-
Dentistry is a profession with a high prevalence of work-related musculoskeletal disorders (WMSDs), with symptoms often appearing very early in one’s career[1]. WMSDs are conditions affecting the muscles, bones, and nervous system due to occupational factors. In 2002, the International Labor Organization included musculoskeletal diseases in the International List of Occupational Diseases. China’s recently updated Classification and Catalog of Occupational Diseases has introduced two new categories of occupational illnesses, including occupational musculoskeletal disorders. WMSDs significantly impact the health and work of dentists, reducing their quality of life and causing economic losses. These disorders are multifactorial in nature, influenced by personal, psychosocial, biomechanical, and environmental factors. Dentists frequently maintain static or awkward postures during procedures, which leads to musculoskeletal strain and discomfort; additionally, long working hours contribute to psychological stress, further increasing the risk of WMSDs[2]. Moreover, various stressors, such as job satisfaction, practice income, work hours, and staff/patient interactions, exacerbate the problem. A 2009 systematic review found that the global prevalence of musculoskeletal disorders among dental professionals ranged from 64% to 93%[3]. In China, rising public awareness of oral health and aesthetics has resulted in an increasing demand for dental services. However, uneven distribution of healthcare resources has intensified the workload for dentists in China, placing greater strain on their musculoskeletal systems. Research by Feng et al. identified a significant correlation between job stress and WMSD symptoms. However, studies on musculoskeletal disorders among dentists in China remain limited, with most focusing on single-factor analyses. To address this gap, this study employs a structural equation model (SEM), a multivariate statistical framework that examines the complex relationship between directly observed and latent variables as well as analyzes the path relationship between variables. By analyzing the complex factors contributing to WMSDs, this study aims to provide insights for self-care strategies among dentists and inform policies to reduce WMSD prevalence, ultimately improving the quality of life of these professionals.
This study employed a cross-sectional design to develop and test an SEM examining the structural relationship between personal characteristics, family function, job satisfaction, mental load, and WMSDs among dentists in China. The participants were dentists from seven hospitals in Shandong Province, China, recruited through cluster sampling based on the following inclusion criteria: (1) actively engaged in clinical work at the time of the study, (2) fully informed of the study’s purpose and providing written informed consent, and (3) no history of trauma or systemic diseases. A total of 300 questionnaires were distributed, with 292 valid responses included in the final analysis. This study was approved by the Ethical Review Committee of Shandong Second Medical University (2023YX066). Personal characteristics were recorded using a general questionnaire, which included factors such as age, body mass index, work experience, professional title, number of procedures per day, smoking status, and physical activity levels. Each item was rated on a four-point scale (1–4), with higher scores indicating greater levels of the corresponding characteristic. Family function was assessed using the Family APGAR questionnaire, with each item rated on a three-point scale from 1 (almost always) to 3 (hardly ever). Job satisfaction was evaluated using the Job Satisfaction Measure Scale developed by Brayfield and Rothe, with responses rated on a five-point scale from 1 (strongly agree) to 5 (strongly disagree). Mental load was measured using the Subjective Workload Assessment Technique, with each item rated on a three-point scale from 1 (mild) to 3 (heavy). WMSDs were evaluated using the Nordic Musculoskeletal Questionnaire, with each item rated on a five-point scale from 1 (less or low) to 5 (more or high). Data collection was conducted by two trained graduate students within this field from September 10 to December 20, 2023. Before completing the questionnaire, participants were informed about the study’s objectives, questionnaire content, and privacy policy. All eligible participants signed the informed consent form to participate voluntarily and anonymously, with the right to withdraw from the study at any time. Data analysis was performed using SPSS version 23.0 (IBM Corporation Armonk, New York, USA) and AMOS 24.0 (IBM Corporation Armonk, New York, USA). Internal reliability of the questionnaires was analyzed using Cronbach’s α coefficient, with a value > 0.70 considered acceptable. Model fitness was evaluated based on several indices, including χ2/df, goodness of fit index (GFI), adjusted GFI (AGFI), comparative fit index (CFI), and root mean square error of approximation (RMSEA), with acceptable thresholds set at χ2/df < 3.0, GFI > 0.90, AGFI > 0.85, CFI > 0.90, and RMSEA < 0.08. To ensure parsimony and fitness of the model, observed variables without a significant relationship with latent variables were excluded from the final SEM analysis.
