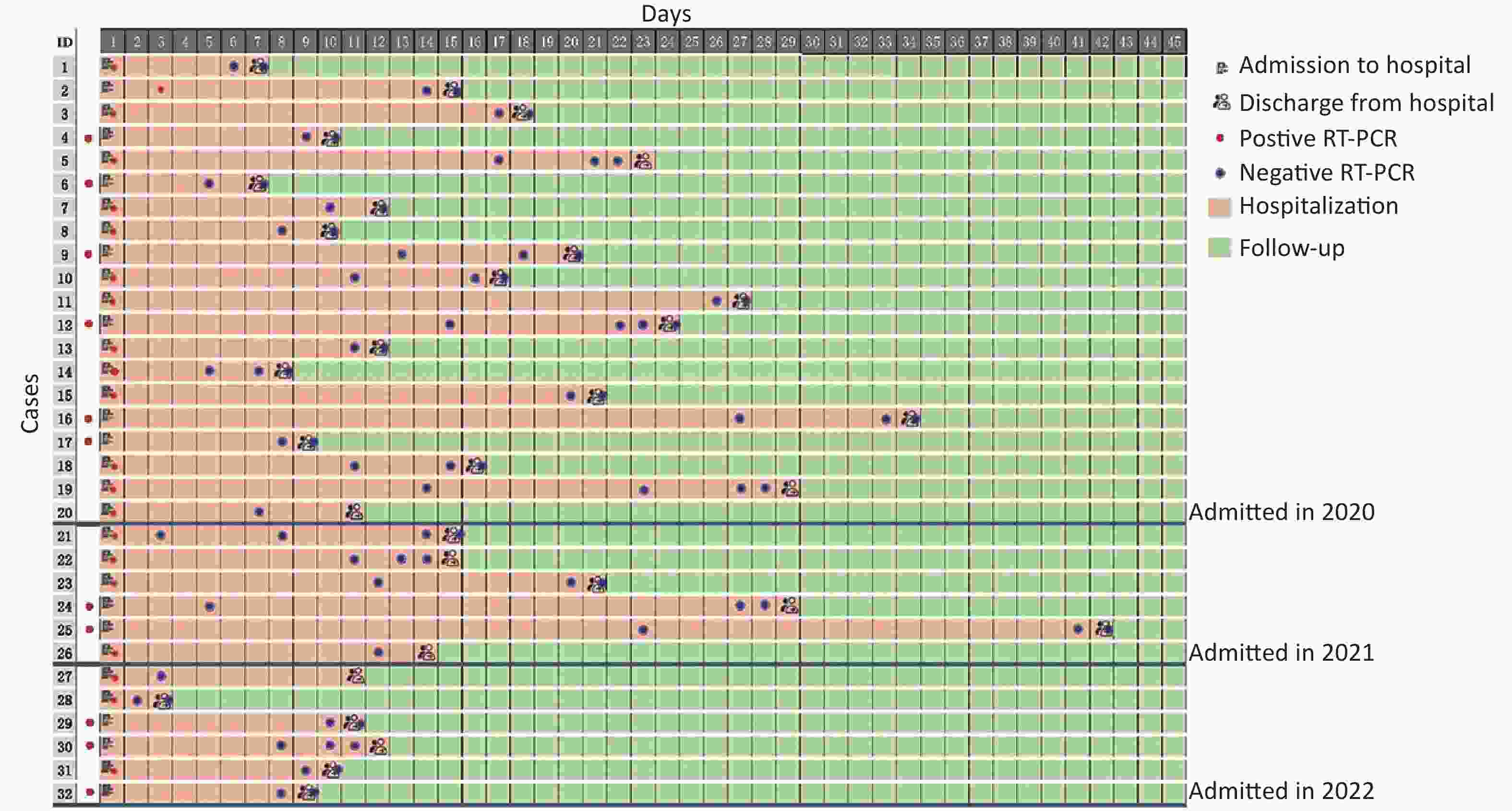
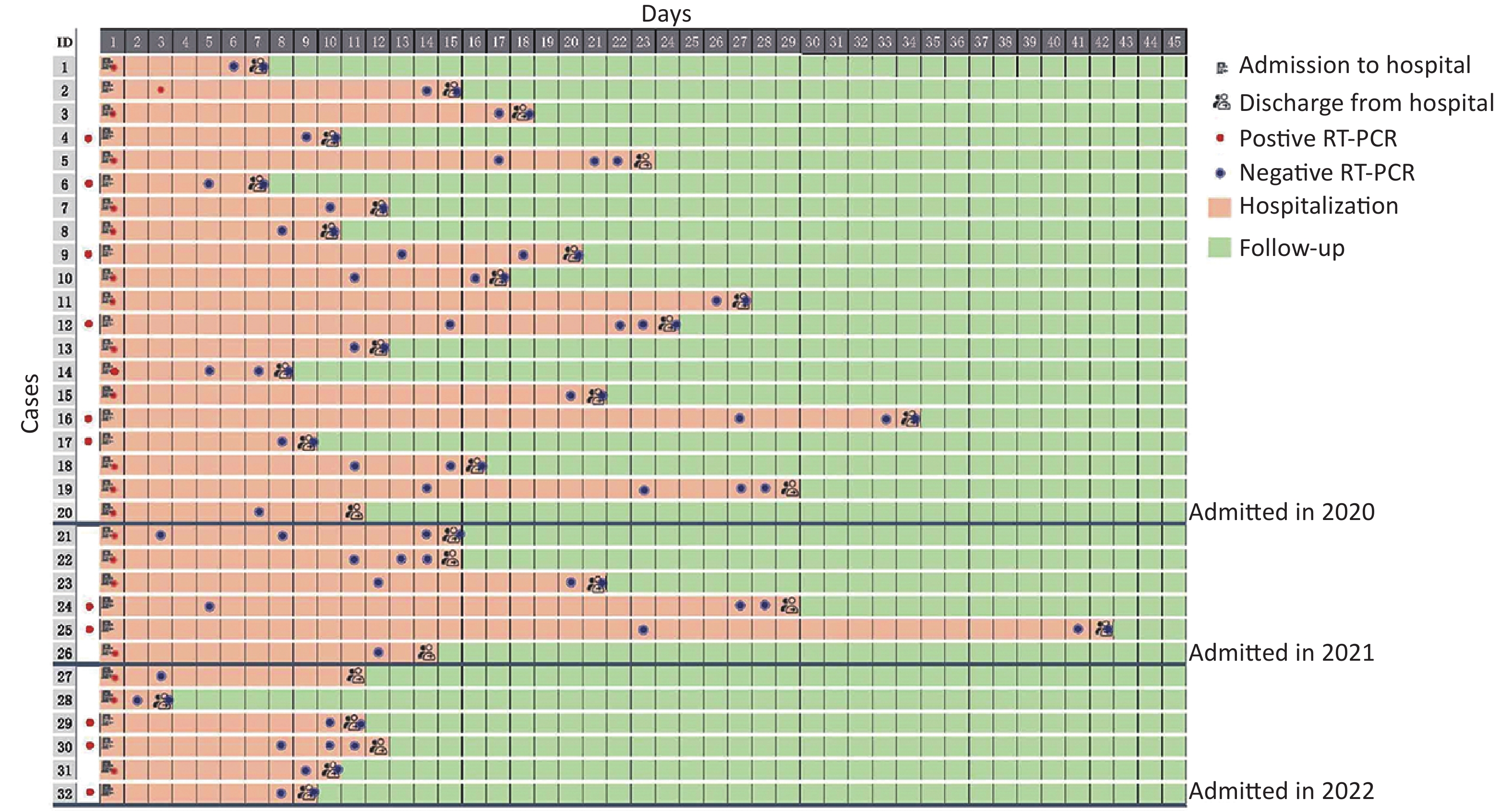
All patients received traditional Chinese medicine (TCM) or/and western medicine (WM). TCM mainly included Qingfei Paidu Decoction (QFPDD) [15 (46.9%)], Lianhua Qingwen Granule [8 (25.0%)], and Yinlian Qingwen oral liquid [6 (18.8%)]. WM mainly included antiviral treatment (Alpha interferon-α, Ribavirin, Arbidol, Oseltamivir, etc.), antibiotics (Moxifloxacin, Ofloxacin, etc.), and supportive treatments, such as oxygen therapy. Moreover, one patient was diagnosed with active PTB after COVID-19. The patient received anti-PTB treatments in addition to the treatment for COVID-19 (Table 1). No serious adverse events were observed in the patients during hospitalization. The median duration of the first viral shedding and hospitalization was 10.0 (7.3, 13.0) and 14.5 (10.0, 21.0) days, respectively. The detailed course of the 32 cases is shown in Figure 1.
