-
Tuberculosis (TB) is a chronic infectious disease caused by Mycobacterium TB (Mtb), and remains a significant global public health issue, especially in low- and middle-income countries(LMICs)[1-3]. In China, the smoking rate among adult males exceeds 50%, and among TB patients, it is even higher, reaching approximately 50%-60%[4-6]. There is a synergistic effect between smoking and TB[7]. Smoking not only increases the risk of TB infection but also exacerbates its progression, resulting in more extensive lesions, increased pulmonary cavities, and poorer treatment outcomes[4,5,7,8]. Our previous research found that the chest X-ray scores of smoking TB patients were significantly higher than those of non-smoking patients, and after anti-TB treatment, lesion absorption was slower, with more severe residual chronic lung damage[9-11]. However, the mechanism by which smoking exacerbates TB remains unclear.
In recent years, the role of tertiary lymphoid structures (TLS) in chronic inflammation and immune responses has garnered increasing attention. TLS are ectopic lymphoid structures formed by the aggregation of lymphocytes from peripheral tissues in response to inflammation or infection, which typically provide localized immune protection[12,13]. Studies have shown that TLS are widely present in the airways and lung parenchyma of patients with chronic pulmonary diseases such as chronic obstructive pulmonary disease (COPD). Furthermore, their numbers are positively correlated with lung function decline and COPD exacerbation, suggesting that TLS may play a critical role in the chronic pathogenesis of COPD[14,15]. As well-known, COPD is a heterogeneous pulmonary condition characterized by persistent airway inflammation and airflow obstruction, mostly associated with cigarette smoking[16], but pulmonary TB is also an important risk factor for COPD in LMICS[16]. However, the potential mechanisms underlying so-called TB-associated COPD are largely unexplored.
Based on our previous observation that cigarette smoking is associated with more severe lung lesions in TB[10],this study focuses on analyzing the structural, cellular and molecular characteristics of pulmonary TLS in the lung tissues of smoking TB patients undergoing surgery. The study aims to explore whether TLS formation is associated with exacerbated lung damage in pulmonary TB, and thereby to provide new perspectives on the interactive mechanisms between TB and cigarette smoking, which may shed light on the understanding of the pathobiology of TB-associated COPD.
-
We enrolled male patients who underwent lobectomy due to pulmonary TB or lung nodules/masses at Beijing Chest Hospital between 2018 and 2024. Postoperative pathological diagnosis confirmed pulmonary TB in all cases, in accordance with the 2018 Chinese TB diagnostic criteria[17]. Patients were divided in two groups based on smoking history: the smoking TB group (smoking index ≥10 pack-years) and the non-smoking TB group (no history of smoking). Patients were matched in a 1:1 case-control matching based on age, and 18 patients from each group were selected for analysis. Paraffin-embedded postoperative lung tissue samples were collected from all enrolled patients.
-
Exclusion criteria included the presence of other chronic respiratory diseases (such as asthma, bronchiectasis, interstitial lung disease, or other structural lung diseases), lung malignancies, HIV, and autoimmune diseases.
-
Baseline information was collected from all study participants, including age, body mass index (BMI), smoking history, pack-years of smoking, comorbidities. Preoperative chest CT scans were collected and analyzed.
-
Preoperative chest CT images were evaluated for TB severity score using a six-zone scoring method proposed by Casarini et al. in 1999[18]. The lungs were divided into six regions: upper (above the carina), middle (between the carina and lower pulmonary veins), and lower (below the lower pulmonary veins) regions for both lungs. The scoring was based on the percentage of lung parenchyma affected by abnormal findings in each region. The scores were as follows: 1 point for <25% involvement, 2 points for 25%-50%, 3 points for 50%-75%, and 4 points for >75%. The total score was obtained by summing the scores of all regions, with a total score range from 0 to 24. The chest CT scoring was performed by two experienced pulmonologists and one radiologist.
-
Lung tissue samples were paraffin-embedded and sectioned into 4 µm thick slices for hematoxylin and eosin (HE) staining to observe the distribution and structural characteristics of pulmonary TLS. The analysis of TLS followed standard methods described in the literature. Aggregates with 50 or more lymphocytes were defined as TLS[19], while areas with fewer than 50 cells were considered lymphocyte aggregates. For each patient's sample, the number of TLS in the peribronchial and lung parenchymal regions was quantified. The infiltration in the peribronchial region was standardized by the number of bronchi in each lung section, while the infiltration in the lung parenchyma was standardized by the area of the parenchyma. All samples were examined by a pulmonologist and a pathologist.
-
Immunohistochemical staining was performed using CD20 (Abcam, USA) and CXCL13 (Abcam, USA) markers to further analyze the cellular composition and molecular characteristics of TLS. CD20, a marker for B cells, was used to assess the distribution and number of B cells within the TLS. CXCL13, a chemokine that attracts B cells and T follicular helper cells (Tfh), was also examined. After immunohistochemical staining, each sample was photographed under a microscope, and the number of CXCL13-positive cells per unit area and the average size of CD20+ B cell follicles were recorded for quantitative analysis.
-
To investigate immune cell subsets within TLS, multicolor immunofluorescence staining was conducted. Markers included: CD4 (Abcam, USA) and CD8 (Abcam, USA) for helper T cells and cytotoxic T cells, respectively; CD20 for B cells and CD138 for plasma cells (activated B cells). The stained sections were analyzed under a fluorescence microscope, where the quantity and distribution patterns of different immune cell subsets were assessed. All samples were reviewed by a pulmonologist and a pathologist.
-
Data were statistically analyzed using SPSS software. The differences in the number of TLS and the expression of immune markers between smoking and non-smoking TB groups were compared using independent sample t-tests or Mann-Whitney U tests. Pearson correlation analysis was used to examine the relationship between CT scores and the number of TLS, in order to explore the correlation between TLS and the severity of TB. A p-value of <0.05 was considered statistically significant.