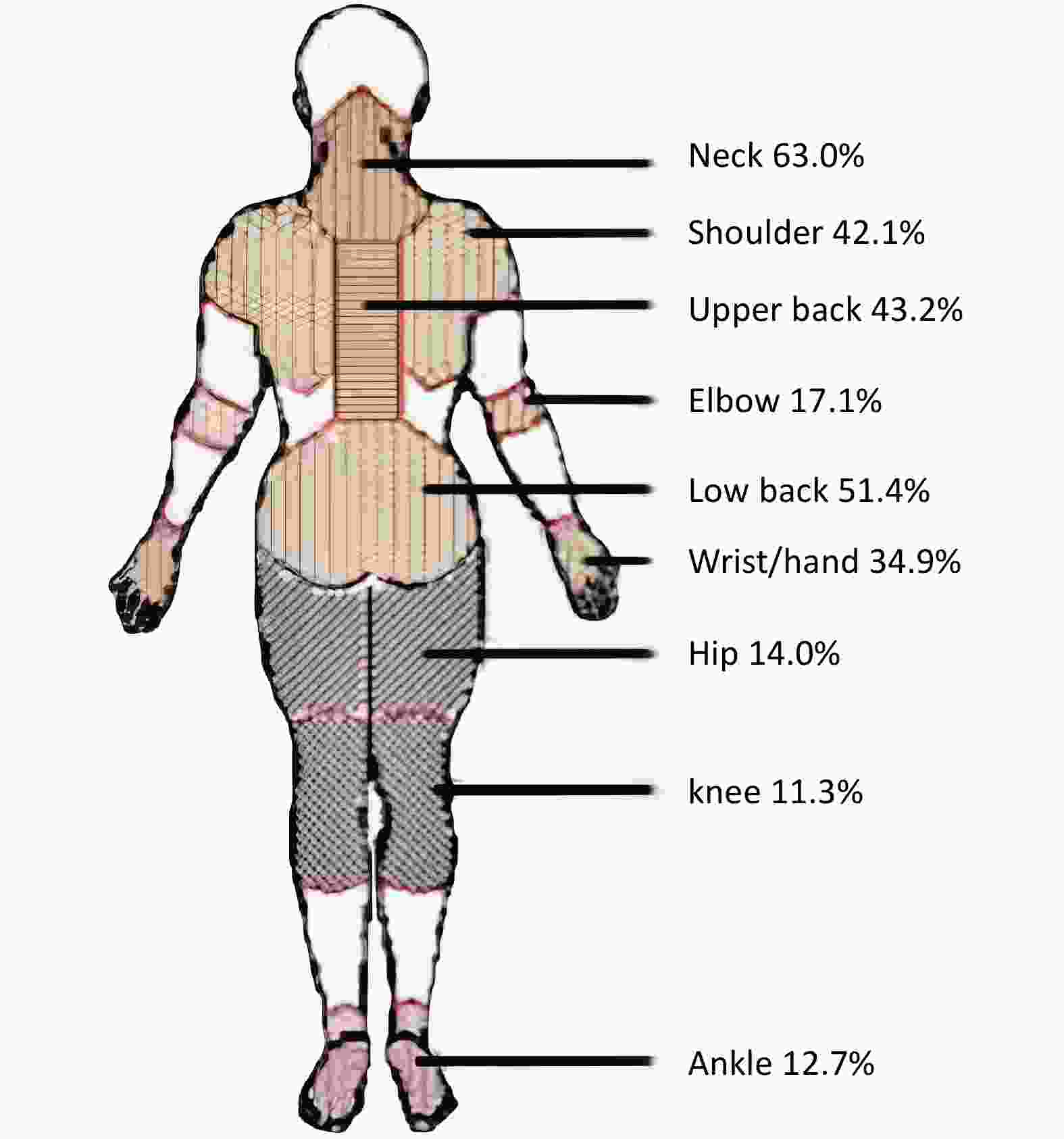
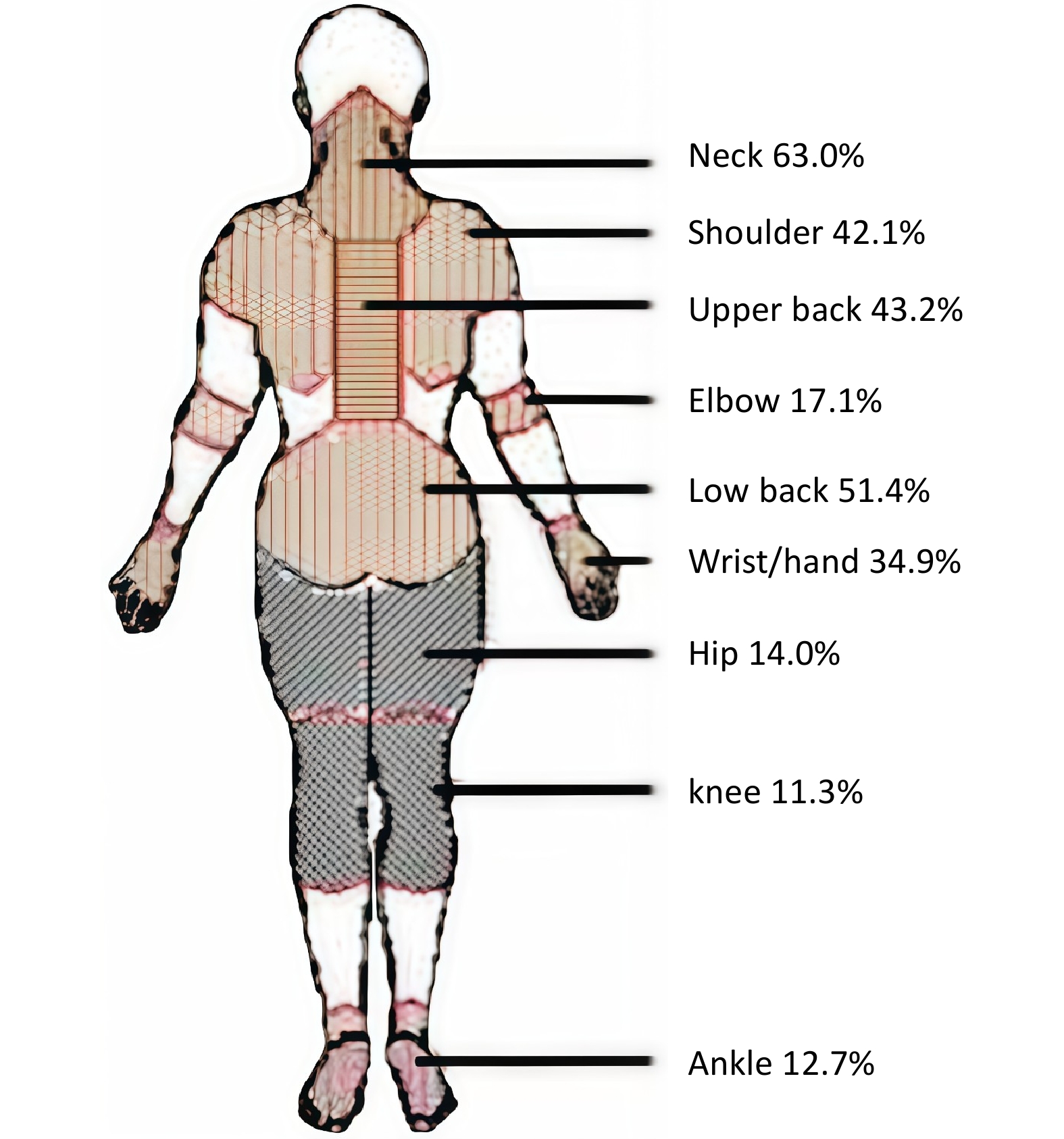
The Cronbach’s α values for personal characteristics, family function, job satisfaction, mental load, and WMSDs were 0.80, 0.79, 0.80, 0.73, and 0.90, respectively, indicating good internal consistency (Supplementary Table S1). Among the 292 participants who completed the questionnaire, 249 (85.3%) reported symptoms of WMSDs. Female dentists (54.8%) were slightly more than males (45.2%), with a higher prevalence of WMSDs among females (86.9%) than males (83.3%). Regarding professional specialization, 38.7% of the participants were physicians in oral medicine, 28.4% were oral surgeons, 21.6% were prosthodontists, and 11.3% were orthodontists. Among these groups, oral surgeons had the highest prevalence of WMSDs (88.0%). The largest age group among participants was those aged 30–40 years (34.2%), and the prevalence of WMSDs increased with age, with the highest prevalence (88.2%) observed in dentists aged > 50 years. Work experience and professional titles also tended to increase with age (Supplementary Table S2). Figure 1 illustrates the most frequently affected body region due to WMSDs. The most commonly reported areas of discomfort included the neck (63.0%), lower back (51.4%), upper back (43.2%), shoulders (42.1%), and wrists/hands (34.9%), while the hips, elbows, knees, and ankles were less frequently affected. The higher susceptibility of female dentists to WMSDs may be attributed to their smaller body size, lower muscle mass, and reduced aerobic capacity. The elevated prevalence among oral surgeons could be linked to the significant and sustained force required for procedures such as tooth extractions. Comparatively, studies on other professions in China have reported WMSD prevalence rates of 48.8% among radiologists, 55.6% among research technicians, 43.9% among workers in the chemical and pharmaceutical industries, and 20.8% among firefighters. These findings highlight the substantial burden of WMSDs on dentists, emphasizing the need for further attention to this occupational health concern.