-
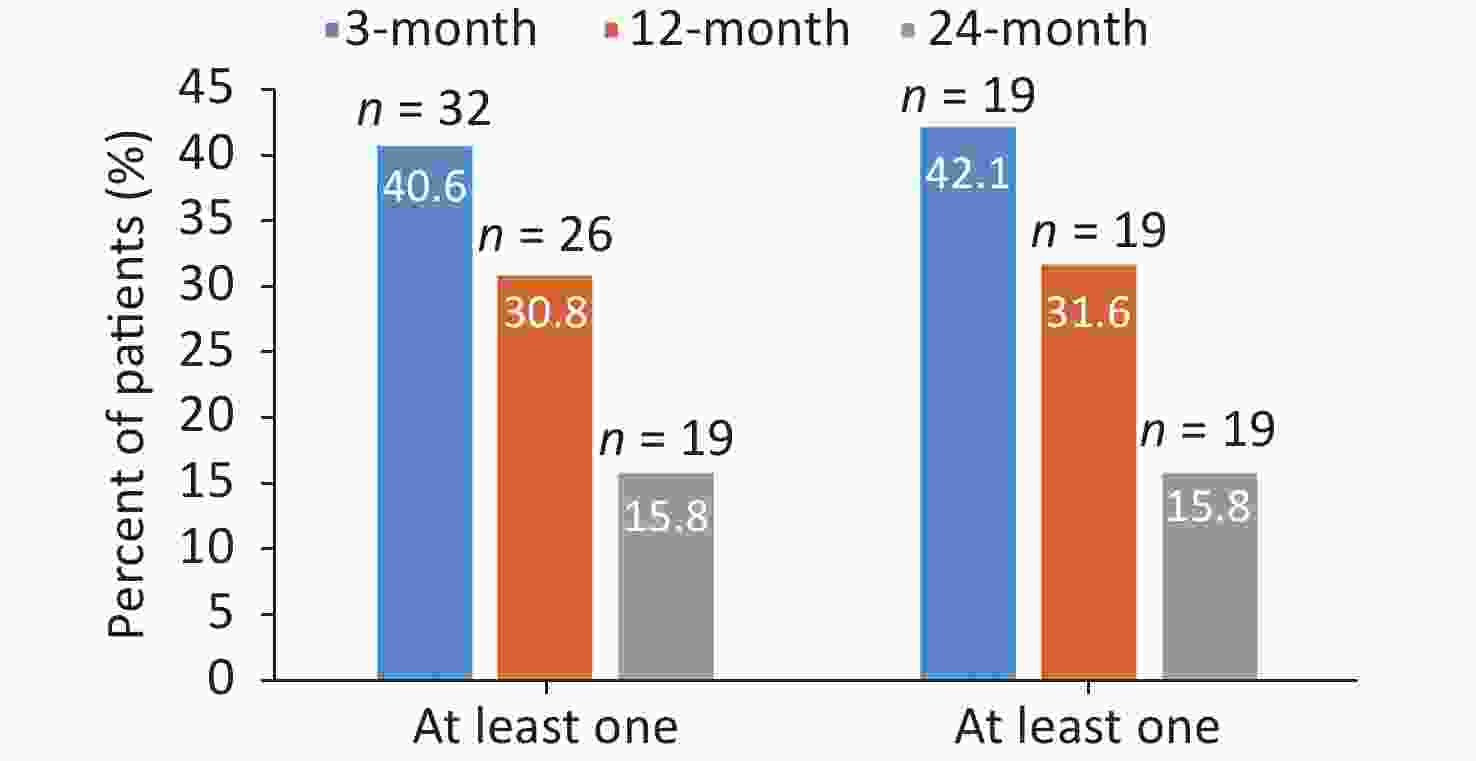
Among 32 patients discharged, not all patients met the interval of 24 months from discharge to follow-up based on the long enrollment period (from January 22, 2020 to May 6, 2022). As of August 26, 2022, 32 patients had completed 3-month follow-ups, while 26 and 19 had completed 12- and 24-month follow-ups, respectively. The proportion of COVID-19 survivors with at least one sequela symptom decreased significantly from 13 (40.6%) of 32 at 3 months to 8 (30.8%) of 26 at 12 months to 3 (15.8%) of 19 at 24 months, with fatigue and anxiety always being the most frequent. Among these, chromatosis disappeared after a 3-month follow-up; cough and amnesia recovered after a 12-month follow-up, but fatigue, anxiety, and trouble sleeping remained after 24 months. Additionally, one (3.1%) had two recurrences of PTB and no COVID-19 re-positive during the follow-up period. Notably, a similar downward trend in sequela was observed among 19 patients who completed three follow-up visits, as shown in Table 2 and Figures 2–3.