-
A total of 36 male TB patients were included in this study, with 18 patients in the smoking group and 18 in the non-smoking group. There were no significant differences between the two groups in terms of age, BMI, and comorbidity such as hypertension and diabetes. The baseline characteristics are summarized in Table 1.
Table 1. Baseline characteristics of 36 male TB patients
Smoker Non-smoker P value Number of patients 18 18 Age (years) 54.28±4.00 54.28±5.28 1.000 Smoking index (pack-year) 36.33±21.15 0 < 0.001 BMI 24.60±4.10 23.37±2.64 0.088 Comorbidity
Hypertension, n (%)
Diabetes mellitus, n (%)
3 (16.7)
8 (44.4)
5 (27.8)
4 (22.2)
0.688
0.157Chest CT TB severity scoring
Total score
Cavitation, n (%)
10.44±2.54
10 (55.6)
7.94±1.63
4 (22.2)
0.001
0.040Note. BMI, Body Mass Index; CT, Computed Tomography; TB, Tuberculosis. -
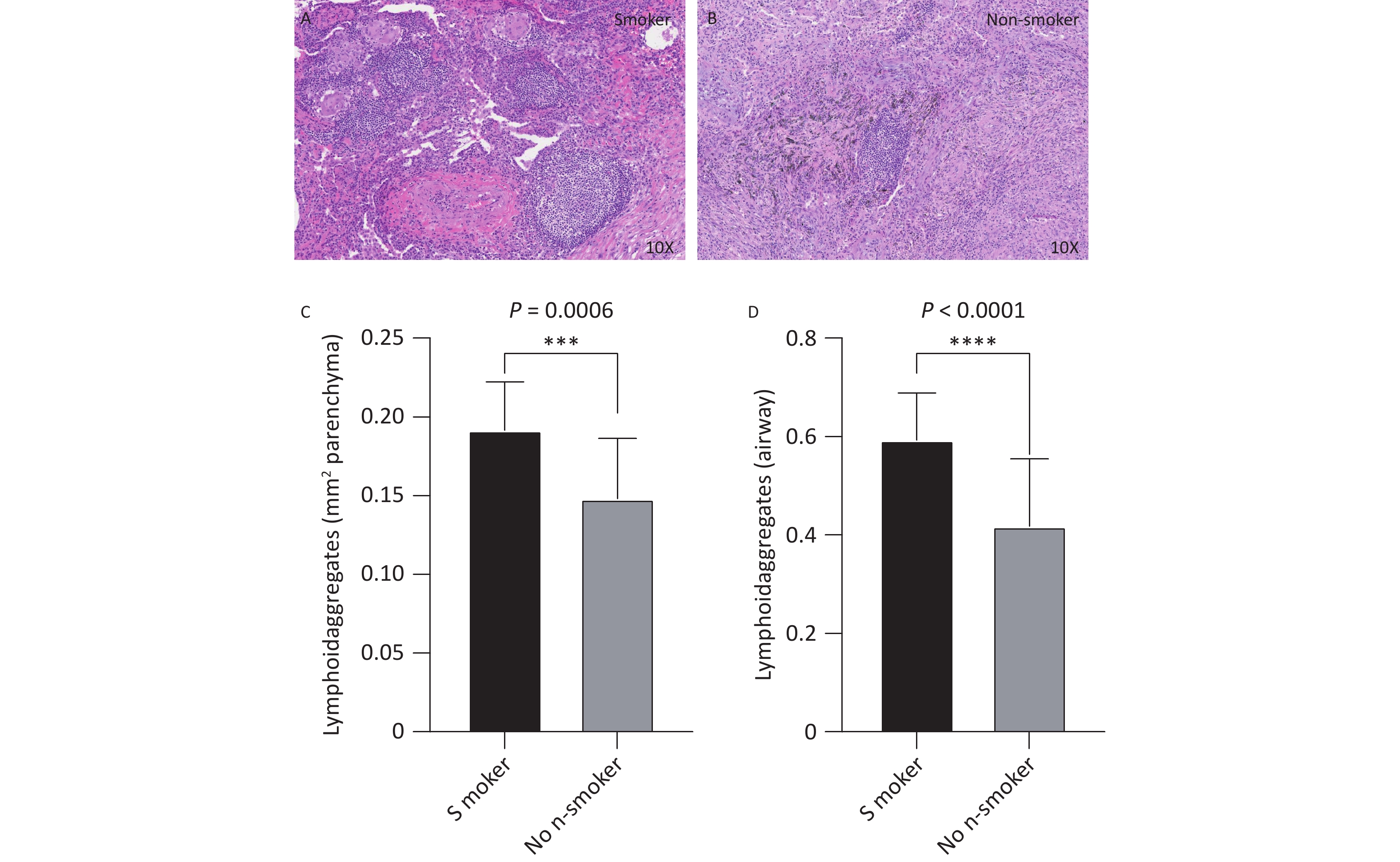
Histopathological analysis of lung tissues revealed that the number of TLS in the lung parenchyma (Figure 1C, P < 0.001) and peribronchial regions (Figure 1D, P < 0.001) was significantly higher in the smoking group (Figure 1A) than that in the non-smoking group (Figure 1B). On average, the number of peribronchial TLS in each sample was 0.59 ± 0.09 in the smoking group, compared to 0.42 ± 0.14 in the non-smoking group. Similarly, the number of TLS in the lung parenchyma was 0.19 ± 0.03 in the smoking group, compared to 0.15 ± 0.04 in the non-smoking group. The smoking group had significantly more TLS in both regions than that in the non-smoking group (both P < 0.001).