The study model demonstrated an acceptable fit to the data (χ2/df = 2.643, GFI = 0.910, AGFI = 0.874, CFI = 0.916, and RMSEA = 0.075) (Supplementary Table S3). The final model, including direct paths between variables, is shown in Figure 2. Based on the path coefficient and related indices, five paths were statistically significant (P < 0.05). The direct, indirect, and total effects of each variable on WMSDs are detailed in Supplementary Table S1. Personal characteristics (β = 0.257, P < 0.05), mental load (β = 0.458, P < 0.05), and job satisfaction (β = 0.492, P < 0.05) had significant direct effects on WMSDs. Additionally, personal characteristics (β = 0.493, P < 0.05) and job satisfaction (β = 0.739, P < 0.05) directly influenced mental load. Both personal characteristics (β = 0.226, P < 0.05) and job satisfaction (β = 0.338, P < 0.05) also had indirect effects on WMSDs through mental load (Table 1). However, the influence of family function on WMSDs was not significant. The parameter estimates for the model are presented in Supplementary Table S4.
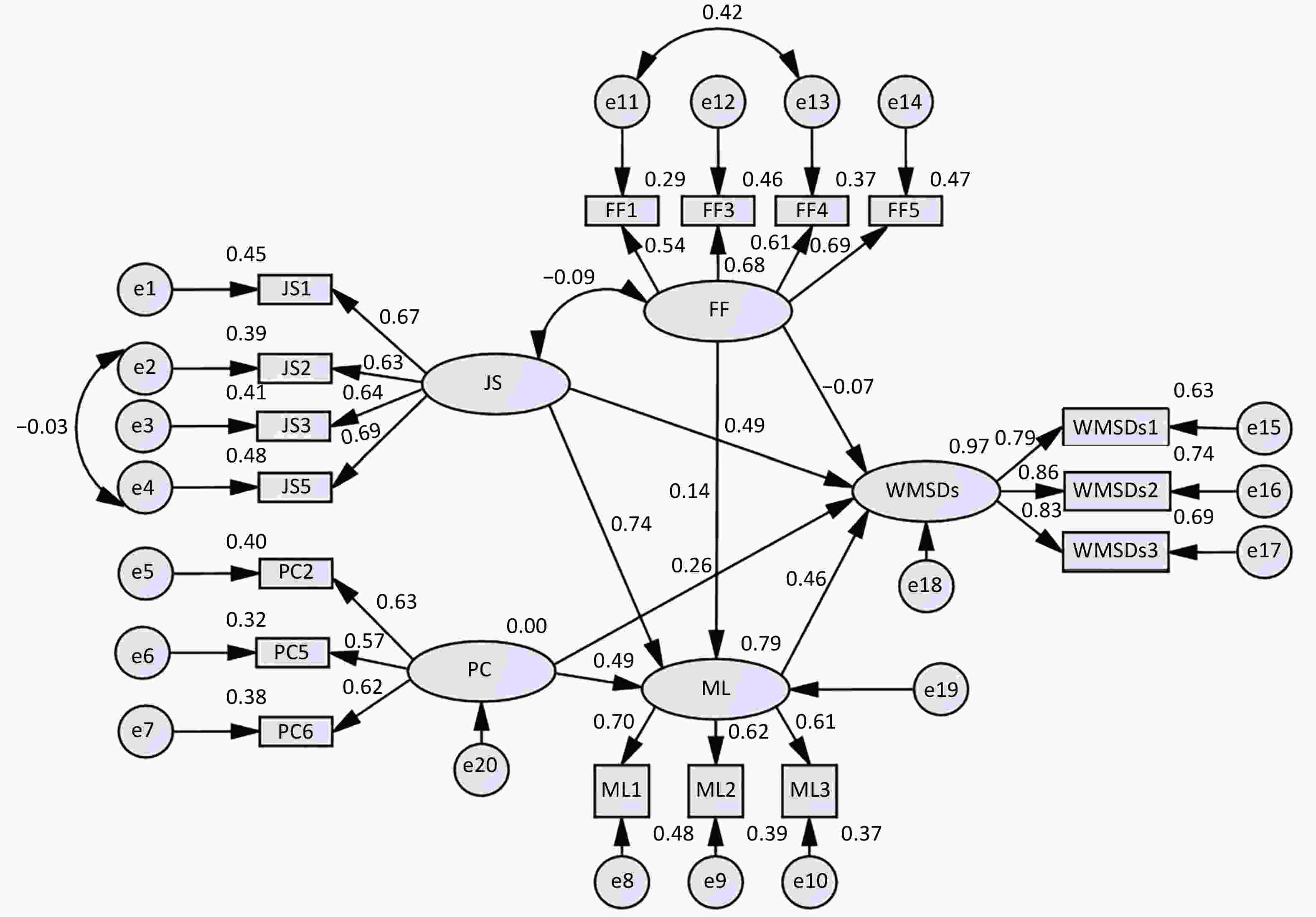
Figure 2. Structural equation model of factors influencing work-related musculoskeletal disorders among dentists.