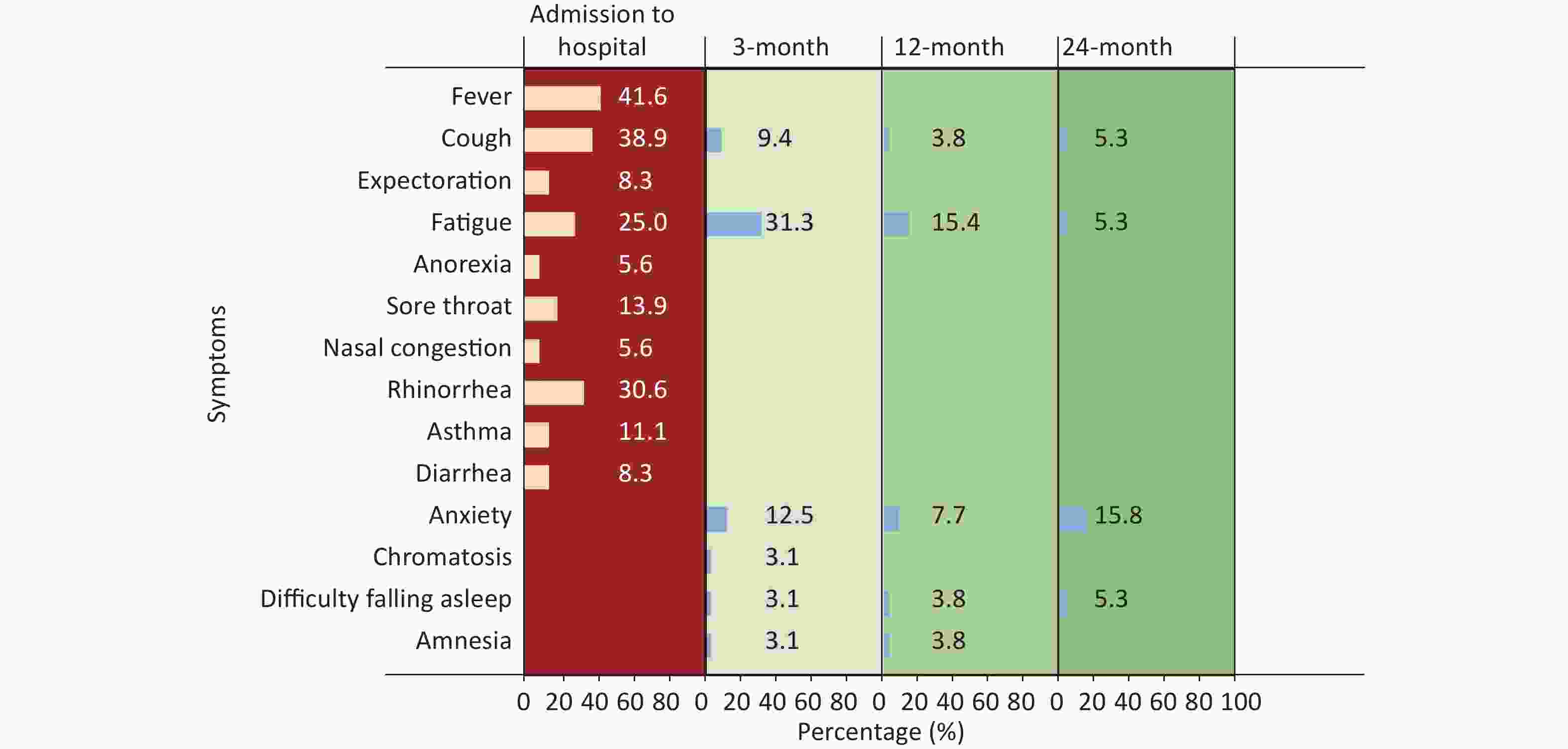
Figure 2. Proportion of clinical symptoms at admission and persistent symptoms at different appointments after discharge.
Table 2-a. The proportion of persistent symptoms in COVID-19 with PTB cases at different appointment after discharge
Characteristics 3-month (n = 32) 12-month (n = 26) 24-month (n = 19) Fatigue, n (%) 10 (31.3) 4 (15.4) 1 (5.3) Anxiety, n (%) 4 (12.5) 2 (7.7) 3 (15.8) Cough, n (%) 3 (9.4) 1 (3.8) 0 (0) Chromatosis, n (%) 1 (3.1) 0 (0) 0 (0) Amnesia, n (%) 1 (3.1) 1 (3.8) 0 (0) Difficulty falling asleep, n (%) 1 (3.1) 1 (3.8) 1 (5.3) Re-positive of COVID-19, n (%) 0 (0) 0 (0) 0 (0) Recurrence of PTB, n (%) 0 (0) 1 (3.8) 1 (5.3) -
To the best of our knowledge, this is the first prospective, multicenter follow-up study among COVID-19 with PTB survivors. This study found that the proportion of sequelae, such as fatigue and cough, decreased with the extension of follow-up time and was as low as 15.8% at 24 months; however, anxiety had a higher proportion (15.8%) among survivors. We also observed no positive results in PCR retests, but one patient had two recurrences, that is, positive sputum culture for Mycobacterium TB.
Growing evidence has shown that COVID-19 survivors may experience long-term sequela and affect different organ systems and quality of life [4,15-19]. A systematic review reported that 80% of COVID-19 patients had long-term symptoms following acute infection [20]. A study from Italy observed that 40.5% of patients reported at least one symptom at a 12-month follow-up [21]. Literature published in China reported that the proportion of patients with at least one sequela symptom was 68% and 49% at 6 and 12 months, respectively [22]. Yang et al. reported that 19.8% of survivors had symptoms at 2 years after discharge [23]. However, the persistence of symptoms among COVID-19 with PTB cases after discharge was still unclear. The results showed that the proportion of patients with at least one sequela symptom was 40.6%, 30.8%, and 15.8% at 3, 12, and 24 months after discharge, which were lower than the above studies. Moreover, we also found that the proportion of one sequela symptom decreased over follow-up, while anxiety was the most common sequela symptom. The results conformed to other studies [5,21], suggesting that the long-term impact of COVID-19 could not be ignored, and more attention should be paid to psychological counseling and humanistic care.