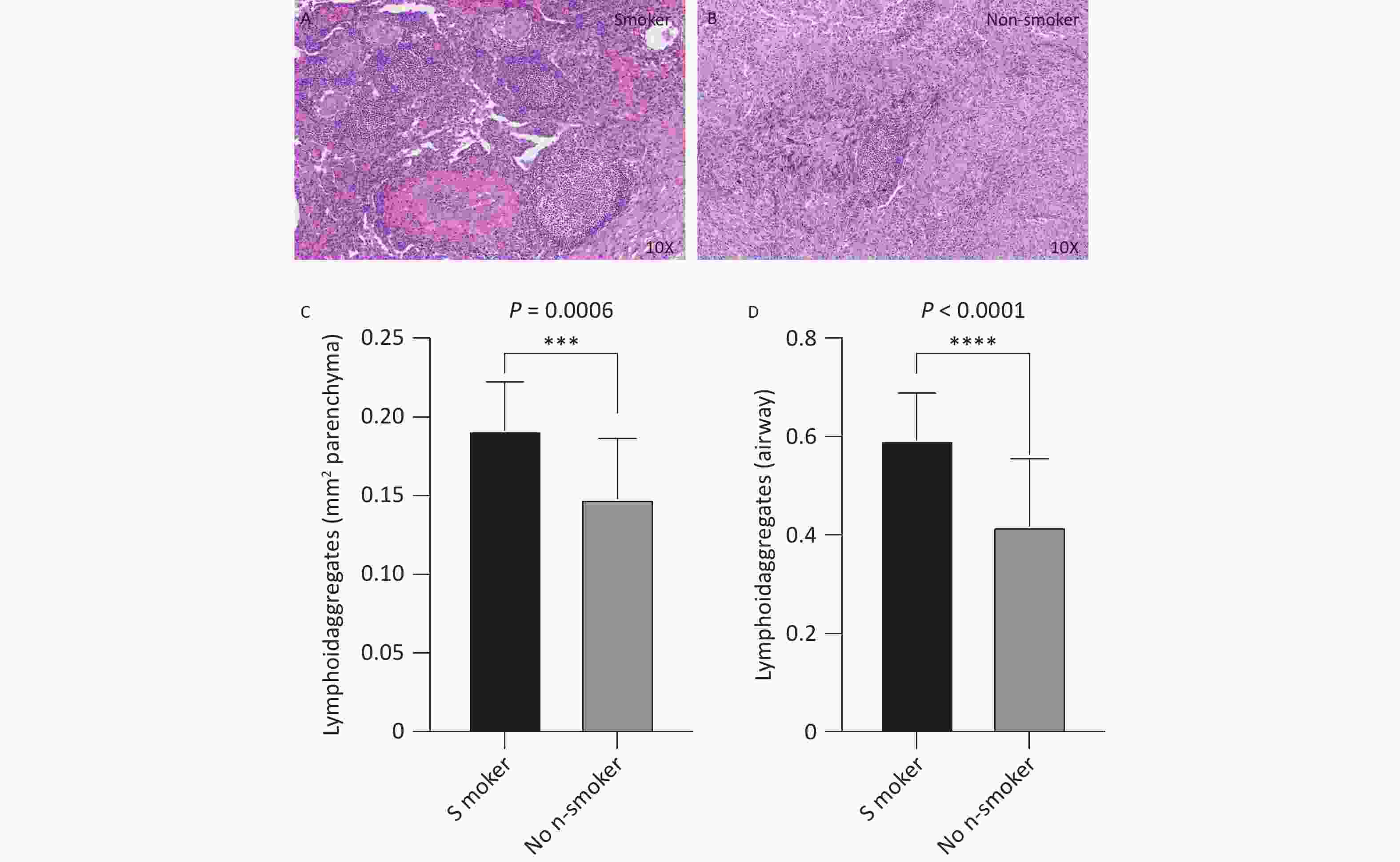
Figure 1. Distribution and quantity of airway and lung parenchyma TLS in smoking and non-smoking TB patients. Smoking group n=18, non-smoking group n = 18. (A, B) Representative images of lung parenchymal TLS in smoking and non-smoking TB patients (10X magnification). (C, D) Analysis of the number of lung parenchymal TLS and peribronchial TLS in smoking and non-smoking TB patients.
-
TB lesion severity, assessed using preoperative chest CT scans,revealed a significantly higher CT score in the smoking group than the non-smoking group (10.44 ± 2.54 vs. 7.94 ± 1.63, P < 0.01, Figure 2A). Correlation analysis between the number of TLS and CT severity scores demonstrated that the number of TLS in the lung parenchymal region (r = 0.5767, R² = 0.3326, P = 0.0002, Figure 2B) and peribronchial region (r = 0.7373, R² = 0.5436, P < 0.0001, Figure 2C) were positively correlated with the CT scores. This indicates that the increase in TLS is associated with greater disease severity, suggesting that TLS may play a role in the exacerbation of TB in smoking patients.
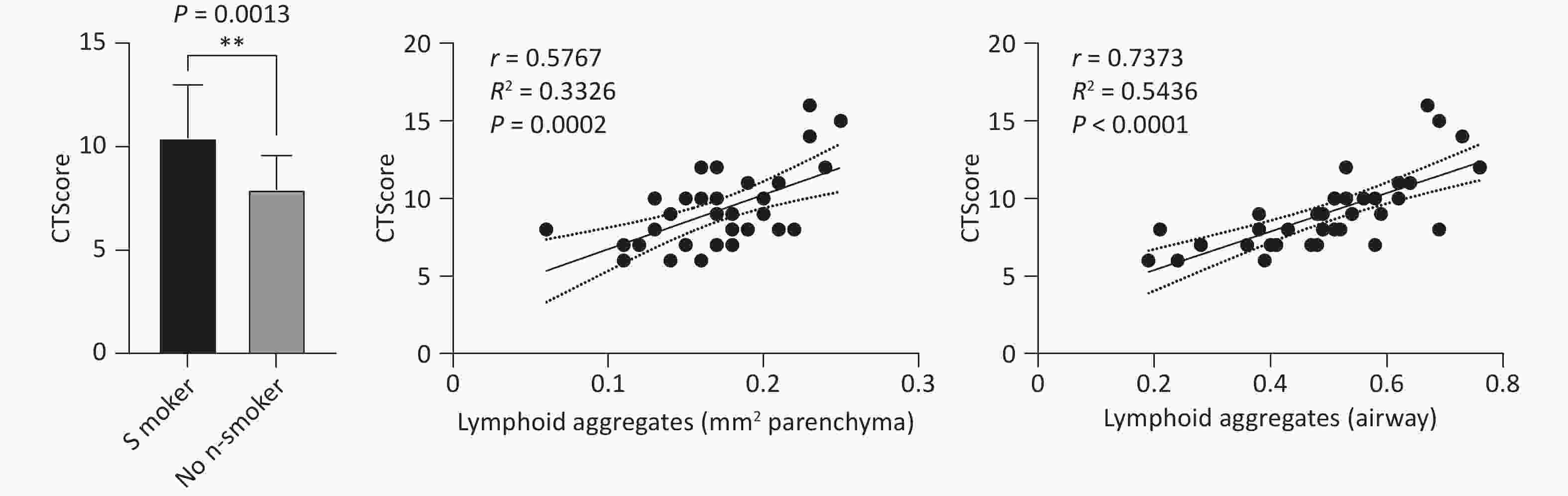
Figure 2. Correlation between lung TLS quantity and imaging TB severity scores in TB patients. (A) Chest CT TB scores in smoking and non-smoking TB patients. (B) Correlation between lung parenchymal TLS accumulation and imaging severity scores in TB patients. (C) Correlation between peribronchial TLS accumulation and imaging severity scores in TB patients.