Personal characteristics (β = 0.483, P < 0.05) had a significant positive impact on WMSDs. The final model identified age, the number of procedures per day, and smoking status as key factors associated with WMSDs. In general, the prevalence and severity of musculoskeletal disorders increase with age, which may be due to the natural decline in muscle mass caused by the atrophy or loss of muscle fibers. Muscle mass decreases by approximately 1% per year in middle-aged adults and can decline by up to 50% by the age of 80–90 years. Moreover, aging joints become increasingly susceptible to inflammation and other disorders[4]. Additionally, patients tend to prefer older doctors with more experience and higher professional titles, resulting in these older doctors treating more patients per day and working longer hours, which increases their risk of developing WMSDs. Furthermore, fatigue and repetitive postures in dentists may damage muscle ultrastructure, leading to further protein degradation, autophagy, and local inflammatory responses, which may further increase the burden on their musculoskeletal system[5]. Smoking is another contributing factor to WMSDs. Nicotine and other toxic substances in tobacco directly interfere with the activity of osteoblasts and osteoclasts in bone tissue while also indirectly affecting the metabolism of gonadal hormones, adrenocorticotropic hormone, and vitamin D. Moreover, substances such as nicotine in tobacco have vasoconstrictive properties that reduce blood flow and oxygen supply to the musculoskeletal system, leading to osteoporosis, delayed fracture healing, back pain, reduced protection of articular cartilage, higher risk of rheumatoid arthritis, and increased incidence of skeletal muscle pain[6].
Job satisfaction (β = 0.830, P < 0.05) had a significant positive impact on WMSDs. Prolonged exposure to an unsatisfactory work environment can lead to burnout, which may negatively affect work ethic, productivity, and job retention, increasing the risk of developing various health disorders[7]. Research suggests that physicians with higher job satisfaction have a lower risk of developing multiple systemic diseases, including musculoskeletal disorders[8]. Therefore, to reduce the burden of WMSDs among dentists, measures should be taken to improve job satisfaction of dentists, such as fostering a supportive work environment, offering competitive remuneration, and ensuring adequate opportunities for career advancement.
Mental load (β = 0.458, P < 0.05) had a significant positive effect on WMSDs. Research indicates that chronic psychological stress can trigger persistent inflammation, promoting osteoclast formation and bone resorption. Additionally, the resulting pro-oxidant microenvironment impairs the function of skeletal muscle mesenchymal stem cells, leading to adipogenesis, skeletal muscle steatosis, and chronic non-infectious diseases[9,10]. Overactivation of the sympathetic nervous system due to stress also negatively affects bone health. Furthermore, mental stress-induced behavioral changes, such as altered eating habits, alcohol abuse, and lack of physical activity, also pose a threat to the musculoskeletal system[9]. This present study demonstrated that mental load is essential in mediating the effects of personal characteristics and job satisfaction on WMSDs, highlighting the critical role of mental health in the overall wellbeing of dentists.
This study has some limitations. First, the relatively small sample size may have affected the accuracy of the findings. Second, the use of cluster sampling may have impacted the representativeness of the sample, limiting the generalizability of the results to dentists in other regions. Third, as a cross-sectional study, it did not establish causality, and longitudinal research is needed to validate effective interventions.
In conclusion, personal characteristics, job satisfaction, and mental load were found to impact WMSDs significantly. The burden of WMSDs among Chinese dentists is substantial, highlighting the need for health education initiatives to increase awareness of associated health risks. Additionally, appropriate public health policies should be implemented to enhance disease surveillance and prevention, addressing key risk factors to help reduce the prevalence of WMSDs among dentists.