Retested positive COVID-19 patients after discharge are the main cause of re-hospitalization and the potential cause of the outbreak. A narrative review demonstrated that the proportion of re-positive tests in discharged COVID-19 patients varied from 2.4% to 69.2% and persisted from 1 to 38 days after discharge [24]. A meta-analysis including 3,644 patients from 41 studies reported that the proportion of re-positive cases was 14% from China and 31% from Korea. Notably, 39% of subjects among re-positive cases had at least one comorbidity [25]. However, the proportion of positive retested among COVID-19 with PTB has not been reported. In this study, no re-positive cases during the 24-month follow-up and showed a favorable outcome. The exact causes and mechanisms of positive retests for SARS-CoV-2 RNA in COVID-19 with PTB cases remain unclear. Therefore, further studies should be conducted to confirm the findings.
The recurrence of TB continues to be a significant problem and remains a challenge for the global control of TB. A previous study reported that the rate of recurrence ranged from 4.9% to 47% [26]. Additionally, a study from South Africa demonstrated a 14% of recurrence rate with a 5-year follow-up [27], and a study from China observed 3.9% and 5.4% at 2- and 5-year follow-ups, respectively [28]. In this study, one (3.12%) case of a 73-year-old COVID-19 with PTB survivor had two recurrences after being cured at 12 and 24 months, respectively. Many factors, including gender, age, inadequate treatment, viral infections, and diabetes, were associated with PTB recurrence [29-32]. COVID-19 with PTB coinfection caused excessive inflammation in the lungs, and a highly inflammatory environment can accelerate the progression of TB [33]. A recent study showed that COVID-19 might lead to recurrence in PTB patients [34]. Meanwhile, glucocorticoids and immunosuppressants used to treat COVID-19 may also promote PTB recurrence by compromising T-cell immunity and weakening immune responses [35-36]. However, whether COVID-19 reactivates or exacerbates active PTB remains unclear and needs to be confirmed by further studies.
-
There are several notable strengths in this study. To the best of our knowledge, this is the first study to investigate the clinical outcome, including the persistence of symptoms and recurrence among COVID-19 with PTB survivors at 24-month follow-up after discharge. Moreover, this study is a multicenter study. The results showed favorable clinical outcomes as the proportion of sequela decreased with the extension of the follow-up period, while anxiety had a higher proportion among the persistence of symptoms. Notably, this study further observed that no retested positive PCR while recurrence of PTB during follow-up. The findings should be confirmed through further studies. Despite the strengths of this study, there are also a number of limitations. First, this study is a small sample size study. Second, no parallel control group was analyzed in this study. Further studies with large samples and multicenter need to be conducted to confirm the findings.
-
Table 2-b. The proportion of persistent symptoms in 19 COVID-19 with PTB cases at different appointment after discharge
Characteristics 3-month (n = 19) 12-month (n = 19) 24-month (n = 19) Fatigue, n (%) 7 (36.8) 3 (15.8) 1 (5.3) Anxiety, n (%) 4 (21.1) 2 (10.5) 3 (15.8) Cough, n (%) 1 (5.3) 0 (0) 0 (0) Chromatosis, n (%) 0 (0) 0 (0) 0 (0) Amnesia, n (%) 0 (0) 0 (0) 0 (0) Difficulty falling asleep, n (%) 1 (5.3) 2 (10.5) 1 (5.3) Re-positive of COVID-19, n (%) 0 (0) 0 (0) 0 (0) Recurrence of PTB, n (%) 0 (0) 1 (5.3) 1 (5.3)
doi: 10.3967/bes2022.126
3- to 24-month Follow-up on COVID-19 with Pulmonary Tuberculosis Survivors after Discharge: Results from a Prospective, Multicenter Study
-
Abstract:
Objective Coronavirus disease 2019 (COVID-19) and tuberculosis (TB) are major public health and social issues worldwide. The long-term follow-up of COVID-19 with pulmonary TB (PTB) survivors after discharge is unclear. This study aimed to comprehensively describe clinical outcomes, including sequela and recurrence at 3, 12, and 24 months after discharge, among COVID-19 with PTB survivors. Methods From January 22, 2020 to May 6, 2022, with a follow-up by August 26, 2022, a prospective, multicenter follow-up study was conducted on COVID-19 with PTB survivors after discharge in 13 hospitals from four provinces in China. Clinical outcomes, including sequela, recurrence of COVID-19, and PTB survivors, were collected via telephone and face-to-face interviews at 3, 12, and 24 months after discharge. Results Thirty-two COVID-19 with PTB survivors were included. The median age was 52 (45, 59) years, and 23 (71.9%) were men. Among them, nearly two-thirds (62.5%) of the survivors were moderate, three (9.4%) were severe, and more than half (59.4%) had at least one comorbidity (PTB excluded). The proportion of COVID-19 survivors with at least one sequela symptom decreased from 40.6% at 3 months to 15.8% at 24 months, with anxiety having a higher proportion over a follow-up. Cough and amnesia recovered at the 12-month follow-up, while anxiety, fatigue, and trouble sleeping remained after 24 months. Additionally, one (3.1%) case presented two recurrences of PTB and no re-positive COVID-19 during the follow-up period. Conclusion The proportion of long symptoms in COVID-19 with PTB survivors decreased over time, while nearly one in six still experience persistent symptoms with a higher proportion of anxiety. The recurrence of PTB and the psychological support of COVID-19 with PTB after discharge require more attention. -
Key words:
- COVID-19 /
- Pulmonary tuberculosis /
- Long-term /
- Sequela /
- Recurrence /
- Re-positive
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
&These authors contributed equally to this work.