-
Immunohistochemical staining revealed that B cells were the predominant lymphocyte type in both the smoking and non-smoking groups, with CD20-positive cells primarily located within the TLS regions. In the smoking group (Figure 3A, B), the average area of the CD20+ B cell follicles was significantly larger than that in the non-smoking group (153,445 vs. 91,501 μm², P = 0.0146, Figure 3C, D).
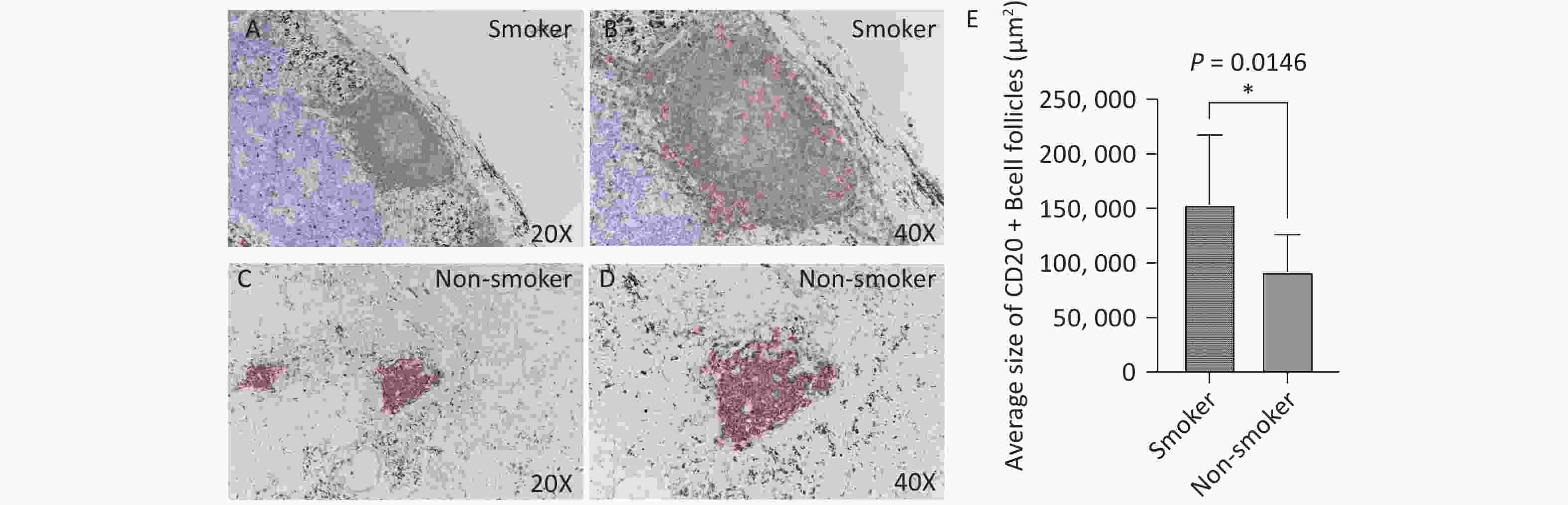
Figure 3. CD20 expression in lung TLS of TB patients. Brown represents CD20-positive staining. (A, B) Representative images of CD20 expression in lung TLS of smoking TB patients (10X and 20X magnification, respectively). (C, D) Representative images of CD20 expression in lung TLS of non-smoking TB patients (10X and 20X magnification, respectively). (E) Quantitative analysis.