Table 1. Standardized direct, indirect, and total effects in the final model
Path Standardized direct effect (β) Standardized indirect effect (β) Standardized Total effect (β) PC→ML 0.493* − 0.493* PC→WMSDs 0.257* 0.226* 0.483* JS→ML 0.739* − 0.739* JS→WMSDs 0.492* 0.338* 0.830* FF→ML 0.138 − 0.138 FF→WMSDs −0.075 0.063 −0.012 ML→WMSDs 0.458* − 0.458* Note. *P < 0.05; PC: personal characteristics; FF: family function; JS: job satisfaction; ML: mental load; WMSDs: work−related musculoskeletal disorders.
doi: 10.3967/bes2025.037
Factors in Work-Related Musculoskeletal Disorders in Dentists: A Structural Equation Model
-
Data collection and analysis and manuscript drafting: Shunhang Li and Yushan Huang. Data visualization: Xiaoshuang Xu, Yilin Zhang, and Weizhen Guan. Study design, manuscript revisions, financial support: Jian Li, Jing Li, Xiaoping Liu, and Xin Xu. Reading and approving the final manuscript: All authors.
The authors declared no competing interests.
This study was approved by the Ethical Review Committee of Shandong Second Medical University (2023YX066). Informed consent was obtained from all participants enrolled in the study.
&These authors contributed equally to this work.
注释:1) Authors’ Contributions: 2) Competing Interests: 3) Ethics: -
Figure 2. Structural equation model of factors influencing work-related musculoskeletal disorders among dentists.
Ovals represent latent variables. Rectangles represent observed variables. Circles represent residuals. The values between latent variables are standardized path coefficients. PC: personal characteristics, JS: job satisfaction, ML: mental load, FF: family function, WMSDs: work-related musculoskeletal disorders.
Table 1. Standardized direct, indirect, and total effects in the final model
Path Standardized direct effect (β) Standardized indirect effect (β) Standardized Total effect (β) PC→ML 0.493* − 0.493* PC→WMSDs 0.257* 0.226* 0.483* JS→ML 0.739* − 0.739* JS→WMSDs 0.492* 0.338* 0.830* FF→ML 0.138 − 0.138 FF→WMSDs −0.075 0.063 −0.012 ML→WMSDs 0.458* − 0.458* Note. *P < 0.05; PC: personal characteristics; FF: family function; JS: job satisfaction; ML: mental load; WMSDs: work−related musculoskeletal disorders. -
[1] Mulimani P, Hoe VCW, Hayes MJ, et al. Ergonomic interventions for preventing musculoskeletal disorders in dental care practitioners. Cochrane Database Syst Rev, 2018; 10, CD011261. [2] Feng BB, Liang Q, Wang YL, et al. Prevalence of work-related musculoskeletal symptoms of the neck and upper extremity among dentists in China. BMJ Open, 2014; 4, e006451. [3] Hayes MJ, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg, 2009; 7, 159−65. [4] Loeser RF. Age-related changes in the musculoskeletal system and the development of osteoarthritis. Clin Geriatr Med, 2010; 26, 371−86. [5] Hotfiel T, Freiwald J, Hoppe MW, et al. Advances in delayed-onset muscle soreness (DOMS): Part I: pathogenesis and diagnostics. Sportverletz Sportschaden, 2018; 32, 243−50. [6] Yoon V, Maalouf NM, Sakhaee K. The effects of smoking on bone metabolism. Osteoporo Int, 2012; 23, 2081−92. [7] Dreison KC, White DA, Bauer SM, et al. Integrating self-determination and job demands–resources theory in predicting mental health provider burnout. Adm Policy Ment Health, 2018; 45, 121−30. [8] Niewiadomska E, Łabuz-Roszak B, Pawłowski P, et al. The physical and mental well-being of medical doctors in the Silesian Voivodeship. Int J Environ Res Public Health, 2022; 19, 13410. [9] Ng JS, Chin KY. Potential mechanisms linking psychological stress to bone health. Int J Med Sci, 2021; 18, 604−14. [10] Rohleder N. Stress and inflammation–The need to address the gap in the transition between acute and chronic stress effects. Psychoneuroendocrinology, 2019; 105, 164−71. -
 24645+Supplementary Materials.pdf
24645+Supplementary Materials.pdf

-




 下载:
下载:





 Quick Links
Quick Links