注释:1) AUTHOR CONTRIBUTIONS: 2) CONFLICTS OF INTEREST: -
Figure 3. Proportion of at least one persistent symptom at 3, 12, and 24 months after discharge.
Among 32 COVID-19 with PTB survivors, 19 cases were discharged before August 26, 2020, and completed follow-up of 24 months after discharge; 26 cases, including 19 cases discharged in 2020, were discharged before August 26, 2021, and these cases completed 12- or 24-month follow-up; 32 cases including 26 cases discharged in 2020–2021 were discharged before August 26, 2022, and these cases completed 3-, 12-, or 24-month follow-up.
Table 1. Characteristics of 32 COVID-19 with PTB patients
Characteristics Total
(n = 32)Non-severe
(n = 22)Severe
(n = 3)Asymptomatic
(n = 7)Age, years [M (P25, P75)] 51.5 (44.5, 62.5) 50.5 (43.2, 59.5) 72 (47.0, 72.0) 52.0 (39.0, 57.0) Gender, n (%) Male 23 (71.9) 15 (68.2) 3 (100.0) 5 (71.4) Female 9 (28.1) 7 (31.8) 0 (0) 2 (28.6) History of close contact with
confirmed COVID-19, n (%)20 (62.5) 15 (68.2) 2 (66.7) 3 (42.9) Comorbidities, n (%) Any 19 (59.4) 12 (54.5) 2 (66.7) 5 (71.4) Hypertension 4 (12.5) 1 (4.5) 2 (66.7) 1 (14.3) Diabetes 2 (6.3) 0 (0) 1 (33.3) 1 (14.3) Coronary heart disease 2 (6.3) 2 (9.0) 0 (0) 0 (0) Fatty liver 3 (9.4) 3 (13.6) 0 (0) 0 (0) Other 12 (37.5) 7 (31.8) 2 (66.7) 3 (42.9) Classification of PTB Active 1 (3.1) 1 (4.5) 0 (0) 0 (0) Non-active 31 (96.9) 21 (95.5) 3 (100.0) 7 (100.0) Symptoms in hospital, n (%) Fever 14 (43.8) 12 (54.5) 2 (66.7) 0 (0) Cough 13 (40.6) 10 (45.5) 3 (75.0) 0 (0) Expectoration 3 (9.4) 1 (4.5) 2 (66.7) 0 (0) Fatigue 8 (25.0) 5 (22.7) 3 (75.0) 0 (0) Anorexia 2 (6.3) 1 (4.5) 1 (33.3) 0 (0) Sore throat 4 (12.5) 4 (18.2) 0 (0) 0 (0) Nasal congestion 2 (6.3) 1 (4.5) 0 (0) 0 (0) Rhinorrhea 1 (3.1) 0 (0) 1 (33.3) 0 (0) Asthma 4 (12.5) 2 (9.0) 2 (66.7) 0 (0) Diarrhea 3 (9.4) 2 (9.0) 1 (33.3) 0 (0) CT findings, n (%) No abnormal lesions 10 (31.3) 3 (13.6) 0 (0) 7 (100.0) Unilateral lung injury 8 (25.0) 8 (36.4) 0 (0) 0 (0) Bilateral lung injury 14 (43.87) 11 (50.0) 3 (100.0) 0 (0) Treatment, n (%) Antiviral 24 (75.0) 17 (77.3) 3 (100.0) 4 (57.1) Antibiotic 11 (34.4) 8 (36.4) 3 (100.0) 0 (0) Glucocorticoids 3 (9.4) 1 (4.5) 2 (66.7) 0 (0) TCM 26 (81.3) 18 (81.8) 2 (66.7) 6 (85.7) Symptomatic treatment 19 (59.4) 13 (59.1) 2 (66.7) 4 (57.1) Outcomes, days [M (P25, P75)] Length of first viral shedding 10.0 (7.3, 13.0) 9.5 (6.7, 13.7) 15.0 (13.0, 15.0) 8.0 (2.0, 11.0) Length of hospital stay 14.5 (10.0, 21.0) 12.0 (9.7, 21.5) 20.0 (18.0, 20.0) 14.0 (11.0, 15.0) Table 2-a. The proportion of persistent symptoms in COVID-19 with PTB cases at different appointment after discharge
Characteristics 3-month (n = 32) 12-month (n = 26) 24-month (n = 19) Fatigue, n (%) 10 (31.3) 4 (15.4) 1 (5.3) Anxiety, n (%) 4 (12.5) 2 (7.7) 3 (15.8) Cough, n (%) 3 (9.4) 1 (3.8) 0 (0) Chromatosis, n (%) 1 (3.1) 0 (0) 0 (0) Amnesia, n (%) 1 (3.1) 1 (3.8) 0 (0) Difficulty falling asleep, n (%) 1 (3.1) 1 (3.8) 1 (5.3) Re-positive of COVID-19, n (%) 0 (0) 0 (0) 0 (0) Recurrence of PTB, n (%) 0 (0) 1 (3.8) 1 (5.3) 2-b. The proportion of persistent symptoms in 19 COVID-19 with PTB cases at different appointment after discharge
Characteristics 3-month (n = 19) 12-month (n = 19) 24-month (n = 19) Fatigue, n (%) 7 (36.8) 3 (15.8) 1 (5.3) Anxiety, n (%) 4 (21.1) 2 (10.5) 3 (15.8) Cough, n (%) 1 (5.3) 0 (0) 0 (0) Chromatosis, n (%) 0 (0) 0 (0) 0 (0) Amnesia, n (%) 0 (0) 0 (0) 0 (0) Difficulty falling asleep, n (%) 1 (5.3) 2 (10.5) 1 (5.3) Re-positive of COVID-19, n (%) 0 (0) 0 (0) 0 (0) Recurrence of PTB, n (%) 0 (0) 1 (5.3) 1 (5.3) -