-
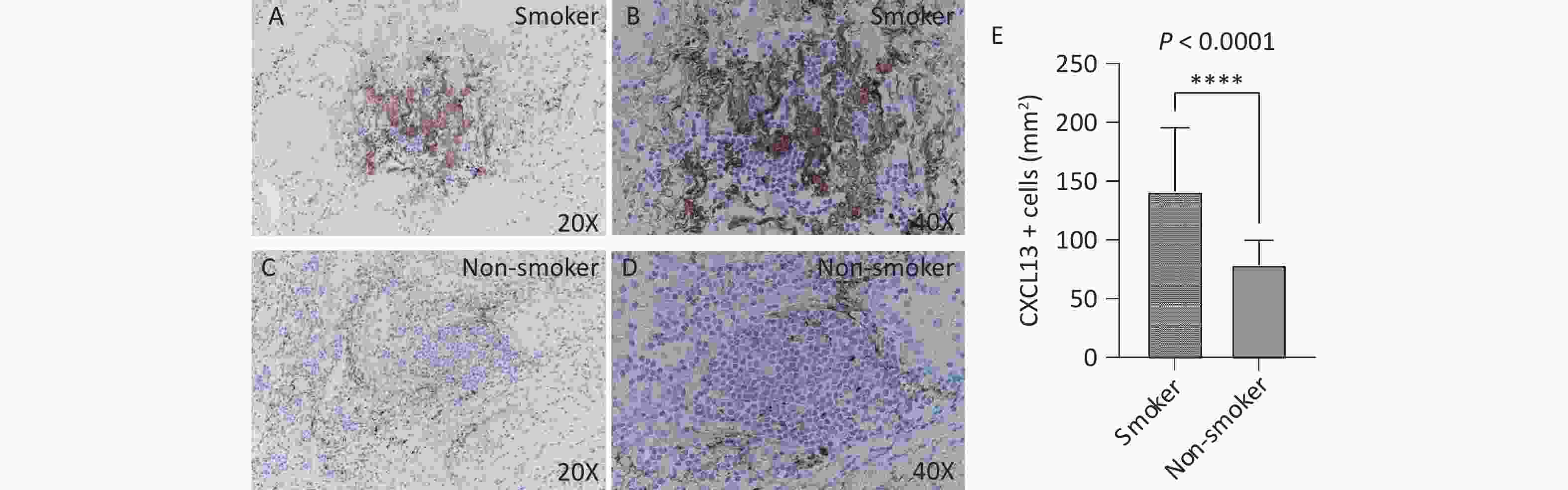
CXCL13 expression in TLS was assessed by immunohistochemistry. The number of CXCL13-positive cells per unit area was significantly higher in the smoking group (Figure 4A, B) than that in the non-smoking group (141.3 vs. 79.06, P < 0.0001, Figure 4C, D). Figure 4 clearly illustrates the increased CXCL13 expression in the TLS of smoking patients.
-
Opal multiplex staining was employed to analyze the distribution of lymphocyte cells and plasma cells in the TLS. Both smoking TB patients (Figure 5A-D, I-L) and non-smoking TB patients (Figure 5E-H, M-P) exhibited a predominance of CD20+ B cells in their TLS, along with a substantial presence of CD4+ and CD8+ T cells and plasma cells (CD138+). Under 20X fluorescence microscopy, the number of CD4+ T cells (237.1 vs. 176.2, P = 0.0150) and CD8+ T cells (117.8 vs. 88.10, P = 0.0320) in the TLS was significantly higher in the smoking group compared to the non-smoking group, while the number of CD138+ plasma cells did not differ significantly between the two groups (33.10 vs. 29.10, P = 0.5872). These findings suggest that smoking may exacerbate immune responses within TLS by promoting lymphocyte cell activation.
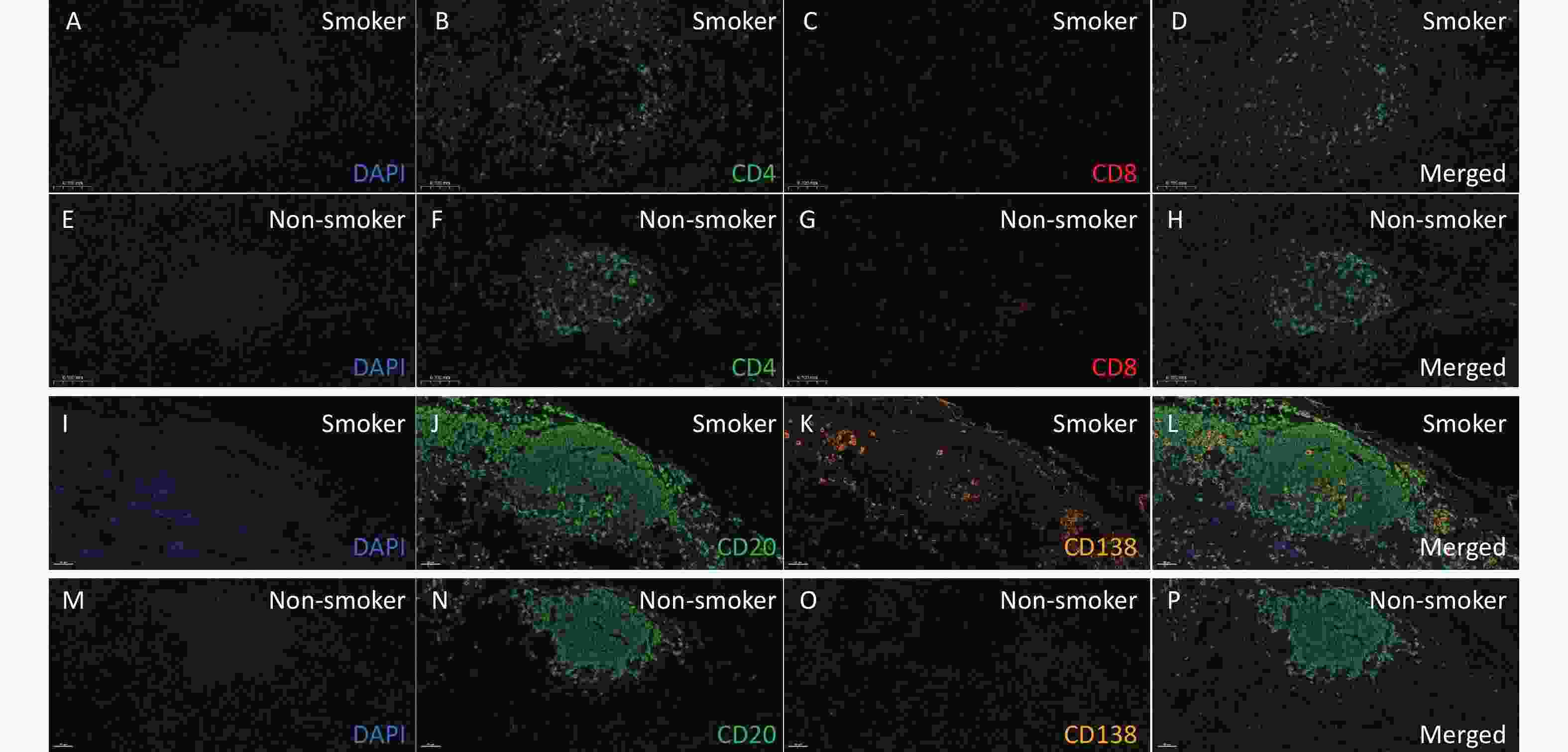
Figure 5. Analysis of T and B lymphocyte subpopulations in lung TLS of TB patients. Lung tissue sections from smoking (A-D) and non-smoking (E-H) TB patients were stained with CD4 (Q) and CD8 (R) antibodies. DAPI: blue; CD4: green; CD8: red. Lung tissue sections from smoking (I-L) and non-smoking (M-P) TB patients were stained with CD20 and CD138 (S) antibodies. DAPI: blue; CD20: green; CD138: orange. (20X magnification).
-
The current study, for the first time to our knowledge, demonstrated that the number of lung TLS was significantly increased, and was associated with increased severity of lung lesions on chest CT in smoking TB patients. The positive correlation between the number of lung TLS and TB severity score highlights a potential role of lung TLS in TB disease progression. Immunohistochemical analysis further revealed a significant increase in the expression of B cells, CXCL13, and T cells within the TLS in the smoking TB group. These findings suggest that smoking may exacerbate lung pathological inflammation and damage in TB patients by promoting TLS formation and immune activation.
Following Mycobacterium tuberculosis (Mtb) infection, B cells aggregate in the lungs to form B-cell follicles (BCFs). Lung TLS, as a localized immune structure, exhibit dual roles in TB. On one hand, TLS enhance local immune responses by aggregating immune cells such as B cells, T cells, and dendritic cells to combat pathogen invasion, thereby offering protective effects. In TB patients, lung TLS contribute to the development of anti-TB immunity through mechanisms involving B cell activation, antibody production, and T cell regulation[19-21]. On the other hand, excessive immune responses may lead to immune-mediated tissue damage, resulting in pulmonary destruction and exacerbating TB[22]. Previous studies have shown that lung TLS play a protective role during latent TB infection, as evidenced by higher TLS numbers in latent TB patients compared to those with active pulmonary TB[21]. Additionally, the duration of TLS in the lungs differs between susceptible and drug-resistant Mtb strain-infected mice. Research has shown that the number of TLS peaks at week 8 post-Mtb infection, after which it gradually declines, with notable strain-specific differences. Mice infected with susceptible strains show a sharp decrease in TLS number by week 16, while mice infected with relatively drug-resistant strains show a more gradual decline, not reaching significant reduction until week 45[23]. These observations suggest that lung TLS may play a more complex, dual role in chronic TB infection. In our study, however, we found that lung TLS numbers were significantly higher in smoking TB patients, and these numbers correlated positively with TB severity as assessed by chest CT. This suggests that, in the context of smoking, an increase in lung TLS may not represent a simple protective immune response, but rather an overactivated immune process. Immunohistochemical analysis revealed a significant increase in the number of B cells, T cells, and CXCL13 within the TLS in smoking TB patients. This excessive lung TLS formation likely intensifies local inflammatory responses, promote sustained inflammatory responses, possibly by inducing the continued release of inflammatory factors such as CXCL12, CXCL13, CCL19, CCL21, and IL-23, leading to overactive immunity and ultimately causing pathogenic tissue damage[24].
Although the role of lung TLS formation and its impact on lung damage in smoking TB patients has not been previously reported, studies have shown that CS exposure can induce airway inflammation and promote TLS formation[25]. In COPD, TLS—primarily composed of B cells—are found in small airways and lung parenchyma, with their presence correlating with disease severity and lung function decline[14,15,26]. Smoking-induced chronic airway inflammation and oxidative stress may disrupt lung immune tolerance, promoting the persistent activation of immune cells and the formation of lung TLS. Harmful substances produced by smoking, such as toxic chemicals in smoke, may influence immune cell function and migration through various pathways, thereby stimulating the proliferation of lung TLS[27].
Regarding the upstream mechanisms that promote lung TLS formation, previous studies have highlighted CXCL13 as a key chemokine involved in recruiting B and Tfh cells to TLS[25]. We hypothesize that the IL-17/CXCL13 axis may be a critical pathway in smoking-induced TLS formation. IL-17, secreted by Th17 cells during the early TB infection, can induce CXCL13 production, attracting B cells and Tfh cells to the TLS regions, thus driving the continuous aggregation and activation of immune cells[24]. Smoking may enhance the activity of the IL-17-related pathway through oxidative stress, inflammation, and other mechanisms. For example, reactive oxygen species (ROS) induced by smoking can activate NF-κB and MAPK signaling pathways, promoting the expression and release of IL-17[14,28]. Under smoking conditions, this chronic immune activation leads to persistent lung TLS formation, potentially triggering pathological inflammation and causing destructive damage to lung tissue[19].
Beyond TB, lung TLS also exhibit dual roles in other chronic inflammatory diseases[12,13,29]. In autoimmune diseases, TLS may play a protective role in the early stages, while in the chronic phase, excessive production of pro-inflammatory cytokines and antibodies by B cells and T cells within TLS may lead to over-inflammation and fibrosis, further impairing organ function[13,30,31]. Whether TLS formation also plays such a dual role in TB pathogenesis, particular in the context of concurrent cigarette smoking, needs further investigation.
-
This study is based on clinical data and lung tissue samples from TB patients, without in vitro cell experiments or animal model validation. The specific functions of lung TLS and the molecular signaling pathways involved in the course of TB infection warrant further investigation.