[1] Zhao Y, Sun DL, Bouchard HC, et al. Coronavirus disease 2019 versus influenza a in children: an observational control study in China. Biomed Environ Sci, 2020; 33, 614−9. [2] Wang N, Yang MB, Yang PY, et al. A case series of olfactory dysfunction in imported COVID-19 patients: a 12-month follow-up study. Biomed Environ Sci, 2022; 35, 402−11. [3] Ma Y, Mishra SR, Han XK, et al. The relationship between time to a high COVID-19 response level and timing of peak daily incidence: an analysis of governments' Stringency Index from 148 countries. Infect Dis Poverty, 2021; 10, 96. doi: 10.1186/s40249-021-00880-x [4] The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Wkly, 2020; 2, 113−22. doi: 10.46234/ccdcw2020.032 [5] Zeng N, Zhao YM, Yan W, et al. A systematic review and meta-analysis of long term physical and mental sequelae of COVID-19 pandemic: call for research priority and action. Mol Psychiatry, 2022. [6] Han Q, Zheng B, Daines L, et al. Long-term sequelae of COVID-19: a systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms. Pathogens, 2022; 11, 269. doi: 10.3390/pathogens11020269 [7] Wang YD, Xu J, Wang Y, et al. Prevalence of comorbid tuberculosis amongst COVID-19 patients: a rapid review and meta-analysis. Int J Clin Pract, 2021; 75, e14867. [8] Gao Y, Liu M, Chen YM, et al. Association between tuberculosis and COVID-19 severity and mortality: a rapid systematic review and meta-analysis. J Med Virol, 2021; 93, 194−6. doi: 10.1002/jmv.26311 [9] Tadolini M, García-García JM, Blanc FX, et al. On tuberculosis and COVID-19 co-infection. Eur Respir J, 2020; 56, 2002328. doi: 10.1183/13993003.02328-2020 [10] Visca D, Ong CWM, Tiberi S, et al. Tuberculosis and COVID-19 interaction: a review of biological, clinical and public health effects. Pulmonology, 2021; 27, 151−65. doi: 10.1016/j.pulmoe.2020.12.012 [11] Aggarwal AN, Agarwal R, Dhooria S, et al. Active pulmonary tuberculosis and coronavirus disease 2019: a systematic review and meta-analysis. PLoS One, 2021; 16, e0259006. doi: 10.1371/journal.pone.0259006 [12] The Central People’s Government of the People's Republic of China. Notice of the state council’s joint prevention and control mechanism for novel coronavirus infected pneumonia on printing and distributing the regulations on the management of asymptomatic infections of the novel coronavirus. http://www.gov.cn/zhengce/content/2020-04/08/content_5500371.htm?trs=1. [2022-08-05]. (In Chinese) [13] National Health and Family Planning Commission of the P.R.C. Diagnosis for pulmonary tuberculosis (WS 288—2017). Chinese Published. 2017. (In Chinese) [14] Ministry of Health Bureau of Disease Control and Prevention, Ministry of Health Department of Medical Administration, Chinese Center for Disease Control and Prevention. China tuberculosis program implementation guide (2008 Edition). Peking Union Medical College Press. 2009. (In Chinese) [15] Stavem K, Ghanima W, Olsen MK, et al. Persistent symptoms 1.5-6 months after COVID-19 in non-hospitalised subjects: a population-based cohort study. Thorax, 2021; 76, 405−7. doi: 10.1136/thoraxjnl-2020-216377 [16] Mandal S, Barnett J, Brill SE, et al. ‘Long-COVID’: a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax, 2021; 76, 396−8. doi: 10.1136/thoraxjnl-2020-215818 [17] Carfì A, Bernabei R, Landi F, et al. Persistent symptoms in patients after acute COVID-19. JAMA, 2020; 324, 603−5. doi: 10.1001/jama.2020.12603 [18] Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol, 2020; 5, 1265−73. doi: 10.1001/jamacardio.2020.3557 [19] D’Cruz RF, Waller MD, Perrin F, et al. Chest radiography is a poor predictor of respiratory symptoms and functional impairment in survivors of severe COVID-19 pneumonia. ERJ Open Res, 2021; 7, 00655−2020. [20] Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep, 2021; 11, 16144. doi: 10.1038/s41598-021-95565-8 [21] Fumagalli C, Zocchi C, Tassetti L, et al. COVID-19 Follow-up study Group. Factors associated with persistence of symptoms 1 year after COVID-19: A longitudinal, prospective phone-based interview follow-up cohort study. Eur J Intern Med, 2022; 97, 36−41. doi: 10.1016/j.ejim.2021.11.018 [22] Huang LX, Yao Q, Gu XY, et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet, 2021; 398, 747−58. doi: 10.1016/S0140-6736(21)01755-4 [23] Yang XY, Hou C, Shen Y, et al. Two-year health outcomes in hospitalized COVID-19 survivors in China. JAMA Netw Open, 2022; 5, e2231790. doi: 10.1001/jamanetworkopen.2022.31790 [24] Dao TL, Hoang VT, Gautret P. Recurrence of SARS-CoV-2 viral RNA in recovered COVID-19 patients: a narrative review. Eur J Clin Microbiol Infect Dis, 2021; 40, 13−25. doi: 10.1007/s10096-020-04088-z [25] Hoang T. Characteristics of COVID-19 recurrence: a systematic review and meta-analysis. Ann Glob Health, 2021; 87, 28. doi: 10.5334/aogh.3163 [26] Mirsaeidi M, Sadikot RT. Patients at high risk of tuberculosis recurrence. Int J Mycobacteriol, 2018; 7, 1−6. doi: 10.4103/ijmy.ijmy_164_17 [27] Verver S, Warren RM, Beyers N, et al. Rate of reinfection tuberculosis after successful treatment is higher than rate of new tuberculosis. Am J Respir Crit Care Med, 2005; 171, 1430−5. doi: 10.1164/rccm.200409-1200OC [28] Ruan QL, Yang QL, Sun F, et al. Recurrent pulmonary tuberculosis after treatment success: a population-based retrospective study in China. Clin Microbiol Infect, 2022; 28, 684−9. doi: 10.1016/j.cmi.2021.09.022 [29] He GQ, Wu J, Shi JC, et al. COVID-19 in tuberculosis patients: a report of three cases. J Med Virol, 2020; 92, 1802−6. doi: 10.1002/jmv.25943 [30] Ji Y, Cao HF, Liu Q, et al. Screening for pulmonary tuberculosis in high-risk groups of diabetic patients. Int J Infect Dis, 2020; 93, 84−9. doi: 10.1016/j.ijid.2020.01.019 [31] Qin F, Barry PM, Pascopella L. Factors associated with extended treatment among tuberculosis patients at risk of relapse in California. Int J Tuberc Lung Dis, 2016; 20, 363−9. doi: 10.5588/ijtld.15.0469 [32] Du J, Zhang L, Ma Y, et al. Treatment and recurrence on re-treatment tuberculosis patients: a randomized clinical trial and 7-year perspective cohort study in China. Eur J Clin Microbiol Infect Dis, 2020; 39, 93−101. doi: 10.1007/s10096-019-03696-8 [33] Sarma U, Mishra V, Goel J, et al. COVID-19 pneumonia with delayed viral clearance in a patient with active drug-resistant pulmonary tuberculosis. Ind J Crit Care Med, 2020; 24, 1132−4. doi: 10.5005/jp-journals-10071-23662 [34] Noori MAM, Younes I, Latif A, et al. Reactivation of tuberculosis in the setting of COVID-19 infection. Cureus, 2022; 14, e23417. [35] Small CL, Shaler CR, McCormick S, et al. Influenza infection leads to increased susceptibility to subsequent bacterial superinfection by impairing NK cell responses in the lung. J Immunol, 2010; 184, 2048−56. doi: 10.4049/jimmunol.0902772 [36] Yang H, Lu SH. COVID-19 and tuberculosis. J Transl Int Med, 2020; 8, 59−65. doi: 10.2478/jtim-2020-0010 -




 下载:
下载:



 Quick Links
Quick Links