-
In summary, our study demonstrated increased TLS formation in lung tissues from smoker patients with TB, and the number of TLS was associated positively with the severity of lung lesions on chest CT. Cigarette smoking was also associated with upregulated expression of B cell chemokines in TB, suggesting that cigarette smoking may exacerbate lung damage by promoting TLS formation in the process of TB pathogenesis.
doi: 10.3967/bes2025.020
Increased Tertiary Lymphoid Structures are Associated with Exaggerated Tissue Damage in the Lung of Smoker Patients with Pulmonary Tuberculosis
-
Abstract:
Objective Cigarette smoking exacerbates progression of pulmonary tuberculosis (TB) . The role of tertiary lymphoid structures (TLS) in chronic lung diseases has gained attention, but it remains unclear whether smoking-exacerbated lung damage in TB is associated with TLS. This study aims to analyze the characteristics of pulmonary TLS in smoking TB patients and therefore to explore the possible role of TLS in smoking-related lung injury in TB. Methods Lung tissues from 36 male patients (18 smokers and 18 non-smokers) who underwent surgical resection due to pulmonary TB were included in this study. Pathological and immunohistological analysis was conducted to evaluate the quantity of TLS, and chest CT was used to assess the severity of lung lesions. The correlation between TLS quantity and TB lesion severity scores was analyzed. Immune cells and chemokines for TLS formation were also evaluated and compared between smoker and nonsmoker patients. Results Smoking TB patients had significantly more TLS than non-smokers (P < 0.001). TLS quantity in both lung parenchyma and peribronchial regions correlated with TB lesion severity on chest CT (parenchyma: r = 0.5767; peribronchial: r = 0.7373; both P < 0.001). Immunohistochemical analysis showed increased B cells, T cells, and CXCL13 expression in smoker patients with TB (P < 0.001). Conclusion Smoking TB patients exhibited increased pulmonary TLS, which was associated with exacerbated lung lesions on chest CT, suggesting that cigarette smoking may exacerbate lung damage by promoting TLS formation. -
Key words:
- Tuberculosis /
- Pulmonary tertiary lymphoid structures /
- Cigarette smoking
There are no conflicts of interest to declare.
This study was approved by the Medical Ethics Committee of Peking University Third Hospital (Ethical approval number: M2022296) and the Medical Ethics Committee of Beijing Chest Hospital (Ethical approval number: YJS-2022-043). All patients signed informed consent forms.
&These authors contributed equally to this work.
注释:1) Authors’ Contributions: 2) Competing Interests: 3) Ethical Approval: -
Figure 1. Distribution and quantity of airway and lung parenchyma TLS in smoking and non-smoking TB patients. Smoking group n=18, non-smoking group n = 18. (A, B) Representative images of lung parenchymal TLS in smoking and non-smoking TB patients (10X magnification). (C, D) Analysis of the number of lung parenchymal TLS and peribronchial TLS in smoking and non-smoking TB patients.
Figure 2. Correlation between lung TLS quantity and imaging TB severity scores in TB patients. (A) Chest CT TB scores in smoking and non-smoking TB patients. (B) Correlation between lung parenchymal TLS accumulation and imaging severity scores in TB patients. (C) Correlation between peribronchial TLS accumulation and imaging severity scores in TB patients.
Figure 3. CD20 expression in lung TLS of TB patients. Brown represents CD20-positive staining. (A, B) Representative images of CD20 expression in lung TLS of smoking TB patients (10X and 20X magnification, respectively). (C, D) Representative images of CD20 expression in lung TLS of non-smoking TB patients (10X and 20X magnification, respectively). (E) Quantitative analysis.
Figure 5. Analysis of T and B lymphocyte subpopulations in lung TLS of TB patients. Lung tissue sections from smoking (A-D) and non-smoking (E-H) TB patients were stained with CD4 (Q) and CD8 (R) antibodies. DAPI: blue; CD4: green; CD8: red. Lung tissue sections from smoking (I-L) and non-smoking (M-P) TB patients were stained with CD20 and CD138 (S) antibodies. DAPI: blue; CD20: green; CD138: orange. (20X magnification).
Table 1. Baseline characteristics of 36 male TB patients
Smoker Non-smoker P value Number of patients 18 18 Age (years) 54.28±4.00 54.28±5.28 1.000 Smoking index (pack-year) 36.33±21.15 0 < 0.001 BMI 24.60±4.10 23.37±2.64 0.088 Comorbidity
Hypertension, n (%)
Diabetes mellitus, n (%)
3 (16.7)
8 (44.4)
5 (27.8)
4 (22.2)
0.688
0.157Chest CT TB severity scoring
Total score
Cavitation, n (%)
10.44±2.54
10 (55.6)
7.94±1.63
4 (22.2)
0.001
0.040Note. BMI, Body Mass Index; CT, Computed Tomography; TB, Tuberculosis. -
[1] World Health Organization. Global tuberculosis report 2024. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2024. [Accessed at Dec 10, 2024]. [2] Li W, Wang X, Bi B, et al. Influence of Temperature and Humidity on the Incidence of Pulmonary Tuberculosis in Hainan, China, 2004–2018. Biomed Environ Sci, 2024; 37(9), 1080-1085. [3] Fan Y, Liu D, Chen Y, et al. Inferring Mycobacterium Tuberculosis Drug Resistance and Transmission using Whole-genome Sequencing in a High TB-burden Setting in China. Biomed Environ Sci, 2024; 37(2), 157-169. [4] Leung CC, Yew WW, Chan CK, et al. Smoking adversely affects treatment response, outcome and relapse in tuberculosis. Eur Respir J, 2015; 45, 738−745. doi: 10.1183/09031936.00114214 [5] Sun Q, Li S, Gao M, et al. Therapeutic Strategies for Tuberculosis: Progress and Lessons Learned. Biomed Environ Sci, 2024; 37(11), 1310-1323. [6] Guo C, Nie L, Song Y, et al. Efficacy and Safety of Combined Bedaquiline and Delamanid Use among Patients with Multidrug-Resistant Tuberculosis in Beijing, China. Biomed Environ Sci, 2024; 37(10), 1195-1203. [7] Quan DH, Kwong AJ, Hansbro PM, et al. No smoke without fire: the impact of cigarette smoking on the immune control of tuberculosis. Eur Respir Rev, 2022; 31. [8] Gai X, Cao W, Rao Y, et al. Risk factors and biomarkers for post-tuberculosis lung damage in a Chinese cohort of male smokers and non-smokers: protocol for a prospective observational study. BMJ Open, 2023; 13, e065990. doi: 10.1136/bmjopen-2022-065990 [9] Gai X, Allwood B, Sun Y. Post-tuberculosis lung disease and chronic obstructive pulmonary disease. Chin Med J (Engl), 2023; 136, 1923−1928. doi: 10.1097/CM9.0000000000002771 [10] Rao Y, Cao W, Qu J, et al. More severe lung lesions in smoker patients with active pulmonary tuberculosis were associated with peripheral NK cell subsets. Tuberculosis (Edinb), 2023; 138, 102293. doi: 10.1016/j.tube.2022.102293 [11] Rao Y, Gai X, Le Y, et al. Enhanced Proinflammatory Cytokine Production and Immunometabolic Impairment of NK Cells Exposed to Mycobacterium tuberculosis and Cigarette Smoke. Front Cell Infect Microbiol, 2021; 11, 799276. [12] Sato Y, Silina K, van den Broek M, et al. The roles of tertiary lymphoid structures in chronic diseases. Nat Rev Nephrol, 2023; 19, 525−537. [13] Zhao R, Zhang J, Ma J, et al. cGAS-activated endothelial cell-T cell cross-talk initiates tertiary lymphoid structure formation. Sci Immunol, 2024; 9, eadk2612. doi: 10.1126/sciimmunol.adk2612 [14] Xiong J, Zhou L, Tian J, et al. Cigarette Smoke-Induced Lymphoid Neogenesis in COPD Involves IL-17/RANKL Pathway. Front Immunol, 2020; 11, 588522. [15] John-Schuster G, Hager K, Conlon TM, et al. Cigarette smoke-induced iBALT mediates macrophage activation in a B cell-dependent manner in COPD. Am J Physiol Lung Cell Mol Physiol, 2014; 307, L692−706. doi: 10.1152/ajplung.00092.2014 [16] Global initiative for chronic obstructive lung disease, GOLD 2025. https://goldcopd.org/wp-content/uploads/2024/11/GOLD-2025-Report-v1.0-15Nov2024_WMV.pdf. [17] National Health and Family Planning Commission of the People's Republic of China. Diagnostic criteria for tuberculosis (WS 288—2017). Electronic Journal of Emerging Infectious Diseases, 2018; 3, 59−61. (In Chinese) [18] Song Q, Guo X, Zhang L, et al. New Approaches in the Classification and Prognosis of Sign Clusters on Pulmonary CT Images in Patients With Multidrug-Resistant Tuberculosis. Front Microbiol, 2021; 12, 714617. doi: 10.3389/fmicb.2021.714617 [19] Linge I, Tsareva A, Kondratieva E, et al. Pleiotropic Effect of IL-6 Produced by B-Lymphocytes During Early Phases of Adaptive Immune Responses Against TB Infection. Front Immunol, 2022; 13, 750068. doi: 10.3389/fimmu.2022.750068 [20] Ulrichs T, Kosmiadi GA, Trusov V, et al. Human tuberculous granulomas induce peripheral lymphoid follicle-like structures to orchestrate local host defence in the lung. J Pathol, 2004; 204, 217−228. doi: 10.1002/path.1628 [21] Chen Y, Bharrhan S, Xu J, et al. B cells promote granulomatous inflammation during chronic Mycobacterium tuberculosis infection in mice. PLoS Pathog, 2023; 19, e1011187. doi: 10.1371/journal.ppat.1011187 [22] Slight SR, Rangel-Moreno J, Gopal R, et al. CXCR5⁺ T helper cells mediate protective immunity against tuberculosis. J Clin Invest, 2013; 123, 712−726. [23] Linge I, Kondratieva E, Apt A. Prolonged B-Lymphocyte-Mediated Immune and Inflammatory Responses to Tuberculosis Infection in the Lungs of TB-Resistant Mice. Int J Mol Sci, 2023; 24. [24] Linge I, Kondratieva T, Apt A. B-cell follicles in tuberculous lung: Active defenders or modest bystanders? Immunology, 2023; 169, 515-518. [25] Gopal R, Rangel-Moreno J, Slight S, et al. Interleukin-17-dependent CXCL13 mediates mucosal vaccine-induced immunity against tuberculosis. Mucosal Immunol, 2013; 6, 972−984. doi: 10.1038/mi.2012.135 [26] Hogg JC, Chu F, Utokaparch S, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med, 2004; 350, 2645−2653. doi: 10.1056/NEJMoa032158 [27] Saint-André V, Charbit B, Biton A, et al. Smoking changes adaptive immunity with persistent effects. Nature, 2024; 626, 827−835. doi: 10.1038/s41586-023-06968-8 [28] Mangan PR, Harrington LE, O'Quinn DB, et al. Transforming growth factor-beta induces development of the T(H)17 lineage. Nature, 2006; 441, 231−234. doi: 10.1038/nature04754 [29] Marin ND, Dunlap MD, Kaushal D, et al. Friend or Foe: The Protective and Pathological Roles of Inducible Bronchus-Associated Lymphoid Tissue in Pulmonary Diseases. J Immunol, 2019; 202, 2519−2526. doi: 10.4049/jimmunol.1801135 [30] Zhao L, Jin S, Wang S, et al. Tertiary lymphoid structures in diseases: immune mechanisms and therapeutic advances. Signal Transduct Target Ther, 2024; 9, 225. doi: 10.1038/s41392-024-01947-5 [31] Yang F, Yang J, Wu M, et al. Tertiary lymphoid structures: new immunotherapy biomarker. Front Immunol, 2024; 15, 1394505. doi: 10.3389/fimmu.2024.1394505 -




 下载:
下载:



 Quick Links
Quick Links